Stability and Thrombogenicity Analysis of Collagen/Carbon Nanotube Nanocomposite Coatings Using a Reversible Microfluidic Device
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Dispersions and Coatings
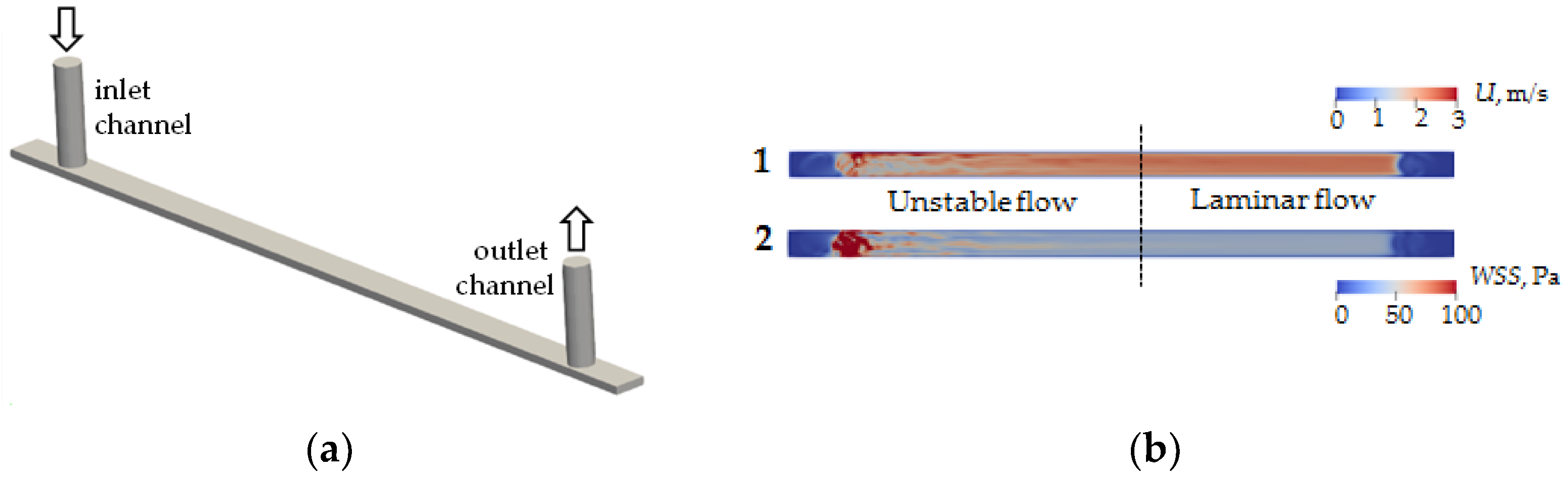
2.3. Microfluidic Device
2.4. Numerical Simulation Methodology
2.5. Investigation of the Resistance of Coatings to the Flow
2.6. Investigation of the Thrombogenicity of Coatings
3. Results and Discussion
3.1. Numerical Simulation
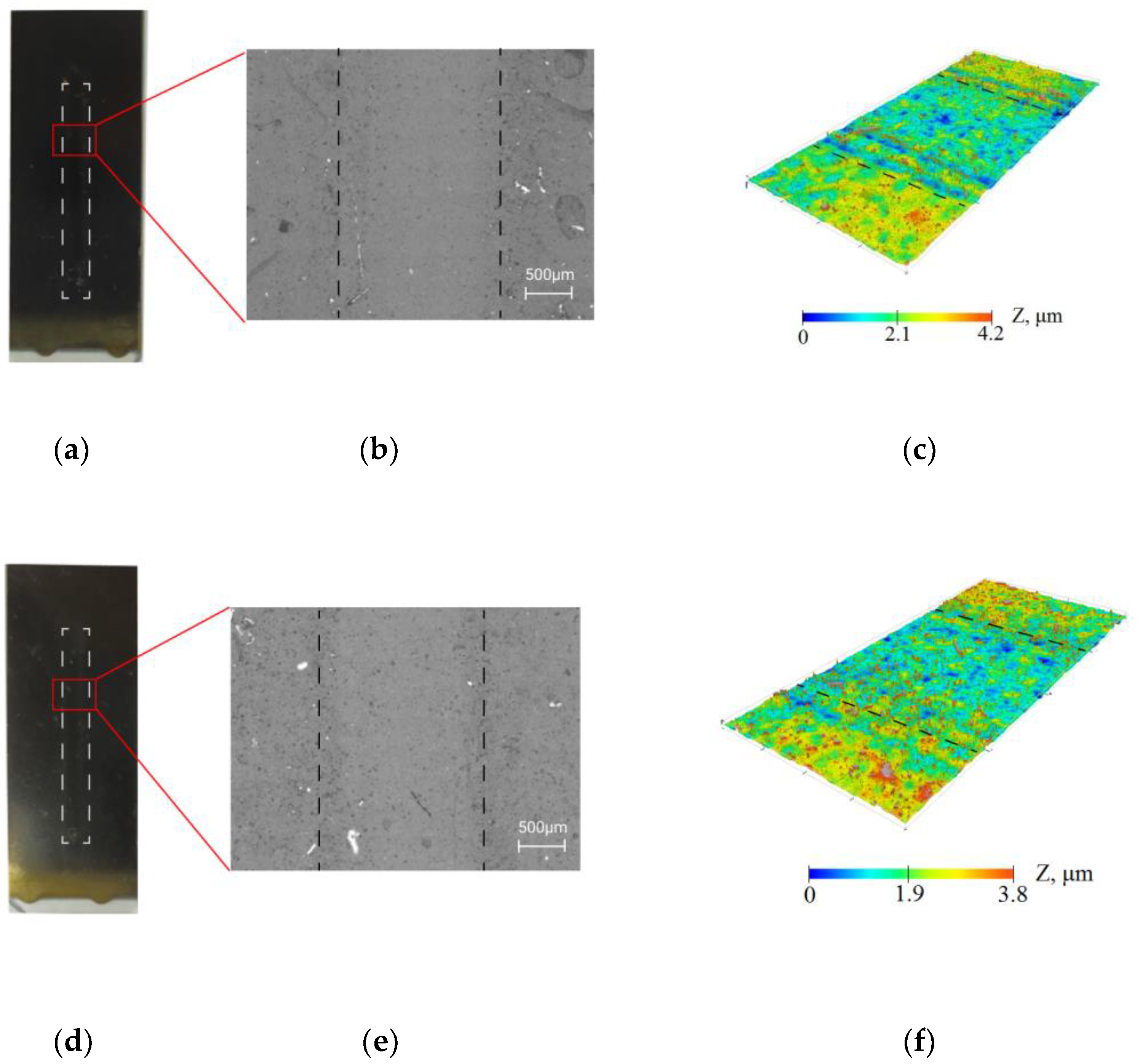
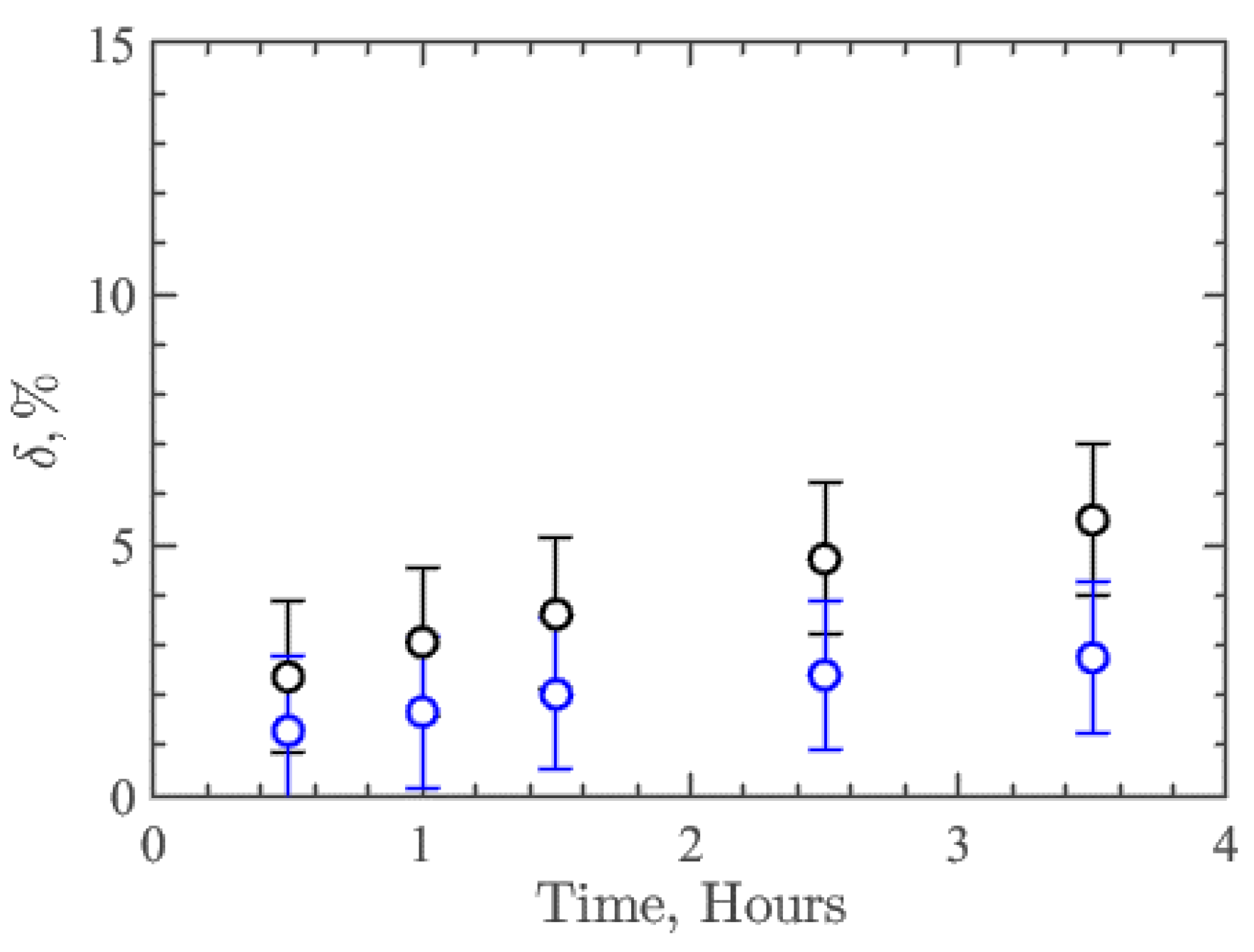
3.2. Resistance of Coatings under the Influence of the Flow
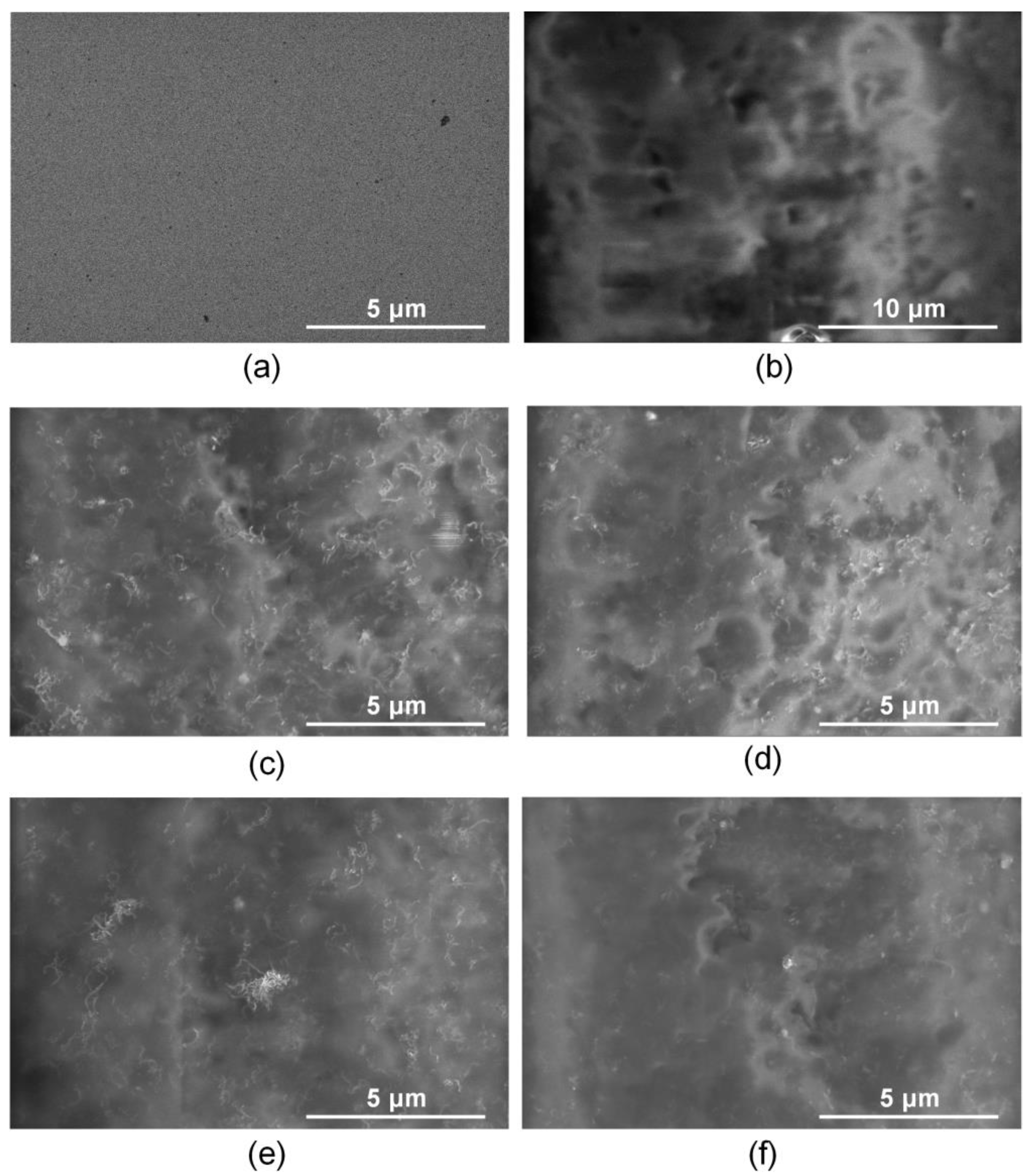
3.3. Thrombogenicity
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ghosh, P.; Azam, S.; Jonkman, M.; Karim, A.; Shamrat, F.J.M.; Ignatious, E.; Shultana, S.; Beeravolu, A.R.; De Boer, F. Efficient Prediction of Cardiovascular Disease Using Machine Learning Algorithms with Relief and LASSO Feature Selection Techniques. IEEE Access 2021, 9, 19304–19326. [Google Scholar] [CrossRef]
- Crespo-Leiro, M.G.; Metra, M.; Lund, L.H.; Milicic, D.; Costanzo, M.R.; Filippatos, G.; Gustafsson, F.; Tsui, S.; Barge-Caballero, E.; Jonge, N.; et al. Advanced heart failure: A position statement of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2018, 20, 1505–1535. [Google Scholar] [CrossRef] [PubMed]
- Habal, M.V.; Garan, A.R. Long-term Management of End-Stage Heart Failure. Best Pract. Res. Clin. Anaesthesiol. 2017, 31, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Telyshev, D.; Denisov, M.; Markov, A.; Fresiello, L.; Verbelen, T.; Selishchev, S. Energetics of Blood Flow in Fontan Circulation under VAD Support. Artif. Organs 2019, 44, 50–57. [Google Scholar] [CrossRef] [Green Version]
- Braune, S.; Latour, R.A.; Reinthaler, M.; Landmesser, U.; Lendlein, A. In Vitro Thrombogenicity Testing of Biomaterials. Adv. Healthc. Mater. 2019, 8, 1900527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zang, L.; Zhu, H.; Wang, K.; Liu, Y.; Yu, F.; Zhao, W. Not Just Anticoagulation—New and Old Applications of Heparin. Molecules 2022, 27, 6968. [Google Scholar] [CrossRef]
- Liu, X.; Yuan, L.; Li, D.; Tang, Z.; Wang, Y.; Chen, G.; Chen, H.; Brash, J.L. Blood Compatible Materials: State of the Art. J. Mater. Chem. B 2014, 2, 5718–5738. [Google Scholar] [CrossRef]
- Henkes, H.; Bhogal, P.; Pérez, M.A.; Lenz-Habijan, T.; Bannewitz, C.; Peters, M.; Sengstock, C.; Ganslandt, O.; Lylyk, P.; Monstadt, H. Anti-thrombogenic Coatings for Devices in Neurointerventional Surgery: Case Report and Review of the Literature. Interv. Neuroradiol. 2019, 25, 619–627. [Google Scholar] [CrossRef]
- Jin, Y.; Zhu, Z.; Liang, L.; Lan, K.; Zheng, Q.; Wang, Y.; Guo, Y.; Zhu, K.; Mehmood, R.; Wang, B. A Facile Heparin/carboxymethyl Chitosan Coating Mediated by Polydopamine on Implants for Hemocompatibility and Antibacterial Properties. Appl. Surf. Sci. 2020, 528, 146539. [Google Scholar] [CrossRef]
- Rahvar, M.; Lakalayeh, G.A.; Nazeri, N.; Karimi, R.; Borzouei, H.; Ghanbari, H. Micro/nanoscale Surface Engineering to Enhance Hemocompatibility and Reduce Bacterial Adhesion for Cardiovascular Implants. Mater. Chem. Phys. 2022, 289, 126445. [Google Scholar] [CrossRef]
- Shimazaki, T.; Miyamoto, H.; Ando, Y.; Noda, I.; Yonekura, Y.; Kawano, S.; Miyazaki, M.; Mawatari, M.; Hotokebuchi, T. In Vivo Antibacterial and Silver-Releasing Properties of Novel Thermal Sprayed Silver-Containing Hydroxyapatite Coating. J. Biomed. Mater. Res. Part B Appl. Biomater. 2009, 92, 386–389. [Google Scholar]
- Akhavan, O.; Ghaderi, E. Enhancement of Antibacterial Properties of Ag Nanorods by Electric Field. Sci. Technol. Adv. Mater. 2009, 10, 015003. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akhavan, O. Lasting Antibacterial Activities of Ag-TiO2/Ag/a-TiO2 Nanocomposite Thin Film Photocatalysts Under Solar Light Irradiation. J. Colloid Interface Sci. 2009, 336, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Pradhaban, G.; Kaliaraj, G.S.; Vishwakarma, V. Antibacterial Effects of Silver–Zirconia Composite Coatings Using Pulsed Laser Deposition onto 316L SS for Bio Implants. Prog. Biomater. 2014, 3, 123–130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gan, J.A.; Berndt, C.C. Nanocomposite Coatings: Thermal Spray Processing, Microstructure and Performance. Int. Mater. Rev. 2015, 60, 195–244. [Google Scholar] [CrossRef]
- Tan, X.Q.; Liu, J.Y.; Niu, J.R.; Liu, J.Y.; Tian, J.Y. Recent Progress in Magnetron Sputtering Technology Used on Fabrics. J. Mater. 2018, 11, 1953. [Google Scholar] [CrossRef] [Green Version]
- Danks, A.E.; Hall, S.R.; Schnepp, Z. The Evolution of ‘Sol–gel’ Chemistry as a Technique for Materials Synthesis. Mater. Horiz. 2016, 3, 91–112. [Google Scholar] [CrossRef] [Green Version]
- Priyadarshini, B.; Priyadarshini, B.; Murugupandian, R. Bioactive Coating as a Surface Modification Technique for Biocompatible Metallic Implants: A Review. J. Asian Ceram. Soc. 2019, 7, 397–406. [Google Scholar] [CrossRef] [Green Version]
- Yang, Z.; Hao, J. Progress in Pulsed Laser Deposited Two-dimensional Layered Materials for Device Applications. J. Mater. Chem. C 2016, 4, 8859–8878. [Google Scholar] [CrossRef] [Green Version]
- Jalilinejad, N.; Rabiee, M.; Baheiraei, N.; Ghahremanzadeh, R.; Salarian, R.; Rabiee, N.; Akhavan, O.; Zarrintaj, P.; Hejna, A.; Saeb, M.R.; et al. Electrically Conductive Carbon-Based (Bio)-Nanomaterials for Cardiac Tissue Engineering. Bioeng. Transl. Med. 2023, 8, e10347. [Google Scholar] [CrossRef]
- Teow, Y.H.; Mohammad, A.W.; Ang, W.L.; Lee, P.H. Development of Graphene Oxide (GO)/Multi-Walled Carbon Nanotubes (MWCNTs) Nanocomposite Conductive Membranes for Electrically Enhanced Fouling Mitigation. J. Membr. Sci. 2018, 552, 189–201. [Google Scholar]
- Gerasimenko, A.Y.; Kurilova, U.E.; Suetina, I.A.; Mezentseva, M.V.; Zubko, A.V.; Sekachev, M.; Glukhova, O.E. Laser Technology for the Formation of Bioelectronic Nanocomposites Based on Single-Walled Carbon Nanotubes and Proteins with Different Structures, Electrical Conductivity and Biocompatibility. Appl. Sci. 2021, 11, 8036. [Google Scholar] [CrossRef]
- Demidenko, N.A.; Kuksin, A.V.; Molodykh, V.V.; Pyankov, E.S.; Ichkitidze, L.P.; Zaborova, V.; Tsymbal, A.A.; Tkachenko, S.A.; Shafaei, H.; Diachkova, E.; et al. Flexible Strain-Sensitive Silicone-CNT Sensor for Human Motion Detection. Bioengineering 2022, 9, 36. [Google Scholar] [CrossRef] [PubMed]
- Simon, J.; Flahaut, E.; Golzio, M. Overview of Carbon Nanotubes for Biomedical Applications. J. Mater. 2019, 12, 624. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.W.; Kim, T.; Kim, Y.S.; Choi, S.H.; Lim, H.J.; Kim, Y.J.; Choi, S.Y. Surface Modifications for the Effective Dispersion of Carbon Nanotubes in Solvents and Polymers. Carbon 2012, 50, 3–33. [Google Scholar] [CrossRef]
- Negri, V.; Pacheco-Torres, J.; Calle, D.; López-Larrubia, P. Carbon Nanotubes in Biomedicine. In Topics in Current Chemistry Collections; Springer: Berlin/Heidelberg, Germany, 2020; p. 378. [Google Scholar]
- Zhou, L.; Forman, H.; Yi, G.; Lunec, G. Multi-Walled Carbon Nanotubes: A Cytotoxicity Study in Relation to Functionalization, Dose and Dispersion. Toxicol. Vitr. 2017, 42, 292–298. [Google Scholar] [CrossRef] [Green Version]
- Gerasimenko, A.; Ten, G.N.; Ryabkin, D.; Shcherbakova, N.E.; Morozova, E.; Ichkitidze, L.P. The Study of the Interaction Mechanism between Bovine Serum Albumin and Single-Walled Carbon Nanotubes Depending on Their Diameter and Concentration in Solid Nanocomposites by Vibrational Spectroscopy. Spectrochim. Acta—Part A Mol. Biomol. Spectrosc. 2019, 227, 117682. [Google Scholar] [CrossRef]
- Vakhrusheva, T.V.; Gusev, A.A.; Gusev, S.A.; Vlasova, I.I. Albumin Reduces Thrombogenic Potential of Single-walled Carbon Nanotubes. Toxicol. Lett. 2013, 221, 137–145. [Google Scholar] [CrossRef]
- Gerasimenko, A.Y.; Kitsyuk, E.; Kurilova, U.E.; Suetina, I.A.; Russu, L.; Mezentseva, M.V.; Markov, A.; Narovlyansky, A.N.; Kravchenko, S.; Selishchev, S.V.; et al. Interfaces Based on Laser-Structured Arrays of Carbon Nanotubes with Albumin for Electrical Stimulation of Heart Cell Growth. Polimers 2022, 14, 1866. [Google Scholar] [CrossRef]
- Gerasimenko, A.Y.; Kurilova, U.E.; Savelyev, M.S.; Murashko, D.; Glukhova, O.E. Laser Fabrication of Composite Layers from Biopolymers with Branched 3D Networks of Single-walled Carbon Nanotubes for Cardiovascular Implants. Compos. Struct. 2021, 260, 113517. [Google Scholar] [CrossRef]
- Gerasimenko, A.Y.; Zhurbina, N.N.; Cherepanova, N.G.; Semak, A.E.; Zar, V.V.; Fedorova, Y.O.; Eganova, E.M.; Pavlov, A.; Telyshev, D.; Selishchev, S.V.; et al. Frame Coating of Single-Walled Carbon Nanotubes in Collagen on PET Fibers for Artificial Joint Ligaments. Int. J. Mol. Sci. 2020, 21, 6163. [Google Scholar] [CrossRef] [PubMed]
- Primavera, R.; Razavi, M.; Kevadiya, B.D.; Wang, J.; Vykunta, A.; Mascolo, D.D.; Decuzzi, P.; Thakor, A.S. Enhancing Islet Transplantation Using a Biocompatible Collagen-PDMS Bioscaffold Enriched with Dexamethasone-Microplates. Biofabrication 2021, 13, 035011. [Google Scholar] [CrossRef]
- Zhang, D.; Wu, X.; Chen, J.; Lin, K. The Development of Collagen Based Composite Scaffolds for Bone Regeneration. Bioact. Mater. 2018, 3, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Tashakori-Miyanroudi, M.; Rakhshan, K.; Ramez, M.; Asgarian, S.; Janzadeh, A.; Azizi, A.; Seifalian, A.; Ramezani, F. Conductive Carbon Nanofibers Incorporated into Collagen Bio-scaffold Assists Myocardial Injury Repair. Int. J. Biol. Macromol. 2020, 163, 1136–1146. [Google Scholar] [CrossRef]
- Cherng, W.J.; Pan, Y.H.; Wu, T.C.; Chou, C.C.; Yeh, C.H.; Ho, J.J. Hemocompatibility and Adhesion of Heparin/Dopamine and Heparin/Collagen Self-assembly Multilayers Coated on a Titanium Substrate. Appl. Surf. Sci. 2019, 463, 732–740. [Google Scholar] [CrossRef]
- Mohan, C.C.; Chennazhi, K.P.; Menon, D. In Vitro Hemocompatibility and Vascular Endothelial Cell Functionality on Titania Nanostructures under Static and Dynamic Conditions for Improved Coronary Stenting Applications. Acta Biomater. 2013, 9, 9568–9577. [Google Scholar] [CrossRef] [PubMed]
- Fenech, M.; Girod, V.; Claveria, V.; Meance, S.; Abkarian, M.; Charlot, B. Microfluidic Blood Vasculature Replicas Using Backside Lithography. Lab Chip 2019, 19, 2096–2106. [Google Scholar] [CrossRef]
- Pinto, E.A.; Faustino, V.; Rodrigues, R.O.; Pinho, D.; Garcia, V.; Miranda, J.; Lima, R.A. Rapid and Low-cost Nonlithographic Method to Fabricate Biomedical Microdevices For Blood Flow Analysis. Micromachines 2014, 6, 121–135. [Google Scholar] [CrossRef] [Green Version]
- Wei, J.; Zhu, X.Y.; Chen, L.X.; Liu, J.; Hei, L.; Li, C.; Zhang, Y. Influence of Ion Source Pretreatment on WC Substrate Surface and Ta Buffer Coating. Cailiao Rechuli Xuebao/Trans. Mater. Heat Treat. 2015, 36, 164–168. [Google Scholar]
- Abdelaal, A.F.; Samad, M.A.; Adesina, A.Y.; Baig, M.M.A. Effect of Plasma Treatment on the Tribological and Adhesion Performance of a Polymer Coating Deposited on Different Metallic Substrates. J. Coat. Technol. Res. 2022, 19, 1673–1686. [Google Scholar] [CrossRef]
- Yang, F.; Xu, L.; Kuang, D.; Ge, Y.; Guo, G.; Wang, Y. Polyzwitterion-crosslinked Hybrid Tissue with Antithrombogenicity, Endothelialization, Anticalcification Properties. Chem. Eng. J. 2021, 410, 128244. [Google Scholar] [CrossRef]
- Bigi, A.; Cojazzi, G.; Panzavolta, S.; Rubini, K.; Roveri, N. Mechanical and Thermal Properties of Gelatin Films at Different Degrees of Glutaraldehyde Crosslinking. Biomaterials 2001, 22, 763–768. [Google Scholar] [CrossRef]
- Kim, S.; Ye, S.-h.; Adamo, A.; Orizondo, R.A.; Jo, J.; Cho, S.K.; Wagner, W.R. A Biostable, Anti-fouling Zwitterionic Polyurethane-Urea Based on PDMS for Use in Blood-Contacting Medical Devices. J. Mater. Chem. B 2020, 8, 8305–8314. [Google Scholar] [CrossRef] [PubMed]
- Fraser, K.H.; Zhang, T.; Taskin, M.E.; Griffith, B.P.; Wu, Z.J. A Quantitative Comparison of Mechanical Blood Damage Parameters in Rotary Ventricular Assist Devices: Shear Stress, Exposure Time and Hemolysis Index. J. Biomech. Eng. 2012, 134, 081002. [Google Scholar] [CrossRef]
- Papaioannou, T.G.; Stefanadis, C. Vascular Wall Shear Stress: Basic Principles and Methods. Hellenic. J. Cardiol. 2005, 46, 9–15. [Google Scholar]
- Pisapia, F.; Balachandran, W.; Rasekh, M. Organ-on-a-Chip: Design and Simulation of Various Microfluidic Channel Geometries for the Influence of Fluid Dynamic Parameters. Appl. Sci. 2022, 12, 3829. [Google Scholar] [CrossRef]
- Thamsen, B.; Blümel, B.; Schaller, J.; Paschereit, C.O.; Affeld, K.; Goubergrits, G.; Kertzscher, U. Numerical Analysis of Blood Damage Potential of the HeartMate II and HeartWare HVAD Rotary Blood Pumps. Artif. Organs 2015, 39, 651–659. [Google Scholar] [CrossRef] [PubMed]
- Bui, A.V.; Manasseh, R.; Liffman, K.; Sutalo, I.D. Development of Optimized Vascular Fractal Tree Models Using Level Set Distance Function. Med. Eng. Phys. 2010, 32, 790–794. [Google Scholar] [CrossRef]
- Regan-Smith, S.; Fritzen, R.; Hierons, S.J.; Ajjan, A.A.; Blindauer, C.A.; Stewart, A. Strategies for Therapeutic Amelioration of Aberrant Plasma Zn2+ Handling in Thrombotic Disease: Targeting Fatty Acid/Serum Albumin-Mediated Effects. Int. J. Mol. Sci. 2022, 23, 10302. [Google Scholar] [CrossRef]
- Liu, K.; Chen, J.; Zhang, K.; Wang, S.; Li, X. A Diagnostic Prediction Model of Acute Symptomatic Portal Vein Thrombosis. Ann. Vasc. Surg. 2019, 61, 394–399. [Google Scholar] [CrossRef]
- Milleret, M.; Buzzi, S.; Gehrig, P.; Ziogas, A.; Grossmannc, J.; Schilcher, K.; Zinkernagel, A.S.; Zucker, A.; Ehrbar, M. Protein Adsorption Steers Blood Contact Activation on Engineered Cobalt Chromium Alloy Oxide Layers. Acta Biomater. 2015, 24, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Bulwan, M.; Wojcik, K.; Zapotoczny, S.; Nowakowska, M. Chitosan-Based Ultrathin Films as Antifouling, Anticoagulant and Antibacterial Protective Coatings. Biomater. Sci. 2012, 23, 1963–1980. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Segade, S.; Rodriguez, J.; Mayan, D.; Camina, F. Plasma Albumin Concentration Is a Predictor of HbA1c Among Type 2 Diabetic Patients, Independently of Fasting Plasma Glucose and Fructosamine. Diabetes Care 2005, 28, 437–439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shadiow, J.A.; Tarumi, T.; Dhindsa, M.; Hunter, S.D. Comparison of Blood Viscosity and Hematocrit Levels between Yoga Practitioners and Sedentary Adults. Int. J. Exerc. Sci. 2019, 12, 425. [Google Scholar] [CrossRef] [PubMed]
- Hirsh, S.L.; McKenzie, D.R.; Nosworthy, N.J.; Denman, J.A.; Sezerman, O.U.; Bilek, M.M.M. The Vroman Effect: Competitive Protein Exchange with Dynamic Multilayer Protein Aggregates. Colloids Surf. B Biointerfaces 2013, 103, 395–404. [Google Scholar] [CrossRef]
- De Mel, A.; Cousins, B.G.; Seifalian, A.M. Surface Modification of Biomaterials: A Quest for Blood Compatibility. Int. J. Biomater. 2012, 2012, 707863. [Google Scholar] [CrossRef]
- Brash, J.L.; Horbett, T.A.; Latour, R.A.; Tengvall, T. The Blood Compatibility Challenge. Part 2: Protein Adsorption Phenomena Governing Blood Reactivity. Acta Biomater. 2019, 94, 11–24. [Google Scholar] [CrossRef]
- Nevídalová, N.; Michalcová, L.; Glatz, Z. Applicability of Capillary Electrophoresis-Frontal Analysis for Displacement Studies: Effect of Several Drugs on l-tryptophan and Lidocaine Binding to Human Serum Albumin. J. Sep. Sci. 2020, 43, 4225–4233. [Google Scholar] [CrossRef]
- Kalbac, M.; Hsieh, Y.P.; Farhat, H.; Kavan, L.; Hofmann, M.; Kong, J.; Dresselhaus, M.S. Defects in Individual Semiconducting Single Wall Carbon Nanotubes: Raman Spectroscopic and in Situ Raman Spectroelectrochemical Study. Nano Lett. 2010, 10, 4619–4626. [Google Scholar] [CrossRef]
- Dresselhaus, M.S.; Dresselhaus, G.; Saito, R.; Jorio, A. Raman Spectroscopy of Carbon Nanotubes. Phys. Rep. 2005, 409, 47–99. [Google Scholar] [CrossRef]
- Ramos, S.C.; Vasconcelos, G.; Antunes, E.F.; Lobo, A.O.; Trava-Airoldi, V.J.; Corat, E.J. Wettability Control on Vertically-Aligned Multi-Walled Carbon Nanotube Surfaces with Oxygen Pulsed DC Plasma and CO2 Laser Treatments. Diam. Relat. Mater. 2010, 19, 752–755. [Google Scholar] [CrossRef]


| Chemical Elements | Titanium Surface (wt.%) | Coating Collagen/c-MWCNT (wt.%) | Coating Collagen/c-MWCNT/Glutaraldehyde (wt.%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Before | After | Difference | Before | After | Difference | Before | After | Difference | |
| Ti | 23.96 | 12.44 | −11.52 | 12.02 | 10.76 | −1.26 | 11.74 | 9.35 | −2.39 |
| C | - | 3.02 | 3.02 | 18.36 | 16.18 | −2.18 | 16.53 | 13.18 | −3.35 |
| N | 2.62 | 13.95 | 11.33 | 1.23 | 4.68 | 3.45 | 1.78 | 8.65 | 6.87 |
| O | 8.09 | 12.37 | 4.28 | 9.47 | 11.98 | 2.51 | 15.69 | 18.92 | 3.23 |
| Na | - | 0.41 | 0.41 | 0.11 | 0.26 | 0.15 | 0.09 | 0.37 | 0.28 |
| P | - | 0.07 | 0.07 | - | 0.05 | 0.05 | - | 1.12 | 1.12 |
| S | - | 1.16 | 1.16 | 0.16 | 1.17 | 1.17 | 0.12 | 1.39 | 1.27 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popovich, K.D.; Vagner, S.A.; Murashko, D.T.; Ten, G.N.; Ryabkin, D.I.; Savelyev, M.S.; Kitsyuk, E.P.; Gerasimenko, E.A.; Edelbekova, P.; Konovalov, A.N.; et al. Stability and Thrombogenicity Analysis of Collagen/Carbon Nanotube Nanocomposite Coatings Using a Reversible Microfluidic Device. Membranes 2023, 13, 403. https://doi.org/10.3390/membranes13040403
Popovich KD, Vagner SA, Murashko DT, Ten GN, Ryabkin DI, Savelyev MS, Kitsyuk EP, Gerasimenko EA, Edelbekova P, Konovalov AN, et al. Stability and Thrombogenicity Analysis of Collagen/Carbon Nanotube Nanocomposite Coatings Using a Reversible Microfluidic Device. Membranes. 2023; 13(4):403. https://doi.org/10.3390/membranes13040403
Chicago/Turabian StylePopovich, Kristina D., Sergey A. Vagner, Denis T. Murashko, Galina N. Ten, Dmitry I. Ryabkin, Mikhail S. Savelyev, Evgeny P. Kitsyuk, Ekaterina A. Gerasimenko, Polina Edelbekova, Anton N. Konovalov, and et al. 2023. "Stability and Thrombogenicity Analysis of Collagen/Carbon Nanotube Nanocomposite Coatings Using a Reversible Microfluidic Device" Membranes 13, no. 4: 403. https://doi.org/10.3390/membranes13040403








