Effect of Acupuncture on Recovery of Consciousness in Patients with Acute Traumatic Brain Injury: A Multi-Institutional Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Study Design
2.3. Covariates
2.4. Outcome
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics of TBI Patients Receiving/Not Receiving Acupuncture
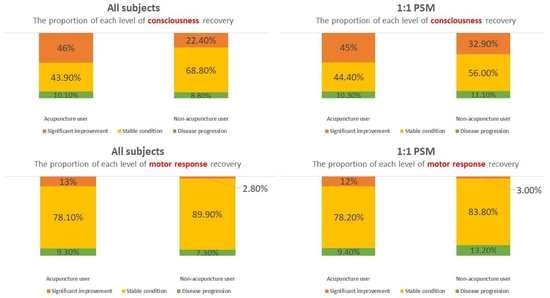
3.2. Acupuncture Significantly Improves the Disturbance of Consciousness in TBI Patients
3.3. Acupuncture Significantly Enhances the Motor Function Response in TBI Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Eapen, B.C.; Allred, D.B.; O’Rourke, J.; Cifu, D.X. Rehabilitation of moderate-to-severe traumatic brain injury. Semin. Neurol. 2015, 35, e1–e3. [Google Scholar] [CrossRef]
- Wright, D.W.; Kellermann, A.; McGuire, L.C.; Chen, B.; Popovic, T. CDC grand rounds: Reducing severe traumatic brain injury in the United States. Morb. Mortal. Wkly. Rep. 2013, 62, 549–552. [Google Scholar] [CrossRef]
- Capizzi, A.; Woo, J.; Verduzco-Gutierrez, M. Traumatic Brain Injury: An Overview of Epidemiology, Pathophysiology, and Medical Management. Med. Clin. N. Am. 2020, 104, 213–238. [Google Scholar] [CrossRef] [PubMed]
- Stocchetti, N.; Carbonara, M.; Citerio, G.; Ercole, A.; Skrifvars, M.B.; Smielewski, P.; Zoerle, T.; Menon, D.K. Severe traumatic brain injury: Targeted management in the intensive care unit. Lancet Neurol. 2017, 16, 452–464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christensen, J.; Pedersen, M.G.; Pedersen, C.B.; Sidenius, P.; Olsen, J.; Vestergaard, M. Long-term risk of epilepsy after traumatic brain injury in children and young adults: A population-based cohort study. Lancet 2009, 373, 1105–1110. [Google Scholar] [CrossRef] [PubMed]
- Dikmen, S.S.; Corrigan, J.D.; Levin, H.S.; Machamer, J.; Stiers, W.; Weisskopf, M.G. Cognitive Outcome Following Traumatic Brain Injury. J. Head Trauma Rehabil. 2009, 24, 430–438. [Google Scholar] [CrossRef] [PubMed]
- Løvstad, M.; Andelic, N.; Knoph, R.; Jerstad, T.; Anke, A.; Skandsen, T.; Hauger, S.L.; Giacino, J.T.; Røe, C.; Schanke, A.K. Rate of disorders of consciousness in a prospective population-based study of adults with traumatic brain injury. J. Head Trauma Rehabil. 2014, 29, E31–E43. [Google Scholar] [CrossRef]
- Andriessen, T.M.; Horn, J.; Franschman, G.; van der Naalt, J.; Haitsma, I.; Jacobs, B.; Steyerberg, E.W.; Vos, P.E. Epidemiology, severity classification, and outcome of moderate and severe traumatic brain injury: A prospective multicenter study. J. Neurotrauma 2011, 28, 2019–2031. [Google Scholar] [CrossRef]
- Boly, M.; Massimini, M.; Garrido, M.I.; Gosseries, O.; Noirhomme, Q.; Laureys, S.; Soddu, A. Brain connectivity in disorders of consciousness. Brain Connect. 2012, 2, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Teasdale, G.; Jennett, B. Assessment of coma and impaired consciousness. A practical scale. Lancet 1974, 2, 81–84. [Google Scholar] [CrossRef]
- Bodien, Y.G.; Barra, A.; Temkin, N.R.; Barber, J.; Foreman, B.; Vassar, M.; Robertson, C.; Taylor, S.R.; Markowitz, A.J.; Manley, G.T.; et al. Diagnosing Level of Consciousness: The Limits of the Glasgow Coma Scale Total Score. J. Neurotrauma 2021, 38, 3295–3305. [Google Scholar] [CrossRef] [PubMed]
- Abdelmalik, P.A.; Draghic, N.; Ling, G.S.F. Management of moderate and severe traumatic brain injury. Transfusion 2019, 59, 1529–1538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pignat, J.M.; Jöhr, J.; Diserens, K. From disorders of consciousness to early neurorehabilitation using assistive technologies in patients with severe brain damage. Curr. Opin. Neurol. 2015, 28, 587–594. [Google Scholar] [CrossRef] [PubMed]
- Galgano, M.; Toshkezi, G.; Qiu, X.; Russell, T.; Chin, L.; Zhao, L.R. Traumatic Brain Injury: Current Treatment Strategies and Future Endeavors. Cell Transplant. 2017, 26, 1118–1130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magee, W.L.; Narayanan, A.; O’Connor, R.; Haughey, F.; Wegener, E.; Chu, B.H.L.; Delargy, M.; Gray, D.; Seu, A.D.; Siegert, R.J.; et al. Validation of the Music Therapy Assessment Tool for Awareness in Disorders of Consciousness With the Coma Recovery Scale-Revised. Arch. Phys. Med. Rehabil. 2023, 104, 1107–1114. [Google Scholar] [CrossRef] [PubMed]
- Upchurch, D.M.; Rainisch, B.W. A sociobehavioral wellness model of acupuncture use in the United States, 2007. J. Altern. Complement. Med. 2014, 20, 32–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gau, B.S.; Yang, H.L.; Huang, S.J.; Lou, M.F. The use of complementary and alternative medicine for patients with traumatic brain injury in Taiwan. BMC Complement. Altern. Med. 2012, 12, 211. [Google Scholar] [CrossRef] [Green Version]
- Shih, C.C.; Lin, J.G.; Liao, C.C.; Su, Y.C. The utilization of traditional Chinese medicine and associated factors in Taiwan in 2002. Chin. Med. J. 2009, 122, 1544–1548. [Google Scholar]
- Wong, V.; Cheuk, D.K.; Lee, S.; Chu, V. Acupuncture for acute management and rehabilitation of traumatic brain injury. Cochrane Database Syst. Rev. 2013, 28, CD007700. [Google Scholar] [CrossRef]
- Tan, L.; Zeng, L.; Wang, N.; Deng, M.; Chen, Y.; Ma, T.; Zhang, L.; Xu, Z. Acupuncture to Promote Recovery of Disorder of Consciousness after Traumatic Brain Injury: A Systematic Review and Meta-Analysis. Evid. Based Complement. Altern. Med. 2019, 2019, 5190515. [Google Scholar] [CrossRef] [Green Version]
- Cai, G.; Zhuang, Z.; Jia, K.; Xu, S.; Wang, X.; Pei, S.; Sun, M.; Cui, C.; Guo, S.; Xu, K.; et al. Effects of cross electro-nape-acupuncture (CENA) on recovery of consciousness and tracheotomy tube sealing in serious cerebral hemorrhage. Am. J. Transl. Res. 2022, 14, 1868–1876. [Google Scholar]
- Li, L.; Wang, X.; Guo, J.; Chen, Y.; Wang, Z. Effect of acupuncture in the acute phase of intracerebral hemorrhage on the prognosis and serum BDNF: A randomized controlled trial. Front. Neurosci. 2023, 17, 1167620. [Google Scholar] [CrossRef] [PubMed]
- Shao, S.C.; Chan, Y.Y.; Yang, Y.H.K.; Lin, S.J.; Hung, M.J.; Chien, R.N.; Lai, C.C.; Lai, E. The Chang Gung Research Database-A multi-institutional electronic medical records database for real-world epidemiological studies in Taiwan. Pharmacoepidemiol. Drug Saf. 2019, 28, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Shao, S.C.; Lai, E.C.; Huang, T.H.; Hung, M.J.; Tsai, M.S.; Yang, Y.H.; Chan, Y.Y. The Chang Gung Research Database: Multi-institutional real-world data source for traditional Chinese medicine in Taiwan. Pharmacoepidemiol. Drug Saf. 2021, 30, 652–660. [Google Scholar] [CrossRef]
- Chen, S.L.; Lin, W.C.; Chen, Y.C.; Chen, J.L.; Wu, Y.H.; Yang, S.H.; Chen, H.Y. The association between mortality and use of Chinese herbal medicine among incident stage IV esophageal cancer patients: A retrospective cohort study with core herbs exploration. Front. Pharmacol. 2022, 13, 1018281. [Google Scholar] [CrossRef]
- De Crescenzo, L.A.; Gabella, B.A.; Johnson, J. Interrupted time series design to evaluate ICD-9-CM to ICD-10-CM coding changes on trends in Colorado emergency department visits related to traumatic brain injury. Inj. Epidemiol. 2021, 8, 15. [Google Scholar] [CrossRef] [PubMed]
- Juan, Y.H.; Livneh, H.; Huang, H.J.; Lu, M.C.; Yeh, C.C.; Tsai, T.Y. Decreased Risk of Dementia Among Patients With Traumatic Brain Injury Receiving Acupuncture Treatment: A Population-Based Retrospective Cohort Study. J. Head Trauma Rehabil. 2019, 34, E17–E23. [Google Scholar] [CrossRef]
- Shih, C.C.; Lee, H.H.; Chen, T.L.; Tsai, C.C.; Lane, H.L.; Chiu, W.T.; Liao, C.C. Reduced use of emergency care and hospitalization in patients with traumatic brain injury receiving acupuncture treatment. Evid. Based Complement. Altern. Med. 2013, 2013, 262039. [Google Scholar] [CrossRef] [Green Version]
- Shih, C.C.; Hsu, Y.T.; Wang, H.H.; Chen, T.L.; Tsai, C.C.; Lane, H.L.; Yeh, C.C.; Sung, F.C.; Chiu, W.T.; Cherng, Y.G.; et al. Decreased risk of stroke in patients with traumatic brain injury receiving acupuncture treatment: A population-based retrospective cohort study. PLoS ONE 2014, 9, e89208. [Google Scholar] [CrossRef]
- Yeh, C.C.; Chen, T.L.; Hu, C.J.; Chiu, W.T.; Liao, C.C. Risk of epilepsy after traumatic brain injury: A retrospective population-based cohort study. J. Neurol. Neurosurg. Psychiatry 2013, 84, 441–445. [Google Scholar] [CrossRef]
- Livernoche Leduc, C.; Roy, S.J.; Paradis, V.; Potvin, M.J. Cognitive profiles in the acute phase of traumatic brain injury according to injury severity. Appl. Neuropsychol. Adult 2022, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Mollayeva, T.; Mollayeva, S.; Colantonio, A. Traumatic brain injury: Sex, gender and intersecting vulnerabilities. Nat. Rev. Neurol. 2018, 14, 711–722. [Google Scholar] [CrossRef] [PubMed]
- de la Plata, C.D.M.; Hart, T.; Hammond, F.M.; Frol, A.B.; Hudak, A.; Harper, C.R.; O’Neil-Pirozzi, T.M.; Whyte, J.; Carlile, M.; Diaz-Arrastia, R. Impact of age on long-term recovery from traumatic brain injury. Arch. Phys. Med. Rehabil. 2008, 89, 896–903. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, J.Y.; Gao, G.Y.; Li, W.P.; Yu, M.K.; Zhu, C. Early indicators of prognosis in 846 cases of severe traumatic brain injury. J. Neurotrauma 2002, 19, 869–874. [Google Scholar] [CrossRef]
- Izzy, S.; Chen, P.M.; Tahir, Z.; Grashow, R.; Radmanesh, F.; Cote, D.J.; Yahya, T.; Dhand, A.; Taylor, H.; Shih, S.L.; et al. Association of Traumatic Brain Injury With the Risk of Developing Chronic Cardiovascular, Endocrine, Neurological, and Psychiatric Disorders. JAMA Netw. Open 2022, 5, e229478. [Google Scholar] [CrossRef] [PubMed]
- Zhong, X.; Shan, A.; Xu, J.; Liang, J.; Long, Y.; Du, B. Hyperbaric oxygen for severe traumatic brain injury: A randomized trial. J. Int. Med. Res. 2020, 48, 300060520939824. [Google Scholar] [CrossRef] [PubMed]
- Ross, S.E.; Leipold, C.; Terregino, C.; O’Malley, K.F. Efficacy of the motor component of the Glasgow Coma Scale in trauma triage. J. Trauma 1998, 45, 42–44. [Google Scholar] [CrossRef] [Green Version]
- Kupas, D.F.; Melnychuk, E.M.; Young, A.J. Glasgow Coma Scale Motor Component (“Patient Does Not Follow Commands”) Performs Similarly to Total Glasgow Coma Scale in Predicting Severe Injury in Trauma Patients. Ann. Emerg. Med. 2016, 68, 744–750.e743. [Google Scholar] [CrossRef] [Green Version]
- Kowalski, R.G.; Hammond, F.M.; Weintraub, A.H.; Nakase-Richardson, R.; Zafonte, R.D.; Whyte, J.; Giacino, J.T. Recovery of Consciousness and Functional Outcome in Moderate and Severe Traumatic Brain Injury. JAMA Neurol. 2021, 78, 548–557. [Google Scholar] [CrossRef]
- Jang, S.H.; Kwon, Y.H. The relationship between consciousness and the ascending reticular activating system in patients with traumatic brain injury. BMC Neurol. 2020, 20, 375. [Google Scholar] [CrossRef]
- Park, J.Y.; Cho, S.J.; Lee, S.H.; Ryu, Y.; Jang, J.H.; Kim, S.N.; Park, H.J. Peripheral ERK modulates acupuncture-induced brain neural activity and its functional connectivity. Sci. Rep. 2021, 11, 5128. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Lu, C.; Wu, X.; Nie, D.; Yu, H. Neuroplasticity of Acupuncture for Stroke: An Evidence-Based Review of MRI. Neural Plast. 2021, 2021, 2662585. [Google Scholar] [CrossRef] [PubMed]
- Tang, W.C.; Hsu, Y.C.; Wang, C.C.; Hu, C.Y.; Chio, C.C.; Kuo, J.R. Early electroacupuncture treatment ameliorates neuroinflammation in rats with traumatic brain injury. BMC Complement. Altern. Med. 2016, 16, 470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.S.; Yao, C.H.; Chen, T.H.; Lin, J.G.; Hsieh, C.L.; Lin, C.C.; Lao, C.J.; Tsai, C.C. Effect of acupuncture stimulation on peripheral nerve regeneration using silicone rubber chambers. Am. J. Chin. Med. 2001, 29, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Lan, R.; Wang, J.; Li, X.Y.; Zhu, D.N.; Ma, Y.Z.; Wu, J.T.; Liu, Z.H. Acupuncture reduced apoptosis and up-regulated BDNF and GDNF expression in hippocampus following hypoxia-ischemia in neonatal rats. J. Ethnopharmacol. 2015, 172, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Hu, R.; Zhong, X.; Zhang, A.; Pang, B.; Sun, X.; Zhu, G. Electric Acupuncture Treatment Promotes Angiogenesis in Rats with Middle Cerebral Artery Occlusion Through EphB4/EphrinB2 Mediated Src/PI3K Signal Pathway. J. Stroke Cerebrovasc. Dis. 2021, 30, 105165. [Google Scholar] [CrossRef] [PubMed]
- Zou, R.; Wu, Z.; Cui, S. Electroacupuncture pretreatment attenuates blood-brain barrier disruption following cerebral ischemia/reperfusion. Mol. Med. Report. 2015, 12, 2027–2034. [Google Scholar] [CrossRef] [Green Version]

| Non-Acupuncture (n = 1926) | Acupuncture (n = 237) | p-Value | |
|---|---|---|---|
| Gender, n (%) | 0.076 | ||
| Male | 1313 (68.2) | 175 (73.8) | |
| Female | 613 (31.8) | 62 (26.2) | |
| Age, M (IQR), year | 54 (38) | 57 (32) | 0.417 |
| <50 | 861 (44.7) | 92 (38.8) | 0.085 |
| ≥50 | 1065 (55.3) | 145 (61.2) | |
| Initial GCS, M (IQR), score | 14 (4) | 11 (5) | <0.001 * |
| Initial GCS subgroups #, n (%) | |||
| Mild (13–15) | 1278 (66.4) | 96 (40.5) | <0.001 * |
| Moderate (9–12) | 465 (24.1) | 89 (37.6) | <0.001 * |
| Severe (3–8) | 183 (9.5) | 52 (21.9) | <0.001 * |
| TBI types, n (%) | |||
| Skull fracture | 789 (41.0) | 55 (23.2) | <0.001 * |
| Brain contusion | 92 (4.8) | 16 (6.8) | 0.188 |
| SAH | 520 (27.0) | 72 (30.4) | 0.271 |
| SDH | 724 (37.6) | 110 (46.4) | 0.008 * |
| EDH | 171 (8.9) | 21 (8.9) | 0.993 |
| ICH | 438 (22.7) | 91 (38.4) | <0.001 * |
| Other | 68 (3.5) | 8 (3.4) | 0.903 |
| Co-morbidities, n (%) | |||
| Hypertension | 306 (15.9) | 53 (22.4) | 0.011 * |
| Diabetes mellitus | 173 (9.0) | 31 (13.1) | 0.042 * |
| Hyperlipidemia | 26 (1.4) | 6 (2.5) | 0.153 |
| Coronary artery disease | 423 (22.0) | 68 (28.7) | 0.020 * |
| Stroke | 423 (22.0) | 68 (28.7) | 0.020 * |
| Dementia | 15 (0.8) | 2 (0.8) | 0.709 |
| Mental disease | 3 (0.2) | 0 (0.0) | 1.000 |
| Parkinsonism | 4 (0.2) | 0 (0.0) | 1.000 |
| Non-Acupuncture (n = 234) | Acupuncture (n = 234) | p-Value | |
|---|---|---|---|
| Gender, n (%) | 0.106 | ||
| Male | 156 (66.7) | 172 (73.5) | |
| Female | 78 (33.3) | 62 (26.5) | |
| Age, M (IQR), year | 55 (36) | 57 (32) | 0.661 |
| <50 | 92 (39.3) | 91 (38.9) | 0.925 |
| ≥50 | 142 (60.7) | 143 (61.1) | |
| Initial GCS, M (IQR), score | 12 (5) | 11 (5) | 0.787 |
| Initial GCS subgroups #, n (%) | |||
| Mild (13–15) | 101 (43.2) | 96 (41.0) | 0.640 |
| Moderate (9–12) | 78 (33.3) | 89 (38.0) | 0.289 |
| Severe (3–8) | 55 (23.5) | 49 (20.9) | 0.505 |
| TBI types, n (%) | |||
| Skull fracture | 48 (20.5) | 55 (23.5) | 0.435 |
| Brain contusion | 8 (3.4) | 16 (6.8) | 0.094 |
| SAH | 78 (33.3) | 71 (30.3) | 0.487 |
| SDH | 111 (47.4) | 108 (46.2) | 0.781 |
| EDH | 27 (11.5) | 21 (9.0) | 0.361 |
| ICH | 93 (39.7) | 88 (37.6) | 0.635 |
| Other | 9 (3.9) | 8 (3.4) | 0.805 |
| Co-morbidities, n (%) | |||
| Hypertension | 43 (18.4) | 51 (21.8) | 0.356 |
| Diabetes mellitus | 27 (11.5) | 29 (12.4) | 0.776 |
| Hyperlipidemia | 2 (0.9) | 6 (2.6) | 0.285 |
| Coronary artery disease | 59 (25.2) | 66 (28.2) | 0.465 |
| Stroke | 59 (25.2) | 66 (28.2) | 0.465 |
| Dementia | 2 (0.9) | 2 (0.9) | 1.000 |
| Mental disease | 1 (0.4) | 0 (0.0) | 1.000 |
| Parkinsonism | 1 (0.4) | 0 (0.0) | 1.000 |
| All Subjects | p-Value | 1:1 PSM | p-Value | |||
|---|---|---|---|---|---|---|
| Non-Acupuncture (n = 1926) | Acupuncture (n = 237) | Non-Acupuncture (n = 234) | Acupuncture (n = 234) | |||
| Significant improvement, n (%) | 432 (22.4) | 109 (46.0) | <0.001 * | 77 (32.9) | 106 (45.3) | 0.020 * |
| Stable condition, n (%) | 1325 (68.8) | 104 (43.9) | 131 (56.0) | 104 (44.4) | ||
| Disease progression, n (%) | 169 (8.8) | 24 (10.1) | 26 (11.1) | 24 (10.3) | ||
| All Subjects | 1:1 PSM | |||||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | aOR (95% CI) | p-Value | OR (95% CI) | p-Value | aOR (95% CI) | p-Value | |
| Non-acupuncture | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | ||||
| Acupuncture | 2.95 (2.23–3.86) | < 0.001 * | 2.01 (1.39–2.90) # | < 0.001 * | 1.69 (1.16–2.46) | 0.006 | 2.11 (1.31–3.40) † | 0.002 * |
| OR (95% CI) | p-Value | aOR (95% CI) | p-Value | |
|---|---|---|---|---|
| Gender † | ||||
| Male | 2.43 (1.75–3.36) | <0.001 * | 1.72 (1.12–2.64) | 0.013 * |
| Female | 4.89 (2.85–8.37) | <0.001 * | 3.67 (1.68–8.04) | 0.001 * |
| Age, years ‡ | ||||
| <50 | 4.85 (3.11–7.56) | <0.001 * | 3.76 (2.01–7.05) | <0.001 * |
| ≥50 | 2.11 (1.47–3.03) | <0.001 * | 1.38 (0.87–2.18) | 0.171 |
| Initial GCS subgroups § | ||||
| Severe (3–10) | 1.56 (0.92–2.63) | 0.009 * | 1.63 (0.93–2.87) | 0.088 |
| Mild (11–15) | 2.59 (1.64–4.09) | <0.001 * | 2.05 (1.27–3.32) | 0.004 * |
| All Subjects | p-Value | 1:1 PSM | p-Value | |||
|---|---|---|---|---|---|---|
| Non-Acupuncture (n = 1926) | Acupuncture (n = 237) | Non-Acupuncture (n = 234) | Acupuncture (n = 234) | |||
| Significant improvement, n (%) | 54 (2.8%) | 30 (12.7) | <0.001 * | 7 (3.0) | 29 (12.4) | <0.001 * |
| Stable condition, n (%) | 1731 (89.9) | 185 (78.1) | 196 (83.8) | 183 (78.2) | ||
| Disease progression, n (%) | 141 (7.3) | 22 (9.3) | 31 (13.2) | 22 (9.4) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, C.-C.; Chen, H.-Y.; Tseng, C.-Y.; Yang, C.-C. Effect of Acupuncture on Recovery of Consciousness in Patients with Acute Traumatic Brain Injury: A Multi-Institutional Cohort Study. Healthcare 2023, 11, 2267. https://doi.org/10.3390/healthcare11162267
Lin C-C, Chen H-Y, Tseng C-Y, Yang C-C. Effect of Acupuncture on Recovery of Consciousness in Patients with Acute Traumatic Brain Injury: A Multi-Institutional Cohort Study. Healthcare. 2023; 11(16):2267. https://doi.org/10.3390/healthcare11162267
Chicago/Turabian StyleLin, Chun-Chieh, Hsing-Yu Chen, Chu-Yao Tseng, and Chien-Chung Yang. 2023. "Effect of Acupuncture on Recovery of Consciousness in Patients with Acute Traumatic Brain Injury: A Multi-Institutional Cohort Study" Healthcare 11, no. 16: 2267. https://doi.org/10.3390/healthcare11162267