Latin American Plants against Microorganisms
Abstract
:1. Introduction
2. Plant Antimicrobials
2.1. Antimicrobial Resistance
2.2. Natural Products and Plant Extracts with Antimicrobial Activity against MDR Strains
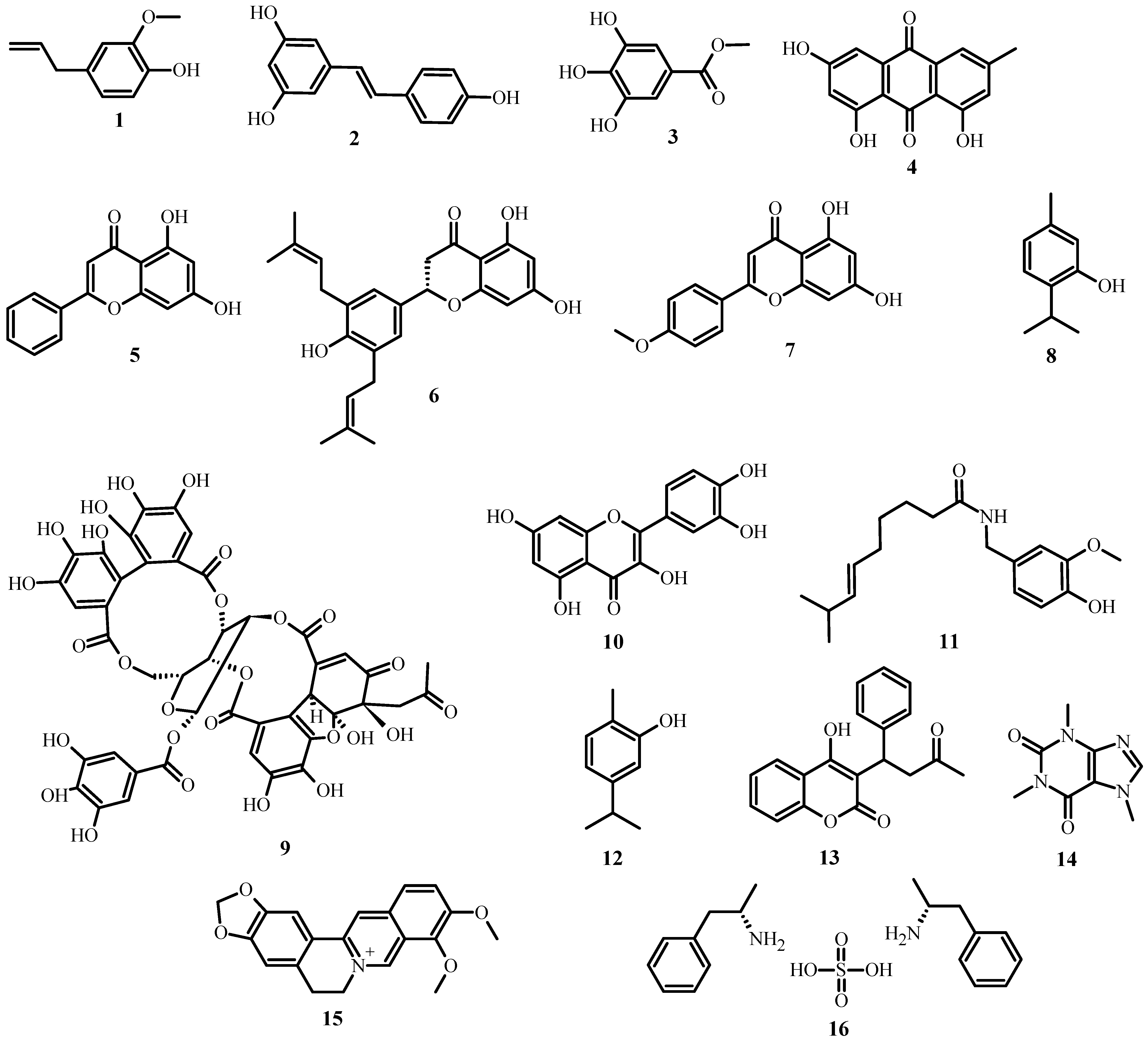
| Class | Subclass | Examples | Source of the Compound | Mechanism | References |
|---|---|---|---|---|---|
| Phenolics | Simple phenols | Eugenol (1) | Syzygium aromaticum | Membrane disruption. | [22,23] |
| Resveratrol (2) | Vitis vinifera | Binds reversibly to ATP synthase. | [22,24] | ||
| Phenolic acids | Methyl gallate (3) | Euphorbia hyssopifolia | Inhibits DNA gyrase or ATPase. | [22,25] | |
| Quinones | Emodin (4) | Rheum rhabarbarum | Destroys the integrity of the cell wall and cell membrane. | [22,26] | |
| Flavonoids | Chrysin (5) | Passiflora caerulea | Binds to adhesins. | [27,28] | |
| Flavones | Abyssinone V (6) | Erythrina abyssinica | Complexes with the cell wall, inactivate enzymes and inhibit HIV reverse transcriptase. | [27] | |
| Acacetin (7) | Robinia pseudoacacia | - | [22] | ||
| Flavonols | Quercetin (10) | Brickellia cavanillesii | Disrupts bacterial cell walls and cell membranes, disrupt nucleic acid synthesis, inhibit biofilm formation, and reduce expression of virulence factors. | [28,29] | |
| Tannins | Ellagitannin (9) | Punica granatum | Binds to proteins, bind to adhesins, enzyme inhibition, substrate deprivation, complex with the cell wall, membrane disruption, metal ion complexation. | [27] | |
| Coumarins | Warfarin (13) | Melilotus officinalis | Interacts with eukaryotic DNA (antiviral activity). | [27] | |
| Terpenoids | Capsaicin (11) | Capsicum annuum | Membrane disruption. | [27] | |
| Carvacrol (12) | Xylopia aromatica | Membrane disruption. | [22,30] | ||
| Thymol (8) | Induces the permeability and depolarization of the cytoplasmic membrane. | [22,31] | |||
| Alkaloids | Caffeine (14) | Coffea arabica | Inhibits biofilm development. | [22,32] | |
| Berberine (15) | Argemone mexicana | Damages bacterial cells by destroying cellular proteins. | [22,33] | ||
| Lectins and polypeptides | Fabatin (16) | Vicia faba | Blocks viral fusion or adsorption and forms disulfide bridges. | [27] |
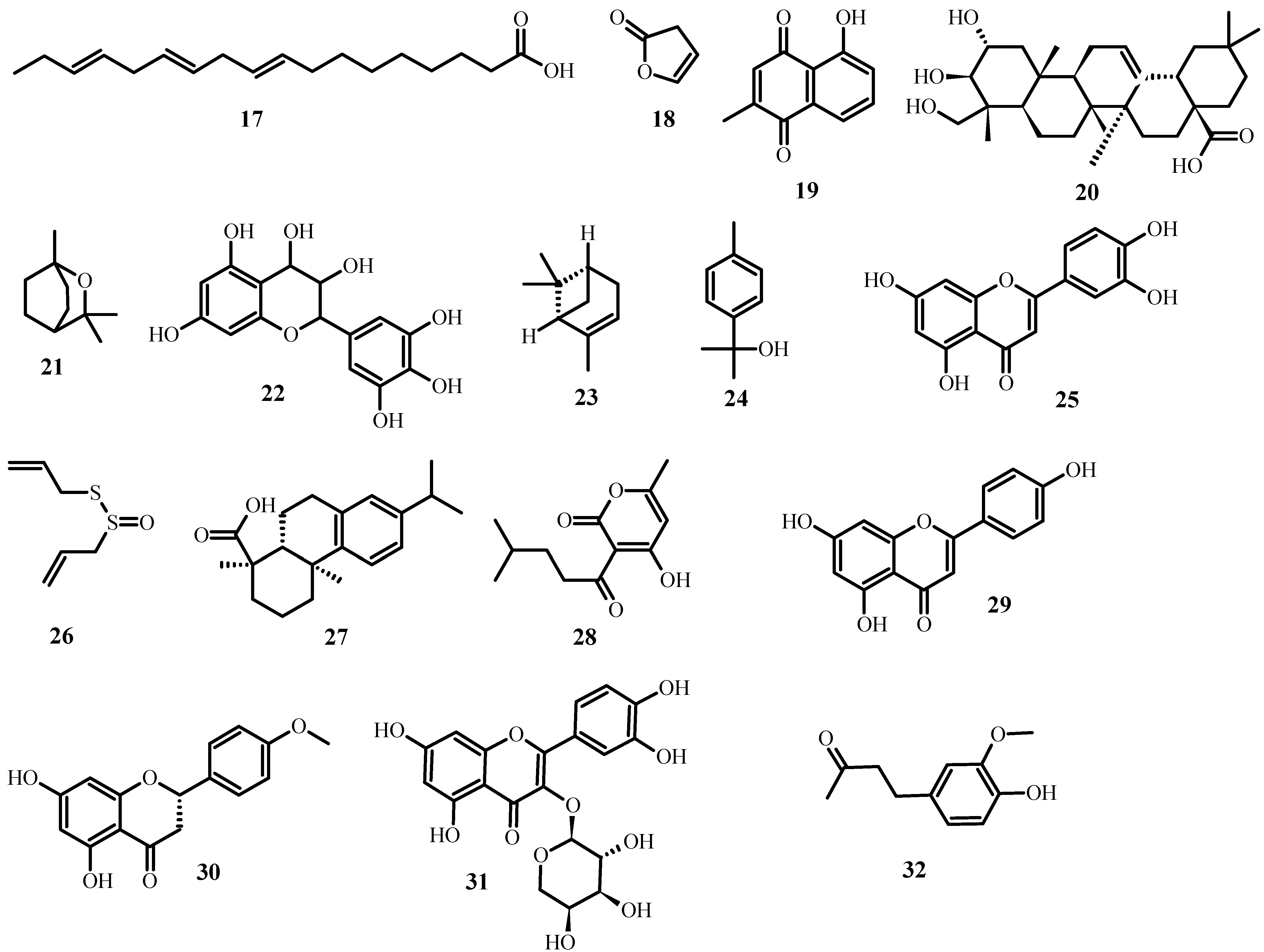
| Name of the Compound | Source of the Compound | Biological Effect on MDR Bacteria | References |
|---|---|---|---|
| 9,12,15-Octadecatrienoic acid (17) | Ocimum basilicum | Used in contesting E. coli, S. aureus, K. pneumonia, P. aeruginosa, and P. mirabilis. | [34] |
| Furanone (18) | Vanilla planifolia | Interferes in the quorum sensing system of P. aeruginosa. | [35] |
| Plumbagin (19) | Plumbago indica | Has antibacterial properties by binding to the ATP cassette transporter. | [36,37] |
| Arjunolic acid (20) | Cercidium microphyllum | Inhibits E. coli, B. subtilis, and S. sonnei. | [38] |
| 1,8-Cineole (21) | Eucalyptus globulus | Has antibacterial (methicillin-resistant S. aureus), antibiofilm, and anti-quorum sensing activities. | [39,40] |
| Leucoanthocyanidin (22) | Umbellularia californica | Has a cidal effect against B. cereus ATCC14579, S. pyogens ATCC10782, and MRSA ATCC-BAA-1683. | [41] |
| Quercetin (10) | Citrus sinensis | Inhibits the proton motive force (PMF) of S. aureus and inhibits P. aeruginosa (POA1), E. coli O157H7, and V. harveyi BB120. | [42] |
| Warfarin (13) | Dipteryx odorata | Inhibits S. viridans, S. mutans and S. aureus. | [16] |
| α-Pinene (23) | Callistemon viminalis | Suppresses the growth of B. cereus, S. typhi, P. aeruginosa, B. subtilis, E. coli, and P. vulgaris. | [43] |
| p-Cymen-8-ol (24) | Senecio nutans | Interferes with the membrane permeability of V. cholerae. | [44] |
| Luteolin (25) | Guazuma ulmifolia | Has a cidal effect against M. tuberculosis. | [45] |
| Allicin (26) | Allium sativum | Interferes with the metabolic systems of H. pylori, S. epidermidis, B. cepacia, P. aeruginosa, and S. aureus. | [46] |
| Thymol (8) | Lippia sidoides | Has activity against L. monocytogen, S. typhimurium, and E. coli O157:H7. | [46,47] |
| Dehydroabietic acid (27) | Pinus elliottii | Has a cidal effect against E. faecalis, S. haemolyticus, S. capitis, and MDR-S. epidermidis. | [48] |
| Pogostone (28) | Pogostemon cablin | Is effective against both gram-negative and gram-positive bacteria. | [49] |
| Apigenin (29) | Mentha pulegium | Interferes with the growth of B. cereus, E. coli, and S. aureus. | [50] |
| Isosakuranetin (30) | Hyptis albida | Inhibits S. aureus and B. subitilis. | [51] |
| Guaijaverin (31) | Psidium guajava | Significantly inhibits the adherence of S. mutans. | [52,53] |
| Zingerone (32) | Zingiber officinale | Inhibits biofilm formation and attenuation of motility properties in P. aeruginosa. | [54,55,56] |
2.3. Pathogenic Fungi for Human
2.4. Mechanism of Action and Drug-Resistance of Pathogenic Fungi
2.5. Latin American Plants with Antifungal Effects
2.6. Medicinal Plant Antiviral Activity against Human-Infecting Viruses
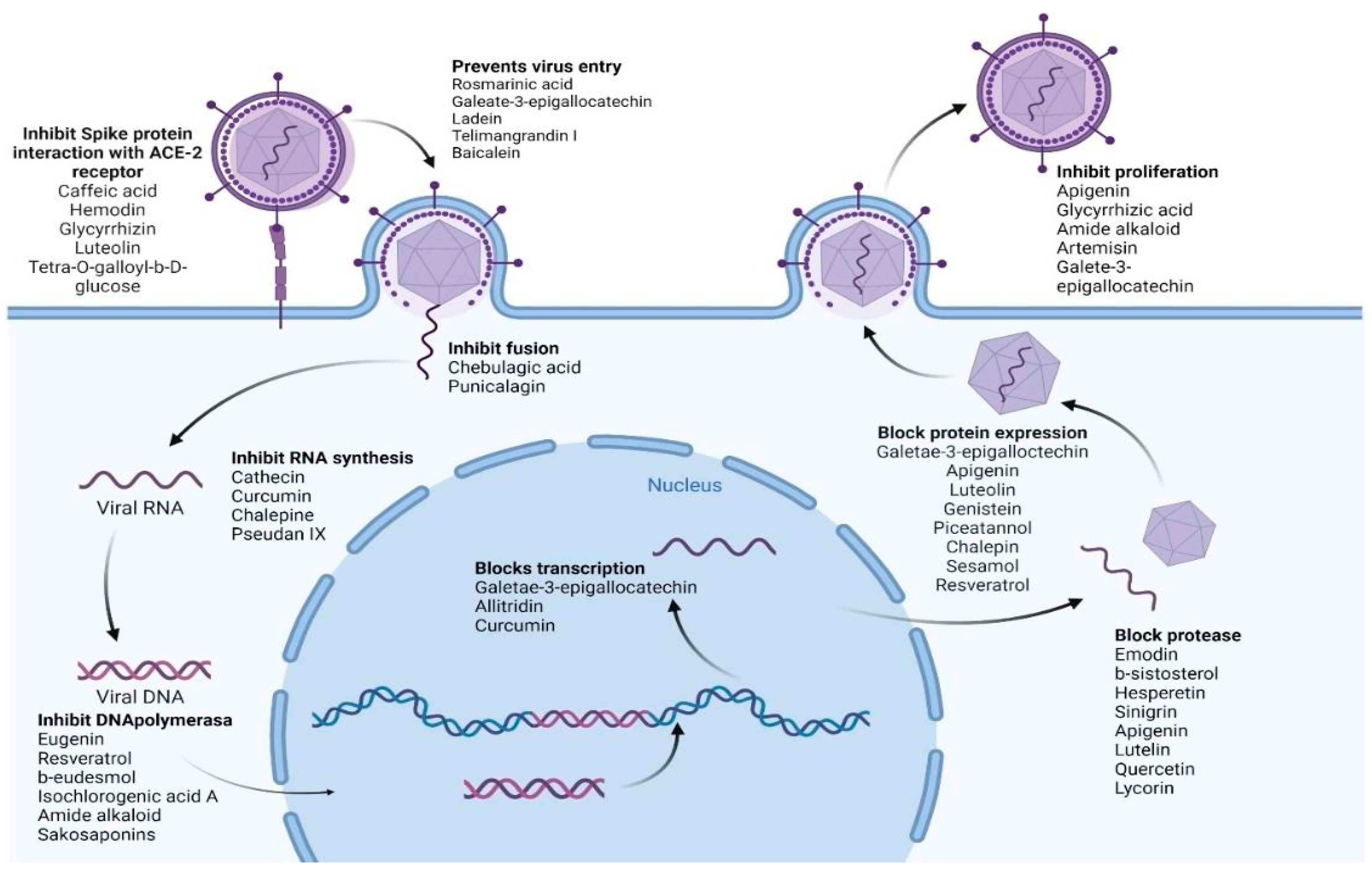
2.6.1. Biological Mechanisms of Antiviral Activity
2.6.2. Antiviral-Active Extracts for Respiratory Infections
2.6.3. Extracts and Biocompounds with Activity against Human Herpes Viruses
2.6.4. Activity against Epstein-Barr Virus
2.6.5. Anti-Cytomegalovirus Activities
2.6.6. Anti-HIV Activity of Extracts and Biocompounds
2.6.7. Antiviral Activity of Extracts and Biocompounds against Hepatitis B and C Viruses
2.6.8. Anti-Influenza Activity of Extracts and Biomolecules
2.6.9. Extracts In Vitro Possess Anti-Papillomavirus Activity
2.6.10. In Vitro Activity of Extracts against Dengue and Chikungunya Viruses
2.6.11. Antiviral Activity of In Vitro Extracted Compounds against SARS-CoV
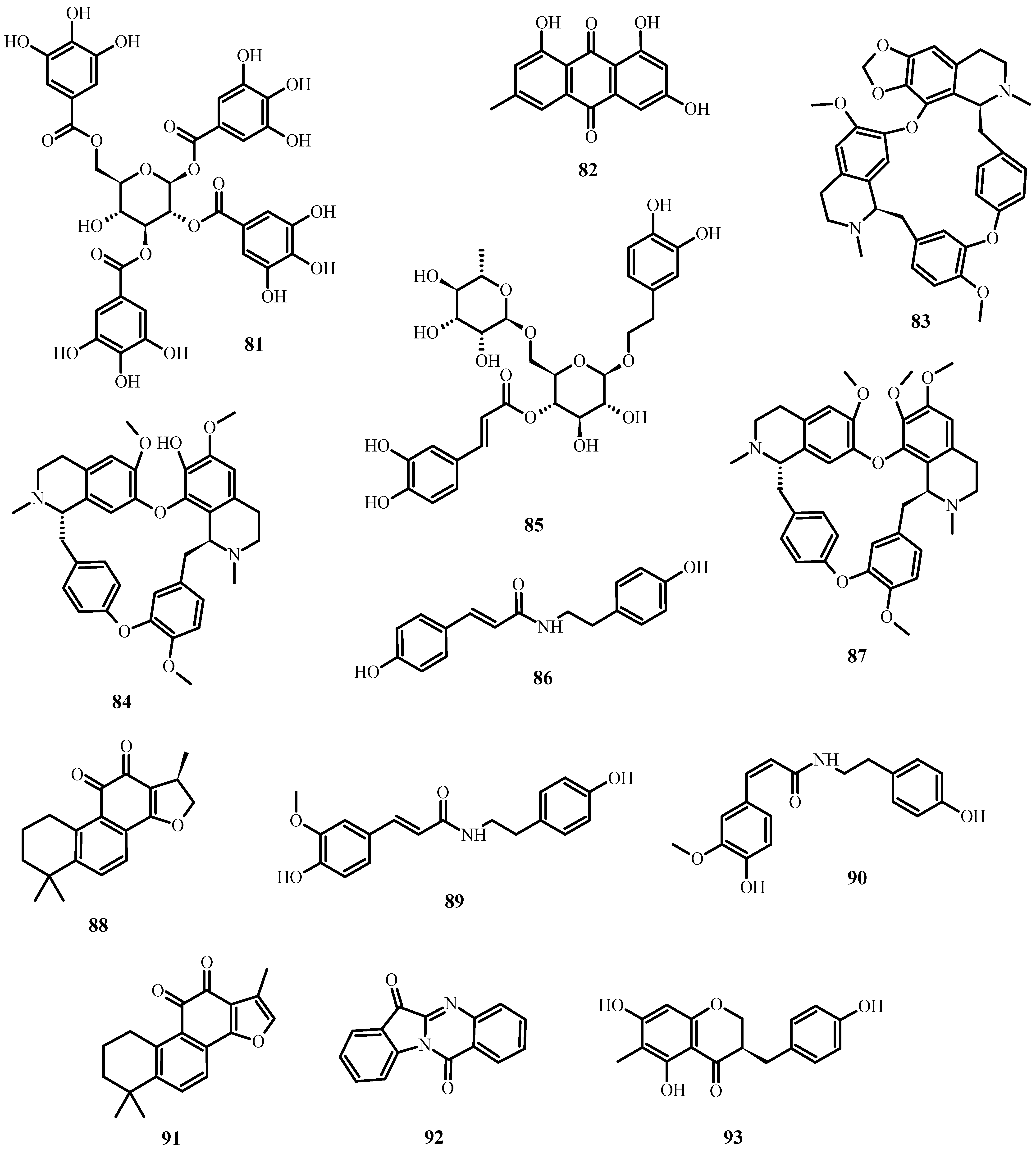
- To inhibit the binding of the spike protein to the ACE-2 receptor: caffeic acid (51), emodin (82), glycyrrhizin (56), luteolin (25), and tetra-O-galloyl-β-D-glucose (81).
- To prevent virus transcription: cepharanthin (83), fangquinoline (84), forystoside A (85), tetrandin (87), coumaroyltyramine (86), cryptoansionone (88), kaempferol (34), moupinamide (89), N-cis-feruloyltyramine (90), quercetin (10), tanshinone IIa (91), and tryptanthrine (92).
- To inhibit viral translation: tryptanthrine (92).
- To inhibit the cellular discharge of virions: emodin (82) and kaempferol (34).
| Plant | Extract | Virus | Possible Antiviral Mechanism | References |
|---|---|---|---|---|
| Echinacea pallida var. angustifolia | Hexane | Rhinovirus | Impedes replication. | [116] |
| Echinacea purpurea | Ethanolic | Coronavirus HcoV-299E | Prevents the invasion of cells. | [117] |
| Sambucus formosana Nakai | Ethanolic | HCoV-NL63 (coronavirus) | Prevents bonding. | [118] |
| Plantago asiatica | Aqueous extract | Respiratory syncytial virus | Replication inhibition. | [119] |
| Clerodendrum trichotomun | Aqueous extract | Respiratory syncytial virus | Replication inhibition. | [119] |
| Clinacanthus mutans Clinacanthus siamensis | Hexane, dichloromethane, and methanolic | Herpes simplex-1 and 2 | Inhibit viral plaques. | [120] |
| Polygonum minus | Methanolic | Herpes simplex-1 and 2 | Inhibits adhesion. | [122] |
| Aloe vera | Glycerol | Herpes simplex 2 | Impedes replication. | [123] |
| Lysimachia mauritania | Ethanolic extract | Varicella-zoster | Impedes replication. | [89] |
| Sesamum indicum Helianthus annuus | Sesame essential oil and Sunflower essential oil | Epstein-Barr Virus | Inhibit precocious antigen activation. | [132] |
| Salvia miltiorrhiza | Aqueous extract | HIV-1 | Interferes with integrase activation. | [143] |
| Rhaphiolepsis indica | Methanolic extract | HIV-1 | Impedes replication. | [144] |
| Acacia arabica | N-butanol fraction | HIV-1 | Inhibits viral proteases and Tat activity. | [145] |
| Phyllanthus amarus Schum. | Ethanolic and aqueous extract | HIV-1 | Impedes replication. | [146] |
| Olea europaea | Aqueous extract | HIV-1 | Prevents infections between cells. | [147] |
| Hyssopus officinalis L. | Aqueous extract | HIV-1 | Inhibits replication. | [148] |
| Polygonum cuspidatum | Ethanolic extract | Hepatitis virus B | Inhibits surface antigen expression. | [157] |
| Punica granatum | Ethanolic and polyphenolic extracts | Influenza virus | Inhibits influenza replication and virions. | [169] |
| Geranium sanguineum | Polyphenolic, methanolic, and ethanolic | Influenza virus | No study. | [170] |
| Chenomeles sinensis | Polyphenols | Influenza virus | Inhibits the attachment of its hemagglutinins. | [172] |
| Sambucus nigra | Aqueous extract | Influenza virus | Modulates cytokine release and inhibits viral entrance. | [173] |
| Phyllanthus emblica | Aqueous extract | Influenza virus | Prevents hemagglutinins and viruses from infecting infected cells. | [174] |
| Echinacea purpurea | Aqueous extract | Influenza A/B viruses H3N2, H1N1, H5N1, H7N7, and S-OIV | Induces IL-6 and IL-8 production. | [177] |
| Euphorbiacea shrub | Polyphenolic polymers | Influenza | No study. | [181] |
| Ficus religiosa | Aqueous extract | Papillomavirus | HPV-16 apoptosis is induced. | [184] |
| Bryophyllum pinnatum | Chloroplast extract | Papillomavirus | Suppresses HPV-18 transcription. | [184] |
| Pinellia pedatisecta | Soluble extract | Papillomavirus | Inhibits the HPV-E6 expression in multiple cell lines. | [184] |
| Carioca papaya | Aqueous and chloroplast extract | Chikungunya | Stops the dengue virus. | [186] |
| Sambucus nigra | Methanolic extract | Dengue serotype 2 | Defends against infection. | [187] |
| Vernonia amygdalina | Ethyl acetate extract | Chikungunya | Minimizes the viral burden. | [188] |
| Picrorhiza kurrooa Ocimum tenuiflorum Terminalia chebula | Aqueous extracts | Chikungunya | Block helicases and proteases. | [189] |
| Lycoris radiate, Artemisia annua, Pyrrosia lingua, Lindera aggregata, and Isatis indigotica | Different extracts | SARS-CoV-1 | Obstruct 3CL protease. | [190] |
| Rheum officinale Bail, Polygonum multiforum Thunb | Different extracts | SARS-CoV-1 | Inhibit the interaction between ACE2 and spike proteins. | [191] |
| Gentiana scabana, Dioscorea batatas, Casssia tora, Taxillus chinensis, and Cibotium barometz | Different extracts | SARS-CoV-1 | Prevent 3CL protease. | [192] |
| Anthemis hyalina, Nigella sativa, and Citrus sinensis | Ethanolic extracts | SARS-CoV-1 | Increase IL-8 and modulate gene expression of TRPA, TRPM, and TRPV. | [193] |
| Secondary Metabolite Class | Biocompound (Species) | Virus | Potential Antiviral Mechanism | Reference |
|---|---|---|---|---|
| Menthane monoterpenoids | Carvacrol (12) (Lippia graveolens) | Herpes viruses | No study. | [125] |
| Furocoumarin | Imperatorin (41) and phellopterin (42) (Angelica archangelica) | Herpes simplex virus type 1 Coxsackievirus B3 | No study. | [126] |
| Chromone | Eugenin (43) (Geum japonicum, Syzygium aromaticum) | Herpes simplex virus | Prevents DNA polymerase. | [127] |
| Cinnamic acid derivative | Rosmarinic acid (47) (M. officinalis) | Herpes simplex type 2 | Prevents virus entry into cells. | [129] |
| Flavan-3-ol | Epigallocatechin-3-gallate (48) (Camellia sinensis) | Epstein–Barr Virus | Blocks transcription and protein expression via ERK1/2 (extracellular-regulated-kinase 12) and PI3-K/Akt (phosphatidylinositol-3-kinase) pathways. | [131] |
| Phenol, Monomeric stilbene | Sesamol (49), resveratrol (2) (Sesamum indicum) | Epstein–Barr Virus | Inhibit early antigen activation. | [132] |
| Isoquinoline alkaloid | Berberine (15) (Barnerini vulgaris) | Epstein–Barr Virus | Inhibits cell proliferation and induces apoptosis in Epstein–Barr virus-infected cells by inhibiting p-STAT3. | [134] |
| Linear diarylheptanoid | Curcumin (33) (Curcuma longa) | Epstein–Barr Virus | Inhibits TPA-, butyrate-, and TGF-b induced levels of BZLF1 mRNA | [135] |
| Flavone | Apigenin (29) (purchased from Sigma-Aldrich Co., St. Louis, MO, USA) | Epstein–Barr Virus | Inhibits lytic proteins Zta, Rta, EAD, and DNase in B and epithelial cells and reduces the production of EBV viruses. | [136] |
| Oleanane triterpenoid | Glycyrrhizic acid (56) (Glycyrrhiza radix) | Epstein–Barr Virus | Interferes with the initial phase of EBV replication. | [137] |
| Flavone | Luteolin (25) (purchased from Sigma-Aldrich Co.) | Epstein–Barr Virus | Inhibits the expression of proteins encoded by the EBV lytic gene. | [138] |
| Isoflavone | Genistein (55) (purchased from Sigma-Aldrich) | Cytomegalovirus | Inhibits immediate-early (ie) protein function. | [139] |
| Flavone | Baicalein (57) (purchased from Sigma-Aldrich) | Cytomegalovirus | Inhibits EGFR’s kinase activity to prevent viral entry. | [139] |
| Monomeric stilbene | Piceatannol (58) (purchased from Sigma-Aldrich) | Cytomegalovirus | Inhibits the lytic modifications and expression of hCMV early (E) and immediate–-early (IE) proteins. | [140] |
| Monomeric stilbene | Resveratrol (2) (purchased from Sigma-Aldrich) | Cytomegalovirus | Reduces DNA replication. | [141] |
| Sulfide | Allitridin (59) (A. sativum) | Cytomegalovirus | Inhibits the IE genes’ transcription. | [142] |
| Neolignan | Monoterpenylmagnolol (52) and β-eudesmol (50) (Magnolia officinalis) | Epstein–Barr Virus | Impede replication. | [133] |
| Cinnamic acid derivative | Isochlorogenic acid A (61) (Laggera alata) | Hepatitis virus B | Impedes replication. | [153] |
| Alkaloid | Amide alkaloids (Piper longum) | Hepatitis virus B | Inhibit replication and surface antigen expression. | [154] |
| Saponin | Saikosaponins (Bupleurum species) | Hepatitis virus B | Inhibit replication and surface antigen expression. | [156] |
| Protoberberine alkaloid | Dehydrocheilanthifoline (60) (Corydalis saxifolia) | Hepatitis virus B | Prevents reproduction. | [155] |
| Linear diarylheptanoid | Curcumin (33) (Curcuma longa) | Hepatitis virus B | Decreases Transcription. | [158] |
| Oleanane triterpenoid | Glycyrrhizinic acid (56) (Glycyrrhiza glabra) | Hepatitis virus B | Prevents viral reproduction. | [159,197] |
| Sesquiterpene lactone | Artemisinin (62) (Artemisia annua) | Hepatitis virus B | Prevents viral reproduction. | [159,197] |
| Isoflavonoid | LPRP-Et-97543 (93) (Liriope platyphylla) | Hepatitis virus B | Prevents viral reproduction. | [159,197] |
| Flavan-3-ol | Epigallocatechin-3-gallate (48) (Camellia sinensis) | Hepatitis virus B | Prevents viral reproduction. | [160] |
| Lignan | Flavonolignans (Silybum marianum) | Hepatitis C virus | No study. | [161] |
| Linear diarylheptanoid | Curcumin (33) (Curcuma longa) | Hepatitis C virus | Inhibits viral replication by blocking Akt-SREBP-1. | [162] |
| Flavan-3-ol | Epigallocatechin-3-gallate (48) (Camellia sinensis) | Hepatitis C virus | Inhibits viral introduction. | [163] |
| Flavone | Ladanein (77) (Marrubium peregrinum) | Hepatitis C virus | Inhibits viral introduction. | [164] |
| Peptide | Recombinant Griffithsin (Nicotiana benthamiana) | Hepatitis C virus | Inhibits viral cell–cell transmission. | [165] |
| Gallotannin | Tellimagrandin I (78) (Rosae rugosae) | Hepatitis C virus | Prevents viral penetration. | [159] |
| Benzopyran tannin and phenol | Chebulagic acid (64) and punicalagin (65) (Terminalia chebula Retz) | Hepatitis C virus | Inhibit fusion and cell–cell transmission. | [166] |
| Oleanane triterpenoid | Saikosaponin B2 (79) (Bupleurum kaoi) | Hepatitis C virus | Prevents viral attachment. | [159] |
| Furocoumarin, Quinoline alkaloid | Chalepine (66), pseudan IX (80) (Ruta angustifolia) | Hepatitis C virus | Reduce viral protein synthesis and viral RNA replication. | [159] |
| Lupane triterpenoids | Betulinic acid (67) and betulin (68) (Betula alba L) | Hepatitis C virus | Induce expression of TNF-α. | [168] |
| Oleanane triterpenoid | Glycyrrhizin (56) (Glycyrrhiza glabra) | Influenza virus | Initiates cell death in H5N1-infected cells. | [171] |
| Catechin | Catechins (Camellia sinensis) | Influenza virus | Inhibit both RNA synthesis and neuraminidase activity. | [175] |
| Dibenzylbutyrolactone lignans | Arctigenin (69) and arcitiin (70) (Arctium lappa) | Influenza virus | Anti-influenza A virus in vitro activity. | [176] |
| Monoterpenaldehydes | Citral a (45) and citral b (46) (Melissa officinalis) | H9N2 influenza virus | Have synergistic activity with oseltamivir. | [180] |
| Flavan-3-ols | Polyphenon E (poly E) (71) and epigallocatechin gallate (48) (Camellia sinensis) | Papillomavirus | Impede growth. | [182] |
| Sesquiterpene lactone | Artemisinin (62) (Artemisia absintium) | Papillomavirus | In ME-180 cells, this compound inhibits the expression of HPV-39, induces apoptosis, and reduces the proliferation of infected cells. | [183] |
| Tannin | Tannins (Hamamelis virginiana) | Papillomavirus | Inhibit HPV-16 | [184] |
| Benzopyrone | Coumarin (33) (Alternanthera philoxeroides) | Chikungunya | Stops the dengue virus. | [185] |
| Anthraquinone, Stigmastane steroid, Flavanone, Anthranilic acid alkaloid, Glucosinolate | Emodin (82), β-sistosterol (63), hesperetin (74), indigo (75), and sinigrin (76) (Isatis indigotica) | SARS-CoV-1 | Block the 3CL protease. | [194] |
| Flavones, Flavonol | Amentoflavone (53), apigenin (29), luteolin (25), quercetin (10) (Torreya nucifera) | SARS-CoV-1 | Block the 3CL protease. | [195] |
| Indolizidine alkaloid | Lycorine (54) (Lycoris radiata) | SARS-CoV-1 | Block 3CL protease. | [190] |
| Cinammic acid derivative, Anthraquinone, Oleanane triterpenoid, Flavonoid, Gallotannin | Caffeic acid (51), emodin (82), glycyrrhizin (56), luteolin (25), and tetra-O-galloyl-β-D-glucose (81) | SARS-CoV-2 | Inhibit the spike protein’s interaction with the ACE-2 receptor. | [196] |
2.6.12. Molecules with Antiviral Activity Identified In Silico
3. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Zhong, C.; Zhang, F.; Yao, J.; Zhu, Y.; Zhu, N.; Zhang, J.; Ouyang, X.; Zhang, T.; Li, B.; Xie, J.; et al. New Antimicrobial Peptides with Repeating Unit against Multidrug-Resistant Bacteria. ACS Infect. Dis. 2021, 7, 1619–1637. [Google Scholar] [CrossRef]
- Fisher, R.A.; Gollan, B.; Helaine, S. Persistent Bacterial Infections and Persister Cells. Nat. Rev. Microbiol. 2017, 15, 453–464. [Google Scholar] [CrossRef] [PubMed]
- Luo, G.G.; Gao, S.J. Global Health Concerns Stirred by Emerging Viral Infections. J. Med. Virol. 2020, 92, 399–400. [Google Scholar] [CrossRef] [PubMed]
- Ji, C.; Liu, N.; Tu, J.; Li, Z.; Han, G.; Li, J.; Sheng, C. Drug Repurposing of Haloperidol: Discovery of New Benzocyclane Derivatives as Potent Antifungal Agents against Cryptococcosis and Candidiasis. ACS Infect. Dis. 2020, 6, 768–786. [Google Scholar] [CrossRef]
- Kingston, D.G.I. Modern Natural Products Drug Discovery and Its Relevance to Biodiversity Conservation. J. Nat. Prod. 2011, 74, 496–511. [Google Scholar] [CrossRef]
- O’Neill, J. Tackling Drug-Resistance Infections Globally: Final Report and Recommendations; Government of the United Kingdom: London, UK, 2016.
- Zhu, Y.; Huang, W.E.; Yang, Q. Clinical Perspective of Antimicrobial Resistance in Bacteria. Infect. Drug Resist. 2022, 15, 735–746. [Google Scholar] [CrossRef] [PubMed]
- Dadgostar, P. Antimicrobial Resistance: Implications and Costs. Infect. Drug Resist. 2019, 12, 3903–3910. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Baño, J.; Rossolini, G.M.; Schultsz, C.; Tacconelli, E.; Murthy, S.; Ohmagari, N.; Holmes, A.; Bachmann, T.; Goossens, H.; Canton, R.; et al. Antimicrobial Resistance Research in a Post-Pandemic World: Insights on Antimicrobial Resistance Research in the COVID-19 Pandemic. J. Glob. Antimicrob. Resist. 2021, 25, 5–7. [Google Scholar] [CrossRef] [PubMed]
- Laxminarayan, R. The Overlooked Pandemic of Antimicrobial Resistance. Lancet 2022, 399, 606–607. [Google Scholar] [CrossRef]
- Rizvi, S.G.; Ahammad, S.Z. COVID-19 and Antimicrobial Resistance: A Cross-Study. Sci. Total Environ. 2022, 807, 150873. [Google Scholar] [CrossRef]
- Christaki, E.; Marcou, M.; Tofarides, A. Antimicrobial Resistance in Bacteria: Mechanisms, Evolution, and Persistence. J. Mol. Evol. 2020, 88, 26–40. [Google Scholar] [CrossRef] [PubMed]
- Reygaert, W.C. An Overview of the Antimicrobial Resistance Mechanisms of Bacteria. AIMS Microbiol. 2018, 4, 482–501. [Google Scholar] [CrossRef] [PubMed]
- Murugaiyan, J.; Kumar, P.A.; Rao, G.S.; Iskandar, K.; Hawser, S.; Hays, J.P.; Mohsen, Y.; Adukkadukkam, S.; Awuah, W.A.; Jose, R.A.M.; et al. Progress in Alternative Strategies to Combat Antimicrobial Resistance: Focus on Antibiotics. Antibiotics 2022, 11, 200. [Google Scholar] [CrossRef] [PubMed]
- Anand, U.; Jacobo-Herrera, N.; Altemimi, A.; Lakhssassi, N. A Comprehensive Review on Medicinal Plants as Antimicrobial Therapeutics: Potential Avenues of Biocompatible Drug Discovery. Metabolites 2019, 9, 258. [Google Scholar] [CrossRef]
- Srivastava, J.; Chandra, H.; Nautiyal, A.R.; Kalra, S.J.S. Antimicrobial Resistance (AMR) and Plant-Derived Antimicrobials (PDAms) as an Alternative Drug Line to Control Infections. 3 Biotech 2014, 4, 451–460. [Google Scholar] [CrossRef]
- Esmael, A.; Hassan, M.G.; Amer, M.M.; Abdelrahman, S.; Hamed, A.M.; Abd-raboh, H.A.; Foda, M.F. Antimicrobial Activity of Certain Natural-Based Plant Oils against the Antibiotic-Resistant Acne Bacteria. Saudi J. Biol. Sci. 2020, 27, 448–455. [Google Scholar] [CrossRef]
- Intorasoot, A.; Chornchoem, P.; Sookkhee, S.; Intorasoot, S. Bactericidal Activity of Herbal Volatile Oil Extracts against Multidrug Resistant Acinetobacter Baumannii. J. Intercult. Ethnopharmacol. 2017, 6, 1. [Google Scholar] [CrossRef]
- Dharmaratne, M.P.J.; Manoraj, A.; Thevanesam, V.; Ekanayake, A.; Kumar, N.S.; Liyanapathirana, V.; Abeyratne, E.; Bandara, B.M.R. Terminalia Bellirica Fruit Extracts: In-Vitro Antibacterial Activity against Selected Multidrug-Resistant Bacteria, Radical Scavenging Activity and Cytotoxicity Study on BHK-21 Cells. BMC Complement. Altern. Med. 2018, 18, 325. [Google Scholar] [CrossRef]
- Khan, S.; Imran, M.; Imran, M.; Pindari, N. Antimicrobial Activity of Various Ethanolic Plant Extracts against Pathogenic Multi-Drug Resistant Candida spp. Bioinformation 2017, 13, 67–72. [Google Scholar] [CrossRef]
- Khan, M.F.; Tang, H.; Lyles, J.T.; Pineau, R.; Mashwani, Z.-R.; Quave, C.L. Antibacterial Properties of Medicinal Plants From Pakistan against Multidrug-Resistant ESKAPE Pathogens. Front. Pharmacol. 2018, 9, 815. [Google Scholar] [CrossRef]
- Alibi, S.; Crespo, D.; Navas, J. Plant-Derivatives Small Molecules with Antibacterial Activity. Antibiotics 2021, 10, 231. [Google Scholar] [CrossRef]
- Jeyakumar, G.E.; Lawrence, R. Mechanisms of Bactericidal Action of Eugenol against Escherichia coli. J. Herb. Med. 2021, 26, 100406. [Google Scholar] [CrossRef]
- Vestergaard, M.; Ingmer, H. Antibacterial and Antifungal Properties of Resveratrol. Int. J. Antimicrob. Agents 2019, 53, 716–723. [Google Scholar] [CrossRef] [PubMed]
- Liang, H.; Huang, Q.; Zou, L.; Wei, P.; Lu, J.; Zhang, Y. Methyl Gallate: Review of Pharmacological Activity. Pharmacol. Res. 2023, 194, 106849. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Fu, J.; Yin, X.; Cao, S.; Li, X.; Lin, L.; Huyiligeqi; Ni, J. Emodin: A Review of Its Pharmacology, Toxicity and Pharmacokinetics. Phytother. Res. 2016, 30, 1207–1218. [Google Scholar] [CrossRef] [PubMed]
- Ferdes, M. Antimicrobial Compounds from Plants. In Fighting Antimicrobial Resistance; Budimir, A., Ed.; IAPC Publishing: Zagreb, Croatia, 2018; pp. 243–271. ISBN 978-953-56942-6-7. [Google Scholar]
- Nguyen, T.L.A.; Bhattacharya, D. Antimicrobial Activity of Quercetin: An Approach to Its Mechanistic Principle. Molecules 2022, 27, 2494. [Google Scholar] [CrossRef]
- Farhadi, F.; Khameneh, B.; Iranshahi, M.; Iranshahy, M. Antibacterial Activity of Flavonoids and Their Structure–Activity Relationship: An Update Review. Phytother. Res. 2019, 33, 13–40. [Google Scholar] [CrossRef]
- Asadi, S.; Nayeri-Fasaei, B.; Zahraei-Salehi, T.; Yahya-Rayat, R.; Shams, N.; Sharifi, A. Antibacterial and Anti-Biofilm Properties of Carvacrol Alone and in Combination with Cefixime against Escherichia coli. BMC Microbiol. 2023, 23, 55. [Google Scholar] [CrossRef]
- Tian, L.; Wang, X.; Liu, R.; Zhang, D.; Wang, X.; Sun, R.; Guo, W.; Yang, S.; Li, H.; Gong, G. Antibacterial Mechanism of Thymol against Enterobacter sakazakii. Food Control 2021, 123, 107716. [Google Scholar] [CrossRef]
- Chakraborty, P.; Dastidar, D.G.; Paul, P.; Dutta, S.; Basu, D.; Sharma, S.R.; Basu, S.; Sarker, R.K.; Sen, A.; Sarkar, A.; et al. Inhibition of Biofilm Formation of Pseudomonas aeruginosa by Caffeine: A Potential Approach for Sustainable Management of Biofilm. Arch. Microbiol. 2020, 202, 623–635. [Google Scholar] [CrossRef]
- Peng, L.; Kang, S.; Yin, Z.; Jia, R.; Song, X.; Li, L.; Li, Z.; Zou, Y.; Liang, X.; Li, L.; et al. Antibacterial Activity and Mechanism of Berberine against Streptococcus agalactiae. Int. J. Clin. Exp. Pathol. 2015, 8, 5217–5223. [Google Scholar]
- Mohanad, J.K.; Azhar, A.S.; Imad, H.H. Evaluation of Anti-Bacterial Activity and Bioactive Chemical Analysis of Ocimum basilicum Using Fourier Transform Infrared (FT-IR) and Gas Chromatography-Mass Spectrometry (GC-MS) Techniques. J. Pharmacogn. Phytother. 2016, 8, 127–146. [Google Scholar] [CrossRef]
- Choo, J.H.; Rukayadi, Y.; Hwang, J.-K. Inhibition of Bacterial Quorum Sensing by Vanilla Extract. Lett. Appl. Microbiol. 2006, 42, 637–641. [Google Scholar] [CrossRef]
- Ohene-Agyei, T.; Mowla, R.; Rahman, T.; Venter, H. Phytochemicals Increase the Antibacterial Activity of Antibiotics by Acting on a Drug Efflux Pump. MicrobiologyOpen 2014, 3, 885–896. [Google Scholar] [CrossRef] [PubMed]
- Castro, F.A.V.; Mariani, D.; Panek, A.D.; Eleutherio, E.C.A.; Pereira, M.D. Cytotoxicity Mechanism of Two Naphthoquinones (Menadione and Plumbagin) in Saccharomyces cerevisiae. PLoS ONE 2008, 3, e3999. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, J.; Sil, P.C. Arjunolic Acid: A New Multifunctional Therapeutic Promise of Alternative Medicine. Biochimie 2013, 95, 1098–1109. [Google Scholar] [CrossRef] [PubMed]
- Merghni, A.; Noumi, E.; Hadded, O.; Dridi, N.; Panwar, H.; Ceylan, O.; Mastouri, M.; Snoussi, M. Assessment of the Antibiofilm and Antiquorum Sensing Activities of Eucalyptus globulus Essential Oil and Its Main Component 1,8-Cineole against Methicillin-Resistant Staphylococcus aureus Strains. Microb. Pathog. 2018, 118, 74–80. [Google Scholar] [CrossRef]
- McLean, R.J.C.; Pierson, L.S.; Fuqua, C. A Simple Screening Protocol for the Identification of Quorum Signal Antagonists. J. Microbiol. Methods 2004, 58, 351–360. [Google Scholar] [CrossRef]
- Carranza, M.G.; Sevigny, M.B.; Banerjee, D.; Fox-Cubley, L. Antibacterial Activity of Native California Medicinal Plant Extracts Isolated from Rhamnus Californica and Umbellularia Californica. Ann. Clin. Microbiol. Antimicrob. 2015, 14, 29. [Google Scholar] [CrossRef]
- Bouyahya, A.; Dakka, N.; Et-Touys, A.; Abrini, J.; Bakri, Y. Medicinal Plant Products Targeting Quorum Sensing for Combating Bacterial Infections. Asian Pac. J. Trop. Med. 2017, 10, 729–743. [Google Scholar] [CrossRef]
- Salem, M.Z.; Ali, H.M.; El-Shanhorey, N.A.; Abdel-Megeed, A. Evaluation of Extracts and Essential Oil from Callistemon viminalis Leaves: Antibacterial and Antioxidant Activities, Total Phenolic and Flavonoid Contents. Asian Pac. J. Trop. Med. 2013, 6, 785–791. [Google Scholar] [CrossRef]
- Paredes, A.; Leyton, Y.; Riquelme, C.; Morales, G. A Plant from the Altiplano of Northern Chile Senecio nutans, Inhibits the Vibrio cholerae Pathogen. SpringerPlus 2016, 5, 1788. [Google Scholar] [CrossRef] [PubMed]
- Alvin, A.; Miller, K.I.; Neilan, B.A. Exploring the Potential of Endophytes from Medicinal Plants as Sources of Antimycobacterial Compounds. Microbiol. Res. 2014, 169, 483–495. [Google Scholar] [CrossRef] [PubMed]
- Barbieri, R.; Coppo, E.; Marchese, A.; Daglia, M.; Sobarzo-Sánchez, E.; Nabavi, S.F.; Nabavi, S.M. Phytochemicals for Human Disease: An Update on Plant-Derived Compounds Antibacterial Activity. Microbiol. Res. 2017, 196, 44–68. [Google Scholar] [CrossRef]
- Botelho, M.A.; Nogueira, N.A.P.; Bastos, G.M.; Fonseca, S.G.C.; Lemos, T.L.G.; Matos, F.J.A.; Montenegro, D.; Heukelbach, J.; Rao, V.S.; Brito, G.A.C. Antimicrobial Activity of the Essential Oil from Lippia sidoides, Carvacrol and Thymol against Oral Pathogens. Braz. J. Med. Biol. Res. 2007, 40, 349–356. [Google Scholar] [CrossRef]
- Subramani, R.; Narayanasamy, M.; Feussner, K.-D. Plant-Derived Antimicrobials to Fight against Multi-Drug-Resistant Human Pathogens. 3 Biotech 2017, 7, 172. [Google Scholar] [CrossRef]
- Swamy, M.; Sinniah, U. A Comprehensive Review on the Phytochemical Constituents and Pharmacological Activities of Pogostemon cablin Benth.: An Aromatic Medicinal Plant of Industrial Importance. Molecules 2015, 20, 8521–8547. [Google Scholar] [CrossRef]
- Proestos, C.; Chorianopoulos, N.; Nychas, G.-J.E.; Komaitis, M. RP-HPLC Analysis of the Phenolic Compounds of Plant Extracts. Investigation of Their Antioxidant Capacity and Antimicrobial Activity. J. Agric. Food Chem. 2005, 53, 1190–1195. [Google Scholar] [CrossRef] [PubMed]
- Rojas, A.; Hernandez, L.; Pereda-Miranda, R.; Mata, R. Screening for Antimicrobial Activity of Crude Drug Extracts and Pure Natural Products from Mexican Medicinal Plants. J. Ethnopharmacol. 1992, 35, 275–283. [Google Scholar] [CrossRef]
- Song, X.; Xia, Y.-X.; He, Z.-D.; Zhang, H.-J. A Review of Natural Products with Anti-Biofilm Activity. Curr. Org. Chem. 2018, 22, 789–817. [Google Scholar] [CrossRef]
- Prabu, G.R.; Gnanamani, A.; Sadulla, S. Guaijaverin—A Plant Flavonoid as Potential Antiplaque Agent against Streptococcus mutans. J. Appl. Microbiol. 2006, 101, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Ali, B.H.; Blunden, G.; Tanira, M.O.; Nemmar, A. Some Phytochemical, Pharmacological and Toxicological Properties of Ginger (Zingiber officinale Roscoe): A Review of Recent Research. Food Chem. Toxicol. 2008, 46, 409–420. [Google Scholar] [CrossRef]
- Kim, H.-S.; Park, H.-D. Ginger Extract Inhibits Biofilm Formation by Pseudomonas aeruginosa PA14. PLoS ONE 2013, 8, e76106. [Google Scholar] [CrossRef]
- Kumar, L.; Chhibber, S.; Harjai, K. Zingerone Inhibit Biofilm Formation and Improve Antibiofilm Efficacy of Ciprofloxacin against Pseudomonas aeruginosa PAO1. Fitoterapia 2013, 90, 73–78. [Google Scholar] [CrossRef] [PubMed]
- GBIF. Sistema Global de Información Sobre Biodiversidad. Available online: https://www.gbif.org/es/ (accessed on 25 July 2023).
- Cheek, M.; Nic Lughadha, E.; Kirk, P.; Lindon, H.; Carretero, J.; Looney, B.; Douglas, B.; Haelewaters, D.; Gaya, E.; Llewellyn, T.; et al. New Scientific Discoveries: Plants and Fungi. Plants People Planet 2020, 2, 371–388. [Google Scholar] [CrossRef]
- Fisher, M.C.; Henk, D.A.; Briggs, C.J.; Brownstein, J.S.; Madoff, L.C.; McCraw, S.L.; Gurr, S.J. Emerging Fungal Threats to Animal, Plant and Ecosystem Health. Nature 2012, 484, 186–194. [Google Scholar] [CrossRef]
- Rokas, A. Evolution of the Human Pathogenic Lifestyle in Fungi. Nat. Microbiol. 2022, 7, 607–619. [Google Scholar] [CrossRef]
- Restrepo-Rivera, L.M.; Cardona-Castro, N. Micobioma: Diversidad Fúngica En El Cuerpo Humano. CES Med. 2021, 35, 113–125. [Google Scholar] [CrossRef]
- Seelbinder, B.; Chen, J.; Brunke, S.; Vazquez-Uribe, R.; Santhaman, R.; Meyer, A.C.; De Oliveira Lino, F.S.; Chan, K.F.; Loos, D.; Imamovic, L.; et al. Antibiotics Create a Shift from Mutualism to Competition in Human Gut Communities with a Longer-Lasting Impact on Fungi than Bacteria. Microbiome 2020, 8, 133. [Google Scholar] [CrossRef]
- Bongomin, F.; Gago, S.; Oladele, R.O.; Denning, D.W. Global and Multi-National Prevalence of Fungal Diseases—Estimate Precision. J. Fungi 2017, 3, 57. [Google Scholar] [CrossRef]
- Guarro, J. Taxonomía y Biología de Los Hongos Causantes de Infección En Humanos. Enferm. Infecc. Microbiol. Clin. 2012, 30, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Köhler, J.R.; Casadevall, A.; Perfect, J. The Spectrum of Fungi That Infects Humans. Cold Spring Harb. Perspect. Med. 2015, 5, a019273. [Google Scholar] [CrossRef] [PubMed]
- Brown, G.D.; Denning, D.W.; Gow, N.A.R.; Levitz, S.M.; Netea, M.G.; White, T.C. Hidden Killers: Human Fungal Infections. Sci. Transl. Med. 2012, 4, 165rv13. [Google Scholar] [CrossRef] [PubMed]
- Pemán, J.; Salavert, M. Epidemiología General de La Enfermedad Fúngica Invasora. Enfermedades Infecc. Microbiol. Clínica 2012, 30, 90–98. [Google Scholar] [CrossRef]
- Shapiro, R.S.; Robbins, N.; Cowen, L.E. Regulatory Circuitry Governing Fungal Development, Drug Resistance, and Disease. Microbiol. Mol. Biol. Rev. 2011, 75, 213–267. [Google Scholar] [CrossRef]
- Perfect, J.R. The Antifungal Pipeline: A Reality Check. Nat. Rev. Drug Discov. 2017, 16, 603–616. [Google Scholar] [CrossRef]
- Oliveira, L.V.N.; Wang, R.; Specht, C.A.; Levitz, S.M. Vaccines for Human Fungal Diseases: Close but Still a Long Way to Go. Npj Vaccines 2021, 6, 33. [Google Scholar] [CrossRef]
- Romani, L. Immunity to Fungal Infections. Nat. Rev. Immunol. 2011, 11, 275–288. [Google Scholar] [CrossRef]
- Carmo, A.; Rocha, M.; Pereirinha, P.; Tomé, R.; Costa, E. Antifungals: From Pharmacokinetics to Clinical Practice. Antibiotics 2023, 12, 884. [Google Scholar] [CrossRef]
- Quiles-Melero, I.; García-Rodríguez, J. Systemic Antifungal Drugs. Rev. Iberoam. Micol. 2021, 38, 42–46. [Google Scholar] [CrossRef]
- Ruiz-Camps, I.; Cuenca-Estrella, M. Antifungals for Systemic Use. Enferm. Infecc. Microbiol. Clin. 2009, 27, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Shaw, K.J.; Ibrahim, A.S. Fosmanogepix: A Review of the First-in-Class Broad Spectrum Agent for the Treatment of Invasive Fungal Infections. J. Fungi 2020, 6, 239. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Lara, M.F.; Sifuentes-Osornio, J.; Ostrosky-Zeichner, L. Drugs in Clinical Development for Fungal Infections. Drugs 2017, 77, 1505–1518. [Google Scholar] [CrossRef] [PubMed]
- Hope, W.W.; McEntee, L.; Livermore, J.; Whalley, S.; Johnson, A.; Farrington, N.; Kolamunnage-Dona, R.; Schwartz, J.; Kennedy, A.; Law, D.; et al. Pharmacodynamics of the Orotomides against Aspergillus fumigatus: New Opportunities for Treatment of Multidrug-Resistant Fungal Disease. mBio 2017, 8, e01157-17. [Google Scholar] [CrossRef] [PubMed]
- Fairlamb, A.H.; Gow, N.A.R.; Matthews, K.R.; Waters, A.P. Drug Resistance in Eukaryotic Microorganisms. Nat. Microbiol. 2016, 1, 16092. [Google Scholar] [CrossRef] [PubMed]
- Berman, J.; Krysan, D.J. Drug Resistance and Tolerance in Fungi. Nat. Rev. Microbiol. 2020, 18, 319–331. [Google Scholar] [CrossRef] [PubMed]
- Fisher, M.C.; Alastruey-Izquierdo, A.; Berman, J.; Bicanic, T.; Bignell, E.M.; Bowyer, P.; Bromley, M.; Brüggemann, R.; Garber, G.; Cornely, O.A.; et al. Tackling the Emerging Threat of Antifungal Resistance to Human Health. Nat. Rev. Microbiol. 2022, 20, 557–571. [Google Scholar] [CrossRef]
- Shrestha, S.K.; Fosso, M.Y.; Garneau-Tsodikova, S. A Combination Approach to Treating Fungal Infections. Sci. Rep. 2015, 5, 17070. [Google Scholar] [CrossRef]
- Carpinella, M.C.; Andrione, D.G.; Ruiz, G.; Palacios, S.M. Screening for Acetylcholinesterase Inhibitory Activity in Plant Extracts from Argentina. Phytother. Res. 2010, 24, 259–263. [Google Scholar] [CrossRef]
- Méndez-Chávez, M.; Ledesma-Escobar, C.A.; Hidalgo-Morales, M.; Rodríguez-Jimenes, G.D.C.; Robles-Olvera, V.J. Antifungal Activity Screening of Fractions from Annona cherimola Mill. Leaf Extract against Fusarium oxysporum. Arch. Microbiol. 2022, 204, 330. [Google Scholar] [CrossRef]
- Campos, L.M.; Silva, T.P.; De Oliveira Lemos, A.S.; Mendonça Diniz, I.O.; Palazzi, C.; Novaes Da Rocha, V.; De Freitas Araújo, M.G.; Melo, R.C.N.; Fabri, R.L. Antibiofilm Potential of Annona muricata L. Ethanolic Extract against Multi-Drug Resistant Candida Albicans. J. Ethnopharmacol. 2023, 315, 116682. [Google Scholar] [CrossRef] [PubMed]
- Diaz Napal, G.N.; Buffa, L.M.; Nolli, L.C.; Defagó, M.T.; Valladares, G.R.; Carpinella, M.C.; Ruiz, G.; Palacios, S.M. Screening of Native Plants from Central Argentina against the Leaf-Cutting Ant Acromyrmex lundi (Guérin) and Its Symbiotic Fungus. Ind. Crops Prod. 2015, 76, 275–280. [Google Scholar] [CrossRef]
- Navarro García, V.M.; Gonzalez, A.; Fuentes, M.; Aviles, M.; Rios, M.Y.; Zepeda, G.; Rojas, M.G. Antifungal Activities of Nine Traditional Mexican Medicinal Plants. J. Ethnopharmacol. 2003, 87, 85–88. [Google Scholar] [CrossRef]
- Poma-Castillo, L.; Espinoza-Poma, M. Antifungal Activity of Ethanol-Extracted Bixa Orellana (L) (Achiote) on Candida Albicans, at Six Different Concentrations. J. Contemp. Dent. Pract. 2019, 20, 1159–1163. [Google Scholar] [CrossRef]
- Wilson, B.; Abraham, G.; Manju, V.S.; Mathew, M.; Vimala, B.; Sundaresan, S.; Nambisan, B. Antimicrobial Activity of Curcuma Zedoaria and Curcuma Malabarica Tubers. J. Ethnopharmacol. 2005, 99, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Wang, C.; Xu, L.; Chen, X.; Wang, W.; Yang, G.; Tan, R.X.; Li, E.; Jin, Y. A Laboratory Evaluation of Medicinal Herbs Used in China for the Treatment of Hand, Foot, and Mouth Disease. Evid. Based Complement. Alternat. Med. 2013, 2013, 504563. [Google Scholar] [CrossRef]
- Mir-Rashed, N.; Cruz, I.; Jessulat, M.; Dumontier, M.; Chesnais, C.; Juliana, N.; Amiguet, V.T.; Golshani, A.; Arnason, J.T.; Smith, M.L. Disruption of Fungal Cell Wall by Antifungal Echinacea Extracts. Med. Mycol. 2010, 48, 949–958. [Google Scholar] [CrossRef]
- Merali, S.; Binns, S.; Paulin-Levasseur, M.; Ficker, C.; Smith, M.; Baum, B.; Brovelli, E.; Arnason, J.T. Antifungal and Anti-Inflammatory Activity of the Genus Echinacea. Pharm. Biol. 2003, 41, 412–420. [Google Scholar] [CrossRef]
- Muschietti, L.; Derita, M.; Sülsen, V.; De Dios Muñoz, J.; Ferraro, G.; Zacchino, S.; Martino, V. In Vitro Antifungal Assay of Traditional Argentine Medicinal Plants. J. Ethnopharmacol. 2005, 102, 233–238. [Google Scholar] [CrossRef]
- Fred-Jaiyesimi, A.A.; Abo, K.A. Phytochemical and Antimicrobial Analysis of the Crude Extract, Petroleum Ether and Chloroform Fractions of Euphorbia Heterophylla Linn Whole Plant. Pharmacogn. J. 2010, 2, 1–4. [Google Scholar] [CrossRef]
- Sharma, A.; Angulo-Bejarano, P.; Madariaga-Navarrete, A.; Oza, G.; Iqbal, H.; Cardoso-Taketa, A.; Luisa Villarreal, M. Multidisciplinary Investigations on Galphimia Glauca: A Mexican Medicinal Plant with Pharmacological Potential. Molecules 2018, 23, 2985. [Google Scholar] [CrossRef]
- Alshami, I.; Alharbi, A.E. Hibiscus sabdariffa Extract Inhibits in Vitro Biofilm Formation Capacity of Candida albicans Isolated from Recurrent Urinary Tract Infections. Asian Pac. J. Trop. Biomed. 2014, 4, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Quiroga, E.N.; Sampietro, A.R.; Vattuone, M.A. Screening Antifungal Activities of Selected Medicinal Plants. J. Ethnopharmacol. 2001, 74, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Moreno, M.A.; Córdoba, S.; Zampini, I.C.; Mercado, M.I.; Ponessa, G.; Sayago, J.E.; Ramos, L.L.P.; Schmeda-Hirschmann, G.; Isla, M.I. Argentinean Larrea Dry Extracts with Potential Use in Vaginal Candidiasis. Nat. Prod. Commun. 2018, 13, 1934578X1801300. [Google Scholar] [CrossRef]
- Navarro-García, V.M.; Rojas, G.; Avilés, M.; Fuentes, M.; Zepeda, G. In Vitro Antifungal Activity of Coumarin Extracted from Loeselia Mexicana Brand: Antifungal Coumarins from Loeselia mexicana. Mycoses 2011, 54, e569–e571. [Google Scholar] [CrossRef]
- Morais-Braga, M.F.B.; Souza, T.M.; Santos, K.K.A.; Andrade, J.C.; Guedes, G.M.M.; Tintino, S.R.; Sobral-Souza, C.E.; Costa, J.G.M.; Menezes, I.R.A.; Saraiva, A.A.F.; et al. Antimicrobial and Modulatory Activity of Ethanol Extract of the Leaves from Lygodium venustum SW. Am. Fern J. 2012, 102, 154–160. [Google Scholar] [CrossRef]
- Navarro García, V.M.; Rojas, G.; Gerardo Zepeda, L.; Aviles, M.; Fuentes, M.; Herrera, A.; Jiménez, E. Antifungal and Antibacterial Activity of Four Selected Mexican Medicinal Plants. Pharm. Biol. 2006, 44, 297–300. [Google Scholar] [CrossRef]
- AL-Rubaey, N.K.F.; Abbas, F.M.; Hameed, I.H. Antibacterial and Anti-Fungal Activity of Methanolic Extract of Passiflora caerulea. Indian J. Public Health Res. Dev. 2019, 10, 930. [Google Scholar] [CrossRef]
- Zabka, M.; Pavela, R.; Slezakova, L. Antifungal Effect of Pimenta Dioica Essential Oil against Dangerous Pathogenic and Toxinogenic Fungi. Ind. Crops Prod. 2009, 30, 250–253. [Google Scholar] [CrossRef]
- Derita, M.G.; Leiva, M.L.; Zacchino, S.A. Influence of Plant Part, Season of Collection and Content of the Main Active Constituent, on the Antifungal Properties of Polygonum Acuminatum Kunth. J. Ethnopharmacol. 2009, 124, 377–383. [Google Scholar] [CrossRef]
- Javed, B.; Farooq, F.; Ibrahim, M.; Abbas, H.A.B.; Jawwad, H.; Zehra, S.S.; Ahmad, H.M.; Sarwer, A.; Malik, K.; Nawaz, K. Antibacterial and Antifungal Activity of Methanolic Extracts of Salix alba L. against Various Disease Causing Pathogens. Braz. J. Biol. 2023, 83, e243332. [Google Scholar] [CrossRef] [PubMed]
- Hnatyszyn, O.; Juárez, S.; Ouviña, A.; Martino, V.; Zacchino, S.; Ferraro, G. Phytochemical Analysis and Antifungal Evaluation of Sebastiania commersoniana. Extracts. Pharm. Biol. 2007, 45, 404–406. [Google Scholar] [CrossRef]
- Cáceres, A.; Cruz, S.M.; Martínez, V.; Gaitán, I.; Santizo, A.; Gattuso, S.; Gattuso, M. Ethnobotanical, Pharmacognostical, Pharmacological and Phytochemical Studies on Smilax Domingensis in Guatemala. Rev. Bras. Farmacogn. 2012, 22, 239–248. [Google Scholar] [CrossRef]
- Pinto, E.; Vale-Silva, L.; Cavaleiro, C.; Salgueiro, L. Antifungal Activity of the Clove Essential Oil from Syzygium Aromaticum on Candida, Aspergillus and Dermatophyte Species. J. Med. Microbiol. 2009, 58, 1454–1462. [Google Scholar] [CrossRef]
- Awere, C.A.; Githae, E.W.; Gichumbi, J.M. Phytochemical Analysis and Antifungal Activity of Tithonia diversifolia and Kigelia africana Extracts against Fusarium Oxysporum in Tomato. Afr. J. Agric. Res. 2021, 17, 726–732. [Google Scholar] [CrossRef]
- Simonetti, G.; Brasili, E.; Pasqua, G. Antifungal Activity of Phenolic and Polyphenolic Compounds from Different Matrices of Vitis vinifera L. against Human Pathogens. Molecules 2020, 25, 3748. [Google Scholar] [CrossRef]
- Svetaz, L.; Agüero, M.; Alvarez, S.; Luna, L.; Feresin, G.; Derita, M.; Tapia, A.; Zacchino, S. Antifungal Activity of Zuccagnia Punctata Cav.: Evidence for the Mechanism of Action. Planta Med. 2007, 73, 1074–1080. [Google Scholar] [CrossRef] [PubMed]
- Lefkowitz, E.J.; Dempsey, D.M.; Hendrickson, R.C.; Orton, R.J.; Siddell, S.G.; Smith, D.B. Virus Taxonomy: The Database of the International Committee on Taxonomy of Viruses (ICTV). Nucleic Acids Res. 2018, 46, D708–D717. [Google Scholar] [CrossRef]
- Ben-Shabat, S.; Yarmolinsky, L.; Porat, D.; Dahan, A. Antiviral Effect of Phytochemicals from Medicinal Plants: Applications and Drug Delivery Strategies. Drug Deliv. Transl. Res. 2020, 10, 354–367. [Google Scholar] [CrossRef]
- Cliver, D.O. Capsid and Infectivity in Virus Detection. Food Environ. Virol. 2009, 1, 123–128. [Google Scholar] [CrossRef]
- Jassim, S.A.; Naji, M.A. Novel Antiviral Agents: A Medicinal Plant Perspective. J. Appl. Microbiol. 2003, 95, 412–427. [Google Scholar] [CrossRef]
- Sharma, N. Efficacy of Garlic and Onion against Virus. Int. J. Res. Pharm. Sci. 2019, 10, 3578–3586. [Google Scholar] [CrossRef]
- Hudson, J.; Vimalanathan, S. Echinacea—A Source of Potent Antivirals for Respiratory Virus Infections. Pharmaceuticals 2011, 4, 1019–1031. [Google Scholar] [CrossRef]
- Signer, J.; Jonsdottir, H.R.; Albrich, W.C.; Strasser, M.; Züst, R.; Ryter, S.; Ackermann-Gäumann, R.; Lenz, N.; Siegrist, D.; Suter, A. In Vitro Virucidal Activity of Echinaforce®, an Echinacea purpurea Preparation, against Coronaviruses, Including Common Cold Coronavirus 229E and SARS-CoV-2. Virol. J. 2020, 17, 136. [Google Scholar] [CrossRef]
- Weng, J.-R.; Lin, C.-S.; Lai, H.-C.; Lin, Y.-P.; Wang, C.-Y.; Tsai, Y.-C.; Wu, K.-C.; Huang, S.-H.; Lin, C.-W. Antiviral Activity of Sambucus Formosana Nakai Ethanol Extract and Related Phenolic Acid Constituents against Human Coronavirus NL63. Virus Res. 2019, 273, 197767. [Google Scholar] [CrossRef]
- Chathuranga, K.; Kim, M.S.; Lee, H.-C.; Kim, T.-H.; Kim, J.-H.; Gayan Chathuranga, W.A.; Ekanayaka, P.; Wijerathne, H.; Cho, W.-K.; Kim, H.I. Anti-Respiratory Syncytial Virus Activity of Plantago asiatica and Clerodendrum trichotomum Extracts in Vitro and in Vivo. Viruses 2019, 11, 604. [Google Scholar] [CrossRef]
- Kunsorn, P.; Ruangrungsi, N.; Lipipun, V.; Khanboon, A.; Rungsihirunrat, K. The Identities and Anti-Herpes Simplex Virus Activity of Clinacanthus nutans and Clinacanthus siamensis. Asian Pac. J. Trop. Biomed. 2013, 3, 284–290. [Google Scholar] [CrossRef]
- Chiang, L.C.; Chiang, W.; Chang, M.Y.; Ng, L.T.; Lin, C.C. Antiviral Activity of Plantago major Extracts and Related Compounds in Vitro. Antivir. Res. 2002, 55, 53–62. [Google Scholar] [CrossRef]
- Wahab, N.Z.A.; Bunawan, H.; Ibrahim, N. Cytotoxicity and Antiviral Activity of Methanol Extract from Polygonum minus. In Proceedings of the AIP Conference Proceedings, Selangor, Malaysia, 15–16 April 2015; AIP Publishing: Melville, NY, USA, 2015; Volume 1678. [Google Scholar]
- Zandi, K.; Zadeh, M.A.; Sartavi, K.; Rastian, Z. Antiviral Activity of Aloe vera against Herpes Simplex Virus Type 2: An in Vitro Study. Afr. J. Biotechnol. 2007, 6, 1770–1773. [Google Scholar] [CrossRef]
- van de Sand, L.; Bormann, M.; Schmitz, Y.; Heilingloh, C.S.; Witzke, O.; Krawczyk, A. Antiviral Active Compounds Derived from Natural Sources Against Herpes Simplex Viruses. Viruses 2021, 13, 1386. [Google Scholar] [CrossRef]
- Pilau, M.R.; Alves, S.H.; Weiblen, R.; Arenhart, S.; Cueto, A.P.; Lovato, L.T. Antiviral Activity of the Lippia graveolens (Mexican Oregano) Essential Oil and Its Main Compound Carvacrol against Human and Animal Viruses. Braz. J. Microbiol. 2011, 42, 1616–1624. [Google Scholar] [CrossRef]
- Rajtar, B.; Skalicka-Woźniak, K.; Świątek, Ł.; Stec, A.; Boguszewska, A.; Polz-Dacewicz, M. Antiviral Effect of Compounds Derived from Angelica archangelica L. on Herpes Simplex Virus-1 and Coxsackievirus B3 Infections. Food Chem. Toxicol. 2017, 109, 1026–1031. [Google Scholar] [CrossRef]
- Kurokawa, M.; Hozumi, T.; Basnet, P.; Nakano, M.; Kadota, S.; Namba, T.; Kawana, T.; Shiraki, K. Purification and Characterization of Eugeniin as an Anti-Herpesvirus Compound from Geum Japonicum Andsyzygium Aromaticum. J. Pharmacol. Exp. Ther. 1998, 284, 728–735. [Google Scholar]
- Schnitzler, P.; Schuhmacher, A.; Astani, A.; Reichling, J. Melissa officinalis Oil Affects Infectivity of Enveloped Herpesviruses. Phytomedicine 2008, 15, 734–740. [Google Scholar] [CrossRef]
- Mazzanti, G.; Battinelli, L.; Pompeo, C.; Serrilli, A.M.; Rossi, R.; Sauzullo, I.; Mengoni, F.; Vullo, V. Inhibitory Activity of Melissa officinalis L. Extract on Herpes Simplex Virus Type 2 Replication. Nat. Prod. Res. 2008, 22, 1433–1440. [Google Scholar] [CrossRef]
- Astani, A.; Heidary Navid, M.; Schnitzler, P. Attachment and Penetration of Acyclovir-Resistant Herpes Simplex Virus Are Inhibited by Melissa officinalis Extract. Phytother. Res. 2014, 28, 1547–1552. [Google Scholar] [CrossRef]
- Liu, S.; Li, H.; Chen, L.; Yang, L.; Li, L.; Tao, Y.; Li, W.; Li, Z.; Liu, H.; Tang, M. (-)-Epigallocatechin-3-Gallate Inhibition of Epstein–Barr Virus Spontaneous Lytic Infection Involves ERK1/2 and PI3-K/Akt Signaling in EBV-Positive Cells. Carcinogenesis 2013, 34, 627–637. [Google Scholar] [CrossRef]
- Kapadia, G.J.; Azuine, M.A.; Tokuda, H.; Takasaki, M.; Mukainaka, T.; Konoshima, T.; Nishino, H. Chemopreventive Effect of Resveratrol, Sesamol, Sesame Oil and Sunflower Oil in the Epstein–Barr Virus Early Antigen Activation Assay and the Mouse Skin Two-Stage Carcinogenesis. Pharmacol. Res. 2002, 45, 499–505. [Google Scholar] [CrossRef]
- Konoshima, T.; Takasaki, M.; Kozuka, M.; Tokuda, H.; Nishino, H.; Iwashima, A.; Haruna, M.; Ito, K.; Tanabe, M. Inhibitory Effects on Epstein-Barr Virus Activation and Anti-Tumor Promoting Activities of Neolignans from Magnolia officinalis. Planta Med. 1990, 56, 653. [Google Scholar] [CrossRef]
- Wang, C.; Wang, H.; Zhang, Y.; Guo, W.; Long, C.; Wang, J.; Liu, L.; Sun, X. Berberine Inhibits the Proliferation of Human Nasopharyngeal Carcinoma Cells via an Epstein-Barr Virus Nuclear Antigen 1-Dependent Mechanism. Oncol. Rep. 2017, 37, 2109–2120. [Google Scholar] [CrossRef]
- Hergenhahn, M.; Soto, U.; Weninger, A.; Polack, A.; Hsu, C.-H.; Cheng, A.-L.; Rösl, F. The Chemopreventive Compound Curcumin Is an Efficient Inhibitor of Epstein-Barr Virus BZLF1 Transcription in Raji DR-LUC Cells. Mol. Carcinog. 2002, 33, 137–145. [Google Scholar] [CrossRef]
- Wu, C.-C.; Fang, C.-Y.; Cheng, Y.-J.; Hsu, H.-Y.; Chou, S.-P.; Huang, S.-Y.; Tsai, C.-H.; Chen, J.-Y. Inhibition of Epstein-Barr Virus Reactivation by the Flavonoid Apigenin. J. Biomed. Sci. 2017, 24, 2. [Google Scholar] [CrossRef]
- Lin, J.-C.; Cherng, J.-M.; Hung, M.-S.; Baltina, L.A.; Baltina, L.; Kondratenko, R. Inhibitory Effects of Some Derivatives of Glycyrrhizic Acid against Epstein-Barr Virus Infection: Structure–Activity Relationships. Antivir. Res. 2008, 79, 6–11. [Google Scholar] [CrossRef]
- Wu, C.-C.; Fang, C.-Y.; Hsu, H.-Y.; Chen, Y.-J.; Chou, S.-P.; Huang, S.-Y.; Cheng, Y.-J.; Lin, S.-F.; Chang, Y.; Tsai, C.-H. Luteolin Inhibits Epstein-Barr Virus Lytic Reactivation by Repressing the Promoter Activities of Immediate-Early Genes. Antivir. Res. 2016, 132, 99–110. [Google Scholar] [CrossRef]
- Evers, D.L.; Chao, C.-F.; Wang, X.; Zhang, Z.; Huong, S.-M.; Huang, E.-S. Human Cytomegalovirus-Inhibitory Flavonoids: Studies on Antiviral Activity and Mechanism of Action. Antivir. Res. 2005, 68, 124–134. [Google Scholar] [CrossRef]
- Wang, S.-Y.; Zhang, J.; Xu, X.-G.; Su, H.-L.; Xing, W.-M.; Zhang, Z.-S.; Jin, W.-H.; Dai, J.-H.; Wang, Y.-Z.; He, X.-Y. Inhibitory Effects of Piceatannol on Human Cytomegalovirus (hCMV) in Vitro. J. Microbiol. 2020, 58, 716–723. [Google Scholar] [CrossRef]
- Evers, D.L.; Wang, X.; Huong, S.-M.; Huang, D.Y.; Huang, E.-S. 3,4′,5-Trihydroxy-Trans-Stilbene (Resveratrol) Inhibits Human Cytomegalovirus Replication and Virus-Induced Cellular Signaling. Antivir. Res. 2004, 63, 85–95. [Google Scholar] [CrossRef]
- Zhen, H.; Fang, F.; Ye, D.; Shu, S.; Zhou, Y.; Dong, Y.; Nie, X.; Li, G. Experimental Study on the Action of Allitridin against Human Cytomegalovirus in Vitro: Inhibitory Effects on Immediate-Early Genes. Antivir. Res. 2006, 72, 68–74. [Google Scholar] [CrossRef]
- Abd-Elazem, I.S.; Chen, H.S.; Bates, R.B.; Huang, R.C.C. Isolation of Two Highly Potent and Non-Toxic Inhibitors of Human Immunodeficiency Virus Type 1 (HIV-1) Integrase from Salvia miltiorrhiza. Antivir. Res. 2002, 55, 91–106. [Google Scholar] [CrossRef]
- Locher, C.P.; Witvrouw, M.; De Béthune, M.P.; Burch, M.T.; Mower, H.F.; Davis, H.; Lasure, A.; Pauwels, R.; De Clercq, E.; Vlietinck, A.J. Antiviral Activity of Hawaiian Medicinal Plants against Human Immunodeficiency Virus Type-1 (HIV-1). Phytomed. Int. J. Phytother. Phytopharm. 1996, 2, 259–264. [Google Scholar] [CrossRef]
- Nutan; Modi, M.; Dezzutti, C.S.; Kulshreshtha, S.; Rawat, A.K.S.; Srivastava, S.K.; Malhotra, S.; Verma, A.; Ranga, U.; Gupta, S.K. Extracts from Acacia catechu Suppress HIV-1 Replication by Inhibiting the Activities of the Viral Protease and Tat. Virol. J. 2013, 10, 309. [Google Scholar] [CrossRef]
- Notka, F.; Meier, G.; Wagner, R. Concerted Inhibitory Activities of Phyllanthus Amarus on HIV Replication in Vitro and Ex Vivo. Antivir. Res. 2004, 64, 93–102. [Google Scholar] [CrossRef]
- Lee-Huang, S.; Zhang, L.; Huang, P.L.; Chang, Y.-T.; Huang, P.L. Anti-HIV Activity of Olive Leaf Extract (OLE) and Modulation of Host Cell Gene Expression by HIV-1 Infection and OLE Treatment. Biochem. Biophys. Res. Commun. 2003, 307, 1029–1037. [Google Scholar] [CrossRef]
- Mukhtar, M.; Arshad, M.; Ahmad, M.; Pomerantz, R.J.; Wigdahl, B.; Parveen, Z. Antiviral Potentials of Medicinal Plants. Virus Res. 2008, 131, 111–120. [Google Scholar] [CrossRef]
- Bessong, P.O.; Obi, C.L.; Andréola, M.-L.; Rojas, L.B.; Pouységu, L.; Igumbor, E.; Meyer, J.J.M.; Quideau, S.; Litvak, S. Evaluation of Selected South African Medicinal Plants for Inhibitory Properties against Human Immunodeficiency Virus Type 1 Reverse Transcriptase and Integrase. J. Ethnopharmacol. 2005, 99, 83–91. [Google Scholar] [CrossRef]
- Zhang, X.; Yang, L.-M.; Liu, G.-M.; Liu, Y.-J.; Zheng, C.-B.; Lv, Y.-J.; Li, H.-Z.; Zheng, Y.-T. Potent Anti-HIV Activities and Mechanisms of Action of a Pine Cone Extract from Pinus yunnanensis. Molecules 2012, 17, 6916–6929. [Google Scholar] [CrossRef]
- Kalvatchev, Z.; Walder, R.; Garzaro, D. Anti-HIV Activity of Extracts from Calendula officinalis Flowers. Biomed. Pharmacother. 1997, 51, 176–180. [Google Scholar] [CrossRef]
- Callies, O.; Bedoya, L.M.; Beltrán, M.; Munoz, A.; Calderón, P.O.; Osorio, A.A.; Jiménez, I.A.; Alcami, J.; Bazzocchi, I.L. Isolation, Structural Modification, and HIV Inhibition of Pentacyclic Lupane-Type Triterpenoids from Cassine xylocarpa and Maytenus cuzcoina. J. Nat. Prod. 2015, 78, 1045–1055. [Google Scholar] [CrossRef]
- Hao, B.-J.; Wu, Y.-H.; Wang, J.-G.; Hu, S.-Q.; Keil, D.J.; Hu, H.-J.; Lou, J.-D.; Zhao, Y. Hepatoprotective and Antiviral Properties of Isochlorogenic Acid A from Laggera alata against Hepatitis B Virus Infection. J. Ethnopharmacol. 2012, 144, 190–194. [Google Scholar] [CrossRef]
- Jiang, Z.-Y.; Liu, W.-F.; Zhang, X.-M.; Luo, J.; Ma, Y.-B.; Chen, J.-J. Anti-HBV Active Constituents from Piper longum. Bioorg. Med. Chem. Lett. 2013, 23, 2123–2127. [Google Scholar] [CrossRef]
- Zeng, F.-L.; Xiang, Y.-F.; Liang, Z.-R.; Wang, X.; Huang, D.-E.; Zhu, S.-N.; Li, M.-M.; Yang, D.-P.; Wang, D.-M.; Wang, Y.-F. Anti-Hepatitis B Virus Effects of Dehydrocheilanthifoline from Corydalis saxicola. Am. J. Chin. Med. 2013, 41, 119–130. [Google Scholar] [CrossRef]
- Chiang, L.-C.; Ng, L.T.; Liu, L.-T.; Shieh, D.-E.; Lin, C.-C. Cytotoxicity and Anti-Hepatitis B Virus Activities of Saikosaponins from Bupleurum Species. Planta Med. 2003, 69, 705–709. [Google Scholar] [CrossRef]
- Chiang, L.-C.; Ng, L.-T.; Cheng, P.-W.; Chiang, W.; Lin, C.-C. Antiviral Activities of Extracts and Selected Pure Constituents of Ocimum basilicum. Clin. Exp. Pharmacol. Physiol. 2005, 32, 811–816. [Google Scholar] [CrossRef]
- Rechtman, M.M.; Har-Noy, O.; Bar-Yishay, I.; Fishman, S.; Adamovich, Y.; Shaul, Y.; Halpern, Z.; Shlomai, A. Curcumin Inhibits Hepatitis B Virus via Down-Regulation of the Metabolic Coactivator PGC-1alpha. FEBS Lett. 2010, 584, 2485–2490. [Google Scholar] [CrossRef]
- Ali, S.I.; Sheikh, W.M.; Rather, M.A.; Venkatesalu, V.; Muzamil Bashir, S.; Nabi, S.U. Medicinal Plants: Treasure for Antiviral Drug Discovery. Phytother. Res. PTR 2021, 35, 3447–3483. [Google Scholar] [CrossRef]
- Karamese, M.; Aydogdu, S.; Karamese, S.A.; Altoparlak, U.; Gundogdu, C. Preventive Effects of a Major Component of Green Tea, Epigallocathechin-3-Gallate, on Hepatitis-B Virus DNA Replication. Asian Pac. J. Cancer Prev. 2015, 16, 4199–4202. [Google Scholar] [CrossRef]
- Polyak, S.J.; Morishima, C.; Lohmann, V.; Pal, S.; Lee, D.Y.W.; Liu, Y.; Graf, T.N.; Oberlies, N.H. Identification of Hepatoprotective Flavonolignans from Silymarin. Proc. Natl. Acad. Sci. USA 2010, 107, 5995–5999. [Google Scholar] [CrossRef]
- Kim, K.; Kim, K.H.; Kim, H.Y.; Cho, H.K.; Sakamoto, N.; Cheong, J. Curcumin Inhibits Hepatitis C Virus Replication via Suppressing the Akt-SREBP-1 Pathway. FEBS Lett. 2010, 584, 707–712. [Google Scholar] [CrossRef]
- Calland, N.; Albecka, A.; Belouzard, S.; Wychowski, C.; Duverlie, G.; Descamps, V.; Hober, D.; Dubuisson, J.; Rouillé, Y.; Séron, K. (-)-Epigallocatechin-3-Gallate Is a New Inhibitor of Hepatitis C Virus Entry. Hepatology 2012, 55, 720–729. [Google Scholar] [CrossRef]
- Haid, S.; Novodomská, A.; Gentzsch, J.; Grethe, C.; Geuenich, S.; Bankwitz, D.; Chhatwal, P.; Jannack, B.; Hennebelle, T.; Bailleul, F.; et al. A Plant-Derived Flavonoid Inhibits Entry of All HCV Genotypes into Human Hepatocytes. Gastroenterology 2012, 143, 213–222.e5. [Google Scholar] [CrossRef]
- Meuleman, P.; Albecka, A.; Belouzard, S.; Vercauteren, K.; Verhoye, L.; Wychowski, C.; Leroux-Roels, G.; Palmer, K.E.; Dubuisson, J. Griffithsin Has Antiviral Activity against Hepatitis C Virus. Antimicrob. Agents Chemother. 2011, 55, 5159–5167. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.-T.; Chen, T.-Y.; Lin, S.-C.; Chung, C.-Y.; Lin, T.-C.; Wang, G.-H.; Anderson, R.; Lin, C.-C.; Richardson, C.D. Broad-Spectrum Antiviral Activity of Chebulagic Acid and Punicalagin against Viruses That Use Glycosaminoglycans for Entry. BMC Microbiol. 2013, 13, 187. [Google Scholar] [CrossRef]
- Wahyuni, T.S.; Widyawaruyanti, A.; Lusida, M.I.; Fuad, A.; Soetjipto; Fuchino, H.; Kawahara, N.; Hayashi, Y.; Aoki, C.; Hotta, H. Inhibition of Hepatitis C Virus Replication by Chalepin and Pseudane IX Isolated from Ruta angustifolia Leaves. Fitoterapia 2014, 99, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Shikov, A.N.; Djachuk, G.I.; Sergeev, D.V.; Pozharitskaya, O.N.; Esaulenko, E.V.; Kosman, V.M.; Makarov, V.G. Birch Bark Extract as Therapy for Chronic Hepatitis C–a Pilot Study. Phytomedicine 2011, 18, 807–810. [Google Scholar] [CrossRef] [PubMed]
- Moradi, M.-T.; Karimi, A.; Shahrani, M.; Hashemi, L.; Ghaffari-Goosheh, M.-S. Anti-Influenza Virus Activity and Phenolic Content of Pomegranate (Punica granatum L.) Peel Extract and Fractions. Avicenna J. Med. Biotechnol. 2019, 11, 285–291. [Google Scholar]
- Pantev, A.; Ivancheva, S.; Staneva, L.; Serkedjieva, J. Biologically Active Constituents of a Polyphenol Extract from Geranium sanguineum L. with Anti-Influenza Activity. Z. Naturforschung C J. Biosci. 2006, 61, 508–516. [Google Scholar] [CrossRef] [PubMed]
- Michaelis, M.; Geiler, J.; Naczk, P.; Sithisarn, P.; Ogbomo, H.; Altenbrandt, B.; Leutz, A.; Doerr, H.W.; Cinatl, J. Glycyrrhizin Inhibits Highly Pathogenic H5N1 Influenza A Virus-Induced pro-Inflammatory Cytokine and Chemokine Expression in Human Macrophages. Med. Microbiol. Immunol. 2010, 199, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Sawai, R.; Kuroda, K.; Shibata, T.; Gomyou, R.; Osawa, K.; Shimizu, K. Anti-Influenza Virus Activity of Chaenomeles sinensis. J. Ethnopharmacol. 2008, 118, 108–112. [Google Scholar] [CrossRef]
- Zakay-Rones, Z.; Varsano, N.; Zlotnik, M.; Manor, O.; Regev, L.; Schlesinger, M.; Mumcuoglu, M. Inhibition of Several Strains of Influenza Virus in Vitro and Reduction of Symptoms by an Elderberry Extract (Sambucus nigra L.) during an Outbreak of Influenza B Panama. J. Altern. Complement. Med. 1995, 1, 361–369. [Google Scholar] [CrossRef]
- Liu, G.; Xiong, S.; Xiang, Y.-F.; Guo, C.-W.; Ge, F.; Yang, C.-R.; Zhang, Y.-J.; Wang, Y.-F.; Kitazato, K. Antiviral Activity and Possible Mechanisms of Action of Pentagalloylglucose (PGG) against Influenza A Virus. Arch. Virol. 2011, 156, 1359–1369. [Google Scholar] [CrossRef]
- Song, J.-M.; Lee, K.-H.; Seong, B.-L. Antiviral Effect of Catechins in Green Tea on Influenza Virus. Antivir. Res. 2005, 68, 66–74. [Google Scholar] [CrossRef]
- Hayashi, K.; Narutaki, K.; Nagaoka, Y.; Hayashi, T.; Uesato, S. Therapeutic Effect of Arctiin and Arctigenin in Immunocompetent and Immunocompromised Mice Infected with Influenza A Virus. Biol. Pharm. Bull. 2010, 33, 1199–1205. [Google Scholar] [CrossRef]
- Schapowal, A. Efficacy and Safety of Echinaforce® in Respiratory Tract Infections. Wien. Med. Wochenschr. 1946 2013, 163, 102–105. [Google Scholar] [CrossRef]
- Dall’Acqua, S.; Perissutti, B.; Grabnar, I.; Farra, R.; Comar, M.; Agostinis, C.; Caristi, G.; Golob, S.; Voinovich, D. Pharmacokinetics and Immunomodulatory Effect of Lipophilic Echinacea Extract Formulated in Softgel Capsules. Eur. J. Pharm. Biopharm. 2015, 97, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Rauš, K.; Pleschka, S.; Klein, P.; Schoop, R.; Fisher, P. Effect of an Echinacea-Based Hot Drink versus Oseltamivir in Influenza Treatment: A Randomized, Double-Blind, Double-Dummy, Multicenter, Noninferiority Clinical Trial. Curr. Ther. Res. 2015, 77, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Pourghanbari, G.; Nili, H.; Moattari, A.; Mohammadi, A.; Iraji, A. Antiviral Activity of the Oseltamivir and Melissa officinalis L. Essential Oil against Avian Influenza A Virus (H9N2). Virus Dis. 2016, 27, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Wyde, P.R.; Meyerson, L.R.; Gilbert, B.E. In Vitro Evaluation of the Antiviral Activity of SP-303, an Euphorbiaceae Shrub Extract, against a Panel of Respiratory Viruses. Drug Dev. Res. 1993, 28, 467–472. [Google Scholar] [CrossRef]
- Zou, C.; Liu, H.; Feugang, J.M.; Hao, Z.; Chow, H.-H.S.; Garcia, F. Green Tea Compound in Chemoprevention of Cervical Cancer. Int. J. Gynecol. Cancer Off. J. Int. Gynecol. Cancer Soc. 2010, 20, 617–624. [Google Scholar] [CrossRef]
- Mondal, A.; Chatterji, U. Artemisinin Represses Telomerase Subunits and Induces Apoptosis in HPV-39 Infected Human Cervical Cancer Cells. J. Cell. Biochem. 2015, 116, 1968–1981. [Google Scholar] [CrossRef]
- Yarnell, E. Herbs against Human Papillomavirus. Altern. Complement. Ther. 2015, 21, 71–76. [Google Scholar] [CrossRef]
- Jiang, W.-L.; Luo, X.-L.; Kuang, S.-J. Effects of Alternanthera philoxeroides Griseb against dengue virus in vitro. 1 Jun Yi Xue Xue Bao Acad. J. First Med. Coll. PLA 2005, 25, 454–456. [Google Scholar]
- Salim, F.; Abu, N.A.; Yaakob, H.; Kadir, L.; Zainol, N.; Taher, Z. Interaction of Carica papaya L. Leaves Optimum Extract on Virus Dengue Infected Cells. Sci. Int. 2018, 30, 437–441. [Google Scholar]
- Castillo-Maldonado, I.; Moreno-Altamirano, M.M.B.; Serrano-Gallardo, L.B. Anti-Dengue Serotype-2 Activity Effect of Sambucus nigra Leaves-and Flowers-Derived Compounds. Virol. Res. Rev. 2017, 1, 1–5. [Google Scholar] [CrossRef]
- Chan, Y.S.; Khoo, K.S.; Sit, N.W.W. Investigation of Twenty Selected Medicinal Plants from Malaysia for Anti-Chikungunya Virus Activity. Int. Microbiol. Off. J. Span. Soc. Microbiol. 2016, 19, 175–182. [Google Scholar] [CrossRef]
- Raghavendhar, S.; Tripati, P.K.; Ray, P.; Patel, A.K. Evaluation of Medicinal Herbs for Anti-CHIKV Activity. Virology 2019, 533, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Li, S.-Y.; Chen, C.; Zhang, H.-Q.; Guo, H.-Y.; Wang, H.; Wang, L.; Zhang, X.; Hua, S.-N.; Yu, J.; Xiao, P.-G.; et al. Identification of Natural Compounds with Antiviral Activities against SARS-Associated Coronavirus. Antivir. Res. 2005, 67, 18–23. [Google Scholar] [CrossRef]
- Ho, T.-Y.; Wu, S.-L.; Chen, J.-C.; Li, C.-C.; Hsiang, C.-Y. Emodin Blocks the SARS Coronavirus Spike Protein and Angiotensin-Converting Enzyme 2 Interaction. Antivir. Res. 2007, 74, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Wen, C.-C.; Shyur, L.-F.; Jan, J.-T.; Liang, P.-H.; Kuo, C.-J.; Arulselvan, P.; Wu, J.-B.; Kuo, S.-C.; Yang, N.-S. Traditional Chinese Medicine Herbal Extracts of Cibotium barometz, Gentiana scabra, Dioscorea batatas, Cassia tora, and Taxillus chinensis Inhibit SARS-CoV Replication. J. Tradit. Complement. Med. 2011, 1, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Ulasli, M.; Gurses, S.A.; Bayraktar, R.; Yumrutas, O.; Oztuzcu, S.; Igci, M.; Igci, Y.Z.; Cakmak, E.A.; Arslan, A. The Effects of Nigella sativa (Ns), Anthemis hyalina (Ah) and Citrus sinensis (Cs) Extracts on the Replication of Coronavirus and the Expression of TRP Genes Family. Mol. Biol. Rep. 2014, 41, 1703–1711. [Google Scholar] [CrossRef]
- Lin, C.-W.; Tsai, F.-J.; Tsai, C.-H.; Lai, C.-C.; Wan, L.; Ho, T.-Y.; Hsieh, C.-C.; Chao, P.-D.L. Anti-SARS Coronavirus 3C-like Protease Effects of Isatis Indigotica Root and Plant-Derived Phenolic Compounds. Antivir. Res. 2005, 68, 36–42. [Google Scholar] [CrossRef]
- Ryu, Y.B.; Jeong, H.J.; Kim, J.H.; Kim, Y.M.; Park, J.-Y.; Kim, D.; Nguyen, T.T.H.; Park, S.-J.; Chang, J.S.; Park, K.H.; et al. Biflavonoids from Torreya Nucifera Displaying SARS-CoV 3CL(pro) Inhibition. Bioorg. Med. Chem. 2010, 18, 7940–7947. [Google Scholar] [CrossRef]
- Remali, J.; Aizat, W.M. A Review on Plant Bioactive Compounds and Their Modes of Action Against Coronavirus Infection. Front. Pharmacol. 2020, 11, 589044. [Google Scholar] [CrossRef]
- Huang, T.-J.; Tsai, Y.-C.; Chiang, S.-Y.; Wang, G.-J.; Kuo, Y.-C.; Chang, Y.-C.; Wu, Y.-Y.; Wu, Y.-C. Anti-Viral Effect of a Compound Isolated from Liriope platyphylla against Hepatitis B Virus in Vitro. Virus Res. 2014, 192, 16–24. [Google Scholar] [CrossRef]
- Gansukh, E.; Kazibwe, Z.; Pandurangan, M.; Judy, G.; Kim, D.H. Probing the Impact of Quercetin-7-O-Glucoside on Influenza Virus Replication Influence. Phytomedicine 2016, 23, 958–967. [Google Scholar] [CrossRef]
- Akher, F.B.; Farrokhzadeh, A.; Ramharack, P.; Shunmugam, L.; Van Heerden, F.R.; Soliman, M.E.S. Discovery of Novel Natural Flavonoids as Potent Antiviral Candidates against Hepatitis C Virus NS5B Polymerase. Med. Hypotheses 2019, 132, 109359. [Google Scholar] [CrossRef]
- Sajitha Lulu, S.; Thabitha, A.; Vino, S.; Mohana Priya, A.; Rout, M. Naringenin and Quercetin—Potential Anti-HCV Agents for NS2 Protease Targets. Nat. Prod. Res. 2016, 30, 464–468. [Google Scholar] [CrossRef] [PubMed]
- Moharana, M.; Pattanayak, S.K.; Khan, F. Molecular Recognition of Bio-Active Triterpenoids from Swertia chirayita towards Hepatitis Delta Antigen: A Mechanism through Docking, Dynamics Simulation, Gibbs Free Energy Landscape. J. Biomol. Struct. Dyn. 2023, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Shadrack, D.M.; Deogratias, G.; Kiruri, L.W.; Onoka, I.; Vianney, J.-M.; Swai, H.; Nyandoro, S.S. Luteolin: A Blocker of SARS-CoV-2 Cell Entry Based on Relaxed Complex Scheme, Molecular Dynamics Simulation, and Metadynamics. J. Mol. Model. 2021, 27, 221. [Google Scholar] [CrossRef] [PubMed]
- Abdelli, I.; Hassani, F.; Bekkel Brikci, S.; Ghalem, S. In Silico Study the Inhibition of Angiotensin Converting Enzyme 2 Receptor of COVID-19 by Ammoides verticillata Components Harvested from Western Algeria. J. Biomol. Struct. Dyn. 2021, 39, 3263–3276. [Google Scholar] [CrossRef] [PubMed]
- Kumar Verma, A.; Kumar, V.; Singh, S.; Goswami, B.C.; Camps, I.; Sekar, A.; Yoon, S.; Lee, K.W. Repurposing Potential of Ayurvedic Medicinal Plants Derived Active Principles against SARS-CoV-2 Associated Target Proteins Revealed by Molecular Docking, Molecular Dynamics and MM-PBSA Studies. Biomed. Pharmacother. 2021, 137, 111356. [Google Scholar] [CrossRef] [PubMed]
- Rudrapal, M.; Issahaku, A.R.; Agoni, C.; Bendale, A.R.; Nagar, A.; Soliman, M.E.S.; Lokwani, D. In Silico Screening of Phytopolyphenolics for the Identification of Bioactive Compounds as Novel Protease Inhibitors Effective against SARS-CoV-2. J. Biomol. Struct. Dyn. 2022, 40, 10437–10453. [Google Scholar] [CrossRef] [PubMed]



| Family of Antifungal Drugs | Mechanism of Action | References |
|---|---|---|
| Azoles (fluconazole) | Inhibit fungal cell cytochrome P-450-3-A, disrupting ergosterol synthesis and intoxicating the cell with sterol intermediates. | [72,73,74] |
| Polyene (anfotericine B) | Binds to ergosterol and generates pores in the membrane, causing oxidative damage and cell death. | [72,73] |
| Echinocandins (micafungin) | Inhibit the enzyme 1,3-β-D-glucan synthase, which weakens the cell wall, causing osmotic instability. | [72,73] |
| Allylamines (terbinafine) | Block the enzyme squalene epoxidase, reducing ergosterol levels and increasing squalene. This increases the permeability of the cell. membrane, causing a decrease in fungal growth. | [72] |
| Pyrimidines (flucytosine) | Bind to cytosine permease, already in the nucleus, and generate fluorardilic acid, which is incorporated into the RNA, rendering it useless. | [72,74] |
| Orotomides (olorofim) | Inhibit dihydroorotate dehydrogenase synthesis, preventing the synthesis of DNA and RNA. | [76,77] |
| Fosmanogepix | Inhibits the enzyme Gwt1, responsible for glycosylphosphatidylinositol synthesis. | [75] |
| Species | Extract | Fungi | References |
|---|---|---|---|
| Achyrocline satureioides | Ethanolic | Fusarium verticillioides | [82] |
| Achyrocline tomentosa | Ethanolic | Fusarium verticillioides | [82] |
| Aloysia citriodora | Ethanolic | Fusarium verticillioides | [82] |
| Annona cherimola | Ethanolic | Fusarium oxysporum | [83] |
| Annona muricata L. | Ethanolic | Candida albicans | [84] |
| Aristolochia argentina Griseb. | Ethanolic | Fusarium verticillioides | [82,85] |
| Asclepias curassavica | Hexanic, Methanolic | Candida albicans | [86] |
| Baccharis artemisioides | Ethanolic | Fusarium verticillioides | [82] |
| Baccharis flabellata | Ethanolic | Fusarium verticillioides | [82] |
| Baccharis salicifolia | Ethanolic | Fusarium verticillioides | [82] |
| Bixa orellana | Ethanolic | Candida albicans | [87] |
| Curcuma zedoaria | Acetone, Hexanic | Candida albicans | [88,89] |
| Dalea elegans | Ethanolic | Fusarium verticillioides | [82] |
| Echinacea angustifolia | Ethanolic | Cryptococcus neoformans | [90] |
| Echinacea atrorubens | Ethanolic | Cryptococcus neoformans | [91] |
| Echinacea pallida | Ethanolic | Candida albicans | [91] |
| Echinacea purpurea | Ethanolic | Saccharomyces cerevisiae | [90] |
| Eupatorium buniifolium | Methanolic | Trichophyton mentagrophytes | [92] |
| Euphorbia hyssopifolia | Methanolic | Aspergillus niger | [93] |
| Flourensia oolepis | Ethanolic | Fusarium verticillioides | [82] |
| Gaillardia megapotamica | Ethanolic | Fusarium verticillioides | [82] |
| Galphimia glauca | Hexanic, Methanolic | Trichophyton mentagrophytes | [86,94] |
| Grindelia pulchella | Ethanolic | Fusarium verticillioides | [82] |
| Heterothalamus alienus | Ethanolic | Fusarium verticillioides | [82] |
| Hibiscus sabdariffa | Methanolic | Candida albicans | [95] |
| Kageneckia lanceolata | Ethanolic | Fusarium verticillioides | [82] |
| Larrea cuneifolia | Ethanolic | Lenzites elegans | [96] |
| Larrea divaricata | Ethanolic | Penicillium notatum; Candida spp. | [96,97] |
| Lepechinia floribunda | Ethanolic | Fusarium verticillioides | [82] |
| Lippia turbinata | Ethanolic | Fusarium verticillioides | [82] |
| Loeselia mexicana | Ethanolic | Trichophyton mentagrophytes | [98] |
| Lygodium venustum | Ethanolic | Candida albicans | [99] |
| Lysiloma acapulcensis | Hexanic | Trichophyton mentagrophytes | [100] |
| Miconia mexicana | Methanolic | Candida albicans | [100] |
| Microliabum candidum | Ethanolic | Fusarium verticillioides | [82] |
| Minthostachys verticillata | Ethanolic | Fusarium verticillioides | [82] |
| Morrenia brachystephana | Ethanolic | Fusarium verticillioides | [82] |
| Otholobium higuerilla | Ethanolic | Fusarium verticillioides | [82] |
| Passiflora caerulea | Methanolic | Aspergillus flavus | [101] |
| Pimenta dioica | Essential oil | Fusarium oxysporum | [102] |
| Polygonum acuminatum | Dichloromethane | Cryptococcus neoformans | [103] |
| Salix alba | Methanolic | Aspergillus ornatus | [104] |
| Salvia cuspidata | Ethanolic | Fusarium verticillioides | [82] |
| Sebastiania commersoniana | Ethanolic | Candida spp. | [105] |
| Senecio vira-vira | Ethanolic | Fusarium verticillioides | [82] |
| Smilax domingensis | Ethanolic | Candida albicans | [106] |
| Syzygium aromaticum | Essential oil | Candida spp. | [107] |
| Terminalia triflora | Methanolic | Trichophyton mentagrophytes | [92] |
| Thalictrum decipiens | Ethanolic | Fusarium verticillioides | [82] |
| Tithonia diversifolia | Aquous | Fusarium oxysporum | [108] |
| Trichocline reptans | Ethanolic | Fusarium verticillioides | [82] |
| Vernonia mollisima | Ethanolic | Fusarium verticillioides | [82] |
| Vernonia nudiflora | Ethanolic | Fusarium verticillioides | [82] |
| Vitis vinifera | Aqueous | Candida spp. | [109] |
| Zanthoxylum coco | Ethanolic | Fusarium verticillioides | [82] |
| Zinnia peruviana | Ethanolic | Fusarium oxysporum | [96] |
| Zuccagnia punctata | Ethanolic | Aspergillus niger | [96] |
| Zuccagnia punctata | Dichloromethane | Candida albicans | [110] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuevas-Cianca, S.I.; Romero-Castillo, C.; Gálvez-Romero, J.L.; Sánchez-Arreola, E.; Juárez, Z.N.; Hernández, L.R. Latin American Plants against Microorganisms. Plants 2023, 12, 3997. https://doi.org/10.3390/plants12233997
Cuevas-Cianca SI, Romero-Castillo C, Gálvez-Romero JL, Sánchez-Arreola E, Juárez ZN, Hernández LR. Latin American Plants against Microorganisms. Plants. 2023; 12(23):3997. https://doi.org/10.3390/plants12233997
Chicago/Turabian StyleCuevas-Cianca, Sofía Isabel, Cristian Romero-Castillo, José Luis Gálvez-Romero, Eugenio Sánchez-Arreola, Zaida Nelly Juárez, and Luis Ricardo Hernández. 2023. "Latin American Plants against Microorganisms" Plants 12, no. 23: 3997. https://doi.org/10.3390/plants12233997







