Orodispersible Membranes from a Modified Coaxial Electrospinning for Fast Dissolution of Diclofenac Sodium
Abstract
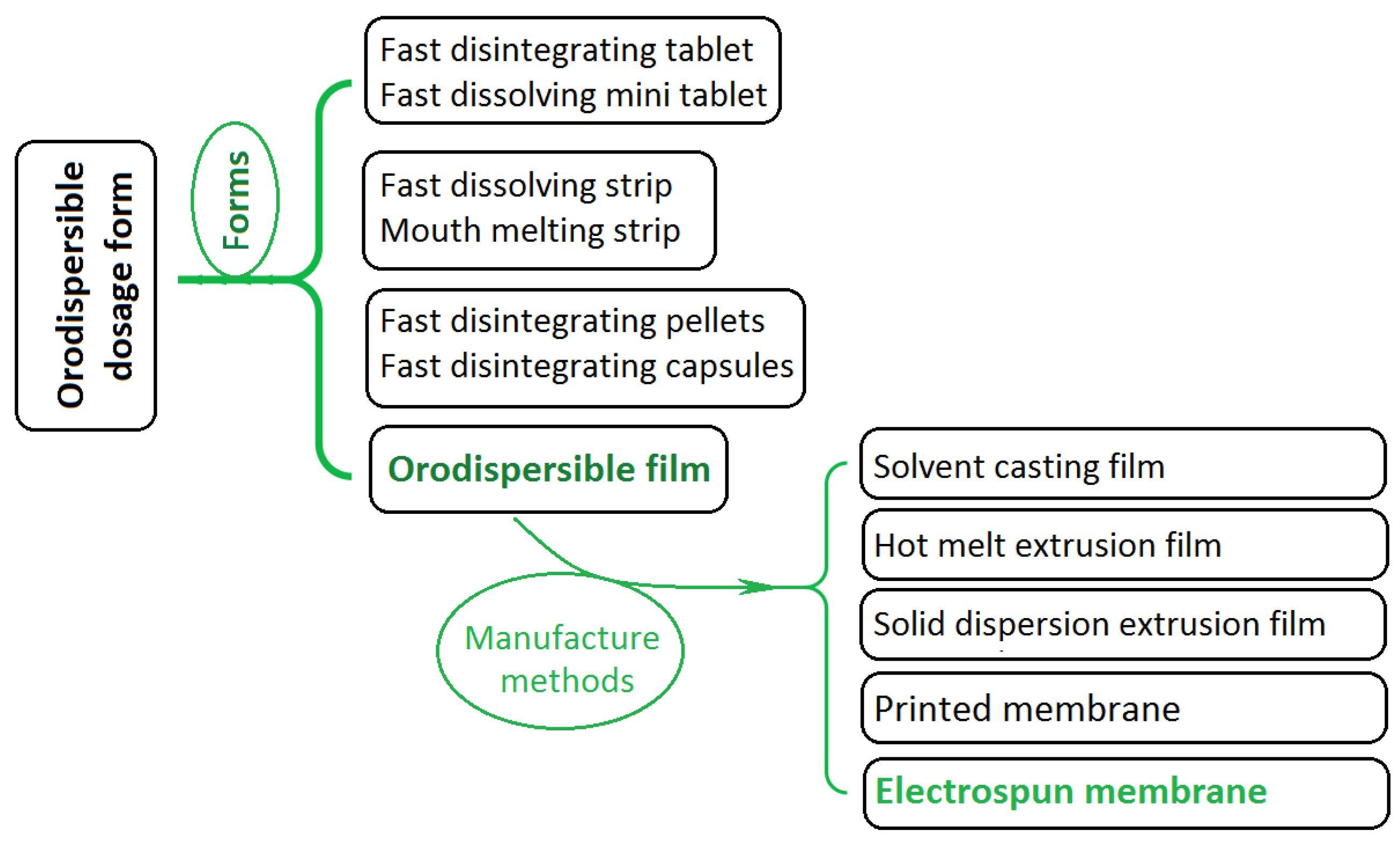
:1. Introduction
2. Experimental
2.1. Materials
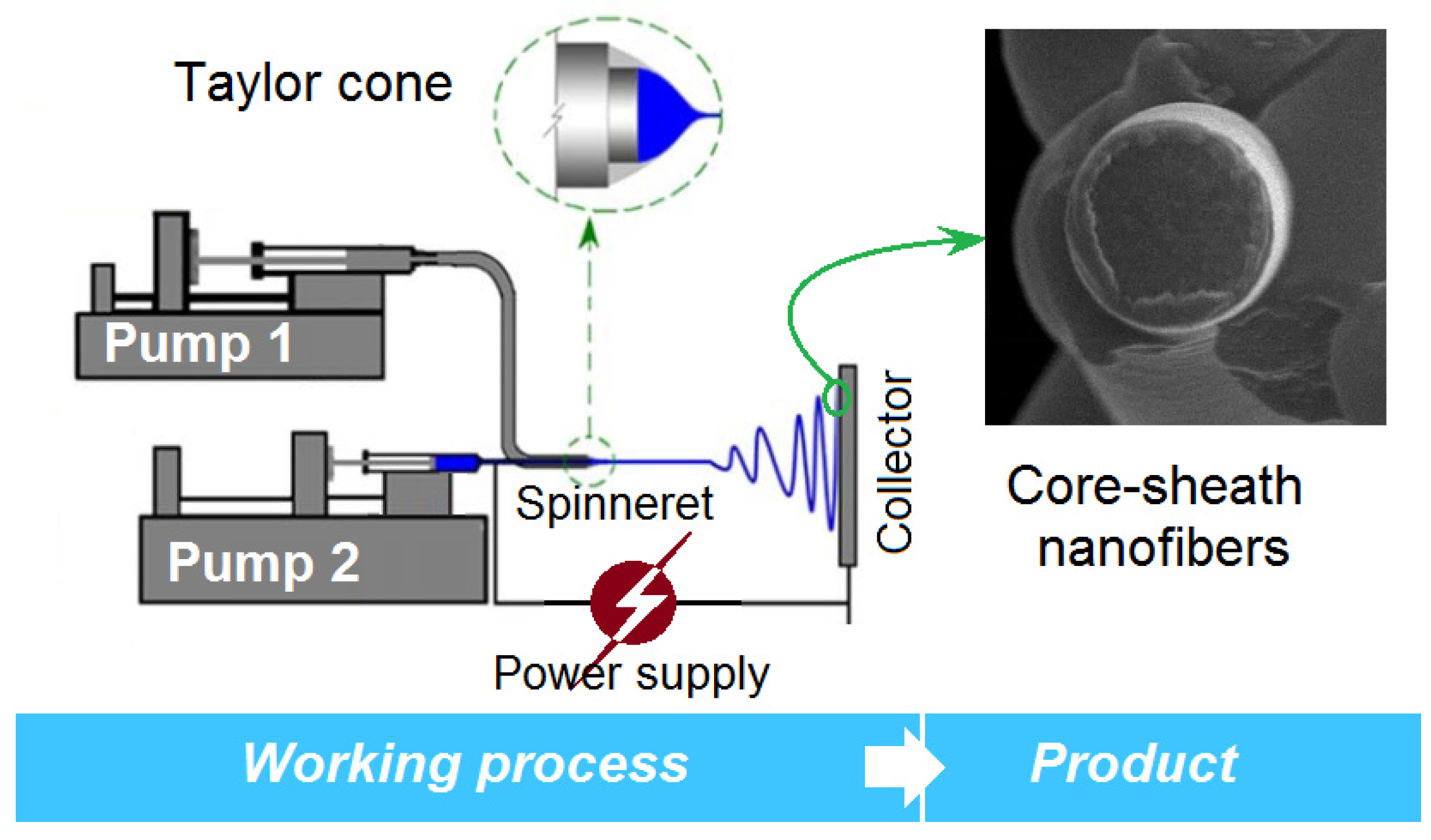
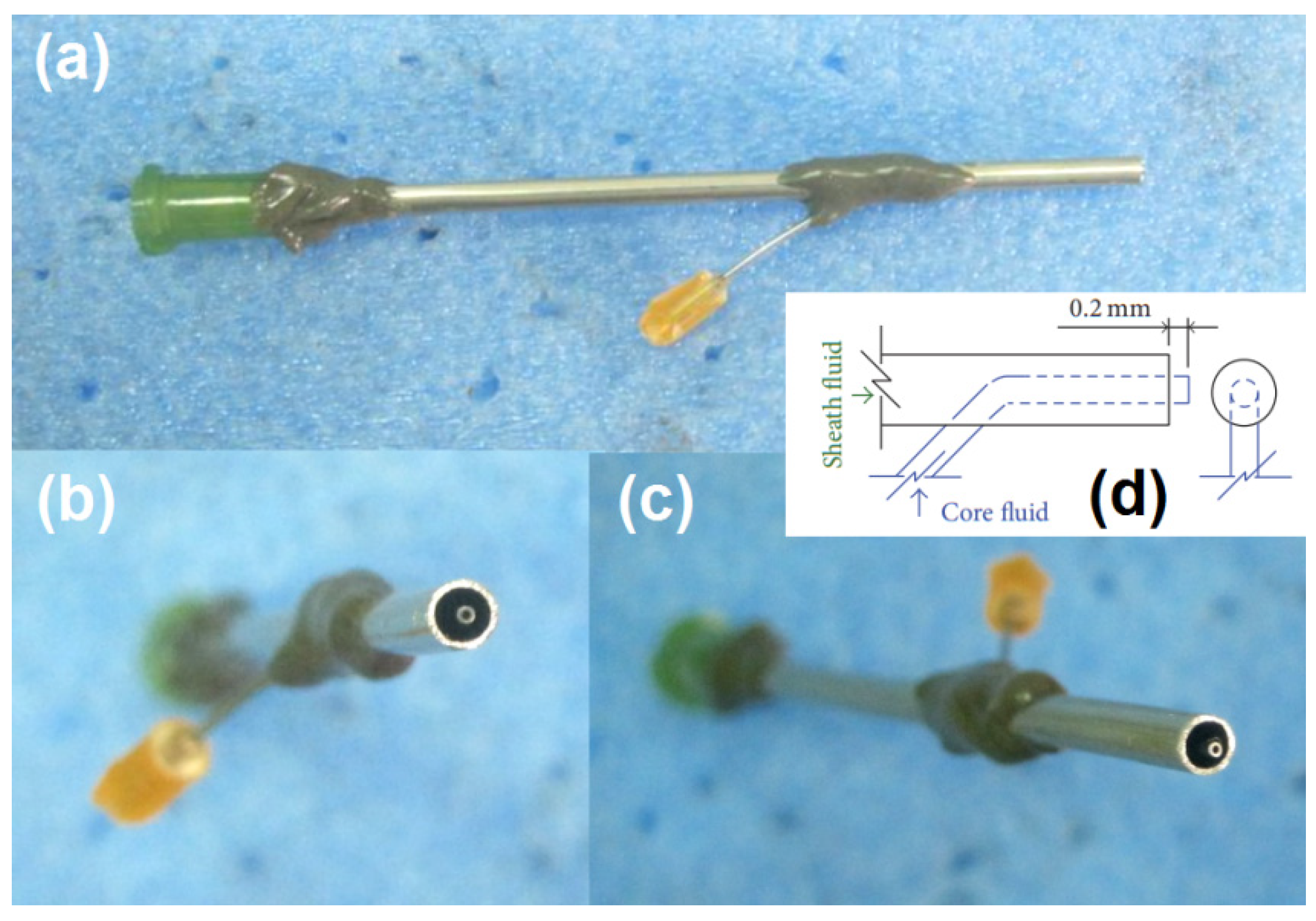
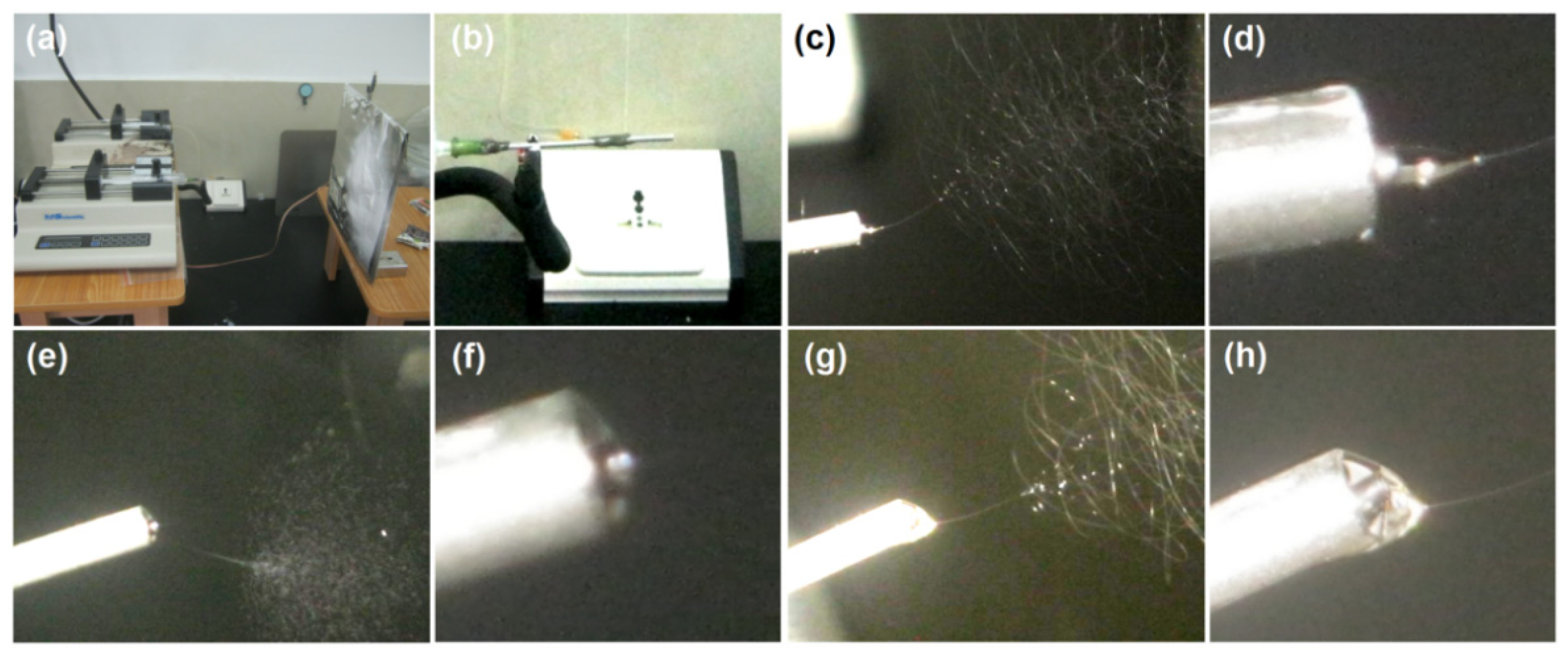
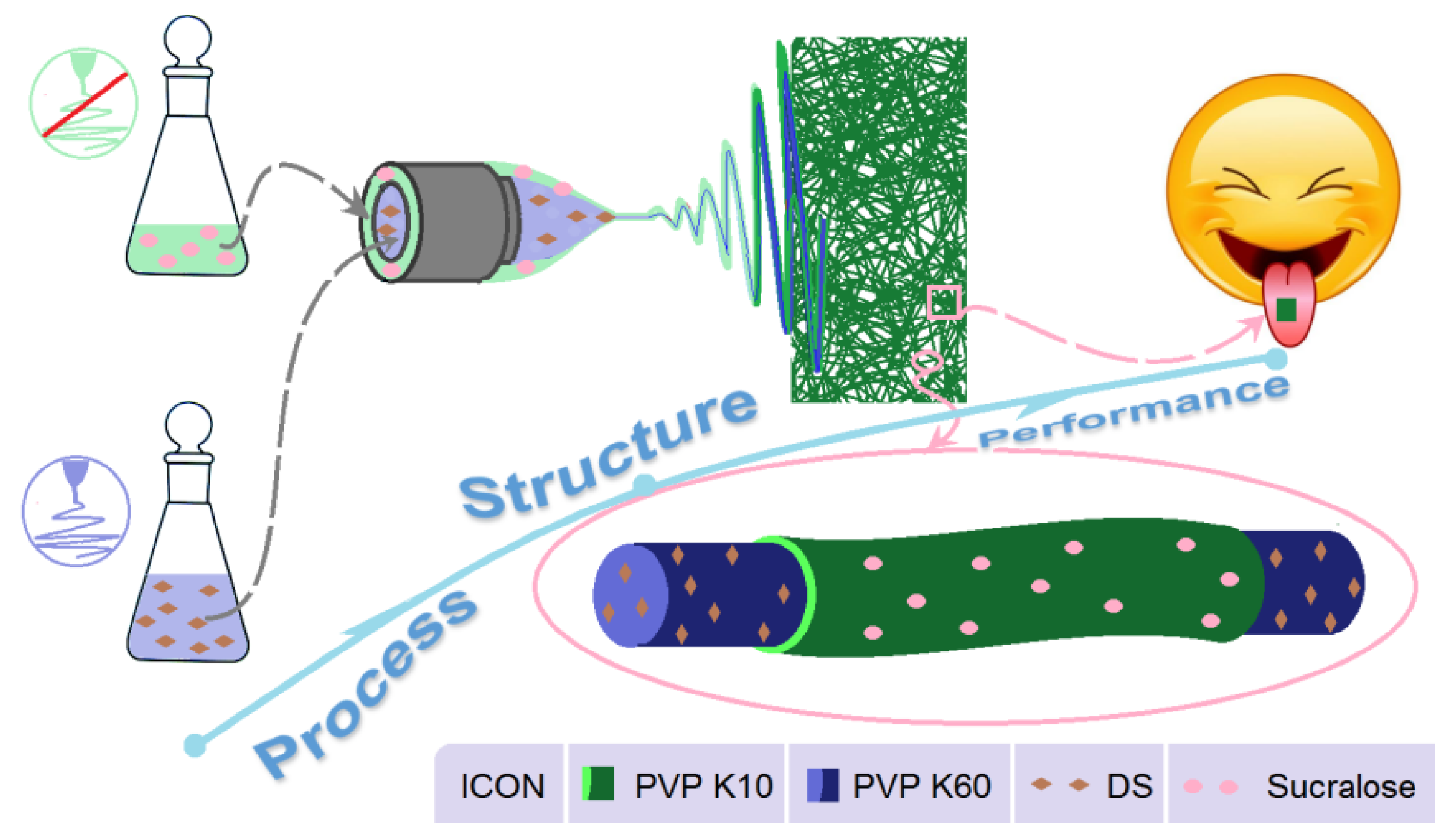
2.2. EHDA Processes
2.3. Characterizations
2.3.1. Morphologies and Structures
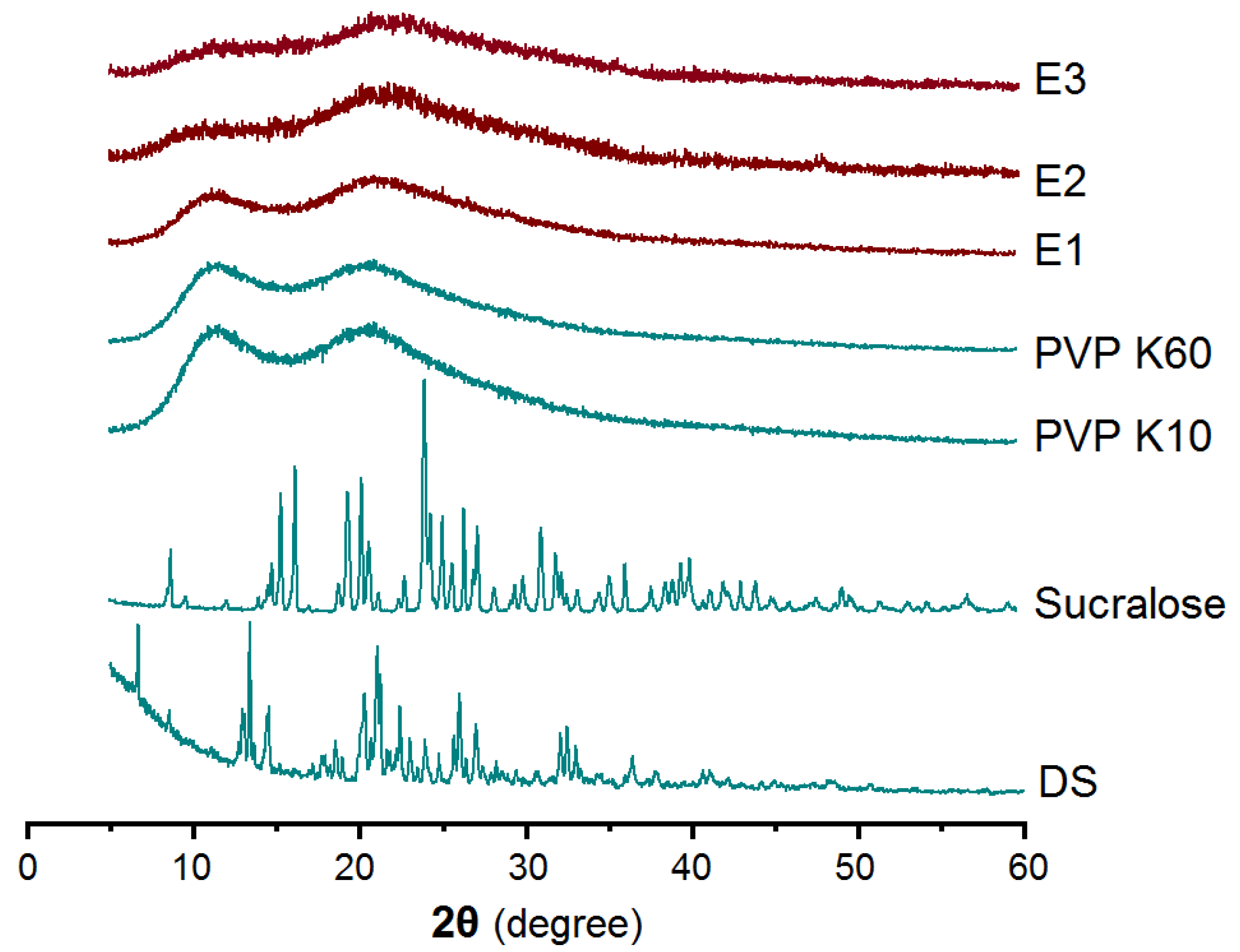
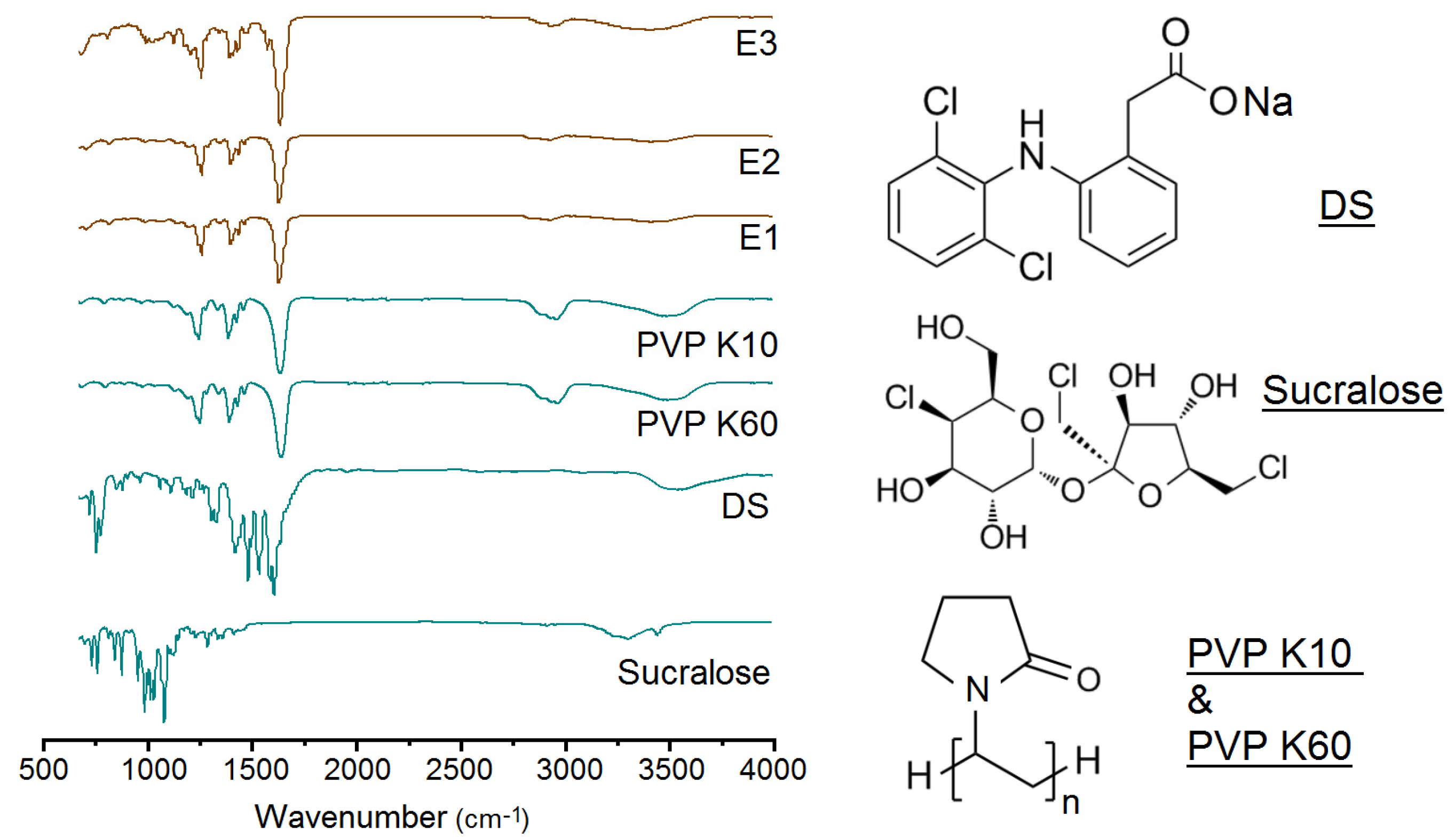
2.3.2. Physical State and Compatibility
2.4. Fast Dissolution Performances
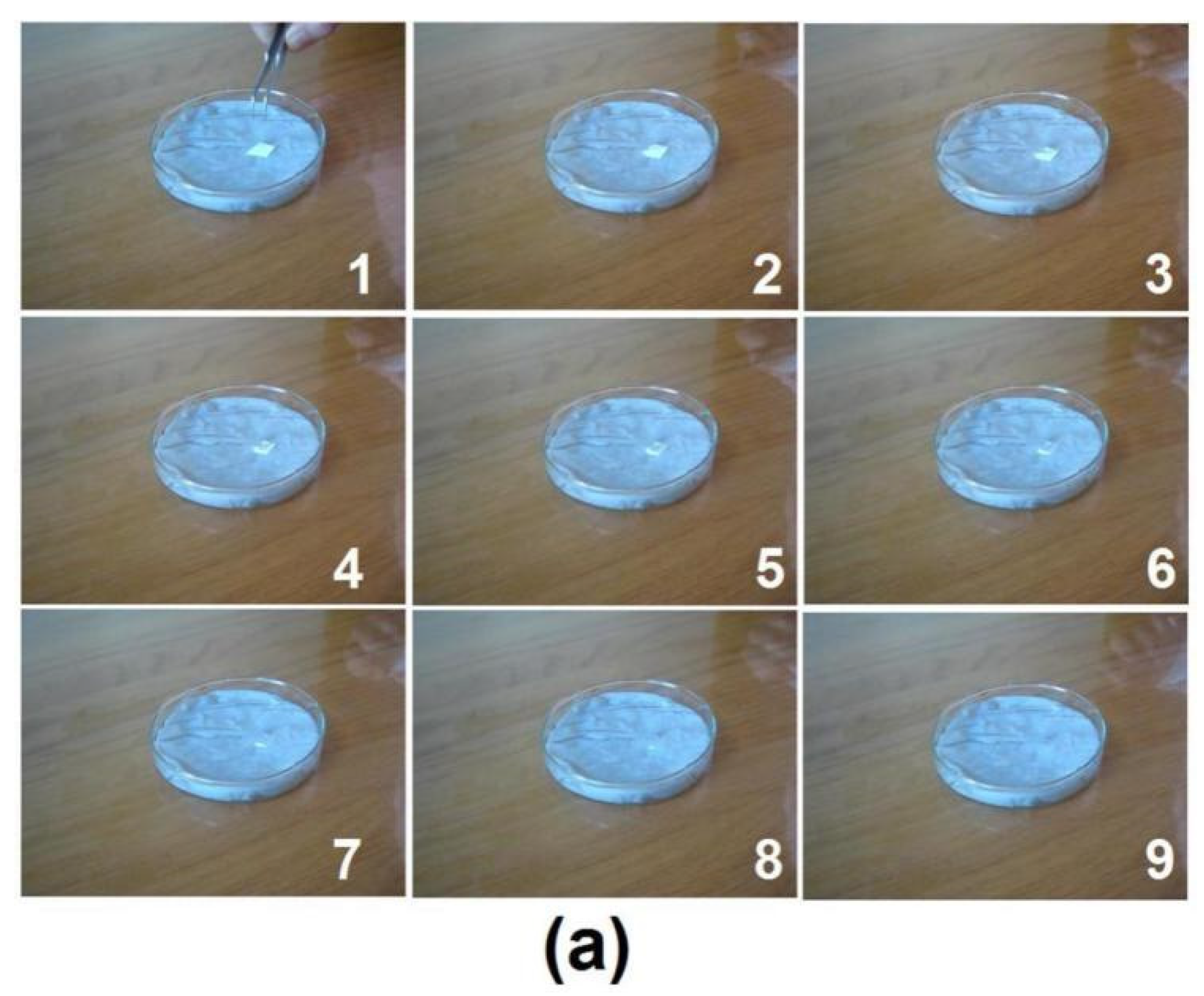
2.4.1. Fast Wetting Process
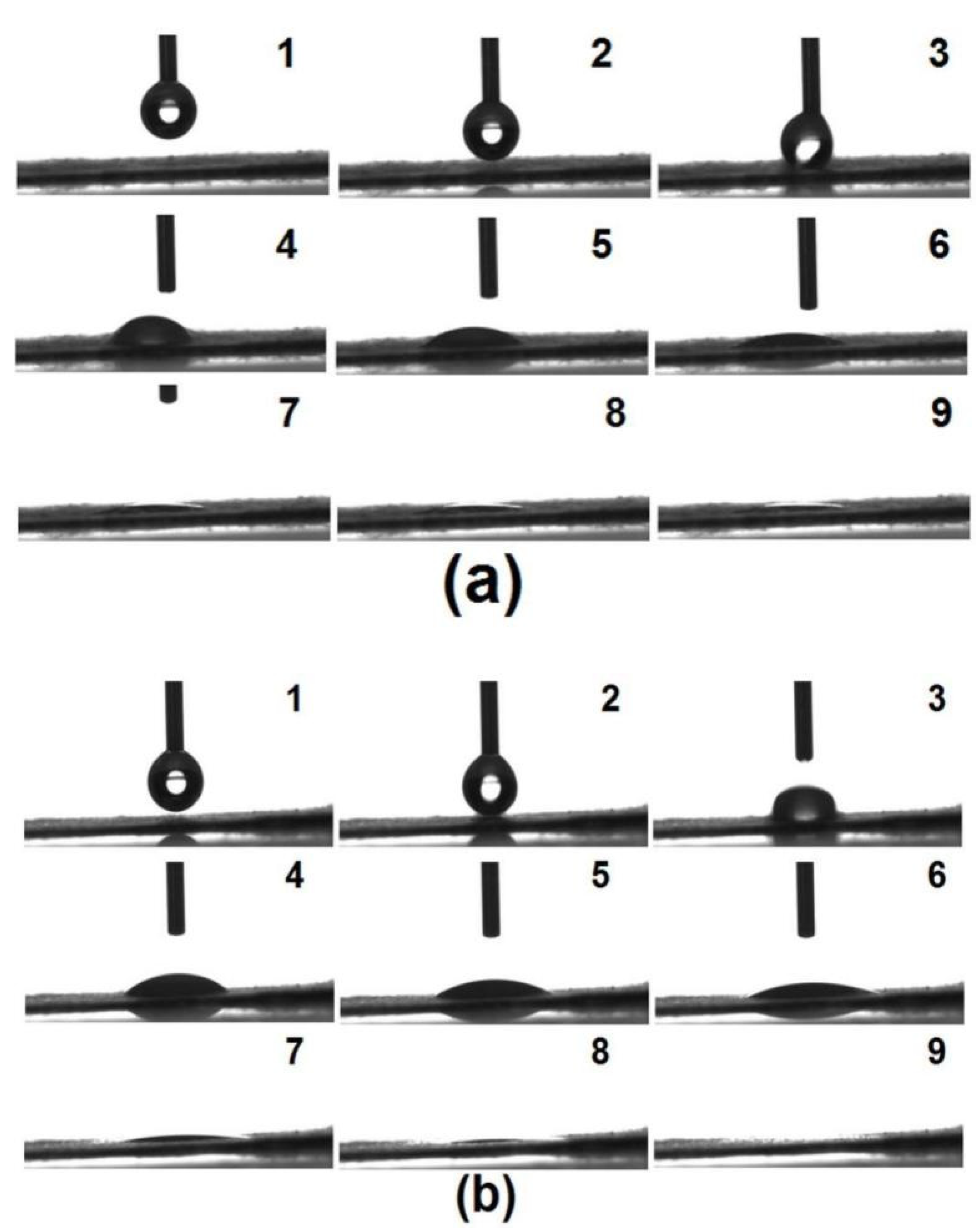
2.4.2. Drop Shape Analyses
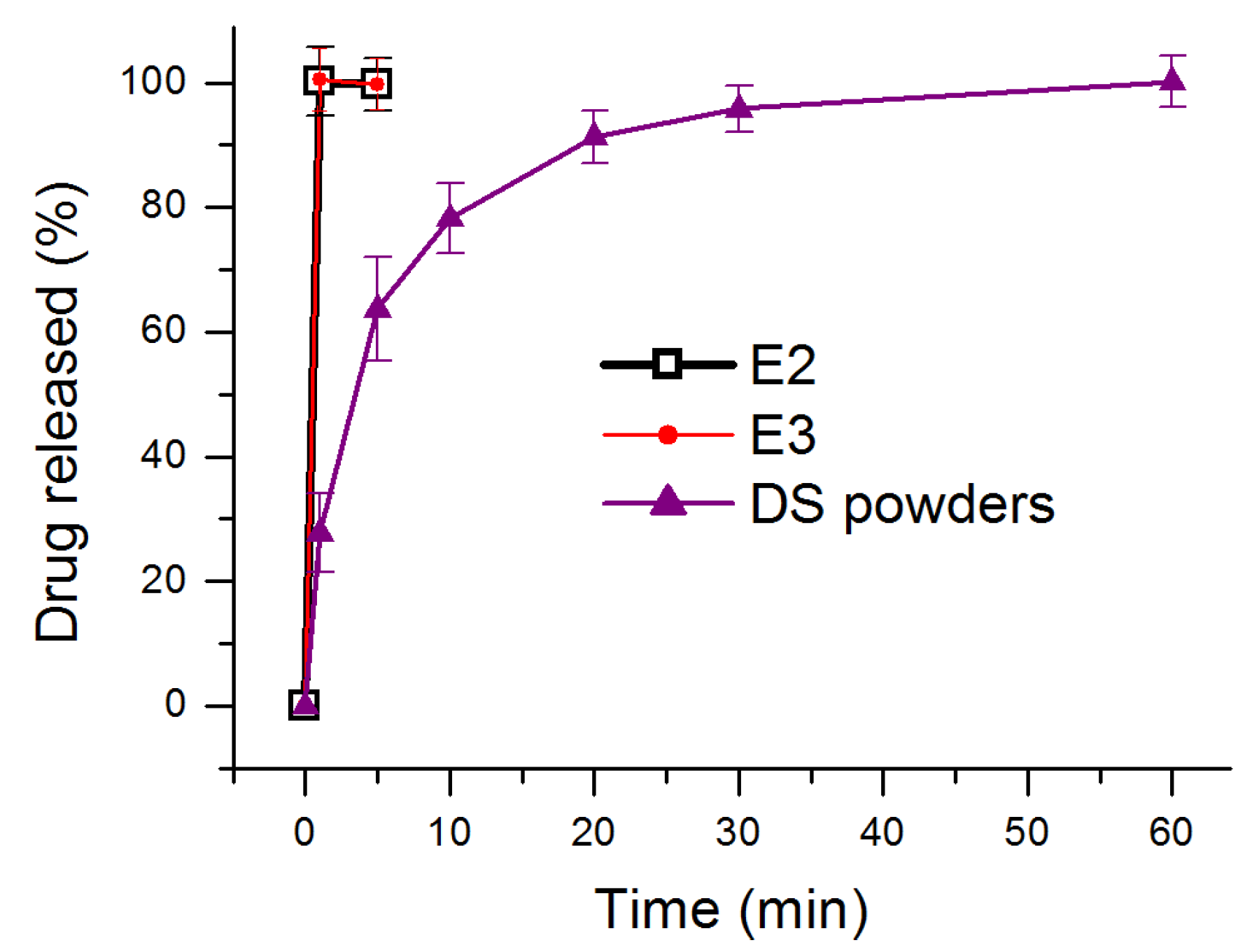
2.4.3. In Vitro Dissolution Tests
3. Results and Discussion
3.1. The EHDA Processes
3.2. Properties of the EHDA Products
3.3. Functional Performance of the EHDA Products
3.4. Strategy for Developing Medicated Membrane Using Modified Coaxial Electrospinning
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Zare, M.; Dziemidowicz, K.; Williams, G.R.; Ramakrishna, S. Encapsulation of pharmaceutical and nutraceutical active ingredients using electrospinning processes. Nanomaterials 2021, 11, 1968. [Google Scholar] [CrossRef]
- Sheikh, F.A.; Aamir, M.N.; Shah, M.A.; Ali, L.; Anwer, K.; Javaid, Z. Formulation design, characterization and in vitro drug release study of orodispersible film comprising BCS class II drugs. Pak. J. Pharm. Sci. 2020, 33, 343–353. [Google Scholar]
- Oh, B.C.; Jin, G.; Park, C.; Park, J.B.; Lee, B.J. Preparation and evaluation of identifiable quick response (QR)-coded orodispersible films using 3D printer with directly feeding nozzle. Int. J. Pharm. 2020, 584, 119405. [Google Scholar] [CrossRef]
- Olechno, K.; Basa, A.; Winnicka, K. Success depends on your backbone—About the use of polymers as essential materials forming orodispersible films. Materials 2021, 14, 4872. [Google Scholar] [CrossRef]
- Yu, D.G. Preface. Curr. Drug Deliv. 2021, 18, 2–3. [Google Scholar] [CrossRef]
- Liu, J.; Guan, J.; Wan, X.; Shang, R.; Shi, X.; Fang, L.; Liu, C. The improved cargo loading and physical stability of ibuprofen orodispersible film: Molecular mechanism of ion-pair complexes on drug-polymer miscibility. J. Pharm. Sci. 2020, 109, 1356–1364. [Google Scholar] [CrossRef]
- Visser, J.C.; Wibier, L.; Kiefer, O.; Orlu, M.; Breitkreutz, J.; Woerdenbag, H.J.; Taxis, K. A pediatrics utilization study in the Netherlands to identify active pharmaceutical ingredients suitable for inkjet printing on orodispersible films. Pharmaceutics 2020, 12, 164. [Google Scholar] [CrossRef] [Green Version]
- Sardesai, M.; Shende, P. Engineering of nanospheres dispersed microneedle system for antihypertensive action. Curr. Drug Deliv. 2020, 17, 776–786. [Google Scholar] [CrossRef]
- Hoffmann, A.; Fischer, J.T.; Daniels, R. Development of probiotic orodispersible tablets using mucoadhesive polymers for buccal mucoadhesion. Drug Dev. Ind. Pharm. 2020, 46, 1753–1762. [Google Scholar] [CrossRef]
- Kirtane, A.R.; Verma, M.; Karandikar, P.; Furin, J.; Langer, R.; Traverso, G. Nanotechnology approaches for global infectious diseases. Nat. Nanotechnol. 2021, 16, 369–384. [Google Scholar] [CrossRef]
- Deng, Y.P.; Shen, L.; Yang, Y.; Shen, J. Development of nanoparticle-based orodispersible palatable pediatric formulations. Int. J. Pharm. 2021, 596, 9. [Google Scholar] [CrossRef] [PubMed]
- Al-Jbour, N.D.; Beg, M.D.; Gimbun, J.; Alam, A.M. An overview of chitosan nanofibers and their applications in the drug delivery process. Curr. Drug Deliv. 2019, 16, 272–294. [Google Scholar] [CrossRef] [PubMed]
- Vlachou, M.; Kikionis, S.; Siamidi, A.; Tragou, K.; Kapoti, S.; Ioannou, E.; Roussis, V.; Tsotinis, A. Fabrication and characterization of electrospun nanofibers for the modified release of the chronobiotic hormone melatonin. Curr. Drug Deliv. 2019, 16, 79–85. [Google Scholar] [CrossRef]
- Padmakumar, S.; Menon, D. Nanofibrous polydioxanone depots for prolonged intraperitoneal paclitaxel delivery. Curr. Drug Deliv. 2019, 16, 654–662. [Google Scholar] [CrossRef]
- de Freitas Neto, J.L.; do Nascimento Gomes Barbosa, I.; de Melo, C.G.; Matheus Alves, Â.; dos Santos Mendes, L.M.; Ferreira, M.R.A.; Rolim, L.A.; Soares, L.A.L.; da Silva, R.M.F.; Neto, P.J.R. Development of pediatric orodispersible tablets based on efavirenz as a new therapeutic alternative. Curr. Hiv Res. 2020, 18, 342–353. [Google Scholar] [CrossRef] [PubMed]
- Ansari, M.R.; Unwan, M.; Ibrahim, N.A.S.; Ahmad, A.A.; Rahman, A.U.; Rehman, J.; Abbas, J. Formulation, evaluation and optimization of orodispersible tablets of naproxen sodium 250 mg by using various super disintegrant. Int. J. Life Sci. Pharm. Res. 2020, 10, 43–47. [Google Scholar]
- Lucendo, A.J.; Miehlke, S.; Schlag, C.; Vieth, M. Efficacy of budesonide orodispersible tablets as induction therapy for eosinophilic esophagitis in a randomized placebo-controlled trial. Gastroenterology 2019, 157, 74–85. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, T.A. Study the pharmacokinetics, pharmacodynamics and hepatoprotective activity of rosuvastatin from drug loaded lyophilized orodispersible tablets containing transfersomes nanoparticles. J. Drug Deliv. Sci. Tec. 2021, 63, 102489. [Google Scholar] [CrossRef]
- Oliveira, L.J.; Veiga, A.; Stofella, N.C.F.; Cunha, A.C.; Toledo, M.D.T.; Andreazza, I.F.; Murakami, F.S. Development and evaluation of orodispersible tablets containing ketoprofen. Curr. Drug Deliv. 2020, 17, 348–360. [Google Scholar] [CrossRef]
- Ortega, C.A.; Favier, L.S.; Cianchino, V.A.; Cifuente, D.A. New orodispersible mini tablets of enalapril maleate by direct compression for pediatric patients. Curr. Drug Deliv. 2020, 17, 505–510. [Google Scholar] [CrossRef]
- Deshpande, A.H.; Wasule, D.D. Formulation and evaluation of wax matrix fast dissolving mini-tablets of montelukast sodium. Asian J. Pharm. 2017, 11, S107–S112. [Google Scholar]
- Wasilewska, K.; Ciosek-Skibinska, P.; Lenik, J.; Srcic, S.; Basa, A.; Winnicka, K. Utilization of ethylcellulose microparticles with rupatadine fumarate in designing orodispersible minitablets with taste masking effect. Materials 2020, 13, 2715. [Google Scholar] [CrossRef]
- Gupta, S.; Kumar, T.P.; Gowda, D.V. Patent perspective on orodispersible films. Recent Pat. Drug Deliv. Formul. 2020, 14, 88–97. [Google Scholar] [CrossRef]
- Gupta, M.S.; Kumar, T.P.; Gowda, D.V. Orodispersible thin film: A new patient-centered innovation. J. Drug Deliv. Sci. Tec. 2020, 59, 10. [Google Scholar] [CrossRef]
- Abdelhakim, H.E.; Williams, G.R.; Craig, D.Q.M.; Orlu, M.; Tuleu, C. Human mouthfeel panel investigating the acceptability of electrospun and solvent cast orodispersible films. Int. J. Pharm. 2020, 585, 8. [Google Scholar] [CrossRef] [PubMed]
- Arora, U.; Thakkar, V.; Baldaniya, L.; Gohel, M.C. Fabrication and evaluation of fast disintegrating pellets of cilostazol. Drug Dev. Ind. Pharm. 2020, 46, 1927–1946. [Google Scholar] [CrossRef] [PubMed]
- Ciper, M.; Bodmeier, R. Modified conventional hard gelatin capsules as fast disintegrating dosage form in the oral cavity. Eur. J. Pharm. Biopharm. 2006, 62, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Selmin, F.; Khalid, G.M.; Musazzi, U.M.; Demartin, F.; Minghetti, P.; Cilurzo, F. Relevance of production method on the physical stability and in vitro biopharmaceutical performances of olanzapine orodispersible film. Int. J. Pharm. 2021, 603, 120697. [Google Scholar] [CrossRef]
- Cupone, I.E.; Dellera, E.; Marra, F.; Giori, A.M. Development and characterization of an orodispersible film for vitamin D3 supplementation. Molecules 2020, 25, 5851. [Google Scholar] [CrossRef]
- Barkat, U.; Latif, S.; Afzal, H.; Abbas, N.; Qamar, S.; Shamim, R.; Hussain, A. Development and characterization of taste masked orodispersible film of chlorpromazine hydrovhl oride. Acta Pol. Pharm. 2021, 78, 97–105. [Google Scholar]
- Visser, J.C.; Wibier, L.; Mekhaeil, M.; Woerdenbag, H.J.; Taxis, K. Orodispersible films as a personalized dosage form for nursing home residents, an exploratory study. Int. J. Clin. Pharm. 2020, 42, 436–444. [Google Scholar] [CrossRef] [Green Version]
- Lyszczarz, E.; Brniak, W.; Szafraniec-Szczęsny, J.; Majka, T.M.; Majda, D.; Zych, M.; Pielichowski, K.; Jachowicz, R. The impact of the preparation method on the properties of orodispersible films with aripiprazole: Electrospinning vs. casting and 3D printing methods. Pharmaceutics 2021, 13, 1122. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Cun, D.M.; Wan, F.; Bera, H.; Song, Q.C.; Tian, X.D.; Chen, Y.; Rantanen, J.; Yang, M.S. Comparative assessment of in vitro/in vivo performances of orodispersible electrospun and casting films containing rizatriptan benzoate. Eur. J. Pharm. Biopharm. 2020, 154, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Butreddy, A.; Nyavanandi, D.; Narala, S.; Austin, F.; Bandari, S. Application of hot melt extrusion technology in the development of abuse-deterrent formulations: An overview. Curr. Drug Deliv. 2021, 18, 4–18. [Google Scholar] [CrossRef] [PubMed]
- Suryawanshi, D.; Wavhule, P.; Shinde, U.; Kamble, M.; Amin, P. Development, optimization and in-vivo evaluation of cyanocobalamin loaded orodispersible films using hot-melt extrusion technology: A quality by design (QbD) approach. J. Drug Deliv. Sci. Tec. 2021, 63, 102559. [Google Scholar] [CrossRef]
- Cho, H.W.; Baek, S.H.; Lee, B.J.; Jin, H.E. Orodispersible polymer films with the poorly water-soluble drug, olanzapine: Hot-melt pneumatic extrusion for single-process 3D printing. Pharmaceutics 2020, 12, 692. [Google Scholar] [CrossRef]
- Lyszczarz, E.; Hofmanova, J.; Szafraniec-Szczesny, J.; Jachowicz, R. Orodispersible films containing ball milled aripiprazole-poloxamer (R) 407 solid dispersions. Int. J. Pharm. 2020, 575, 9. [Google Scholar] [CrossRef]
- Eduardo, D.T.; Ana, S.E.; Jose, B.F. A micro-extrusion 3D printing platform for fabrication of orodispersible printlets for pediatric use. Int. J. Pharm. 2021, 605, 12. [Google Scholar] [CrossRef]
- Gupta, M.S.; Kumar, T.P.; Davidson, R.; Kuppu, G.R.; Pathak, K.; Gowda, D.V. Printing methods in the production of orodispersible films. AAPS PharmSciTech 2021, 22, 17. [Google Scholar] [CrossRef]
- Elbl, J.; Gajdziok, J.; Kolarczyk, J. 3D printing of multilayered orodispersible films with in-process drying. Int. J. Pharm. 2020, 575, 8. [Google Scholar] [CrossRef]
- Turkovic, E.; Vasiljevic, I.; Draskovic, M.; Obradovic, N.; Vasiljevic, D.; Parojcic, J. An investigation into mechanical properties and printability of potential substrates for inkjet printing of orodispersible films. Pharmaceutics 2021, 13, 468. [Google Scholar] [CrossRef]
- Chachlioutaki, K.; Tzimtzimis, E.K.; Tzetzis, D.; Chang, M.W.; Ahmad, Z.; Karavasili, C.; Fatouros, D.G. Electrospun orodispersible films of isoniazid for pediatric tuberculosis treatment. Pharmaceutics 2020, 12, 470. [Google Scholar] [CrossRef]
- Musazzi, U.M.; Khalid, G.M.; Selmin, F.; Minghetti, P.; Cilurzo, F. Trends in the production methods of orodispersible films. Int. J. Pharm. 2020, 576, 10. [Google Scholar] [CrossRef]
- Yu, D.G.; Shen, X.X.; Branford-White, C.; White, K.; Zhu, L.M.; Bligh, S.W.A. Oral fast-dissolving drug delivery membranes prepared from electrospun polyvinylpyrrolidone ultrafine fibers. Nanotechnology 2009, 20, 055104. [Google Scholar] [CrossRef] [PubMed]
- Ramakrishnan, R.; Gimbun, J.; Ramakrishnan, P.; Ranganathan, B.; Reddy, S.M.M.; Shanmugam, G. Effect of solution properties and operating parameters on needleless electrospinning of poly (ethylene oxide) nanofibers loaded with bovine serum albumin. Curr. Drug Deliv. 2019, 16, 913–922. [Google Scholar] [CrossRef]
- Kang, S.; Hou, S.; Chen, X.; Yu, D.-G.; Wang, L.; Li, X.; Williams, G. Energy-saving electrospinning with a concentric Teflon-core rod spinneret to create medicated nanofibers. Polymers 2020, 12, 2421. [Google Scholar] [CrossRef] [PubMed]
- Zheng, G.; Peng, H.; Jiang, J.; Kang, G.; Liu, J.; Zheng, J.; Liu, Y. Surface functionalization of PEO nanofibers using a TiO2 suspension as sheath fluid in a modified coaxial electrospinning process. Chem. Res. Chin. Univ. 2021, 37, 571–577. [Google Scholar] [CrossRef]
- Wang, K.; Wen, H.-F.; Yu, D.G.; Yang, Y.; Zhang, D.F. Electrosprayed hydrophilic nanocomposites coated with shellac for colon-specific delayed drug delivery. Mater. Des. 2018, 143, 248–255. [Google Scholar] [CrossRef]
- Kang, S.; He, Y.; Yu, D.-G.; Li, W.; Wang, K. Drug–zein@lipid hybrid nanoparticles: Electrospraying preparation and drug extended release application. Colloid Surface B 2021, 201, 111629. [Google Scholar] [CrossRef]
- Hou, J.; Yang, Y.; Yu, D.G.; Chen, Z.; Wang, K.; Liu, Y.; Williams, G.R. Multifunctional fabrics finished using electrosprayed hybrid Janus particles containing nanocatalysts. Chem. Eng. J. 2021, 411, 128474. [Google Scholar] [CrossRef]
- Mofidfar, M.; Prausnitz, M.R. Electrospun transdermal patch for contraceptive hormone delivery. Curr. Drug Deliv. 2019, 16, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Mouro, C.; Fangueiro, R.; Gouveia, I.C. Preparation and characterization of electrospun double-layered nanocomposites membranes as a carrier for Centella asiatica (L.). Polymers 2020, 12, 2653. [Google Scholar] [CrossRef]
- Mehta, P.; Rasekh, M.; Patel, M.; Onaiwu, E.; Nazari, K.; Kucuk, I.; Wilson, P.B.; Arshad, M.S.; Ahmad, Z.; Chang, M.W. Recent applications of electrical, centrifugal, and pressurised emerging technologies for fibrous structure engineering in drug delivery, regenerative medicine and theranostics. Adv. Drug Deliv. Rev. 2021, 175, 113823. [Google Scholar] [CrossRef] [PubMed]
- Hajjari, M.M.; Golmakani, M.-T.; Sharif, N.; Niakousari, M. In-vitro and in-silico characterization of zein fiber incorporating cuminaldehyde. Food Bioprod. Process. 2021, 128, 166–176. [Google Scholar] [CrossRef]
- Wang, P.; Wang, M.L.; Wan, X.; Zhou, H.L.; Zhang, H.; Yu, D.G. Dual-stage release of ketoprofen from electrosprayed core-shell hybrid polyvinyl pyrrolidone/ethyl cellolose nanoparticles. Mater. Highlights 2020, 1, 14–21. [Google Scholar] [CrossRef]
- Celebioglu, A.; Uyar, T. Electrospun formulation of acyclovir/cyclodextrin nanofibers for fast-dissolving antiviral drug delivery. Mater. Sci. Eng. C 2021, 118, 111514. [Google Scholar] [CrossRef]
- Nagy, Z.K.; Nyul, K.; Wagner, I.; Molnar, K.; Marosi, G. Electrospun water soluble polymer mat for ultrafast release of Donepezil HCl. Express Polym. Lett. 2010, 4, 763–772. [Google Scholar] [CrossRef]
- Kwak, H.W.; Woo, H.; Kim, I.C.; Lee, K.H. Fish gelatin nanofibers prevent drug crystallization and enable ultrafast delivery. RSC Adv. 2017, 7, 40411–40417. [Google Scholar] [CrossRef] [Green Version]
- Szabo, E.; Zahonyi, P.; Brecska, D.; Galata, D.L.; Meszaros, L.A.; Madarasz, L.; Csorba, K.; Vass, P.; Hirsch, E.; Szafraniec-Szczesny, J.; et al. Comparison of amorphous solid dispersions of spironolactone prepared by spray drying and electrospinning: The influence of the preparation method on the dissolution properties. Mol. Pharm. 2021, 18, 317–327. [Google Scholar] [CrossRef]
- Ma, Y.D.; Guan, R.; Gao, S.Y.; Song, W.; Liu, Y.B.; Yang, Y.; Liu, H.Z. Designing orodispersible films containing everolimus for enhanced compliance and bioavailability. Expert Opin. Drug Del. 2020, 17, 1499–1508. [Google Scholar] [CrossRef]
- Balusamy, B.; Celebioglu, A.; Senthamizhan, A.; Uyar, T. Progress in the design and development of „fast-dissolving” electrospun nanofibers based drug delivery systems—A systematic review. J. Control. Release 2020, 326, 482–509. [Google Scholar] [CrossRef]
- Gupta, M.S.; Kumar, T.P. Characterization of orodispersible films: An overview of methods and introduction to a new disintegration test apparatus using LDR-LED sensors. J. Pharm. Sci. 2020, 109, 2925–2942. [Google Scholar] [CrossRef] [PubMed]
- Panhale, D.P.; Bachhav, R.S.; Gondkar, S.B. Formulation and evaluation of orodispersible tablets of apremilast by inclusion complexation using beta-cyclodextrin. Ind. J. Pharm. Edu. Res. 2021, 55, S112–S121. [Google Scholar] [CrossRef]
- Singh, S.; Mandal, S.; Verma, N. Formulation and evaluation of orodispersible tablets of ofloxacin by using different natural super disintegrating agents. Int. J. Pharm. Sci. Res. 2020, 11, 884–895. [Google Scholar]
- Song, Y.; Huang, H.; He, D.; Yang, M.; Wang, H.; Zhang, H.; Li, J.; Li, Y.; Wang, C. Gallic acid/2-hydroxypropyl-β-cyclodextrin inclusion complexes electrospun nanofibrous webs: Fast dissolution, improved aqueous solubility and antioxidant property of gallic acid. Chem. Res. Chin. Univ. 2021, 37, 450–455. [Google Scholar] [CrossRef]
- Wang, Y.; Tian, L.; Zhu, T.; Mei, J.; Chen, Z.; Yu, D.G. Electrospun aspirin/Eudragit/lipid hybrid nanofibers for colon-targeted delivery using an energy-saving process. Chem. Res. Chin. Univ. 2021, 37, 443–449. [Google Scholar] [CrossRef]
- Xu, H.; Xu, X.; Li, S.; Song, W.-L.; Yu, D.-G.; Annie Bligh, S.W. The effect of drug heterogeneous distributions within core-sheath nanostructures on its sustained release profiles. Biomolecules 2021, 11, 1330. [Google Scholar] [CrossRef]
- Zhao, K.; Lu, Z.H.; Zhao, P.; Kang, S.X.; Yang, Y.Y.; Yu, D.G. Modified tri-axial electrospun functional core-shell nanofibrous membranes for natural photodegradation of antibiotics. Chem. Eng. J. 2021, 425, 131455. [Google Scholar] [CrossRef]
- Li, D.; Wang, M.; Song, W.-L.; Yu, D.-G.; Annie-Bligh, S.W. Electrospun Janus beads-on-a-string structures for different types of controlled release profiles of double drugs. Biomolecules 2021, 11, 635. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Li, D.; Li, J.; Li, S.; Chen, Z.; Yu, D.-G.; Liu, Z.; Guo, J.Z. Electrospun Janus zein–PVP nanofibers provide a two-stage controlled release of poorly water-soluble drugs. Mater. Des. 2020, 196, 109075. [Google Scholar] [CrossRef]
- Ding, Y.; Dou, C.; Chang, S.; Xie, Z.; Yu, D.-G.; Liu, Y.; Shao, J. Core–shell Eudragit S100 nanofibers prepared via triaxial electrospinning to provide a colon-targeted extended drug release. Polymers 2020, 12, 2034. [Google Scholar] [CrossRef]
- Wang, M.; Hou, J.; Yu, D.-G.; Li, S.; Zhu, J.; Chen, Z. Electrospun tri-layer nanodepots for sustained release of acyclovir. J. Alloy. Compd. 2020, 846, 156471. [Google Scholar] [CrossRef]
- Aidana, Y.; Wang, Y.; Li, J.; Chang, S.; Wang, K.; Yu, D.-G. Fast dissolution electrospun medicated nanofibers for effective delivery of poorly water-soluble drugs. Curr. Drug Deliv. 2021, 18. [Google Scholar] [CrossRef]
- Ghosal, K.; Augustine, R.; Zaszczynska, A.; Barman, M.; Jain, A.; Hasan, A.; Kalarikkal, N.; Sajkiewicz, P.; Thomas, S. Novel drug delivery systems based on triaxial electrospinning based nanofibers. React. Funct. Polym. 2021, 163, 104895. [Google Scholar] [CrossRef]
- Mariyam, M.; Ghosal, K.; Thomas, S.; Kalarikkal, N.; Latha, M.S. Dendrimers: General aspects, applications and structural exploitations as prodrug/ drug-delivery vehicles in current medicine. Mini-Rev. Med. Chem. 2018, 18, 439–457. [Google Scholar] [CrossRef] [PubMed]
- Ghosal, K.; Adak, S.; Agatemor, C.; Praveen, G.; Thomas, S. Novel interpenetrating polymeric network based microbeads for delivery of poorly water soluble drug. J. Polym. Res. 2020, 27, 98. [Google Scholar] [CrossRef]
- Liu, X.; Xu, H.; Zhang, M.; Yu, D.-G. Electrospun medicated nanofibers for wound healing: Review. Membranes 2021, 11, 770. [Google Scholar] [CrossRef]
- Ghosal, K.; Hazra, B.; Bhowmik, B.; Thomas, S. Formulation development, physicochemical characterization and in vitro-in vivo drug release of vaginal films. Curr. HIV Res. 2016, 14, 295–306. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, X.; Yu, D.G.; Liu, H.; Liu, Y.; Liu, P. Electrospun PVP-core/PHBV-shell nanofibers to eliminate tailing off for an improved sustained release of curcumin. Mol. Pharm. 2021, 559. [Google Scholar] [CrossRef]
- Ren, G.; Zhang, J.; Xie, Y.; Liu, L.; Yu, Q.; Tian, Q. Research on equilibrium solubility and apparent octanol/water partition coefficient of diclofenac sodium (In Chinese). Drug Eval. Res. 2013, 36, 448–451. [Google Scholar]
- Sa’adon, S.; Ansari, M.N.M.; Razak, S.I.A.; Anand, J.S.; Nayan, N.H.M.; Ismail, A.E.; Khan, M.U.A.; Haider, A. Preparation and physicochemical characterization of a diclofenac sodium-dual layer polyvinyl alcohol patch. Polymers 2021, 13, 2459. [Google Scholar] [CrossRef] [PubMed]
- Wsoo, M.A.; Abd Razak, S.I.; Bohari, S.P.M.; Shahir, S.; Salihu, R.; Kadir, M.R.A.; Nayan, N.H.M. Vitamin D-3-loaded electrospun cellulose acetate/polycaprolactone nanofibers: Characterization, in-vitro drug release and cytotoxicity studies. Int. J. Biol. Macromol. 2021, 181, 82–98. [Google Scholar] [CrossRef] [PubMed]
- He, H.; Wu, M.; Zhu, J.; Yang, Y.; Ge, R.; Yu, D.G. Engineered spindles of little molecules around electrospun nanofibers for biphasic drug release. Adv. Fiber Mater. 2021, 3, 66. [Google Scholar]
- Singh, S.; Lohani, A.; Mishra, A.K.; Verma, A. Formulation and evaluation of carrot seed oil-based cosmetic emulsions. J. Cosmet. Laser 2019, 21, 99–107. [Google Scholar] [CrossRef] [PubMed]


| No. | Process | Applied Voltage (kV) | Pumping Rate (mL/h) | Morphology | |
|---|---|---|---|---|---|
| Sheath a | Core b | ||||
| E1 | 1-fluid electrospraying | 15 | 0.5 | -- | Microparticles |
| E2 | 1-fluid electrospinning | 15 | -- | 1.0 | Nanofibers |
| E3 | Coaxial electrospinning | 15 | 0.5 | 1.0 | Nanofibers |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ning, T.; Zhou, Y.; Xu, H.; Guo, S.; Wang, K.; Yu, D.-G. Orodispersible Membranes from a Modified Coaxial Electrospinning for Fast Dissolution of Diclofenac Sodium. Membranes 2021, 11, 802. https://doi.org/10.3390/membranes11110802
Ning T, Zhou Y, Xu H, Guo S, Wang K, Yu D-G. Orodispersible Membranes from a Modified Coaxial Electrospinning for Fast Dissolution of Diclofenac Sodium. Membranes. 2021; 11(11):802. https://doi.org/10.3390/membranes11110802
Chicago/Turabian StyleNing, Tingbao, Yangjian Zhou, Haixia Xu, Shiri Guo, Ke Wang, and Deng-Guang Yu. 2021. "Orodispersible Membranes from a Modified Coaxial Electrospinning for Fast Dissolution of Diclofenac Sodium" Membranes 11, no. 11: 802. https://doi.org/10.3390/membranes11110802






