Longer-Term Mental and Behavioral Health Effects of the Deepwater Horizon Gulf Oil Spill
Abstract
:1. Introduction
1.1. Longer Term Effects of Oil Spills
1.2. Longer-Term Disaster Recovery
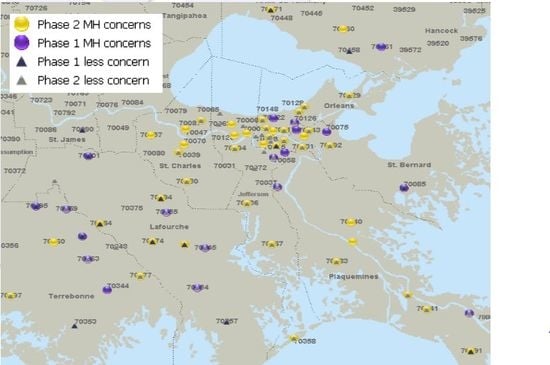
2. Deepwater Horizon Gulf Oil Spill
3. Experimental Design
4. Measures
5. Participants
6. Statistical Analysis
7. Results
| Time 1 | Time 2 | 95% CI Difference | 90% CI Equivalence | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mental Health | M | SD | M | SD | MΔ (change) | L | U | t | df | p | d | L | U |
| Anxiety | 8.0 | 7.2 | 8.0 | 7.1 | −0.05 | −1.01 | 0.90 | −0.11 | 171 | 0.91 | 0.01 | −0.14 | 0.16 |
| Serious Mental Illness | 6.8 | 6.6 | 6.2 | 6.6 | 0.65 | −0.04 | 1.34 | 1.84 | 301 | 0.07 | 0.11 | −0.01 | 0.22 |
| Depression | 9.7 | 9.3 | 10.3 | 9.5 | −0.63 | −1.98 | 0.73 | −0.91 | 170 | 0.36 | 0.07 | −0.08 | 0.22 |
| Posttraumatic Stress | 35.0 | 16.6 | 34.0 | 18.2 | 0.94 | −0.95 | 2.83 | 0.98 | 292 | 0.33 | 0.06 | −0.06 | 0.17 |
| B | SE | β | T | p | 95% CI | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Married or cohabitating | −1.53 | 0.69 | −0.11 | −2.21 | 0.028 | −2.89 | −0.17 |
| Oil/Gulf dependent occupation | 1.36 | 1.13 | 0.06 | 1.20 | 0.231 | −0.87 | 3.58 |
| Litigant | 1.35 | 1.14 | 0.06 | 1.18 | 0.237 | −0.89 | 3.59 |
| Oil spill concerns | 0.10 | 0.16 | 0.03 | 0.59 | 0.559 | −0.23 | 0.42 |
| Oil spill disruption | 0.73 | 0.10 | 0.42 | 7.16 | 0.000 | 0.53 | 0.93 |
| Hurricane Katrina Losses | 0.59 | 0.15 | 0.19 | 3.89 | 0.000 | 0.29 | 0.90 |
| Income above 40,000 | −2.41 | 0.72 | −0.16 | −3.36 | 0.001 | −3.82 | −1.00 |
| Post spill financial assistance | −2.02 | 0.89 | −0.12 | −2.26 | 0.025 | −3.78 | −0.26 |
8. Discussion
9. Conclusions
Author Contributions
Conflicts of Interest
References
- Goldstein, B.D.; Osofsky, H.J.; Lichtveld, M.Y. The Gulf oil spill. N. Engl. J. Med. 2011, 364, 1334–1348. [Google Scholar] [PubMed]
- Palinkas, L.A.; Petterson, J.S.; Russell, J.C.; Downs, M.A. Community patterns of psychiatric disorders after the Exxon Valdez oil spill. Am. J. Psychiatry 1993, 150, 1517–1524. [Google Scholar] [PubMed]
- Palinkas, L.A.; Russell, J.C.; Downs, M.A.; Petterson, J.S. Ethnic difference in stress: Coping and depressive symptoms after the Exxon Valdez oil spill. J. Nerv. Mental Disorder 1992, 180, 287–295. [Google Scholar] [CrossRef]
- Lyons, R.A.; Temple, J.M.; Evans, D.; Fone, D.L.; Palmer, S.R. Acute health effects of the Sea Empress oil spill. J. Epidemiol. Commun. Health 1999, 53, 306–310. [Google Scholar] [CrossRef]
- Gallacher, J.; Brostering, K.; Palmer, S.; Fone, D.; Lyon, R.S. Symptomatology attributable to psychological exposure to a chemical incident: A natural experiment. J. Epidemiol. Commun. Health 2007, 61, 506–512. [Google Scholar] [CrossRef] [PubMed]
- Carrasco, J.M.; Perez-Gomez, B.; Garcia-Mendizabal, M.J. Health-related quality of life and mental health in the medium-term aftermath of the Prestige oil spill in Galiza (Spain): A cross-sectional study. BMC Public Health 2007, 7, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Sabucedo, J.M.; Arce, C.; Senra, C.; Seoane, G.; Vazquez, I. Symptomatic profile and health-related quality of life of persons affected by the Prestige catastrophe. Disasters 2009, 34, 809–820. [Google Scholar] [CrossRef] [PubMed]
- Palinkas, L.A.; Petterson, J.S.; Russell, J.C.; Downs, M.A. Ethnic differences in symptoms of posttraumatic stress after the Exxon Valdez oil spill. Prehospital Disaster Med. 2004, 19, 102–112. [Google Scholar] [PubMed]
- Picou, S.; Formichella, C.; Marshall, B.; Arata, C. Community Impacts of the Exxon Valdez Oil Spill: A synthesis and elaboration of social science research. In Synthesis: Three Decades of Research on Socioeconomic Effects Related to Offshore Petroleum Development in Coastal Alaska; Stephen R. Braund & Associates: Anchorage, AK, USA, 2009; pp. 279–310. [Google Scholar]
- Picou, S.; Arata, C. Chronic Impacts of the Exxon Valdez Oil Spill: Resource Loss and Commercial Fishers. In Coping with Technological Disasters; Prince William Sound Regional Citizens’ Advisory Council: Anchorage, AK, USA, 1997; pp. J2–J43. [Google Scholar]
- National Commission on the BP Deepwater Horizon Oil Spill and Offshore Drilling. Deep Water: The Gulf Oil Disaster and the Future of Offshore Drilling; Report to the President of the USA: New Orleans, LA, USA, 2011. [Google Scholar]
- Gill, D.A.; Picou, J.S. Technological disaster and chronic community stress. Soc. Nat. Resour. 1998, 11, 795–815. [Google Scholar] [CrossRef]
- McFarlane, A.C.; Williams, R. Mental Health Services Required after Disasters: Learning from the Lasting Effects of Disasters. Depress Res. Treat. 2012, 2012. [Google Scholar] [CrossRef]
- Danya Institute. Disaster Mental Health Responder Certification Training at the DC Department of Behavioral Health. Available online: http://www.danyainstitute.org/2014/02/disaster-mental-health-responder-certification-training-at-the-dc-department-of-behavioral-health/ (accessed on 19 October 2015).
- Substance Abuse and Mental Health Services Administration (SAMHSA). Field Manual for Mental Health and Human Service Workers in Major Disasters; ERIC: Washington, DC, USA, 2000. [Google Scholar]
- Federal Emergency Management Agency. Deadlines & Timelines. Available online: http://www.fema.gov/public-assistance-local-state-tribal-and-non-profit/deadlines-timelines (accessed on 19 October 2015).
- Kessler, R.C.; Sonnega, A.; Bromet, E.; Hughes, M.; Nelson, C.B. Posttraumatic stress disorder in the National Comorbidity Survey. Arch. General Psychiatry 1995, 52, 1048–1060. [Google Scholar] [CrossRef]
- Kessler, R.C.; Galea, S.; Gruber, M.J.; Sampson, N.A.; Ursano, R.J.; Wessely, S. Trends in mental illness and suicidality after Hurricane Katrina. Mol. Psychiatry 2008, 13, 374–384. [Google Scholar] [CrossRef] [PubMed]
- Osofsky, H.J.; Osofsky, J.D.; Hansel, T.C. Deepwater Horizon Oil Spill: Mental health effects on residents in heavily affected areas. Disaster Med. Public Health Prep. 2011, 5, 280–286. [Google Scholar] [CrossRef] [PubMed]
- Abramson, D.M.; Redlener, I.E.; Stehling-Ariza, T.; Sury, J.; Banister, A.N.; Park, Y.S. Impact on Children and Families of the Deepwater Horizon Oil Spill: Preliminary Findings of the Costal Population Impact Study; Report for National Center for Disaster Preparedness: New York, NY, USA, 2010. [Google Scholar]
- Witters, D. Gulf Coast Residents Worse of Emotionally after BP Oil Spill; Gallup: Washington, DC, USA, 2010. [Google Scholar]
- Morris, J.G.; Grattan, L.M.; Mayer, B.M.; Blackburn, J.K. Psychological responses and resilience of people and communities impacted by the Deepwater Horizon oil spill. Trans. Am. Clin. Climatol. 2013, 124, 191–201. [Google Scholar]
- Buttke, D.; Vagi, S.; Bayleyegn, T.; Sircar, K.; Strine, T.; Morrison, M.; Allen, M.; Wolkin, A. Mental health needs assessment after the gulf coast oil spill—Alabama and Mississippi, 2010. Prehosp. Disaster Med. 2012, 27, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Grattan, L.M.; Roberts, S.; Mahan, W.T.; McLaughlin, P.K.; Otwell, W.S.; Morris, J.G. Early psychological impacts of the Deepwater Horizon oil spill on Florida and Alabama communities. Environ. Health Perspect. 2011, 119, 838–843. [Google Scholar] [CrossRef] [PubMed]
- Substance Abuse and Mental Health Services Administration and Centers for Disease Control and Prevention. Behavioral Health in the Gulf Coast Region Following the Deepwater Horizon Oil Spill; HHS Publication No. (SMA) 13-4737; Rockville, M.D., Ed.; Substance Abuse and Mental Health Services Administration and Centers for Disease Control and Prevention: Atlanta, GA, USA, 2013. [Google Scholar]
- Sheehan, D.V.; Harnett-Sheehan, K.; Raj, B.A. The measurement of disability. Int. Clin. Psychopharmacol. 1996, 11, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.-L.T.; Walters, E.E.; Zaslavsky, A. Short screening scales to monitor population prevalence and trends in nonspecific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef] [PubMed]
- Weathers, F.W.; Litz, B.T.; Herman, D.S.; Huska, J.A.; Keane, T.M. The PTSD Checklist (PCL): Reliability; Validity; and Diagnostic Utility. In Annual Convention of the International Society for Traumatic Stress Studies; International Society for Traumatic Stress Studies: San Antonio, TX, USA, 1993. [Google Scholar]
- Radloff, L.S.; Locke, B.Z. The community mental health assessment survey and the CES-D Scale. In Community Surveys of Psychiatric Disorders; Weissman, M.M., Myers, J.K., Ross, C.E., Eds.; Rutgers University Press: New Brunswick, NJ, USA, 1986; pp. 177–189. [Google Scholar]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Lowe, B. A brief measure for assessing generalized anxiety disorder. Arch. Inern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Wuensch, K.L. Confidence Intervals; Pooled and Separate Variances T; Department of Psychology, East Carolina University: Greenville, NC, USA, 2010. [Google Scholar]
- Lachenbruch, P.A. Equvalence Testing; United States Food and Drug Administration: Silver Spring, MD, USA, 2001. [Google Scholar]
- Osofsky, H.J.; Hansel, T.C.; Osofsky, J.D.; Speier, A. Factors Contributing to Mental and Physical Health Care in a Disaster-Prone Environment. Behav. Med. 2015, 31, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control and Prevention. Disaster Mental Health Primer: Key Principles, Issues and Questions. 2012. Available online: http://emergency.cdc.gov/mentalhealth/primer.asp (accessed on 19 October 2015). [Google Scholar]
- Picou, J.S.; Marshall, B.K.; Gill, D.A. Disaster; Litigation; and the Corrosive Community. Soc. Forces 2004, 82, 1493–1522. [Google Scholar] [CrossRef]
- Kessler, R.C.; Chiu, W.T.; Demler, O.; Walters, E.E. Prevalence; severity; and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Arch. General Psychiatry 2005, 62, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control and Prevention. An Estimated 1 in 10 U.S. Adults Report Depression. Available online: http://www.cdc.gov/features/dsdepression/ (accessed on 19 October 2015).
- National Institute of Mental Health. The Numbers Count: Mental Disorders in America 2010. Available online: http://www.nimh.nih.gov/health/publications/the-numbers-count-mental-disorders-in-america/index.shtml (accessed on 19 October 2015).
- Anxiety and Depression Association of America. Facts & Statistics. Available online: http://www.adaa.org/about-adaa/press-room/facts-statistics (accessed on 19 October 2015).
- Osofsky, H.J.; Osofsky, J.D.; Wells, J.H.; Weems, C. Integrated care: Meeting mental health needs after the Gulf oil spill. Psychiatr. Serv. 2014, 65, 280–283. [Google Scholar] [CrossRef] [PubMed]
- Masten, A.S.; Osofsky, J.D. Disasters and their impact on child development: Introduction to the special section. Child Dev. 2010, 81, 1029–1039. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hansel, T.C.; Osofsky, H.J.; Osofsky, J.D.; Speier, A. Longer-Term Mental and Behavioral Health Effects of the Deepwater Horizon Gulf Oil Spill. J. Mar. Sci. Eng. 2015, 3, 1260-1271. https://doi.org/10.3390/jmse3041260
Hansel TC, Osofsky HJ, Osofsky JD, Speier A. Longer-Term Mental and Behavioral Health Effects of the Deepwater Horizon Gulf Oil Spill. Journal of Marine Science and Engineering. 2015; 3(4):1260-1271. https://doi.org/10.3390/jmse3041260
Chicago/Turabian StyleHansel, Tonya Cross, Howard J. Osofsky, Joy D. Osofsky, and Anthony Speier. 2015. "Longer-Term Mental and Behavioral Health Effects of the Deepwater Horizon Gulf Oil Spill" Journal of Marine Science and Engineering 3, no. 4: 1260-1271. https://doi.org/10.3390/jmse3041260