Creation of Mitochondrial Disease Models Using Mitochondrial DNA Editing
Abstract
:1. Introduction
2. Mitochondrial Biology and Functions
3. Mitochondrial Diseases
4. The Role of mtDNA Mutations in the Development of Mitochondrial Diseases
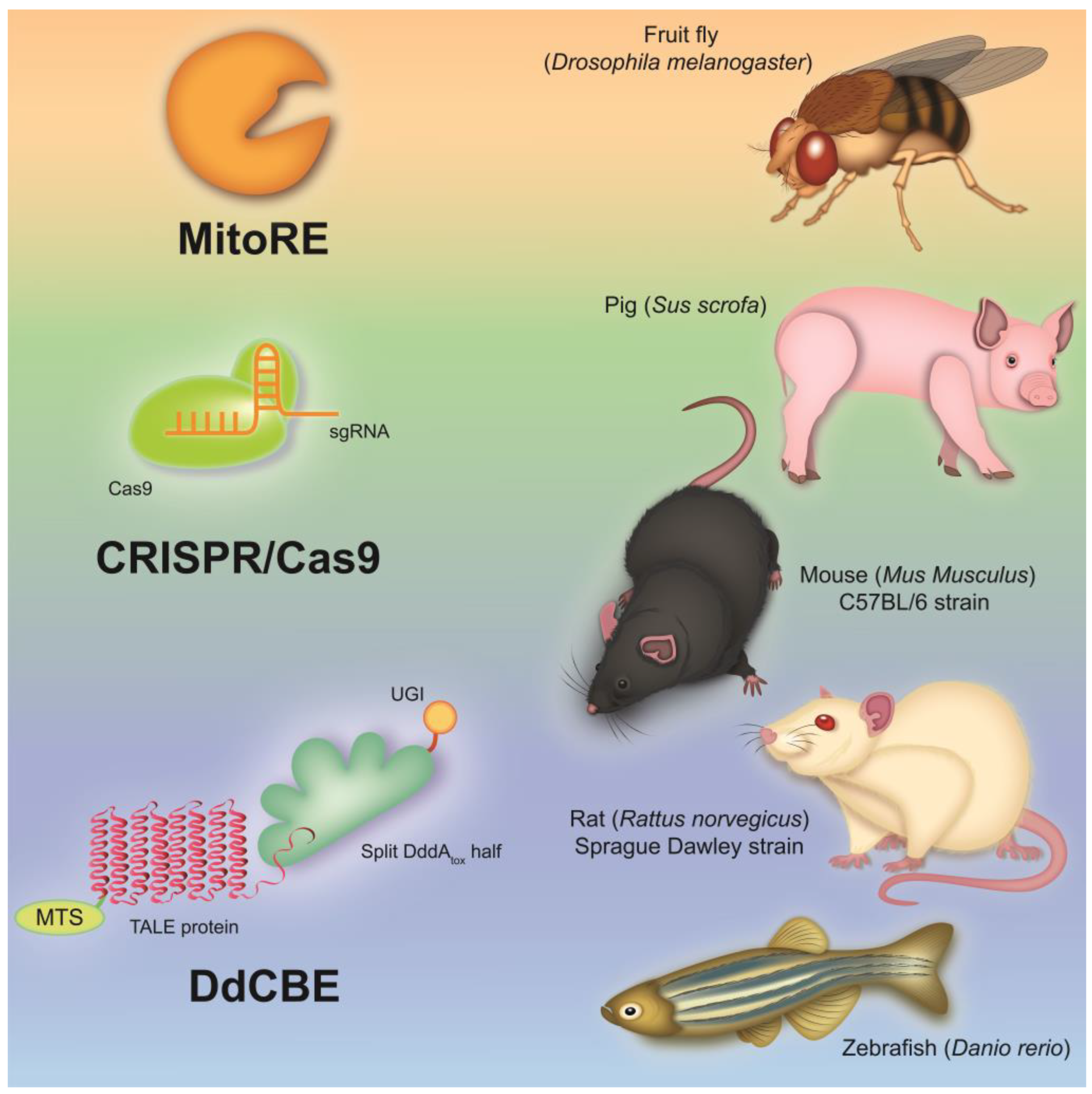
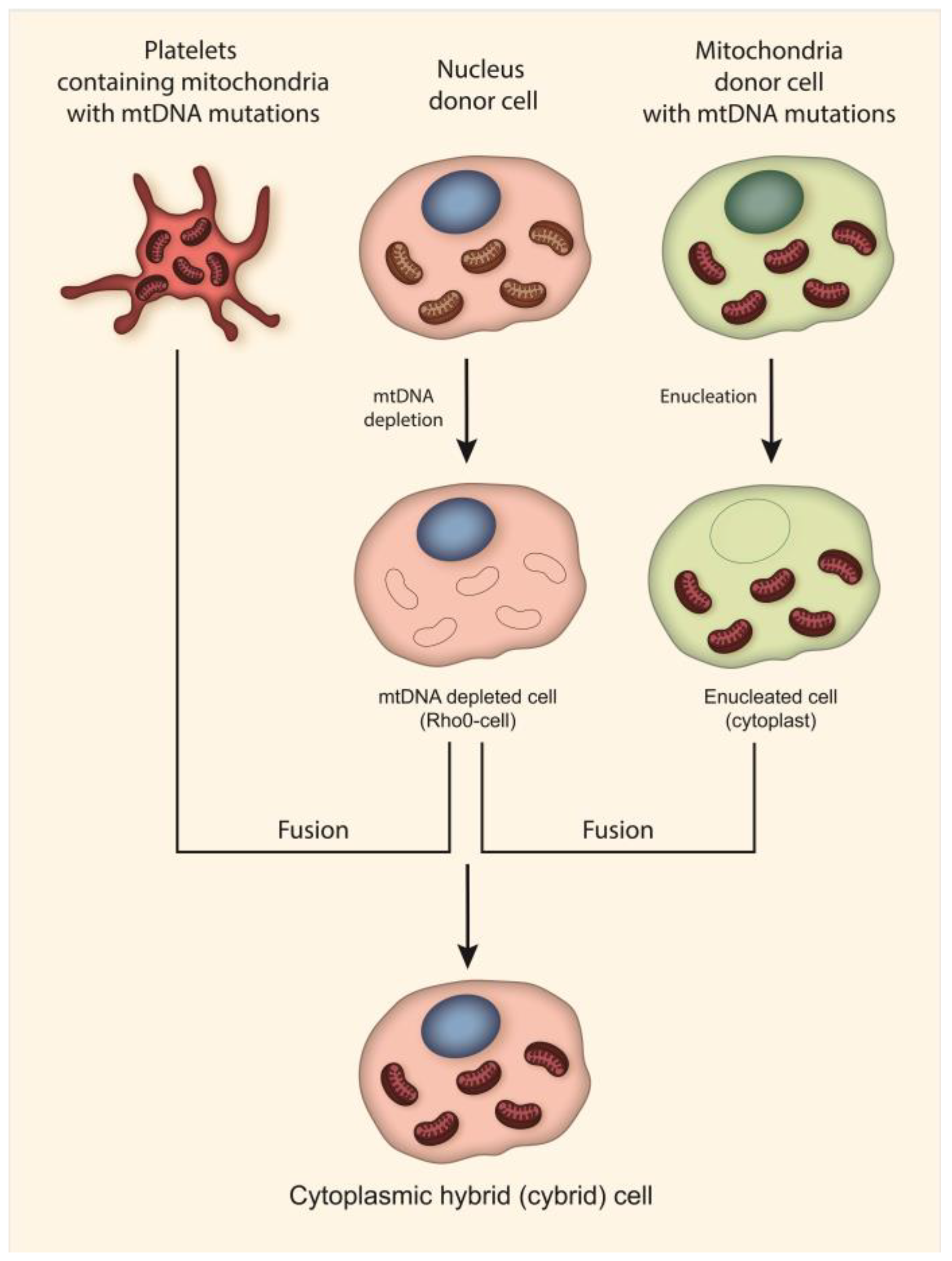
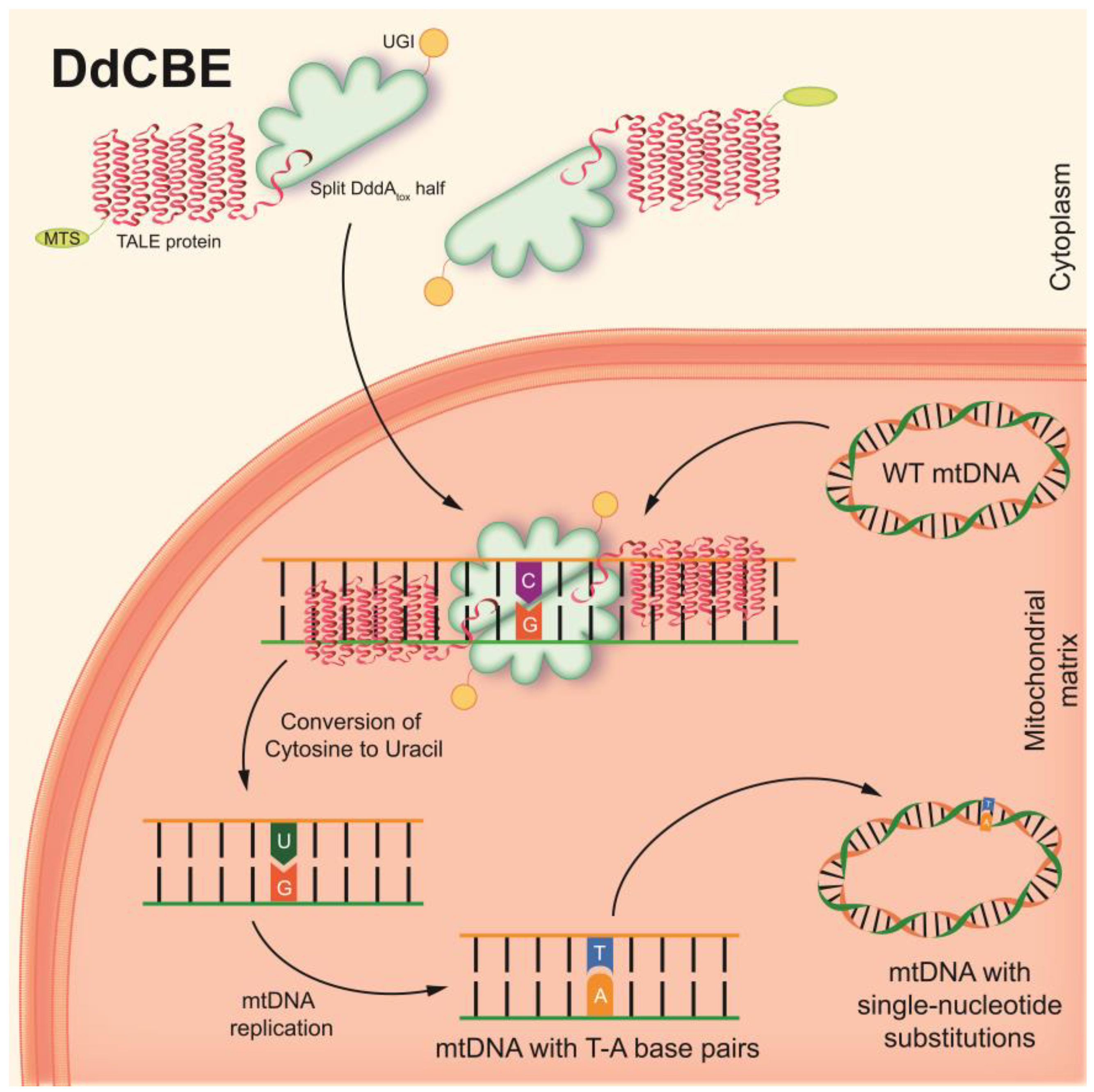
5. Current Progress in the Development of Cellular and Animal Models of Human Mitochondrial Diseases
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ATP | adenosine triphosphate |
| CI | complex I (NADH:ubiquinone oxidoreductase) |
| CII | complex II (succinate dehydrogenase) |
| CIII | complex III (cytochrome c oxidoreductase) |
| CIV | complex IV (cytochrome c oxidase) |
| CV | complex V (ATP synthase) |
| CPEO | chronic progressive external ophthalmoplegia |
| DddAtox | deaminase-like toxin |
| DdCBE | DddA-derived cytosine base editor |
| DNA | deoxyribonucleic acid |
| DSB | double-strand break |
| dsDNA | double-stranded DNA |
| ETC | electron transport chain |
| FusXTBE | FusX TALE Base Editor |
| IBM | inner boundary membrane |
| IMM | inner mitochondrial membrane |
| IMS | intermembrane space |
| iPSC | induced pluripotent stem cell |
| LHON | Leber Hereditary Optic Neuropathy |
| MD | mitochondrial disease |
| MELAS | mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes |
| MERRF | myoclonus epilepsy associated with ragged-red fibers |
| MIDD | maternally inherited diabetes and deafness |
| mito-CRISPR/Cas9 | mitochondria-targeted clustered regularly interspaced short palindromic repeat (CRISPR)-associated protein 9 |
| MitoRE | mitochondria-targeted restriction endonuclease |
| mitoTALEN | mitochondria-targeted transcription activator-like effector nuclease |
| mitoZFN | mitochondria-targeted zinc finger nuclease |
| mRNA | messenger RNA |
| mtDNA | mitochondrial DNA |
| MTS | mitochondrial targeting sequence |
| NARP | neuropathy, ataxia and pigmentary retinopathy |
| NES | nuclear export signal |
| OMM | outer mitochondrial membrane |
| OXPHOS | oxidative phosphorylation |
| PACE | phage-assisted continuous evolution |
| PANCE | phage-assisted non-continuous evolution |
| PBMC | peripheral blood mononuclear cell |
| RET | reverse electron transfer |
| RNA | ribonucleic acid |
| ROS | reactive oxygen species |
| rRNA | ribosomal RNA |
| TALE | transcription activator-like effector |
| TALED | TALE-linked deaminase |
| TCA | tricarboxylic acid |
| tRNA | transfer RNA |
| UGI | uracil glycosylase inhibitor |
| ΔΨm | mitochondrial transmembrane potential |
References
- Bruce Stewart, J.; James Bruce Stewart, C. Current Progress with Mammalian Models of Mitochondrial DNA Disease. J. Inherit. Metab. Dis. 2021, 44, 325–342. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Lee, S.; Baek, G.; Kim, A.; Kang, B.C.; Seo, H.; Kim, J.S. Mitochondrial DNA Editing in Mice with DddA-TALE Fusion Deaminases. Nat. Commun. 2021, 12, 1190. [Google Scholar] [CrossRef] [PubMed]
- Duchen, M.R. Mitochondria and Calcium: From Cell Signalling to Cell Death. J. Physiol. 2000, 529, 57–68. [Google Scholar] [CrossRef]
- Martínez-Reyes, I.; Chandel, N.S. Mitochondrial TCA Cycle Metabolites Control Physiology and Disease. Nat. Commun. 2020, 11, 102. [Google Scholar] [CrossRef]
- Kastaniotis, A.J.; Autio, K.J.; Kerätär, J.M.; Monteuuis, G.; Mäkelä, A.M.; Nair, R.R.; Pietikäinen, L.P.; Shvetsova, A.; Chen, Z.; Hiltunen, J.K. Mitochondrial Fatty Acid Synthesis, Fatty Acids and Mitochondrial Physiology. Biochim. Biophys. Acta-Mol. Cell Biol. Lipids 2017, 1862, 39–48. [Google Scholar] [CrossRef]
- Spinelli, J.B.; Haigis, M.C. The Multifaceted Contributions of Mitochondria to Cellular Metabolism. Nat. Cell Biol. 2018, 20, 745–754. [Google Scholar] [CrossRef]
- Kühlbrandt, W. Structure and Function of Mitochondrial Membrane Protein Complexes. BMC Biol. 2015, 13, 89. [Google Scholar] [CrossRef]
- Skulachev, V.P. Mitochondrial Physiology and Pathology; Concepts of Programmed Death of Organelles, Cells and Organisms. Mol. Asp. Med. 1999, 20, 139–184. [Google Scholar] [CrossRef]
- Giacomello, M.; Pyakurel, A.; Glytsou, C.; Scorrano, L. The Cell Biology of Mitochondrial Membrane Dynamics. Nat. Rev. Mol. Cell Biol. 2020, 21, 204–224. [Google Scholar] [CrossRef]
- Protasoni, M.; Zeviani, M. Mitochondrial Structure and Bioenergetics in Normal and Disease Conditions. Int. J. Mol. Sci. 2021, 22, 586. [Google Scholar] [CrossRef]
- Signes, A.; Fernandez-Vizarra, E. Assembly of Mammalian Oxidative Phosphorylation Complexes I–V and Supercomplexes. Essays Biochem. 2018, 62, 255–270. [Google Scholar] [CrossRef] [PubMed]
- Vartak, R.S.; Semwal, M.K.; Bai, Y. An Update on Complex I Assembly: The Assembly of Players. J. Bioenerg. Biomembr. 2014, 46, 323–328. [Google Scholar] [CrossRef]
- Vinothkumar, K.R.; Zhu, J.; Hirst, J. Architecture of Mammalian Respiratory Complex I. Nature 2014, 515, 80–84. [Google Scholar] [CrossRef]
- Rutter, J.; Winge, D.R.; Schiffman, J.D. Succinate Dehydrogenase—Assembly, Regulation and Role in Human Disease. Mitochondrion 2010, 10, 393–401. [Google Scholar] [CrossRef]
- Schägger, H.; Link, T.A.; Engel, W.D.; von Jagow, G. Isolation of the Eleven Protein Subunits of the Bc1 Complex from Beef Heart. Methods Enzymol. 1986, 126, 224–237. [Google Scholar] [CrossRef]
- Capaldi, R.A. Structure and Function of Cytochrome c Oxidase. Annu. Rev. Biochem. 1990, 59, 569–596. [Google Scholar] [CrossRef]
- Jonckheere, A.I.; Smeitink, J.A.M.; Rodenburg, R.J.T. Mitochondrial ATP Synthase: Architecture, Function and Pathology. J. Inherit. Metab. Dis. 2012, 35, 211–225. [Google Scholar] [CrossRef]
- Abrahams, J.P.; Leslie, A.G.W.; Lutter, R.; Walker, J.E. Structure at 2.8 Â Resolution of F1-ATPase from Bovine Heart Mitochondria. Nature 1994, 370, 621–628. [Google Scholar] [CrossRef]
- He, J.; Ford, H.C.; Carroll, J.; Douglas, C.; Gonzales, E.; Ding, S.; Fearnley, I.M.; Walker, J.E. Assembly of the Membrane Domain of ATP Synthase in Human Mitochondria. Proc. Natl. Acad. Sci. USA 2018, 115, 2988–2993. [Google Scholar] [CrossRef]
- Taanman, J.W. The Mitochondrial Genome: Structure, Transcription, Translation and Replication. Biochim. Biophys. Acta-Bioenerg. 1999, 1410, 103–123. [Google Scholar] [CrossRef] [Green Version]
- Chinnery, P.F.; Hudson, G. Mitochondrial Genetics. Br. Med. Bull. 2013, 106, 135–159. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, C.M.; Falkenberg, M.; Larsson, N.G. Maintenance and Expression of Mammalian Mitochondrial DNA. Annu. Rev. Biochem. 2016, 85, 133–160. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Herrmann, J.M.; Becker, T. Quality Control of the Mitochondrial Proteome. Nat. Rev. Mol. Cell Biol. 2021, 22, 54–70. [Google Scholar] [CrossRef] [PubMed]
- Shtolz, N.; Mishmar, D. The Mitochondrial Genome–on Selective Constraints and Signatures at the Organism, Cell, and Single Mitochondrion Levels. Front. Ecol. Evol. 2019, 7, 342. [Google Scholar] [CrossRef]
- Schmidt, O.; Pfanner, N.; Meisinger, C. Mitochondrial Protein Import: From Proteomics to Functional Mechanisms. Nat. Rev. Mol. Cell Biol. 2010, 11, 655–667. [Google Scholar] [CrossRef]
- Wallace, D.C.; Chalkia, D. Mitochondrial DNA Genetics and the Heteroplasmy Conundrum in Evolution and Disease. Cold Spring Harb. Perspect. Biol. 2013, 5, a021220. [Google Scholar] [CrossRef]
- Filograna, R.; Mennuni, M.; Alsina, D.; Larsson, N.G. Mitochondrial DNA Copy Number in Human Disease: The More the Better? FEBS Lett. 2021, 595, 976–1002. [Google Scholar] [CrossRef]
- Gardner, J.L.; Craven, L.; Turnbull, D.M.; Taylor, R.W. Experimental Strategies towards Treating Mitochondrial DNA Disorders. Biosci. Rep. 2007, 27, 139–150. [Google Scholar] [CrossRef]
- Pickles, S.; Vigié, P.; Youle, R.J. Mitophagy and Quality Control Mechanisms in Mitochondrial Maintenance. Curr. Biol. 2018, 28, R170–R185. [Google Scholar] [CrossRef]
- Yan, C.; Duanmu, X.; Zeng, L.; Liu, B.; Song, Z. Mitochondrial DNA: Distribution, Mutations, and Elimination. Cells 2019, 8, 379. [Google Scholar] [CrossRef] [Green Version]
- Saneto, R.P. Mitochondrial Diseases: Expanding the Diagnosis in the Era of Genetic Testing. J. Transl. Genet. Genom. 2020, 4, 384–428. [Google Scholar] [CrossRef] [PubMed]
- Muraresku, C.C.; McCormick, E.M.; Falk, M.J. Mitochondrial Disease: Advances in Clinical Diagnosis, Management, Therapeutic Development, and Preventative Strategies. Curr. Genet. Med. Rep. 2018, 6, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Hage, R.; Vignal-Clermont, C. Leber Hereditary Optic Neuropathy: Review of Treatment and Management. Front. Neurol. 2021, 12, 651639. [Google Scholar] [CrossRef] [PubMed]
- Schubert, M.B.; Vilarinho, L. Molecular Basis of Leigh Syndrome: A Current Look. Orphanet J. Rare Dis. 2020, 15, 31. [Google Scholar] [CrossRef] [PubMed]
- Tetsuka, S.; Ogawa, T.; Hashimoto, R.; Kato, H. Clinical Features, Pathogenesis, and Management of Stroke-like Episodes Due to MELAS. Metab. Brain Dis. 2021, 36, 2181–2193. [Google Scholar] [CrossRef]
- Gilson, R.C.; Osswald, S. Madelung Lipomatosis Presenting as a Manifestation of Myoclonic Epilepsy with Ragged Red Fibers (MERRF) Syndrome. JAAD Case Rep. 2018, 4, 822–823. [Google Scholar] [CrossRef]
- Finsterer, J.; Zarrouk-Mahjoub, S.; Shoffner, J.M. MERRF Classification: Implications for Diagnosis and Clinical Trials. Pediatr. Neurol. 2018, 80, 8–23. [Google Scholar] [CrossRef] [PubMed]
- Li, H.Z.; Li, R.Y.; Li, M. A Review of Maternally Inherited Diabetes and Deafness. Front. Biosci.-Landmark 2014, 19, 777–782. [Google Scholar] [CrossRef] [PubMed]
- Claeys, K.G.; Abicht, A.; Häusler, M.; Kleinle, S.; Wiesmann, M.; Schulz, J.B.; Horvath, R.; Weis, J. Novel Genetic and Neuropathological Insights in Neurogenic Muscle Weakness, Ataxia, and Retinitis Pigmentosa (NARP). Muscle Nerve 2016, 54, 328–333. [Google Scholar] [CrossRef]
- Heighton, J.N.; Brady, L.I.; Newman, M.C.; Tarnopolsky, M.A. Clinical and Demographic Features of Chronic Progressive External Ophthalmoplegia in a Large Adult-Onset Cohort. Mitochondrion 2019, 44, 15–19. [Google Scholar] [CrossRef]
- Klopstock, T.; Priglinger, C.; Yilmaz, A.; Kornblum, C.; Distelmaier, F.; Prokisch, H. Mitochondrial Disorders. Dtsch. Arztebl. Int. 2021, 118, 741–748. [Google Scholar] [CrossRef] [PubMed]
- Chiaratti, M.R.; Macabelli, C.H.; Neto, J.D.A.; Grejo, M.P.; Pandey, A.K.; Perecin, F.; Collado, M. Del Maternal Transmission of Mitochondrial Diseases. Genet. Mol. Biol. 2020, 43. [Google Scholar]
- Schon, E.A.; Dimauro, S.; Hirano, M. Human Mitochondrial DNA: Roles of Inherited and Somatic Mutations. Nat. Rev. Genet. 2012, 13, 878–890. [Google Scholar] [CrossRef]
- Xu, C.; Tong, L.; Rao, J.; Ye, Q.; Chen, Y.; Zhang, Y.; Xu, J.; Mao, X.; Meng, F.; Shen, H.; et al. Heteroplasmic and Homoplasmic m.616T>C in Mitochondria TRNAPhe Promote Isolated Chronic Kidney Disease and Hyperuricemia. JCI Insight 2022, 7, e157418. [Google Scholar] [CrossRef]
- MITOMAP: A Human Mitochondrial Genome Database. 2023. Available online: http://www.mitomap.org (accessed on 3 February 2023).
- Ding, Y.; Xia, B.H.; Zhang, C.J.; Zhuo, G.C. Mitochondrial tRNALeu(UUR) C3275T, TRNAGln T4363C and TRNALys A8343G Mutations May Be Associated with PCOS and Metabolic Syndrome. Gene 2018, 642, 299–306. [Google Scholar] [CrossRef]
- Guerrero-Molina, M.P.; Morales-Conejo, M.; Delmiro, A.; Morán, M.; Domínguez-González, C.; Arranz-Canales, E.; Ramos-González, A.; Arenas, J.; Martín, M.A.; González de la Aleja, J. Elevated Glutamate and Decreased Glutamine Levels in the Cerebrospinal Fluid of Patients with MELAS Syndrome. J. Neurol. 2022, 269, 3238–3248. [Google Scholar] [CrossRef]
- Belal, S.; Goudenège, D.; Bocca, C.; Dumont, F.; Chao De La Barca, J.M.; Desquiret-Dumas, V.; Gueguen, N.; Geffroy, G.; Benyahia, R.; Kane, S.; et al. Glutamate-Induced Deregulation of Krebs Cycle in Mitochondrial Encephalopathy Lactic Acidosis Syndrome Stroke-Like Episodes (MELAS) Syndrome Is Alleviated by Ketone Body Exposure. Biomedicines 2022, 10, 1665. [Google Scholar] [CrossRef] [PubMed]
- Aras, S.; Purandare, N.; Gladyck, S.; Somayajulu-Nitu, M.; Zhang, K.; Wallace, D.C.; Grossman, L.I. Mitochondrial Nuclear Retrograde Regulator 1 (MNRR1) Rescues the Cellular Phenotype of MELAS by Inducing Homeostatic Mechanisms. Proc. Natl. Acad. Sci. USA 2020, 117, 32056–32065. [Google Scholar] [CrossRef]
- Bhattacharya, S.; Yin, J.; Huo, W.; Chaum, E. Modeling of Mitochondrial Bioenergetics and Autophagy Impairment in MELAS-Mutant IPSC-Derived Retinal Pigment Epithelial Cells. Stem Cell Res. Ther. 2022, 13, 260. [Google Scholar] [CrossRef]
- Ryytty, S.; Modi, S.R.; Naumenko, N.; Shakirzyanova, A.; Rahman, M.O.; Vaara, M.; Suomalainen, A.; Tavi, P.; Hämäläinen, R.H. Varied Responses to a High m.3243A>G Mutation Load and Respiratory Chain Dysfunction in Patient-Derived Cardiomyocytes. Cells 2022, 11, 2593. [Google Scholar] [CrossRef]
- Chung, C.Y.; Singh, K.; Kotiadis, V.N.; Valdebenito, G.E.; Ahn, J.H.; Topley, E.; Tan, J.; Andrews, W.D.; Bilanges, B.; Pitceathly, R.D.S.; et al. Constitutive Activation of the PI3K-Akt-MTORC1 Pathway Sustains the m.3243 A > G MtDNA Mutation. Nat. Commun. 2021, 12, 6409. [Google Scholar] [CrossRef]
- Chung, C.Y.; Valdebenito, G.E.; Chacko, A.R.; Duchen, M.R. Rewiring Cell Signalling Pathways in Pathogenic MtDNA Mutations. Trends Cell Biol. 2022, 32, 391–405. [Google Scholar] [CrossRef]
- Sazonova, M.A.; Ryzhkova, A.I.; Sinyov, V.V.; Galitsyna, E.V.; Orekhova, V.A.; Melnichenko, A.A.; Orekhov, A.N.; Ravani, A.L.; Sobenin, I.A. New Markers of Atherosclerosis: A Threshold Level of Heteroplasmy in MtDNA Mutations. Vessel Plus 2017, 1, 182–191. [Google Scholar] [CrossRef]
- Zhou, M.; Xue, L.; Chen, Y.; Li, H.; He, Q.; Wang, B.; Meng, F.; Wang, M.; Guan, M.X. A Hypertension-Associated Mitochondrial DNA Mutation Introduces Anm1G37 Modification into TRNAMet, Altering Its Structure and Function. J. Biol. Chem. 2018, 293, 1425–1438. [Google Scholar] [CrossRef]
- Meng, F.; Jia, Z.; Zheng, J.; Ji, Y.; Wang, J.; Xiao, Y.; Fu, Y.; Wang, M.; Ling, F.; Guan, M.-X. A Deafness-Associated Mitochondrial DNA Mutation Caused Pleiotropic Effects on DNA Replication and TRNA Metabolism. Nucleic Acids Res. 2022, 50, 9453–9469. [Google Scholar] [CrossRef]
- Hippen, M.; Zsurka, G.; Peeva, V.; Machts, J.; Schwiecker, K.; Debska-Vielhaber, G.; Wiesner, R.J.; Vielhaber, S.; Kunz, W.S. Novel Pathogenic Sequence Variation m.5789T>C Causes NARP Syndrome and Promotes Formation of Deletions of the Mitochondrial Genome. Neurol. Genet. 2022, 8, e660. [Google Scholar] [CrossRef] [PubMed]
- Kripps, K.A.; Friederich, M.W.; Chen, T.; Larson, A.A.; Mirsky, D.M.; Wang, Y.; Tanji, K.; Knight, K.M.; Wong, L.J.; Van Hove, J.L.K. A Novel Acceptor Stem Variant in Mitochondrial TRNATyr Impairs Mitochondrial Translation and Is Associated with a Severe Phenotype. Mol. Genet. Metab. 2020, 131, 398–404. [Google Scholar] [CrossRef]
- Blakely, E.L.; Alston, C.L.; Lecky, B.; Chakrabarti, B.; Falkous, G.; Turnbull, D.M.; Taylor, R.W.; Gorman, G.S. Distal Weakness with Respiratory Insufficiency Caused by the m.8344A > G “MERRF” Mutation. Neuromuscul. Disord. 2014, 24, 533–536. [Google Scholar] [CrossRef] [PubMed]
- Enriquez, J.A.; Chomyn, A.; Attardi, G. MtDNA Mutation in MERRF Syndrome Causes Defective Aminoacylation of TRNALys and Premature Translation Termination. Nat. Genet. 1995, 10, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Jia, Z.; Zhang, Y.; Li, Q.; Ye, Z.; Liu, Y.; Fu, C.; Cang, X.; Wang, M.; Guan, M.X. A Coronary Artery Disease-Associated TRNAThr Mutation Altered Mitochondrial Function, Apoptosis and Angiogenesis. Nucleic Acids Res. 2019, 47, 2056–2074. [Google Scholar] [CrossRef]
- Ji, Y.; Zhang, J.; Yu, J.; Wang, Y.; Lu, Y.; Liang, M.; Li, Q.; Jin, X.; Wei, Y.; Meng, F.; et al. Contribution of Mitochondrial ND1 3394T>C Mutation to the Phenotypic Manifestation of Leber’s Hereditary Optic Neuropathy. Hum. Mol. Genet. 2019, 28, 1515–1529. [Google Scholar] [CrossRef]
- Cortés, N.G.; Pertuiset, C.; Dumon, E.; Börlin, M.; Da Costa, B.; Le Guédard, M.; Stojkovic, T.; Loundon, N.; Rouillon, I.; Nadjar, Y.; et al. Mutation m.3395A > G in MT-ND1 Leads to Variable Pathologic Manifestations. Hum. Mol. Genet. 2020, 29, 980–990. [Google Scholar] [CrossRef]
- Chen, S.; Bao, X.; Chen, H.; Jia, M.; Li, W.; Zhang, L.; Fan, R.; Fang, H.; Jin, L. Thyroid Cancer-Associated Mitochondrial DNA Mutation G3842A Promotes Tumorigenicity via ROS-Mediated ERK1/2 Activation. Oxid. Med. Cell. Longev. 2022, 2022, 9982449. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Kopajtich, R.; Elstner, M.; Li, H.; Liu, Z.; Wang, J.; Prokisch, H.; Fang, F. Identification of a Novel m.3955G > A Variant in MT-ND1 Associated with Leigh Syndrome. Mitochondrion 2022, 62, 13–23. [Google Scholar] [CrossRef]
- Ren, H.; Lin, Y.; Li, Y.; Zhang, X.; Wang, W.; Xu, X.; Ji, K.; Zhao, Y.; Yan, C. Leber’s Hereditary Optic Neuropathy plus Dystonia Caused by the Mitochondrial ND1 Gene m.4160 T > C Mutation. Neurol. Sci. 2022, 43, 5581–5592. [Google Scholar] [CrossRef]
- Sazonova, M.A.; Sinyov, V.V.; Ryzhkova, A.I.; Sazonova, M.D.; Khasanova, Z.B.; Sobenin, I.A. MtDNA Mutations Linked with Left Ventricular Hypertrophy. Vessel Plus 2019, 3, 5. [Google Scholar] [CrossRef]
- Sobenin, I.A.; Sazonova, M.A.; Postnov, A.Y.; Bobryshev, Y.V.; Orekhov, A.N. Mitochondrial Mutations Are Associated with Atherosclerotic Lesions in the Human Aorta. Clin. Dev. Immunol. 2012, 2012, 832464. [Google Scholar] [CrossRef]
- Ji, Y.; Zhang, J.; Lu, Y.; Yi, Q.; Chen, M.; Xie, S.; Mao, X.; Xiao, Y.; Meng, F.; Zhang, M.; et al. Complex I Mutations Synergize to Worsen the Phenotypic Expression of Leber’s Hereditary Optic Neuropathy. J. Biol. Chem. 2020, 295, 13224–13238. [Google Scholar] [CrossRef]
- Jankauskaitė, E.; Ambroziak, A.M.; Hajieva, P.; Ołdak, M.; Tońska, K.; Korwin, M.; Bartnik, E.; Kodroń, A. Testosterone Increases Apoptotic Cell Death and Decreases Mitophagy in Leber’s Hereditary Optic Neuropathy Cells. J. Appl. Genet. 2020, 61, 195–203. [Google Scholar] [CrossRef]
- Galera-Monge, T.; Zurita-Díaz, F.; Canals, I.; Hansen, M.G.; Rufián-Vázquez, L.; Ehinger, J.K.; Elmér, E.; Martin, M.A.; Garesse, R.; Ahlenius, H.; et al. Mitochondrial Dysfunction and Calcium Dysregulation in Leigh Syndrome Induced Pluripotent Stem Cell Derived Neurons. Int. J. Mol. Sci. 2020, 21, 3191. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Ji, K.; Lin, Y.; Xu, X.; Wang, W.; Li, Y.; Lu, J.Q.; Zhao, Y.; Yan, C. Leber Hereditary Optic Neuropathy and Dystonia Overlapping Mitochondrial Encephalomyopathy with Lactic Acidosis and Stroke-like Episodes Due to m.14459G>A Mutation. Neurol. Sci. 2021, 42, 5123–5130. [Google Scholar] [CrossRef] [PubMed]
- Kishita, Y.; Ishikawa, K.; Nakada, K.; Hayashi, J.I.; Fushimi, T.; Shimura, M.; Kohda, M.; Ohtake, A.; Murayama, K.; Okazaki, Y. A High Mutation Load of m.14597A>G in MT-ND6 Causes Leigh Syndrome. Sci. Rep. 2021, 11, 11123. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Sun, Y.; Zhuang, Q.; Song, Y.; Wu, B.; Jia, Z.; Pan, H.; Zhou, H.; Hu, S.; Zhang, B.; et al. Mitochondrial Dysfunction Caused by m.2336T>C Mutation with Hypertrophic Cardiomyopathy in Cybrid Cell Lines. Mitochondrion 2019, 46, 313–320. [Google Scholar] [CrossRef]
- Skoczeń, N.; Dautant, A.; Binko, K.; Godard, F.; Bouhier, M.; Su, X.; Lasserre, J.P.; Giraud, M.F.; Tribouillard-Tanvier, D.; Chen, H.; et al. Molecular Basis of Diseases Caused by the MtDNA Mutation m.8969G>A in the Subunit a of ATP Synthase. Biochim. Biophys. Acta-Bioenerg. 2018, 1859, 602–611. [Google Scholar] [CrossRef]
- Su, X.; Dautant, A.; Godard, F.; Bouhier, M.; Zoladek, T.; Kucharczyk, R.; Rago, J.P.D.; Tribouillard-Tanvier, D. Molecular Basis of the Pathogenic Mechanism Induced by the m.9191t>c Mutation in Mitochondrial Atp6 Gene. Int. J. Mol. Sci. 2020, 21, 5083. [Google Scholar] [CrossRef]
- Kasinathan, D.; Matrougui, K.; Elango, S.; Belmandani, S.; Srinivas, B.; Muthusamy, K.; Narayanasamy Marimuthu, P. Mitochondrial ATP6 and ND3 Genes Are Associated with Type 2 Diabetic Peripheral Neuropathy. Diabetes Metab. Syndr. Clin. Res. Rev. 2022, 16, 102501. [Google Scholar] [CrossRef]
- Haumann, S.; Boix, J.; Knuever, J.; Bieling, A.; Vila Sanjurjo, A.; Elson, J.L.; Blakely, E.L.; Taylor, R.W.; Riet, N.; Abken, H.; et al. Mitochondrial DNA Mutations Induce Mitochondrial Biogenesis and Increase the Tumorigenic Potential of Hodgkin and Reed-Sternberg Cells. Carcinogenesis 2020, 41, 1735–1745. [Google Scholar] [CrossRef]
- Ng, Y.S.; Thompson, K.; Loher, D.; Hopton, S.; Falkous, G.; Hardy, S.A.; Schaefer, A.M.; Shaunak, S.; Roberts, M.E.; Lilleker, J.B.; et al. Novel MT-ND Gene Variants Causing Adult-Onset Mitochondrial Disease and Isolated Complex I Deficiency. Front. Genet. 2020, 11, 24. [Google Scholar] [CrossRef] [PubMed]
- Danese, A.; Patergnani, S.; Maresca, A.; Peron, C.; Raimondi, A.; Caporali, L.; Marchi, S.; La Morgia, C.; Del Dotto, V.; Zanna, C.; et al. Pathological Mitophagy Disrupts Mitochondrial Homeostasis in Leber’s Hereditary Optic Neuropathy. Cell Rep. 2022, 40, 111124. [Google Scholar] [CrossRef]
- Greaves, L.C.; Yu-Wai-Man, P.; Blakely, E.L.; Krishnan, K.J.; Beadle, N.E.; Kerin, J.; Barron, M.J.; Griffiths, P.G.; Dickinson, A.J.; Turnbull, D.M.; et al. Mitochondrial DNA Defects and Selective Extraocular Muscle Involvement in CPEO. Investig. Ophthalmol. Vis. Sci. 2010, 51, 3340–3346. [Google Scholar] [CrossRef]
- Ogasawara, E.; Nakada, K.; Ishihara, N. Distal Control of Mitochondrial Biogenesis and Respiratory Activity by Extracellular Lactate Caused by Large-Scale Deletion of Mitochondrial DNA. Pharmacol. Res. 2020, 160, 105204. [Google Scholar] [CrossRef] [PubMed]
- Bakare, A.B.; Dean, J.; Chen, Q.; Thorat, V.; Huang, Y.; Laframboise, T.; Lesnefsky, E.J.; Iyer, S. Evaluating the Bioenergetics Health Index Ratio in Leigh Syndrome Fibroblasts to Understand Disease Severity. Int. J. Mol. Sci. 2021, 22, 10344. [Google Scholar] [CrossRef]
- Evangelisti, S.; Gramegna, L.L.; La Morgia, C.; Di Vito, L.; Maresca, A.; Talozzi, L.; Bianchini, C.; Mitolo, M.; Manners, D.N.; Caporali, L.; et al. Molecular Biomarkers Correlate with Brain Grey and White Matter Changes in Patients with Mitochondrial m.3243A > G Mutation. Mol. Genet. Metab. 2022, 135, 72–81. [Google Scholar] [CrossRef]
- Bakare, A.B.; Daniel, J.; Stabach, J.; Rojas, A.; Bell, A.; Henry, B.; Iyer, S. Quantifying Mitochondrial Dynamics in Patient Fibroblasts with Multiple Developmental Defects and Mitochondrial Disorders. Int. J. Mol. Sci. 2021, 22, 6263. [Google Scholar] [CrossRef]
- Orekhov, A.N.; Nikiforov, N.G.; Omelchenko, A.V.; Sinyov, V.V.; Sobenin, I.A.; Vinokurov, A.Y.; Orekhova, V.A. The Role of Mitochondrial Mutations in Chronification of Inflammation: Hypothesis and Overview of Own Data. Life 2022, 12, 1153. [Google Scholar] [CrossRef]
- Wang, J.; Xu, J.; Xia, M.; Yang, Y.; Shen, Z.; Chen, G.; Dong, R.; Zheng, S. Correlation between Hepatic Oxidative Damage and Clinical Severity and Mitochondrial Gene Sequencing Results in Biliary Atresia. Hepatol. Res. 2019, 49, 695–704. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.Y.; Li, X.Y.; Li, Z.Q.; Song, J.Q.; Hou, J.; Li, J.H.; Sun, L.; Jiang, J.; Yang, Y.L. Clinical, Biochemical, and Genetic Analysis of the Mitochondrial Respiratory Chain Complex i Deficiency. Medicine 2018, 97, e11606. [Google Scholar] [CrossRef]
- Yin, Z.; Burger, N.; Kula-Alwar, D.; Aksentijević, D.; Bridges, H.R.; Prag, H.A.; Grba, D.N.; Viscomi, C.; James, A.M.; Mottahedin, A.; et al. Structural Basis for a Complex I Mutation That Blocks Pathological ROS Production. Nat. Commun. 2021, 12, 707. [Google Scholar] [CrossRef]
- Raimundo, N.; Song, L.; Shutt, T.E.; McKay, S.E.; Cotney, J.; Guan, M.X.; Gilliland, T.C.; Hohuan, D.; Santos-Sacchi, J.; Shadel, G.S. Mitochondrial Stress Engages E2F1 Apoptotic Signaling to Cause Deafness. Cell 2012, 148, 716–726. [Google Scholar] [CrossRef]
- Wolstenholme, D.R. Animal Mitochondrial DNA: Structure and Evolution. Int. Rev. Cytol. 1992, 141, 173–216. [Google Scholar] [CrossRef] [PubMed]
- Ruhoy, I.S.; Saneto, R.P. The Genetics of Leigh Syndrome and Its Implications for Clinical Practice and Risk Management. Appl. Clin. Genet. 2014, 7, 221–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kruse, S.E.; Watt, W.C.; Marcinek, D.J.; Kapur, R.P.; Schenkman, K.A.; Palmiter, R.D. Mice with Mitochondrial Complex I Deficiency Develop a Fatal Encephalomyopathy. Cell Metab. 2008, 7, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Jain, I.H.; Goldberger, O.; Rezoagli, E.; Thoonen, R.; Chen, K.H.; Sosnovik, D.E.; Scherrer-Crosbie, M.; Mootha, V.K.; Zapol, W.M. Hypoxia Treatment Reverses Neurodegenerative Disease in a Mouse Model of Leigh Syndrome. Proc. Natl. Acad. Sci. USA 2017, 114, E4241–E4250. [Google Scholar] [CrossRef]
- Silva-Pinheiro, P.; Cerutti, R.; Luna-Sanchez, M.; Zeviani, M.; Viscomi, C. A Single Intravenous Injection of AAV-PHP.B-HNDUFS4 Ameliorates the Phenotype of Ndufs4−/− Mice. Mol. Ther.-Methods Clin. Dev. 2020, 17, 1071–1078. [Google Scholar] [CrossRef]
- Quadalti, C.; Brunetti, D.; Lagutina, I.; Duchi, R.; Perota, A.; Lazzari, G.; Cerutti, R.; Di Meo, I.; Johnson, M.; Bottani, E.; et al. SURF1 Knockout Cloned Pigs: Early Onset of a Severe Lethal Phenotype. Biochim. Biophys. Acta-Mol. Basis Dis. 2018, 1864, 2131–2142. [Google Scholar] [CrossRef]
- Dell’Agnello, C.; Leo, S.; Agostino, A.; Szabadkai, G.; Tiveron, C.C.; Zulian, A.A.; Prelle, A.; Roubertoux, P.; Rizzuto, R.; Zeviani, M. Increased Longevity and Refractoriness to Ca(2+)-Dependent Neurodegeneration in Surf1 Knockout Mice. Hum. Mol. Genet. 2007, 16, 431–444. [Google Scholar] [CrossRef] [PubMed]
- Swerdlow, R.H.; Parks, J.K.; Miller, S.W.; Tuttle, J.B.; Trimmer, P.A.; Sheehan, J.P.; Bennett, J.P.; Davis, R.E.; Parker, W.D. Origin and Functional Consequences of the Complex I Defect in Parkinson’s Disease. Ann. Neurol. 1996, 40, 663–671. [Google Scholar] [CrossRef]
- Swerdlow, R.H. Does Mitochondrial DNA Play a Role in Parkinson’s Disease? A Review of Cybrid and Other Supportive Evidence. Antioxid. Redox Signal. 2012, 16, 950–964. [Google Scholar] [CrossRef]
- Sazonova, M.A.; Sinyov, V.V.; Ryzhkova, A.I.; Sazonova, M.D.; Khasanova, Z.B.; Shkurat, T.P.; Karagodin, V.P.; Orekhov, A.N.; Sobenin, I.A. Creation of Cybrid Cultures Containing Mtdna Mutations m.12315G>a and m.1555G>a, Associated with Atherosclerosis. Biomolecules 2019, 9, 499. [Google Scholar] [CrossRef]
- Picard, M.; Zhang, J.; Hancock, S.; Derbeneva, O.; Golhar, R.; Golik, P.; O’Hearn, S.; Levy, S.; Potluri, P.; Lvova, M.; et al. Progressive Increase in MtDNA 3243A>G Heteroplasmy Causes Abrupt Transcriptional Reprogramming. Proc. Natl. Acad. Sci. USA 2014, 111, E4033–E4042. [Google Scholar] [CrossRef]
- Chomyn, A.; Martinuzzi, A.; Yoneda, M.; Daga, A.; Hurko, O.; Johns, D.; Lai, S.T.; Nonaka, I.; Angelini, C.; Attardi, G. MELAS Mutation in MtDNA Binding Site for Transcription Termination Factor Causes Defects in Protein Synthesis and in Respiration but No Change in Levels of Upstream and Downstream Mature Transcripts. Proc. Natl. Acad. Sci. USA 1992, 89, 4221–4225. [Google Scholar] [CrossRef] [Green Version]
- Koga, Y.; Davidson, M.; Schon, E.A.; King, M.P. Analysis of Cybrids Harboring MELAS Mutations in the Mitochondrial tRNALeu(UUR) Gene. Muscle Nerve 1995, 18, S119–S123. [Google Scholar] [CrossRef]
- Brown, M.D.; Trounce, I.A.; Jun, A.S.; Allen, J.C.; Wallace, D.C. Functional Analysis of Lymphoblast and Cybrid Mitochondria Containing the 3460, 11778, or 14484 Leber’s Hereditary Optic Neuropathy Mitochondrial DNA Mutation. J. Biol. Chem. 2000, 275, 39831–39836. [Google Scholar] [CrossRef]
- Trounce, I.; Neill, S.; Wallace, D.C. Cytoplasmic Transfer of the MtDNA Nt 8993 T → G (ATP6) Point Mutation Associated with Leigh Syndrome into MtDNA-Less Cells Demonstrates Cosegregation with a Decrease in State III Respiration and ADP/O Ratio. Proc. Natl. Acad. Sci. USA 1994, 91, 8334–8338. [Google Scholar] [CrossRef] [PubMed]
- Vergani, L.; Rossi, R.; Brierley, C.H.; Hanna, M.; Holt, I.J. Introduction of Heteroplasmic Mitochondrial DNA (MtDNA) from a Patient with NARP into Two Human ρ° Cell Lines Is Associated Either with Selection and Maintenance of NARP Mutant MtDNA or Failure to Maintain MtDNA. Hum. Mol. Genet. 1999, 8, 1751–1755. [Google Scholar] [CrossRef]
- Masucci, J.P.; Davidson, M.; Koga, Y.; Schon, E.A.; King, M.P. In Vitro Analysis of Mutations Causing Myoclonus Epilepsy with Ragged-Red Fibers in the Mitochondrial TRNA(Lys)Gene: Two Genotypes Produce Similar Phenotypes. Mol. Cell. Biol. 1995, 15, 2872–2881. [Google Scholar] [CrossRef] [PubMed]
- Orekhov, A.N.; Nikiforov, N.N.; Ivanova, E.A.; Sobenin, I.A. Possible Role of Mitochondrial DNA Mutations in Chronification of Inflammation: Focus on Atherosclerosis. J. Clin. Med. 2020, 9, 978. [Google Scholar] [CrossRef]
- Tani, H.; Ishikawa, K.; Tamashiro, H.; Ogasawara, E.; Yasukawa, T.; Matsuda, S.; Shimizu, A.; Kang, D.; Hayashi, J.-I.; Wei, F.-Y.; et al. Aberrant RNA Processing Contributes to the Pathogenesis of Mitochondrial Diseases in Trans -Mitochondrial Mouse Model Carrying Mitochondrial tRNALeu(UUR) with a Pathogenic A2748G Mutation. Nucleic Acids Res. 2022, 50, 9382–9396. [Google Scholar] [CrossRef]
- Ding, Y.U.; Zhuo, G.; Zhang, C. The Mitochondrial tRNALeu(UUR) A3302G Mutation May Be Associated with Insulin Resistance in Woman with Polycystic Ovary Syndrome. Reprod. Sci. 2016, 23, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Goto, M.; Komaki, H.; Saito, T.; Saito, Y.; Nakagawa, E.; Sugai, K.; Sasaki, M.; Nishino, I.; Goto, Y. ichi MELAS Phenotype Associated with m.3302A>G Mutation in Mitochondrial tRNALeu(UUR) Gene. Brain Dev. 2014, 36, 180–182. [Google Scholar] [CrossRef]
- Ballhausen, D.; Guerry, F.; Hahn, D.; Schaller, A.; Nuoffer, J.M.; Bonafé, L.; Jeannet, P.Y.; Jacquemont, S. Mitochondrial tRNALeu(UUR) Mutation m.3302A>G Presenting as Childhood-Onset Severe Myopathy: Threshold Determination through Segregation Study. J. Inherit. Metab. Dis. 2010, 33, 219–226. [Google Scholar] [CrossRef] [Green Version]
- Hutchison, W.M.; Thyagarajan, D.; Poulton, J.; Marchington, D.R.; Kirby, D.M.; Manji, S.S.M.; Dahl, H.H.M. Clinical and Molecular Features of Encephalomyopathy Due to the A3302G Mutation in the Mitochondrial tRNALeu(UUR) Gene. Arch. Neurol. 2005, 62, 1920–1923. [Google Scholar] [CrossRef] [PubMed]
- Kasahara, A.; Ishikawa, K.; Yamaoka, M.; Ito, M.; Watanabe, N.; Akimoto, M.; Sato, A.; Nakada, K.; Endo, H.; Suda, Y.; et al. Generation of Trans-Mitochondrial Mice Carrying Homoplasmic MtDNAs with a Missense Mutation in a Structural Gene Using ES Cells. Hum. Mol. Genet. 2006, 15, 871–881. [Google Scholar] [CrossRef] [PubMed]
- Hashizume, O.; Shimizu, A.; Yokota, M.; Sugiyama, A.; Nakada, K.; Miyoshi, H.; Itami, M.; Ohira, M.; Nagase, H.; Takenaga, K.; et al. Specific Mitochondrial DNA Mutation in Mice Regulates Diabetes and Lymphoma Development. Proc. Natl. Acad. Sci. USA 2012, 109, 10528–10533. [Google Scholar] [CrossRef]
- Shimizu, A.; Mito, T.; Hashizume, O.; Yonekawa, H.; Ishikawa, K.; Nakada, K.; Hayashi, J.I. G7731A Mutation in Mouse Mitochondrial TRNALys Regulates Late-Onset Disorders in Transmitochondrial Mice. Biochem. Biophys. Res. Commun. 2015, 459, 66–70. [Google Scholar] [CrossRef]
- McKnight, C.L.; Low, Y.C.; Elliott, D.A.; Thorburn, D.R.; Frazier, A.E. Modelling Mitochondrial Disease in Human Pluripotent Stem Cells: What Have We Learned? Int. J. Mol. Sci. 2021, 22, 7730. [Google Scholar] [CrossRef]
- Lin, D.S.; Huang, Y.W.; Ho, C.S.; Hung, P.L.; Hsu, M.H.; Wang, T.J.; Wu, T.Y.; Lee, T.H.; Huang, Z.D.; Chang, P.C.; et al. Oxidative Insults and Mitochondrial DNA Mutation Promote Enhanced Autophagy and Mitophagy Compromising Cell Viability in Pluripotent Cell Model of Mitochondrial Disease. Cells 2019, 8, 65. [Google Scholar] [CrossRef]
- Kodaira, M.; Hatakeyama, H.; Yuasa, S.; Seki, T.; Egashira, T.; Tohyama, S.; Kuroda, Y.; Tanaka, A.; Okata, S.; Hashimoto, H.; et al. Impaired Respiratory Function in MELAS-Induced Pluripotent Stem Cells with High Heteroplasmy Levels. FEBS Open Bio 2015, 5, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Lorenz, C.; Lesimple, P.; Bukowiecki, R.; Zink, A.; Inak, G.; Mlody, B.; Singh, M.; Semtner, M.; Mah, N.; Auré, K.; et al. Human IPSC-Derived Neural Progenitors Are an Effective Drug Discovery Model for Neurological MtDNA Disorders. Cell Stem Cell 2017, 20, 659–674.e9. [Google Scholar] [CrossRef]
- Yang, Y.P.; Nguyen, P.N.N.; Lin, T.C.; Yarmishyn, A.A.; Chen, W.S.; Hwang, D.K.; Chiou, G.Y.; Lin, T.W.; Chien, C.S.; Tsai, C.Y.; et al. Glutamate Stimulation Dysregulates Ampa Receptors-Induced Signal Transduction Pathway in Leber’s Inherited Optic Neuropathy Patient-Specific Hipsc-Derived Retinal Ganglion Cells. Cells 2019, 8, 625. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.C.; Yarmishyn, A.A.; Yang, Y.P.; Lu, P.C.; Chou, S.J.; Wang, M.L.; Lin, T.C.; Hwang, D.K.; Chou, Y.B.; Chen, S.J.; et al. Mitochondrial Transport Mediates Survival of Retinal Ganglion Cells in Affected LHON Patients. Hum. Mol. Genet. 2020, 29, 1454–1464. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.R.; Wang, A.G.; Chen, Y.T.; Yarmishyn, A.A.; Buddhakosai, W.; Yang, T.C.; Hwang, D.K.; Yang, Y.P.; Shen, C.N.; Lee, H.C.; et al. Bioactivity and Gene Expression Profiles of HiPSC-Generated Retinal Ganglion Cells in MT-ND4 Mutated Leber’s Hereditary Optic Neuropathy. Exp. Cell Res. 2018, 363, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.C.B.; Lim, S.Y.; Hung, S.S.C.; Jackson, S.; Khan, S.; Van Bergen, N.J.; De Smit, E.; Liang, H.H.; Kearns, L.S.; Clarke, L.; et al. Mitochondrial Replacement in an IPSC Model of Leber’s Hereditary Optic Neuropathy. Aging 2017, 9, 1341–1350. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Qi, Y.; French, S.; Zhang, G.; Garcia, R.C.; Balaban, R.; Xu, H. Genetic Mosaic Analysis of a Deleterious Mitochondrial DNA Mutation in Drosophila Reveals Novel Aspects of Mitochondrial Regulation and Function. Mol. Biol. Cell 2015, 26, 674–684. [Google Scholar] [CrossRef]
- Xu, H.; DeLuca, S.Z.; O’Farrell, P.H. Manipulating the Metazoan Mitochondrial Genome with Targeted Restriction Enzymes. Science 2008, 321, 575–577. [Google Scholar] [CrossRef]
- Srivastava, S.; Moraes, C.T. Manipulating Mitochondrial DNA Heteroplasmy by a Mitochondrially Targeted Restriction Endonuclease. Hum. Mol. Genet. 2001, 10, 3093–3099. [Google Scholar] [CrossRef]
- Peeva, V.; Blei, D.; Trombly, G.; Corsi, S.; Szukszto, M.J.; Rebelo-Guiomar, P.; Gammage, P.A.; Kudin, A.P.; Becker, C.; Altmüller, J.; et al. Linear Mitochondrial DNA Is Rapidly Degraded by Components of the Replication Machinery. Nat. Commun. 2018, 9, 1727. [Google Scholar] [CrossRef]
- Bian, W.P.; Chen, Y.L.; Luo, J.J.; Wang, C.; Xie, S.L.; Pei, D.S. Knock-In Strategy for Editing Human and Zebrafish Mitochondrial DNA Using Mito-CRISPR/Cas9 System. ACS Synth. Biol. 2019, 8, 621–632. [Google Scholar] [CrossRef]
- Bacman, S.R.; Williams, S.L.; Pinto, M.; Peralta, S.; Moraes, C.T. Specific Elimination of Mutant Mitochondrial Genomes in Patient-Derived Cells by MitoTALENs. Nat. Med. 2013, 19, 1111–1113. [Google Scholar] [CrossRef]
- Gammage, P.A.; Viscomi, C.; Simard, M.L.; Costa, A.S.H.; Gaude, E.; Powell, C.A.; Van Haute, L.; McCann, B.J.; Rebelo-Guiomar, P.; Cerutti, R.; et al. Genome Editing in Mitochondria Corrects a Pathogenic MtDNA Mutation in Vivo. Nat. Med. 2018, 24, 1691–1695. [Google Scholar] [CrossRef]
- Bacman, S.R.; Kauppila, J.H.K.; Pereira, C.V.; Nissanka, N.; Miranda, M.; Pinto, M.; Williams, S.L.; Larsson, N.G.; Stewart, J.B.; Moraes, C.T. MitoTALEN Reduces Mutant MtDNA Load and Restores TRNAAla Levels in a Mouse Model of Heteroplasmic MtDNA Mutation. Nat. Med. 2018, 24, 1696–1700. [Google Scholar] [CrossRef] [PubMed]
- Sukhorukov, V.N.; Kalmykov, V.A.; Khotina, V.A.; Sinyov, V.V.; Khasanova, Z.B.; Sobenin, I.A. Approach to Edit Mitochondrial DNA Mutations Associated with Atherosclerosis. Atherosclerosis 2021, 331, e70–e71. [Google Scholar] [CrossRef]
- Sukhorukov, V.N.; Kalmykov, V.A.; Khotina, V.A.; Omelchenko, A.V.; Orekhova, V.A.; Orekhov, A.N. Mitochondrial DNA CRISPR/CAS9 Editing: An Approach to Establishing the Role of Mitochondrial Mutations in Atherogenesis. Atherosclerosis 2022, 355, 53. [Google Scholar] [CrossRef]
- Gaudelli, N.M.; Komor, A.C.; Rees, H.A.; Packer, M.S.; Badran, A.H.; Bryson, D.I.; Liu, D.R. Programmable Base Editing of T to G C in Genomic DNA without DNA Cleavage. Nature 2017, 551, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Anzalone, A.V.; Randolph, P.B.; Davis, J.R.; Sousa, A.A.; Koblan, L.W.; Levy, J.M.; Chen, P.J.; Wilson, C.; Newby, G.A.; Raguram, A.; et al. Search-and-Replace Genome Editing without Double-Strand Breaks or Donor DNA. Nature 2019, 576, 149–157. [Google Scholar] [CrossRef]
- Gammage, P.A.; Moraes, C.T.; Minczuk, M. Mitochondrial Genome Engineering: The Revolution May Not Be CRISPR-Ized. Trends Genet. 2018, 34, 101–110. [Google Scholar] [CrossRef]
- Anzalone, A.V.; Koblan, L.W.; Liu, D.R. Genome Editing with CRISPR–Cas Nucleases, Base Editors, Transposases and Prime Editors. Nat. Biotechnol. 2020, 38, 824–844. [Google Scholar] [CrossRef]
- Mok, B.Y.; de Moraes, M.H.; Zeng, J.; Bosch, D.E.; Kotrys, A.V.; Raguram, A.; Hsu, F.S.; Radey, M.C.; Peterson, S.B.; Mootha, V.K.; et al. A Bacterial Cytidine Deaminase Toxin Enables CRISPR-Free Mitochondrial Base Editing. Nature 2020, 583, 631–637. [Google Scholar] [CrossRef]
- Mok, B.Y.; Kotrys, A.V.; Raguram, A.; Huang, T.P.; Mootha, V.K.; Liu, D.R. CRISPR-Free Base Editors with Enhanced Activity and Expanded Targeting Scope in Mitochondrial and Nuclear DNA. Nat. Biotechnol. 2022, 40, 1378–1387. [Google Scholar] [CrossRef]
- Cho, S.I.; Lee, S.; Mok, Y.G.; Lim, K.; Lee, J.; Lee, J.M.; Chung, E.; Kim, J.S. Targeted A-to-G Base Editing in Human Mitochondrial DNA with Programmable Deaminases. Cell 2022, 185, 1764–1776.e12. [Google Scholar] [CrossRef]
- Sabharwal, A.; Campbell, J.M.; Schwab, T.L.; WareJoncas, Z.; Wishman, M.D.; Ata, H.; Liu, W.; Ichino, N.; Hunter, D.E.; Bergren, J.D.; et al. A Primer Genetic Toolkit for Exploring Mitochondrial Biology and Disease Using Zebrafish. Genes 2022, 13, 1317. [Google Scholar] [CrossRef]
- Guo, J.; Zhang, X.; Chen, X.; Sun, H.; Dai, Y.; Wang, J.; Qian, X.; Tan, L.; Lou, X.; Shen, B. Precision Modeling of Mitochondrial Diseases in Zebrafish via DdCBE-Mediated MtDNA Base Editing. Cell Discov. 2021, 7, 78. [Google Scholar] [CrossRef]
- Virgilio, R.; Ronchi, D.; Bordoni, A.; Fassone, E.; Bonato, S.; Donadoni, C.; Torgano, G.; Moggio, M.; Corti, S.; Bresolin, N.; et al. Mitochondrial DNA G8363A Mutation in the TRNALys Gene: Clinical, Biochemical and Pathological Study. J. Neurol. Sci. 2009, 281, 85–92. [Google Scholar] [CrossRef]
- Jia, X.; Li, S.; Xiao, X.; Guo, X.; Zhang, Q. Mutations in MT-ND4, MT-ND6 and MT-ND1 Genes of 3013 Chinese Patients Suspected with Leber Hereditary Optic Neuropathy: A 20-Year Retrospective. Investig. Ophthalmol. Vis. Sci. 2016, 57, 6582. [Google Scholar]
- Shanske, S.; Coku, J.; Lu, J.; Ganesh, J.; Krishna, S.; Tanji, K.; Bonilla, E.; Naini, A.B.; Hirano, M.; DiMauro, S. The G13513A Mutation in the ND5 Gene of Mitochondrial DNA as a Common Cause of MELAS or Leigh Syndrome: Evidence from 12 Cases. Arch. Neurol. 2008, 65, 368–372. [Google Scholar] [CrossRef] [PubMed]
- Zsurka, G.; Schröder, R.; Kornblum, C.; Rudolph, J.; Wiesner, R.J.; Elger, C.E.; Kunz, W.S. Tissue Dependent Co-Segregation of the Novel Pathogenic G12276A Mitochondrial tRNALeu(CUN) Mutation with the A185G D-Loop Polymorphism. J. Med. Genet. 2004, 41, e124. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Chen, X.; Guo, J.; Zhang, X.; Sun, H.; Wang, J.; Qian, X.; Li, B.; Tan, L.; Yu, L.; et al. Precision Modeling of Mitochondrial Disease in Rats via DdCBE-Mediated MtDNA Editing. Cell Discov. 2021, 7, 95. [Google Scholar] [CrossRef] [PubMed]
- Anitori, R.; Manning, K.; Quan, F.; Weleber, R.G.; Buist, N.R.M.; Shoubridge, E.A.; Kennaway, N.G. Contrasting Phenotypes in Three Patients with Novel Mutations in Mitochondrial TRNA Genes. Mol. Genet. Metab. 2005, 84, 176–188. [Google Scholar] [CrossRef] [PubMed]
- Chol, M.; Lebon, S.; Bénit, P.; Chretien, D.; De Lonlay, P.; Goldenberg, A.; Odent, S.; Hertz-Pannier, L.; Vincent-Delorme, C.; Cormier-Daire, V.; et al. The Mitochondrial DNA G13513A MELAS Mutation in the NADH Dehydrogenase 5 Gene Is a Frequent Cause of Leigh-like Syndrome with Isolated Complex I Deficiency. J. Med. Genet. 2003, 40, 188–191. [Google Scholar] [CrossRef]
- Wei, Y.; Li, Z.; Xu, K.; Feng, H.; Xie, L.; Li, D.; Zuo, Z.; Zhang, M.; Xu, C.; Yang, H.; et al. Mitochondrial Base Editor DdCBE Causes Substantial DNA Off-Target Editing in Nuclear Genome of Embryos. Cell Discov. 2022, 8, 27. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, H.; Baek, G.; Namgung, E.; Park, J.M.; Kim, S.; Hong, S.; Kim, J.S. Enhanced Mitochondrial DNA Editing in Mice Using Nuclear-Exported TALE-Linked Deaminases and Nucleases. Genome Biol. 2022, 23, 211. [Google Scholar] [CrossRef] [PubMed]
- Sabharwal, A.; Kar, B.; Restrepo-Castillo, S.; Holmberg, S.R.; Mathew, N.D.; Kendall, B.L.; Cotter, R.P.; Warejoncas, Z.; Seiler, C.; Nakamaru-Ogiso, E.; et al. The FusX TALE Base Editor (FusXTBE) for Rapid Mitochondrial DNA Programming of Human Cells in Vitro and Zebrafish Disease Models in Vivo. Cris. J. 2021, 4, 799–821. [Google Scholar] [CrossRef]
- Hanna, M.G.; Nelson, I.P.; Rahman, S.; Lane, R.J.M.; Land, J.; Heales, S.; Cooper, M.J.; Schapira, A.H.V.; Morgan-Hughes, J.A.; Wood, N.W. Cytochrome c Oxidase Deficiency Associated with the First Stop-Codon Point Mutation in Human MtDNA. Am. J. Hum. Genet. 1998, 63, 29–36. [Google Scholar] [CrossRef]
- Koilkonda, R.D.; Guy, J. Leber’s Hereditary Optic Neuropathy-Gene Therapy: From Benchtop to Bedside. J. Ophthalmol. 2011, 2011, 179412. [Google Scholar] [CrossRef]
- Rak, M.; Bénit, P.P.; Chrétien, D.; Bouchereau, J.; Schiff, M.; El-Khoury, R.; Tzagoloff, A.; Rustin, P. Mitochondrial Cytochrome c Oxidase Deficiency. Clin. Sci. 2016, 130, 393–407. [Google Scholar] [CrossRef]
- Ciafaloni, E.; Ricci, E.; Shanske, S.; Moraes, C.T.; Silvestri, G.; Hirano, M.; Simonetti, S.; Angelini, C.; Donati, M.A.; Garcia, C.; et al. MELAS: Clinical Features, Biochemistry, and Molecular Genetics. Ann. Neurol. 1992, 31, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Niedermayr, K.; Pölzl, G.; Scholl-Bürgi, S.; Fauth, C.; Schweigmann, U.; Haberlandt, E.; Albrecht, U.; Zlamy, M.; Sperl, W.; Mayr, J.A.; et al. Mitochondrial DNA Mutation “m.3243A>G”—Heterogeneous Clinical Picture for Cardiologists (“m.3243A>G”: A Phenotypic Chameleon). Congenit. Heart Dis. 2018, 13, 671–677. [Google Scholar] [CrossRef]
- Chakrabarty, S.; Govindaraj, P.; Sankaran, B.P.; Nagappa, M.; Kabekkodu, S.P.; Jayaram, P.; Mallya, S.; Deepha, S.; Ponmalar, J.N.J.; Arivinda, H.R.; et al. Contribution of Nuclear and Mitochondrial Gene Mutations in Mitochondrial Encephalopathy, Lactic Acidosis, and Stroke-like Episodes (MELAS) Syndrome. J. Neurol. 2021, 268, 2192–2207. [Google Scholar] [CrossRef]
- Kodroń, A.; Hajieva, P.; Kulicka, A.; Paterczyk, B.; Jankauskaite, E.; Bartnik, E. Analysis of BNIP3 and BNIP3L/Nix Expression in Cybrid Cell Lines Harboring Two LHON-Associated Mutations. Acta Biochim. Pol. 2019, 66, 427–435. [Google Scholar] [CrossRef]
| Clinical Syndrome | Clinical Symptoms and Complications | References |
|---|---|---|
| Leber Hereditary Optic Neuropathy (LHON) | Acute and painless central vision loss (optic atrophy) | [33] |
| Leigh syndrome | Bilateral symmetric necrotic lesions in the basal ganglia, brainstem and midbrain, hypotonia, epilepsy, respiratory stress, neurodevelopmental delay, ataxia, lactic acidosis, intellectual decline, movement disorders, headaches, memory loss | [34] |
| Mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes (MELAS) | Calcification in basal ganglia, cortical and cerebellar atrophy, stroke-like episodes, seizure, disturbance of consciousness, cognitive impairment, blindness, headache, myopathy, short stature, hemiplegia, cardiomyopathy, gait disturbance, teichopsia, speech disturbance, cerebellar ataxia, diabetes mellitus | [35] |
| Myoclonus epilepsy associated with ragged-red fibers (MERRF) | Myoclonus, myoclonic seizures, myopathy, sensorineural hearing loss, lipomatosis, dementia, generalized epilepsy, ataxia, ragged-red fibers in the muscle, peripheral neuropathy, renal dysfunction, cardiomyopathy | [36,37] |
| Maternally inherited diabetes and deafness (MIDD) | Diabetes mellitus, hearing loss | [38] |
| Neuropathy, ataxia and pigmentary retinopathy (NARP) | Peripheral neuropathy, ataxia, pigmentary retinopathy | [39] |
| Chronic progressive external ophthalmoplegia (CPEO) | Progressive loss of muscle activity (myopathy), progressive external ophthalmoplegia, ptosis, high-frequency sensorineural hearing loss, progressive dysphagia | [40] |
| Mutation | Gene | Associated Process | Disease | References |
|---|---|---|---|---|
| m.616T > C | tRNAPhe (MT-TF) | Abolishment of the highly conserved base pair A31-U39 in the anticodon stem reduces levels of ND1, ND4, CO1, CO3, CYTB and ATP8 | Isolated chronic kidney disease and hyperuricemia | [44,45] |
| m.3275C > T | tRNALeu (MT-TL1) | Decreased mtDNA content and mitochondrial membrane potential and 30% reduction in ATP production result in increased ROS production and possible oxidative stress in polymononuclear leukocytes | Polycystic ovary syndrome | [45,46] |
| m.4363T > C | tRNAGln (MT-TQ) | |||
| m.8343A > G | tRNALys (MT-TK) | |||
| m.3243A > G m.3271T > C m.3258T > C | tRNALeu (MT-TL1) | Decreased ATP production due to dysfunction of CI cannot support the energy consumption process of glutamate transport and leads to increased glutamate extracellular concentration and excitotoxicity | MELAS | [45,47,48] |
| m.3243A > G | Mutation-bearing cells have reduced expression of Mitochondrial Nuclear Retrograde Regulator 1 (MNRR1), which, in normal cells, stimulates mitochondrial unfolded protein response, autophagy and mitochondrial biogenesis | MELAS | [45,49] | |
| iPS-derived retinal pigment epithelium cells with high and low heteroplasmy levels are characterized by a decreased level of basal and CCCP-induced AMPKα activity and lysosomal function and diminished relative autophagy. Mitochondrial dysfunctions, including reduced respiration rate and ATP production, lead to a shift from oxidative phosphorylation to aerobic glycolysis | Age-related macular degeneration in MELAS | [45,50] | ||
| High heteroplasmy mutation level in iPS-derived cardiomyocytes leads to cardiomyopathy associated with reduced respiration rate and ATP production, increased ROS generation in matrix of mitochondria and dysregulation of energy-consuming process of calcium homeostasis | Cardiomyopathy | [45,51] | ||
| Decreased assembly of supercomplexes I2 + III2 + IVn, III2 + IV1 and III2/IV2 and decreased CII level modify glucose metabolism due to constitutive hyperactivation of the PI3K-Akt-mTORC1 pathway | Diabetes, sensorineural deafness and MELAS | [45,52] | ||
| Decreased mitochondrial oxygen consumption, mitochondrial membrane potential and ATP synthesis; increased NADH:NAD ratio | MIDD | [45,53] | ||
| m.3256C > T | Dysfunction of the mitochondrial ribosomes due to impossible separation of the newly synthesized proteins | Atherosclerosis | [54] | |
| m.4435A > G | tRNAMet (MT-TM) | Decreased levels of ND3, ND4, ND5, ATP6, ATP8, CYTB and CO2 | Hypertension | [45,55] |
| m.5783C > T | tRNACys (MT-TC) | Defective mtDNA replication and decreased mtDNA content lead to instability and reduced activity of the respiratory chain enzymes CI, CIII and CIV and intact supercomplexes | Deafness | [45,56] |
| m.5789T > C | Reduction in CI and CIV levels, cytochrome c oxidase deficiency in single skeletal muscle fibers and promotion of multiple mtDNA deletions through hybridization between different regions of the mitochondrial genome | NARP | [45,57] | |
| m.5889A > G | tRNALeu (MT-TL1) | Deficient cytochrome c oxidase function, lowered activity of CI and CIII with a tendency towards low activity of CIV and abnormal structure of CV in mitochondria of muscle, but not fibroblasts cells | Childhood-onset severe multi-system disorder characterized by a neurodegenerative course including ataxia and seizures, failure-to-thrive, combined myopathy and neuropathy, and hearing and vision loss | [45,58] |
| m.8344A > G m.8356T > C m.8361G > A m.8363G > A | tRNALys (MT-TK) | High COX deficiency and corresponding respiratory insufficiency; decrease in specific tRNALys aminoacylation capacity and premature termination of translation at or near each lysine codon | MERRF, CPEO | [37,45,59,60] |
| m.15927G > A | tRNAThr (MT-TT) | Reduced levels of ND1, ND3, ND4, ND5, CO2, CYTB, ATP6 and ATP8 | Coronary artery disease | [61] |
| m.3394T > C | ND1 (MT-ND1) | Reduced level, altered assembly and decreased activity of ND1 and subsequent increase in mitochondrial ROS generation and reduction in mitochondrial membrane potential and ATP production | LHON | [45,62] |
| m.3395A > G | Mitochondrial dysfunction development due to decreased CI quantity because of misfolding protein degradation by ATPase associated with diverse cellular activity of proteases anchored in the inner mitochondrial membrane | Deafness, diabetes and cerebellar syndrome | [45,63] | |
| m.3842G > A | Altered oxidative phosphorylation function leads to ROS-mediated activation of ERK1/2 signaling, increased cell proliferation, migration and invasion, resulting in metastasis promotion | Thyroid cancer | [64] | |
| m.3955G > A | Decreased levels of mtDNA-encoded CI subunits (MT-ND4 and MT-ND5) and NDUFB8, mitochondrial respiration activity and mitochondrial membrane potential and increased ROS production in mitochondrial matrix | Leigh syndrome | [65] | |
| m.4160T > C | Significant decrease of not only encoded ND1, but also ND4, ND5, ATP6 and nDNA-encoding subunits SDHB and NDUFB8, leads to basal respiration deficiency due to CI, CII and CIV dysfunctions | LHON plus dystonia | [45,66] | |
| m.5178C > A | ND2 (MT-ND2) | Defective function of CI, leading to decreased ATP synthesis and energy deficit | Atherosclerosis and left ventricular hypertrophy | [45,67,68] |
| m.11778G > A | ND4 (MT-ND4) | Destabilization of ND4 structure leads to reduced level of protein, deficient respiration activity, mitochondrial ATP production and mitochondrial membrane potential and increased rate of ROS production in matrix of mitochondria. Cells are characterized by decreased level of mitophagy and promotion of apoptosis. Mutation effect increases under testosterone influence | LHON | [45,69,70] |
| m.13513G > A | ND5 (MT-ND5) | Diminished respiration is associated with decreased mitochondrial mass but not decreased quantity of respiratory chain complexes. Mutant cells are characterized by altered calcium homeostasis due to buffering defect and increased refractory period of neurons | Leigh syndrome | [45,71] |
| m.14459G > A | ND6 (MT-ND6) | Decreased CI activity due to its incorrect assembly in immortalized lymphoblastic cell bearing 39.1% mutated gene | LHON and dystonia overlapping with MELAS episode phenotype | [45,72] |
| Energy deprivation due to CI dysfunction leads to atherosclerotic lesion development | Atherosclerosis | [45,54,68] | ||
| m.14597A > G | Replacement of Ile with Thr at 26 position leads to decreased CI activity in muscle tissue and skin fibroblasts, ATP production and oxygen consumption rate | Leigh syndrome | [45,73] | |
| m.15059G > A | CYTB (MT-CYTB) | Decreased protein length by 244 amino acids leads to CIII dysfunction and to development of atherosclerotic lesions | Atherosclerosis | [45,54,68] |
| m.652delG | 12S rRNA (MT-RNR1) | Mitochondrial ribosome dysfunction leads to decreased synthesis of respiratory chain proteins and ATP production, and subsequent energy failure in intimal cells of arteries | Atherosclerosis | [54] |
| m.1555A > G | Hypermethylation of mitochondrial ribosomes leads to deficient respiration and increased ROS production in matrix of mitochondria that activate AMPK, and subsequently, proapoptotic nuclear transcription factor E2F1 in the stria vascularis and spiral ganglion neurons of the inner ear | Deafness | [45,51] | |
| Decreased synthesis of respiratory chain proteins due to instability of mitochondrial ribosomes | Atherosclerosis and left ventricular hypertrophy | [45,67,68] | ||
| m.2336T > C | 16S rRNA (MT-RNR2) | Impaired ribosomal assembly due to decreased level of 16S rRNA and ribosomal proteins causes reduced steady-state level of some proteins of respiratory chain (ATP8 and CO2), decreased ATP production and mitochondrial membrane potential level, and elevation of ROS production in matrix of mitochondria | Hypertrophic cardiomyopathy | [45,74] |
| m.8969G > A | ATP6 (MT-ATP6) | Prevention of proton translocation through IMM | Isolated nephropathy followed by a complex clinical presentation with brain and muscle problems | [45,75] |
| m.9191T > C | 90% reduced ATP production prevents ATP synthase subunit a from adopting a stable conformation and makes it prone to proteolytic degradation | Leigh syndrome | [45,76] | |
| m.8597T > C | Oxidative stress due to elevated ROS production and diminished antioxidant status in peripheral mononuclear cells | Type 2 diabetic peripheral neuropathy | [77] | |
| m.8699T > C | ||||
| m.8966T > C | ||||
| m.10188A > G | ||||
| 9bp deletion | ND3 (MT-D3) COX2 (MT-CO2) tRNALys (MT-TK) | |||
| m.1782G > A | 16S rRNA (MT-RNR2) | Reduction in steady-state levels of COX1, COX2, COX4, NDUFA9, NDUFV2 and NDUFB8 leads to increased glycolysis rate, but also stimulated mitochondrial biogenesis, and no defects of mitochondrial function and respiratory rate, and as a result, acceleration of cell proliferation and tumor growth | Hodgkin’s lymphoma | [78] |
| m.8133C > T | COX2 (MTCO2) | |||
| m.14512_14513del | ND6 (MT-D6) | Dysfunction of CI due to loss of immunoreactive CI subunits (ND1, NDUFV1, NDUFS3 and NDUFB8) in muscle | Exercise intolerance, mild myopathy, deafness and relapsing–remitting neurological presentations | [45,79] |
| m.3761C > A | ND1 (MT-D1) | |||
| m.3460G > A | ND1 (MT-D1) | Excessive autophagy and mitophagy processes in patient-derived cells (fibroblasts, iPS neurons and osteosarcoma cell line-based cybrids) lead to defects in respiration chain and increased ROS production | LHON | [45,80] |
| m.11778G > A | ND4 (MT-D4) | |||
| Large-scale deletion of mtDNA | Decreased mitochondrial oxygen consumption, mitochondrial membrane potential and ATP synthesis; increased ROS production; COX deficiency | CPEO | [53,81] |
| Model Type | Disease | mtDNA Mutation | Approach | References |
|---|---|---|---|---|
| Cybrid cells | MELAS | m.3243A > G (MT-TL1) | Transmitochondrial technique | [48,49,101,103] |
| m.3271T > C (MT-TL1) | ||||
| m.14484T > C (MT-ND6) | [104] | |||
| m.3460G >A (MT-ND1) | ||||
| m.11778G > A (MT-ND4) | ||||
| Leigh syndrome NARP | m.8993T > G (MT-ATP6) | [105,106] | ||
| MERRF | m.8344A > G (MT-TK) | [107] | ||
| m.8356T > C (MT-TK) | ||||
| Hodgkin’s lymphoma | m.1555A > G (MT-RNR1) | [90] | ||
| Atherosclerosis | m.13513G > A (MT-ND5) m.12315G > A (MT-TL2) m.3256C > T (MT-TL1) m.15059G > A (MT-CYB) m.14846G > A (MT-CYB) m.1555G > A (MT-RNR1) | [86,100,108] | ||
| Induced pluripotent stem cells | MELAS | m.3243A > G (MT-TL1) | Isolation of fibroblasts or PBMCs from patients | [118,119] |
| Leigh syndrome | m.9185T > C (MT-ATP6) | [120] | ||
| m.13513G > A (MT-ND5) | [71] | |||
| LHON | m.11778G > A (MT-ND4) | [121,122,123] | ||
| m.4160T > C (MT-ND1) | [124] | |||
| m.14484T > C (MT-ND6) | ||||
| Drosophila melanogaster (fly) | Leigh syndrome MELAS | mt:CoIT300I and mt:CoIR301S (MT-COI) | MitoRE | [125,126] |
| mt:ND2Ins1 and mt:ND2Del1 (MT-ND2) | ||||
| Danio rerio (zebrafish) | MERRF-like syndrome Cardiomyopathy Leigh syndrome | m.8363G > A (MT-TK) | DdCBE | [143] |
| LHON | m.3733G > A (MT-ND1) | |||
| Leigh syndrome MELAS | m.13513G > A (MT-ND5) | |||
| CPEO | m.12276G > A (MT-TL1) | |||
| LHON | m.3376G > A (MT-ND1) | |||
| Leber optic atrophy Lactic acidosis Encephalopathy Myopathy | zebrafish m.7106C > T (MT-CO1) | FusXTBE | [153] | |
| zebrafish m.10215C > T (MT-CO3) | ||||
| MELAS | zebrafish m.3744G > A (MT-TL1) | |||
| Mouse C57BL/6J (mito-mice) | Polycystic ovary syn-drome with insulin resistance Childhood mitochondrial myopathy Encephalomyopathy MELAS | m.2748A > G (human m.3302A > G) (MT-TL1) | Transmitochondrial technique | [109,114] |
| m.6589T > C (MT-COI) | ||||
| Diabetes development Lymphoma formation and metastasis | m.13997G > A (MT-ND6) | [115] | ||
| MERRF | m.7731G > A (human m.8328G > A) (MT-TK) | [116] | ||
| Leigh disease MELAS LHON syndrome LHON/MELAS overlap syndrome | m.12918G > A (human m.13513G > A) (MT-ND5) | DdCBE DdCBE-NES Simultaneous use of DdCBE and mitoTALEN | [2,152] | |
| m.12336C > T (MT-ND5) | DdCBE | [2] | ||
| Rat (Sprague Dawley) | MELAS Cardiomyopathy Leigh syndrome | m.7755G > A (human m.8363G > A) (MT-TK) | DdCBE | [148] |
| Mitochondrial myopathy | m.14098G > A (human m.14710G > A) (MT-TE) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khotina, V.A.; Vinokurov, A.Y.; Bagheri Ekta, M.; Sukhorukov, V.N.; Orekhov, A.N. Creation of Mitochondrial Disease Models Using Mitochondrial DNA Editing. Biomedicines 2023, 11, 532. https://doi.org/10.3390/biomedicines11020532
Khotina VA, Vinokurov AY, Bagheri Ekta M, Sukhorukov VN, Orekhov AN. Creation of Mitochondrial Disease Models Using Mitochondrial DNA Editing. Biomedicines. 2023; 11(2):532. https://doi.org/10.3390/biomedicines11020532
Chicago/Turabian StyleKhotina, Victoria A., Andrey Y. Vinokurov, Mariam Bagheri Ekta, Vasily N. Sukhorukov, and Alexander N. Orekhov. 2023. "Creation of Mitochondrial Disease Models Using Mitochondrial DNA Editing" Biomedicines 11, no. 2: 532. https://doi.org/10.3390/biomedicines11020532








