Designing and Developing a Mobile Smartphone Application for Women with Gestational Diabetes Mellitus Followed-Up at Diabetes Outpatient Clinics in Norway
Abstract
:1. Introduction
2. Experimental Section
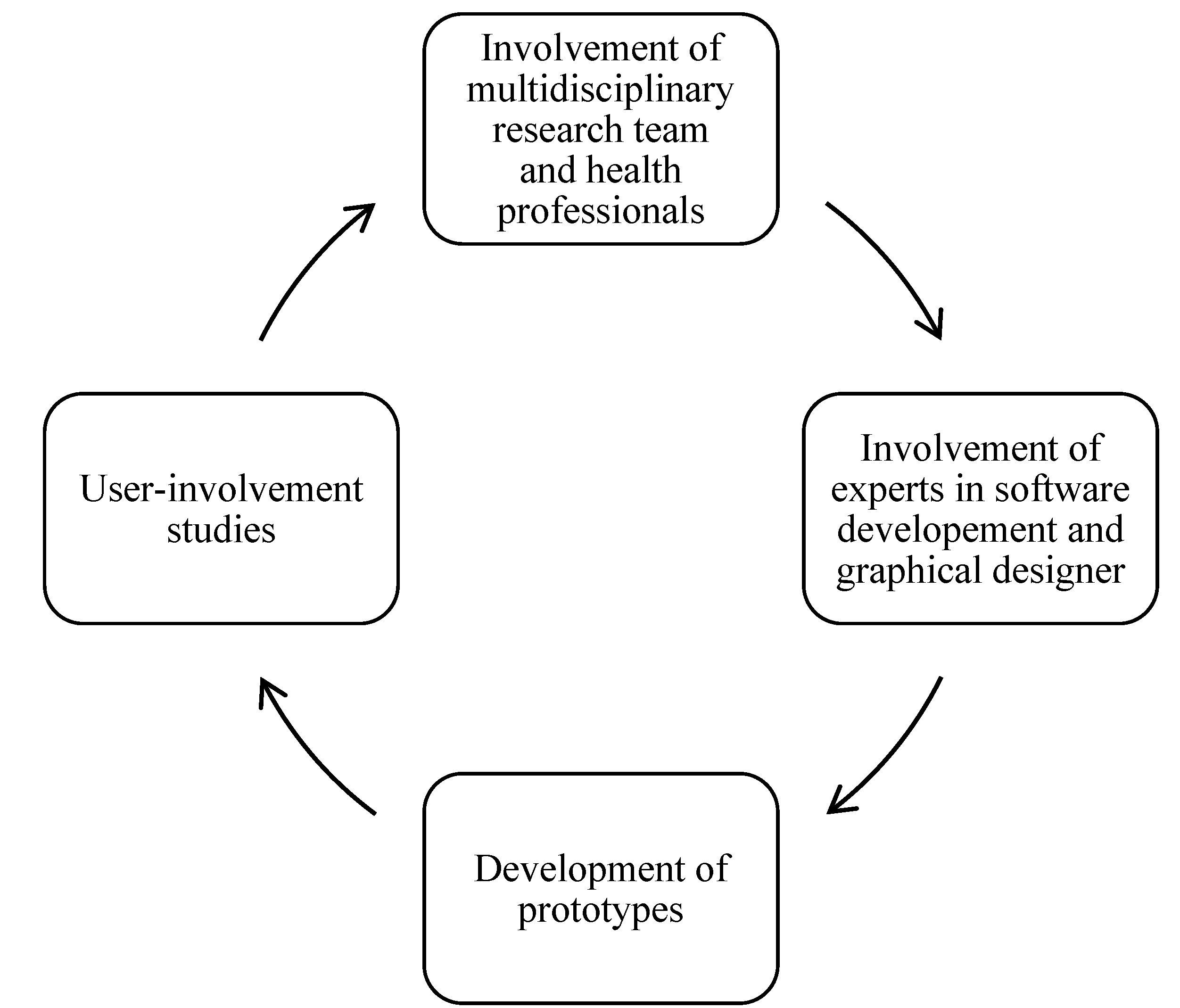
2.1. Involvement of Researchers and Health Professionals
2.2. Application Development
2.2.1. Software Development Challenges
2.3. User-Involvement
3. Results and Discussion
3.1. Group Discussions among Researchers and Health Professionals
3.2. Interviews and Task Performance among Patients
“I think it is very good. You get inspired to do things right. It’s pretty easy, yes, because you have your phone with you all the time. I always forget about the registration booklet and have to find a pen.”
| Characteristics | Number of Participants | Number of Participants | |
|---|---|---|---|
| User-Involvement Study 1 | User-Involvement Study 2 | ||
| Region of origin | Norway | 4 | 6 |
| Africa | 0 | 2 | |
| Asia | 4 | 1 | |
| Eastern-Europe | 1 | 1 | |
| South-America | 1 | 1 | |
| Previous diagnosis of GDM | Never | 6 | 10 |
| Once | 3 | 0 | |
| Twice | 1 | 1 | |
3.2.1. Initial Interviews
| Theme of Feedback | Quote | Adjustments to the App |
|---|---|---|
| Use of language | “What is whole grain” | Use easier language; avoid jargon; develop a diabetes lexicon in the application. |
| Conflicting information compared to advice from health professionals | “But, here at the clinic, they told me that I should not eat too much rice” | Standardize app content with content of leaflets from diabetes outpatient clinics. |
| Information about gestational diabetes | “Women need more risk awareness. They think that GDM disappears after delivery”. | Add more information about the risks of having GDM and future health consequences for mother and child. |
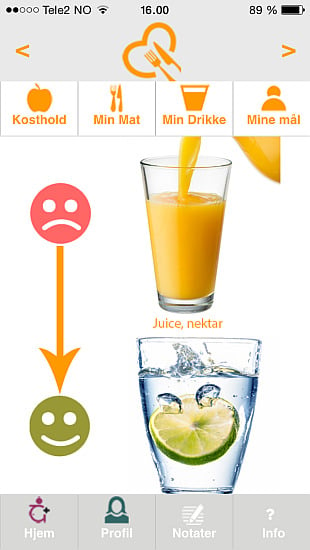
| More specific and individualized dietary information about GDM | “Pears are dangerous” | Add diabetes-sensitive pictures; |
| Design | “I can’t see it” | Enlarge pictures. |
| Presentation of blood sugar levels | “I mean, I am a person who loves information provided in a graph” | Provide feedback on individual blood sugar levels in a graph with graduated transitions and smileys. |
3.2.2 Task Performance
| Task | Percentage of Participants Who Succeeded (n = 11) |
|---|---|
| Finding where to register blood sugar levels | 100% |
| Finding information about healthy eating | 91% |
| Finding inspiration for physical activity | 91% |
| Finding information about gestational diabetes | 91% |
| Entering appointments for medical consultations | 82% |
| Finding how to register body weight | 45% |
3.3. Presentation of the Pregnant+ App
3.3.1. Individually Targeted Information
3.3.2. Pregnant+ Main Content
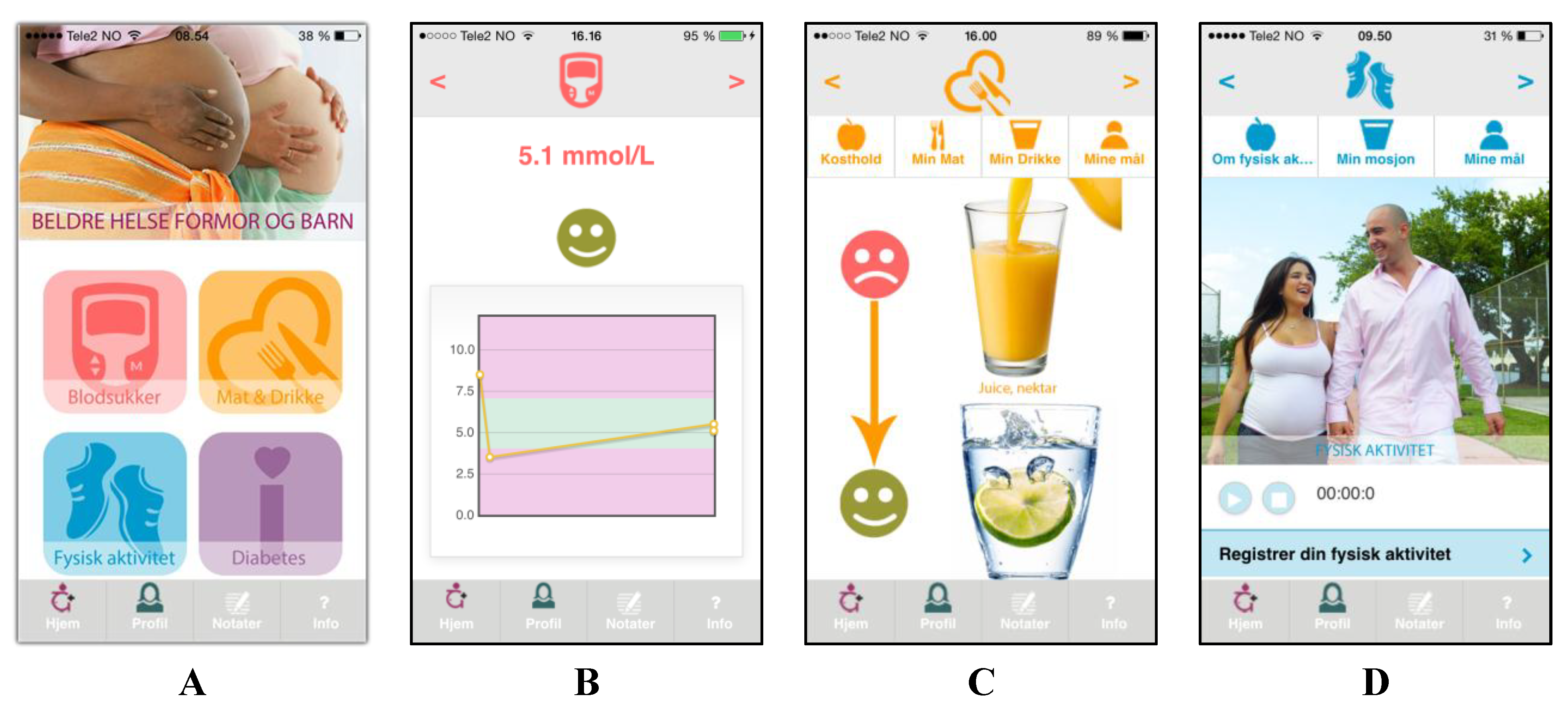
3.3.3. A Smartphone Application for Behavior Change
4. Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Metzger, B.E. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010, 33, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Galtier, F. Definition, epidemiology, risk factors. Diabetes Metab. 2010, 36, 628–651. [Google Scholar] [CrossRef] [PubMed]
- Skupien, J.; Cyganek, K.; Malecki, M.T. Diabetic pregnancy: An overview of current guidelines and clinical practice. Curr. Opin. Obstet. Gynecol. 2014, 26, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Schneider, S.; Hoeft, B.; Freerksen, N.; Fischer, B.; Roehrig, S.; Yamamoto, S.; Maul, H. Neonatal complications and risk factors among women with gestational diabetes mellitus. Acta Obstet. Gynecol. Scand. 2011, 90, 231–237. [Google Scholar] [PubMed]
- Makgoba, M.; Savvidou, M.D.; Steer, P.J. An analysis of the interrelationship between maternal age, body mass index and racial origin in the development of gestational diabetes mellitus. BJOG 2012, 119, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Kim, C. Gestational diabetes: Risks, management, and treatment options. Int. J. Womens Health 2010, 2, 339–351. [Google Scholar] [CrossRef]
- Wikström, K.; Peltonen, M.; Eriksson, J.G.; Aunola, S.; Ilanne-Parikka, P.; Keinänen-Kiukaanniemi, S.; Uusitupa, M.; Tuomilehto, J.; Lindström, J. Educational attainment and effectiveness of lifestyle intervention in the finnish diabetes prevention study. Diabetes Res. Clin. Pract. 2009, 86, e1–e5. [Google Scholar] [CrossRef] [PubMed]
- Norwegian Directorate of Health. Diabetes-National Guidelines 2009. Available online: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/415/Nasjonal-faglig-retningslinje-diabetes-fullversjon-IS1674.pdf (accessed on 18/5/2015).
- Szwajcer, E.M.; Hiddink, G.J.; Koelen, M.A.; van Woerkum, C.M. Nutrition-related information-seeking behaviours before and throughout the course of pregnancy: Consequences for nutrition communication. Eur. J. Clin. Nutr. 2005, 59, S57–S65. [Google Scholar] [CrossRef] [PubMed]
- Olson, C.M. Tracking of food choices across the transition to motherhood. J. Nutr. Educ. Behav. 2005, 37, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Garnweidner, L.; Sverre Pettersen, K.; Mosdøl, A. Experiences with nutrition-related information during antenatal care of pregnant women of different ethnic backgrounds residing in the area of Oslo, Norway. Midwifery 2013, 29, e130–e137. [Google Scholar] [CrossRef] [PubMed]
- Mills, A.; Schmied, V.A.; Dahlen, H.G. “Get alongside us”, women’s experiences of being overweight and pregnant in Sydney, Australia. Matern. Child Nutr. 201 2013, 9, 309–321. [Google Scholar] [CrossRef]
- Smith-Morris, C.M. Diagnostic controversy: Gestational diabetes and the meaning of risk for pima Indian women. Med. Anthropol. 2005, 24, 145–177. [Google Scholar] [CrossRef]
- Carolan, M.; Steele, C.; Margetts, H. Knowledge of gestational diabetes among a multi-ethnic cohort in Australia. Midwifery 2010, 26, 579–588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fagerli, R.A.A.; Lien, M.E.; Botten, G.S.; Wandel, M. Role dilemmas among health-workers in cross-cultural patient encounters around dietary advice. Scand. J. Public Health 2005, 33, 360–369. [Google Scholar] [CrossRef] [PubMed]
- Schouten, B.C.; Meeuwesen, L. Cultural differences in medical communication: A review of the literature. Patient Educ. Couns. 2006, 64, 21–34. [Google Scholar] [CrossRef] [PubMed]
- Medie Norge. Andelen Som Har Smartphone; Medienorge: Oslo, Norwey, 2014. (In Norwegian) [Google Scholar]
- Demidowich, A.P.; Lu, K.; Tamler, R.; Bloomgarden, Z. An evaluation of diabetes self-management applications for android smartphones. J. Telemed. Telecare 2012, 18, 235–238. [Google Scholar] [CrossRef] [PubMed]
- Boulos, M.N.K.; Brewer, A.C.; Karimkhani, C.; Buller, D.B.; Dellavalle, R.P. Mobicle medical and health apps: State of the art, concerns, regulatory control and certification. J. Public Health Inform. 2014. [Google Scholar] [CrossRef]
- Mackillop, L.; Loerup, L.; Bartlett, K.; Farmer, A.; Gibson, O.J.; Hirst, J.E.; Kenworthy, Y.; Kevat, D.A.; Levy, J.C.; Tarassenko, L. Development of a real-time smartphone solution for the management of women with or at high risk of gestational diabetes. J. Diabetes Sci. Technol. 2014, 8, 1105–1114. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Crowther, C.A.; Middleton, P.; Heatley, E. Different types of dietary advice for women with gestational diabetes mellitus. Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef] [Green Version]
- Evert, A.B.; Boucher, J.L.; Cypress, M.; Dunbar, S.A.; Franz, M.J.; Mayer-Davis, E.J.; Neumiller, J.J.; Nwankwo, R.; Verdi, C.L.; Urbanski, P.; et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2014, 37, S120–S143. [Google Scholar] [CrossRef] [PubMed]
- Directorate for Health and Social Affairs. A National Clinical Guideline for Antenatal Care. Short Version; Medienorge: Oslo, Norwey, 2005. [Google Scholar]
- Directorate for Health and Social Affairs. Recommendations on Diet, Nutrition and Physical Activity; Medienorge: Oslo, Norwey, 2014. [Google Scholar]
- Glanz, K.; Rimer, B.; Viswanath, K. Health Behaviour and Health Education: Theory, Research, and Practice, 4th ed.; Jossey-Bass: San Francisco, CA, USA, 2008. [Google Scholar]
- Arnold, M.; Quade, M.; Kirch, W. Mobile applications for diabetics: A systematic review and expert-based usability evaluation considering the special requirements of diabetes patients age 50 years or older. J. Med. Int. Res. 2014. [Google Scholar] [CrossRef]
- Gartner, I. Gartner Says Sales of Smartphones Grew 20 Percent in Third Quarter of 2014; Gartner: Stamford, CT, USA, 2015. [Google Scholar]
- Jaap, H. Bluetooth-the universal radio interface for ad hoc, wireless connectivity. Ericsson review 1998, 1, 110–117. [Google Scholar]
- Min, C.; Shiwen, M.; Yunhao, L. Big data: A survey. Mobile Networks and Applications 2014, 2, 171–209. [Google Scholar]
- Buller, D.B.; Berwick, M.; Shane, J.; Kane, I.; Lantz, K.; Buller, M.K. User-centered development of a smart phone mobile application delivering personalized real-time advice on sun protection. Translational behavioral medicine 2013, 3, 326–334. [Google Scholar] [CrossRef]
- LeRouge, C.; Ma, J.; Sneha, S.; Tolle, K. User profiles and personas in the design and development of consumer health technologies. Int. J. Med. Inf. 2013, 82, e251–e268. [Google Scholar] [CrossRef]
- Schiavo, R. Health Communication: From Theory to Practice, 1st ed.; Jossey-Bass: San Francisco, CA, USA, 2007. [Google Scholar]
- Kreuter, M.W.; McClure, S.M. The role of culture in health communication. Annu. Rev. Public Health 2004, 25, 439–455. [Google Scholar] [CrossRef] [PubMed]
- Kreps, G.; Sparks, L. Meeting the health literacy need of immigrant populations. Patient Educ. Couns. 2008, 71, 328–332. [Google Scholar] [CrossRef] [PubMed]
- Attridge, M.; Creamer, J.; Ramsden, M.; Cannings-John, R.; Hawthorne, K. Culturally appropriate health education for people in ethnic minority groups with type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2014. [Google Scholar] [CrossRef] [Green Version]
- Jenum, A.K.; Diep, L.M.; Holmboe-Ottesen, G.; Holme, I.M.; Kumar, B.N.; Birkeland, K.I. Diabetes susceptibility in ethnic minority groups from turkey, vietnam, sri lanka and pakistan compared with norwegians—The association with adiposity is strongest for ethnic minority women. BMC Public Health 2012. [Google Scholar] [CrossRef]
- Resnicow, K.; Baranowski, T.; Ahluwalia, J.; Braithwaite, R. Cultural sensitivity in public health: Defined and demystified. Ethn. Dis. 1999, 9, 10–21. [Google Scholar] [PubMed]
- Kreuter, M.; Farell, D.; Olevitch, L.; Brennan, L.M. Tailoring Health Messages: Customizing Communication with Computer Technology; Lawrence Erlbaum Associates: New Jersey, NJ, USA, 2000. [Google Scholar]
- Doak, C.; Doak, L.; Root, J. Teaching patients with low literacy skills, 2nd ed.; J.B. Lippincott Company: Philadelphia, PA, USA, 1996. [Google Scholar]
- Goldberg, J.P.; Sliwa, S.A. Communicating actionable nutrition messages: Challenges and opportunities. Proc. Nutr. Soc. 2011, 70, 26–37. [Google Scholar] [CrossRef] [PubMed]
- Niés, J.; Pelayo, S. From users involvement to users’ needs understanding: A case study. Int. J. Med. Inf. 2010, 79, e76–e82. [Google Scholar] [CrossRef]
- Kujala, S. User involvement: A review of the benefits and challenges. Behav. Inf. Technol. 2003, 22, 1–6. [Google Scholar] [CrossRef]
- Hawkins, R.P.; Kreuter, M.; Resnicow, K.; Fishbein, M.; Dijkstra, A. Understanding tailoring in communicating about health. Health Educ. Res. 2008, 23, 454–466. [Google Scholar] [CrossRef] [PubMed]
- Kreuter, M.; Wray, R. Tailored and targeted health communication: Strategies for enhancing information relevance. Am. J. Health Behav. 2003, 27, 227–232. [Google Scholar] [CrossRef]
- Antypas, K.; Wangberg, S.C. Combining users’ needs with health behavior models in designing an internet- and mobile-based intervention for physical activity in cardiac rehabilitation. JMIR Res. Protoc. 2014. [Google Scholar] [CrossRef]
- Middelweerd, A.; Mollee, J.S.; van der Wal, C.N.; Brug, J.; te Velde, S.J. Apps to promote physical activity among adults: A review and content analysis. Int. J. Behav. Nutr. and Phys. Act. 2014. [Google Scholar] [CrossRef]
- Webb, T.L.; Joseph, J.; Yardley, L.; Michi, S. Using the internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J. Med. Int. Res. 2010. [Google Scholar] [CrossRef]
- Lane, S.; Heddle, N.; Arnold, E.; Walker, I. A review of randomized controlled trials comparing the effectiveness of hand held computers with paper methods for data collection. BMC Med. Inf. Decis. Mak. 2006, 83, 9–17. [Google Scholar]
- Kieffer, E.C.; Willis, S.K.; Arellano, N.; Guzman, R. Perspectives of pregnant and postpartum latino women on diabetes, physical activity, and health. Health Educ. Behav. 2002, 29, 542–556. [Google Scholar] [CrossRef] [PubMed]
- Krumeich, A.; Weijts, W.; Reddy, P.; Meijer-Weitz, A. The benefits of anthropological approaches for health promotion research and practice. Health Educ. Res. 2001, 16, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I.M. The health belief model and preventive health behavior. Health Educ. Monogr. 1974, 2, 354–386. [Google Scholar]
- Pearce, E.E.; Evenson, K.R.; Downs, D.S.; Steckler, A. Strategies to promote physical activity during pregnancy: A systematic review of intervention evidence. Am. J. Lifestyle Med. 2013. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garnweidner-Holme, L.M.; Borgen, I.; Garitano, I.; Noll, J.; Lukasse, M. Designing and Developing a Mobile Smartphone Application for Women with Gestational Diabetes Mellitus Followed-Up at Diabetes Outpatient Clinics in Norway. Healthcare 2015, 3, 310-323. https://doi.org/10.3390/healthcare3020310
Garnweidner-Holme LM, Borgen I, Garitano I, Noll J, Lukasse M. Designing and Developing a Mobile Smartphone Application for Women with Gestational Diabetes Mellitus Followed-Up at Diabetes Outpatient Clinics in Norway. Healthcare. 2015; 3(2):310-323. https://doi.org/10.3390/healthcare3020310
Chicago/Turabian StyleGarnweidner-Holme, Lisa Maria, Iren Borgen, Iñaki Garitano, Josef Noll, and Mirjam Lukasse. 2015. "Designing and Developing a Mobile Smartphone Application for Women with Gestational Diabetes Mellitus Followed-Up at Diabetes Outpatient Clinics in Norway" Healthcare 3, no. 2: 310-323. https://doi.org/10.3390/healthcare3020310
APA StyleGarnweidner-Holme, L. M., Borgen, I., Garitano, I., Noll, J., & Lukasse, M. (2015). Designing and Developing a Mobile Smartphone Application for Women with Gestational Diabetes Mellitus Followed-Up at Diabetes Outpatient Clinics in Norway. Healthcare, 3(2), 310-323. https://doi.org/10.3390/healthcare3020310