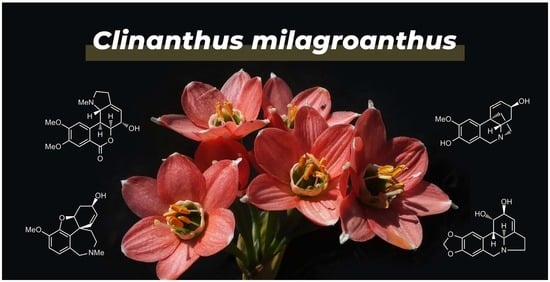
Antileishmanial Activity of Clinanthus milagroanthus S. Leiva & Meerow (Amaryllidaceae) Collected in Peru
Abstract
:1. Introduction
2. Results and Discussion
2.1. Alkaloid Profiling
2.2. In Vitro Antileishmanial Activity
2.3. In Vivo Antileishmanial Activity
2.4. Molecular Docking In Silico Analysis
3. Materials and Methods
3.1. Plant Material
3.2. Extraction
3.3. GC-MS Analysis
3.4. Alkaloid Identification and Quantification
3.5. Parasite Culture
3.6. In Vitro Assay
3.7. In Vivo Assay
3.7.1. Animal
3.7.2. Infection and Treatment of Animals
3.8. Statistical Analysis
3.9. In Silico Assay—Homology Modeling
3.10. In Silico Assay—Molecular Docking
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mannan, S.; Elhadad, H.; Loc, T.; Sadik, M.; Mohamed, M.; Nami, N.; Thuong, N.; Trong, B.; Duc, N.T.M.; Hoang, A.N. Prevalence and associated factors of asymptomatic leishmaniasis: A systematic review and meta-analysis. Int. J. Parasitol. 2021, 81, 102229. [Google Scholar] [CrossRef]
- Veasey, J.; Zampieri, R.; Lellis, R.; Freitas, T.; Winter, L. Identification of Leishmania species by high-resolution DNA dissociation in cases of American cutaneous leishmaniasis. An. Bras. Dermatol. 2020, 95, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Valero, N.; Uriarte, N. Environmental and socioeconomic risk factors associated with visceral and cutaneous leishmaniasis: A systematic review. Parasitol Res. 2020, 119, 365–384. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization—Leishmaniosis. Available online: https://www.who.int/news-room/fact-sheets/detail/leishmaniasis (accessed on 20 May 2022).
- Abdrrahman, S.; Surur, A.; Fekadu, A.; Makonnen, E.; Hailu, A. Challenges and Opportunities for Drug Discovery in Developing Countries: The Example of Cutaneous Leishmaniasis. ACS Med. Chem. Lett. 2020, 11, 2058–2062. [Google Scholar] [CrossRef]
- Newman, D.; Cragg, G.M. Natural products as sources of new drugs over the nearly four decades from 01/1981 to 09/2019. J. Nat. Prod. 2020, 83, 770–803. [Google Scholar] [CrossRef] [Green Version]
- Berkov, S.; Osorio, E.; Viladomat, F.; Bastida, J. Chemodiversity, chemotaxonomy and chemoecology of Amaryllidaceae alkaloids. In The Alkaloids: Chemistry and Biology; Knölker, H.-J., Ed.; Elsevier: Amsterdam, The Netherlands, 2020; Volume 83, pp. 113–185. [Google Scholar] [CrossRef]
- Evidente, A.; Kireev, S.; Jenkins, A.; Romero, A.; Steelant, W.; Van, S.; Kornienko, A. Biological evaluation of structurally diverse Amaryllidaceae alkaloids and their synthetic derivatives: Discovery of novel leads for anticancer drug design. Planta Med. 2009, 75, 501–507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bastida, J.; Lavilla, R.; Viladomat, F. Chemical and biological aspects of Narcissus alkaloids. In The Alkaloids: Chemistry and Physiology; Cordell, G.A., Ed.; Elsevier: Amsterdam, The Netherlands, 2006; Volume 63, pp. 87–179. [Google Scholar] [CrossRef]
- Leiva, S.; Meerow, A.W. A new species of Clinanthus from northern Peru (Asparagales, Amaryllidaceae, Amarylloideae, Clinantheae). PhytoKeys 2016, 63, 99–106. [Google Scholar] [CrossRef] [Green Version]
- León, B.; Sagástegui, A.; Sánchez, I.; Zapata, M.; Meerow, A. Amaryllidaceae endémicas del Perú. Rev. Peru. Biol. 2006, 13, 690–697. [Google Scholar] [CrossRef]
- Schnoes, H.K.; Smith, D.H.; Burlingame, A.L.; Jeffs, P.W.; Doepke, W. High resolution mass spectrometry in molecular structure studies. IX. Mass spectra of Amaryllidaceae alkaloids. Lycorenine series. Tetrahedron 1968, 24, 2825–2837. [Google Scholar] [CrossRef]
- Ortiz, J.E.; Pigni, N.B.; Andujar, S.A.; Roitman, G.; Suvire, F.D.; Enriz, R.D.; Tapia, A.; Bastida, J.; Feresin, G.E. Alkaloids from Hippeastrum argentinum and their cholinesterase-inhibitory activities: An in vitro and in silico study. J. Nat. Prod. 2016, 79, 1241–1248. [Google Scholar] [CrossRef] [PubMed]
- Soto-Vásquez, M.R.; Horna-Pinedo, M.V.; Tallini, L.R.; Bastida, J. Chemical Composition and In Vitro Antiplasmodial Activity of the Total Alkaloids of the Bulbs of Two Amaryllidaceae Species from Northern Peru. Pharmacogn. J. 2021, 13, 1046–1052. [Google Scholar] [CrossRef]
- Adessi, T.G.; Borioni, J.L.; Pigni, N.B.; Bastida, J.; Cavallaro, V.; Murray, A.P.; Puiatti, M.; Oberti, J.C.; Segundo, L.; Nicotra, V.E.; et al. Clinanthus microstephium, an Amaryllidaceae Species with Cholinesterase Inhibitor Alkaloids: Structure-Activity Analysis of Haemanthamine Skeleton Derivatives. Chem. Biodivers. 2019, 16, 1800662. [Google Scholar] [CrossRef] [PubMed]
- Kaya, G.I.; Polat, D.C.; Sarikaya, B.; Onur, M.A.; Somer, N.U. Quantititative determination of lycorine and galanthamine in Galanthus trojanus and G. cilicicus by HPLC-DAD. Nat. Prod. Commun. 2014, 9, 115. [Google Scholar] [CrossRef] [Green Version]
- Kaya, G.I.; Cicek, D.; Sarikaya, B.; Onur, M.A.; Somer, N.U. HPLC-DAD analysis of lycorine in Amaryllidaceae species. Nat. Prod. Commun. 2010, 5, 873–876. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huaylla, H.; Llalla, O.; Torras-Claveria, L.; Bastida, J. Alkaloid profile in Pyrolirion albicans Herb. (Amaryllidaceae), a Peruvian endemic species. S. Afr. J. Bot. 2021, 136, 76–80. [Google Scholar] [CrossRef]
- Ahmet, E.; Ceren, E.; Buket, B.; Mustafa, A.; Nehir, U.; Gulen, I. Application of HPLC-DAD for the quantification of Lycorine in Galanthus elwesii Hook. Braz. J. Pharm. Sci. 2017, 53, 15063–15069. [Google Scholar] [CrossRef] [Green Version]
- Roy, M.; Liang, L.; Xiao, X.; Feng, P.; Ye, M.; Liu, J. Lycorine: A prospective natural lead for anticancer drug discovery. Biomed. Pharmacother. 2018, 107, 615–624. [Google Scholar] [CrossRef]
- Nair, J.J.; van Staden, J. Antiprotozoal alkaloid principles of the plant family Amaryllidaceae. Bioorg. Med. Chem. Lett. 2019, 29, 12664. [Google Scholar] [CrossRef]
- Osorio, E.D.; Berkov, S.; Brun, R.; Codina, C.; Viladomat, F.; Cabezas, F.; Bastida, J. In vitro antiprotozoal activity of alkaloids from Phaedranassa dubia (Amaryllidaceae). Phytochem. Lett. 2010, 3, 161–163. [Google Scholar] [CrossRef]
- Tallini, L.R.; de Andrade, J.P.; Kaiser, M.; Viladomat, F.; Nair, J.J.; Zuanazzi, J.A.S.; Bastida, J. Alkaloid constituents of the Amaryllidaceae plant Amaryllis belladonna L. Molecules 2017, 22, 1437. [Google Scholar] [CrossRef] [Green Version]
- Labraña, L.; Machocho, A.K.; Kricsfalusy, V.; Brun, R.; Codina, C.; Viladomat, F.; Bastida, J. Alkaloids from Narcissus angustifolius subsp. transcarpathicus (Amaryllidaceae). Phytochemistry 2002, 60, 847–852. [Google Scholar] [CrossRef]
- Kaya, G.I.; Sarikaya, B.; Onur, M.A.; Somer, N.U.; Viladomat, F.; Codina, C.; Bastida, J.; Lauinger, I.L.; Kaiser, M.; Tasdemir, D. Antiprotozoal alkaloids from Galanthus trojanus. Phytochem. Lett. 2011, 4, 301–305. [Google Scholar] [CrossRef]
- Tallini, L.R.; Torras-Claveria, L.; de Borges, S.W.; Kaiser, M.; Viladomat, F.; Zuanazzi, J.A.S.; Bastida, J. N-oxide alkaloids from Crinum amabile (Amaryllidaceae). Molecules 2018, 23, 127. [Google Scholar] [CrossRef] [Green Version]
- Machocho, A.; Chhabra, S.C.; Viladomat, F.; Codina, C.; Bastida, J. Alkaloids from Crinum stuhlmannii. Planta Med. 1998, 64, 679–680. [Google Scholar] [CrossRef] [PubMed]
- Nair, J.J.; Machocho, A.K.; Campbell, W.E.; Brun, R.; Viladomat, F.; Codina, C.; Bastida, J. Alkaloids from Crinum macowanii. Phytochemistry 2000, 54, 945–950. [Google Scholar] [CrossRef]
- Herrera, M.R.; Machocho, A.K.; Brun, R.; Viladomat, F.; Codina, C.; Bastida, J. Crinane and lycorane type alkaloids from Zephyranthes citrina. Planta Med. 2001, 67, 191–193. [Google Scholar] [CrossRef] [PubMed]
- Osorio, E.; Robledo, S.; Bastida, J. Alkaloids with antiprotozoal activity. In The Alkaloids Chemistry and Biology; Cordell, G.A., Ed.; Elsevier: Amsterdam, The Netherlands, 2008; Volume 66, pp. 113–190. [Google Scholar]
- Ponte-Sucre, A.; Faber, J.H.; Gulder, T.; Kajahn, I.; Pedersen, S.E.H.; Schultheis, M.; Bringmann, G.; Moll, H. Activities of Naphthylisoquinoline Alkaloids and Synthetic Analogs against Leishmania major. Antimicrob. Agents Chemother. 2007, 51, 188–194. [Google Scholar] [CrossRef] [Green Version]
- Tempone, A.G.; Treiger, S.E.; de Andrade, H.F.; de Amorin, G.; Yogi, A.; Salerno, C.; Bachiega, D.; Lupo, N.C.; Bonotto, S.V.; Fischer, D.C.H. Antiprotozoal activity of Brazilian plant extracts from isoquinoline alkaloid-producing families. Phytomedicine 2005, 12, 382–390. [Google Scholar] [CrossRef] [PubMed]
- Ponte-Sucre, A.; Vicik, R.; Schultheis, M.; Schirmeister, T.; Moll, H. Aziridine-2,3-dicarboxylates: Peptidomimetic cysteine protease inhibitors with antileishmanial activity. Antimicrob. Agents Chemother. 2006, 50, 2439–2447. [Google Scholar] [CrossRef] [Green Version]
- Da Silva, M.A.; Fokoue, H.H.; Fialho, S.N.; de A. dos Santos, A.P.; Rossi, N.R.D.L.P.; de J. Gouveia, A.; Ferreira, A.S.; Passarini, G.M.; Garay, A.F.G.; Alfonso, J.J.; et al. Antileishmanial activity evaluation of a natural amide and its synthetic analogs against Leishmania (V.) braziliensis: An integrated approach in vitro and in silico. Parasitol. Res. 2021, 120, 2199–2218. [Google Scholar] [CrossRef]
- Colotti, G.; Baiocco, P.; Fiorillo, A.; Boffi, A.; Poser, E.; Di Chiaro, F.; Ilari, A. Structural insights into the enzymes of the trypanothione pathway: Targets for antileishmaniasis drugs. Future Med. Chem. 2013, 5, 1861–1875. [Google Scholar] [CrossRef] [PubMed]
- Battista, T.; Colotti, G.; Ilari, A.; Fiorillo, A. Targeting Trypanothione Reductase, a Key Enzyme in the Redox Trypanosomatid Metabolism, to Develop New Drugs against Leishmaniasis and Trypanosomiases. Molecules 2020, 25, 1924. [Google Scholar] [CrossRef] [Green Version]
- Bodade, R.G.; Beedkar, S.D.; Manwar, A.V.; Khobragade, C.N. Homology modeling and docking study of xanthine oxidase of Arthrobacter sp. XL26. Int. J. Biol. Macromol. 2010, 47, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Baiocco, P.; Colotti, G.; Franceschini, S.; Ilari, A. Molecular basis of antimony treatment in Leishmaniasis. J. Med. Chem. 2009, 52, 2603–2612. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, G.N.; Ramakrishnan, C.; Sasisekharan, V. Stereochemistry of polypeptide chain configurations. J. Mol. Biol. 1963, 7, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Laskowski, R.A.; MacArthur, M.W.; Moss, D.S.; Thornton, J.M. PROCHECK: A program to check the stereochemical quality of protein structures. J. Appl. Crystallogr. 1993, 26, 283–291. [Google Scholar] [CrossRef]
- Bond, C.S.; Zhang, Y.; Berriman, M.; Cunningham, M.L.; Fairlamb, A.H.; Hunter, W.N. Crystal structure of Trypanosoma cruzi trypanothione reductase in complex with trypanothione, and the structure-based discovery of new natural product inhibitors. Structure 1999, 7, 81–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saccoliti, F.; Angiulli, G.; Pupo, G.; Pescatori, L.; Madia, V.N.; Messore, A.; Colotti, G.; Fiorillo, A.; Scipione, L.; Gramiccia, M.; et al. Inhibition of Leishmania infantum trypanothione reductase by diaryl sulfide derivatives. J. Enzym. Inhib. Med. Chem. 2017, 32, 304–310. [Google Scholar] [CrossRef]
- Meerow, A.W.; Nakamura, K. Two new species of Peruvian Amaryllidaceae, an expanded concept of the genus Paramongaia, and taxonomic notes in Stenomesson. Phytotaxa 2019, 416, 184–196. [Google Scholar] [CrossRef]
- Soto-Vásquez, M.R.; Rodríguez-Muñoz, C.A.; Tallini, L.R.; Bastida, J. Alkaloid Composition and Biological Activities of the Amaryllidaceae Species Ismene amancaes (Ker Gawl.) Herb. Plants 2022, 11, 1906. [Google Scholar] [CrossRef]
- Antwi, C.A.; Amisigo, C.M.; Adjimani, J.P.; Gwira, T.M. In vitro activity and mode of action of phenolic compounds on Leishmania donovani. PLoS Negl. Trop. Dis. 2019, 13, e0007206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, S.; Mohapatra, D.P.; Sivakumar, R. Successful replacement of fetal calf serum with human urine for in vitro culture of Leishmania donovani. J. Commun. Dis. 2000, 32, 289–294. [Google Scholar]
- Mosmann, T. Rapid colorimetric assay for cellular growth and survival: Application to proliferation and cytotoxicity assays. J. Immunol. Methods 1983, 65, 55–63. [Google Scholar] [CrossRef]
- Comandolli-Wyrepkowski, C.D.; Grafova, I.; Naiff, M.F.; Avella, M.; Gentile, G.; Grafov, A.; Franco, A.M.R. Topical treatment of experimental cutaneous leishmaniasis in golden hamster (Mesocricetus auratus) with formulations containing pentamidine. Acta Amaz. 2017, 47, 39–46. [Google Scholar] [CrossRef] [Green Version]
- Varela, -M.R.E.; Villa-Pulgarin, J.A.; Yepes, E.; Müller, I.; Modolell, M.; Muñoz, D.L.; Robledo, S.M.; Muskus, C.E.; López-Abán, J.; Muro, A.; et al. In vitro and in vivo efficacy of ether lipid edelfosine against Leishmania spp. and SbV-resistant parasites. PLoS Negl. Trop. Dis. 2012, 6, 1612. [Google Scholar] [CrossRef] [Green Version]
- Robledo, S.M.; Carrillo, L.M.; Daza, A.; Restrepo, A.M.; Muñoz, D.L.; Tobón, J.; Murillo, J.D.; López, A.; Ríos, C.; Mesa, C.V.; et al. Cutaneous Leishmaniasis in the Dorsal Skin of Hamsters: A Useful Model for the Screening of Antileishmanial Drugs. J. Vis. Exp. 2012, 62, 3533. [Google Scholar] [CrossRef]
- Altschul, S.F.; Gish, W.; Miller, W.; Myers, E.W.; Lipman, D.J. Basci local alignment search tool. J. Mol. Biol. 1990, 215, 403–410. [Google Scholar] [CrossRef] [PubMed]
- Šali, A.; Blundell, T.L. Comparative protein modelling by satisfaction of spatial restraints. J. Mol. Biol. 1993, 234, 779–815. [Google Scholar] [CrossRef] [PubMed]
- Pettersen, E.F.; Goddard, T.D.; Huang, C.C.; Couch, G.S.; Greenblatt, D.M.; Meng, E.C.; Ferrin, T.E. UCSF Chimera—A visualization system for exploratory research and analysis. J. Comput. Chem. 2004, 25, 1605–1612. [Google Scholar] [CrossRef]
- Morris, G.M.; Huey, R.; Lindstrom, W.; Sanner, M.F.; Belew, R.K.; Goodsell, D.S.; Olson, A.J. AutoDock4 and AutoDockTools4: Automated docking with selective receptor flexibility. J. Comput. Chem. 2009, 30, 2785–2791. [Google Scholar] [CrossRef] [Green Version]
- Dallakyan, S.; Olson, A.J. Small-molecule library screening by docking with PyRx. Methods Mol. Biol. 2015, 1263, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Morris, G.M.; Goodsell, D.S.; Halliday, R.S.; Huey, R.; Hart, W.E.; Belew, R.K.; Olson, A.J. Automated docking using a Lamarckinan genetic algorithm and an empirical binding free energy function. J. Comput. Chem. 1999, 19, 1639–1662. [Google Scholar] [CrossRef]
- Schrödinger Release 2022-3: Maestro; Schrödinger, LLC.: New York, NY, USA, 2021.





| Alkaloid | [M+] | MS | RI 1 | Values | TIC (%) 2 |
|---|---|---|---|---|---|
| galanthamine (1) | 287 (87) | 286(100), 270 (15), 216 (26), 174 (23) | 2429.6 | 6.8 | 0.5 |
| vittatine/crinine (2a/2b) | 271 (100) | 228 (19), 199 (48), 187 (41), 115 (13) | 2510.8 | 6.0 | 0.3 |
| 8-O-demethylmaritidine (3) | 273 (100) | 244 (14), 230 (19), 201 (62), 189 (44) | 2537.5 | 6.1 | 0.4 |
| anhydrolycorine (4) | 251 (48) | 250 (100), 192 (11) | 2542.9 | 12.1 | 1.6 |
| 11,12-dehydroanhydrolycorine (5) | 249 (67) | 248 (100), 190 (15) | 2645.1 | 8.0 | 0.6 |
| hippamine (6) | 301 (20) | 268 (14), 250 (18), 227 (92), 226 (100) | 2706.0 | 6.2 | 0.4 |
| lycorine (7) | 287 (39) | 268 (29), 250 (16), 227 (76), 226 (100) | 2817.3 | 191.2 | 28.5 |
| 2-hydroxyanhydrolycorine 3 (8) | 267 (56) | 266 (100), 208 (9), 132 (6) | 2893.5 | 49.3 | 9.7 |
| 7-hydroxyclivonine 3 (9) | 333 (57) | 96 (56), 83 (100), 82 (31) | 2963.2 | 23.5 | 4.6 |
| 2α-hydroxyhomolycorine (10) | 331 (<1) | 125 (100), 96 (25) | 3000.9 | 10.3 | 1.6 |
| 7-hydroxyclivonine isomer 3 (11) | 333 (64) | 96 (81), 83 (100), 82 (32) | 3017.2 | 56.2 | 12.0 |
| Alkaloids | Estimated Free Energy of Binding |
|---|---|
| galanthamine (1) | −8.29 |
| vittatine (2a) | −7.01 |
| crinine (2b) | −8.14 |
| 8-O-demethylmaritidine (3) | −6.88 |
| anhydrolycorine (4) | −7.20 |
| 11,12-dehydroanhydrolycorine (5) | −7.05 |
| hippamine (6) | −7.60 |
| lycorine (7) | −7.69 |
| 2-hydroxyanhydrolycorine (8) | −7.04 |
| 7-hydroxyclivonine (9) | −7.76 |
| 2α-hydroxyhomolycorine (10) | −7.73 |
| 7-hydroxyclivonine isomer (11) | −8.24 |
| amphotericin B (positive control) | −7.94 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soto-Vásquez, M.R.; Alvarado-García, P.A.A.; Osorio, E.H.; Tallini, L.R.; Bastida, J. Antileishmanial Activity of Clinanthus milagroanthus S. Leiva & Meerow (Amaryllidaceae) Collected in Peru. Plants 2023, 12, 322. https://doi.org/10.3390/plants12020322
Soto-Vásquez MR, Alvarado-García PAA, Osorio EH, Tallini LR, Bastida J. Antileishmanial Activity of Clinanthus milagroanthus S. Leiva & Meerow (Amaryllidaceae) Collected in Peru. Plants. 2023; 12(2):322. https://doi.org/10.3390/plants12020322
Chicago/Turabian StyleSoto-Vásquez, Marilú Roxana, Paul Alan Arkin Alvarado-García, Edison H. Osorio, Luciana R. Tallini, and Jaume Bastida. 2023. "Antileishmanial Activity of Clinanthus milagroanthus S. Leiva & Meerow (Amaryllidaceae) Collected in Peru" Plants 12, no. 2: 322. https://doi.org/10.3390/plants12020322