A Novel Pulsatile Bioreactor for Mechanical Stimulation of Tissue Engineered Cardiac Constructs
Abstract
:1. Introduction
2. Experimental Section
2.1. Bioreactor Construction
2.2. Bioreactor Sterilization
2.3. Bioreactor Functionality
2.4. Cell Seeding on Non-Degradable Synthetic Scaffolds
2.4.1. Cell Type
2.4.2. Scaffold Type
2.4.3. Seeding Procedure
2.5. Adherence Rate of UCMSC
2.6. Scanning Electron Microscopy (SEM)
3. Results and Discussion
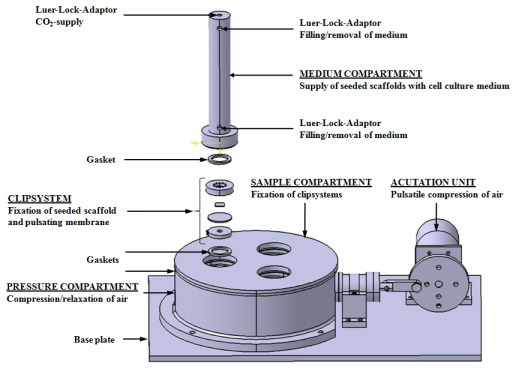
3.1. Bioreactor Design

a) Core Unit
b) Actuation Unit

3.2. Bioreactor Function


3.3. Bioreactor Sterility
3.4. Bioreactor Functionality

3.5. Adherence of UCMSC after Mechanical Stress

3.6. Morphology of UCMSC after Mechanical Stress

4. Conclusions
Acknowledgments
References
- Morsi, Y.S.; Yang, W.W.; Owida, A.; Wong, C.S. Development of a novel pulsatile bioreactor for tissue culture. J. Artif. Organs 2007, 10, 109–114. [Google Scholar]
- Wintermantel, E.; Ha, S.W. Medizintechnik Life Science Engineering; Springer Verlag: Berlin, Heidelberg, Germany, 2008; pp. 733–740. [Google Scholar]
- Barron, V.; Lyons, E.; Stenson-Cox, C.; McHugh, P.E.; Pandit, A. Bioreactors for cardiovascular cell and tissue growth: A review. Ann. Biomed. Eng. 2003, 31, 1017–1030. [Google Scholar]
- Shachar, M.; Cohen, S. Cardiac tissue engineering, ex-vivo: Design principles in biomaterials and bioreactors. Heart Fail. Rev. 2003, 8, 271–276. [Google Scholar]
- Bilodeau, K.; Mantovani, D. Bioreactors for tissue engineering: Focus on mechanical constraints. A comparative review. Tissue Eng. 2006, 12, 2367–2383. [Google Scholar]
- Chen, H.C.; Hu, Y.C. Bioreactors for tissue engineering. Biotechnol. Lett. 2006, 28, 1415–1423. [Google Scholar]
- Goldstein, A.S.; Christ, G. Functional tissue engineering requires bioreactor strategies. Tissue Eng. Part A 2009, 15, 739–740. [Google Scholar]
- Dumont, K.; Yperman, J.; Verbeken, E.; Segers, P.; Meuris, B.; Vandenberghe, S.; Flameng, W.; Verdonck, P.R. Design of a new pulsatile bioreactor for tissue engineered aortic heart valve formation. Artif. Organs 2002, 26, 710–714. [Google Scholar]
- Engelmayr, G.C., Jr.; Hildebrand, D.K.; Sutherland, F.W.; Mayer, J.E., Jr.; Sacks, M.S. A novel bioreactor for the dynamic flexural stimulation of tissue engineered heart valve biomaterials. Biomaterials 2003, 24, 2523–2532. [Google Scholar]
- Akins, R.E.; Boyce, R.A.; Madonna, M.L.; Schroedl, N.A.; Gonda, S.R.; McLaughlin, T.A.; Hartzell, C.R. Cardiac organogenesis in vitro: Reestablishment of three-dimensional tissue architecture by dissociated neonatal rat ventricular cells. Tissue Eng. 1999, 5, 103–118. [Google Scholar]
- Freed, L.E.; Vunjak-Novakovic, G. Microgravity tissue engineering. In Vitro Cell Dev. Biol. Anim. 1997, 33, 381–385. [Google Scholar]
- Brown, M.A.; Iyer, R.K.; Radisic, M. Pulsatile perfusion bioreactor for cardiac tissue engineering. Biotechnol. Prog. 2008, 24, 907–920. [Google Scholar]
- Akhyari, P.; Fedak, P.W.; Weisel, R.D.; Lee, T.Y.; Verma, S.; Mickle, D.A.; Li, R.K. Mechanical stretch regimen enhances the formation of bioengineered autologous cardiac muscle grafts. Circulation 2002, 106, I137–I142. [Google Scholar]
- Fink, C.; Ergun, S.; Kralisch, D.; Remmers, U.; Weil, J.; Eschenhagen, T. Chronic stretch of engineered heart tissue induces hypertrophy and functional improvement. FASEB J. 2000, 14, 669–679. [Google Scholar]
- Zimmermann, W.H.; Schneiderbanger, K.; Schubert, P.; Didie, M.; Munzel, F.; Heubach, J.F.; Kostin, S.; Neuhuber, W.L.; Eschenhagen, T. Tissue engineering of a differentiated cardiac muscle construct. Circ. Res. 2002, 90, 223–230. [Google Scholar]
- Sodian, R.; Lemke, T.; Loebe, M.; Hoerstrup, S.P.; Potapov, E.V.; Hausmann, H.; Meyer, R.; Hetzer, R. New pulsatile bioreactor for fabrication of tissue-engineered patches. J. Biomed. Mater. Res. 2001, 58, 401–405. [Google Scholar]
- Birla, R.K.; Huang, Y.C.; Dennis, R.G. Development of a novel bioreactor for the mechanical loading of tissue-engineered heart muscle. Tissue Eng. 2007, 13, 2239–2248. [Google Scholar]
- Hollweck, T.; Marschmann, M.; Hartmann, I.; Akra, B.; Meiser, B.; Reichart, B.; Eblenkamp, M.; Wintermantel, E.; Eissner, G. Comparative analysis of adherence, viability, proliferation and morphology of umbilical cord tissue-derived mesenchymal stem cells seeded on different titanium-coated expanded polytetrafluoroethylene scaffolds. Biomed. Mater. 2010, 5, 065004. [Google Scholar]
- Seshareddy, K.; Troyer, D.; Weiss, M.L. Method to isolate mesenchymal-like cells from Wharton's Jelly of umbilical cord. Methods Cell Biol. 2008, 86, 101–119. [Google Scholar]
- Hartmann, I.; Hollweck, T.; Haffner, S.; Krebs, M.; Meiser, B.; Reichart, B.; Eissner, G. Umbilical cord tissue-derived mesenchymal stem cells grow best under GMP-compliant culture conditions and maintain their phenotypic and functional properties. J. Immunol. Methods 2010, 363, 80–89. [Google Scholar]
- Campard, D.; Lysy, P.A.; Najimi, M.; Sokal, E.M. Native umbilical cord matrix stem cells express hepatic markers and differentiate into hepatocyte-like cells. Gastroenterology 2008, 134, 833–848. [Google Scholar]
- Chen, M.Y.; Lie, P.C.; Li, Z.L.; Wei, X. Endothelial differentiation of Wharton's jelly-derived mesenchymal stem cells in comparison with bone marrow-derived mesenchymal stem cells. Exp. Hematol. 2009, 37, 629–640. [Google Scholar]
© 2011 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Hollweck, T.; Akra, B.; Häussler, S.; Überfuhr, P.; Schmitz, C.; Pfeifer, S.; Eblenkamp, M.; Wintermantel, E.; Eissner, G. A Novel Pulsatile Bioreactor for Mechanical Stimulation of Tissue Engineered Cardiac Constructs. J. Funct. Biomater. 2011, 2, 107-118. https://doi.org/10.3390/jfb2030107
Hollweck T, Akra B, Häussler S, Überfuhr P, Schmitz C, Pfeifer S, Eblenkamp M, Wintermantel E, Eissner G. A Novel Pulsatile Bioreactor for Mechanical Stimulation of Tissue Engineered Cardiac Constructs. Journal of Functional Biomaterials. 2011; 2(3):107-118. https://doi.org/10.3390/jfb2030107
Chicago/Turabian StyleHollweck, Trixi, Bassil Akra, Simon Häussler, Peter Überfuhr, Christoph Schmitz, Stefan Pfeifer, Markus Eblenkamp, Erich Wintermantel, and Günther Eissner. 2011. "A Novel Pulsatile Bioreactor for Mechanical Stimulation of Tissue Engineered Cardiac Constructs" Journal of Functional Biomaterials 2, no. 3: 107-118. https://doi.org/10.3390/jfb2030107