Aggression, Impulsivity and Suicidal Behavior in Depressive Disorders: A Comparison Study between New York City (US), Madrid (Spain) and Florence (Italy)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Statistics
3. Results
3.1. Characteristics of the Samples
3.2. Differences in Aggression and Impulsivity Levels across Sites
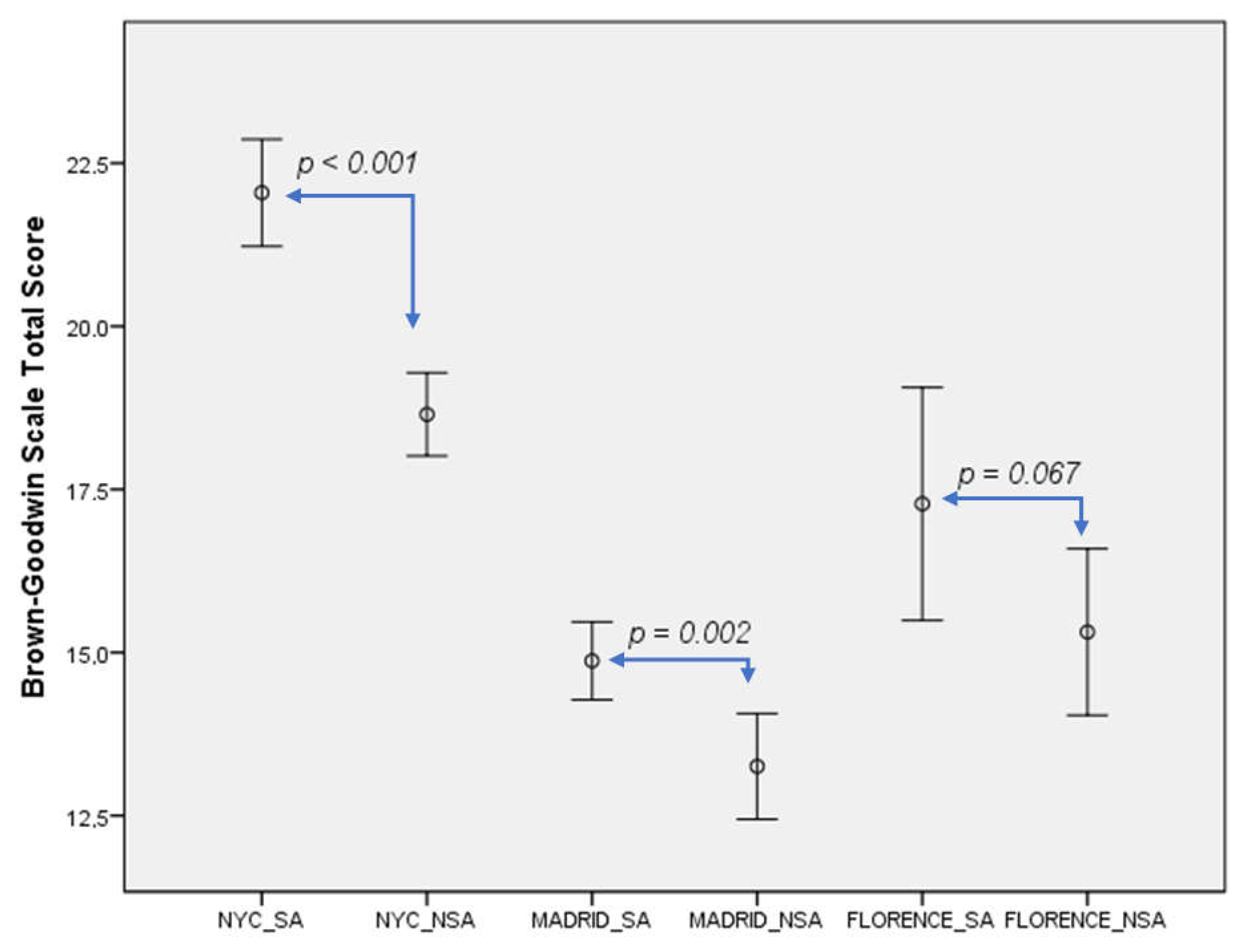
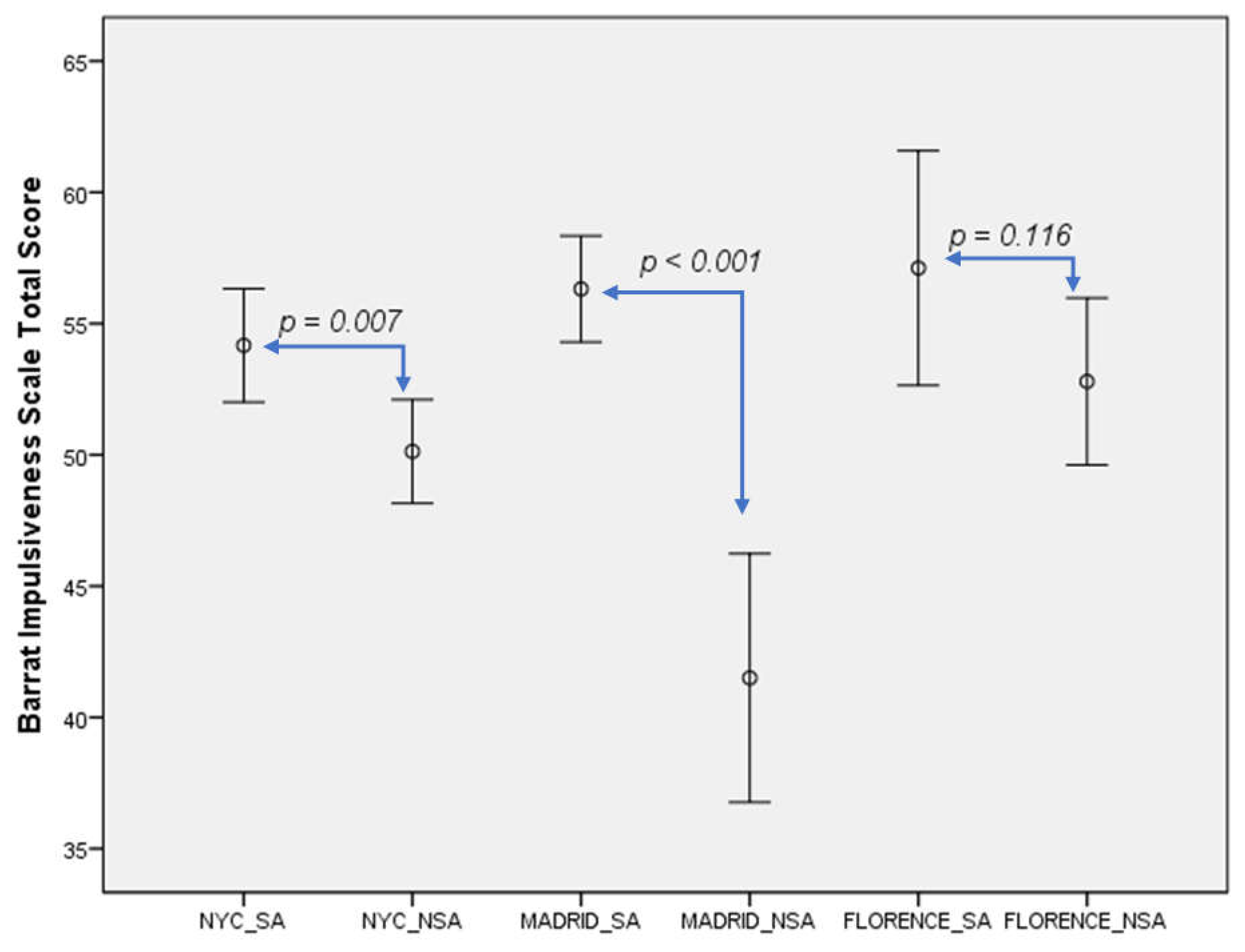
3.3. Differences in Aggression and Impulsivity Levels between Suicide Attempters and Non-Attempters
3.4. Association of Previous Suicidal Behaviour with Aggression and Impulsivity across Sites
4. Discussion
4.1. Main Findings
4.2. Aggression, Impulsivity and Suicidal Behaviour: Differences across Sites
4.3. Strengths and Limitations
4.4. Implications on Suicide Prevention and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization Suicide in the World. Global Health Estimates 2019. Available online: https://apps.who.int/iris/handle/10665/326948 (accessed on 28 April 2021).
- Gunnell, D.; Appleby, L.; Arensman, E.; Hawton, K.; John, A.; Kapur, N.; Khan, M.; O’Connor, R.C.; Pirkis, J. COVID-19 Suicide Prevention Research Collaboration. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 468–471. [Google Scholar] [CrossRef]
- Courtet, P.; Olié, E.; Debien, C.; Vaiva, G. Keep Socially (but Not Physically) Connected and Carry on. J. Clin. Psychiatry 2020, 81, 81. [Google Scholar] [CrossRef] [Green Version]
- Sher, L. The impact of the COVID-19 pandemic on suicide rates. Qjm Int. J. Med. 2020, 113, 707–712. [Google Scholar] [CrossRef]
- Kawohl, W.; Nordt, C. COVID-19, unemployment, and suicide. Lancet Psychiatry 2020, 7, 389–390. [Google Scholar] [CrossRef]
- Oyesanya, M.; Lopez-Morinigo, J.-D.; Dutta, R. Systematic review of suicide in economic recession. World J. Psychiatry 2015, 5, 243–254. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention (CDC). The 2019 AR Threats Report. Available online: www.cdc.gov/DrugResistance/Biggest-Threats.html (accessed on 24 April 2021).
- Cavanagh, J.T.O.; Carson, A.J.; Sharpe, M.; Lawrie, S.M. Psychological autopsy studies of suicide: A systematic review. Psychol. Med. 2003, 33, 395–405. [Google Scholar] [CrossRef] [PubMed]
- Mann, J.J. Neurobiology of suicidal behaviour. Nat. Rev. Neurosci. 2003, 4, 819–828. [Google Scholar] [CrossRef]
- Mann, J.J.; Waternaux, C.; Haas, G.L.; Malone, K.M. Toward a clinical model of suicidal behavior in psychiatric patients. Am. J. Psychiatry 1999, 156, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Gvion, Y.; Apter, A. Aggression, Impulsivity, and Suicide Behavior: A Review of the Literature. Arch. Suicide Res. 2011, 15, 93–112. [Google Scholar] [CrossRef] [PubMed]
- Malone, K.M.; Haas, G.L.; Sweeney, J.A.; Mann, J. Major depression and the risk of attempted suicide. J. Affect. Disord. 1995, 34, 173–185. [Google Scholar] [CrossRef]
- Oquendo, M.A.; Waternaux, C.; Brodsky, B.; Parsons, B.; Haas, G.L.; Malone, K.M.; Mann, J. Suicidal behavior in bipolar mood disorder: Clinical characteristics of attempters and nonattempters. J. Affect. Disord. 2000, 59, 107–117. [Google Scholar] [CrossRef]
- Mann, J.; Currier, D. Stress, genetics and epigenetic effects on the neurobiology of suicidal behavior and depression. Eur. Psychiatry 2010, 25, 268–271. [Google Scholar] [CrossRef]
- Oquendo, M.A.; Sullivan, G.M.; Sudol, K.; Baca-García, E.; Stanley, B.H.; Sublette, M.E.; Mann, J.J. Toward a Biosignature for Suicide. Am. J. Psychiatry 2014, 171, 1259–1277. [Google Scholar] [CrossRef]
- van Heeringen, K.; Mann, J.J. The neurobiology of suicide. Lancet Psychiatry 2014, 1, 63–72. [Google Scholar] [CrossRef]
- Lopez-Castroman, J.; Jaussent, I.; Gorwood, P.; Courtet, P. Suicidal Depressed Patients Respond Less Well to Antidepressants in the Short Term. Depress. Anxiety 2016, 33, 483–494. [Google Scholar] [CrossRef] [PubMed]
- Baca-García, E.; Oquendo, M.A.; Saiz-Ruiz, J.; Mann, J.J.; De Leon, J. A Pilot Study on Differences in Aggression in New York City and Madrid, Spain, and Their Possible Impact on Suicidal Behavior. J. Clin. Psychiatry 2006, 67, 375–380. [Google Scholar] [CrossRef]
- Baca-García, E.; Vaquero, C.; Diaz-Sastre, C.; García-Resa, E.; Saiz-Ruiz, J.; Fernández-Piqueras, J.; de Leon, J. Lack of association between the serotonin transporter promoter gene polymorphism and impulsivity or aggressive behavior among suicide attempters and healthy volunteers. Psychiatry Res. 2004, 126, 99–106. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, R.C.; Platt, S.; Gordon, J. (Eds.) International Handbook of Suicide Prevention Research, Policy and Practice; John Wiley & Sons: Chichester, UK; Malden, MA, USA, 2011; ISBN 978-0-470-68384-2. [Google Scholar]
- O’Carroll, P.W.; Berman, A.L.; Maris, R.W.; Moscicki, E.K.; Tanney, B.L.; Silverman, M.M. Beyond the Tower of Babel: A Nomenclature for Suicidology. Suicide Life Threat. Behav. 1996, 26, 237–252. [Google Scholar] [CrossRef] [PubMed]
- First, M.B. Structured Clinical Interview for DSM-IV Axis I Disorders SCID-I: Clinician Version, Scoresheet; American Psychiatric Press: Washington, DC, USA, 1997; ISBN 978-0-88048-933-1. [Google Scholar]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59, 22–33. [Google Scholar] [PubMed]
- Brown, G.L.; Goodwin, F.K.; Ballenger, J.C.; Goyer, P.F.; Major, L.F. Aggression in humans correlates with cerebrospinal fluid amine metabolites. Psychiatry Res. 1979, 1, 131–139. [Google Scholar] [CrossRef]
- Barratt, E.S. Factor Analysis of Some Psychometric Measures of Impulsiveness and Anxiety. Psychol. Rep. 1965, 16, 547–554. [Google Scholar] [CrossRef]
- Oquendo, M.A.; Baca-Garcia, E.; Graver, R. Spanish Adaptation of the Barratt Impulsiveness Scale (BIS-11). Eur. J. Psychiatry 2001, 15, 147–155. [Google Scholar]
- Fossati, A.; Di Ceglie, A.; Acquarini, E.; Barratt, E.S. Psychometric properties of an Italian version of the Barratt Impulsiveness Scale-11 (BIS-11) in nonclinical subjects. J. Clin. Psychol. 2001, 57, 815–828. [Google Scholar] [CrossRef]
- Franklin, J.C.; Ribeiro, J.D.; Fox, K.R.; Bentley, K.H.; Kleiman, E.M.; Huang, X.; Musacchio, K.M.; Jaroszewski, A.C.; Chang, B.P.; Nock, M.K. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol. Bull. 2017, 143, 187–232. [Google Scholar] [CrossRef]
- Huang, F.L. Alternatives to logistic regression models in experimental studies. J. Exp. Educ. 2019, 1–16. [Google Scholar] [CrossRef]
- McGirr, A.; Renaud, J.; Bureau, A.; Seguin, M.; Lesage, A.; Turecki, G. Impulsive-aggressive behaviours and completed suicide across the life cycle: A predisposition for younger age of suicide. Psychol. Med. 2007, 38, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Carpiniello, B.; Lai, L.; Pirarba, S.; Sardu, C.; Pinna, F. Impulsivity and aggressiveness in bipolar disorder with co-morbid borderline personality disorder. Psychiatry Res. 2011, 188, 40–44. [Google Scholar] [CrossRef]
- Fossati, A.; Barratt, E.S.; Borroni, S.; Villa, D.; Grazioli, F.; Maffei, C. Impulsivity, aggressiveness, and DSM-IV personality disorders. Psychiatry Res. 2007, 149, 157–167. [Google Scholar] [CrossRef]
- Lawrence, R.E.; Oquendo, M.A.; Stanley, B. Religion and Suicide Risk: A Systematic Review. Arch. Suicide Res. 2015, 20, 1–21. [Google Scholar] [CrossRef]
- Lawrence, R.E.; Brent, D.; Mann, J.J.; Burke, A.K.; Grunebaum, M.F.; Galfalvy, H.; Oquendo, M.A. Religion as a Risk Factor for Suicide Attempt and Suicide Ideation Among Depressed Patients. J. Nerv. Ment. Dis. 2016, 204, 845–850. [Google Scholar] [CrossRef] [Green Version]
- Carballo, J.J.; The Stop Consortium; Llorente, C.; Kehrmann, L.; Flamarique, I.; Zuddas, A.; Purper-Ouakil, D.; Hoekstra, P.J.; Coghill, D.; Schulze, U.M.E.; et al. Psychosocial risk factors for suicidality in children and adolescents. Eur. Child. Adolesc. Psychiatry 2020, 29, 759–776. [Google Scholar] [CrossRef] [Green Version]
- Bellino, S.; Patria, L.; Paradiso, E.; Di Lorenzo, R.; Zanon, C.; Zizza, M.; Bogetto, F. Major Depression in Patients with Borderline Personality Disorder: A Clinical Investigation. Can. J. Psychiatry 2005, 50, 234–238. [Google Scholar] [CrossRef]
- Saddichha, S.; Schuetz, C. Impulsivity in remitted depression: A meta-analytical review. Asian J. Psychiatry 2014, 9, 13–16. [Google Scholar] [CrossRef]
- Looper, K.J.; Paris, J. What dimensions underlie cluster B personality disorders? Compr. Psychiatry 2000, 41, 432–437. [Google Scholar] [CrossRef]
- Mehlum, L.; Friis, S.; Vaglum, P.; Karterud, S. The longitudinal pattern of suicidal behaviour in borderline personality disorder: A prospective follow-up study. Acta Psychiatr. Scand. 1994, 90, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Links, P.S.; Heslegrave, R.; Van Reekum, R. Impulsivity: Core Aspect of Borderline Personality Disorder. J. Pers. Disord. 1999, 13, 1–9. [Google Scholar] [CrossRef]
- Colborn, V.A.; Lacroix, J.M.; Neely, L.L.; Tucker, J.; Perera, K.; Daruwala, S.E.; Grammer, G.; Weaver, J.; Ghahramanlou-Holloway, M. Motor impulsivity differentiates between psychiatric inpatients with multiple versus single lifetime suicide attempts. Psychiatry Res. 2017, 253, 18–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bender, T.W.; Gordon, K.H.; Bresin, K.; Joiner, T.E. Impulsivity and suicidality: The mediating role of painful and provocative experiences. J. Affect. Disord. 2011, 129, 301–307. [Google Scholar] [CrossRef]
- Jordan, J.T.; Samuelson, K.W.; Tiet, Q.Q. Impulsivity, Painful and Provocative Events, and Suicide Intent: Testing the Interpersonal Theory of Suicide. Suicide Life Threat. Behav. 2018, 49, 1187–1195. [Google Scholar] [CrossRef] [PubMed]
- Joiner, T.E.; Brown, J.S.; Wingate, L.R. The Psychology and Neurobiology of Suicidal Behavior. Annu. Rev. Psychol. 2005, 56, 287–314. [Google Scholar] [CrossRef]
- Braquehais, M.D.; Oquendo, M.A.; Baca-García, E.; Sher, L. Is impulsivity a link between childhood abuse and suicide? Compr. Psychiatry 2010, 51, 121–129. [Google Scholar] [CrossRef]
- Gvion, Y.; Levi-Belz, Y. Serious Suicide Attempts: Systematic Review of Psychological Risk Factors. Front. Psychiatry 2018, 9, 56. [Google Scholar] [CrossRef]
- Perroud, N.; Baud, P.; Mouthon, D.; Courtet, P.; Malafosse, A. Impulsivity, aggression and suicidal behavior in unipolar and bipolar disorders. J. Affect. Disord. 2011, 134, 112–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Instituto Nacional de Estadística. 2015. Available online: https://www.ines.es/ (accessed on 7 July 2019).
- World Health Organisation. Suicide. Available online: https://www.who.int/news-room/fact-sheets/detail/suicide (accessed on 7 May 2021).
- Felthous, A.R.; Lake, S.L.; Rundle, B.K.; Stanford, M.S. Pharmacotherapy of impulsive aggression: A quality comparison of controlled studies. Int. J. Law Psychiatry 2013, 36, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Tondo, L.; Baldessarini, R.J. Suicidal Behavior in Mood Disorders: Response to Pharmacological Treatment. Curr. Psychiatry Rep. 2016, 18, 88. [Google Scholar] [CrossRef] [PubMed]
- Sim, K.; Lau, W.K.; Sim, J.; Sum, M.Y.; Baldessarini, R.J. Prevention of Relapse and Recurrence in Adults with Major Depressive Disorder: Systematic Review and Meta-Analyses of Controlled Trials. Int. J. Neuropsychopharmacol. 2016, 19, pyv076. [Google Scholar] [CrossRef] [PubMed]
- Pacchiarotti, I.; Bond, D.; Baldessarini, R.J.; Nolen, W.A.; Grunze, H.; Licht, R.W.; Post, R.M.; Berk, M.; Goodwin, G.M.; Sachs, G.S.; et al. The International Society for Bipolar Disorders (ISBD) Task Force Report on Antidepressant Use in Bipolar Disorders. Am. J. Psychiatry 2013, 170, 1249–1262. [Google Scholar] [CrossRef] [PubMed]
- Ingenhoven, T.; Lafay, P.; Rinne, T.; Passchier, J.; Duivenvoorden, H. Effectiveness of Pharmacotherapy for Severe Personality Disorders. J. Clin. Psychiatry 2009, 71, 14–25. [Google Scholar] [CrossRef]
- Hill, A.B. The Environment and Disease: Association or Causation? Proc. R. Soc. Med. 1965, 58, 295–300. [Google Scholar] [CrossRef] [Green Version]
- Pompili, M.; Innamorati, M.; Raja, M.; Falcone, I.; Ducci, G.; Angeletti, G.; Lester, D.; Girardi, P.; Tatarelli, R.; De Pisa, E. Suicide risk in depression and bipolar disorder: Do impulsiveness-aggressiveness and pharmacotherapy predict suicidal intent? Neuropsychiatr. Dis. Treat. 2008, 4, 247–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopez-Castroman, J.; Blasco-Fontecilla, H.; Courtet, P.; Baca-García, E.; Oquendo, M.A. Are we studying the right populations to understand suicide? World Psychiatry 2015, 14, 368–369. [Google Scholar] [CrossRef]
- Soloff, P.; White, R.; Diwadkar, V.A. Impulsivity, aggression and brain structure in high and low lethality suicide attempters with borderline personality disorder. Psychiatry Res. Neuroimaging 2014, 222, 131–139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reich, R.; Gilbert, A.; Clari, R.; Burdick, K.E.; Szeszko, P.R. A preliminary investigation of impulsivity, aggression and white matter in patients with bipolar disorder and a suicide attempt history. J. Affect. Disord. 2019, 247, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Insel, T.R. Digital Phenotyping. JAMA 2017, 318, 1215–1216. [Google Scholar] [CrossRef] [PubMed]
| NYC (n = 647) | MADRID (n = 658) | FLORENCE (n = 93) | p-Value | |
|---|---|---|---|---|
| Mean ± SD n (%) | Mean ± SD n (%) | Mean ± SD n (%) | ||
| Age | 37.8 ± 13.0 | 41.1 ± 15.1 | 47.3 ± 14.1 | <0.001 |
| Gender (males) | 266 (41.1) | 229 (34.8) | 33 (35.5) | 0.57 |
| Education (high) | 301 (48.2) | 162 (27.2) | 5 (14.3) | <0.001 |
| Unmarried | 491 (76.2) | 400 (65.1) | 50 (53.8) | <0.001 |
| Unemployed | 388 (60.7) | 411 (62.5) | 32 (43.2) | 0.006 |
| Children | 245 (40.0) | 274 (50.4) | 44 (47.3) | 0.002 |
| Religion (vs. none) | 485 (77.6) | 187 (66.8) | 52 (80.0) | <0.001 |
| MDD | 482 (74.5) | 516 (78.4) | 45 (48.4) | <0.001 |
| BD | 165 (25.5) | 149 (22.6) | 48 (51.6) | <0.001 |
| Alcohol abuse | 210 (32.5) | 126 (23.8) | 1 (1.0) | <0.001 |
| Drugs abuse | 160 (24.8) | 93 (17.5) | 7 (7.6) | <0.001 |
| Childhood abuse | 191 (34.3) | 117 (23.5) | 5 (5.4) | <0.001 |
| Abuse lifetime | 242 (43.9) | 173 (34.8) | 6 (6.4) | <0.001 |
| Suicide attempters | 303 (46.8) | 465 (74.9) | 39 (41.9) | <0.001 |
| NYC | MADRID | FLORENCE | Statistic | p-Value | ||
|---|---|---|---|---|---|---|
| BGS score | n = 441 | n = 465 | n = 87 | |||
| Mean ± SD, 95% CI | 20.2 ± 5.6, 19.6–20.7 | 14.4 ± 5.3, 13.9–14.9 | 16.1 ± 4.9, 15.1–17.2 | F = 12.62 | NYC > M, p < 0.001 NYC > F, p < 0.001 F > M, p = 0.022 | |
| BIS score | n = 494 | n = 251 | n = 50 | |||
| Mean ± SD, 95% CI | 52.0 ± 16.6, 50.5–53.5 | 53.2 ± 20.1, 51.2–55.1 | 55.0 ± 9.7, 52.3–57.8 | F = 0.932 | F > M, p = 0.766 F > NYC, p = 0.490 M > NYC, p = 0.598 |
| NYC | MADRID | FLORENCE | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Attempters | Non-Attempters | t | p-Value | Attempters | Non-Attempters | t | p-Value | Attempters | Non-Attempters | t | p-Value | |
| BGS | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||||||
| 193 (45.2) | 234 (54.8) | 343 (75.7) | 110 (24.3) | 36 (41.4) | 51 (58.6) | |||||||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||||||
| 22.0 ± 5.8 | 18.6 ± 4.9 | 6.45 | <0.001 | 14.9 ± 5.6 | 13.2 ± 4.3 | 3.17 | 0.002 | 17.3 ± 5.3 | 15.3 ± 4.5 | 1.86 | 0.067 | |
| 95% CI Mean | 95% CI Mean | 95% CI Mean | 95% CI Mean | 95% CI Mean | 95% CI Mean | |||||||
| 21.2–22.9 | 18.0–19.3 | 14.3–15.5 | 12.4–14.1 | 15.5–19.1 | 14.0–16.6 | |||||||
| BIS | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||||||
| 231 (46.6) | 265 (53.4) | 321 (79.6) | 82 (20.3) | 26 (52.0) | 24 (48.0) | |||||||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||||||
| 54.2 ± 16.6 | 50.1 ± 16.3 | 2.72 | 0.007 | 56.3 ± 18.4 | 41.4 ± 21.6 | 5.71 | <0.001 | 57.1 ± 11.0 | 52.8 ± 7.5 | 1.60 | 0.116 | |
| 95% CI Mean | 95% CI Mean | 95% CI Mean | 95% CI Mean | 95% CI Mean | 95% CI Mean | |||||||
| 52.0–56.3 | 48.1–52.1 | 54.3–58.3 | 36.8–46.2 | 52.6–61.6 | 49.6–56.0 | |||||||
| NYC | MADRID | FLORENCE | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| n = 427 | n = 453 | n = 87 | |||||||
| Alcohol | 1.26 | 0.78–2.04 | 0.343 | 1.46 | 0.79–2.67 | 0.222 | |||
| Drugs | 1.37 | 0.80–2.34 | 0.248 | 1.25 | 0.61–2.53 | 0.543 | 0.19 | 0.02–2.22 | 1.86 |
| BGS | 1.12 | 1.07–1.16 | <0.001 | 1.05 | 0.99–1.11 | 0.055 | 1.11 | 1.01–1.22 | 0.032 |
| n = 496 | n = 251 | n = 50 | |||||||
| Alcohol | 1.41 | 0.93–2.13 | 0.104 | 1.49 | 0.72–3.07 | 0.280 | |||
| Drugs | 1.26 | 0.67–2.81 | 0.124 | 1.41 | 0.57–3.50 | 0.461 | 0.17 | 0.02–1.81 | 0.343 |
| BIS | 1.01 | 1.00–1.02 | 0.044 | 1.03 | 1.02–1.05 | <0.001 | 1.07 | 0.98–1.17 | 0.12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lopez-Morinigo, J.-D.; Boldrini, M.; Ricca, V.; Oquendo, M.A.; Baca-García, E. Aggression, Impulsivity and Suicidal Behavior in Depressive Disorders: A Comparison Study between New York City (US), Madrid (Spain) and Florence (Italy). J. Clin. Med. 2021, 10, 3057. https://doi.org/10.3390/jcm10143057
Lopez-Morinigo J-D, Boldrini M, Ricca V, Oquendo MA, Baca-García E. Aggression, Impulsivity and Suicidal Behavior in Depressive Disorders: A Comparison Study between New York City (US), Madrid (Spain) and Florence (Italy). Journal of Clinical Medicine. 2021; 10(14):3057. https://doi.org/10.3390/jcm10143057
Chicago/Turabian StyleLopez-Morinigo, Javier-David, Maura Boldrini, Valdo Ricca, Maria A. Oquendo, and Enrique Baca-García. 2021. "Aggression, Impulsivity and Suicidal Behavior in Depressive Disorders: A Comparison Study between New York City (US), Madrid (Spain) and Florence (Italy)" Journal of Clinical Medicine 10, no. 14: 3057. https://doi.org/10.3390/jcm10143057
APA StyleLopez-Morinigo, J.-D., Boldrini, M., Ricca, V., Oquendo, M. A., & Baca-García, E. (2021). Aggression, Impulsivity and Suicidal Behavior in Depressive Disorders: A Comparison Study between New York City (US), Madrid (Spain) and Florence (Italy). Journal of Clinical Medicine, 10(14), 3057. https://doi.org/10.3390/jcm10143057







