Precision Diagnostics by Affinity-Mass Spectrometry: A Novel Approach for Fetal Growth Restriction Screening during Pregnancy
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient and Control Individual Cohorts
2.2. Blood Collection, Generation, and Storage of Peripheral Blood Serum
2.3. Protein Extract Preparation from Peripheral Blood Serum
2.4. MALDI-ToF MS Profiling of Serum Proteins and Internal Calibration of Mass Spectra
2.5. Raw Data Processing and Formation of Quotients from Ion Signal Areas
2.6. Youden Index Analyses for Determining Cut-Off Values
2.7. Cumulative Score Assignment
2.8. Bioinformatic and Biostatistical Analysis
2.9. Power Analysis
3. Results
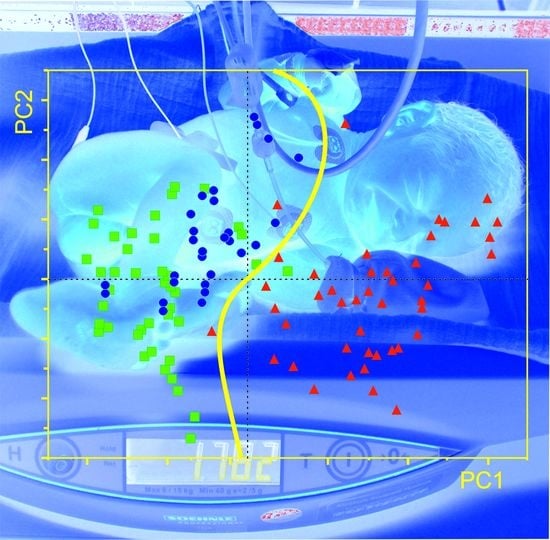
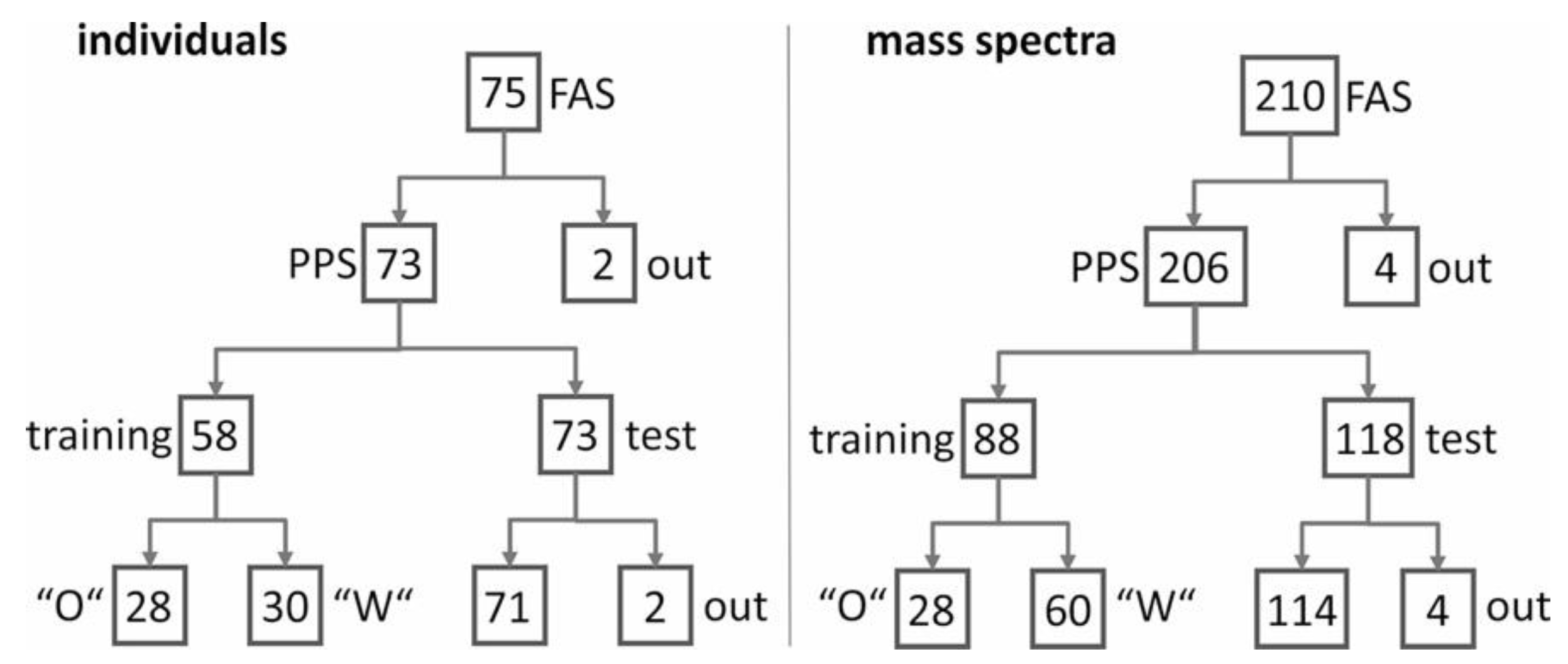
3.1. Patient Cohorts and MALDI Mass Spectrometric Profiling
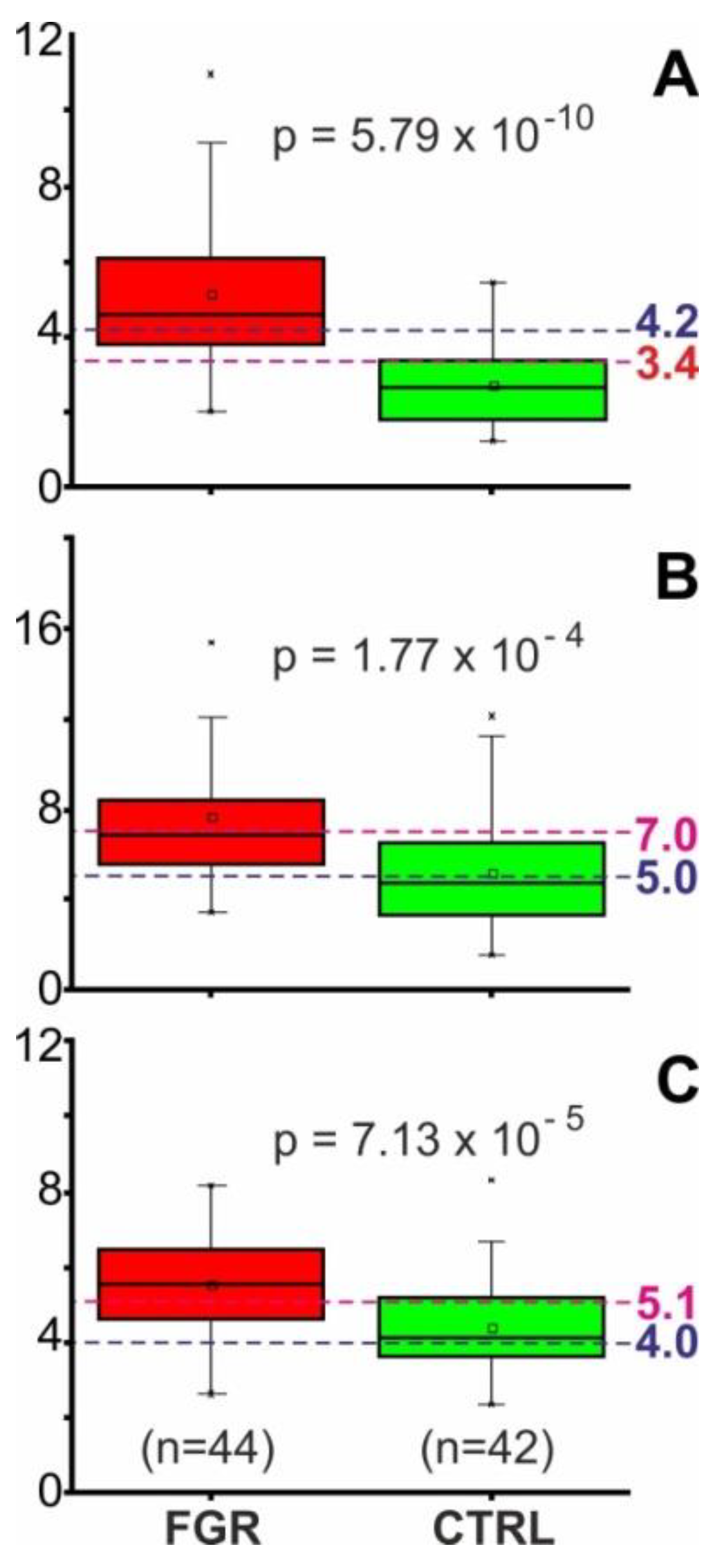
3.2. Determination of “Best Cut-Off” Values for Quotients A, B, and C to Separate FGR from CTRL
3.3. Combination of “Best Cut-Off” Values and Weighting of Cumulative Scores for Separating FGR from CTRL
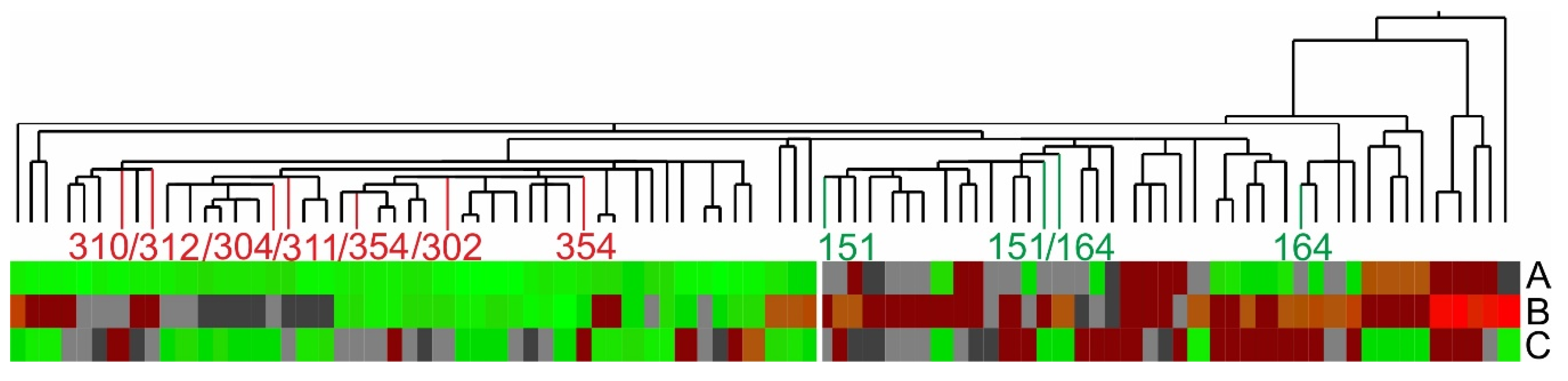
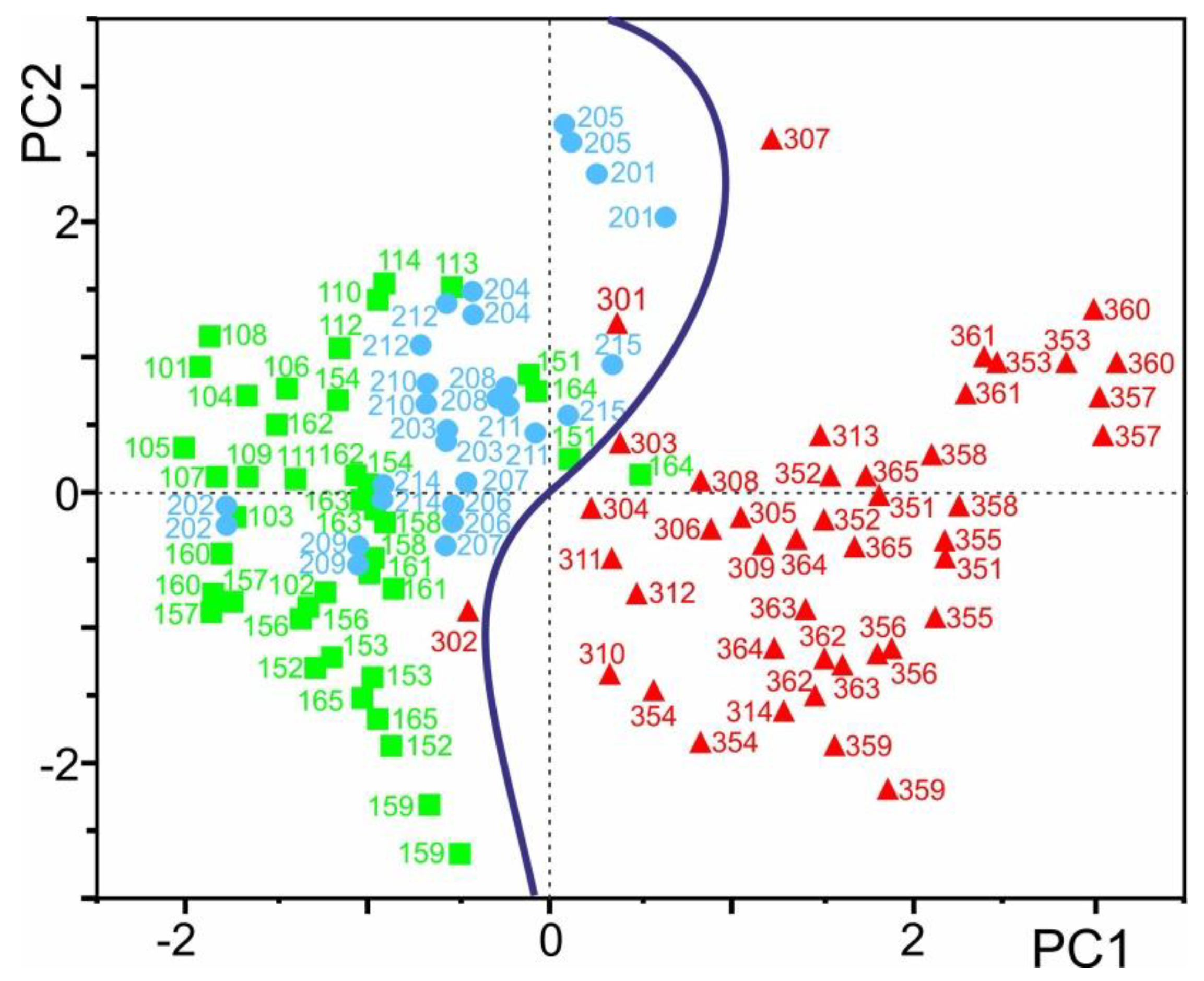
3.4. Application of “Weighted Cumulative Scores” for Separating FGR from CTRL and from SGA
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ACOG | American College of Obstetricians and Gynecologists |
| MALDI ToF MS | Matrix-Assisted Laser Desorption/Ionization Time of Flight Mass Spectrometry |
| m/z | mass to charge ratio |
References
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 204: Fetal Growth Restriction. Obstet. Gynecol. 2019, 133, e97–e109. [Google Scholar] [CrossRef]
- Figueras, F.; Gratacos, E. Update on the diagnosis and classification of fetal growth restriction and proposal of a stage-based management protocol. Fetal Diagn. Ther. 2014, 36, 86–98. [Google Scholar] [CrossRef] [PubMed]
- Kehl, S.; Dotsch, J.; Hecher, K.; Schlembach, D.; Schmitz, D.; Stepan, H.; Gembruch, U. Intrauterine Growth Restriction. Guideline of the German Society of Gynecology and Obstetrics (S2k-Level, AWMF Registry No. 015/080, October 2016). Geburtshilfe Und Frauenheilkd. 2017, 77, 1157–1173. [Google Scholar] [CrossRef] [PubMed]
- Mazarico, E.; Martinez-Cumplido, R.; Diaz, M.; Sebastiani, G.; Ibanez, L.; Gomez-Roig, M.D. Postnatal Anthropometric and Body Composition Profiles in Infants with Intrauterine Growth Restriction Identified by Prenatal Doppler. PLoS ONE 2016, 11, e0150152. [Google Scholar] [CrossRef]
- Figueras, F.; Gardosi, J. Intrauterine growth restriction: New concepts in antenatal surveillance, diagnosis, and management. Am. J. Obstet. Gynecol. 2011, 204, 288–300. [Google Scholar] [CrossRef]
- Gardosi, J. Customized charts and their role in identifying pregnancies at risk because of fetal growth restriction. J. Obstet. Gynaecol. Can. 2014, 36, 408–415. [Google Scholar] [CrossRef]
- Wölter, M.; Röwer, C.; Koy, C.; Rath, W.; Pecks, U.; Glocker, M.O. Proteoform profiling of peripheral blood serum proteins from pregnant women provides a molecular IUGR signature. J. Proteom. 2016, 149, 44–52. [Google Scholar] [CrossRef]
- Jayawardena, L.; Sheehan, P. Introduction of a customised growth chart protocol increased detection of small for gestational age pregnancies in a tertiary Melbourne hospital. Aust. N. Z. J. Obstet. Gynaecol. 2019, 59, 493–500. [Google Scholar] [CrossRef]
- Ernst, S.A.; Brand, T.; Reeske, A.; Spallek, J.; Petersen, K.; Zeeb, H. Care-Related and Maternal Risk Factors Associated with the Antenatal Nondetection of Intrauterine Growth Restriction: A Case-Control Study from Bremen, Germany. Biomed Res. Int. 2017, 2017, 1746146. [Google Scholar] [CrossRef]
- Visan, V.; Scripcariu, I.S.; Socolov, D.; Costescu, A.; Rusu, D.; Socolov, R.; Avasiloaiei, A.; Boiculese, L.; Dimitriu, C. Better prediction for FGR (fetal growth restriction) with the sFlt-1/PIGF ratio: A case-control study. Medicine 2019, 98, e16069. [Google Scholar] [CrossRef]
- Wölter, M.; Russ, M.; Okai, C.A.; Rath, W.; Pecks, U.; Glocker, M.O. Comparison of blood serum protein analysis by MALDI-MS from either conventional frozen samples or storage disc-deposited samples: A study with human serum from pregnant donors and from patients with intrauterine growth restriction. Eur. J. Mass Spectrom. 2019, 25, 381–390. [Google Scholar] [CrossRef] [PubMed]
- Pecks, U.; Kirschner, I.; Wölter, M.; Schlembach, D.; Koy, C.; Rath, W.; Glocker, M.O. Mass spectrometric profiling of cord blood serum proteomes to distinguish infants with intrauterine growth restriction from those who are small for gestational age and from control individuals. Transl. Res. J. Lab. Clin. Med. 2014, 164, 57–69. [Google Scholar] [CrossRef] [PubMed]
- Wölter, M.; Röwer, C.; Koy, C.; Reimer, T.; Rath, W.; Pecks, U.; Glocker, M.O. A proteome signature for intrauterine growth restriction derived from multifactorial analysis of mass spectrometry-based cord blood serum profiling. Electrophoresis 2012, 33, 1881–1893. [Google Scholar] [CrossRef] [PubMed]
- Pecks, U.; Seidenspinner, F.; Röwer, C.; Reimer, T.; Rath, W.; Glocker, M.O. Multifactorial analysis of affinity-mass spectrometry data from serum protein samples: A strategy to distinguish patients with preeclampsia from matching control individuals. J. Am. Soc. Mass Spectrom. 2010, 21, 1699–1711. [Google Scholar] [CrossRef] [PubMed]
- Hadlock, F.P.; Harrist, R.B.; Sharman, R.S.; Deter, R.L.; Park, S.K. Estimation of fetal weight with the use of head, body, and femur measurements—A prospective study. Am. J. Obstet. Gynecol. 1985, 151, 333–337. [Google Scholar] [CrossRef]
- Pecks, U.; Brieger, M.; Schiessl, B.; Bauerschlag, D.O.; Piroth, D.; Bruno, B.; Fitzner, C.; Orlikowsky, T.; Maass, N.; Rath, W. Maternal and fetal cord blood lipids in intrauterine growth restriction. J. Perinat. Med. 2012, 40, 287–296. [Google Scholar] [CrossRef]
- Wölter, M.; Okai, C.A.; Smith, D.S.; Russ, M.; Rath, W.; Pecks, U.; Borchers, C.H.; Glocker, M.O. Maternal Apolipoprotein B100 Serum Levels are Diminished in Pregnancies with Intrauterine Growth Restriction and Differentiate from Controls. Proteom. Clin. Appl. 2018, 12, e1800017. [Google Scholar] [CrossRef]
- Glocker, M.O.; Röwer, C.; Wölter, M.; Koy, C.; Reimer, T.; Pecks, U. Multiparametric Analysis of Mass Spectrometry-Based Proteome Profiling in Gestation-Related Diseases. In Handbook of Spectroscopy, 2nd ed.; Gauglitz, G., Moore, D.S., Eds.; Wiley-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2014; pp. 407–428. [Google Scholar] [CrossRef]
- Kiernan, U.A.; Tubbs, K.A.; Nedelkov, D.; Niederkofler, E.E.; Nelson, R.W. Detection of novel truncated forms of human serum amyloid A protein in human plasma. FEBS Lett. 2003, 537, 166–170. [Google Scholar] [CrossRef]
- Koy, C.; Heitner, J.C.; Woisch, R.; Kreutzer, M.; Serrano-Fernandez, P.; Gohlke, R.; Reimer, T.; Glocker, M.O. Cryodetector mass spectrometry profiling of plasma samples for HELLP diagnosis: An exploratory study. Proteomics 2005, 5, 3079–3087. [Google Scholar] [CrossRef]
- Nelsestuen, G.L.; Zhang, Y.; Martinez, M.B.; Key, N.S.; Jilma, B.; Verneris, M.; Sinaiko, A.; Kasthuri, R.S. Plasma protein profiling: Unique and stable features of individuals. Proteomics 2005, 5, 4012–4024. [Google Scholar] [CrossRef]
- Yang, J.; Finke, J.C.; Yang, J.; Percy, A.J.; von Fritschen, U.; Borchers, C.H.; Glocker, M.O. Early risk prognosis of free-flap transplant failure by quantitation of the macrophage colony-stimulating factor in patient plasma using 2-dimensional liquid-chromatography multiple reaction monitoring-mass spectrometry. Medicine 2016, 95, e4808. [Google Scholar] [CrossRef] [PubMed]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef]
- Davis, P.J. Interpolation and Approximation; Courier Corporation: Chelmsford, MA, USA, 1975. [Google Scholar]
- Metz, C.E. Basic principles of ROC analysis. Semin. Nucl. Med. 1978, 8, 283–298. [Google Scholar] [CrossRef]
- Benjamini, Y. Opening the box of a boxplot. Am. Stat. 1988, 42, 257–262. [Google Scholar]
- Faraggi, D.; Reiser, B. Estimation of the area under the ROC curve. Stat. Med. 2002, 21, 3093–3106. [Google Scholar] [CrossRef]
- Greiner, M.; Pfeiffer, D.; Smith, R.D. Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Prev. Vet. Med. 2000, 45, 23–41. [Google Scholar] [CrossRef]
- Röwer, C.; Koy, C.; Hecker, M.; Reimer, T.; Gerber, B.; Thiesen, H.J.; Glocker, M.O. Mass spectrometric characterization of protein structure details refines the proteome signature for invasive ductal breast carcinoma. J. Am. Soc. Mass Spectrom. 2011, 22, 440–456. [Google Scholar] [CrossRef]
- Röwer, C.; Vissers, J.P.; Koy, C.; Kipping, M.; Hecker, M.; Reimer, T.; Gerber, B.; Thiesen, H.J.; Glocker, M.O. Towards a proteome signature for invasive ductal breast carcinoma derived from label-free nanoscale LC-MS protein expression profiling of tumorous and glandular tissue. Anal. Bioanal. Chem. 2009, 395, 2443–2456. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Hegi, M.E.; Genbrugge, E.; Gorlia, T.; Stupp, R.; Gilbert, M.R.; Chinot, O.L.; Nabors, L.B.; Jones, G.; Van Criekinge, W.; Straub, J.; et al. MGMT Promoter Methylation Cutoff with Safety Margin for Selecting Glioblastoma Patients into Trials Omitting Temozolomide: A Pooled Analysis of Four Clinical Trials. Clin. Cancer Res. 2019, 25, 1809–1816. [Google Scholar] [CrossRef]
- Ho, S.; Lukacs, Z.; Hoffmann, G.F.; Lindner, M.; Wetter, T. Feature construction can improve diagnostic criteria for high-dimensional metabolic data in newborn screening for medium-chain acyl-CoA dehydrogenase deficiency. Clin. Chem. 2007, 53, 1330–1337. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rana, S.; Powe, C.E.; Salahuddin, S.; Verlohren, S.; Perschel, F.H.; Levine, R.J.; Lim, K.H.; Wenger, J.B.; Thadhani, R.; Karumanchi, S.A. Angiogenic factors and the risk of adverse outcomes in women with suspected preeclampsia. Circulation 2012, 125, 911–919. [Google Scholar] [CrossRef] [PubMed]
- Zeisler, H.; Llurba, E.; Chantraine, F.; Vatish, M.; Staff, A.C.; Sennstrom, M.; Olovsson, M.; Brennecke, S.P.; Stepan, H.; Allegranza, D.; et al. Predictive Value of the sFlt-1:PlGF Ratio in Women with Suspected Preeclampsia. N. Engl. J. Med. 2016, 374, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Sharp, A.; Chappell, L.C.; Dekker, G.; Pelletier, S.; Garnier, Y.; Zeren, O.; Hillerer, K.M.; Fischer, T.; Seed, P.T.; Turner, M.; et al. Placental Growth Factor informed management of suspected pre-eclampsia or fetal growth restriction: The MAPPLE cohort study. Pregnancy Hypertens. 2018, 14, 228–233. [Google Scholar] [CrossRef]
- Grimes, D.A.; Schulz, K.F. Compared to what? Finding controls for case-control studies. Lancet 2005, 365, 1429–1433. [Google Scholar] [CrossRef]
- Miettinen, O.S. The “case-control” study: Valid selection of subjects. J. Chronic Dis. 1985, 38, 543–548. [Google Scholar] [CrossRef]
- Abbassi-Ghanavati, M.; Greer, L.G.; Cunningham, F.G. Pregnancy and laboratory studies: A reference table for clinicians. Obstet. Gynecol. 2009, 114, 1326–1331. [Google Scholar] [CrossRef]
- Flood-Nichols, S.K.; Tinnemore, D.; Wingerd, M.A.; Abu-Alya, A.I.; Napolitano, P.G.; Stallings, J.D.; Ippolito, D.L. Longitudinal analysis of maternal plasma apolipoproteins in pregnancy: A targeted proteomics approach. Mol. Cell. Proteom. MCP 2013, 12, 55–64. [Google Scholar] [CrossRef]
- Winkler, K.; Wetzka, B.; Hoffmann, M.M.; Friedrich, I.; Kinner, M.; Baumstark, M.W.; Wieland, H.; Marz, W.; Zahradnik, H.P. Low density lipoprotein (LDL) subfractions during pregnancy: Accumulation of buoyant LDL with advancing gestation. J. Clin. Endocrinol. Metab. 2000, 85, 4543–4550. [Google Scholar] [CrossRef]
- Verlohren, S.; Herraiz, I.; Lapaire, O.; Schlembach, D.; Zeisler, H.; Calda, P.; Sabria, J.; Markfeld-Erol, F.; Galindo, A.; Schoofs, K.; et al. New gestational phase-specific cutoff values for the use of the soluble fms-like tyrosine kinase-1/placental growth factor ratio as a diagnostic test for preeclampsia. Hypertension 2014, 63, 346–352. [Google Scholar] [CrossRef]
- Reimer, T.; Rohrmann, H.; Stubert, J.; Pecks, U.; Glocker, M.O.; Richter, D.U.; Gerber, B. Angiogenic factors and acute-phase proteins in serum samples of preeclampsia and HELLP patients: A matched-pair analysis. J. Matern.-Fetal Neonatal Med. 2013, 26, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Mongelli, M.; Ek, S.; Tambyrajia, R. Screening for fetal growth restriction: A mathematical model of the effect of time interval and ultrasound error. Obstet. Gynecol. 1998, 92, 908–912. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.A.; Chernausek, S.D.; Hokken-Koelega, A.C.; Czernichow, P. International Small for Gestational Age Advisory Board consensus development conference statement: Management of short children born small for gestational age, April 24–October 1, 2001. Pediatrics 2003, 111, 1253–1261. [Google Scholar] [CrossRef]
- Morse, K.; Williams, A.; Gardosi, J. Fetal growth screening by fundal height measurement. Best Pract. Res. Clin. Obstet. Gynaecol. 2009, 23, 809–818. [Google Scholar] [CrossRef] [PubMed]
- Chappell, L.C.; Duckworth, S.; Seed, P.T.; Griffin, M.; Myers, J.; Mackillop, L.; Simpson, N.; Waugh, J.; Anumba, D.; Kenny, L.C.; et al. Diagnostic accuracy of placental growth factor in women with suspected preeclampsia: A prospective multicenter study. Circulation 2013, 128, 2121–2131. [Google Scholar] [CrossRef] [PubMed]
- Benton, S.J.; McCowan, L.M.; Heazell, A.E.; Grynspan, D.; Hutcheon, J.A.; Senger, C.; Burke, O.; Chan, Y.; Harding, J.E.; Yockell-Lelievre, J.; et al. Placental growth factor as a marker of fetal growth restriction caused by placental dysfunction. Placenta 2016, 42, 1–8. [Google Scholar] [CrossRef]
- Quezada, M.S.; Rodriguez-Calvo, J.; Villalain, C.; Gomez-Arriaga, P.I.; Galindo, A.; Herraiz, I. sFlt-1/PlGF ratio and timing of delivery in early-onset fetal growth restriction with antegrade umbilical artery flow. Ultrasound Obstet. Gynecol. 2019. [Google Scholar] [CrossRef]
- Heazell, A.E.; Hayes, D.J.; Whitworth, M.; Takwoingi, Y.; Bayliss, S.E.; Davenport, C. Biochemical tests of placental function versus ultrasound assessment of fetal size for stillbirth and small-for-gestational-age infants. Cochrane Database Syst. Rev. 2019, 5, CD012245. [Google Scholar] [CrossRef]


| Parameter | CTRL I (101–115) i | CTRL II (151–165) j | FGR I (301–315) i | FGR II (351–365) j | SGA I (201–215) i | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | 95% CI | Min. | Max. | n | Mean | 95% CI | Min. | Max. | n | Mean | 95% CI | Min. | Max. | n | Mean | 95% CI | Min. | Max. | n | Mean | 95% CI | Min. | Max. | |
| Mat. Age (years) a | 15 | 29.4 | 26.5–32.3 | 21.5 | 39.2 | 15 | 30.5 | 27.7–33.3 | 24.2 | 39.0 | 15 | 28.1 | 25.1-31.1 | 22.0 | 41.8 | 15 | 30.4 | 26.8-34.0 | 19.1 | 41.5 | 15 | 28.9 | 24.9–32.8 | 17.6 | 40.2 |
| Mat. BMI, (kg/m2) b | 15 | 22.8 | 21.7–23.9 | 19.5 | 26.9 | 15 | 23.3 | 20.4–26.2 | 17.6 | 35.7 | 15 | 22.2 | 20.6–23.9 | 18.0 | 28.9 | 15 | 24.2 | 22.4–26.1 | 19.9 | 31.9 | 15 | 22.4 | 20.6–24.3 | 16.2 | 28.1 |
| Primiparity, (%) | 15 | 100.0 | n.a. | n.a. | n.a. | 15 | 80.0 | n.a. | n.a. | n.a. | 15 | 93.3 | n.a. | n.a. | n.a. | 15 | 86.7 | n.a. | n.a. | n.a. | 15 | 86.7 | n.a. | n.a. | n.a. |
| Smoking Status, (%) | 15 | 20.0 | n.a. | n.a. | n.a. | 15 | 20.0 | n.a. | n.a. | n.a. | 15 | 46.7 | n.a. | n.a. | n.a. | 15 | 26.7 | n.a. | n.a. | n.a. | 15 | 26.7 | n.a. | n.a. | n.a. |
| Systolic bp, (mmHg) c | 15 | 115.6 | 109.2–122.0 | 99 | 135 | 15 | 116.2 | 121.1–120.3 | 106 | 129 | 15 | 120.4 | 113.6–127.2 | 96 | 139 | 15 | 130.9 | 118.6–143.1 | 83 | 162 | 15 | 117.5 | 108.9–126.2 | 84 | 146 |
| Diastolic bp, (mmHg) c | 15 | 68.9 | 63.1–74.6 | 54 | 87 | 15 | 64.9 | 60.5–69.4 | 53 | 81 | 15 | 69.1 | 63.6–74.5 | 52 | 82 | 15 | 77.3 | 68.2–86.3 | 52 | 101 | 15 | 66.3 | 60.2–72.3 | 45 | 84 |
| ga at sample, (weeks) d | 15 | 29.4 | 28.3–30.5 | 25.7 | 32.6 | 15 | 32.4 | 29.8–35.0 | 25 | 39.3 | 15 | 29.6 | 28.3–30.9 | 25.4 | 33.9 | 15 | 32.3 | 29.7–34.9 | 24 | 40.4 | 15 | 31.0 | 29.3–32.7 | 22.9 | 34.6 |
| ga at delivery, (weeks) d | 15 | 39.6 | 38.9–40.3 | 37.4 | 41.6 | 15 | 32.8 | 30.2–35.3 | 25 | 39.3 | 15 | 30.5 | 29.2–31.8 | 25.9 | 34.1 | 15 | 33.0 | 30.5–35.5 | 26.7 | 40.4 | 15 | 38.1 | 37.4–38.8 | 36.1 | 40.7 |
| Δt (days) e | 15 | 71.3 | 62.7–79.8 | 50 | 105 | 15 | 2.7 | 0.01–5.3 | 0 | 18 | 15 | 6.3 | 2.1–10.6 | 0 | 31 | 15 | 4.7 | 0.95–8.4 | 0 | 19 | 15 | 49.9 | 37.1–62.8 | 22 | 105 |
| C-section, (%) f | 15 | 20.0 | n.a. | n.a. | n.a. | 15 | 86.7 | n.a. | n.a. | n.a. | 15 | 100.0 | n.a. | n.a. | n.a. | 15 | 100.0 | n.a. | n.a. | n.a. | 15 | 66.7 | n.a. | n.a. | n.a. |
| Fetal Birth Weight, (g) | 15 | 3399 | 3232–3565 | 2960 | 3765 | 15 | 2129 | 1584–2673 | 740 | 3895 | 15 | 1015 | 845–1185 | 495 | 1525 | 15 | 1383 | 1005–1761 | 490 | 2665 | 15 | 2465 | 2299–2630 | 1950 | 2780 |
| fbw Percentile g | 15 | 47.1 | 37.5–56.8 | 14 | 70 | 15 | 50.7 | 40.8–60.5 | 25 | 85 | 15 | 5.2 | 3.8–6.6 | 2 | 9 | 15 | 4.0 | 2.5–5.5 | 1 | 9 | 15 | 4.5 | 3.2–5.7 | 1 | 9 |
| Female, (%) h | 15 | 60.0 | n.a. | n.a. | n.a. | 15 | 53.3 | n.a. | n.a. | n.a. | 15 | 40.0 | n.a. | n.a. | n.a. | 15 | 53.3 | n.a. | n.a. | n.a. | 15 | 46.7 | n.a. | n.a. | n.a. |
| No | Type of Data Set/Cohort | TP | FP | TN | FN | Sens | Spec | FPR | FNR | PPV | NPV | ROC AUC |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | training “O”/CTRL I vs. FGR I (CTRL I, n = 14; FGR I, n = 14) b | 13 | 1 | 13 | 1 | 0.93 | 0.93 | 0.07 | 0.07 | 0.93 | 0.93 | 0.95 |
| 2 | “development” test/CTRL I + II vs. FGR I + II (CTRL, I + II, n = 28; FGR I + II, n = 29) c | 26 | 6 | 22 | 3 | 0.90 | 0.79 | 0.21 | 0.10 | 0.81 | 0.88 | 0.88 |
| 3 | “valid” test/CTRL I + II and SGA I vs. FGR I + II (CTRL I + II, n = 28; SGA I, n = 14; FGR I + II, n = 29) c | 26 | 9 | 33 | 3 | 0.90 | 0.79 | 0.21 | 0.10 | 0.74 | 0.92 | 0.88 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okai, C.A.; Russ, M.; Wölter, M.; Andresen, K.; Rath, W.; Glocker, M.O.; Pecks, U. Precision Diagnostics by Affinity-Mass Spectrometry: A Novel Approach for Fetal Growth Restriction Screening during Pregnancy. J. Clin. Med. 2020, 9, 1374. https://doi.org/10.3390/jcm9051374
Okai CA, Russ M, Wölter M, Andresen K, Rath W, Glocker MO, Pecks U. Precision Diagnostics by Affinity-Mass Spectrometry: A Novel Approach for Fetal Growth Restriction Screening during Pregnancy. Journal of Clinical Medicine. 2020; 9(5):1374. https://doi.org/10.3390/jcm9051374
Chicago/Turabian StyleOkai, Charles A., Manuela Russ, Manja Wölter, Kristin Andresen, Werner Rath, Michael O. Glocker, and Ulrich Pecks. 2020. "Precision Diagnostics by Affinity-Mass Spectrometry: A Novel Approach for Fetal Growth Restriction Screening during Pregnancy" Journal of Clinical Medicine 9, no. 5: 1374. https://doi.org/10.3390/jcm9051374
APA StyleOkai, C. A., Russ, M., Wölter, M., Andresen, K., Rath, W., Glocker, M. O., & Pecks, U. (2020). Precision Diagnostics by Affinity-Mass Spectrometry: A Novel Approach for Fetal Growth Restriction Screening during Pregnancy. Journal of Clinical Medicine, 9(5), 1374. https://doi.org/10.3390/jcm9051374