Quantitative Microvascular Change Analysis Using a Semi-Automated Software in Macula-off Rhegmatogenous Retinal Detachment Assessed by Swept-Source Optical Coherence Tomography Angiography
Abstract
:1. Introduction
2. Methods
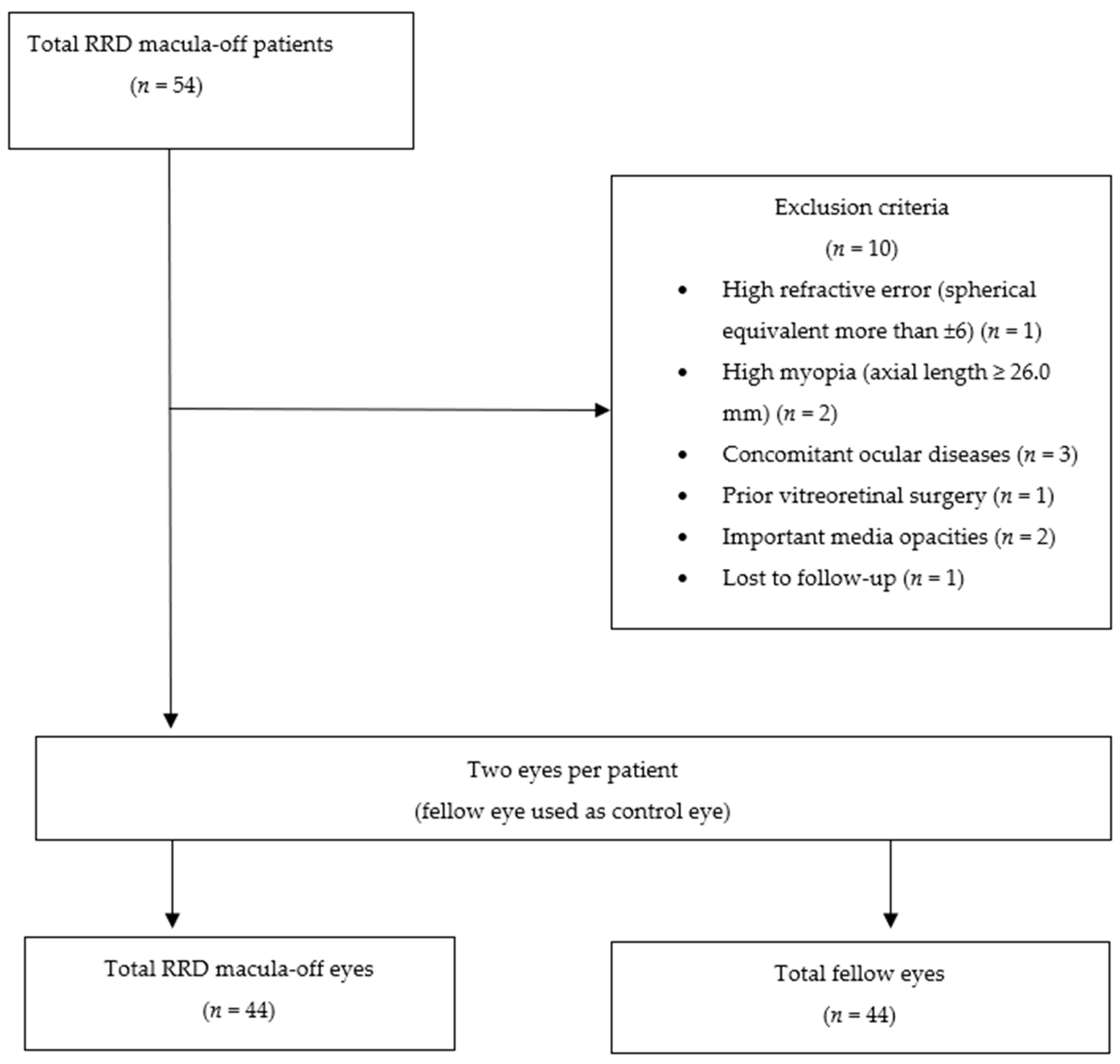
2.1. Study Design
2.2. Study Participants
2.2.1. Surgical Technique
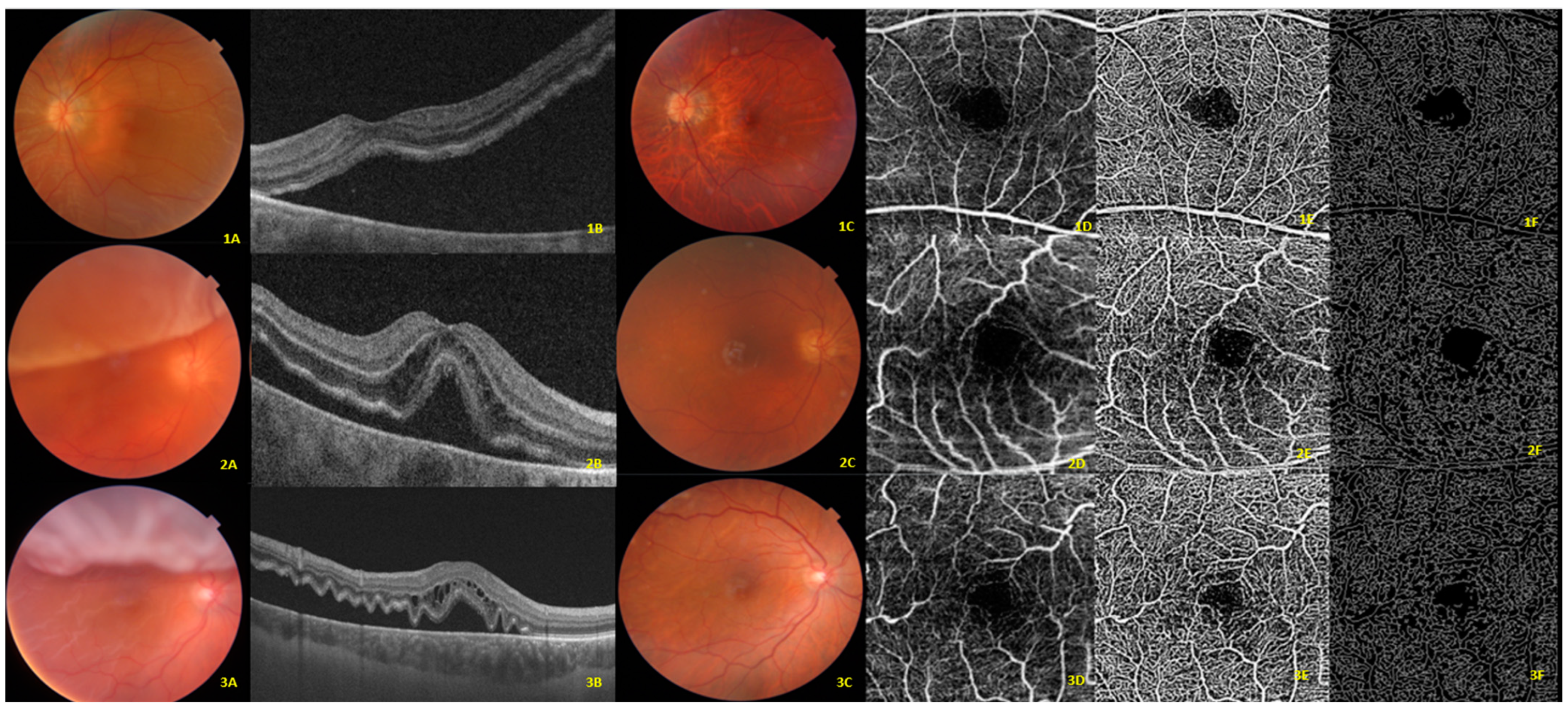
2.2.2. Optical Coherence Tomography Angiography
2.3. Main Outcomes
2.4. Statistical Analysis
3. Results
3.1. Preoperative Demographic and Clinical Characteristics
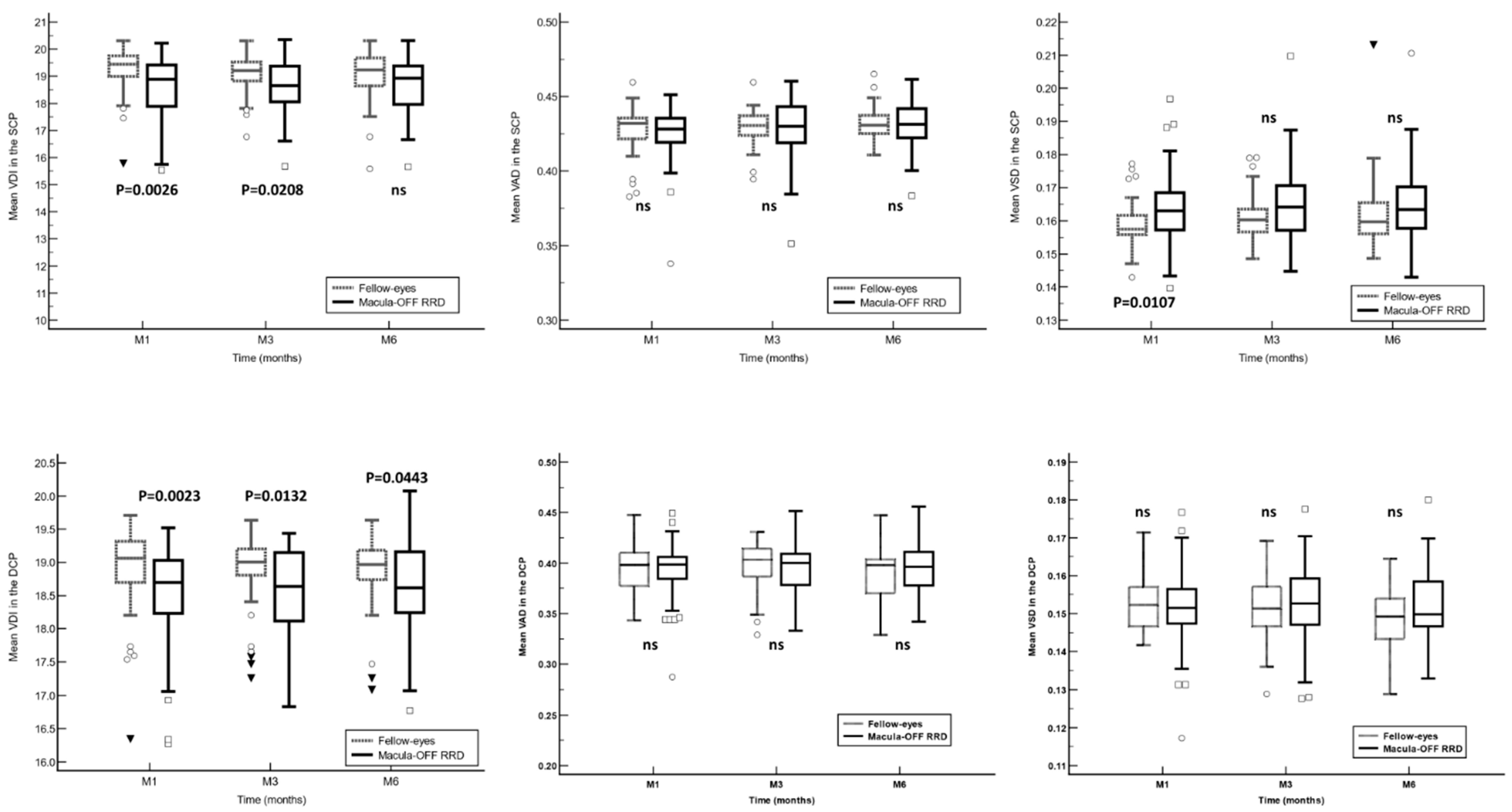
3.2. Semi-Automated Software Parameters
3.3. OCTA Built-In Software Parameters
3.4. Best Corrected Visual Acuity
3.5. Predictive Factors for Functional Outcome
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liao, L.; Zhu, X.H. Advances in the treatment of rhegmatogenous retinal detachment. Int. J. Ophthalmol. 2019, 12, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Nemet, A.; Moshiri, A.; Yiu, G.; Loewenstein, A.; Moisseiev, E. A Review of Innovations in Rhegmatogenous Retinal Detachment Surgical Techniques. J. Ophthalmol. 2017, 2017, 4310643. [Google Scholar] [CrossRef] [PubMed]
- Yorston, D.; Donachie, P.H.J.; Laidlaw, D.A.; Steel, D.H.; Sparrow, J.M.; Aylward, G.W.; Williamson, T.H.; Members of the BEAVRS Retinal Detachment Outcomes Group. Factors affecting visual recovery after successful repair of macula-off retinal detachments: Findings from a large prospective UK cohort study. Eye 2021, 35, 1431–1439. [Google Scholar] [CrossRef] [PubMed]
- Zheng, C.; Wen, D.; Xu, K.; Zhang, X.; Ren, X.; Li, X. Advances in biomaterials as a retinal patch for the repair of rhegmatogenous retinal detachment. Front. Bioeng. Biotechnol. 2022, 10, 997243. [Google Scholar] [CrossRef]
- Haugstad, M.; Moosmayer, S.; Bragadόttir, R. Primary rhegmatogenous retinal detachment—Surgical methods and anatomical outcome. Acta Ophthalmol. 2017, 95, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Sborgia, G.; Niro, A.; Sborgia, L.; Grassi, M.O.; Gigliola, S.; Romano, M.R.; Boscia, F.; Sborgia, A.; Alessio, G. One-year outcomes of 27-gauge versus 25-gauge pars plana vitrectomy for uncomplicated rhegmatogenous retinal detachment repair. Int. J. Retin. Vitr. 2019, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Boden, K.T.; Januschowski, K.; Szurman, P.; Seuthe, A.M.; Rickmann, A.; Seitz, B.; Alsharairi, M.; Leers, S.; Wakili, P. New optical coherence tomography grading system for macula-off rhegmatogenous retinal detachment: How off is off? BMJ Open Ophthalmol. 2021, 6, e000419. [Google Scholar] [CrossRef] [PubMed]
- Auger, G.; Winder, S. Spectral Domain OCT: An Aid to Diagnosis and Surgical Planning of Retinal Detachments. J. Ophthalmol. 2011, 2011, 725362. [Google Scholar] [CrossRef]
- Chua, J.; Sim, R.; Tan, B.; Wong, D.; Yao, X.; Liu, X.; Ting, D.S.W.; Schmidl, D.; Ang, M.; Garhöfer, G.; et al. Optical Coherence Tomography Angiography in Diabetes and Diabetic Retinopathy. J. Clin. Med. 2020, 9, 1723. [Google Scholar] [CrossRef]
- Markan, A.; Agarwal, A.; Arora, A.; Bazgain, K.; Rana, V.; Gupta, V. Novel imaging biomarkers in diabetic retinopathy and diabetic macular edema. Ther. Adv. Ophthalmol. 2020, 12, 2515841420950513. [Google Scholar] [CrossRef]
- Spaide, R.F.; Fujimoto, J.G.; Waheed, N.K.; Sadda, S.R.; Staurenghi, G. Optical coherence tomography angiography. Prog. Retin. Eye Res. 2018, 64, 1–55. [Google Scholar] [CrossRef] [PubMed]
- Laíns, I.; Wang, J.C.; Cui, Y.; Katz, R.; Vingopoulos, F.; Staurenghi, G.; Vavvas, D.G.; Miller, J.W.; Miller, J.B. Retinal applications of swept source optical coherence tomography (OCT) and optical coherence tomography angiography (OCTA). Prog. Retin. Eye Res. 2021, 84, 100951. [Google Scholar] [CrossRef] [PubMed]
- Zheng, F.; Deng, X.; Zhang, Q.; He, J.; Ye, P.; Liu, S.; Li, P.; Zhou, J.; Fang, X. Advances in swept-source optical coherence tomography and optical coherence tomography angiography. Adv. Ophthalmol. Pract. Res. 2023, 3, 67–79. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Zhang, Q.; Chen, C.L.; Wang, R.K. Methods and algorithms for optical coherence tomography-based angiography: A review and comparison. J. Biomed. Opt. 2015, 20, 100901. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Aljaro, P.; Valldeperas, X.; Broc-Iturralde, L.; Romanic-Bubalo, N.; Díaz-Aljaro, I.; Chu, Z.; Wang, R.K.; Zarranz-Ventura, J. Quantitative Microvascular Change Analysis Using a Semi-Automated Algorithm in Macula-on Rhegmatogenous Retinal Detachment Assessed by Swept-Source Optical Coherence Tomography Angiography. Diagnostics 2024, 14, 750. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zhang, A.; Lee, C.S.; Lee, A.Y.; Rezaei, K.A.; Roisman, L.; Miller, A.; Zheng, F.; Gregori, G.; Durbin, M.K.; et al. Projection artifact removal improves visualization and quantitation of macular neovascularization imaged by optical coherence tomography angiography. Ophthalmol. Retin. 2017, 1, 124–136. [Google Scholar] [CrossRef] [PubMed]
- Chu, Z.; Lin, J.; Gao, C.; Xin, C.; Zhang, Q.; Chen, C.L.; Roisman, L.; Gregori, G.; Rosenfeld, P.J.; Wang, R.K. Quantitative assessment of the retinal microvasculature using optical coherence tomography angiography. J. Biomed. Opt. 2016, 21, 66008. [Google Scholar] [CrossRef] [PubMed]
- Reif, R.; Qin, J.; An, L.; Zhi, Z.; Dziennis, S.; Wang, R. Quantifying optical microangiography images obtained from a spectral domain optical coherence tomography system. Int. J. Biomed. Imaging 2012, 2012, 509783. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.Y.; Chu, Z.; Shahidzadeh, A.; Wang, R.K.; Puliafito, C.A.; Kashani, A.H. Quantifying Microvascular Density and Morphology in Diabetic Retinopathy Using Spectral- Domain Optical Coherence Tomography Angiography. Investig. Ophthalmol. Vis. Sci. 2016, 57, OCT362-70. [Google Scholar] [CrossRef]
- Kim, A.Y.; Rodger, D.C.; Shahidzadeh, A.; Chu, Z.; Koulisis, N.; Burkemper, B.; Jiang, X.; Pepple, K.L.; Wang, R.K.; Puliafito, C.A.; et al. Quantifying Retinal Microvascular Changes in Uveitis Using Spectral-Domain Optical Coherence Tomography Angiography. Am. J. Ophthalmol. 2016, 171, 101–112. [Google Scholar] [CrossRef]
- Chen, F.K.; Menghini, M.; Hansen, A.; Mackey, D.A.; Constable, I.J.; Sampson, D.M. Intrasession Repeatability and Interocular Symmetry of Foveal Avascular Zone and Retinal Vessel Density in OCT Angiography. Transl. Vis. Sci. Technol. 2018, 7, 6. [Google Scholar] [CrossRef]
- Diederen, R.M.; La Heij, E.C.; Kessels, A.G.; Goezinne, F.; Liem, A.T.; Hendrikse, F. Scleral buckling surgery after macula-off retinal detachment: Worse visual outcome after more than 6 days. Ophthalmology 2007, 114, 705–709. [Google Scholar] [CrossRef]
- Tan, H.S.; Oberstein, S.Y.; Mura, M.; Bijl, H.M. Air versus gas tamponade in retinal detachment surgery. Br. J. Ophthalmol. 2013, 97, 80–82. [Google Scholar] [CrossRef] [PubMed]
- Hirata, N.; Iwase, T.; Kobayashi, M.; Yamamoto, K.; Ra, E.; Terasaki, H. Correlation between preoperative factors and final visual acuity after successful rhegmatogenous retinal reattachment. Sci. Rep. 2019, 9, 3217. [Google Scholar] [CrossRef]
- Sharma, T.; Challa, J.K.; Ravishankar, K.V.; Murugesan, R. Scleral buckling for retinal detachment: Predictors for anatomic failure. Retina 1994, 14, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Oshima, Y.; Yamanishi, S.; Sawa, M.; Motokura, M.; Harino, S.; Emi, K. Two-year follow-up study comparing primary vitrectomy with scleral buckling for macula-off rhegmatogenous retinal detachment. Jpn. J. Ophthalmol. 2000, 44, 538–549. [Google Scholar] [CrossRef]
- Lee, J.; Seo, E.J.; Yoon, Y.H. Rhegmatogenous retinal detachment induces more severe macular capillary changes than central serous chorioretinopathy. Sci. Rep. 2022, 12, 7018. [Google Scholar] [CrossRef] [PubMed]
- Chatziralli, I.; Chatzirallis, A.; Kazantzis, D.; Dimitriou, E.; Machairoudia, G.; Theodossiadis, G.; Parikakis, E.; Theodossiadis, P. Predictive Factors for Long-Term Postoperative Visual Outcome in Patients with Macula-Off Rhegmatogenous Retinal Detachment Treated with Vitrectomy. Ophthalmologica 2021, 244, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Bonfiglio, V.; Ortisi, E.; Scollo, D.; Reibaldi, M.; Russo, A.; Pizzo, A.; Faro, G.; Macchi, I.; Fallico, M.; Toro, M.D.; et al. Vascular changes after vitrectomy for rhegmatogenous retinal detachment: Optical coherence tomography angiography study. Acta Ophthalmol. 2020, 98, e563–e569. [Google Scholar] [CrossRef]
- Lee, J.Y.; Kim, J.Y.; Lee, S.Y.; Jeong, J.H.; Lee, E.K. Foveal Microvascular Structures in Eyes with Silicone Oil Tamponade for Rhegmatogenous Retinal Detachment: A Swept- source Optical Coherence Tomography Angiography Study. Sci. Rep. 2020, 10, 2555. [Google Scholar] [CrossRef]
- McKay, K.M.; Vingopoulos, F.; Wang, J.C.; Papakostas, T.D.; Silverman, R.F.; Marmalidou, A.; Lains, I.; Eliott, D.; Vavvas, D.G.; Kim, L.A.; et al. Retinal Microvasculature Changes After Repair of Macula-off Retinal Detachment Assessed with Optical Coherence Tomography Angiography. Clin. Ophthalmol. 2020, 14, 1759–1767. [Google Scholar] [CrossRef] [PubMed]
- Woo, J.M.; Yoon, Y.S.; Woo, J.E.; Min, J.K. Foveal Avascular Zone Area Changes Analyzed Using OCT Angiography after Successful Rhegmatogenous Retinal Detachment Repair. Curr. Eye Res. 2018, 43, 674–678. [Google Scholar] [CrossRef] [PubMed]
- Machairoudia, G.; Kazantzis, D.; Chatziralli, I.; Theodossiadis, G.; Georgalas, I.; Theodossiadis, P. Microvascular changes after pars plana vitrectomy for rhegmatogenous retinal detachment repair: A comparative study based on gas tamponade agent. Eur. J. Ophthalmol. 2023. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Kanai, M.; Busch, C.; Wakabayashi, T. Foveal avascular zone area after macula-off rhegmatogenous retinal detachment repair: An optical coherence tomography angiography study. Graefe’s Arch. Clin. Exp. Ophthalmol. 2017, 255, 2071–2072. [Google Scholar] [CrossRef] [PubMed]
- Piccolino, C. Vascular Changes in Rhegmatogenous Retinal Detachment. Ophthalmologica 1983, 86, 17–24. [Google Scholar] [CrossRef]
- Agarwal, A.; Aggarwal, K.; Akella, M.; Agrawal, R.; Khandelwal, N.; Bansal, R.; Sinh, R.; Gupta, V. Fractal Dimension and Optical Coherence Tomography Angiography Features of the Central Macula After Repair of Rhegmatogenous Retinal Detachments. Retina 2019, 39, 2167–2177. [Google Scholar] [CrossRef] [PubMed]
- Çetinkaya-Yaprak, A.; Küçük, M.F.; Yaprak, L.; Erol, M.K. Change in retinal and choroidal microvascular structures after rhegmatogenous retinal detachment surgery and effects on visual recovery. J. Français D’ophtalmologie 2021, 44, 804–812. [Google Scholar] [CrossRef] [PubMed]
- Hong, E.H.; Cho, H.; Kim, D.R.; Kang, M.H.; Shin, Y.U.; Seong, M. Changes in Retinal Vessel and Retinal Layer Thickness After Vitrectomy in Retinal Detachment via Swept- Source OCT Angiography. Investig. Ophthalmol. Vis. Sci. 2020, 61, 35. [Google Scholar] [CrossRef]
- Wang, H.; Xu, X.; Sun, X.; Ma, Y.; Sun, T. Macular perfusion changes assessed with optical coherence tomography angiography after vitrectomy for rhegmatogenous retinal detachment. Graefe’s Arch. Clin. Exp. Ophthalmol. 2019, 257, 733–740. [Google Scholar] [CrossRef]
- Ricker, L.J.; Kijlstra, A.; de Jager, W.; Liem, A.T.; Hendrikse, F.; La Heij, E.C. Chemokine levels in subretinal fluid obtained during scleral buckling surgery after rhegmatogenous retinal detachment. Investig. Ophthalmol. Vis. Sci. 2010, 51, 4143–4150. [Google Scholar] [CrossRef]
- Sato, M.; Iwase, T. Differences in Vascular Density between Detached and Nondetached Areas in Eyes with Rhegmatogenous Retinal Detachment. J. Clin. Med. 2022, 11, 2881. [Google Scholar] [CrossRef] [PubMed]
| Study Sample (n = 44) | |
|---|---|
| Age, years | |
| Mean ± SD | 68.9 ± 11.8 |
| Median (IqR) | 68.0 (62.3 to 77.1) |
| Sex, n (%) | |
| Women | 11 (25.0) |
| Men | 33 (75.0) |
| Systemic diseases, n (%) | |
| DM | 13 (29.5) |
| HBP | 22 (50.0) |
| Dyslipidemia | 22 (50.0) |
| Smoker | 5 (12.2) |
| Other | 13 (29.5) |
| Eye, n (%) | |
| Right | 23 (52.3) |
| Left | 21 (47.7) |
| PVR, n (%) | |
| No | 25 (56.8) |
| Degree A | 7 (15.9) |
| Degree B | 9 (20.5) |
| Degree C | 3 (6.8) |
| Time, n (%) | |
| <7 days | 28 (63.6) |
| ≥7 days | 16 (36.4) |
| Extension, n (%) | |
| 1 quadrant | 1 (2.3) |
| 2 quadrants | 27 (61.4) |
| 3 quadrants | 7 (15.9) |
| 4 quadrants | 9 (20.5) |
| Lens status, n (%) | |
| Phakia | 21 (47.7) |
| Pseudophakia | 23 (52.3) |
| IOP, mmHg | |
| Mean ± SD | 16.4 ± 3.3 |
| Median (IqR) | 16.0 (16.0 to 18.0) |
| Axial length, mm | |
| Mean ± SD | 24.9 ± 1.6 |
| Median (IqR) | 24.9 (23.8 to 26.0) |
| BCVA, logMAR | |
| Mean ± SD | 0.83 ± 0.29 |
| Median (IqR) | 1.00 (0.70 to 1.00) |
| CMT ⁂, µm | |
| Mean ± SD | 288.0 ± 25.5 |
| Median (IqR) | 283.0 (275.5 to 304.0) |
| Superficial Capillary Plexus (n = 44) | |||||
|---|---|---|---|---|---|
| Preoperative * | Month 1 | Month 3 | Month 6 | p | |
| VDI | |||||
| Mean ± SE | 19.2 ± 0.1 | 18.6 ± 0.2 | 18.6 ± 0.2 | 18.7 ± 0.2 | 0.0087 a |
| 95% CI | 19.0–19.4 | 18.3–18.9 | 18.3–18.9 | 18.3–19.0 | 0.9649 b |
| VAD | |||||
| Mean ± SE | 0.43 ± 0.00 | 0.43 ± 0.00 | 0.43 ± 0.00 | 0.43 ± 0.00 | 0.2729 a |
| 95% CI | 0.42–0.43 | 0.43–0.44 | 0.43–0.44 | 0.42–0.43 | 0.1854 b |
| VSD | |||||
| Mean ± SE | 0.16 ± 0.00 | 0.17 ± 0.00 | 0.17 ± 0.00 | 0.16 ± 0.00 | 0.0278 a |
| 95% CI | 0.16–0.16 | 0.16–0.17 | 0.16–0.17 | 0.16–0.17 | 0.5748 b |
| Deep capillary plexus (n = 44) | |||||
| Preoperative * | Month 1 | Month 3 | Month 6 | p | |
| VDI | |||||
| Mean ± SE | 18.9 ± 0.1 | 18.5 ± 0.2 | 18.7 ± 0.1 | 18.6 ± 0.1 | 0.0402 a |
| 95% CI | 18.7–19.1 | 18.2–18.8 | 18.5–19.0 | 18.4.18.9 | 0.2926 b |
| VAD | |||||
| Mean ± SE | 0.40 ± 0.00 | 0.40 ± 0.01 | 0.40 ± 0.01 | 0.39 ± 0.01 | 0.5564 a |
| 95% CI | 0.39–0.40 | 0.39–0.41 | 0.38–0.41 | 0.38–0.40 | 0.6508 b |
| VSD | |||||
| Mean ± SE | 0.15 ± 0.00 | 0.15 ± 0.00 | 0.15 ± 0.00 | 0.15 ± 0.00 | 0.5210 a |
| 95% CI | 0.15–0.15 | 0.15–0.16 | 0.15–0.16 | 0.15–0.15 | 0.9003 b |
| Fellow Eyes (n = 44 Eyes) | ||||||||
|---|---|---|---|---|---|---|---|---|
| FSCP | PFSCP | WSCP | FDCP | PFDCP | WDCP | FAZ | CMT | |
| Preoperative | ||||||||
| Mean ± SE | 20.9 ± 0.7 | 48.3 ± 0.3 | 42.8 ± 0.3 | 20.8 ± 1.1 | 56.7 ± 0.4 | 49.5 ± 0.4 | 0.24 ± 0.02 | 288.0 ± 3.8 |
| 95% CI | 19.6 to 22.3 | 47.7 to 48.9 | 42.3 to 43.4 | 18.5 to 23.0 | 55.8 to 57.6 | 48.8 to 50.3 | 0.21 to 0.27 | 280.3 to 295.8 |
| Month 1 | ||||||||
| Mean ± SE | 20.8 ± 0.7 | 48.4 ± 0.3 | 42.9 ± 0.3 | 20.9 ± 1.1 | 56.7 ± 0.5 | 49.5 ± 0.4 | 0.24 ± 0.02 | 287.5 ± 3.9 |
| 95% CI | 19.4 to 22.2 | 47.7 to 49.1 | 42.3 to 43.5 | 18.8 to 23.1 | 55.7 to 57.6 | 48.8 to 50.3 | 0.22 to 0.27 | 279.7 to 295.3 |
| Month 3 | ||||||||
| Mean ± SE | 21.0 ± 0.7 | 48.4 ± 0.3 | 42.9 ± 0.3 | 20.9 ± 1.1 | 56.7 ± 0.5 | 49.5 ± 0.4 | 0.25 ± 0.01 | 287.6 ± 4.0 |
| 95% CI | 19.6 to 22.3 | 47.8 to 49.1 | 42.4 to 43.5 | 18.7 to 23.1 | 55.7 to 57.6 | 48.8 to 50.3 | 0.22 to 0.27 | 279.5 to 295.7 |
| Month 6 | ||||||||
| Mean ± SE | 20.9 ± 0.7 | 48.4 ± 0.3 | 42.9 ± 0.3 | 21.0 ± 1.1 | 56.7 ± 0.5 | 49.5 ± 0.4 | 0.24 ± 0.01 | 285.2 ± 4.4 |
| 95% CI | 19.6 to 22.3 | 47.8 to 49.1 | 42.3 to 43.5 | 18.8 to 23.2 | 55.8 to 57.6 | 48.7 to 50.4 | 0.22 to 0.27 | 276.3 to 294.1 |
| Intragroup Significance | 0.6932 | 0.3363 | 0.3367 | 0.1053 | 0.8919 | 0.7830 | 0.6644 | 0.2845 |
| RRD eyes (n = 44 eyes) | ||||||||
| FSCP | PFSCP | WSCP | FDCP | PFDCP | WDCP | FAZ | CMT | |
| Preoperative * | ||||||||
| Mean ± SE | 20.9 ± 0.7 | 48.3 ± 0.3 | 42.8 ± 0.3 | 20.8 ± 1.1 | 56.7 ± 0.4 | 49.5 ± 0.4 | 0.24 ± 0.02 | 288.0 ± 3.8 |
| 95% CI | 19.6 to 22.3 | 47.7 to 48.9 | 42.3 to 43.4 | 18.5 to 23.0 | 55.8 to 57.6 | 48.8 to 50.3 | 0.21 to 0.27 | 280.3 to 295.8 |
| Month 1 | ||||||||
| Mean ± SE | 22.9 ± 0.9 | 47.4 ± 0.3 | 42.5 ± 0.3 | 21.3 ± 0.7 | 55.4 ± 0.6 | 48.6 ± 0.4 | 0.25 ± 0.01 | 292.3 ± 6.6 |
| 95% CI | 21.0 to 24.8 | 46.8 to 48.1 | 41.9 to 43.1 | 19.9 to 22.6 | 54.3 to 56.5 | 47.7 to 49.5 | 0.23 to 0.28 | 278.9 to 305.7 |
| Month 3 | ||||||||
| Mean ± SE | 21.8 ± 0.7 | 46.5 ± 0.3 | 41.6 ± 0.3 | 20.5 ± 0.7 | 54.1 ± 0.6 | 47.4 ± 0.5 | 0.26 ± 0.01 | 269.3 ± 6.4 |
| 95% CI | 20.4 to 23.3 | 45.9 to 47.2 | 41.1 to 42.1 | 19.2 to 21.8 | 52.8 to 55.4 | 46.4 to 48.4 | 0.23 to 0.28 | 256.3 to 282.3 |
| Month 6 | ||||||||
| Mean ± SE | 20.0 ± 0.7 | 47.8 ± 0.4 | 40.8 ± 0.3 | 20.0 ± 0.7 | 52.9 ± 0.7 | 46.3 ± 0.6 | 0.26 ± 0.01 | 258.3 ± 6.4 |
| 95% CI | 18.6 to 21.3 | 45.0 to 46.6 | 40.2 to 41.4 | 18.6 to 21.3 | 51.4 to 54.3 | 45.1 to 47.4 | 0.24 to 0.28 | 245.5 to 271.1 |
| Intragroup Significance a | 0.0459 | <0.0001 | <0.0001 | 0.3006 | <0.0001 | <0.0001 | 0.0194 | <0.0001 |
| Intragroup Significance b | 0.0052 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.0235 | <0.0001 |
| Study Sample (n = 44) | ||
|---|---|---|
| Variable | OR (95% CI) | p |
| Age a | 1.02 (0.97 to 1.07) | 0.5104 |
| Sex | ||
| Ref Men | ||
| Women | 1.29 (0.32 to 5.28) | 0.7236 |
| DM | ||
| Ref No | ||
| Yes | 1.85 (0.47 to 7.32) | 0.3789 |
| HBP | ||
| Ref No | ||
| Yes | 1.46 (0.44 to 4.88) | 0.5404 |
| Dyslipidemia | ||
| Ref No | ||
| Yes | 1.46 (0.44 to 4.88) | 0.5404 |
| RD extension | ||
| Ref 1 quadrant | ||
| ≥2 quadrants | 1.86 (0.54 to 6.41) | 0.3279 |
| Time | ||
| Ref < 7 days | ||
| ≥7 days | 0.83 (0.24 to 2.89) | 0.7721 |
| PVR | ||
| Ref No | ||
| Yes | 1.35 (0.40 to 4.57) | 0.6328 |
| Axial length b | 1.01 (0.53 to 1.91) | 0.9853 |
| Preop BCVA | 11.6 (7.45 to 19.3) | 0.0037 |
| Preop VDI SCP c,1 | 0.56 (0.21 to 1.49) | 0.2451 |
| Preop VAD SCP d,1 | 0.48 (0.23 to 3.94) | 0.5820 |
| Preop VSD SCP d,1 | 1.83 (0.69 to 4.81) | 0.6182 |
| Preop VDI DCP c,1 | 1.20 (0.40 to 3.59) | 0.7470 |
| Preop VAD DCP d,1 | 0.43 (0.09 to 2.78) | 0.3058 |
| Preop VSD DCP d,1 | 0.50 (0.21 to 1.23) | 0.2428 |
| Mean change 2 VDI SCP e | 1.10 (0.61 to 1.99) | 0.7480 |
| Mean change 2 VAD SCP d | 1.55 (0.09 to 2.62) | 0.4255 |
| Mean change 2 VSD SCP d | 1.63 (0.94 to 2.71) | 0.7669 |
| Mean change 2 VDI DCP e | 0.96 (0.41 to 2.25) | 0.9326 |
| Mean change 2 VAD DCP d | 1.21 (0.24 to 1.68) | 0.3263 |
| Mean change 2 VSD DCP d | 1.28 (0.60 to 2.72) | 0.3507 |
| Preop FSCP c,1 | 1.05 (0.92 to 1.20) | 0.4818 |
| Preop PFSCP c,1 | 1.21 (0.83 to 1.76) | 0.3230 |
| Preop WSCP c,1 | 1.32 (0.85 to 2.05) | 0.2168 |
| Preop FDCP c,1 | 1.04 (0.94 to 1.14) | 0.4803 |
| Preop PFDCP c,1 | 1.16 (0.93 to 1.46) | 0.1885 |
| Preop WDCP c,1 | 1.25 (0.95 to 1.66) | 0.1099 |
| FAZ | 0.06 (0.00 to 32.67) | 0.3851 |
| CMT | 1.02 (0.99 to 1.04) | 0.2624 |
| Mean change FSCP 3 | 2.48 (0.68 to 9.04) | 0.1685 |
| Mean change PFSCP 3 | 0.78 (0.38 to 1.58) | 0.4833 |
| Mean change WSCP 3 | 0.84 (0.37 to 1.88) | 0.6629 |
| Mean change FDCP 3 | 0.69 (0.31 to 1.54) | 0.3628 |
| Mean change PFDCP 3 | 1.06 (0.44 to 2.53) | 0.8961 |
| Mean change WDCP 3 | 0.93 (0.35 to 2.48) | 0.8859 |
| Mean change FAZ 3 | 0.94 (0.42 to 3.07) | 0.6551 |
| Mean change CMT 3,f | 1.03 (0.99 to 1.07) | 0.1617 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Díaz-Aljaro, P.; Zarranz-Ventura, J.; Broc-Iturralde, L.; Romanic-Bubalo, N.; Díaz-Aljaro, I.; Chu, Z.; Wang, R.K.; Valldeperas, X. Quantitative Microvascular Change Analysis Using a Semi-Automated Software in Macula-off Rhegmatogenous Retinal Detachment Assessed by Swept-Source Optical Coherence Tomography Angiography. J. Clin. Med. 2024, 13, 2835. https://doi.org/10.3390/jcm13102835
Díaz-Aljaro P, Zarranz-Ventura J, Broc-Iturralde L, Romanic-Bubalo N, Díaz-Aljaro I, Chu Z, Wang RK, Valldeperas X. Quantitative Microvascular Change Analysis Using a Semi-Automated Software in Macula-off Rhegmatogenous Retinal Detachment Assessed by Swept-Source Optical Coherence Tomography Angiography. Journal of Clinical Medicine. 2024; 13(10):2835. https://doi.org/10.3390/jcm13102835
Chicago/Turabian StyleDíaz-Aljaro, Pablo, Javier Zarranz-Ventura, Laura Broc-Iturralde, Nevena Romanic-Bubalo, Ignacio Díaz-Aljaro, Zhongdi Chu, Ruikang K. Wang, and Xavier Valldeperas. 2024. "Quantitative Microvascular Change Analysis Using a Semi-Automated Software in Macula-off Rhegmatogenous Retinal Detachment Assessed by Swept-Source Optical Coherence Tomography Angiography" Journal of Clinical Medicine 13, no. 10: 2835. https://doi.org/10.3390/jcm13102835
APA StyleDíaz-Aljaro, P., Zarranz-Ventura, J., Broc-Iturralde, L., Romanic-Bubalo, N., Díaz-Aljaro, I., Chu, Z., Wang, R. K., & Valldeperas, X. (2024). Quantitative Microvascular Change Analysis Using a Semi-Automated Software in Macula-off Rhegmatogenous Retinal Detachment Assessed by Swept-Source Optical Coherence Tomography Angiography. Journal of Clinical Medicine, 13(10), 2835. https://doi.org/10.3390/jcm13102835








