Circulating Growth Differentiation Factor 15 Is Associated with Diabetic Neuropathy
Abstract
:1. Introduction
2. Subjects and Methods
3. Baseline Clinical and Laboratory Measurements
4. Methods for Determination of GDF15 (ELISA)
5. Nerve Conduction Studies
6. Statistical Analysis
7. Results
7.1. Comparisons between DM and Non-DM Group
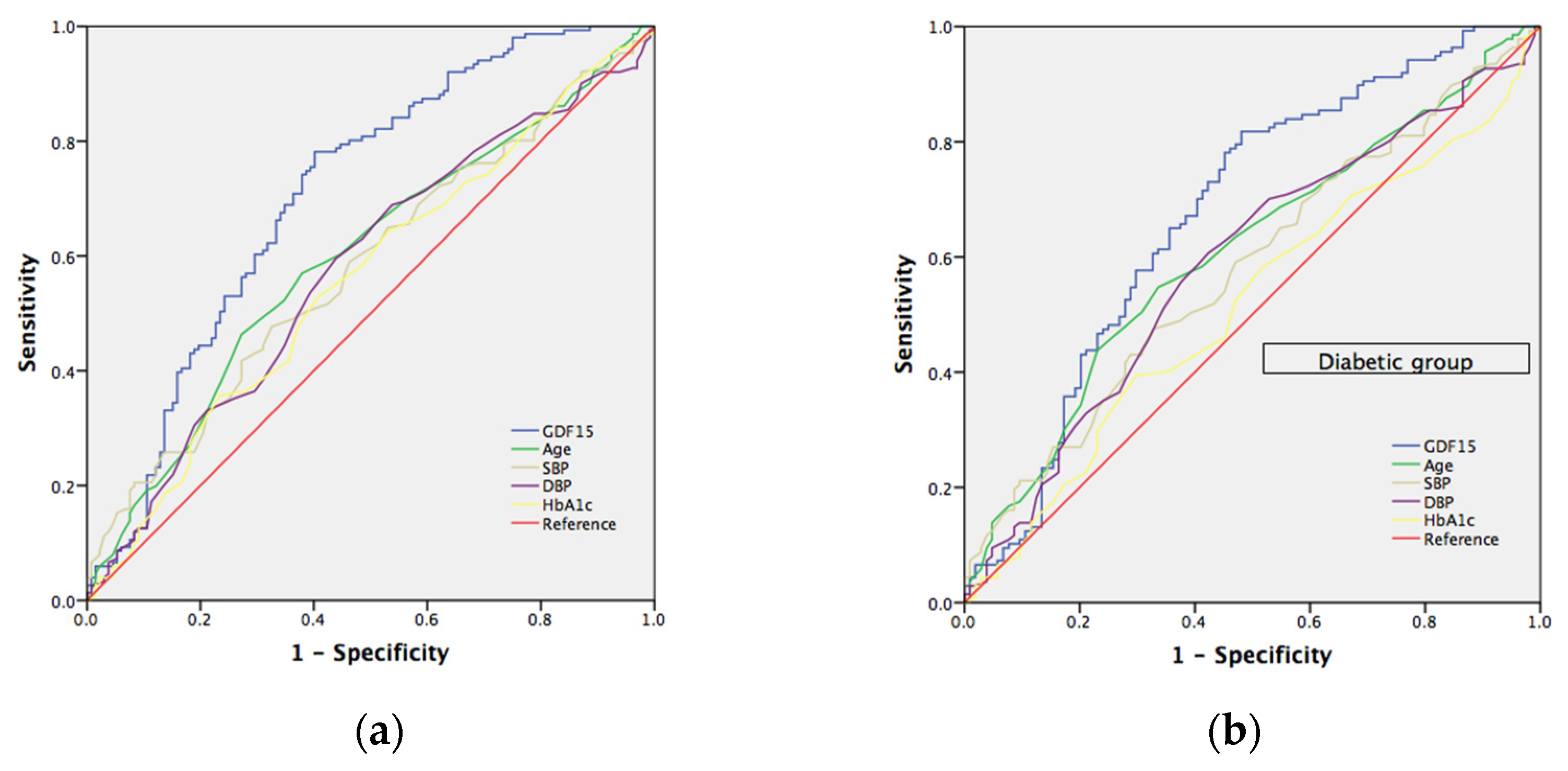
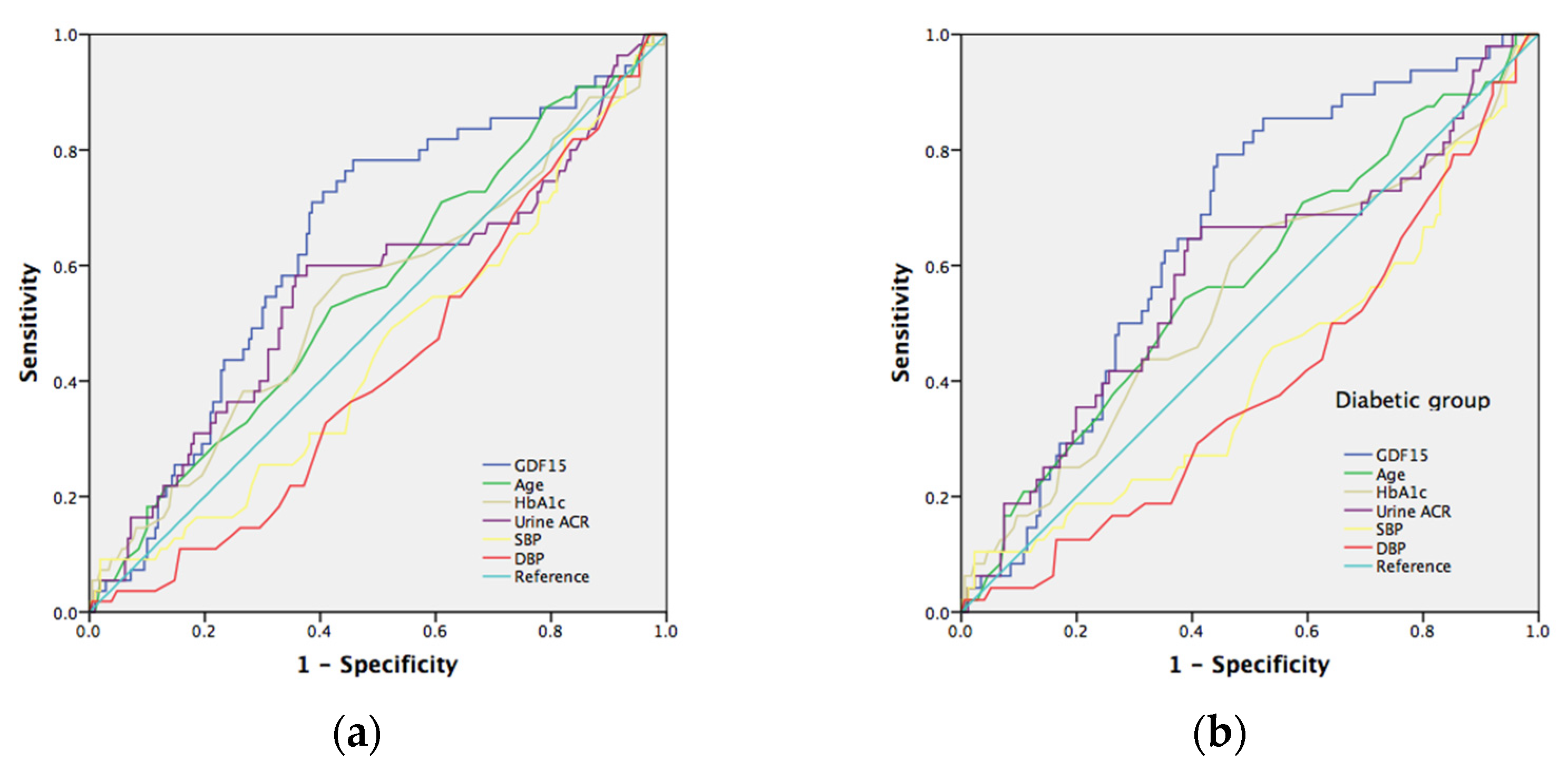
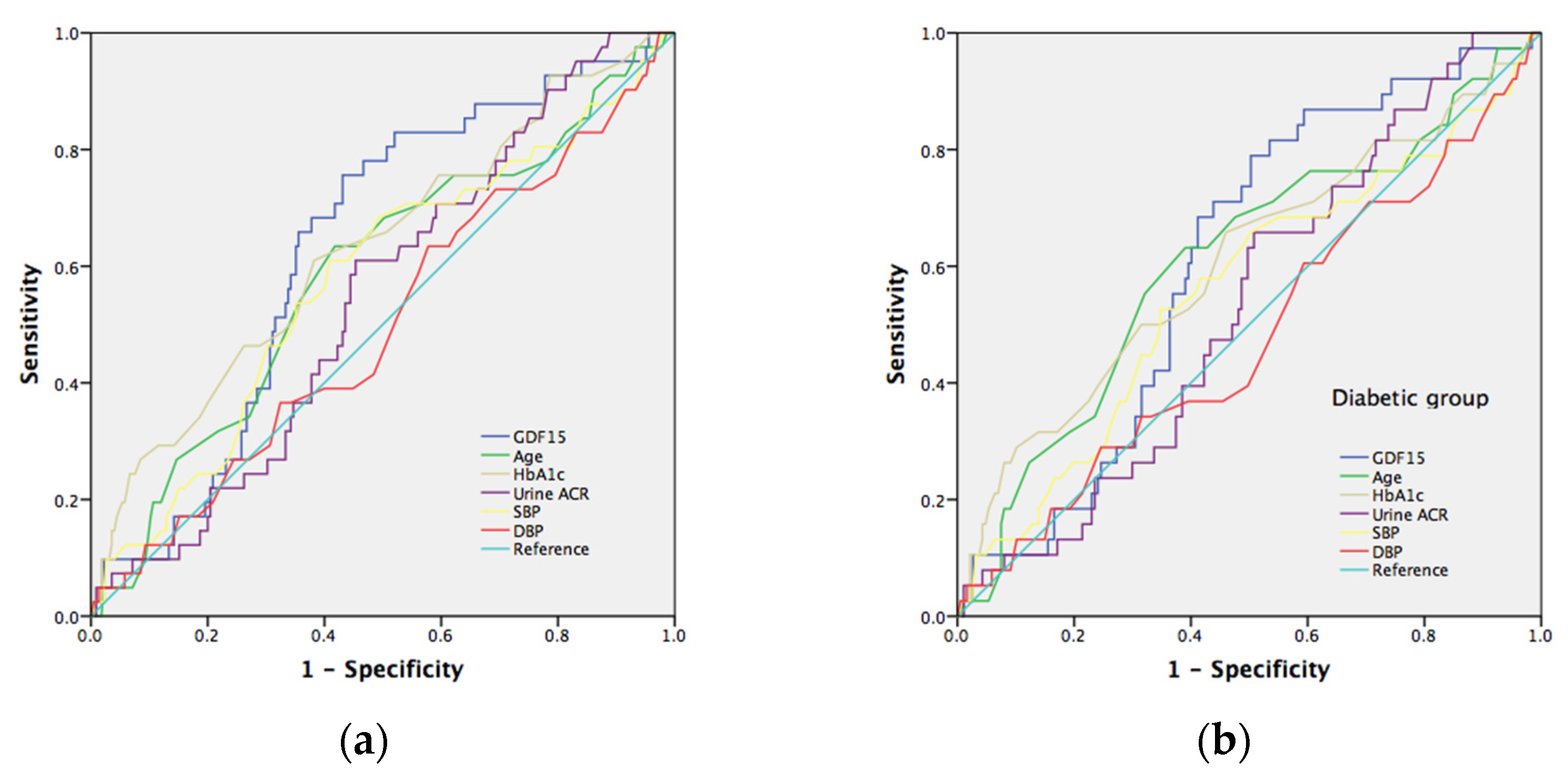
7.2. The Risk Prediction Model for Nephropathy
7.3. Comparisons between Different Levels of GDF15
7.4. Correlation between GDF15 and Nerve Conductive Study
7.5. The Risk Prediction Model for Neuropathy
8. Discussion
9. Study Limitations
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Sheen, Y.-J.; Hsu, C.-C.; Jiang, Y.-D.; Huang, C.-N.; Liu, J.-S.; Sheu, W.H.-H. Trends in prevalence and incidence of diabetes mellitus from 2005 to 2014 in Taiwan. J. Formos. Med. Assoc. 2019, 118 (Suppl. S2), S66–S73. [Google Scholar] [CrossRef]
- Chang, C.-J.; Lu, F.-H.; Yang, Y.-C.; Wu, J.-S.; Wu, T.-J.; Chen, M.-S.; Chuang, L.-M.; Tai, T.-Y. Epidemiologic study of type 2 diabetes in Taiwan. Diabetes Res. Clin. Pract. 2000, 50 (Suppl. S2), S49–S59. [Google Scholar] [CrossRef]
- Li, H.-Y.; Jiang, Y.-D.; Chang, C.-H.; Chung, C.-H.; Lin, B.J.; Chuang, L.-M. Mortality trends in patients with diabetes in Taiwan: A nationwide survey in 2000–2009. J. Formos. Med. Assoc. 2012, 111, 645–650. [Google Scholar] [CrossRef] [Green Version]
- Sheen, Y.-J.; Sheu, W.H. Association between hypoglycemia and dementia in patients with type 2 diabetes. Diabetes Res. Clin. Pract. 2016, 116, 279–287. [Google Scholar] [CrossRef]
- Tseng, L.-N.; Tseng, Y.-H.; Jiang, Y.-D.; Chang, C.-H.; Chung, C.-H.; Lin, B.J.; Chuang, L.-M.; Tai, T.-Y.; Sheu, W.H.-H. Prevalence of hypertension and dyslipidemia and their associations with micro- and macrovascular diseases in patients with diabetes in Taiwan: An analysis of nationwide data for 2000–2009. J. Formos. Med. Assoc. 2012, 111, 625–636. [Google Scholar] [CrossRef] [Green Version]
- Domingueti, C.P.; Dusse, L.M.S.; Carvalho, M.D.G.; Sousa, L.; Gomes, K.B.; Fernandes, A.P. Diabetes mellitus: The linkage between oxidative stress, inflammation, hypercoagulability and vascular complications. J. Diabetes Complicat. 2016, 30, 738–745. [Google Scholar] [CrossRef]
- Song, J.; Chen, S.; Liu, X.; Duan, H.; Kong, J.; Li, Z. Relationship between C-Reactive Protein Level and Diabetic Retinopathy: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0144406. [Google Scholar] [CrossRef]
- Chuengsamarn, S.; Rattanamongkolgul, S.; Sittithumcharee, G.; Jirawatnotai, S. Association of serum high-sensitivity C-reactive protein with metabolic control and diabetic chronic vascular complications in patients with type 2 diabetes. Diabetes Metab. Syndr. Clin. Res. Rev. 2017, 11, 103–108. [Google Scholar] [CrossRef]
- Nakamura, A.; Shikata, K.; Hiramatsu, M.; Nakatou, T.; Kitamura, T.; Wada, J.; Itoshima, T.; Makino, H. Serum Interleukin-18 Levels Are Associated With Nephropathy and Atherosclerosis in Japanese Patients With Type 2 Diabetes. Diabetes Care 2005, 28, 2890–2895. [Google Scholar] [CrossRef] [Green Version]
- Doupis, J.; Lyons, T.E.; Wu, S.; Gnardellis, C.; Dinh, T.; Veves, A. Microvascular Reactivity and Inflammatory Cytokines in Painful and Painless Peripheral Diabetic Neuropathy. J. Clin. Endocrinol. Metab. 2009, 94, 2157–2163. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Renier, G. The Connection between C-Reactive Protein (CRP) and Diabetic Vasculopathy. Focus on Preclinical Findings. Curr. Diabetes Rev. 2010, 6, 27–34. [Google Scholar] [CrossRef]
- Kuo, J.Z.; Guo, X.; Klein, R.; Klein, B.E.; Cui, J.; Rotter, J.I.; Ipp, E.; Chen, Y.-D.I. Systemic Soluble Tumor Necrosis Factor Receptors 1 and 2 Are Associated with Severity of Diabetic Retinopathy in Hispanics. Ophthalmology 2012, 119, 1041–1046. [Google Scholar] [CrossRef] [Green Version]
- Tan, M.; Wang, Y.; Guan, K.; Sun, Y. PTGF-β, a type β transforming growth factor (TGF-β) superfamily member, is a p53 target gene that inhibits tumor cell growth via TGF-β signaling pathway. Proc. Natl. Acad. Sci. USA 2000, 97, 109–114. [Google Scholar] [CrossRef] [Green Version]
- Wischhusen, J.; Melero, I.; Fridman, W.H. Growth/Differentiation Factor-15 (GDF-15): From Biomarker to Novel Targetable Immune Checkpoint. Front. Immunol. 2020, 11, 951. [Google Scholar] [CrossRef]
- Tsai, V.W.W.; Husaini, Y.; Sainsbury, A.; Brown, D.A.; Breit, S.N. The MIC-1/GDF15-GFRAL Pathway in Energy Homeostasis: Implications for Obesity, Cachexia, and Other Associated Diseases. Cell Metab. 2018, 28, 353–368. [Google Scholar] [CrossRef] [Green Version]
- Lockhart, S.M.; Saudek, V.; O’Rahilly, S. GDF15: A Hormone Conveying Somatic Distress to the Brain. Endocr. Rev. 2020, 41, bnaa007. [Google Scholar] [CrossRef] [Green Version]
- Macia, L.; Tsai, V.W.-W.; Nguyen, A.D.; Johnen, H.; Kuffner, T.; Shi, Y.-C.; Lin, S.; Herzog, H.; Brown, D.A.; Breit, S.N.; et al. Macrophage Inhibitory Cytokine 1 (MIC-1/GDF15) Decreases Food Intake, Body Weight and Improves Glucose Tolerance in Mice on Normal & Obesogenic Diets. PLoS ONE 2012, 7, e34868. [Google Scholar] [CrossRef] [Green Version]
- Tsai, V.W.; Macia, L.; Johnen, H.; Kuffner, T.; Manadhar, R.; Jørgensen, S.B.; Lee-Ng, K.K.M.; Zhang, H.P.; Wu, L.; Marquis, C.P.; et al. TGF-b superfamily cytokine MIC-1/GDF15 is a physiological appetite and body weight regulator. PLoS ONE 2013, 8, e55174. [Google Scholar] [CrossRef] [Green Version]
- Wollert, K.C.; Kempf, T.; Wallentin, L. Growth Differentiation Factor 15 as a Biomarker in Cardiovascular Disease. Clin. Chem. 2017, 63, 140–151. [Google Scholar] [CrossRef]
- Lajer, M.; Jorsal, A.; Tarnow, L.; Parving, H.-H.; Rossing, P. Plasma Growth Differentiation Factor-15 Independently Predicts All-Cause and Cardiovascular Mortality As Well As Deterioration of Kidney Function in Type 1 Diabetic Patients With Nephropathy. Diabetes Care 2010, 33, 1567–1572. [Google Scholar] [CrossRef] [Green Version]
- Hellemons, M.E.; Mazagova, M.; Gansevoort, R.T.; Henning, R.H.; de Zeeuw, D.; Bakker, S.J.; Lambers-Heerspink, H.J.; Deelman, L.E. Growth-Differentiation Factor 15 Predicts Worsening of Albuminuria in Patients With Type 2 Diabetes. Diabetes Care 2012, 35, 2340–2346. [Google Scholar] [CrossRef] [Green Version]
- Chung, J.O.; Park, S.-Y.; Cho, D.H.; Chung, D.J.; Chung, M.Y. Relationship between plasma growth differentiation factor-15 levels and diabetic retinopathy in individuals with type 2 diabetes. Sci. Rep. 2020, 10, 20568. [Google Scholar] [CrossRef]
- Niu, Y.; Zhang, W.; Shi, J.; Liu, Y.; Zhang, H.; Lin, N.; Li, X.; Qin, L.; Yang, Z.; Su, Q. The Relationship Between Circulating Growth Differentiation Factor 15 Levels and Diabetic Retinopathy in Patients With Type 2 Diabetes. Front. Endocrinol. 2021, 12, 627395. [Google Scholar] [CrossRef]
- Young, M.J.; Boulton, A.J.M.; MacLeod, A.F.; Williams, D.R.R.; Sonksen, P.H. A multicentre study of the prevalence of diabetic peripheral neuropathy in the United Kingdom hospital clinic population. Diabetologia 1993, 36, 150–154. [Google Scholar] [CrossRef] [Green Version]
- Al-Mahroos, F.; Al-Roomi, K. Diabetic neuropathy, foot ulceration, peripheral vascular disease and potential risk factors among patients with diabetes in bahrain: A nationwide primary care diabetes clinic-based study. Ann. Saudi Med. 2007, 27, 25–31. [Google Scholar] [CrossRef]
- Callaghan, B.C.; Gao, L.; Li, Y.; Zhou, X.; Reynolds, E.; Banerjee, M.; Pop-Busui, R.; Feldman, E.; Ji, L. Diabetes and obesity are the main metabolic drivers of peripheral neuropathy. Ann. Clin. Transl. Neurol. 2018, 5, 397–405. [Google Scholar] [CrossRef]
- Yang, C.P.; Lin, C.C.; Li, C.I.; Liu, C.S.; Lin, W.Y.; Hwang, K.L.; Yang, S.; Chen, H.; Li, T. Cardiovascular Risk Factors Increase the Risks of Diabetic Peripheral Neuropathy in Patients With Type 2 Diabetes Mellitus: The Taiwan Diabetes Study. Medicine 2015, 94, e1783. [Google Scholar] [CrossRef]
- Liu, X.; Xu, Y.; An, M.; Zeng, Q. The risk factors for diabetic peripheral neuropathy: A meta-analysis. PLoS ONE 2019, 14, e0212574. [Google Scholar] [CrossRef]
- Zhang, Y.; Jiang, Y.; Shen, X.; Yan, S. Can both normal and mildly abnormal albuminuria and glomerular filtration rate be a danger signal for diabetic peripheral neuropathy in type 2 diabetes mellitus? Neurol. Sci. 2017, 38, 1381–1390. [Google Scholar] [CrossRef]
- Meekins, D.A.; Morozov, I.; Trujillo, J.D.; Gaudreault, N.N.; Bold, D.; Carossino, M.; Artiaga, B.L.; Indran, S.V.; Kwon, T.; Balaraman, V.; et al. Susceptibility of swine cells and domestic pigs to SARS-CoV-2. Emerg. Microbes Infect. 2020, 9, 2278–2288. [Google Scholar] [CrossRef]
- Ponirakis, G.; Petropoulos, I.N.; Alam, U.; Ferdousi, M.; Asghar, O.; Marshall, A.; Azmi, S.; Jeziorska, M.; Mahfoud, Z.; Boulton, A.J.M.; et al. Hypertension Contributes to Neuropathy in Patients With Type 1 Diabetes. Am. J. Hypertens. 2019, 32, 796–803. [Google Scholar] [CrossRef]
- Huang, L.; Zhang, Y.; Wang, Y.; Shen, X.; Yan, S. Diabetic Peripheral Neuropathy Is Associated With Higher Systolic Blood Pressure in Adults With Type 2 Diabetes With and Without Hypertension in the Chinese Han Population. Can. J. Diabetes 2019, 44, 615–623. [Google Scholar] [CrossRef]
- Feldman, E.L.; Callaghan, B.C.; Pop-Busui, R.; Zochodne, D.W.; Wright, D.E.; Bennett, D.L.; Bril, V.; Russell, J.W.; Viswanathan, V. Diabetic neuropathy. Nat. Rev. Dis. Primers 2019, 5, 41. [Google Scholar] [CrossRef]
- Sloan, G.; Selvarajah, D.; Tesfaye, S. Pathogenesis, diagnosis and clinical management of diabetic sensorimotor peripheral neuropathy. Nat. Rev. Endocrinol. 2021, 17, 400–420. [Google Scholar] [CrossRef]
- Stevens, P.E.; Levin, A. Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group M. Evaluation and management of chronic kidney disease: Synopsis of the kidney disease: Improving global outcomes 2012 clinical practice guideline. Ann. Intern. Med. 2013, 158, 825–830. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.-R.; Chang, W.-N.; Chang, H.-W.; Tsai, N.-W.; Lu, C.-H. Effects of age, gender, height, and weight on late responses and nerve conduction study parameters. Acta Neurol. Taiwanica 2009, 18, 242–249. [Google Scholar]
- Adela, R.; Banerjee, S.K. GDF-15 as a Target and Biomarker for Diabetes and Cardiovascular Diseases: A Translational Prospective. J. Diabetes Res. 2015, 2015, 490842. [Google Scholar] [CrossRef]
- Perez-Gomez, M.V.; Pizarro-Sanchez, S.; Gracia-Iguacel, C.; Cano, S.; Cannata-Ortiz, P.; Sanchez-Rodriguez, J.; Sanz, A.B.; Sanchez-Niño, M.D.; Ortiz, A. Urinary Growth Differentiation Factor-15 (GDF15) levels as a biomarker of adverse outcomes and biopsy findings in chronic kidney disease. J. Nephrol. 2021, 34, 1819–1832. [Google Scholar] [CrossRef]
- Falkowski, B.; Rogowicz-Frontczak, A.; Szczepanek-Parulska, E.; Krygier, A.; Wrotkowska, E.; Uruska, A.; Araszkiewicz, A.; Ruchala, M.; Zozulinska-Ziolkiewicz, D. Novel Biochemical Markers of Neurovascular Complications in Type 1 Diabetes Patients. J. Clin. Med. 2020, 9, 198. [Google Scholar] [CrossRef] [Green Version]
- Carlsson, A.C.; Nowak, C.; Lind, L.; Östgren, C.J.; Nyström, F.H.; Sundström, J.; Carrero, J.J.; Riserus, U.; Ingelsson, E.; Fall, T.; et al. Growth differentiation factor 15 (GDF-15) is a potential biomarker of both diabetic kidney disease and future cardiovascular events in cohorts of individuals with type 2 diabetes: A proteomics approach. Upsala J. Med Sci. 2019, 125, 37–43. [Google Scholar] [CrossRef] [Green Version]
- Bansal, N.; Zelnick, L.; Shlipak, M.G.; Anderson, A.; Christenson, R.; Deo, R.; Defilippi, C.; Feldman, H.; Lash, J.; He, J.; et al. Cardiac and Stress Biomarkers and Chronic Kidney Disease Progression: The CRIC Study. Clin. Chem. 2019, 65, 1448–1457. [Google Scholar] [CrossRef] [PubMed]
- Nair, V.; Robinson-Cohen, C.; Smith, M.R.; Bellovich, K.A.; Bhat, Z.Y.; Bobadilla, M.; Brosius, F.; De Boer, I.H.; Essioux, L.; Formentini, I.; et al. Growth Differentiation Factor–15 and Risk of CKD Progression. J. Am. Soc. Nephrol. 2017, 28, 2233–2240. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.; Wei, L.; Yang, X.; Zhong, J.J. Roles of Growth Differentiation Factor 15 in Atherosclerosis and Coronary Artery Disease. J. Am. Hear. Assoc. 2019, 8, e012826. [Google Scholar] [CrossRef]
- He, X.; Su, J.; Ma, X.; Lu, W.; Zhu, W.; Wang, Y.; Bao, Y.; Zhou, J. The association between serum growth differentiation factor 15 levels and lower extremity atherosclerotic disease is independent of body mass index in type 2 diabetes. Cardiovasc. Diabetol. 2020, 19, 40. [Google Scholar] [CrossRef] [Green Version]
- Kempf, T.; Zarbock, A.; Widera, C.; Butz, S.; Stadtmann, A.; Rossaint, J.; Bolomini-Vittori, M.; Korf-Klingebiel, M.; Napp, L.C.; Hansen, B.; et al. GDF-15 is an inhibitor of leukocyte integrin activation required for survival after myocardial infarction in mice. Nat. Med. 2011, 17, 581–588. [Google Scholar] [CrossRef]
- Schlittenhardt, D.; Schober, A.; Strelau, J.; Bonaterra, G.A.; Schmiedt, W.; Unsicker, K.; Metz, J.; Kinscherf, R. Involvement of growth differentiation factor-15/macrophage inhibitory cytokine-1 (GDF-15/MIC-1) in oxLDL-induced apoptosis of human macrophages in vitro and in arteriosclerotic lesions. Cell Tissue Res. 2004, 318, 325–333. [Google Scholar] [CrossRef]
- Bootcov, M.R.; Bauskin, A.R.; Valenzuela, S.M.; Moore, A.G.; Bansal, M.; He, X.Y.; Zhang, H.P.; Donnellan, M.; Mahler, S.; Pryor, K.; et al. MIC-1, a novel macrophage inhibitory cytokine, is a divergent member of the TGF-beta superfamily. Proc. Natl. Acad. Sci. USA 1997, 94, 11514–11519. [Google Scholar] [CrossRef] [Green Version]
- Liu, H.; Liu, J.; Si, L.; Guo, C.; Liu, W.; Liu, Y. GDF-15 promotes mitochondrial function and proliferation in neuronal HT22 cells. J. Cell. Biochem. 2019, 120, 10530–10547. [Google Scholar] [CrossRef]
- Wang, C.-Y.; Huang, A.-Q.; Zhou, M.-H.; Mei, Y.-A. GDF15 regulates Kv2.1-mediated outward K+ current through the Akt/mTOR signalling pathway in rat cerebellar granule cells. Biochem. J. 2014, 460, 35–47. [Google Scholar] [CrossRef] [Green Version]
- Machado, V.; Haas, S.J.; von Bohlen Und Halbach, O.; Wree, A.; Krieglstein, K.; Unsicker, K.; Spittau, B. Growth/differentiation factor-15 deficiency compromises dopaminergic neuron survival and microglial response in the 6-hydroxydopamine mouse model of Parkinson’s disease. Neurobiol. Dis. 2016, 88, 1–15. [Google Scholar] [CrossRef]
- Strelau, J.; Sullivan, A.; Bottner, M.; Lingor, P.; Falkenstein, E.; Suter-Crazzolara, C.; Galter, D.; Jaszai, J.; Krieglstein, K.; Unsicker, K. Growth/differentiation factor-15/macrophage inhibitory cytokine-1 is a novel trophic factor for midbrain dopaminergic neurons in vivo. J. Neurosci. 2000, 20, 8597–8603. [Google Scholar] [CrossRef] [Green Version]

| DM | Non-DM | p-Value | |
|---|---|---|---|
| Number | 241 | 42 | |
| Age (years) | 64.7 ± 8.9 | 68.9 ± 9.3 | 0.006 |
| Men, n (%) | 144 (59.8) | 21 (50.0) | 0.237 |
| B.H (cm) | 162 ± 8.5 | 159 ± 7.2 | 0.030 |
| B.W (kg) | 69.3 ± 12.8 | 63.5 ± 9.6 | 0.001 |
| BMI (kg/m2) | 26.3 ± 3.7 | 25.2 ± 3.1 | 0.033 |
| WC (cm) | 85.4 ± 10.2 | 78.8 ± 8.9 | <0.001 |
| HbA1c (%) | 7.23 ± 1.0 | 5.78 ± 0.28 | <0.001 |
| Creatinine | 1.03 ± 0.50 | 0.93 ± 0.32 | 0.196 |
| eGFR (mL∙min−11.73 m−2) | 74.3 ± 23.8 | 75.2 ± 17.3 | 0.765 |
| Urine ACR (mg/g) | 30.5 (10.3–139.9) | 11.4 (6.25–17.2) | <0.001 |
| GDF15 (pg/mL) | 606 (344–1127) | 185 (144–326) | <0.001 |
| GDF15 > 530 pg/mL, n (%) | 121 (50.2) | 4 (9.5) | <0.001 |
| Hyperlipidemia, n (%) | 182 (75.5) | 26 (61.9) | 0.065 |
| HTN, n (%) | 180 (74.7) | 33 (78.6) | 0.590 |
| CKD, n (%) | 137 (56.8) | 14 (30.3) | 0.005 |
| DM | Non-DM | p-Value | |
|---|---|---|---|
| Sensory | |||
| Median nerve | N = 229 | N = 42 | |
| Latencies (ms) | 1.33 ± 0.38 | 1.19 ± 0.14 | <0.001 |
| Amp, µV | 36.4 ± 20.1 | 43.2 ± 17.9 | 0.039 |
| NCV, m/s | 54.6 ± 9.2 | 58.6 ± 7.1 | 0.008 |
| Ulnar nerve | N = 230 | N = 42 | |
| Latencies (ms) | 2.34 ± 0.35 | 2.28 ± 0.29 | 0.239 |
| Amp, µV | 25.8 ± 13.0 | 31.2 ± 14.6 | 0.021 |
| NCV, m/s | 51.8 ± 6.4 | 52.8 ± 6.3 | 0.395 |
| Motor | |||
| Median nerve | N = 240 | N = 42 | |
| Latencies (ms) | 4.45 ± 1.25 | 3.70 ± 0.40 | <0.001 |
| Amp, µV | 9.14 ± 2.5 | 9.41 ± 2.3 | 0.5 |
| NCV, m/s | 52.3 ± 4.3 | 54.5 ± 4.2 | 0.002 |
| Ulnar nerve | N = 241 | N = 42 | |
| Latencies (ms) | 2.92 ± 0.41 | 2.78 ± 0.33 | 0.039 |
| Amp, µV | 9.12 ± 2.11 | 9.39 ± 2.00 | 0.45 |
| NCV, m/s | 53.4 ± 4.6 | 55.3 ± 4.3 | 0.038 |
| Peroneal nerve | N = 231 | N = 41 | |
| Latencies (ms) | 3.92 ± 0.61 | 3.72 ± 0.41 | 0.011 |
| Amp, mV | 4.55 ± 2.1 | 4.88 ± 2.1 | 0.359 |
| NCV, m/s | 44.8 ± 5.1 | 46.7 ± 5.2 | 0.026 |
| Tibial nerve | N = 235 | N = 41 | |
| Latencies (ms) | 4.00 ± 0.67 | 3.94 ± 0.74 | 0.6 |
| Amp, mV | 10.87 ± 4.4 | 12.22 ± 4.2 | 0.067 |
| NCV, m/s | 44.2 ± 4.5 | 46.6 ± 4.5 | 0.002 |
| F-wave | |||
| Median nerve | N = 236 | N = 41 | |
| Latencies (ms) | 28.3 ± 3.0 | 26.7 ± 3.6 | 0.002 |
| Ulnar nerve | N = 238 | N = 41 | |
| Latencies (ms) | 27.9 ± 3.0 | 26.2 ± 2.0 | <0.001 |
| Peroneal nerve | N = 186 | N = 31 | |
| Latencies (ms) | 50.0 ± 4.9 | 46.9 ± 3.4 | <0.001 |
| Tibial nerve | N = 232 | N = 40 | |
| Latencies (ms) | 50.3 ± 4.9 | 47.7 ± 3.6 | 0.001 |
| H-reflex | |||
| Tibial nerve | N = 227 | N = 40 | |
| Latencies (ms) | 32.3 ± 3.0 | 30.8 ± 2.4 | 0.003 |
| GDF15 Level | <530 | ≥530 | p-Value |
|---|---|---|---|
| Number | 142 | 141 | |
| Age (years) | 64.6 ± 9.5 | 66.1 ± 8.6 | 0.185 |
| Men, n (%) | 77 (54.2) | 88 (62.4) | 0.163 |
| B.H (cm) | 161.5 ± 8.5 | 161.5 ± 8.3 | 0.997 |
| B.W (kg) | 68.3 ± 12.3 | 68.6 ± 12.8 | 0.804 |
| BMI (kg/m2) | 26.1 ± 3.5 | 26.2 ± 3.9 | 0.747 |
| WC (cm) | 82.1 ± 9.7 | 86.8 ± 10.3 | <0.001 |
| HC (cm) | 89.1 ± 6.4 | 91.4 ± 7.8 | 0.007 |
| HbA1c (%) | 6.81 ± 1.0 | 7.22 ± 1.0 | 0.001 |
| Creatinine | 0.93 ± 0.33 | 1.11 ± 0.57 | 0.001 |
| eGFR (mL∙min−11.73m−2) | 78.2 ± 21.5 | 70.0 ± 23.3 | <0.001 |
| Urine ACR (mg/g) | 14.3 (6.7–69.5) | 42.0 (12.5–177.5) | <0.001 |
| 0.68 (0.26–1.52) 0.94 (0.42–2.09) 1.99 (1.40–2.76) 2.22 (1.35–3.39) hsCRP (mg/L) | 14.3 (6.7–69.5) | 42.0 (12.5–177.5) | 0.709 |
| HOMA-IR | 0.68 (0.26–1.52) | 0.94 (0.42–2.09) | 0.003 |
| DM, n (%) | 105 (73.9) | 136 (96.5) | <0.001 |
| Hyperlipidemia, n (%) | 104 (73.2) | 104 (73.8) | 0.921 |
| HTN, n (%) | 98 (69.0) | 115 (81.6) | 0.014 |
| CKD, n (%) | 54 (38) | 97 (68.8) | <0.001 |
| GDF15 < 530 | GDF15 ≥ 530 | p | p * | p ** | |
|---|---|---|---|---|---|
| Sensory | |||||
| Median nerve | N = 136 | N = 135 | |||
| Latencies (ms) | 1.25 ± 0.38 | 1.36 ± 0.33 | 0.007 | 0.013 | 0.065 |
| Amp, µV | 39.1 ± 19.0 | 35.7 ± 20.7 | 0.158 | ||
| NCV, m/s | 57.6 ± 7.2 | 52.8 ± 9.9 | <0.001 | <0.001 | <0.001 |
| Ulnar nerve | N = 140 | N = 132 | |||
| Latencies (ms) | 2.25 ± 0.27 | 2.42 ± 0.38 | <0.001 | <0.001 | <0.001 |
| Amp, µV | 28.4 ± 14.0 | 24.8 ± 13.8 | 0.034 | 0.055 | 0.198 |
| NCV, m/s | 53.6 ± 5.5 | 50.3 ± 6.9 | <0.001 | <0.001 | <0.001 |
| Motor | |||||
| Median nerve | N = 142 | N = 140 | |||
| Latencies (ms) | 4.19 ± 1.11 | 4.49 ± 1.27 | 0.038 | 0.06 | 0.249 |
| Amp, µV | 9.41 ± 2.15 | 8.95 ± 2.74 | 0.113 | ||
| NCV, m/s | 53.3 ± 4.3 | 52.1 ± 4.3 | 0.019 | 0.36 | 0.213 |
| Ulnar nerve | N = 142 | N = 141 | |||
| Latencies (ms) | 2.82 ± 0.36 | 2.98 ± 0.43 | 0.001 | 0.001 | 0.008 |
| Amp, mV | 9.30 ± 1.97 | 9.02 ± 2.21 | 0.522 | ||
| NCV, m/s | 54.5 ± 4.4 | 52.9 ± 4.7 | 0.018 | 0.019 | 0.113 |
| Peroneal nerve | N = 141 | N = 131 | |||
| Latencies (ms) | 3.82 ± 0.55 | 3.96 ± 0.63 | 0.048 | 0.04 | 0.064 |
| Amp, mV | 4.71 ± 1.93 | 4.78 ± 2.28 | 0.37 | ||
| NCV, m/s | 45.8 ± 4.6 | 44.3 ± 5.5 | 0.013 | 0.016 | 0.034 |
| Tibial nerve | N = 142 | N = 134 | |||
| Latencies (ms) | 3.93 ± 0.66 | 4.06 ± 0.69 | 0.119 | ||
| Amp, mV | 11.37 ± 4.15 | 10.75 ± 4.60 | 0.25 | ||
| NCV, m/s | 45.3 ± 4.4 | 43.8 ± 4.6 | 0.006 | 0.005 | 0.029 |
| F-wave | |||||
| Median nerve | N = 141 | N = 136 | |||
| Latencies (ms) | 27.5 ± 2.7 | 28.6 ± 3.5 | 0.004 | 0.006 | 0.052 |
| Ulnar nerve | N = 141 | N = 138 | |||
| Latencies (ms) | 27.0 ± 2.7 | 28.3 ± 3.1 | <0.001 | <0.001 | <0.001 |
| Peroneal nerve | N = 115 | N = 102 | |||
| Latencies (ms) | 48.7 ± 4.7 | 50.6 ± 4.8 | 0.004 | 0.002 | 0.008 |
| Tibial nerve | N = 141 | N = 131 | |||
| Latencies (ms) | 49.1 ± 4.4 | 50.8 ± 5.1 | 0.004 | 0.001 | 0.007 |
| H-reflex | |||||
| Tibial nerve | N = 139 | N = 128 | |||
| Latencies (ms) | 31.6 ± 2.8 | 32.6 ± 3.2 | 0.006 | 0.002 | 0.012 |
| LogGDF15 (pg/mL) | Correlation Coefficient (r) | p-Value |
|---|---|---|
| Sensory | ||
| Median nerve | N = 271 | |
| Latencies (ms) | 0.229 (0.118 *,0.062 **) | <0.001 (0.054 *,0.314 **) |
| Amp, µV | −0.109 | 0.073 |
| NCV, m/s | −0.224 (−0.155 *,−0.083 **) | <0.001 (0.012 *,0.179 **) |
| Ulnar nerve | N = 272 | |
| Latencies (ms) | 0.152 (0.119 *,0.068 **) | 0.012 (0.052 *,0.267 **) |
| Amp, µV | −0.147 (−0.101 *,−0.044 **) | 0.016 (0.099 *,0.473 **) |
| NCV, m/s | −0.188 (−0.139 *,−0.095 **) | 0.002 (0.024 *,0.123 **) |
| Motor | ||
| Ulnar nerve | N = 283 | |
| Latencies (ms) | 0.178 (0.130 *,0.074 **) | 0.003 (0.029 *,0.217 **) |
| Amp, mV | −0.075 (−0.106 *,−0.64 **) | 0.207 (0.075 *,0.283 **) |
| NCV, m/s | −0.143 (−0.131 *,−0.045 **) | 0.055 (0.080 *,0.546 **) |
| Peroneal nerve | N = 272 | |
| Latencies (ms) | 0.104 | 0.086 |
| Amp, mV | −0.116 | 0.056 |
| NCV, m/s | −0.138 (−0.088 *,−0.065 **) | 0.023 (0.150 *,0.287 **) |
| Tibial nerve | N = 277 | |
| Latencies (ms) | 0.168 (0.199 *,0.153 **) | 0.005 (0.001 *,0.011 **) |
| Amp, mV | −0.165 (−0.094 *,−0.060 **) | 0.006 (0.121 *,0.320 **) |
| NCV, m/s | −0.203 (−0.198 *,−0.152 **) | 0.001 (0.001 *,0.012 **) |
| F-wave | ||
| Median nerve | N = 277 | |
| Latencies (ms) | 0.137 (0.067 *,−0.008 **) | 0.022 (0.266 *,0.890 **) |
| Ulnar nerve | N = 279 | |
| Latencies (ms) | 0.192 (0.147 *,0.088 **) | 0.001 (0.014 *,0.147 **) |
| Peroneal nerve | N = 217 | |
| Latencies (ms) | 0.192 (0.181 *,0.125 **) | 0.005 (0.008 *,0.067 **) |
| Tibial nerve | N = 272 | |
| Latencies (ms) | 0.209 (0.263 *,0.203 **) | 0.001 (<0.001 *,0.001 **) |
| H-reflex | ||
| Tibial nerve | N = 267 | |
| Latencies (ms) | 0.205 (0.226 *,0.174 **) | 0.001 (<0.001 *,0.005 **) |
| LogGDF15 (pg/mL) | ||
|---|---|---|
| Correlation Coefficient (r) | p-Value | |
| Age (years) | 0.083 | 0.162 |
| B.H (cm) | −0.012 | 0.843 |
| B.W (kg) | 0.018 | 0.757 |
| BMI (kg/m2) | 0.029 | 0.621 |
| WC (cm) | 0.254 (0.332 *) | <0.001 (<0.001 *) |
| HC (cm) | 0.165 (0.339 *) | 0.005 (<0.001 *) |
| HbA1c (%) | 0.306 (0.302 *) | <0.001 (<0.001 *) |
| Creatinine | 0.240 (0.146 *) | <0.001 (0.017 *) |
| eGFR (mL∙min−11.73 m−2) | −0.275 (−0.190 *) | <0.001 (<0.002 *) |
| Urine ACR (mg/g) | 0.318 (0.126 *) | <0.001 (0.040 *) |
| HOMA-IR | 0.107 (0.166 *) | 0.079 (0.007 *) |
| hsCRP (mg/L) | 0.102 (0.050 *) | 0.086 (0.419 *) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weng, S.-W.; Chen, W.-C.; Shen, F.-C.; Wang, P.-W.; Chen, J.-F.; Liou, C.-W. Circulating Growth Differentiation Factor 15 Is Associated with Diabetic Neuropathy. J. Clin. Med. 2022, 11, 3033. https://doi.org/10.3390/jcm11113033
Weng S-W, Chen W-C, Shen F-C, Wang P-W, Chen J-F, Liou C-W. Circulating Growth Differentiation Factor 15 Is Associated with Diabetic Neuropathy. Journal of Clinical Medicine. 2022; 11(11):3033. https://doi.org/10.3390/jcm11113033
Chicago/Turabian StyleWeng, Shao-Wen, Wen-Chieh Chen, Feng-Chih Shen, Pei-Wen Wang, Jung-Fu Chen, and Chia-Wei Liou. 2022. "Circulating Growth Differentiation Factor 15 Is Associated with Diabetic Neuropathy" Journal of Clinical Medicine 11, no. 11: 3033. https://doi.org/10.3390/jcm11113033






