Factors Affecting the Severity of Placental Abruption in Pregnant Vehicle Drivers: Analysis with a Novel Finite Element Model
Abstract
:1. Introduction
2. Materials and Methods
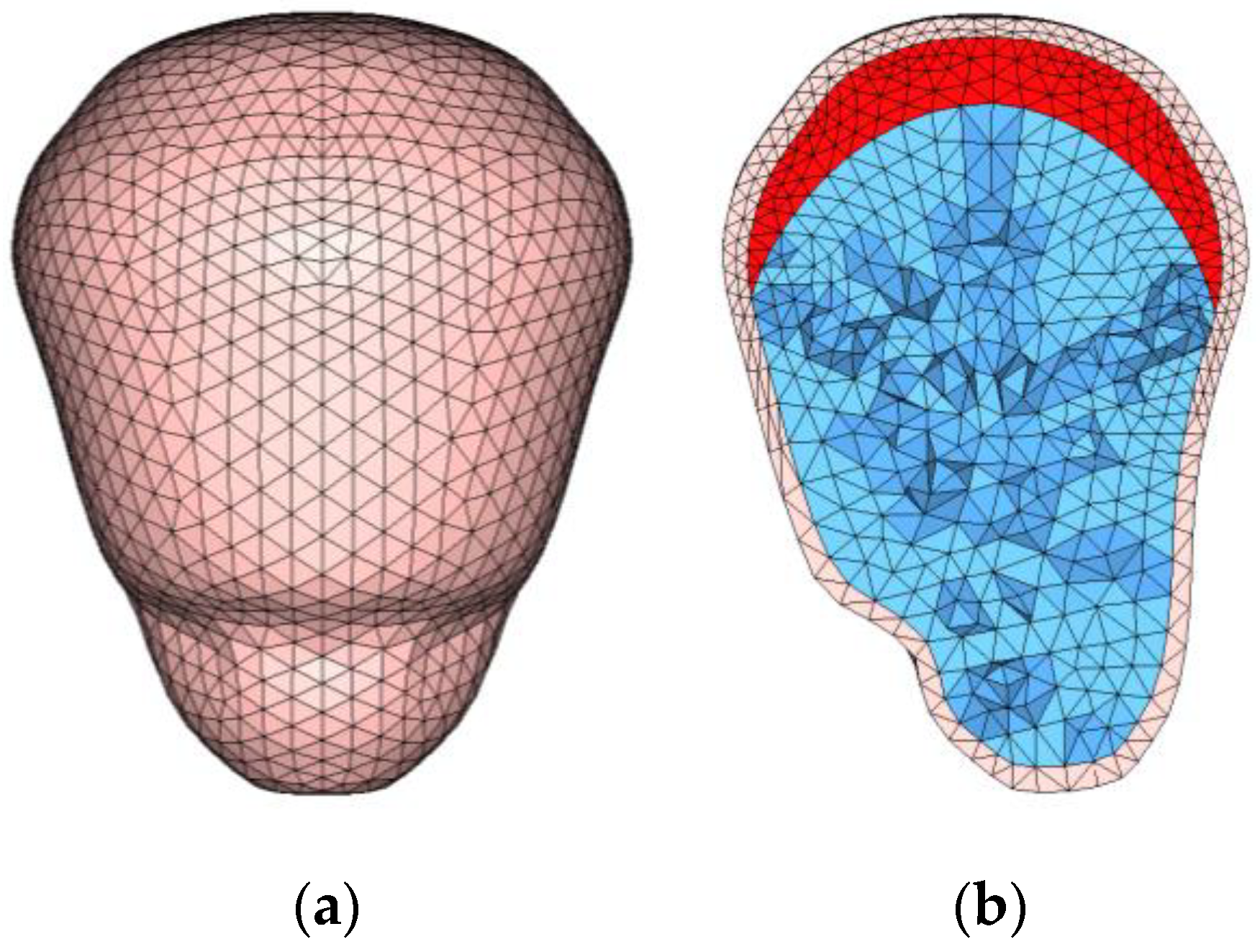
2.1. FE Model of a Pregnant Woman
2.2. Impact Simulation
3. Results
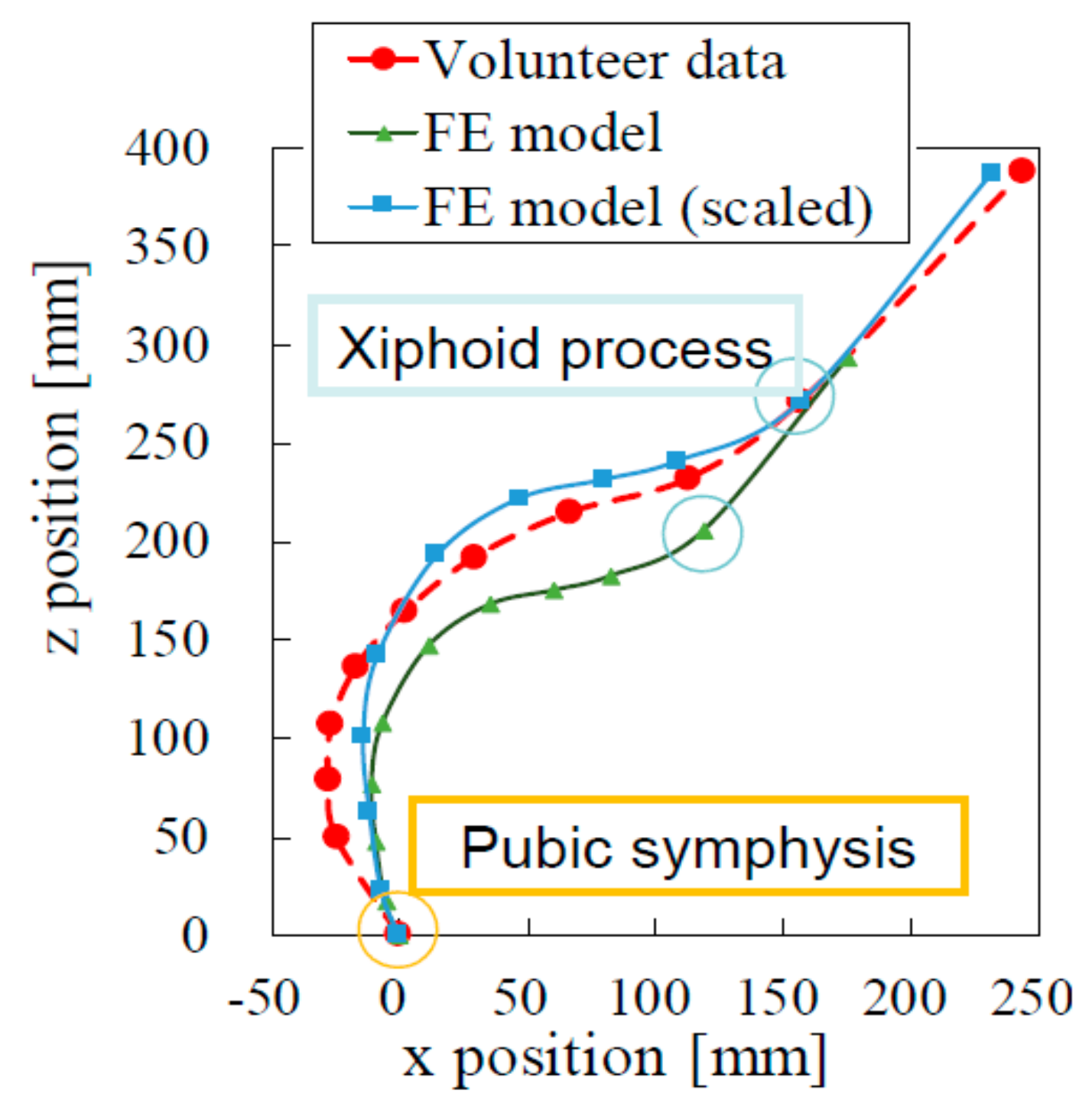
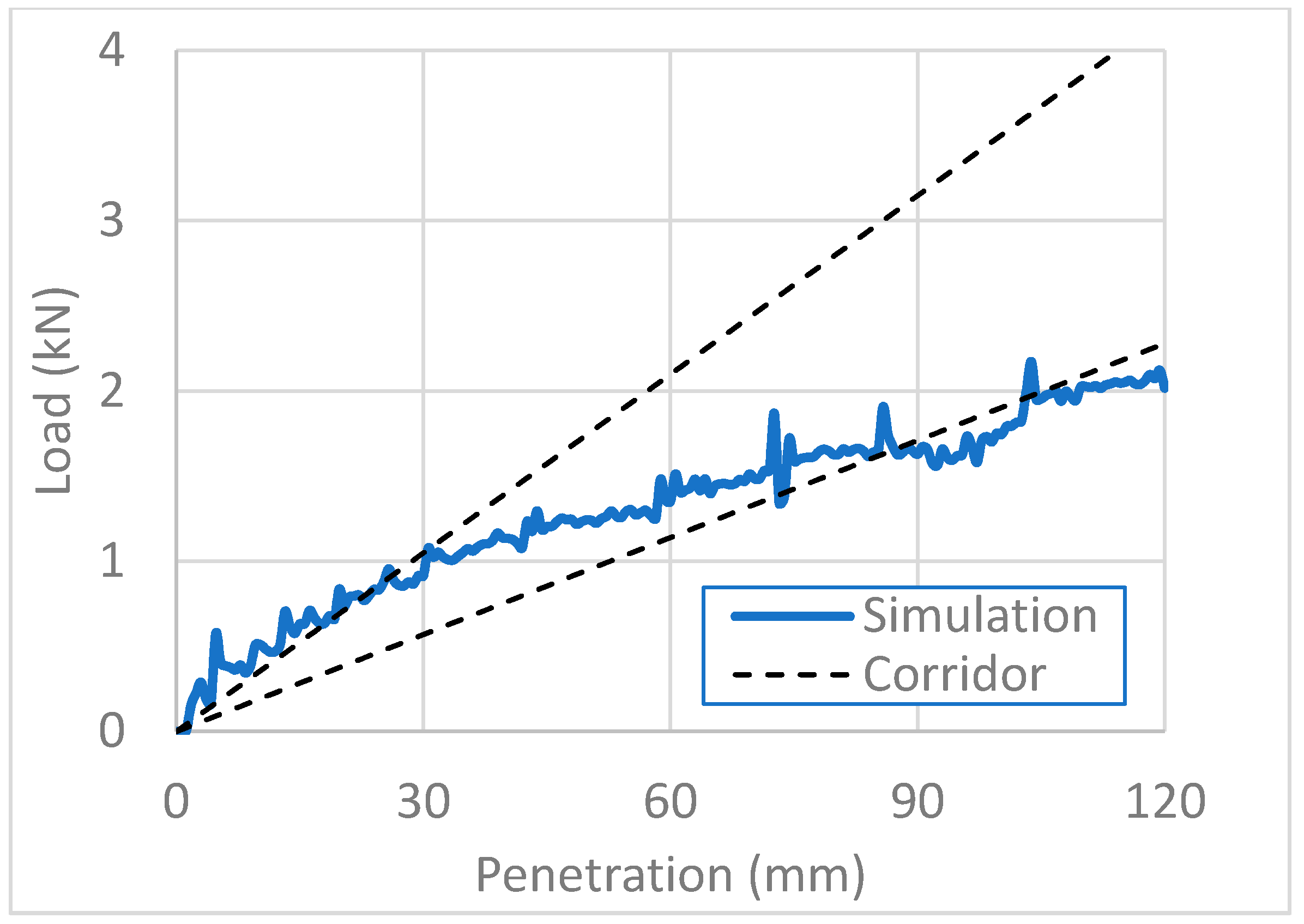
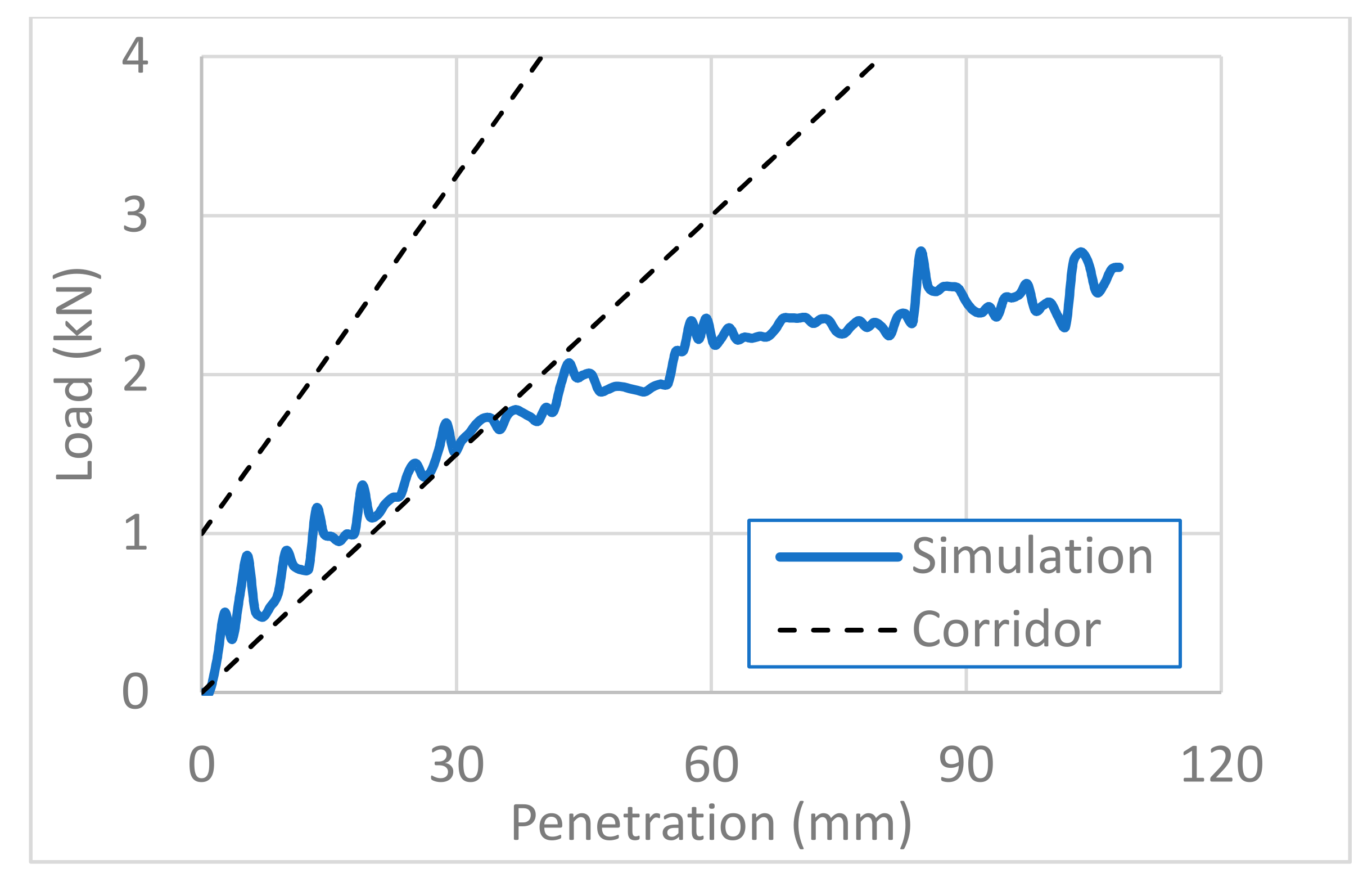
3.1. Validation of the Model
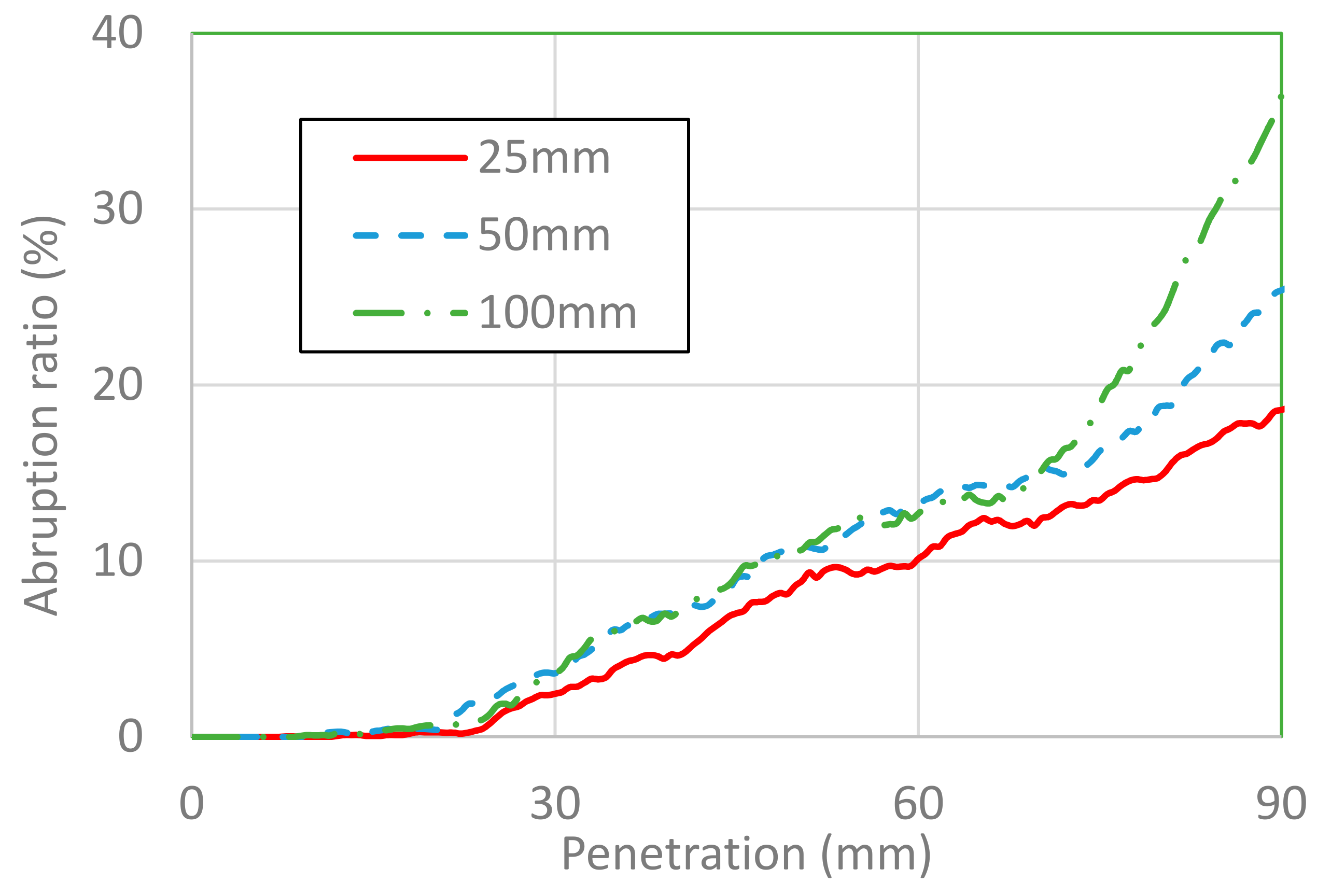
3.2. Placental Abruption Area
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Status Report on Road Safety. Available online: https://www.who.int/publications/i/item/global-status-report-on-road-safety-2018 (accessed on 6 September 2020).
- The United Nations. World Fertility Report. Available online: https://www.un.org/en/development/desa/population/publications/fertility/world-fertility-2015.asp (accessed on 6 September 2020).
- Mendez-Figueroa, H.; Dahlke, J.D.; Vrees, R.A.; Rouse, D.J. Trauma in pregnancy: An updated systematic review. Am. J. Obstet. Gynecol. 2013, 209, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hyde, L.K. Effect of motor vehicle crashes on adverse fetal outcomes. Obstet. Gynecol. 2003, 102, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Schiff, M.; Albers, L.; McFeeley, P. Motor vehicle crashes and maternal mortality in New Mexico: The significance of seat belt use. West. J. Med. 1997, 167, 19–22. [Google Scholar] [PubMed]
- Morikawa, M.; Yamada, T.; Kato-Hirayama, E.; Nishikawa, A.; Watari, M.; Maeda, N.; Kogo, H.; Minakami, H. Seatbelt use and seat preference among pregnant women in Sapporo, Japan. J. Obstet. Gynaecol. Res. 2016, 42, 810–815. [Google Scholar] [CrossRef] [PubMed]
- El Kady, D.; Gilbert, W.M.; Anderson, J.; Danielsen, B.; Towner, D.; Smith, L.H. Trauma during pregnancy: An analysis of maternal and fetal outcomes in a large population. Am. J. Obstet. Gynecol. 2004, 190, 1661–1668. [Google Scholar] [CrossRef] [PubMed]
- Schiff, M.A.; Holt, V.L. Pregnancy Outcomes following Hospitalization for Motor Vehicle Crashes in Washington State from 1989 to 2001. Am. J. Epidemiol. 2005, 161, 503–510. [Google Scholar] [CrossRef]
- Griffiths, M. Pregnant women should wear seat belts. BMJ 1995, 311, 1501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klinich, K.; Flannagan, C.A.; Rupp, J.; Sochor, M.; Schneider, L.W.; Pearlman, M.D. Fetal outcome in motor-vehicle crashes: Effects of crash characteristics and maternal restraint. Am. J. Obstet. Gynecol. 2008, 198, 450.e1–450.e9. [Google Scholar] [CrossRef]
- Hattori, S.; Hitosugi, M.; Moriguchi, S.; Baba, M.; Takaso, M.; Nakamura, M.; Tsujimura, S.; Miyata, Y. Factors Influencing Pregnant Women’s Injuries and Fetal Loss Due to Motor Vehicle Collisions: A National Crash Data-Based Study. Healthcare 2021, 9, 273. [Google Scholar] [CrossRef] [PubMed]
- Koh, S.; Hitosugi, M.; Moriguchi, S.; Baba, M.; Tsujimura, S.; Takeda, A.; Takaso, M.; Nakamura, M. Comparison of Motor Vehicle Collision Injuries between Pregnant and Non-Pregnant Women: A Nationwide Collision Data-Based Study. Healthcare 2021, 9, 1414. [Google Scholar] [CrossRef]
- Rupp, J.D.; Klinich, K.D.; Moss, S.; Zhou, J.; Pearlman, M.D.; Schneider, L.W. Development and Testing of a Prototype Pregnant Abdomen for the Small-Female Hybrid III ATD. Stapp Car Crash J. 2001, 45, 61–78. [Google Scholar] [CrossRef] [PubMed]
- Motozawa, Y.; Hitosugi, M.; Abe, T.; Tokudome, S. Effects of seat belts worn by pregnant drivers during low-impact collisions. Am. J. Obstet. Gynecol. 2010, 203, 62.e1–62.e8. [Google Scholar] [CrossRef] [PubMed]
- Takeda, A.; Motozawa, Y.; Takaso, M.; Nakamura, M.; Hattori, S.; Hitosugi, M. Mechanisms of Negative Fetal Outcome in Frontal Vehicle Colli-Sions Involving Unbelted Pregnant Drivers. Healthcare 2020, 9, 25. [Google Scholar] [CrossRef]
- Pearlman, M.D.; Tintinalli, J.E.; Lorenz, R.P. A prospective controlled study of outcome after trauma during pregnancy. Am. J. Obstet. Gynecol. 1990, 162, 1502–1510. [Google Scholar] [CrossRef]
- Dave, D.D.; Jha, B.K. 3D mathematical modeling of calcium signaling in Alzheimer’s disease. Netw. Model. Anal. Health Inform. Bioinform. 2019, 9, 9. [Google Scholar] [CrossRef]
- Dave, D.D.; Jha, B.K. On finite element estimation of calcium advection diffusion in a multipolar neuron. J. Eng. Math. 2021, 128, 1–15. [Google Scholar] [CrossRef]
- Naik, P.A. Modeling the mechanics of calcium regulation in T lymphocyte: A finite element method approach. Int. J. Biomath. 2020, 13, 2050038. [Google Scholar] [CrossRef]
- Kumar, H.; Naik, P.A.; Pardasani, K.R. Finite Element Model to Study Calcium Distribution in T Lymphocyte Involving Buffers and Ryanodine Receptors. Proc. Natl. Acad. Sci. India Sect. A Phys. Sci. 2018, 88, 585–590. [Google Scholar] [CrossRef]
- Moorcroft, D.M.; Stitzel, J.D.; Duma, G.G.; Duma, S.M. Computational model of the pregnant occupant: Predicting the risk of injury in automobile crashes. Am. J. Obstet. Gynecol. 2003, 189, 540–544. [Google Scholar] [CrossRef]
- Auriault, F.; Thollon, L.; Pérès, J.; Behr, M. Adverse fetal outcome in road accidents: Injury mechanism study and injury criteria development in a pregnant woman finite element model. Accid. Anal. Prev. 2016, 97, 96–102. [Google Scholar] [CrossRef]
- Auriault, F.; Thollon, L.; Peres, J.; Delotte, J.; Kayvantash, K.; Brunet, C.; Behr, M. Virtual traumatology of pregnant women: The PRegnant car Occupant Model for Impact Simulations (PROMIS). J. Biomech. 2014, 47, 207–213. [Google Scholar] [CrossRef]
- Page, E.W.; King, E.B.; A Merrill, J. Abruptio placentae; dangers of delay in delivery. Obstet. Gynecol. 1954, 3, 385–393. [Google Scholar] [PubMed]
- Ananth, C.V.; Berkowitz, G.S.; Savitz, D.A.; Lapinski, R.H. Placental Abruption and Adverse Perinatal Outcomes. JAMA 1999, 282, 1646–1651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delotte, J.; Behr, M.; Thollon, L.; Bongain, A.; Brunet, C. Does placenta position modify the risk of placental abruption in car crashes? Comput. Methods Biomech. Biomed. Eng. 2009, 12, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Loftis, K.; Halsey, M.; Anthony, E.; Duma, S.M.; Stitzel, J. Pregnant female anthropometry from ct scans for finite element model development. Biomed. Sci. Instrum. 2008, 44, 355–360. [Google Scholar]
- Manoogian, S.J. Protecting the Pregnant Occupant: Dynamic Material Properties of Uterus and Placenta. Ph.D. Dissertation, Virginia Polytechnic Institute and State University, Blacksburg, Virginia, 29 May 2008. [Google Scholar]
- Sivarao, S.; Vidyadaran, M.; Jammal, A.; Zainab, S.; Goh, Y.; Ramesh, K. Weight, Volume and Surface Area of Placenta of Normal Pregnant Women and their Relation to Maternal and Neonatal Parameters in Malay, Chinese and Indian Ethnic Groups. Placenta 2002, 23, 691–696. [Google Scholar] [CrossRef]
- Acar, B.S.; Meric, M.; Acar, M. The effect of including a fetus in the uterus model on the risk of fetus mortality through drop test and frontal crash simulations. Int. J. Crashworthiness 2016, 21, 452–459. [Google Scholar] [CrossRef] [Green Version]
- Rupp, J.D.; Schneider, L.W.; Klinich, K.D. Design, Development and Testing of a New Pregnant Abdomen for the Hybrid III Small Female Crash Test Dummy; University of Michigan Transportation Research Institute: Ann Arbor, MI, USA, 2001. [Google Scholar]
- Klinich, K.D.; Schneider, L.W.; Eby, B.; Rupp, J.; Pearlman, M.D. Seated Anthropometry During Pregnancy; University of Michigan Medical School: Ann Arbor, MI, USA, 1999. [Google Scholar]
- Hardy, W.N.; Schneider, L.W.; Rouhana, S.W. Abdominal Impact Response to Rigid-Bar, Seatbelt, and Airbag Loading. SAE Tech. Paper Ser. 2001, 45, 1–32. [Google Scholar] [CrossRef]
- Ishiko, A.; Hitosugi, M.; Takaso, M.; Mizuno, K.; Tsuji, S.; Ono, T.; Kimura, F.; Murakami, T. Chest compression of a pregnant woman by a seatbelt might affect fetal outcome, even in minor to moderate frontal vehicle collisions. Forensic Sci. Int. 2019, 302, 109888. [Google Scholar] [CrossRef]
- Richardson, J.D. Changes in the Management of Injuries to the Liver and Spleen. J. Am. Coll. Surg. 2005, 200, 648–669. [Google Scholar] [CrossRef]
- Afifi, I.; Abayazeed, S.; El-Menyar, A.; Abdelrahman, H.; Peralta, R.; Al-Thani, H. Blunt liver trauma: A descriptive analysis from a level I trauma center. BMC Surg. 2018, 18, 42. [Google Scholar] [CrossRef] [PubMed]
- Kaptanoglu, L.; Kurt, N.; Sikar, H.E. Current approach to liver traumas. Int. J. Surg. 2017, 39, 255–259. [Google Scholar] [CrossRef] [PubMed]





| Tissues | Specific Gravity (kg/m3) | Young’s Modulus (kPa) | Poisson Coefficient |
|---|---|---|---|
| Uterine wall | 1006 | 467 | 0.49 |
| Placenta | 1006 | 38 | 0.49 |
| Amniotic fluid | 1000 | 2 | 0.49 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanaka, K.; Motozawa, Y.; Takahashi, K.; Maki, T.; Hitosugi, M. Factors Affecting the Severity of Placental Abruption in Pregnant Vehicle Drivers: Analysis with a Novel Finite Element Model. Healthcare 2022, 10, 27. https://doi.org/10.3390/healthcare10010027
Tanaka K, Motozawa Y, Takahashi K, Maki T, Hitosugi M. Factors Affecting the Severity of Placental Abruption in Pregnant Vehicle Drivers: Analysis with a Novel Finite Element Model. Healthcare. 2022; 10(1):27. https://doi.org/10.3390/healthcare10010027
Chicago/Turabian StyleTanaka, Katsunori, Yasuki Motozawa, Kentaro Takahashi, Tetsuo Maki, and Masahito Hitosugi. 2022. "Factors Affecting the Severity of Placental Abruption in Pregnant Vehicle Drivers: Analysis with a Novel Finite Element Model" Healthcare 10, no. 1: 27. https://doi.org/10.3390/healthcare10010027






