Assessing the Preservation of Lumbar Lordotic Curvature in Everyday Sitting Conditions Assessed with an Inertial Measurement System
Abstract
:1. Introduction
2. Methods
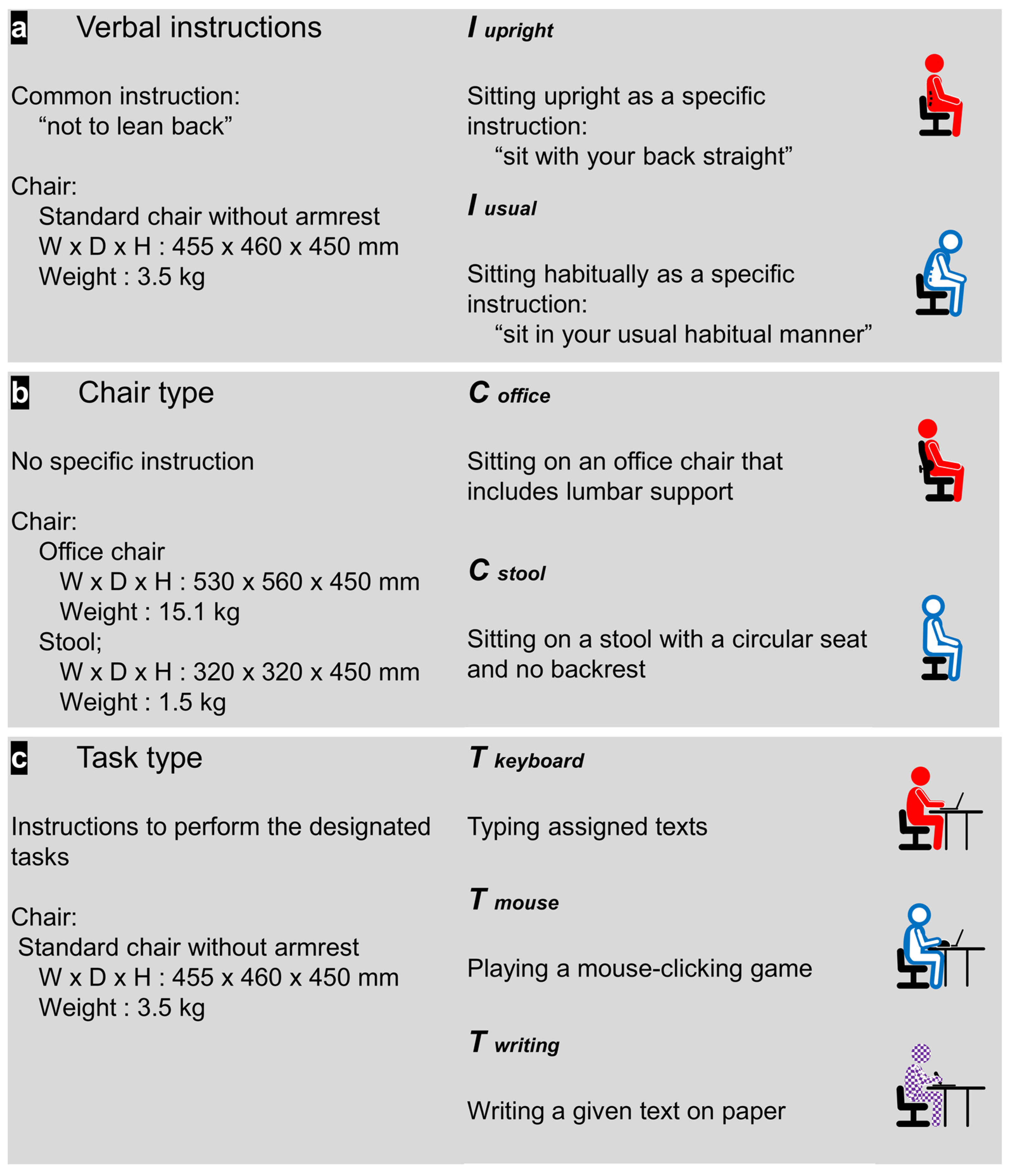
2.1. Design
2.2. Participants
2.3. Experimental Set-Up
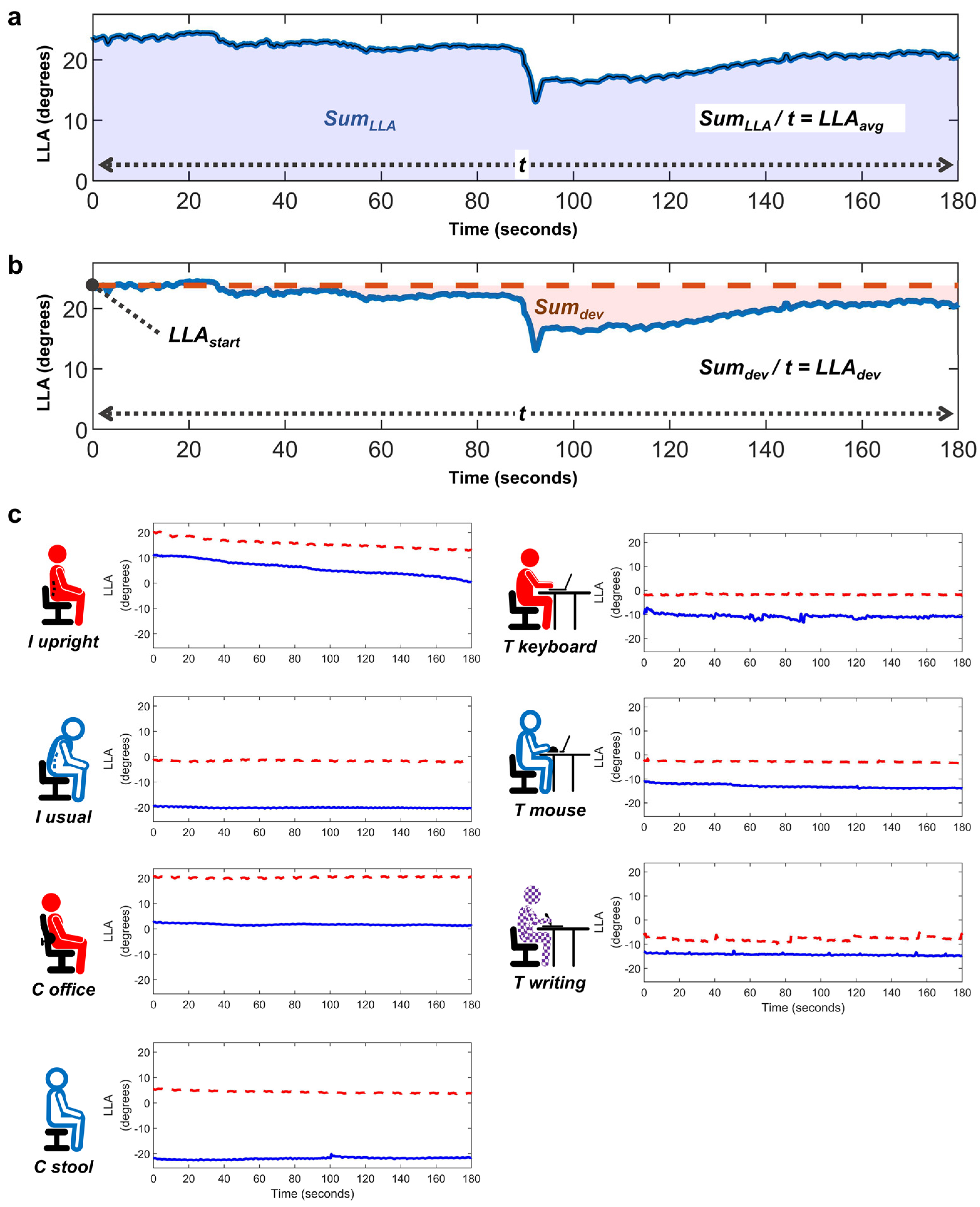
2.4. Data Processing
2.5. Test Protocol
2.6. Outcome Variables
2.7. Statistical Analysis
3. Results
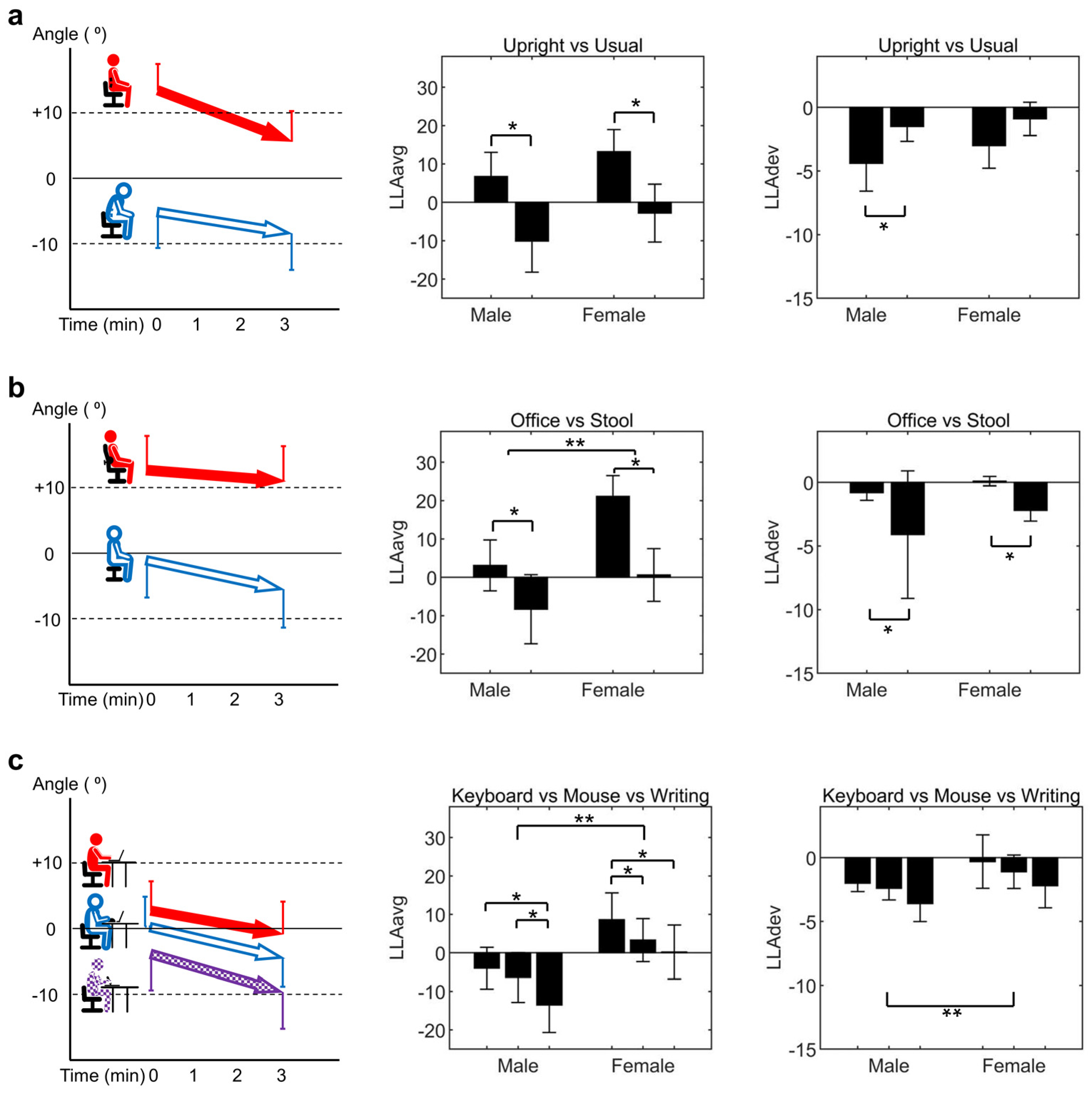
3.1. Comparison within Verbal Instruction Category
3.2. Comparison within Chair Type Category
3.3. Comparison within Task Type Category
3.4. Sex-Related Differences in LLA across Sitting Conditions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Williams, S.A.; Russo, G.A. Evolution of the hominoid vertebral column: The long and the short of it. Evol. Anthropol. 2015, 24, 15–32. [Google Scholar] [CrossRef] [PubMed]
- Farfan, H.F. The biomechanical advantage of lordosis and hip extension for upright activity. Man as compared with other anthropoids. Spine 1978, 3, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Aspden, R. The Spine as an Arch A New Mathematical Model. Spine 1989, 14, 266–274. [Google Scholar] [CrossRef]
- Edmondston, S.J.; Song, S.; Bricknell, R.V.; Davies, P.A.; Fersum, K.; Humphries, P.; Wickenden, D.; Singer, K.P. MRI evaluation of lumbar spine flexion and extension in asymptomatic individuals. Man. Ther. 2000, 5, 158–164. [Google Scholar] [CrossRef]
- Adams, M.A.; Hutton, W.C. The effect of posture on the role of the apophysial joints in resisting intervertebral compressive forces. J. Bone Jt. Surg. Br. Vol. 1980, 62, 358–362. [Google Scholar] [CrossRef] [PubMed]
- Adams, M.A.; Mannion, A.F.; Dolan, P. Personal risk factors for first-time low back pain. Spine 1999, 24, 2497–2505. [Google Scholar] [CrossRef]
- Chun, S.W.; Lim, C.Y.; Kim, K.; Hwang, J.; Chung, S.G. The relationships between low back pain and lumbar lordosis: A systematic review and meta-analysis. Spine J. Off. J. N. Am. Spine Soc. 2017, 17, 1180–1191. [Google Scholar] [CrossRef]
- Adams, M.A.; Dolan, P. Time-dependent changes in the lumbar spine’s resistance to bending. Clin. Biomech. 1996, 11, 194–200. [Google Scholar] [CrossRef]
- McGill, S.M.; Brown, S. Creep response of the lumbar spine to prolonged full flexion. Clin. Biomech. 1992, 7, 43–46. [Google Scholar] [CrossRef]
- Solomonow, M.; Zhou, B.H.; Baratta, R.V.; Burger, E. Biomechanics and electromyography of a cumulative lumbar disorder: Response to static flexion. Clin. Biomech. 2003, 18, 890–898. [Google Scholar] [CrossRef]
- Twomey, L.; Taylor, J. Flexion creep deformation and hysteresis in the lumbar vertebral column. Spine 1982, 7, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Andersson, B.J.; Ortengren, R.; Nachemson, A.; Elfstrom, G. Lumbar disc pressure and myoelectric back muscle activity during sitting. IV. Studies on a car driver’s seat. Scand. J. Rehabil. Med. 1974, 6, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Wade, K.R.; Robertson, P.A.; Thambyah, A.; Broom, N.D. How healthy discs herniate: A biomechanical and microstructural study investigating the combined effects of compression rate and flexion. Spine 2014, 39, 1018–1028. [Google Scholar] [CrossRef] [PubMed]
- Shah, J.S.; Hampson, W.G.; Jayson, M.I. The distribution of surface strain in the cadaveric lumbar spine. J. Bone Jt. Surg. Br. Vol. 1978, 60, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Andersson, G.B.; Schultz, A.B. Effects of fluid injection on mechanical properties of intervertebral discs. J. Biomech. 1979, 12, 453–458. [Google Scholar] [CrossRef]
- Sato, K.; Kikuchi, S.; Yonezawa, T. In vivo intradiscal pressure measurement in healthy individuals and in patients with ongoing back problems. Spine 1999, 24, 2468–2474. [Google Scholar] [CrossRef] [PubMed]
- Wilke, H.J.; Neef, P.; Caimi, M.; Hoogland, T.; Claes, L.E. New in vivo measurements of pressures in the intervertebral disc in daily life. Spine 1999, 24, 755–762. [Google Scholar] [CrossRef]
- Cholewicki, J.; Pathak, P.; Reeves, N.P.; Popovich, J.M. Simulation of multifactorial causes of low back pain. Spine J. 2016, 16, S277. [Google Scholar] [CrossRef]
- Omokhodion, F.O.; Sanya, A.O. Risk factors for low back pain among office workers in Ibadan, Southwest Nigeria. Occup. Med. 2003, 53, 287–289. [Google Scholar] [CrossRef]
- Toh, S.H.; Coenen, P.; Howie, E.K.; Straker, L.M. The associations of mobile touch screen device use with musculoskeletal symptoms and exposures: A systematic review. PLoS ONE 2017, 12, e0181220. [Google Scholar] [CrossRef]
- Lis, A.M.; Black, K.M.; Korn, H.; Nordin, M. Association between sitting and occupational LBP. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2007, 16, 283–298. [Google Scholar] [CrossRef]
- Black, K.M.; McClure, P.; Polansky, M. The influence of different sitting positions on cervical and lumbar posture. Spine 1996, 21, 65–70. [Google Scholar] [CrossRef]
- O’Sullivan, K.; O’Dea, P.; Dankaerts, W.; O’Sullivan, P.; Clifford, A.; O’Sullivan, L. Neutral lumbar spine sitting posture in pain-free subjects. Man. Ther. 2010, 15, 557–561. [Google Scholar] [CrossRef] [PubMed]
- Czaprowski, D.; Pawlowska, P.; Kolwicz-Ganko, A.; Sitarski, D.; Kedra, A. The Influence of the “Straighten Your Back” Command on the Sagittal Spinal Curvatures in Children with Generalized Joint Hypermobility. BioMed Res. Int. 2017, 2017, 9724021. [Google Scholar] [CrossRef]
- Paloschi, D.; Bravi, M.; Schena, E.; Miccinilli, S.; Morrone, M.; Sterzi, S.; Saccomandi, P.; Massaroni, C. Validation and Assessment of a Posture Measurement System with Magneto-Inertial Measurement Units. Sensors 2021, 21, 6610. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.; Parthasarathy, S.; Taylor, S.J.; Pucci, D.; Hendrix, R.W.; Makhsous, M. Effect of Different Sitting Postures on Lung Capacity, Expiratory Flow, and Lumbar Lordosis. Arch. Phys. Med. Rehabil. 2006, 87, 504–509. [Google Scholar] [CrossRef]
- Makhsous, M.; Lin, F.; Hendrix, R.W.; Hepler, M.; Zhang, L.Q. Sitting with adjustable ischial and back supports: Biomechanical changes. Spine 2003, 28, 1113–1121; discussion 1121–1122. [Google Scholar] [CrossRef]
- Wong, A.Y.L.; Chan, T.P.M.; Chau, A.W.M.; Tung Cheung, H.; Kwan, K.C.K.; Lam, A.K.H.; Wong, P.Y.C.; De Carvalho, D. Do different sitting postures affect spinal biomechanics of asymptomatic individuals? Gait Posture 2019, 67, 230–235. [Google Scholar] [CrossRef]
- Baumgartner, D.; Zemp, R.; List, R.; Stoop, M.; Naxera, J.; Elsig, J.P.; Lorenzetti, S. The spinal curvature of three different sitting positions analysed in an open MRI scanner. Sci. World J. 2012, 2012, 184016. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.S.; Jang, J.S.; Lee, S.H.; Kim, J.U. A comparison study on the change in lumbar lordosis when standing, sitting on a chair, and sitting on the floor in normal individuals. J. Korean Neurosurg. Soc. 2012, 51, 20–23. [Google Scholar] [CrossRef]
- Cho, I.Y.; Park, S.Y.; Park, J.H.; Kim, T.K.; Jung, T.W.; Lee, H.M. The Effect of Standing and Different Sitting Positions on Lumbar Lordosis: Radiographic Study of 30 Healthy Volunteers. Asian Spine J. 2015, 9, 762–769. [Google Scholar] [CrossRef] [PubMed]
- De Carvalho, D.; Grondin, D.; Callaghan, J. The impact of office chair features on lumbar lordosis, intervertebral joint and sacral tilt angles: A radiographic assessment. Ergonomics 2017, 60, 1393–1404. [Google Scholar] [CrossRef]
- Alamin, T.F.; Agarwal, V.; Zagel, A.; Qeli, A. The effect of standing vs. variants of the seated position on lumbar intersegmental angulation and spacing: A radiographic study of 20 asymptomatic subjects. J. Spine Surg. 2018, 4, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Van Dieën, J.; De Looze, M.; Hermans, V. Effects of dynamic office chairs on trunk kinematics, trunk extensor EMG and spinal shrinkage. Ergonomics 2001, 44, 739–750. [Google Scholar] [CrossRef]
- Dunk, N.M.; Callaghan, J.P. Gender-based differences in postural responses to seated exposures. Clin. Biomech. 2005, 20, 1101–1110. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.E.; Harrison, D.D.; Cailliet, R.; Janik, T.J.; Holland, B. Radiographic analysis of lumbar lordosis: Centroid, Cobb, TRALL, and Harrison posterior tangent methods. Spine 2001, 26, E235–E242. [Google Scholar] [CrossRef]
- Troyanovich, S.J.; Cailliet, R.; Janik, T.J.; Harrison, D.D.; Harrison, D.E. Radiographic mensuration characteristics of the sagittal lumbar spine from a normal population with a method to synthesize prior studies of lordosis. J. Spinal Disord. 1997, 10, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Lord, M.J.; Small, J.M.; Dinsay, J.M.; Watkins, R.G. Lumbar lordosis. Effects of sitting and standing. Spine 1997, 22, 2571–2574. [Google Scholar] [CrossRef]
- De Carvalho, D.E.; Soave, D.; Ross, K.; Callaghan, J.P. Lumbar spine and pelvic posture between standing and sitting: A radiologic investigation including reliability and repeatability of the lumbar lordosis measure. J. Manip. Physiol. Ther. 2010, 33, 48–55. [Google Scholar] [CrossRef]
- Wong, W.Y.; Wong, M.S. Detecting spinal posture change in sitting positions with tri-axial accelerometers. Gait Posture 2008, 27, 168–171. [Google Scholar] [CrossRef]
- Chhikara, A.; McGregor, A.H.; Hadjilucas, L.; Bello, F.; Rice, A.S. Quantitative Assessment of the Motion of the Lumbar Spine and Pelvis with Wearable Inertial Sensors. In Proceedings of the 2010 International Conference on Body Sensor Networks, Singapore, 7–9 June 2010; pp. 9–15. [Google Scholar]
- Stenlund, T.C.; Öhberg, F.; Lundström, R.; Lindroos, O.; Häger, C.; Rehn, B. Inter- and intra-tester reliability when measuring seated spinal postures with inertial sensors. Int. J. Ind. Ergon. 2014, 44, 732–738. [Google Scholar] [CrossRef]
- Yoon, C.; Lee, J.; Kim, K.; Kim, H.C.; Chung, S.G. Quantification of Lumbar Stability During Wall Plank-and-Roll Activity Using Inertial Sensors. PM R J. Inj. Funct. Rehabil. 2015, 7, 803–813. [Google Scholar] [CrossRef] [PubMed]
- Dunk, N.M.; Callaghan, J.P. Lumbar spine movement patterns during prolonged sitting differentiate low back pain developers from matched asymptomatic controls. Work 2010, 35, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.; Desmoulin, G.T.; Khan, A.H.; Park, E.J. Comparison of 3D spinal motions during stair-climbing between individuals with and without low back pain. Gait Posture 2011, 34, 222–226. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Yoon, C.; Kim, K.; Cho, M.; Kim, H.C.; Chung, S.G. Lumbar Stability in Healthy Individuals and Low Back Pain Patients Quantified by Wall Plank-and-Roll Test. PM R J. Inj. Funct. Rehabil. 2018, 11, 483–494. [Google Scholar] [CrossRef] [PubMed]
- Paulich, M.; Schepers, M.; Rudigkeit, N.; Bellusci, G. Xsens MTw Awinda: Miniature wireless inertial-magnetic motion tracker for highly accurate 3D kinematic applications. Xsens Enschede Neth. 2018, 1, 1–9. [Google Scholar]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Chakraverty, R.; Pynsent, P.; Isaacs, K. Which spinal levels are identified by palpation of the iliac crests and the posterior superior iliac spines? J. Anat. 2007, 210, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Milani, G.B.; Natal Filho, A.; Amado Joao, S.M. Correlation between lumbar lordosis angle and degree of gynoid lipodystrophy (cellulite) in asymptomatic women. Clinics 2008, 63, 503–508. [Google Scholar] [CrossRef]
- Dankaerts, W.; O’Sullivan, P.; Burnett, A.; Straker, L. Differences in sitting postures are associated with nonspecific chronic low back pain disorders when patients are subclassified. Spine 2006, 31, 698–704. [Google Scholar] [CrossRef]
- O’Sullivan, K.; O’Sullivan, L.; O’Sullivan, P.; Dankaerts, W. Investigating the effect of real-time spinal postural biofeedback on seated discomfort in people with non-specific chronic low back pain. Ergonomics 2013, 56, 1315–1325. [Google Scholar] [CrossRef] [PubMed]
- Van Almkerk, M.; Bierling, B.L.; Leermakers, N.; Vinken, J.; Timmermans, A.A. Improving posture and sitting behavior through tactile and visual feedback in a sedentary environment. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 4570–4573. [Google Scholar]
- Rezaee, M.; Ghasemi, M.; Jafari, N.J.; Izadi, M. Low back pain and related factors among Iranian office workers. Int. J. Occup. Hyg. 2011, 3, 23–28. [Google Scholar]
- Arshad, R.; Pan, F.; Reitmaier, S.; Schmidt, H. Effect of age and sex on lumbar lordosis and the range of motion. A systematic review and meta-analysis. J. Biomech. 2019, 82, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Vialle, R.; Levassor, N.; Rillardon, L.; Templier, A.; Skalli, W.; Guigui, P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J. Bone Jt. Surg. Am. 2005, 87, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Xu, L.; Zhu, F.; Jiang, L.; Wang, Z.; Liu, Z.; Qian, B.P.; Qiu, Y. Sagittal alignment of spine and pelvis in asymptomatic adults: Norms in Chinese populations. Spine 2014, 39, E1–E6. [Google Scholar] [CrossRef] [PubMed]
- Damasceno, L.H.F.; Catarin, S.R.G.; Campos, A.D.; Defino, H.L.A. Lumbar lordosis: A study of angle values and of vertebral bodies and intervertebral discs role. Acta Ortopédica Bras. 2006, 14, 193–198. [Google Scholar] [CrossRef]
- Endo, K.; Suzuki, H.; Nishimura, H.; Tanaka, H.; Shishido, T.; Yamamoto, K. Sagittal lumbar and pelvic alignment in the standing and sitting positions. J. Orthop. Sci. 2012, 17, 682–686. [Google Scholar] [CrossRef]
- MacDonald, D.A.; Moseley, G.L.; Hodges, P.W. The lumbar multifidus: Does the evidence support clinical beliefs? Man. Ther. 2006, 11, 254–263. [Google Scholar] [CrossRef]
- Ranger, T.A.; Cicuttini, F.M.; Jensen, T.S.; Peiris, W.L.; Hussain, S.M.; Fairley, J.; Urquhart, D.M. Are the size and composition of the paraspinal muscles associated with low back pain? A systematic review. Spine J. 2017, 17, 1729–1748. [Google Scholar] [CrossRef]
- O’Sullivan, P.B.; Dankaerts, W.; Burnett, A.F.; Farrell, G.T.; Jefford, E.; Naylor, C.S.; O’Sullivan, K.J. Effect of different upright sitting postures on spinal-pelvic curvature and trunk muscle activation in a pain-free population. Spine 2006, 31, E707–E712. [Google Scholar] [CrossRef]
- O’Sullivan, P.B.; Grahamslaw, K.M.; Kendell, M.; Lapenskie, S.C.; Möller, N.E.; Richards, K.V. The effect of different standing and sitting postures on trunk muscle activity in a pain-free population. Spine 2002, 27, 1238–1244. [Google Scholar] [CrossRef] [PubMed]
- Makhsous, M.; Lin, F.; Bankard, J.; Hendrix, R.W.; Hepler, M.; Press, J. Biomechanical effects of sitting with adjustable ischial and lumbar support on occupational low back pain: Evaluation of sitting load and back muscle activity. BMC Musculoskelet. Disord. 2009, 10, 17. [Google Scholar] [CrossRef] [PubMed]
- Andersson, B.G.; Örtengren, R.; Nachemson, A.L.; Elfström, G.; Broman, H. The sitting posture: An electromyographic and discometric study. Orthop. Clin. N. Am. 1975, 6, 105–120. [Google Scholar] [CrossRef]
- Gregory, D.E.; Dunk, N.M.; Callaghan, J.P. Stability ball versus office chair: Comparison of muscle activation and lumbar spine posture during prolonged sitting. Hum. Factors 2006, 48, 142–153. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.M.; Hawley, J.A.; McKenzie, R.A.; van Wijmen, P.M. A comparison of the effects of two sitting postures on back and referred pain. Spine 1991, 16, 1185–1191. [Google Scholar] [CrossRef] [PubMed]
- Aota, Y.; Iizuka, H.; Ishige, Y.; Mochida, T.; Yoshihisa, T.; Uesugi, M.; Saito, T. Effectiveness of a lumbar support continuous passive motion device in the prevention of low back pain during prolonged sitting. Spine 2007, 32, E674–E677. [Google Scholar] [CrossRef]
- Pillastrini, P.; Mugnai, R.; Bertozzi, L.; Costi, S.; Curti, S.; Guccione, A.; Mattioli, S.; Violante, F.S. Effectiveness of an ergonomic intervention on work-related posture and low back pain in video display terminal operators: A 3 year cross-over trial. Appl. Erg. 2010, 41, 436–443. [Google Scholar] [CrossRef]

| All (n = 29) | Male (n = 15) | Female (n = 14) | |
|---|---|---|---|
| Age, years | 35.5 ± 13.6 | 32.2 ± 12.6 | 39.1 ± 14.1 |
| Body mass, kg | 64.0 ± 12.3 | 72.0 ± 11.9 | 55.4 ± 4.9 |
| Height, cm | 167.1 ± 8.9 | 173.8 ± 6.0 | 159.8 ± 4.6 |
| BMI, kg/m2 | 22.8 ± 3.1 | 23.8 ± 3.3 | 21.8 ± 2.5 |
| Sitting Category | Sitting Posture | LLAavg (°) | LLAdev (°) | ||||
|---|---|---|---|---|---|---|---|
| All | Male | Female | All | Male | Female | ||
| Verbal instruction | Iupright | 9.9 ± 12.0 | 6.7 ± 12.5 | 13.2 ± 11.0 | −3.7 ± 3.9 | −4.4 ± 4.3 | −3.0 ± 3.4 |
| Iusual | −6.6 ± 15.4 | −10.1 ± 16.0 | −2.8 ± 14.4 | −1.2 ± 2.4 | −1.5 ± 2.3 | −0.9 ± 2.5 | |
| Chair type | Coffice | 11.8 ± 14.8 | 3.1 ± 13.1 | 21.1 ± 10.3 | −0.4 ± 1.1 | −0.8 ± 1.2 | 0.1 ± 0.7 |
| Cstool | −4.0 ± 16.0 | −8.3 ± 17.8 | 0.6 ± 13.1 | −3.2 ± 7.1 | −4.1 ± 9.9 | −2.2 ± 1.6 | |
| Deks tasks | Tkeyboard | 2.0 ± 13.4 | −4.0 ± 10.7 | 8.6 ± 13.3 | −1.2 ± 3.0 | −2.0 ± 1.3 | −0.3 ± 4.0 |
| Tmouse | −1.7 ± 12.6 | −6.4 ± 12.8 | 3.3 ± 10.7 | −1.8 ± 2.2 | −2.4 ± 1.8 | −1.1 ± 2.5 | |
| Twriting | −6.9 ± 15.3 | −13.5 ± 14.2 | 0.2 ± 13.4 | −2.9 ± 3.1 | −3.6 ± 2.8 | −2.2 ± 3.3 | |
| Sitting Category | LLAavg (°) | LLAdev (°) | ||||
|---|---|---|---|---|---|---|
| Item | F | p-Value | Item | Wald χ2 | p-Value | |
| Verbal instruction | Instruction | 72.159 | <0.001 * | Instruction | 11.123 | 0.001 * |
| Sex | 2.177 | 0.152 | Sex | 1.328 | 0.249 | |
| Instruction × Sex | 0.045 | 0.834 | Instruction × Sex | 0.221 | 0.638 | |
| Chair type | Chair | 38.166 | <0.001 * | Chair | 4.543 | 0.033 * |
| Sex | 9.025 | 0.006 * | Sex | 1.363 | 0.243 | |
| Chair × Sex | 3.080 | 0.091 | Chair × Sex | 0.155 | 0.694 | |
| Deks tasks | Task | 17.574 | <0.001 * | Task | 5.402 | 0.067 |
| Sex | 7.646 | 0.010 * | Sex | 4.611 | 0.032 * | |
| Task × Sex | 0.959 | 0.390 | Task × Sex | 0.133 | 0.936 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.C.; Kim, J.-G.; Kim, B.S.; Kim, C.K.; Choi, M.; Lee, J.; Chung, S.G. Assessing the Preservation of Lumbar Lordotic Curvature in Everyday Sitting Conditions Assessed with an Inertial Measurement System. J. Clin. Med. 2024, 13, 2728. https://doi.org/10.3390/jcm13092728
Kim JC, Kim J-G, Kim BS, Kim CK, Choi M, Lee J, Chung SG. Assessing the Preservation of Lumbar Lordotic Curvature in Everyday Sitting Conditions Assessed with an Inertial Measurement System. Journal of Clinical Medicine. 2024; 13(9):2728. https://doi.org/10.3390/jcm13092728
Chicago/Turabian StyleKim, Ju Chan, Jeong-Gil Kim, Beom Suk Kim, Cheol Ki Kim, Minseok Choi, Joonnyong Lee, and Sun Gun Chung. 2024. "Assessing the Preservation of Lumbar Lordotic Curvature in Everyday Sitting Conditions Assessed with an Inertial Measurement System" Journal of Clinical Medicine 13, no. 9: 2728. https://doi.org/10.3390/jcm13092728
APA StyleKim, J. C., Kim, J.-G., Kim, B. S., Kim, C. K., Choi, M., Lee, J., & Chung, S. G. (2024). Assessing the Preservation of Lumbar Lordotic Curvature in Everyday Sitting Conditions Assessed with an Inertial Measurement System. Journal of Clinical Medicine, 13(9), 2728. https://doi.org/10.3390/jcm13092728






