Comparison of an In-Person versus a Virtual Interprofessional Education Activity Focused on Professional Communication
Abstract
:1. Introduction
2. Materials and Methods
2.1. Training on TeamSTEPPS Concepts
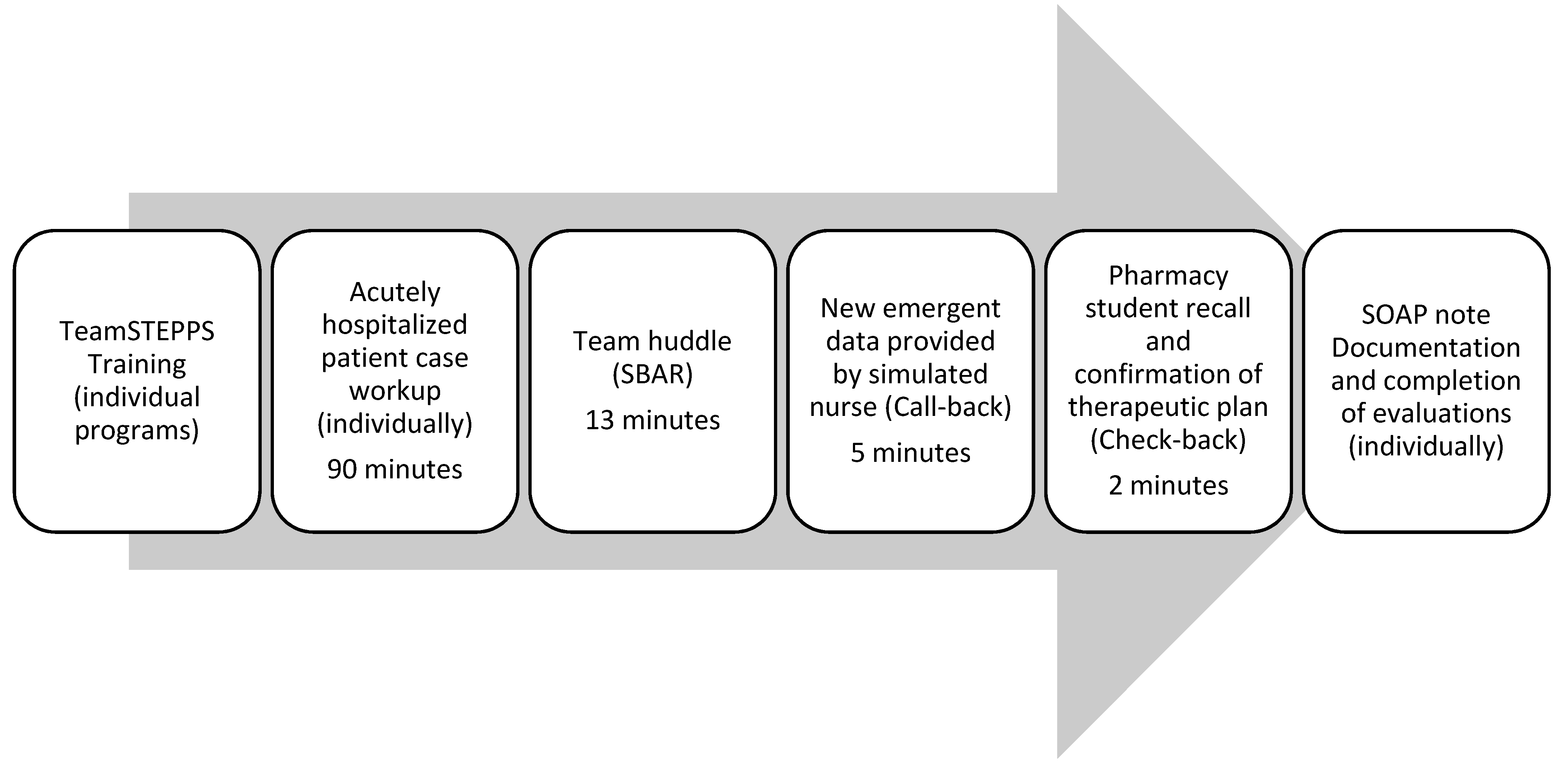
2.2. IPE Activity
2.3. Evaluation
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Interprofessional Education Collaborative Expert Panel. Core Competencies for Interprofessional Collaborative Practice: 2016 Update; Interprofessional Education Collaborative: Washington, DC, USA, 2016. [Google Scholar]
- Institute of Medicine Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century; National Academy Press: Washington, DC, USA, 2001. [Google Scholar]
- Kostoff, M.; Burkhardt, C.; Winter, A.; Shrader, S. An Interprofessional Simulation Using the SBAR Communication Tool. Am. J. Pharm. Educ. 2016, 80, 157. [Google Scholar] [CrossRef] [PubMed]
- Brust-Sisti, L.A.; Sturgill, M.; Volino, L.R. Situation, background, assessment, recommendation (SBAR) technique education enhances pharmacy student communication ability and confidence. Curr. Pharm. Teach. Learn. 2019, 11, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Shrader, S.; Dunn, B.; Blake, E.; Phillips, C. Incorporating Standardized Colleague Simulations in a Clinical Assessment Course and Evaluating the Impact on Interprofessional Communication. Am. J. Pharm. Educ. 2015, 79, 57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barnett, S.; Nagy, M.W.; Hakim, R.C. Integration and assessment of the situation-background-assessment-recommendation framework into a pharmacotherapy skills laboratory for interprofessional communication and documentation. Curr. Pharm. Teach. Learn. 2017, 9, 794–801. [Google Scholar] [CrossRef]
- Thomas, C.M.; Bertram, E.; Johnson, D. The SBAR communication technique: Teaching nursing students professional communication skills. Nurse Educ. 2009, 34, 176–180. [Google Scholar] [CrossRef]
- TeamSTEPPS 2.0. Agency for Healthcare Research and Quality, Rockville, MD. Available online: https://www.ahrq.gov/teamstepps/instructor/index.html (accessed on 10 May 2021).
- Chen, A.S.; Yau, B.; Revere, L.; Swails, J. Implementation, evaluation, and outcome of TeamSTEPPS in interprofessional education: A scoping review. J. Interprof. Care 2019, 33, 795–804. [Google Scholar] [CrossRef] [PubMed]
- Institute for Healthcare Improvement. SBAR Communication Technique. Available online: http://www.ihi.org/explore/SBARCommunicationTechnique/Pages/default.aspx (accessed on 1 July 2017).
- Liaw, S.Y.; Zhou, W.T.; Lau, T.C.; Siau, C.; Chan, S.W.-C. An interprofessional communication training using simulation to enhance safe care for a deteriorating patient. Nurse Educ. Today 2014, 34, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, L.S.; Mohammed, C.A.; Gilbert, J.H. Interprofessional simulation education to enhance teamwork and communication skills among medical and nursing undergraduates using the TeamSTEPPS® framework. Med. J. Armed Forces India 2021, 77 (Suppl. S1), S42–S48. [Google Scholar] [CrossRef] [PubMed]
- Robertson, B.; Kaplan, B.; Atallah, H.; Higgins, M.; Lewitt, M.J.; Ander, D.S. The use of simulation and a modified TeamSTEPPS curriculum for medical and nursing student team training. Simul. Healthc. 2010, 5, 332–337. [Google Scholar] [CrossRef] [PubMed]
- Sherman, E.; Berg, K.; Cooper, D.; Gustitus, R.; Tiernan, C. Does mode matter? Perception of student competence following an IPE communication experience. J. Interprof. Educ. Pract. 2020, 21, 100363. [Google Scholar] [CrossRef]
- Djukic, M.; Adams, J.; Fulmer, T.; Szyld, D.; Lee, S.; Oh, S.-Y.; Triola, M. E-Learning with virtual teammates: A novel approach to interprofessional education. J. Interprof. Care 2015, 29, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Lempicki, K.A.; Holland, C.S. Web-based versus face-to-face interprofessional team encounters with standardized patients. Curr. Pharm. Teach. Learn. 2018, 10, 344–351. [Google Scholar] [CrossRef] [PubMed]
| Rubric Item | 2019 Score Mean (SD) (n = 213) | 2020 Score Mean (SD) (n = 194) |
|---|---|---|
| Accuracy of the clinical information provided by the PA student | 3.67 (0.49) | 3.72 (0.44) |
| Respected your authority and encouraged shared decision making | 3.78 (0.49) | 3.81 (0.4) |
| Used appropriate medical terminology | 3.79 (0.4) | 3.81 (0.4) |
| Engaged in consultation | 3.76 (0.47) | 3.79 (0.4) |
| Appeared confident when questioned on his/her recommendation | 3.71 (0.49) | 3.77 (0.43) |
| Accurately resolved any questions that you had | 3.70 (0.5) | 3.79 (0.4) |
| Ability to convince you to change the patient’s medication plan | 3.61 (0.55) | 3.76 (0.47) * |
| Rubric Item | 2019 Score Mean (SD) (n = 45) | 2020 Score Mean (SD) (n = 45) |
|---|---|---|
| The pharmacy student described the situation (S) to you (the provider) | 3.44 (0.77) | 3.62 (0.66) * |
| The pharmacy student provided background (B) to familiarize you (provider) with the patient | 3.46 (0.75) | 3.61 (0.63) * |
| The pharmacy student provided his/her own assessment (A) of the patient | 3.54 (0.7) | 3.61 (0.61) |
| The pharmacy student provided a recommendation (R) for managing the patient | 3.59 (0.6) | 3.66 (0.52) |
| Accuracy of the clinical recommendation | 3.48 (0.67) | 3.52 (0.61) |
| The pharmacy student respected your authority and encouraged shared decision making | 3.65 (0.6) | 3.82 (0.4) * |
| Used appropriate medical terminology | 3.62 (0.6) | 3.78 (0.4) * |
| The pharmacy student was engaged in the consultation | 3.64 (0.6) | 3.79 (0.4) |
| Maintained eye contact | 3.58 (0.64) | 3.65 (0.6) |
| Appeared confident when questioned on his/her recommendation | 3.40 (0.8) | 3.49 (0.7) |
| Accurately resolved your questions | 3.46 (0.7) | 3.68 (0.5) * |
| Was the pharmacy student able to convince you to change the patient’s medication regimen? | 3.50 (0.7) | 3.69 (0.5) * |
| How did the pharmacy student grade him/herself? | 3.14 (0.6) | 3.22 (0.6) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
DelNero, T.; Vyas, D. Comparison of an In-Person versus a Virtual Interprofessional Education Activity Focused on Professional Communication. Pharmacy 2021, 9, 111. https://doi.org/10.3390/pharmacy9020111
DelNero T, Vyas D. Comparison of an In-Person versus a Virtual Interprofessional Education Activity Focused on Professional Communication. Pharmacy. 2021; 9(2):111. https://doi.org/10.3390/pharmacy9020111
Chicago/Turabian StyleDelNero, Tracey, and Deepti Vyas. 2021. "Comparison of an In-Person versus a Virtual Interprofessional Education Activity Focused on Professional Communication" Pharmacy 9, no. 2: 111. https://doi.org/10.3390/pharmacy9020111






