Introducing Pharmaceutical Care to Primary Care in Iceland—An Action Research Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Setting
2.3. Data Collection and Analysis
2.4. Ethical Approval
3. Results
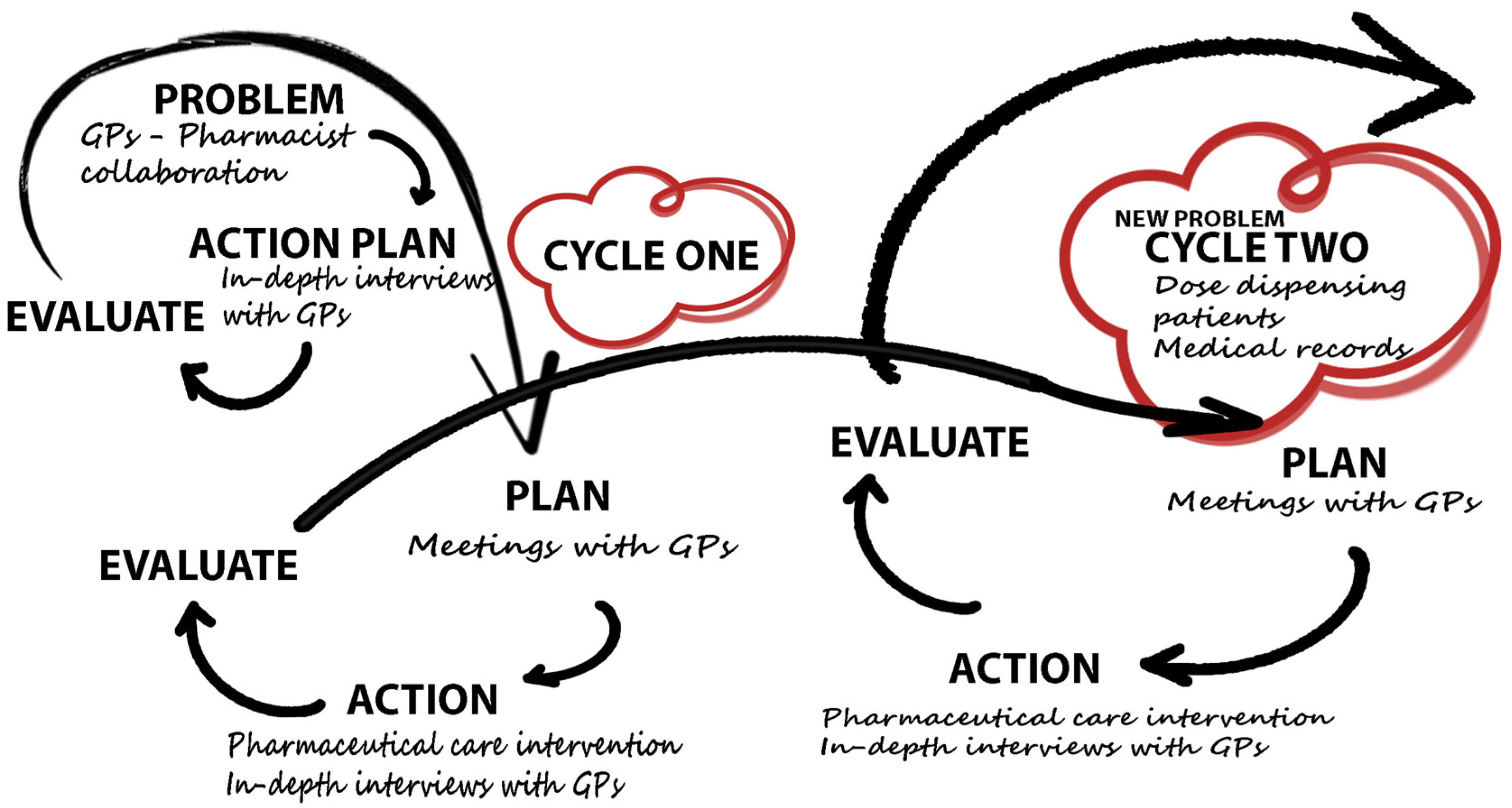
3.1. Description of Action Research Cycles
3.2. Cycle One
3.2.1. Diagnosing the Problem
3.2.2. Plan
3.2.3. Action
3.2.4. Evaluation/Reflection
3.3. Cycle Two
3.3.1. Plan
3.3.2. Action
3.3.3. Evaluation/Reflection
GPs’ view of pharmacists as health care providers:
Pharmacist-led pharmaceutical care:
The future of GP-pharmacist collaboration in Iceland:
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Berenguer, B.; La Casa, C.; de la Matta, M.J.; Martín-Calero, M.J. Pharmaceutical Care: Past, Present and Future. Curr. Pharm. Des. 2004, 10, 3931–3946. [Google Scholar] [CrossRef] [PubMed]
- Hepler, C.D.; Strand, L. Opportunities and Responsibilities in Pharmaceutical Care. Am. J. Hosp. Pharm. 1990, 47, 533–543. [Google Scholar] [PubMed]
- Cipolle, R.J.; Strand, L.; Morley, P. Pharmaceutical Care Practice: The Patient-Centered Approach to Medication Management, 3rd ed.; McGraw-Hill Medical: New York, NY, USA, 2012. [Google Scholar]
- Cipolle, R.J.; Strand, L.; Morley, P.; Cipolle, R. Pharmaceutical Care Practice: The Clinician’s Guide, 2nd ed.; McGraw-Hill Medical: New York, NY, USA, 2004. [Google Scholar]
- Cipolle, R.J.; Morley, P.; Strand, L. Pharmaceutical Care Practice; McGraw-Hill: Manhattan, NY, USA, 1998. [Google Scholar]
- Cipolle, R.J.; Strand, L.; Morley, P. The Global Perspective. In Pharmaceutical Care Practice: The Patient-Centered Approach to Medication Management, 3rd ed.; McGraw-Hill Medical: New York, NY, USA, 2012; pp. 435–644. [Google Scholar]
- Sreelalitha, N.; Vigneshwaran, E.; Narayana, G.; Reddy, Y. Review of Pharmaceutical Care Services Provided by the Pharmacists. Int. Res. J. Pharm. 2012, 3, 78–79. [Google Scholar]
- Patient Centered Primary Care Collaborative. The Patient Centered Medical Home: Integrating Comprehensive Medication Management to Optimize Patient Outcomes. Available online: https://www.pcpcc.org/sites/default/files/media/medmanagement.pdf (accessed on 4 October 2016).
- Chen, T.F. Pharmacist-Led Home Medicines Review and Residential Medication Management Review: The Australian Model. Drugs Aging 2016, 33, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Canadian Society of Hospital Pharmacists. Hospital Pharmacists: Information Paper on Direct Patient Care and Beyond; Canadian Society of Hospital Pharmacists: Ottawa, ON, Canada, 2010. [Google Scholar]
- Al-Quteimat, O.M.; Amer, A.M. Evidence-Based Pharmaceutical Care: The next Chapter in Pharmacy Practice. Saudi Pharm. J. 2016, 24, 447–451. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, M.A.; Moles, R.J.; Chen, T.F. Impact of Pharmaceutical Care Interventions on Health-Related Quality-of-Life Outcomes: A Systematic Review and Meta-Analysis. Ann. Pharmacother. 2016, 50, 862–881. [Google Scholar] [CrossRef] [PubMed]
- Van Mil, J.F.; Schulz, M. A Review of Pharmaceutical Care in Community Pharmacy in Europe. Harv. Health Policy Rev. 2006, 7, 155–168. [Google Scholar]
- Martins, S.F.; van Mil, J.F.; da Costa, F.A. The Organizational Framework of Community Pharmacies in Europe. Int. J. Clin. Pharm. 2015, 37, 896–905. [Google Scholar] [CrossRef] [PubMed]
- Farris, K.B.; Fernandez-Llimos, F.; Benrimoj, S. Pharmaceutical Care in Community Pharmacies: Practice and Research from Around the World. Ann. Pharmacother. 2005, 39, 1539–1541. [Google Scholar] [CrossRef] [PubMed]
- Van Mil, J.F.; de Boer, W.O.; Tromp, T.F.J. European Barriers to the Implementation of Pharmaceutical Care. Int. J. Pharm. Pract. 2001, 9, 163–168. [Google Scholar]
- Uema, S.A.; Vega, E.M.; Armando, P.D.; Fontana, D. Barriers to Pharmaceutical Care in Argentina. Pharm. World Sci. 2008, 30, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Chan, P.; Grindrod, K.A.; Bougher, D.; Pasutto, F.M.; Wilgosh, C.; Eberhart, G.; Tsuyuki, R. A Systematic Review of Remuneration Systems for Clinical Pharmacy Care Services. Can. Pharm. J. 2008, 141, 102–112. [Google Scholar] [CrossRef]
- Almarsdottir, A.B. The Global Perspective: Iceland and Scandinavia. In Pharmaceutical Care Practice: The Patient-Centered Approach to Medication Management, 3rd ed.; Cipolle, R.J., Strand, L., Morley, P.C., Eds.; McGraw-Hill Medical: New York, NY, USA, 2012; pp. 566–580. [Google Scholar]
- Blondal, A.B.; Jonsson, J.S.; Sporrong, S.K.; Almarsdottir, A.B. General Practitioners’ Perceptions of the Current Status and Pharmacists’ Contribution to Primary Care in Iceland. Int. J. Clin. Pharm. 2016. under review. [Google Scholar]
- Nkansah, N.; Mostovetsky, O.; Yu, C.; Chheng, T.; Beney, J.; Bond, C.M.; Bero, L. Effect of Outpatient Pharmacists’ Non-Dispensing Roles on Patient Outcomes and Prescribing Patterns. Cochrane Database Syst. Rev. 2010, 7, CD000336. Available online: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD000336.pub2/pdf/ (accessed on 10 October 2016).
- Geurts, M.M.E.; Talsma, J.; Brouwers, J.R.B.J.; de Gier, J.J. Medication Review and Reconciliation with Cooperation between Pharmacist and General Practitioner and the Benefit for the Patient: A Systematic Review. Br. J. Clin. Pharmacol. 2012, 74, 16–33. [Google Scholar] [CrossRef] [PubMed]
- Tanna, N.K. Action Research: A Valuable Research Technique for Service Delivery Development. Pharm. World Sci. 2005, 27, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Marrow, A.J. The Practical Theorist: The Life and Work of Kurt Lewin. Can. Fam. Physician 1970, 16, 93. [Google Scholar]
- Reason, P.; Bradbury, H. The Sage Handbook of Action Research Participative Inquiry and Practice, 2nd ed.; SAGE Publications: London, UK, 2008. [Google Scholar]
- McNiff, J. Action Research for Professional Development and Experienced, 1st ed.; September Books: Dorset, UK, 2010. [Google Scholar]
- Coghlan, D.; Brannick, T. Doing Action Research in Your Own Organization, 4th ed.; SAGE Publications: London, UK, 2014. [Google Scholar]
- Sigurgeirsdóttir, S.; Waagfjörð, J.; Maresso, A. Iceland: Health System Review. Health Syst. Transit. 2014, 16, 1–182. [Google Scholar] [PubMed]
- Campbell Research and Consulting. Home Medicines Review Program Qualitative Research Project Final Report; Department of Health and Ageing: Canberra, Australia, 2008. [Google Scholar]
- Hsieh, H.-F.; Shannon, S.E. Three Approaches to Qualitative Content Analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Muijrers, P.E.; Knottnerus, J.A.; Sijbrandij, J.; Janknegt, R.; Grol, R.P. Changing Relationships: Attitudes and Opinions of General Practitioners and Pharmacists Regarding the Role of the Community Pharmacist. Pharm. World Sci. 2003, 25, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Howard, M.; Trim, K.; Woodward, C.; Dolovich, L.; Sellors, C.; Kaczorowski, J.; Sellors, J. Collaboration Between Community Pharmacists and Family Physicians: Lessons Learned from the Seniors Medication Assessment Research Trial. J. Am. Pharm. Assoc. 2003, 43, 566–572. [Google Scholar] [CrossRef]
- Bradley, F.; Ashcroft, D.M.; Noyce, P.R. Integration and Differentiation: A Conceptual Model of General Practitioner and Community Pharmacist Collaboration. Res. Soc. Adm. Pharm. 2012, 8, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Kolodziejak, L.; Rémillard, A.; Neubauer, S. Integration of a Primary Healthcare Pharmacist. J. Interprof. Care 2010, 24, 274–284. [Google Scholar] [CrossRef] [PubMed]
- Nancarrow, S.A.; Booth, A.; Ariss, S.; Smith, T.; Enderby, P.; Roots, A. Ten Principles of Good Interdisciplinary Team Work. Hum. Resour. Health 2013, 11, 19. [Google Scholar] [CrossRef] [PubMed]
- Sinnemäki, J.; Sihvo, S.; Isojärvi, J.; Blom, M.; Airaksinen, M.; Mäntylä, A. Automated Dose Dispensing Service for Primary Healthcare Patients: A Systematic Review. Syst. Rev. 2013, 2, 1. [Google Scholar] [CrossRef] [PubMed]
- Bradley, F.; Elvey, R.; Ashcroft, D.M.; Hassell, K.; Kendall, J.; Sibbald, B.; Noyce, P. The Challenge of Integrating Community Pharmacists into the Primary Health Care Team: A Case Study of Local Pharmaceutical Services (LPS) Pilots and Interprofessional Collaboration. J. Interprof. Care 2008, 22, 387–398. [Google Scholar] [CrossRef] [PubMed]
- Dolovich, L.; Pottie, K.; Kaczorowski, J.; Farrell, B.; Austin, Z.; Rodriguez, C.; Gaebel, K.; Sellors, C. Integrating Family Medicine and Pharmacy to Advance Primary Care Therapeutics. Clin. Pharmacol. Ther. 2008, 83, 913–917. [Google Scholar] [CrossRef] [PubMed]
- Isetts, B.J.; Schondelmeyer, S.W.; Artz, M.B.; Lenarz, L.A.; Heaton, A.H.; Wadd, W.B.; Brown, L.M.; Cipolle, R.J. Clinical and Economic Outcomes of Medication Therapy Management Services: The Minnesota Experience. J. Am. Pharm. Assoc. 2008, 2, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Karim, K. Assessing the Strengths and Weaknesses of Action Research. Nurs. Stand. 2001, 15, 33–35. [Google Scholar] [CrossRef] [PubMed]
| Time Period/Cycle Stage | Objective | Process | Output |
|---|---|---|---|
| September to December 2013 Diagnosing the problem cycle one | Understand GPs’ perspective on various issues | Conduct and analysis of the first round of in-depth interview with participant GPs | There are several unmet needs regarding medicines and patient monitoring, and GPs are not familiar with pharmacist clinical service. |
| January 2014 Plan cycle one | Find common ground to move forward with the program from the results | Meeting with participating GPs | GPs are unfamiliar with pharmacist services. It was decided to provide pharmaceutical care to 50 patients and focus on elderly home dwelling polypharmacy patients and then interview GPs immediately after. |
| February to October 2014 Action cycle one | Provide pharmaceutical care and focus on polypharmacy patients | Pharmaceutical care process as defined by Cipolle et al. [3,4,5] | The participating researcher provided pharmaceutical care to 50 elderly home-dwelling patients with no access to medical records. |
| November and December 2014 Action cycle one | Get GPs views on the pharmacist service provided | Conduct of the second round of in-depth interviews with GPs | The second round of in-depth interviews with participating GPs. |
| December 2014 and January 2015 Evaluation/Reflection cycle one | Describe the results from the pharmaceutical care intervention and in-depth interviews | Analysis of the second round of interviews with GPs and research notes | GPs found the pharmaceutical care service useful but that it needed more structure. They found the service most needed in dose dispensing polypharmacy patients. Pharmacist needed medical records and increased contact with GPs to provide proper pharmaceutical care service. |
| January 2015 Plan cycle two | Find common ground to move forward with the program | Meeting with participating GPs | It was decided to provide pharmaceutical care to 50 dose dispensing patients at the primary care clinic with access to medical records and then interview GPs immediately after. |
| February to June 2015 Action cycle two | Provide pharmaceutical care and focus on polypharmacy dose dispensing patients | Pharmaceutical care process as defined by Cipolle et al. [3,4,5] | The participating researcher provided pharmaceutical care to 50 patients. The service was provided at the primary care clinic with access to medical records. |
| June 2015 Action cycle two | Get GPs’ views on the pharmacist service provided | Conduct of the third round of in-depth interviews with GPs | The third round of in-depth interviews with participating GPs. |
| August to October 2015 Evaluation/Reflection cycle two | Describe the result from the pharmaceutical care intervention and in-depth interviews | Analysis of the third round of interviews and research notes | GPs found this second type of intervention to be an improvement and that it gave useful input into clinical decision-making. Direct contact between the pharmacist and GPs is increased when working in the same physical space. Pharmacist’s access to medical records is necessary for optimal care. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blondal, A.B.; Sporrong, S.K.; Almarsdottir, A.B. Introducing Pharmaceutical Care to Primary Care in Iceland—An Action Research Study. Pharmacy 2017, 5, 23. https://doi.org/10.3390/pharmacy5020023
Blondal AB, Sporrong SK, Almarsdottir AB. Introducing Pharmaceutical Care to Primary Care in Iceland—An Action Research Study. Pharmacy. 2017; 5(2):23. https://doi.org/10.3390/pharmacy5020023
Chicago/Turabian StyleBlondal, Anna Bryndis, Sofia Kälvemark Sporrong, and Anna Birna Almarsdottir. 2017. "Introducing Pharmaceutical Care to Primary Care in Iceland—An Action Research Study" Pharmacy 5, no. 2: 23. https://doi.org/10.3390/pharmacy5020023







