Effects of High-Intensity Interval Training on Selected Adipokines and Cardiometabolic Risk Markers in Normal-Weight and Overweight/Obese Young Males—A Pre-Post Test Trial
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Participants
2.3. Study Protocol
2.4. Training Program
2.5. Blood Sampling and Methods of Analysis
2.6. Statistical Analysis
3. Results
3.1. Associations of the Adipokines with Cardiometabolic Risk Markers
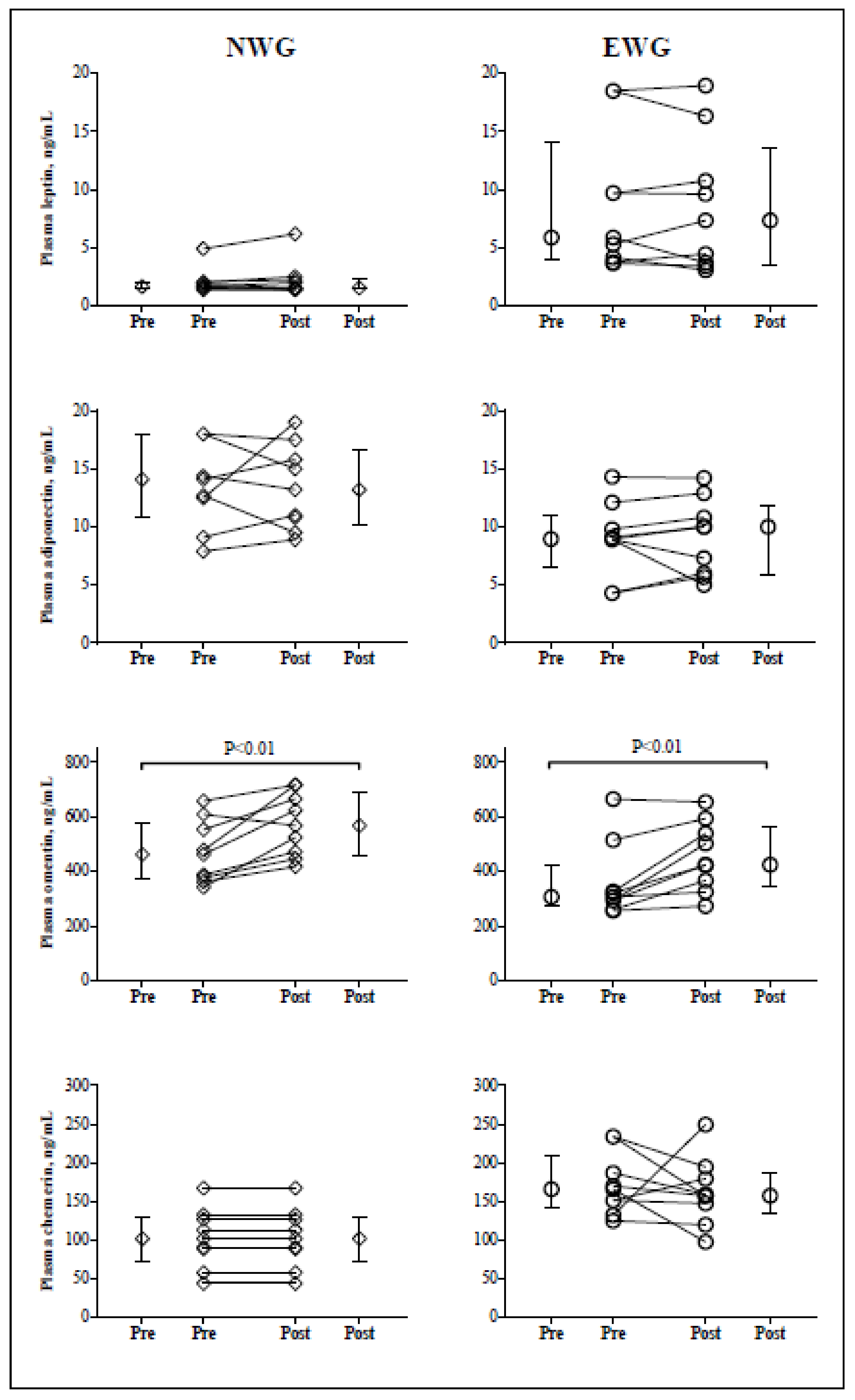
3.2. Adipokines Responses to HIIT
3.3. Correlations of Training-Induced Adipokines and Cardiometabolic Markers Changes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fantuzzi, G. Adipose tissue, adipokines, and inflammation. J. Allergy Clin. Immunol. 2005, 115, 911–919; quiz 920. [Google Scholar] [CrossRef] [PubMed]
- Ouerghi, N.; Ben Fradj, M.K.; Talbi, E.; Bezrati, I.; Feki, M.; Bouassida, A. Association of selected adipokines with metabolic syndrome and cardio-metabolic risk factors in young males. Cytokine 2020, 133, 155170. [Google Scholar] [CrossRef] [PubMed]
- Lihn, A.S.; Pedersen, S.B.; Richelsen, B. Adiponectin: Action, regulation, and association to insulin sensitivity. Obes. Rev. 2005, 6, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Esteghamati, A.; Khalilzadeh, O.; Anvari, M.; Rashidi, A.; Mokhtari, M.; Nakhjavani, M. Association of serum leptin levels with homeostasis model assessment-estimated insulin resistance and metabolic syndrome: The key role of central obesity. Metab. Syndr. Relat. Disord. 2009, 7, 447–452. [Google Scholar] [CrossRef]
- Yamawaki, H.; Kameshima, S.; Usui, T.; Okada, M.; Hara, Y. A novel adipocytokine, chemerin exerts anti-inflammatory roles in human vascular endothelial cells. Biochem. Biophys. Res. Commun. 2012, 423, 152–157. [Google Scholar] [CrossRef]
- Menzel, J.; di Giuseppe, R.; Biemann, R.; Wittenbecher, C.; Aleksandrova, K.; Pischon, T.; Fritsche, A.; Schulze, M.B.; Boeing, H.; Iser-mann, B.; et al. Omentin-1 and risk of myocardial infarction and stroke: Results from the EPIC-Potsdam cohort study. Atherosclerosis 2016, 251, 415–421. [Google Scholar] [CrossRef] [Green Version]
- Wittenbecher, C.; Menzel, J.; Carstensen-Kirberg, M.; Biemann, R.; di Giuseppe, R.; Fritsche, A.; Isermann, B.; Herder, C.; Aleksandrova, K.; Boeing, H.; et al. Omentin-1, adiponectin, and the risk of developing type 2 diabetes. Diabetes Care 2016, 39, e79–e80. [Google Scholar] [CrossRef] [Green Version]
- Zhang, M.; Tan, X.; Yin, C.; Wang, L.; Tie, Y.; Xiao, Y. Serum levels of omentin-1 are increased after weight loss and are particularly associated with increases in obese children with metabolic syndrome. Acta Paediatr. 2017, 106, 1851–1856. [Google Scholar] [CrossRef]
- Wang, L.; Jia, J.; Hong, Z.; Zhang, L.; Zhang, J. Effects of chemerin and homocysteine levels and their associations with occurrence and development of ischemic cerebrovascular disease. Lipids Health Dis. 2021, 20, 108. [Google Scholar] [CrossRef]
- Saeidi, A.; Haghighi, M.M.; Kolahdouzi, S.; Daraei, A.; Abderrahmane, A.B.; Essop, M.F.; Laher, I.; Hackney, A.C.; Zouhal, H. The effects of physical activity on adipokines in individuals with overweight/obesity across the lifespan: A narrative review. Obes. Rev. 2021, 22, e13090. [Google Scholar] [CrossRef]
- Batacan, R.B., Jr.; Duncan, M.J.; Dalbo, V.J.; Tucker, P.S.; Fenning, A.S. Effects of high-intensity interval training on cardiometabolic health: A systematic review and meta-analysis of intervention studies. Br. J. Sports Med. 2017, 51, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Blüher, S.; Käpplinger, J.; Herget, S.; Reichardt, S.; Böttcher, Y.; Grimm, A.; Kratzschd, J.; Petroff, D. Cardiometabolic risk markers, adipocyte fatty acid binding protein (aFABP) and the impact of high-intensity interval training (HIIT) in obese adolescents. Metabolism 2017, 68, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Racil, G.; Ben Ounis, O.; Hammouda, O.; Kallel, A.; Zouhal, H.; Chamari, K.; Amri, M. Effects of high vs. moderate exercise intensity during interval training on lipids and adiponectin levels in obese young females. Eur. J. Appl. Physiol. 2013, 113, 2531–2540. [Google Scholar] [CrossRef] [PubMed]
- Madsen, S.M.; Thorup, A.C.; Bjerre, M.; Jeppesen, P.B. Does 8 weeks of strenuous bicycle exercise improve diabetes-related inflammatory cytokines and free fatty acids in type 2 diabetes patients and individuals at high-risk of metabolic syndrome? Arch. Physiol. Biochem. 2015, 121, 129–138. [Google Scholar] [CrossRef]
- Sim, A.Y.; Wallman, K.E.; Fairchild, T.J.; Guelfi, K.J. Effects of high-intensity intermittent exercise training on appetite regulation. Med. Sci. Sports Exerc. 2015, 47, 2441–2449. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.S.; Yoo, J.H.; So, Y.S. Effect of the low-versus high-intensity exercise training on endoplasmic reticulum stress and GLP-1 in adolescents with type 2 diabetes mellitus. J. Phys. Ther. Sci. 2015, 27, 3063–3068. [Google Scholar] [CrossRef] [Green Version]
- Racil, G.; Coquart, J.B.; Elmontassar, W.; Haddad, M.; Goebel, R.; Chaouachi, A.; Amri, M.; Chamari, K. Greater effects of high- compared with moderate-intensity interval training on cardio-metabolic variables, blood leptin concentration and ratings of perceived exertion in obese adolescent females. Biol. Sport. 2016, 33, 145–152. [Google Scholar] [CrossRef]
- Racil, G.; Zouhal, H.; Elmontassar, W.; Ben Abderrahmane, A.; De Sousa, M.V.; Chamari, K.; Amri, M.; Coquart, J.B. Plyometric exercise combined with high-intensity interval training improves metabolic abnormalities in young obese females more so than interval training alone. Appl. Physiol. Nutr. Metab. 2016, 41, 103–109. [Google Scholar] [CrossRef]
- Gerosa-Neto, J.; Antunes, B.M.; Campos, E.Z.; Rodrigues, J.; Ferrari, G.D.; Rosa Neto, J.C.; Bueno CRJunior Lira, F.S. Impact of long-term high-intensity interval and moderate-intensity continuous training on subclinical inflammation in overweight/obese adults. J. Exerc. Rehabil. 2016, 12, 575–580. [Google Scholar] [CrossRef]
- Mokhtarzade, M.; Ranjbar, R.; Majdinasab, N.; Patel, D.; Molanouri Shamsi, M. Effect of aerobic interval training on serum IL-10, TNFα, and adipokines levels in women with multiple sclerosis: Possible relations with fatigue and quality of life. Endocrine 2017, 57, 262–271. [Google Scholar] [CrossRef]
- Vardar, S.A.; Karaca, A.; Güldiken, S.; Palabıyık, O.; Süt, N.; Demir, A.M. High-intensity interval training acutely alters plasma adipokine levels in young overweight/obese women. Arch. Physiol. Biochem. 2018, 124, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Fealy, C.E.; Nieuwoudt, S.; Foucher, J.A.; Scelsi, A.R.; Malin, S.K.; Pagadala, M.; Cruz, L.A.; Li, M.; Rocco, M.; Burguera, B.; et al. Functional high-intensity exercise training ameliorates insulin resistance and cardiometabolic risk factors in type 2 diabetes. Exp. Physiol. 2018, 103, 985–994. [Google Scholar] [CrossRef] [PubMed]
- Caldeira, R.S.; Panissa, V.L.G.; Inoue, D.S.; Campos, E.Z.; Monteiro, P.A.; Giglio, B.M.; Pimentel, G.D.; Hofmann, P.; Lira, F.S. Impact to short-term high intensity intermittent training on different storages of body fat, leptin, and soluble leptin receptor levels in physically active non-obese men: A pilot investigation. Clin. Nutr. ESPEN 2018, 28, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Taheri Chadorneshin, H.; Cheragh-Birjandi, S.; Goodarzy, S.; Ahmadabadi, F. The impact of high intensity interval training on serum chemerin, tumor necrosis factor-alpha and insulin resistance in overweight women. Obes. Med. 2019, 14, 100101. [Google Scholar] [CrossRef]
- Steckling, F.M.; Farinha, J.B.; Figueiredo, F.D.C.; Santos, D.L.D.; Bresciani, G.; Kretzmann, N.A.; Stefanello, S.T.; Courtes, A.A.; Beck, M.O.; Sangoi Cardoso, M.; et al. High-intensity interval training improves inflammatory and adipokine profiles in postmenopausal women with metabolic syndrome. Arch. Physiol. Biochem. 2019, 125, 85–91. [Google Scholar] [CrossRef]
- Heiston, E.M.; Eichner, N.Z.; Gilbertson, N.M.; Malin, S.K. Exercise improves adiposopathy, insulin sensitivity and metabolic syndrome severity independent of intensity. Exp. Physiol. 2020, 105, 632–640. [Google Scholar] [CrossRef]
- Golestani, F.; Mogharnasi, M.; Erfani-Far, M.; Abtahi-Eivari, S.H. The effects of spirulina under high-intensity interval training on levels of nesfatin-1, omentin-1, and lipid profiles in overweight and obese females: A randomized, controlled, single-blind trial. J. Res. Med. Sci. 2021, 26, 10. [Google Scholar] [CrossRef]
- Aktaş, H.Ş.; Uzun, Y.E.; Kutlu, O.; Pençe, H.H.; Özçelik, F.; Çil, E.Ö.; Irak, L.; Altun, Ö.; Özcan, M.; Özsoy, N.; et al. The effects of high intensity-interval training on vaspin, adiponectin and leptin levels in women with polycystic ovary syndrome. Arch. Physiol. Biochem. 2022, 128, 37–42. [Google Scholar] [CrossRef]
- Kong, Z.; Sun, S.; Liu, M.; Shi, Q. Short-term high-intensity interval training on body composition and blood glucose in overweight and obese young women. J. Diabetes Res. 2016, 2016, 4073618. [Google Scholar] [CrossRef]
- Almenning, I.; Rieber-Mohn, A.; Lundgren, K.M.; SheteligLøvvik, T.; Garnæs, K.K.; Moholdt, T. Effects of high intensity interval training and strength training on metabolic, cardiovascular, and hormonal outcomes in women with polycystic ovary syndrome: A pilot study. PLoS ONE 2015, 10, e0138793. [Google Scholar] [CrossRef] [Green Version]
- Bartlett, D.B.; Shepherd, S.O.; Wilson, O.J.; Adlan, A.M.; Wagenmakers, A.J.M.; Shaw, C.S.; Lord, J.M. Neutrophil and Monocyte Bactericidal Responses to 10 Weeks of Low-Volume High-Intensity Interval or Moderate-Intensity Continuous Training in Sedentary Adults. Oxidative Med. Cell. Longev. 2017, 2017, 8148742. [Google Scholar] [CrossRef] [PubMed]
- Barry, J.C.; Simtchouk, S.; Durrer, C.; Jung, M.E.; Little, J.P. Short-term exercise training alters leukocyte chemokine receptors in obese adults. Med. Sci. Sports Exerc. 2017, 49, 1631–1640. [Google Scholar] [CrossRef] [PubMed]
- Vella, C.A.; Taylor, K.; Drummer, D. High-intensity interval, and moderate-intensity continuous training elicit similar enjoyment and adherence levels in overweight and obese adults. Eur. J. Sport Sci. 2017, 17, 1203–1211. [Google Scholar] [CrossRef] [PubMed]
- Dünnwald, T.; Melmer, A.; Gatterer, H.; Salzmann, K.; Ebenbichler, C.; Burtscher, M.; Schobersberger, W.; Grander, W. Supervised Short-term High-intensity Training on Plasma Irisin Concentrations in Type 2 Diabetic Patients. Int. J. Sports Med. 2019, 40, 158–164. [Google Scholar] [CrossRef]
- Saghebjoo, M.; Farrokhi-Fard, M.; Hedayati, M.; Sadeghi-Tabas, S. The effect of high-intensity interval training and L-arginine supplementation on the serum levels of adiponectin and lipid profile in overweight and obese young men. Obes. Med. 2019, 16, 100139. [Google Scholar] [CrossRef]
- Soltani, N.; Marandi, S.M.; Kazemi, M.; Esmaeil, N. Meta-inflammatory state and insulin resistance can improve after 10 weeks of combined all-extremity high-intensity interval training in sedentary overweight/obese females: A quasi-experimental study. J. Diabetes Metab. Disord. 2020, 19, 717–726. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Durnin, J.V.; Womersley, J. Body fat assessed from total body density and its estimation from skinfold thickness: Measurements on 481 men and women aged from 16 to 72 years. Br. J. Nutr. 1974, 32, 77–97. [Google Scholar] [CrossRef] [Green Version]
- Siri, W.E. Body composition from fluid space and density. In Techniques for Measuring Body Composition; Brozek, J., Hanschel, A., Eds.; National Academy of Science: Washington, DC, USA, 1961; pp. 223–244. [Google Scholar]
- Cazorla, G. Field tests to evaluate aerobic capacity and maximal aerobic speed. In Proceedings of the International Symposium of Guadeloupe, Basse-terre, Guadeloupe, France, 23 November 1990. (In French). [Google Scholar]
- Ouerghi, N.; Ben Fradj, M.K.; Bezrati, I.; Khammassi, M.; Feki, M.; Kaabachi, N.; Bouassida, A. Effects of high-intensity interval training on body composition, aerobic and anaerobic performance, and plasma lipids in overweight/obese and normal-weight young men. Biol. Sport 2017, 34, 385–392. [Google Scholar] [CrossRef]
- Buchan, D.S.; Ollis, S.; Young, J.D.; Cooper, S.M.; Shield, J.P.; Baker, J.S. High intensity interval running enhances measures of physical fitness but not metabolic measures of cardiovascular disease risk in healthy adolescents. BMC Public Health 2013, 13, 498. [Google Scholar] [CrossRef] [Green Version]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nikseresht, M.; Hafezi Ahmadi, M.R.; Hedayati, M. Detraining-induced alterations in adipokines and cardiometabolic risk factors after nonlinear periodized resistance and aerobic interval training in obese men. Appl. Physiol. Nutr. Metab. 2016, 41, 1018–1025. [Google Scholar] [CrossRef] [PubMed]
- Saremi, A.; Asghari, M.; Ghorbani, A. Effects of aerobic training on serum omentin-1 and cardiometabolic risk factors in overweight and obese men. J. Sports Sci. 2010, 28, 993–998. [Google Scholar] [CrossRef] [PubMed]
- Wilms, B.; Ernst, B.; Gerig, R.; Schultes, B. Plasma omentin-1 levels are related to exercise performance in obese women and increase upon aerobic endurance training. Exp. Clin. Endocrinol. Diabetes 2015, 123, 187–192. [Google Scholar] [CrossRef] [PubMed]
- AminiLari, Z.; Fararouei, M.; Amanat, S.; Sinaei, E.; Dianatinasab, S.; AminiLari, M.; Daneshi, N.; Dianatinasab, M. The effect of 12 weeks aerobic, resistance, and combined exercises on omentin-1 levels and insulin resistance among type 2 diabetic middle-aged women. Diabetes Metab. J. 2017, 41, 205–212. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Tian, Y.; Valenzuela, P.L.; Huang, C.; Zhao, J.; Hong, P.; He, Z.; Yin, S.; Lucia, A. Myokine/adipokine response to “aerobic” exercise: Is it just a matter of exercise load? Front. Physiol. 2019, 10, 691. [Google Scholar] [CrossRef]
- Faramarzi, M.; Banitalebi, E.; Nori, S.; Farzin, S.; Taghavian, Z. Effects of rhythmic aerobic exercise plus core stability training on serum omentin, chemerin and vaspin levels and insulin resistance of overweight women. J. Sports Med. Phys. Fit. 2016, 56, 476–482. [Google Scholar] [PubMed]
- Verheggen, R.J.; Poelkens, F.; Roerink, S.H.; Ramakers, R.E.; Catoire, M.; Hermus, A.R.; Thijssen, D.H.; Hopman, M.T. Exercise improves insulin sensitivity in the absence of changes in cytokines. Med. Sci. Sports Exerc. 2016, 48, 2378–2386. [Google Scholar] [CrossRef] [Green Version]
- Watanabe, T.; Watanabe-Kominato, K.; Takahashi, Y.; Kojima, M.; Watanabe, R. Adipose tissue-derived omentin-1 function and regulation. Compr. Physiol. 2017, 7, 765–781. [Google Scholar] [CrossRef]
- Moreno-Navarrete, J.M.; Catalán, V.; Ortega, F.; Gómez-Ambrosi, J.; Ricart, W.; Frühbeck, G.; Fernández-Real, J.M. Circulating omentin concentration increases after weight loss. Nutr. Metab. 2010, 7, 27. [Google Scholar] [CrossRef] [Green Version]
- De Castro, C.A.; da Silva, K.A.; Rocha, M.C.; Sene-Fiorese, M.; Nonaka, K.O.; Malavazi, I.; Anibal, F.F.; Duarte, A.C.G.O. Exercise and omentin: Their role in the crosstalk between muscle and adipose tissues in type 2 diabetes mellitus rat models. Front. Physiol. 2019, 9, 1881. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zhu, L.; Zheng, M.; Fan, C.; Li, Y.; Zhang, D.; He, Y.; Yang, H. Changes of serum omentin-1 levels in normal subjects, type 2 diabetes, and type 2 diabetes with overweight and obesity in Chinese adults. Ann. Endocrinol. 2014, 75, 171–175. [Google Scholar] [CrossRef]
- Kelly, B.M.; Xenophontos, S.; King, J.A.; Nimmo, M.A. An evaluation of low volume high-intensity intermittent training (HIIT) for health risk reduction in overweight and obese men. BMC Obes. 2017, 4, 17. [Google Scholar] [CrossRef] [Green Version]
- Leggate, M.; Carter, W.G.; Evans, M.J.; Vennard, R.A.; Sribala-Sundaram, S.; Nimmo, M.A. Determination of inflammatory and prominent proteomic changes in plasma and adipose tissue after high-intensity intermittent training in overweight and obese males. J. Appl. Physiol. 2012, 112, 1353–1360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boyd, J.C.; Simpson, C.A.; Jung, M.E.; Gurd, B.J. Reducing the intensity and volume of interval training diminishes cardiovascular adaptation but not mitochondrial biogenesis in overweight/obese men. PLoS ONE 2013, 8, e68091. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sirico, F.; Bianco, A.; D’Alicandro, G.; Castaldo, C.; Montagnani, S.; Spera, R.; Di Meglio, F.; Nurzynska, D. Effects of physical exercise on adiponectin, leptin, and inflammatory markers in childhood obesity: Systematic review and meta-analysis. Child. Obes. 2018, 14, 207–217. [Google Scholar] [CrossRef] [Green Version]
- Aghapour, A.; Farzanegi, P. Effect of six-week aerobic exercise on chemerin and resistin concentration in hypertensive postmenopausal women. Electron. Physician 2013, 5, 623–630. [Google Scholar] [CrossRef]
- Bozaoglu, K.; Bolton, K.; McMillan, J.; Zimmet, P.; Jowett, J.; Collier, G.; Walder, K.; Segal, D. Chemerin is a novel adipokine associated with obesity and metabolic syndrome. Endocrinology 2007, 148, 4687–4694. [Google Scholar] [CrossRef]
- Alfadda, A.A.; Sallam, R.M.; Chishti, M.A.; Moustafa, A.S.; Fatma, S.; Alomaim, W.S.; Al-Naami, M.Y.; Bassas, A.F.; Chrousos, G.P.; Jo, H. Differential patterns of serum concentration and adipose tissue expression of chemerin in obesity: Adipose depot specificity and gender dimorphism. Mol. Cells 2012, 33, 591–596. [Google Scholar] [CrossRef] [Green Version]
| Normal-Weight Group (n = 9) | Excess-Weight Group (n = 9) | Interaction (Time × Group) a | ||||
|---|---|---|---|---|---|---|
| Pre-HIIT | Post-HIIT | Pre-HIIT | Post-HIIT | F | ηp2 | |
| Age, years | 18.1 ± 0.93 | 18.3 ± 1.22 | ||||
| Body mass, kg | 62.6 ± 4.61 | 62.5 ± 4.90 | 93.7 ± 16.9 ### | 92.0 ± 15.9 * | 5.96 † | 0.271 |
| Body mass index, kg/m2 | 20.5 ± 1.51 | 20.5 ± 1.67 | 30.8 ± 4.56 ### | 30.3 ± 4.25 * | 6.24 † | 0.280 |
| Body fat, % | 12.0 ± 3.28 | 11.9 ± 3.10 | 22.5 ± 1.87 ### | 22.1 ± 1.82 * | 2.17 | 0.119 |
| MAV, km/h | 14.9 ± 0.53 | 15.4 ± 0.74 ** | 11.5 ± 1.15 ### | 12.1 ± 0.96 ** | 0.64 | 0.039 |
| VO2max, mL/kg/min | 54.1 ± 1.84 | 55.6 ± 2.58 ** | 42.0 ± 4.03 ### | 44.2 ± 3.37 ** | 0.58 | 0.035 |
| Heart rate max, beat/min | 190 ± 10.0 | 189 ± 10.2 | 193 ± 8.65 | 192 ± 7.58 | 0.03 | 0.002 |
| Total cholesterol, mg/dL | 136 ± 20.0 | 127 ± 19.8 | 171 ± 36.2 ### | 150 ± 15.0 * | 2.39 | 0.130 |
| Triglycerides, mg/dL | 81.6 ± 30.9 | 68.4 ± 16.1 | 122 ± 39.3 ### | 89.7 ± 21.4 * | 1.25 | 0.072 |
| HOMA-IR | 1.87 ± 1.43 | 1.26 ± 0.51 | 4.99 ± 2.62 ## | 3.12 ± 1.47 * | 1.96 | 0.108 |
| C-reactive protein, mg/L | 0.85 ± 0.67 | 1.27 ± 1.42 | 2.78 ± 1.57 ## | 2.97 ± 1.77 | 0.98 | 0.006 |
| Leptin, ng/mL | 2.05 ± 1.09 | 2.23 ± 1.54 | 8.78 ± 5.96 ## | 8.62 ± 5.84 | 0.47 | 0.028 |
| Chemerin, ng/mL | 103 ± 37.9 | 106 ± 41.9 | 172 ± 39.6 ## | 162 ± 43.5 | 0.38 | 0.023 |
| Adiponectin, ng/mL | 14.2 ± 4.23 | 13.4 ± 3.61 | 8.96 ± 3.21 ## | 9.10 ± 3.28 | 0.30 | 0.018 |
| Omentin-1, ng/mL | 470 ± 114 | 572 ± 115 ** | 359 ± 138 # | 455 ± 126 ** | 0.27 | 0.020 |
| BMI | BF | TC | TG | CRP | HOMA-IR | ||
|---|---|---|---|---|---|---|---|
| Leptin | Pre Post | 0.874 *** 0.848 *** | 0.687 ** 0.673 *** | 0.702 *** 0.651 ** | 0.805 *** 0.634 *** | 0.767 *** 0.599 ** | 0.619 ** 0.860 *** |
| Chemerin | Pre Post | 0.782 *** 0.573 * | 0.767 *** 0.684 ** | 0.687 ** 0.244 | 0.775 *** 0.562 * | 0.766 *** 0.591 ** | 0.674 ** 0.555 * |
| Adiponectin | Pre Post | −0.582 * −0.547 * | −0.448 −0.563 * | −0.379 −0.454 | −0.590 −0.480 * | −0.564 * −0.681 ** | −0.369 −0.415 |
| Omentin-1 | Pre Post | −0.552 * −0.547 * | −0.585 * −0.563 * | −0.531 * −0.369 | −0.385 −0.523* | −0.411 −0.263 | −0.409 −0.268 |
| ∆ BMI | ∆ BF | ∆ TC | ∆ TG | ∆ CRP | ∆ HOMA-IR | ||
| ∆ Leptin | −0.345 | −0.331 | 0.389 | 0.386 | 0.038 | 0.037 | |
| ∆ Chemerin | 0.133 | -0.203 | 0.271 | 0.585 ** | 0.269 | −0.010 | |
| ∆ Adiponectin | −0.247 | 0.209 | −0.196 | −0.545 * | −0.561 * | −0.192 | |
| ∆ Omentin-1 | 0.088 | 0.294 | −0.094 | −0.424 | 0.025 | 0.231 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ouerghi, N.; Fradj, M.K.B.; Duclos, M.; Bouassida, A.; Feki, M.; Weiss, K.; Knechtle, B. Effects of High-Intensity Interval Training on Selected Adipokines and Cardiometabolic Risk Markers in Normal-Weight and Overweight/Obese Young Males—A Pre-Post Test Trial. Biology 2022, 11, 853. https://doi.org/10.3390/biology11060853
Ouerghi N, Fradj MKB, Duclos M, Bouassida A, Feki M, Weiss K, Knechtle B. Effects of High-Intensity Interval Training on Selected Adipokines and Cardiometabolic Risk Markers in Normal-Weight and Overweight/Obese Young Males—A Pre-Post Test Trial. Biology. 2022; 11(6):853. https://doi.org/10.3390/biology11060853
Chicago/Turabian StyleOuerghi, Nejmeddine, Mohamed Kacem Ben Fradj, Martine Duclos, Anissa Bouassida, Moncef Feki, Katja Weiss, and Beat Knechtle. 2022. "Effects of High-Intensity Interval Training on Selected Adipokines and Cardiometabolic Risk Markers in Normal-Weight and Overweight/Obese Young Males—A Pre-Post Test Trial" Biology 11, no. 6: 853. https://doi.org/10.3390/biology11060853








