Prayer, Meditation, and Anxiety: Durkheim Revisited
Abstract
1. Introduction
2. Empirical Background
3. Theory and Hypotheses
To extend this point, Durkheim (1915, pp. 427–28) then proceeds to compare group-based religious activities (ritual ceremonies) with their secular counterparts (festivals or games), arguing that the former is a moral endeavor while the latter is a more frivolous affair. Religious rites aim toward re-creation, that is, the moral remaking of persons and society, while festivals or games are purely recreational.the moral forces expressed by religious symbols are real forces with which we must reckon…The representations which [a religious rite] seeks to awaken and maintain in our minds are not vain images which correspond to nothing in reality…They are as necessary for the well working of our moral life as our food is for the maintenance of our physical life, for it is through them that the group affirms and maintains itself, and we know the point to which this is indispensible for the individual…So a rite is something different from a game; it is a part of the serious life…It has its share in the feeling of comfort which the worshipper draws from the rite performed; for recreation [re-creation] is one of the forms of the moral remaking which is the principal object of the positive rite.
4. Methods
4.1. Data
4.2. Dependent Variable and Focal Independent Variables
4.3. Control Variables
4.4. Analytical Strategy
5. Results
6. Discussion and Conclusions
Acknowledgments
Conflicts of Interest
Appendix A
| Questionnaire Items Included in BRS Anxiety Index (Cronbach’s α = 0.92) |
| (Q33A) Over the past month, how often have you felt nervous, anxious, or on edge? |
| (Q33B) Over the past month, how often have you thought too much about pointless matters? |
| (Q33C) Over the past month, how often have you been afraid something terrible would happen if you did not perform certain rituals? |
| (Q33D) Over the past month, how often have you felt that it is not safe to trust anyone? |
| (Q33E) Over the past month, how often have you not been able to stop or control worrying? |
| (Q33F) Over the past month, how often have you felt compelled to perform certain actions, for no justifiable reason? |
| (Q33G) Over the past month, how often have you become anxious doing things because people were watching? |
| (Q33H) Over the past month, how often have you been plagued by thoughts or images that you cannot get out of your mind? |
| (Q33I) Over the past month, how often have you repeated simple actions that realistically did not need to be repeated? |
| (Q33J) Over the past month, how often have you thought too much about things that would not bother other people? |
| (Q33K) Over the past month, how often have you feared that you might do something to embarrass yourself in a social situation? |
| (Q33L) Over the past month, how often have you endured intense anxiety in social or performance situations? |
| (Q33M) Over the past month, how often have you felt that people were taking advantage of you? |
| (Q33N) Over the past month, how often have you worried too much about different things? |
| (Q33O) Over the past month, how often have you felt like you were being watched or talked about by others? |
References
- Acevedo, Gabriel A., Christopher G. Ellison, and Xiaohe Xu. 2014. Is it really religion? Comparing the main and stress-buffering effects of religious and secular civic engagement on psychological distress. Society and Mental Health 4: 111–28. [Google Scholar] [CrossRef]
- Ai, Amy L., Christopher Peterson, Steven F. Bolling, and Harold G. Koenig. 2002. Private prayer and the optimism of middle-aged and older patients awaiting cardiac surgery. The Gerontologist 42: 70–81. [Google Scholar] [CrossRef] [PubMed]
- Ai, Amy L., Christopher Peterson, Terrence N. Tice, Bu Huang, Willard Rogers, and Steven F. Bolling. 2007. The influence of prayer coping on mental health among cardiac surgery patients. Journal of Health Psychology 12: 580–96. [Google Scholar] [CrossRef] [PubMed]
- Alvarado, Katherine A., Donald I. Templer, Charles Bresler, and Shan Thomas-Dobson. 1995. The relationship of religious variables to death depression and death anxiety. Journal of Clinical Psychology 51: 202–4. [Google Scholar] [CrossRef]
- Atkinson, Bruce E., and H. Newton Maloney. 1994. Religious maturity and psychological distress among older Christian women. International Journal for the Psychology of Religion 4: 165–79. [Google Scholar] [CrossRef]
- Belding, Jennifer N., Malcolm G. Howard, Anne M. McGuire, Amanda C. Schwartz, and Janie H. Wilson. 2010. Social buffering by God: Prayer and measures of stress. Journal of Religion and Health 49: 179–87. [Google Scholar] [CrossRef] [PubMed]
- Boelens, Peter A., Roy R. Reeves, William H. Replogle, and Harold G. Koenig. 2009. A randomized trial of the effect of prayer on depression and anxiety. The International Journal of Psychiatry in Medicine 39: 377–92. [Google Scholar] [CrossRef] [PubMed]
- Boelens, Peter A., Roy R. Reeves, William H. Replogle, and Harold G. Koenig. 2012. The effect of prayer on depression and anxiety: Maintenance of positive influence one year after prayer intervention. The International Journal of Psychiatry in Medicine 43: 85–98. [Google Scholar] [CrossRef] [PubMed]
- Bonelli, Raphael M., and Harold G. Koenig. 2013. Mental disorders, religion, and spirituality 1990 to 2010: A systematic evidence-based review. Journal of Religion and Health 52: 657–73. [Google Scholar] [CrossRef] [PubMed]
- Bradshaw, Matt, Christopher G. Ellison, and Kevin J. Flannelly. 2008. Prayer, God imagery, and symptoms of psychopathology. Journal for the Scientific Study of Religion 47: 644–59. [Google Scholar] [CrossRef]
- Clarke, Tainya C., Lindsey I. Black, Barbara J. Stussman, Patricia M. Barnes, and Richard L. Nahin. 2015. Trends in the Use of Complementary Health Approaches among Adults: United States, 2002–2012. National Health Statistics Report, no. 79. Hyattsville: National Center for Health Statistics. [Google Scholar]
- Connell, Raewyn. 2011. Southern Bodies and disability: Re-thinking concepts. Third World Quarterly 32: 1369–81. [Google Scholar] [CrossRef]
- Delmonte, Michael M. 1985. Meditation and anxiety reduction: A literature review. Clinical Psychology Review 5: 91–102. [Google Scholar] [CrossRef]
- Diagnostic and Statistical Manual of Mental Disorders (Text Revision) (DSM-IV-TR). 2000. Washington: American Psychiatric Association.
- Durkheim, Emile. 1915. The Elementary Forms of the Religious Life. New York: The Free Press. [Google Scholar]
- Durkheim, Emile. 1951. Suicide: A Study in Sociology. New York: The Free Press. [Google Scholar]
- Durkheim, Emile. 1973. On Morality and Society. Edited and with an introduction by Robert N. Bellah. Chicago: University of Chicago Press. [Google Scholar]
- Ellison, Christopher G. 1991. Religious involvement and subjective well-being. Journal of Health and Social Behavior 32: 80–99. [Google Scholar] [CrossRef] [PubMed]
- Ellison, Christopher G. 1995. Race, religious involvement, and depressive symptomatology in a Southeastern U.S. community. Social Science and Medicine 40: 1561–72. [Google Scholar] [CrossRef]
- Ellison, Christopher G., and Daisy Fan. 2008. Daily spiritual experiences and psychological well-being among US adults. Social Indicators Research 88: 247–71. [Google Scholar] [CrossRef]
- Ellison, Christopher G., and Robert J. Taylor. 1996. Turning to prayer: Social and situational antecedents of religious coping among African American adults. Review of Religious Research 38: 111–31. [Google Scholar] [CrossRef]
- Ellison, Christopher G., Jason D. Boardman, David R. Williams, and James S. Jackson. 2001. Religious involvement, stress, and mental health: Findings from the 1995 Detroit Area Study. Social Forces 80: 215–49. [Google Scholar] [CrossRef]
- Ellison, Christopher G., Amy M. Burdette, and Terrence D. Hill. 2009. Blessed assurance: Religion, anxiety, and tranquility among U.S. adults. Social Science Research 38: 656–67. [Google Scholar] [CrossRef] [PubMed]
- Ellison, Christopher G., Matt Bradshaw, Kevin J. Flannelly, and Kathleen C. Galek. 2014. Prayer, attachment to God, and symptoms of anxiety-related disorders among U.S. adults. Sociology of Religion 75: 208–33. [Google Scholar] [CrossRef]
- Evans, Susan, Stephen Ferrando, Marianne Findler, Charles Stowell, Colette Smart, and Dean Haglin. 2008. Mindfulness-based cognitive therapy for generalized anxiety disorder. Journal of Anxiety Disorders 22: 716–21. [Google Scholar] [CrossRef] [PubMed]
- Gordon, William Van, Edo Shonin, Masood Zangeneh, and Mark D. Griffiths. 2014. Work-related mental health and job performance: Can mindfulness help? International Journal of Mental Health and Addiction 12: 129–37. [Google Scholar] [CrossRef][Green Version]
- Goyal, Madhav, Sonal Singh, and Erica M. S. Sabinga. 2014. Meditation programs for psychological stress and well-being: A systematic review and meta-anlaysis. JAMA Internal Medicine 174: 357–68. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, Paul E., Tamar Sisitsky, Ronald G. Kessler, and A. J. Fyer. 1999. The economic burden of anxiety in the 1990s. Journal of Clinical Psychiatry 60: 427–35. [Google Scholar] [CrossRef] [PubMed]
- Greenfield, Emily A., George E. Vaillant, and Nadine F. Marks. 2009. Do formal religious participation and spiritual perceptions have independent linkages with diverse dimensions of psychological well-being? Journal of Health and Social Behavior 50: 196–212. [Google Scholar] [CrossRef] [PubMed]
- Gu, Jenny, Clara Strauss, Rod Bond, and Kate Cavanagh. 2015. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review 37: 1–12. [Google Scholar] [CrossRef] [PubMed]
- Harris, J. Irene, Sean W. Schoneman, and Stephanie R. Carrera. 2005. Preferred prayer styles and anxiety control. Journal of Religion and Health 44: 403–12. [Google Scholar] [CrossRef]
- Hill, Peter C., and Kenneth I. Pargament. 2008. Advances in the conceptualization and measurement of religion and spirituality: Implications for physical and mental health research. American Psychologist 58: 64–74. [Google Scholar] [CrossRef]
- Hoge, Elizabeth A., Eric Bui, Luana Marques, Christina A. Metcalf, Laura K. Morris, Donald J. Robinaugh, John J. Worthington, Mark H. Pollack, and Naomi M. Simon. 2013. Randomized controlled trial of Mindfulness Meditation for generalized anxiety disorder: Effects on anxiety and stress reactivity. Journal of Clinical Psychiatry 74: 786–92. [Google Scholar] [CrossRef] [PubMed]
- Kessler, Ronald C., Wai Tat Chiu, Olga Demler, and Ellen E. Walters. 2005a. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62: 617–27. [Google Scholar] [CrossRef] [PubMed]
- Kessler, Ronald C., Patricia Berglund, Olga Demler, Robert Jin, Kathleen R. Merikangas, and Ellen E. Walters. 2005b. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62: 593–602. [Google Scholar] [CrossRef] [PubMed]
- Koenig, Harold G. 1993. The relationship between Judeo-Christian religion and mental health among middle-aged and older adults. Advances 9: 33–39. [Google Scholar]
- Koenig, Harold G. 2009. Research on religion, spirituality, and mental health: A review. The Canadian Journal of Psychiatry 54: 283–91. [Google Scholar] [CrossRef] [PubMed]
- Koenig, Harold G. 2015. Religion, spirituality, and health: A review and update. Advances in Mind-Body Medicine 29: 19–26. [Google Scholar] [PubMed]
- Koenig, Harold G., Stephen M. Ford, Linda K. George, Dan G. Blazer, and Keith G. Meador. 1993a. Religion and anxiety disorder: An examination and comparison of associations in young, middle-aged, and elderly adults. Journal of Anxiety Disorders 7: 321–42. [Google Scholar] [CrossRef]
- Koenig, Harold G., Linda K. George, Judith C. Hays, David B. Larson, Harvey J. Cohen, and Dan G. Blazer. 1993b. The relationship between religion and anxiety in a sample of community-dwelling older adults. Journal of Geriatric Psychiatry 26: 65–93. [Google Scholar]
- Koenig, Harold G., Linda K. George, Dan G. Blazer, Keith G. Meador, and Peter B. Dyck. 1994. Religious affiliation and psychiatric disorder among Protestant Baby Boomers. Psychiatric Services 45: 586–96. [Google Scholar] [CrossRef]
- Koenig, Harold G., Judith C. Hays, Linda K. George, Dan G. Blazer, David B. Larson, and Lawrence R. Landerman. 1997. Modeling the cross-sectional relationships between religion, physical health, social support, and depressive symptoms. American Journal of Geriatric Psychiatry 5: 131–44. [Google Scholar] [CrossRef] [PubMed]
- Krause, Neal, Christopher G. Ellison, Benjamin A. Shaw, John P. Marcum, and Jason D. Boardman. 2001. Church-based social support and religious coping. Journal for the Scientific Study of Religion 40: 637–56. [Google Scholar] [CrossRef]
- Krisanaprakornkit, Thawatchai, Wimonrat Sriraj, Nawanant Piyavhatkul, and Malinee Laopaiboon. 2006. Meditation therapy for anxiety disorders. Cochrane Database of Systematic Reviews. [Google Scholar] [CrossRef]
- Levin, Jeffrey S. 2004. Prayer, love, and transcendence: An epidemiologic perspective. In Religious Influences on Health and Well-Being in the Elderly. Edited by K. Warner Schaie, Neal Krause and Alan Booth. New York: Springer, pp. 69–95. [Google Scholar]
- Maltby, John, Christopher Alan Lewis, and Liza Day. 1999. Religious orientation and psychological well-being: The role of the frequency of personal prayer. British Journal of Health Psychology 4: 363–78. [Google Scholar] [CrossRef]
- McCullough, Michael E. 1995. Prayer and health: Conceptual issues, research review, and research agenda. Journal of Psychology and Theology 23: 15–29. [Google Scholar]
- Moreira-Almeida, Alexander, Francisco Lotufo Neto, and Harold G. Koenig. 2006. Religiousness and mental health: A review. Revista brasileira de psiquiatria 28: 242–50. [Google Scholar]
- Musick, Marc A., Harold G. Koenig, Judith C. Hays, and Harvey J. Cohen. 1998. Religious activity and depression among community-dwelling elderly persons with cancer: The moderating effect of race. Journal of Gerontology: Social Sciences 53B: S218–S227. [Google Scholar] [CrossRef]
- NIMH (National Institute of Mental Health). 2016. Anxiety disorders. Available online: https://www.nimh.nih.gov/health/topics/anxiety-disorders/index.shtml (accessed on 30 May 2017).
- Park, Crystal L., Lawrence H. Cohen, and Lisa Herb. 1990. Intrinsic religiousness and religious coping as life stress moderators for Catholics versus Protestants. Journal of Personality and Social Psychology 59: 562–74. [Google Scholar] [CrossRef] [PubMed]
- Peterson, Linda Gay, and Lori Pbert. 1992. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry 149: 936–43. [Google Scholar]
- Schieman, Scott, Tetyana Pudrovska, Leonard I. Pearlin, and Christopher G. Ellison. 2006. The sense of divine control and mental health: Variations by race and socioeconomic status. Journal for the Scientific Study of Religion 45: 529–49. [Google Scholar] [CrossRef]
- Schieman, Scott, Alex Bierman, and Christopher G. Ellison. 2013. Religion and mental health. In Handbook of the Sociology of Mental Health. New York: Springer, pp. 457–78. [Google Scholar]
- Shreve-Neiger, Andrea K., and Barry A. Edelstein. 2004. Religion and anxiety: A critical review of the literature. Clinical Psychology Review 24: 379–97. [Google Scholar] [CrossRef] [PubMed]
- Stratton, Stephen P. 2015. Mindfulness and contemplation: Secular and religious traditions in Western context. Counseling and Values 60: 100–18. [Google Scholar] [CrossRef]
- Thorson, James A. 1998. Religion and anxiety: Which anxiety? Which religion? In Handbook of Religion and Mental Health. Edited by Harold G. Koenig. San Diego: Academic Press, pp. 147–60. [Google Scholar]
- Toneatto, Tony, and Linda Nguyen. 2007. Does mindfulness meditation improve anxiety and mood symptoms? A review of the controlled research. The Canadian Journal of Psychiatry 52: 260–66. [Google Scholar] [CrossRef] [PubMed]
- Unterrainer, Human-Friedrich, Andrew J. Lewis, and Andreas Fink. 2014. Religious/spiritual well-being, personality and mental health: A review of results and conceptual issues. Journal of Religion and Health 53: 382–92. [Google Scholar] [CrossRef] [PubMed]
- Wang Philip S., Michael Lane, Mark Olfson, Harold A. Pincus, Kenneth B. Wells, and Ronald C. Kessler. 2005. Twelve month use of mental health services in the United States. Archives of General Psychiatry 62: 629–40. [Google Scholar] [CrossRef] [PubMed]
- West, Michael A., ed. 2016. The Psychology of Meditation: Research and Practice. New York: Oxford University Press. [Google Scholar]
- Wiegand, Katherine Elizabeth Kurek. 2004. The Effects of Prayer on Anxiety and Performance. Ph.D. dissertation, Purdue University, West Lafayette, IN, USA. [Google Scholar]
- Zeidan, Fadel, Katherine T. Martucci, Robert A. Kraft, John G. McHaffie, and Robert C. Coghill. 2014. Neural correlates of mindfulness meditation-related anxiety relief. Social Cognitive and Affective Neuroscience 9: 751–59. [Google Scholar] [CrossRef] [PubMed]
| 1 | Tests of variance inflation factors (VIFs) indicate the absence of multicollinearity in Model 5, with VIF scores for all variables below 2. |
| Range | Mean (%) | SD | α | |
|---|---|---|---|---|
| Dependent Variable | ||||
| Anxiety | 0−2 | 0.82 | 0.39 | 0.92 |
| Meditation, Prayer, and Attendance | ||||
| Meditation (yes/no) | 0−1 | (27) | ||
| Individual prayer | 0−5 | 3.01 | 1.83 | |
| Communal prayer | 1−4 | 1.35 | 0.78 | |
| Religious attendance | 0−8 | 3.90 | 2.97 | |
| Denominational Affiliation | ||||
| Evangelical Protestant (reference) | 0−1 | (30) | ||
| Mainline Protestant | 0−1 | (25) | ||
| Catholic | 0−1 | (24) | ||
| Other | 0−1 | (11) | ||
| None | 0−1 | (10) | ||
| Controls | ||||
| Age | 18−108 | 55.87 | 16.25 | |
| Female | 0−1 | (54) | ||
| Male (reference) | 0−1 | (46) | ||
| White (reference) | 0−1 | (74) | ||
| Black | 0−1 | (9) | ||
| Hispanic | 0−1 | (6) | ||
| Other | 0−1 | (11) | ||
| Married | 0−1 | (63) | ||
| Not married (reference) | 0−1 | (37) | ||
| Some college or less (reference) | 0−1 | (62) | ||
| College graduate | 0−1 | (19) | ||
| Post-graduate | 0−1 | (19) | ||
| Household income | 1−7 | 4.31 | 1.63 |
| (1) | (2) | (3) | (4) | (5) | (6) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Religious Engagement | ||||||||||||
| Individual prayer | −0.012 | * | −0.004 | −0.005 | ||||||||
| Communal prayer | 0.007 | 0.026 | * | 0.051 | ** | |||||||
| Religious attendance | −0.015 | *** | −0.020 | *** | −0.022 | *** | ||||||
| Meditation | −0.001 | 0.007 | 0.009 | |||||||||
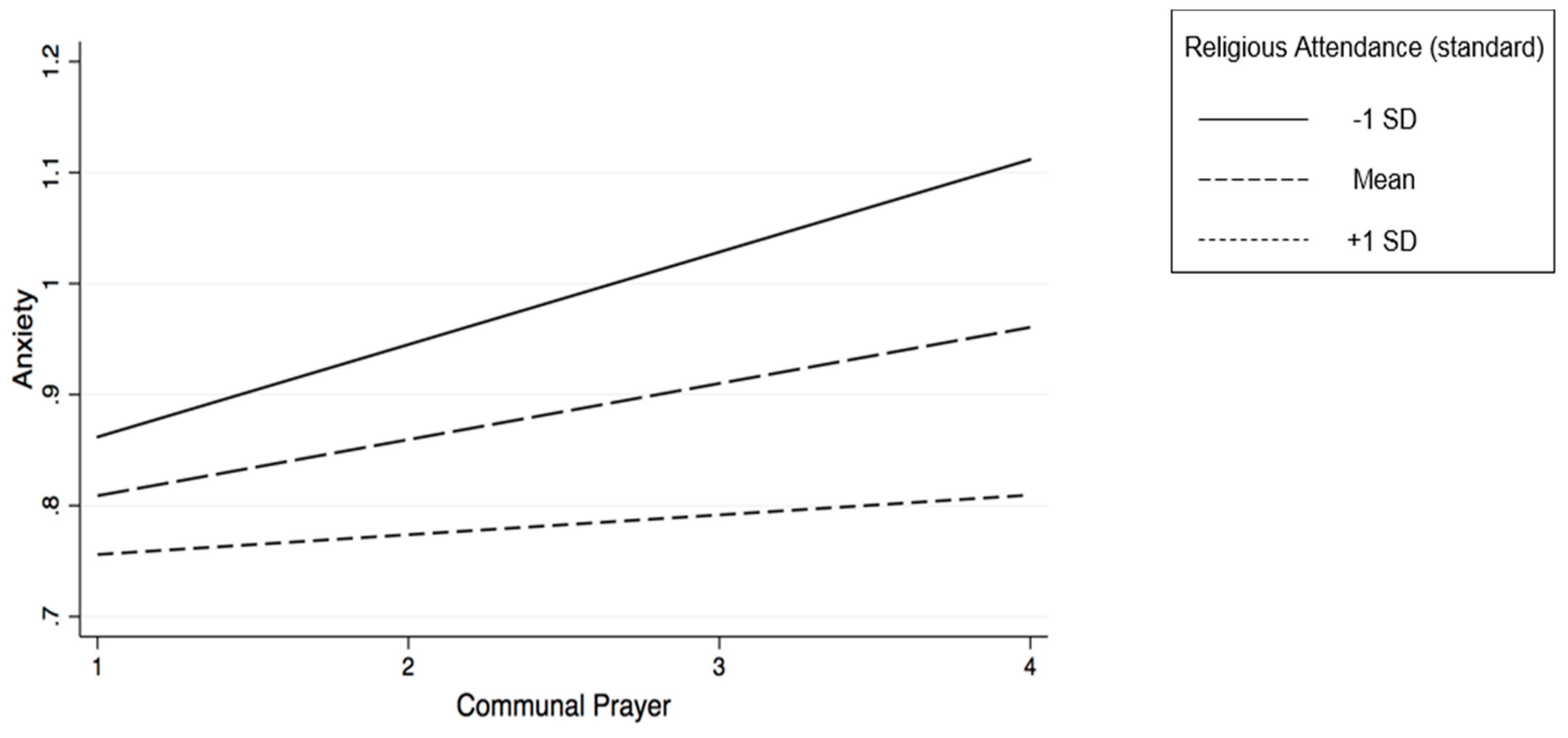
| Communal prayer x attendance | −0.011 | * | ||||||||||
| Denominational Affiliation | ||||||||||||
| Mainline Protestant | 0.012 | 0.016 | 0.012 | 0.016 | 0.012 | 0.012 | ||||||
| Catholic | −0.006 | −0.003 | −0.008 | −0.003 | −0.009 | −0.009 | ||||||
| Other | −0.011 | −0.006 | −0.014 | −0.006 | −0.015 | −0.018 | ||||||
| None | −0.090 | * | −0.054 | −0.121 | ** | −0.055 | −0.111 | ** | −0.107 | |||
| Controls | ||||||||||||
| Age | −0.002 | ** | −0.002 | ** | −0.002 | ** | −0.002 | ** | −0.002 | ** | −0.002 | ** |
| Female | 0.023 | 0.015 | 0.017 | 0.015 | 0.018 | 0.016 | ||||||
| Black | −0.003 | −0.014 | −0.004 | −0.012 | −0.013 | −0.016 | ||||||
| Hispanic | −0.005 | −0.003 | −0.009 | −0.003 | −0.005 | −0.004 | ||||||
| Other | 0.011 | 0.008 | 0.002 | 0.008 | 0.002 | −0.002 | ||||||
| Married | −0.070 | ** | −0.073 | ** | −0.061 | ** | −0.072 | ** | −0.062 | ** | −0.062 | ** |
| College graduate | −0.112 | *** | −0.112 | *** | −0.105 | *** | −0.112 | *** | −0.103 | *** | −0.104 | *** |
| Post-graduate | −0.080 | ** | −0.078 | ** | −0.070 | ** | −0.079 | ** | −0.068 | ** | −0.068 | ** |
| Household income | −0.030 | *** | −0.028 | *** | −0.030 | *** | −0.029 | *** | −0.029 | *** | −0.029 | *** |
| Intercept | 1.161 | 1.112 | 1.172 | 1.124 | 1.129 | 1.099 | ||||||
| R2 | 0.066 | 0.064 | 0.075 | 0.064 | 0.078 | 0.080 | ||||||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bartkowski, J.P.; Acevedo, G.A.; Van Loggerenberg, H. Prayer, Meditation, and Anxiety: Durkheim Revisited. Religions 2017, 8, 191. https://doi.org/10.3390/rel8090191
Bartkowski JP, Acevedo GA, Van Loggerenberg H. Prayer, Meditation, and Anxiety: Durkheim Revisited. Religions. 2017; 8(9):191. https://doi.org/10.3390/rel8090191
Chicago/Turabian StyleBartkowski, John P., Gabriel A. Acevedo, and Harriet Van Loggerenberg. 2017. "Prayer, Meditation, and Anxiety: Durkheim Revisited" Religions 8, no. 9: 191. https://doi.org/10.3390/rel8090191
APA StyleBartkowski, J. P., Acevedo, G. A., & Van Loggerenberg, H. (2017). Prayer, Meditation, and Anxiety: Durkheim Revisited. Religions, 8(9), 191. https://doi.org/10.3390/rel8090191






