Exploring the Process of Conveying Information about Side Effects: A Qualitative Study among Pharmacists
Abstract
:1. Introduction
2. Experimental Section
2.1. Methodology
2.2. Data Collection and Participants
2.3. Data Analysis
3. Results and Discussion
3.1. Respondents
| Participants | (n) | |
|---|---|---|
| Gender | Female | 22 |
| Male | 11 | |
| Missing data | 2 | |
| Age group (years) | 25–34 | 12 |
| 35–44 | 6 | |
| 45–54 | 8 | |
| 55–64 | 6 | |
| Missing data | 3 | |
| Experience (years) | 5–14 | 13 |
| 15–24 | 8 | |
| 25–34 | 4 | |
| 35–44 | 7 | |
| Missing data | 3 |
3.2. Themes
| Raw data: Examples of quotes | Code | Category | Theme |
|---|---|---|---|
| “Approximately 1 in 100 people who take this medicine will experience diarrhoea. Usually it is not debilitating nor does it last very long.” | Side Effect Probability Side Effect Severity Side Effect Duration | Discussion of Side Effect(s) | Allay fears |
| “CMIs* can scare the patients at times but…” | Empathy | Easing Anxiety | |
| “Hopefully this adverse reaction would not be a problem for you.” | Reassurance | ||
| “Speak with your doctor to see if a different lipid lowering drug would suit you.” | Referral, to encourage use of medication | GP Referral | Minimise harm |
| “If the headache continues for more than a few days, you need to see your GP.” | Referral, to ensure well-being | ||
| “If you get a headache, you can take Panadol.” | Side effect advice | Side Effect Management | |
| “If you experience diarrhoea, ensure you maintain your fluid intake.” | Lifestyle Advice | ||
| “Good cholesterol control reduces your risk of having a heart attack or stroke.” | Medication Benefits | Encourage Use of Medication | Promote medication use |
| “I would suggest starting the medication, giving it a 2 week trial and then…” | Medication Advice |
3.3. Descriptors and Strategies
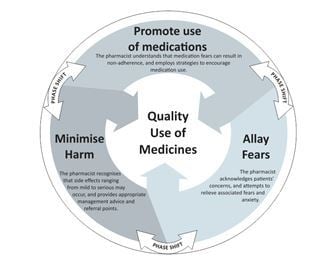
3.4. Emergence of a Theoretical Model for Counselling about Side Effects
| Strategy | Strategy Combinations | Diarrhoea N = 34 | Headache N = 32 |
|---|---|---|---|
| Allay fears | ( single process) | 4 | 3 |
| Allay fears AND minimise harm | 11 | 15 | |
| Allay fears AND promote medication use | 3 | 2 | |
| Allay fears AND minimise harm AND promote medication use | 14 | 8 | |
| Minimise harm | (single process) | 1 | 1 |
| Promote medication use | ( single process) | 0 | 0 |
| Promote medication use AND minimise harm | 1 | 3 |

3.5. Discussion of Findings
3.5.1. Allaying Fears
3.5.2. Descriptors of Side Effects
3.5.3. Strategies for Side Effect Counselling
3.5.4. Limitations
4. Conclusions
Acknowledgments
Conflicts of Interest
References
- Ziegler, D.; Mosier, M.; Buenaver, M.; Okuyemi, L. How Much Information About Adverse Effects of Medication Do Patients Want From Physicians? Arch. Intern. Med. 2001, 161, 706–713. [Google Scholar] [CrossRef]
- Bowskill, R.; Clatworthy, J.; Parham, R.; Rank, T.; Horne, R. Patients’ perceptions of information received about medication prescribed for bipolar disorder: implications for informed choice. J. Affect. Disord. 2007, 100, 253–257. [Google Scholar] [CrossRef]
- Enlund, H.; Vainio, K.; Wallenius, S.; Poston, J.W. Adverse drug effects and the need for drug information. Med. Care 1991, 29, 558–564. [Google Scholar] [CrossRef]
- Nair, K.; Dolovich, L.; Cassels, A.; McCormack, J.; Levine, M.; Gray, J.; Mann, K.; Burns, S. What patients want to know about their medications. Focus group study of patient and clinician perspectives. Can. Fam. Physician. 2002, 48, 104–110. [Google Scholar]
- Tarn, D.M.; Paterniti, D.A.; Williams, B.R.; Cipri, C.S.; Wenger, N.S. Which providers should communicate which critical information about a new medication? Patient, pharmacist, and physician perspectives. J. Am. Geriatr. Soc. 2009, 57, 462–469. [Google Scholar] [CrossRef]
- Bajcar, J. Task analysis of patients' medication-taking practice and the role of making sense: A grounded theory study. Res. Soc. Admin. Pharm. 2006, 2, 59–82. [Google Scholar] [CrossRef]
- Horne, R.; Weinman, J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J. Psychosom. Res. 1999, 47, 555–567. [Google Scholar] [CrossRef]
- Okuyan, B.; Sancar, M.; Izzettin, F.V. Assessment of medication knowledge and adherence among patients under oral chronic medication treatment in community pharmacy settings. Pharmacoepidem. Dr. S. 2013, 22, 209–214. [Google Scholar] [CrossRef]
- McGrath, J.M. Physicians’ perspectives on communicating prescription drug information. Qual. Health Res. 1999, 9, 731–745. [Google Scholar] [CrossRef]
- Schommer, J.; Wiederholt, J. Pharmacists’ views of patient counselling. Am. Pharm. 1994, NS34, 46–53. [Google Scholar]
- Makoul, G.; Arntson, P.; Schofield, T. Health promotion in primary care: physician-patient communication and decision making about precription medications. Soc. Sci. Med. 1995, 41, 1241–1254. [Google Scholar] [CrossRef]
- Berry, D.; Michas, I.; Gillie, T.; Forster, M. What do patients want to know about their medicines, and what do doctors want to tell them?: A comparative study. Psych. Health. 1997, 12, 467–480. [Google Scholar] [CrossRef]
- Mottram, D.R.; Reed, C. Comparative evaluation of patient information leaflets by pharmacists, doctors and the general public. J. Clin. Pharm. Ther. 1997, 22, 127–134. [Google Scholar] [CrossRef]
- Sleath, B.; Wurst, K. Patient receipt of, and preferences for receiving, antidepressant information. Int. J. Pharm. Pract. 2002, 10, 235–241. [Google Scholar] [CrossRef]
- McAuley, J.W.; Miller, M.A.; Klatte, E.; Shneker, B.F. Patients with epilepsy’s perception on community pharmacist’s current and potential role in their care. Epilepsy Behav. 2009, 14, 141–145. [Google Scholar] [CrossRef]
- Wiedenmayer, K.; Summers, R.; Mackie, C.; Gous, A.; Everard, M. Developing pharmacy practice: A focus on patient care. Available online: http://www.fip.org/files/fip/publications/DevelopingPharmacyPractice/DevelopingPharmacyPracticeEN.pdf. (accessed on 10 September 2013).
- Professional Practice Standards version 4: Standard 3: Counselling. Available online: http://www.psa.org.au/supporting-practice/professional-practice-standards/version-4 (accessed on 10 September 2013).
- Barnett, N. Developing your consultation skills to support medicines adherence. Clin. Pharm. 2012, 4, 266–268. [Google Scholar]
- Pilnick, A. “Patient counseling” by pharmacists: Four approaches to the delivery of counselling sequences and their interactional reception. Soc. Sci. Med. 2003, 56, 835–849. [Google Scholar] [CrossRef]
- Dyck, A.; Deschamps, M.; Taylor, J. Pharmacists’ discussions of medication side effects: A descriptive study. Patient Educ. Couns. 2005, 56, 21–27. [Google Scholar] [CrossRef]
- Shah, B.; Chewning, B. Conceptualising and measuring pharmacist-patient communications: A review of published studies. Res. Soc. Admin. Pharm. 2006, 2, 153–185. [Google Scholar] [CrossRef]
- Charmaz, K. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis; Thousand Oaks: California, CA, USA, 2006. [Google Scholar]
- Australian Government Department of Health. PBS Expenditure and Prescriptions: Expenditure and Prescriptions twelve months to 30 June 2012. Available online: http://www.pbs.gov.au/info/statistics/expenditure-and-prescriptions-30-06-2012 (accessed on 21 November 2013).
- Ferrari, A. Headache: One of the most common and troublesome adverse reactions to drugs. Curr. Drug. Saf. 2006, 1, 43–58. [Google Scholar] [CrossRef]
- Triantafyllou, K.; Vlachogiannakos, J.; Ladas, S.D. Gastrointestinal and liver side effects of drugs in elderly patients. Best. Pract. Res. Cl. Ga. 2010, 24, 203–215. [Google Scholar] [CrossRef]
- Pharmacy Board of Australia. Available online: http://www.pharmacyboard.gov.au/Codes-Guidelines.aspx (accessed on 30 October 2013).
- The Society of Hospital Pharmacists of Australia. Available online: http://www.shpa.org.au/About (accessed on 30 October 2013).
- Australian Association of Consultant Pharmacy. Available online: http://www.aacp.com.au/ (accessed on 30 October 2013).
- Corbin, J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory; Thousand Oaks: California, CA, USA, 2008. [Google Scholar]
- Glaser, B.G.; Strauss, A.L. The Discovery of Grounded Theory; Aldine Publishing Company: Chicago, IL, USA, 1967. [Google Scholar]
- Australian Health Practitioner Registration Authority. Pharmacy Board of Australia: Data tables. June 2012. Available online: http://www.ahpra.gov.au (accessed on 10 September 2013).
- Australian Government Deaprtment of Health. Quality Use of Medicines (QUM). Available online: http://www.health.gov.au/internet/main/publishing.nsf/Content/nmp-quality.htm (accessed on 30 October 2013).
- Hargie, O.; Morrow, N.; Woodman, C. Pharmacists’ evaluation of key communication skills in practice. Patient Educ. Couns. 2000, 39, 61–70. [Google Scholar] [CrossRef]
- Kimberlin, C.L. Communicating with patients: Skills assessment in US colleges of pharmacy. Am. J. Pharm. Educ. 2006, 70, 67. [Google Scholar] [CrossRef]
- Blom, L.; Wolters, M.; Hoor-Suykerbuyk, M.T.; van Paassen, J.; van Oyen, A. Pharmaceutical education in patient counselling: 20 h spread over 6 years? Patient Educ. Couns. 2011, 83, 465–471. [Google Scholar] [CrossRef]
- Kokkinn, B.; Stupans, I. Improving pharmacy counseling skills: an interdisciplinary model of support for students with English as an additional language. Int. J. Pharm. Pract. 2011, 19, 435–437. [Google Scholar] [CrossRef]
- Krueger, K.P.; Berger, B.A.; Felkey, B. Medication adherence and persistence: A comprehensive review. Adv. Ther. 2005, 22, 313–356. [Google Scholar] [CrossRef]
- Berry, D.C.; Raynor, D.K.; Knapp, P.; Bersellini, E. Patients’ understanding of risk associated with medication use: Impact of European Commission Guidelines and other risk scales. Drug Safety 2003, 26, 1–11. [Google Scholar] [CrossRef]
- Knapp, P.; Raynor, D.K.; Berry, D.C. Comparison of two methods of presenting risk information to patients about the side effects of medicines. Qual. Saf. Health Care 2004, 13, 176–180. [Google Scholar] [CrossRef]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef]
- Lipkus, I.M. Numeric, verbal, and visual formats of conveying health risks: Suggested best practices and future recommendations. Med. Decis. Making. 2007, 27, 696–713. [Google Scholar] [CrossRef]
- Frankel, R.M.; Stein, T. Getting the most out of the clinic encounter: The Four Habits Model. Perm. J. 1999, 3, 79–88. [Google Scholar]
- McHorney, C.A. The Adherence Estimator: A brief, proximal screener for patient propensity to adhere to prescription medications for chronic disease. Curr. Med. Res. Opin. 2009, 25, 215–238. [Google Scholar] [CrossRef]
- ABC News. Brisbane floods: before and after. Available online: http://www.abc.net.au/news/specials/qld-floods/ (accessed on 30 October 2013).
Appendix
- Tell your doctor if you notice any of the following and if they worry you:
- Constipation, diarrhea
- Unusual tiredness or weakness
- Stomach or belly pain, nausea
- Headache
- Trouble sleeping
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Kairuz, T.; Krehula, D.; Huynh, T.; Bellamy, K. Exploring the Process of Conveying Information about Side Effects: A Qualitative Study among Pharmacists. Pharmacy 2013, 1, 256-268. https://doi.org/10.3390/pharmacy1020256
Kairuz T, Krehula D, Huynh T, Bellamy K. Exploring the Process of Conveying Information about Side Effects: A Qualitative Study among Pharmacists. Pharmacy. 2013; 1(2):256-268. https://doi.org/10.3390/pharmacy1020256
Chicago/Turabian StyleKairuz, Therése, Damir Krehula, Thanh Huynh, and Kim Bellamy. 2013. "Exploring the Process of Conveying Information about Side Effects: A Qualitative Study among Pharmacists" Pharmacy 1, no. 2: 256-268. https://doi.org/10.3390/pharmacy1020256