Ultrasonographic Evaluation of the Second Stage of Labor according to the Mode of Delivery: A Prospective Study in Greece
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design/Parameters
2.2. Technique
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liao, J.B.; Buhimschi, C.S.; Norwitz, E.R. Normal labor: Mechanism and duration. Obstet. Gynecol. Clin. N. Am. 2005, 32, 145–164. [Google Scholar] [CrossRef] [PubMed]
- Wright, A.; Nassar, A.H.; Visser, G.; Ramasauskaite, D.; Theron, G.; Motherhood, F.S.; Newborn Health, C. FIGO good clinical practice paper: Management of the second stage of labor. Int. J. Gynaecol. Obstet. 2021, 152, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.W.; Caughey, A.B. Defining and Managing Normal and Abnormal Second Stage of Labor. Obstet. Gynecol. Clin. N. Am. 2017, 44, 547–566. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, E.F.; Simoneau, G.; Ciampi, A.; Warrick, P.; Collins, K.; Smith, S.; Garite, T.J. Descent of the fetal head (station) during the first stage of labor. Am. J. Obstet. Gynecol. 2016, 214, 360.e1–360.e6. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Landy, H.J.; Ware Branch, D.; Burkman, R.; Haberman, S.; Gregory, K.D.; Hatjis, C.G.; Ramirez, M.M.; Bailit, J.L.; Gonzalez-Quintero, V.H.; et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet. Gynecol. 2010, 116, 1281–1287. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Troendle, J.F.; Yancey, M.K. Reassessing the labor curve in nulliparous women. Am. J. Obstet. Gynecol. 2002, 187, 824–828. [Google Scholar] [CrossRef] [PubMed]
- Caughey, A.B.; Cahill, A.G.; Guise, J.M.; Rouse, D.J.; American College of Obstetricians and Gynecologists and Society for Maternal–Fetal Medicine. Safe prevention of the primary cesarean delivery. Am. J. Obstet. Gynecol. 2014, 210, 179–193. [Google Scholar] [CrossRef]
- Oboro, V.O.; Tabowei, T.O.; Bosah, J.O. Fetal station at the time of labour arrest and risk of caesarean delivery. J. Obstet. Gynaecol. 2005, 25, 20–22. [Google Scholar] [CrossRef]
- Akmal, S.; Kametas, N.; Tsoi, E.; Hargreaves, C.; Nicolaides, K.H. Comparison of transvaginal digital examination with intrapartum sonography to determine fetal head position before instrumental delivery. Ultrasound Obstet. Gynecol. 2003, 21, 437–440. [Google Scholar] [CrossRef]
- Dietz, H.P.; Lanzarone, V. Measuring engagement of the fetal head: Validity and reproducibility of a new ultrasound technique. Ultrasound Obstet. Gynecol. 2005, 25, 165–168. [Google Scholar] [CrossRef]
- Dupuis, O.; Ruimark, S.; Corinne, D.; Simone, T.; Andre, D.; Rene-Charles, R. Fetal head position during the second stage of labor: Comparison of digital vaginal examination and transabdominal ultrasonographic examination. Eur. J. Obstet. Gynecol. Reprod. Biol. 2005, 123, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Ghi, T.; Farina, A.; Pedrazzi, A.; Rizzo, N.; Pelusi, G.; Pilu, G. Diagnosis of station and rotation of the fetal head in the second stage of labor with intrapartum translabial ultrasound. Ultrasound Obstet. Gynecol. 2009, 33, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Sherer, D.M.; Miodovnik, M.; Bradley, K.S.; Langer, O. Intrapartum fetal head position I: Comparison between transvaginal digital examination and transabdominal ultrasound assessment during the active stage of labor. Ultrasound Obstet. Gynecol. 2002, 19, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Sherer, D.M.; Miodovnik, M.; Bradley, K.S.; Langer, O. Intrapartum fetal head position II: Comparison between transvaginal digital examination and transabdominal ultrasound assessment during the second stage of labor. Ultrasound Obstet. Gynecol. 2002, 19, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Tutschek, B.; Torkildsen, E.A.; Eggebo, T.M. Comparison between ultrasound parameters and clinical examination to assess fetal head station in labor. Ultrasound Obstet. Gynecol. 2013, 41, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Eggebo, T.M.; Hassan, W.A.; Salvesen, K.A.; Torkildsen, E.A.; Ostborg, T.B.; Lees, C.C. Prediction of delivery mode by ultrasound-assessed fetal position in nulliparous women with prolonged first stage of labor. Ultrasound Obstet. Gynecol. 2015, 46, 606–610. [Google Scholar] [CrossRef] [PubMed]
- Eggebo, T.M.; Heien, C.; Okland, I.; Gjessing, L.K.; Romundstad, P.; Salvesen, K.A. Ultrasound assessment of fetal head-perineum distance before induction of labor. Ultrasound Obstet. Gynecol. 2008, 32, 199–204. [Google Scholar] [CrossRef]
- Kalache, K.D.; Duckelmann, A.M.; Michaelis, S.A.; Lange, J.; Cichon, G.; Dudenhausen, J.W. Transperineal ultrasound imaging in prolonged second stage of labor with occipitoanterior presenting fetuses: How well does the ’angle of progression’ predict the mode of delivery? Ultrasound Obstet. Gynecol. 2009, 33, 326–330. [Google Scholar] [CrossRef]
- Torkildsen, E.A.; Salvesen, K.A.; Eggebo, T.M. Prediction of delivery mode with transperineal ultrasound in women with prolonged first stage of labor. Ultrasound Obstet. Gynecol. 2011, 37, 702–708. [Google Scholar] [CrossRef]
- Tutschek, B.; Braun, T.; Chantraine, F.; Henrich, W. A study of progress of labour using intrapartum translabial ultrasound, assessing head station, direction, and angle of descent. BJOG Int. J. Obstet. Gynaecol. 2011, 118, 62–69. [Google Scholar] [CrossRef]
- Ghi, T.; Eggebo, T.; Lees, C.; Kalache, K.; Rozenberg, P.; Youssef, A.; Salomon, L.J.; Tutschek, B. ISUOG Practice Guidelines: Intrapartum ultrasound. Ultrasound Obstet. Gynecol. 2018, 52, 128–139. [Google Scholar] [CrossRef]
- Tsakiridis, I.; Mamopoulos, A.; Athanasiadis, A.; Dagklis, T. Induction of Labor: An Overview of Guidelines. Obstet. Gynecol. Surv. 2020, 75, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Tsakiridis, I.; Giouleka, S.; Mamopoulos, A.; Athanasiadis, A.; Daniilidis, A.; Dagklis, T. Operative vaginal delivery: A review of four national guidelines. J. Perinat. Med. 2020, 48, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Barbera, A.F.; Pombar, X.; Perugino, G.; Lezotte, D.C.; Hobbins, J.C. A new method to assess fetal head descent in labor with transperineal ultrasound. Ultrasound Obstet. Gynecol. 2009, 33, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Eggebo, T.M.; Gjessing, L.K.; Heien, C.; Smedvig, E.; Okland, I.; Romundstad, P.; Salvesen, K.A. Prediction of labor and delivery by transperineal ultrasound in pregnancies with prelabor rupture of membranes at term. Ultrasound Obstet. Gynecol. 2006, 27, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Walsh, J.M.; Hehir, M.P.; Robson, M.S.; Mahony, R.M. Mode of delivery and outcomes by birth weight among spontaneous and induced singleton cephalic nulliparous labors. Int. J. Gynaecol. Obstet. 2015, 129, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Lundborg, L.; Aberg, K.; Sandstrom, A.; Liu, X.; Tilden, E.; Stephansson, O.; Ahlberg, M. Association between first and second stage of labour duration and mode of delivery: A population-based cohort study. Paediatr. Perinat. Epidemiol. 2022, 36, 358–367. [Google Scholar] [CrossRef]
- Gardberg, M.; Tuppurainen, M. Effects of persistent occiput posterior presentation on mode of delivery. Z. Geburtshilfe Perinatol. 1994, 198, 117–119. [Google Scholar]
- Dall’Asta, A.; Angeli, L.; Masturzo, B.; Volpe, N.; Schera, G.B.L.; Di Pasquo, E.; Girlando, F.; Attini, R.; Menato, G.; Frusca, T.; et al. Prediction of spontaneous vaginal delivery in nulliparous women with a prolonged second stage of labor: The value of intrapartum ultrasound. Am. J. Obstet. Gynecol. 2019, 221, 642.e1–642.e13. [Google Scholar] [CrossRef]
- Jung, J.E.; Lee, Y.J. Intrapartum transperineal ultrasound: Angle of progression to evaluate and predict the mode of delivery and labor progression. Obstet. Gynecol. Sci. 2023, 67, 1–16. [Google Scholar] [CrossRef]
- Marsoosi, V.; Pirjani, R.; Mansouri, B.; Eslamian, L.; Jamal, A.; Heidari, R.; Rahimi-Foroushani, A. Role of ’angle of progression’ in prediction of delivery mode. J. Obstet. Gynaecol. Res. 2015, 41, 1693–1699. [Google Scholar] [CrossRef]
- Bibbo, C.; Rouse, C.E.; Cantonwine, D.E.; Little, S.E.; McElrath, T.F.; Robinson, J.N. Angle of Progression on Ultrasound in the Second Stage of Labor and Spontaneous Vaginal Delivery. Am. J. Perinatol. 2018, 35, 413–420. [Google Scholar] [CrossRef]
- Gurewitsch, E.D.; Johnson, E.; Allen, R.H.; Diament, P.; Fong, J.; Weinstein, D.; Chervenak, F.A. The descent curve of the grand multiparous woman. Am. J. Obstet. Gynecol. 2003, 189, 1036–1041. [Google Scholar] [CrossRef]

| Characteristics | Mode of Delivery | |||
|---|---|---|---|---|
| Vaginal Delivery (VD) n = 60 (73.2%) | Operative Vaginal Delivery (OVD) n = 11 (13.4%) | Cesarean Section (CS) n = 11 (13.4%) | p-Value | |
| Maternal age (years) | 27.7 (6.9) | 29.1 (4.3) | 28.9 (6.7) | 0.736 |
| Maternal BMI (kg/m2) | 29.5 (5.3) | 29.6 (4.4) | 30.4 (4.6) | 0.876 |
| Gestational age at delivery (weeks) | 39 (1.4) | 39.3 (1.2) | 39.4 (0.9) | 0.053 |
| Parity | 1.3 (0.6) | 1.3 (1.2) | 1 (0.3) | 0.545 |
| Birth weight (g) | 3161 (508) | 3429 (249) | 3572 (416) | 0.015 |
| Duration of second stage of labor (minutes) | 65.3 (57.6) | 88.6 (67.6) | 160 (61.2) | <0.001 |
| Total duration of labor (hours) | 8.8 (4.9) | 14.2 (5.8) | 16.1 (8.3) | <0.001 |
| Mode of Delivery | Head Position | ORs | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Occiput Anterior | Occiput Posterior | ||||
| Vaginal delivery | 58 (96.7%) | 2 (3.3%) | 24.167 | 3.8–152.5 | <0.001 |
| Operative vaginal delivery | 10 (90.9%) | 1 (9.1%) | 8.333 | 0.7–89.4 | 0.080 |
| Cesarean section | 6 (54.5%) | 5 (45.5%) | Reference | ||
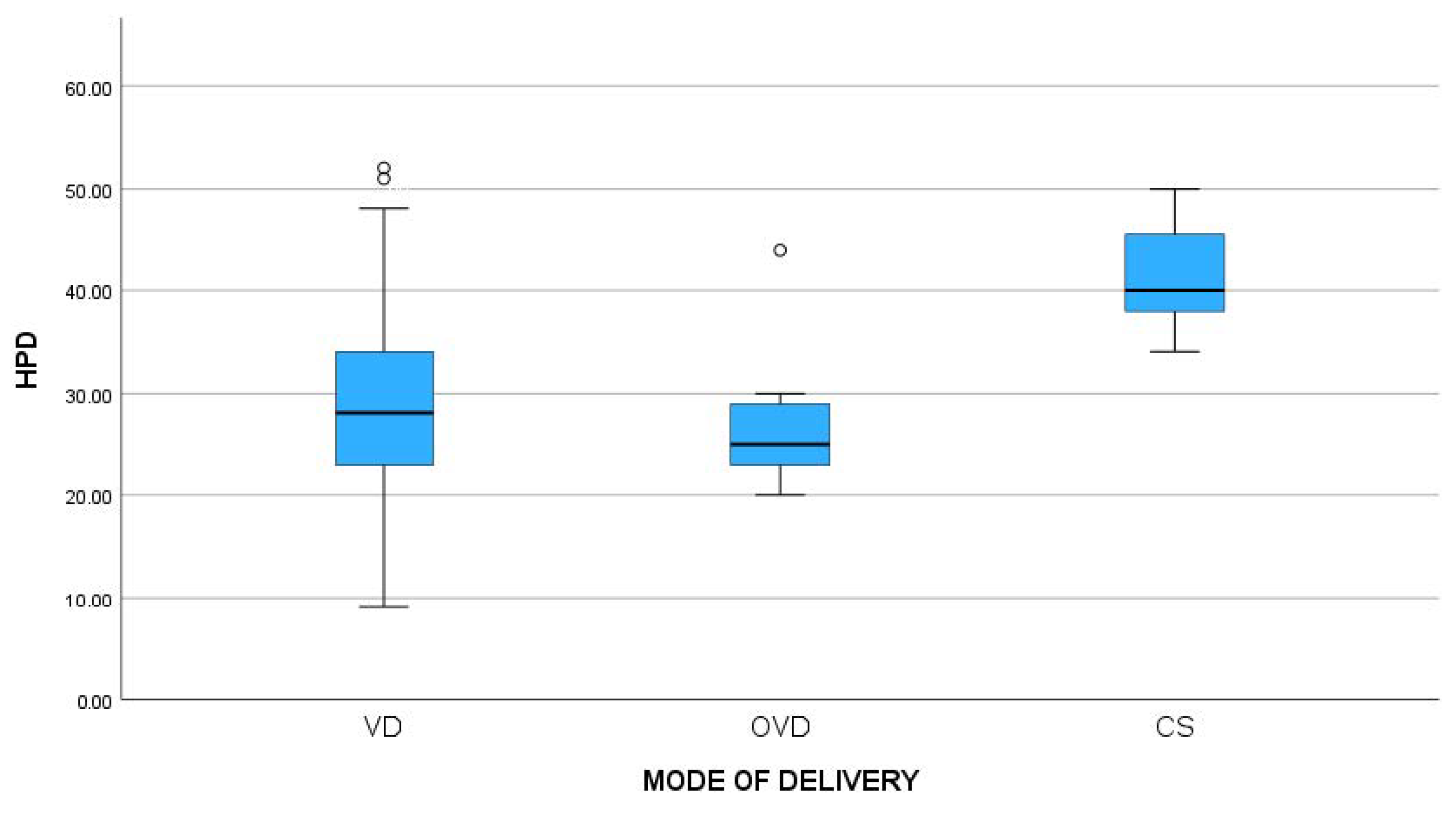
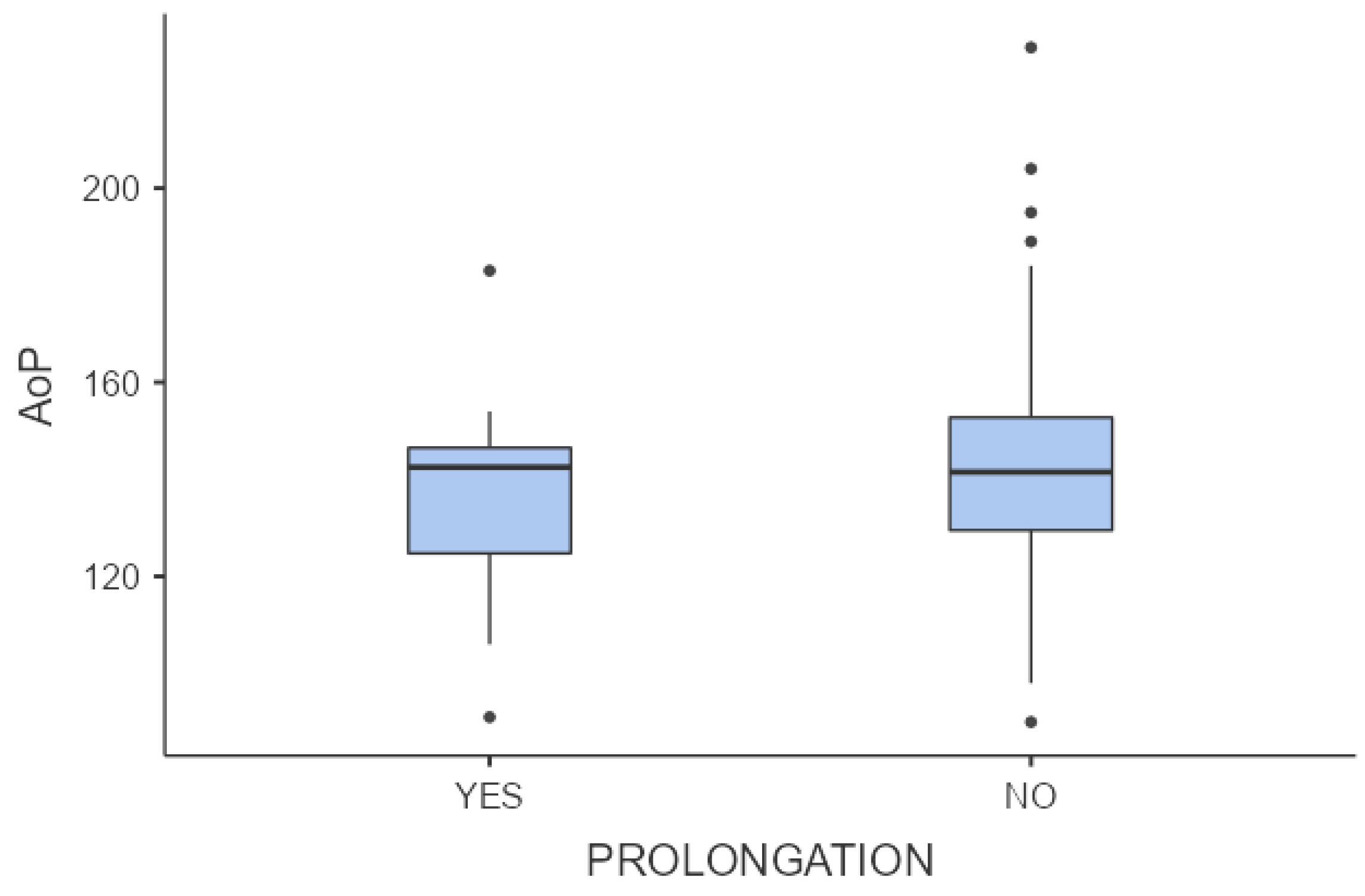
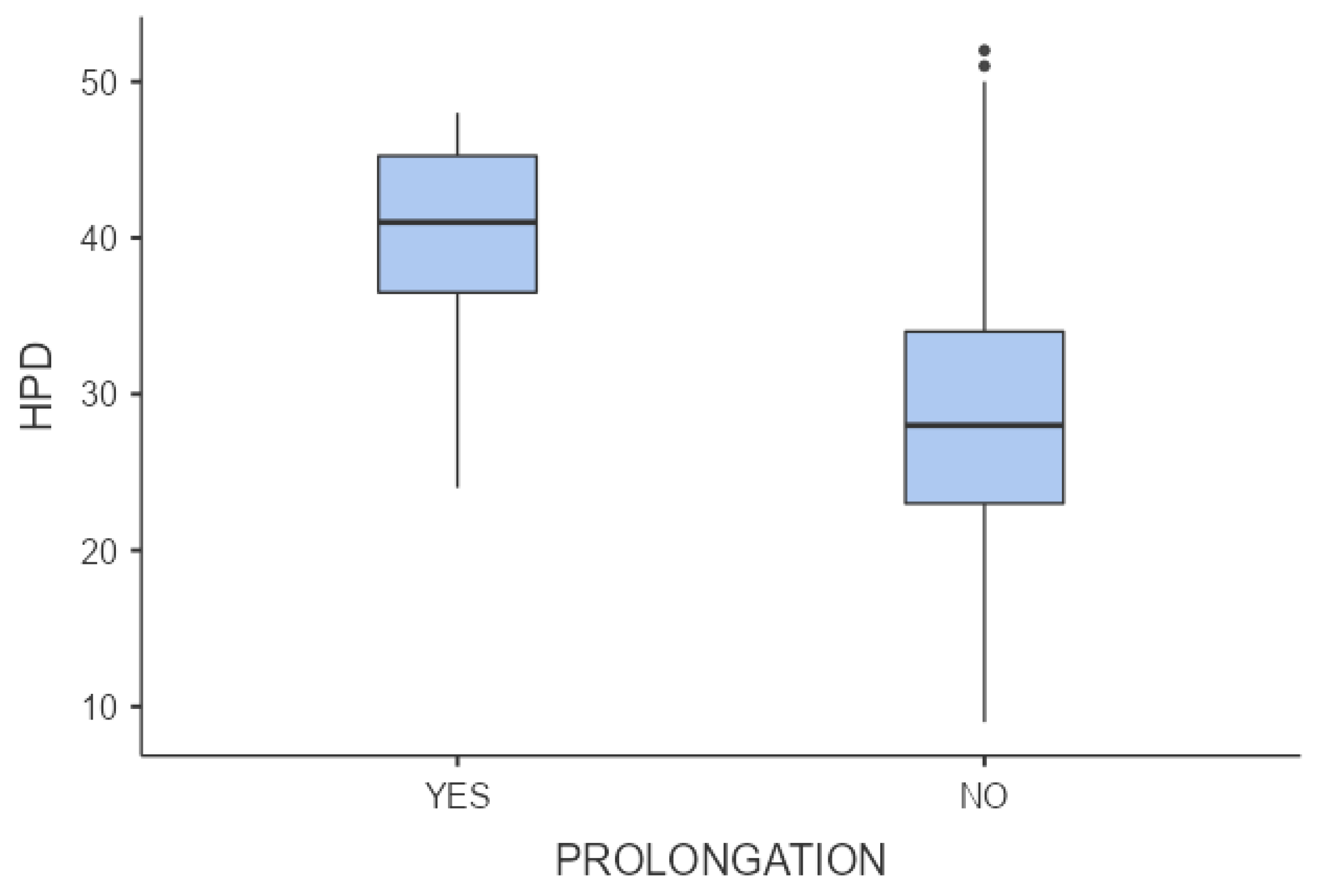
| Ultrasonographic Characteristics | Mode of Delivery | p-Value | ||
|---|---|---|---|---|
| Vaginal Delivery | Operative Vaginal Delivery | Cesarean Section | ||
| HPD (mm) | 28.6 (10.1) | 26.9 (6.84) | 41.4 (5.3) | <0.001 |
| AoP (°) | 145.7 (24.9) | 139.9 (23.8) | 132.1 (26.2) | 0.289 |
| Fetal–Maternal Characteristics | HPD | AoP | ||
|---|---|---|---|---|
| Pearson r Correlation Coefficient | p-Value | Pearson r Correlation Coefficient | p-Value | |
| Age (years) | 0.084 | 0.484 | 0.045 | 0.686 |
| Gestational age (weeks) | 0.128 | 0.288 | −0.187 | 0.093 |
| Parity | 0.226 | 0.060 | −0.221 | 0.047 |
| BMI (kg/m2) | 0.268 | 0.024 | 0.011 | 0.921 |
| Birth weight (grams) | −0.002 | 0.985 | 0.013 | 0.909 |
| Duration of the second stage of labor (min) | 0.256 | 0.031 | −0.186 | 0.095 |
| Total duration of labor (hours) | 0.098 | 0.418 | 0.012 | 0.918 |
| Mode of Delivery | Predictor | ORs | 95% CI | p-Value |
|---|---|---|---|---|
| Cesarean section vs. Vaginal delivery (Ref) | Age | 1.2 | 0.003–0.003 | 0.451 |
| Gestational age | 0.68 | 0.42–1.12 | 0.133 | |
| Low parity | 12.024 | 6.320–22.876 | <0.001 | |
| BMI | 0.903 | 0.700–1.164 | 0.432 | |
| Birth weight | 1 | 0.99–1 | 0.079 | |
| Duration of the second stage of labor | 1 | 0.99–1.03 | 0.208 | |
| Total duration of labor | 1.1 | 0.94–1.34 | 0.178 | |
| High AoP | 1 | 0.9–1.06 | 0.655 | |
| High HPD | 1.23 | 1.05–1.43 | 0.007 | |
| Operative vaginal delivery vs. Vaginal delivery (Ref) | Age | 1.06 | 0.942–1.202 | 0.312 |
| Gestational age | 1.29 | 0.96–1.73 | 0.086 | |
| Low parity | 1.99 | 0.55–7.166 | 0.292 | |
| BMI | 1.04 | 0.86–1.2 | 0.645 | |
| Birth weight | 1 | 0.99–1 | 0.292 | |
| Duration of the second stage of labor | 1 | 0.98–1.01 | 0.821 | |
| Total duration of labor | 1.24 | 1.05–1.46 | 0.009 | |
| High AoP | 0.98 | 0.94–1.02 | 0.421 | |
| High HPD | 0.91 | 0.78–1.06 | 0.244 |
| Mode of Delivery | Labor Characteristics | ORs | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Cesarean section | Oxytocin | 4.603 | 0.547–38.76 | 0.160 | |
| Yes | 10 (16.9%) | ||||
| No | 1 (4.3%) | ||||
| Epidural | 1.121 | 0.286–4.390 | 0.870 | ||
| Yes | 6 (14.6%) | ||||
| No | 5 (12.2%) | ||||
| Onset of labor | 1.051 | 0.248–4.124 | 0.943 | ||
| Spontaneous | 5 (14.3%) | ||||
| Induction | 6 (12.8%) | ||||
| Operative Vaginal Delivery | Oxytocin | 1.168 | 0.267–5.107 | 0.837 | |
| Yes | 8 (13.6%) | ||||
| No | 3 (13.0%) | ||||
| Epidural | 0.572 | 0.147–2.233 | 0.422 | ||
| Yes | 5 (12.2%) | ||||
| No | 6 (14.6%) | ||||
| Onset of labor | 0.219 | 0.041–1.159 | 0.074 | ||
| Spontaneous | 2 (5.7%) | ||||
| Induction | 9 (19.1%) | ||||
| Vaginal Delivery | Oxytocin | Reference | |||
| Yes | 41 (69.5%) | ||||
| No | 19 (82.6%) | ||||
| Epidural | |||||
| Yes | 30 (73.2%) | ||||
| No | 30 (73.2%) | ||||
| Onset of labor | |||||
| Spontaneous | 28 (80.0%) | ||||
| Induction | 32 (68.1%) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitta, K.; Tsakiridis, I.; Dagklis, T.; Kalogiannidis, I.; Mamopoulos, A.; Michos, G.; Virgiliou, A.; Athanasiadis, A. Ultrasonographic Evaluation of the Second Stage of Labor according to the Mode of Delivery: A Prospective Study in Greece. J. Clin. Med. 2024, 13, 1068. https://doi.org/10.3390/jcm13041068
Mitta K, Tsakiridis I, Dagklis T, Kalogiannidis I, Mamopoulos A, Michos G, Virgiliou A, Athanasiadis A. Ultrasonographic Evaluation of the Second Stage of Labor according to the Mode of Delivery: A Prospective Study in Greece. Journal of Clinical Medicine. 2024; 13(4):1068. https://doi.org/10.3390/jcm13041068
Chicago/Turabian StyleMitta, Kyriaki, Ioannis Tsakiridis, Themistoklis Dagklis, Ioannis Kalogiannidis, Apostolos Mamopoulos, Georgios Michos, Andriana Virgiliou, and Apostolos Athanasiadis. 2024. "Ultrasonographic Evaluation of the Second Stage of Labor according to the Mode of Delivery: A Prospective Study in Greece" Journal of Clinical Medicine 13, no. 4: 1068. https://doi.org/10.3390/jcm13041068
APA StyleMitta, K., Tsakiridis, I., Dagklis, T., Kalogiannidis, I., Mamopoulos, A., Michos, G., Virgiliou, A., & Athanasiadis, A. (2024). Ultrasonographic Evaluation of the Second Stage of Labor according to the Mode of Delivery: A Prospective Study in Greece. Journal of Clinical Medicine, 13(4), 1068. https://doi.org/10.3390/jcm13041068








