Fabrication of a Smart Fibrous Biomaterial That Harbors an Active TGF-β1 Peptide: A Promising Approach for Cartilage Regeneration
Abstract
:1. Introduction
2. Materials and Methods
2.1. De Novo Synthesis of a Gene Encoding the Polypeptide [TGF-β1 Peptide—(ELP10-Silk2-Mussel15)2-Mussel-6xHis]
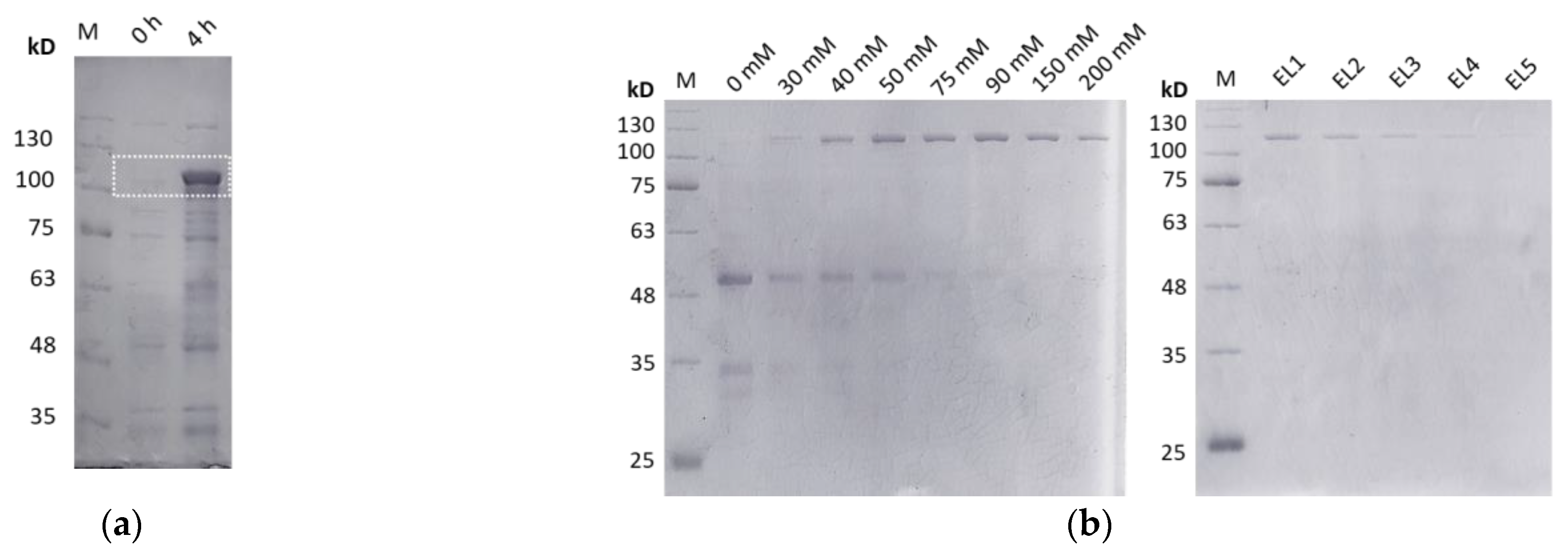
2.2. Overexpression and Purification of the Polypeptide [TGF-β1 Peptide—(ELP10-Silk2-Mussel15)2-Mussel-6xHis]
2.3. Crosslinking and Porous Scaffold Manufacturing
2.4. Rheological Measurements
2.5. Imaging of Surface Morphology by Scanning Electron Microscopy (SEM)
2.6. Culture of Human Dental Pulp Stem Cells on the Scaffolds
2.7. MTT Assay
2.8. BrdU Assay
2.9. Alcian Blue Staining Assay
2.10. SEM Analysis
2.11. RNA Isolation and cDNA Synthesis
2.12. Real-Time PCR
2.13. Protein Extracts and Western Blotting Analysis
2.14. Statistical Analysis
3. Results
3.1. Synthesis of Biomaterial with Elastin, Silk Fibroin, and Mussel-Foot Adhesive Protein Properties That Contains a Genetically Incorporated TGF-β1 Peptide
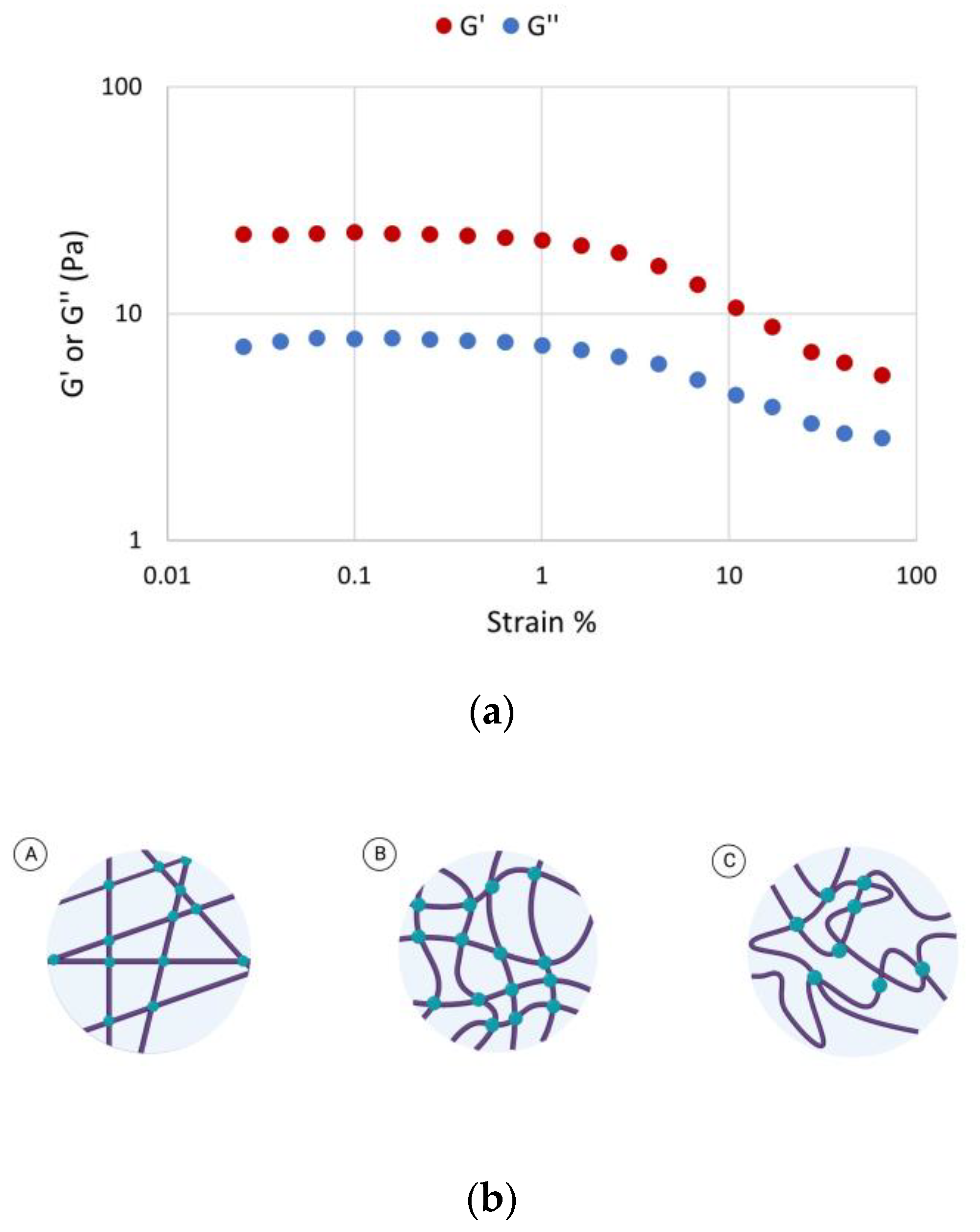
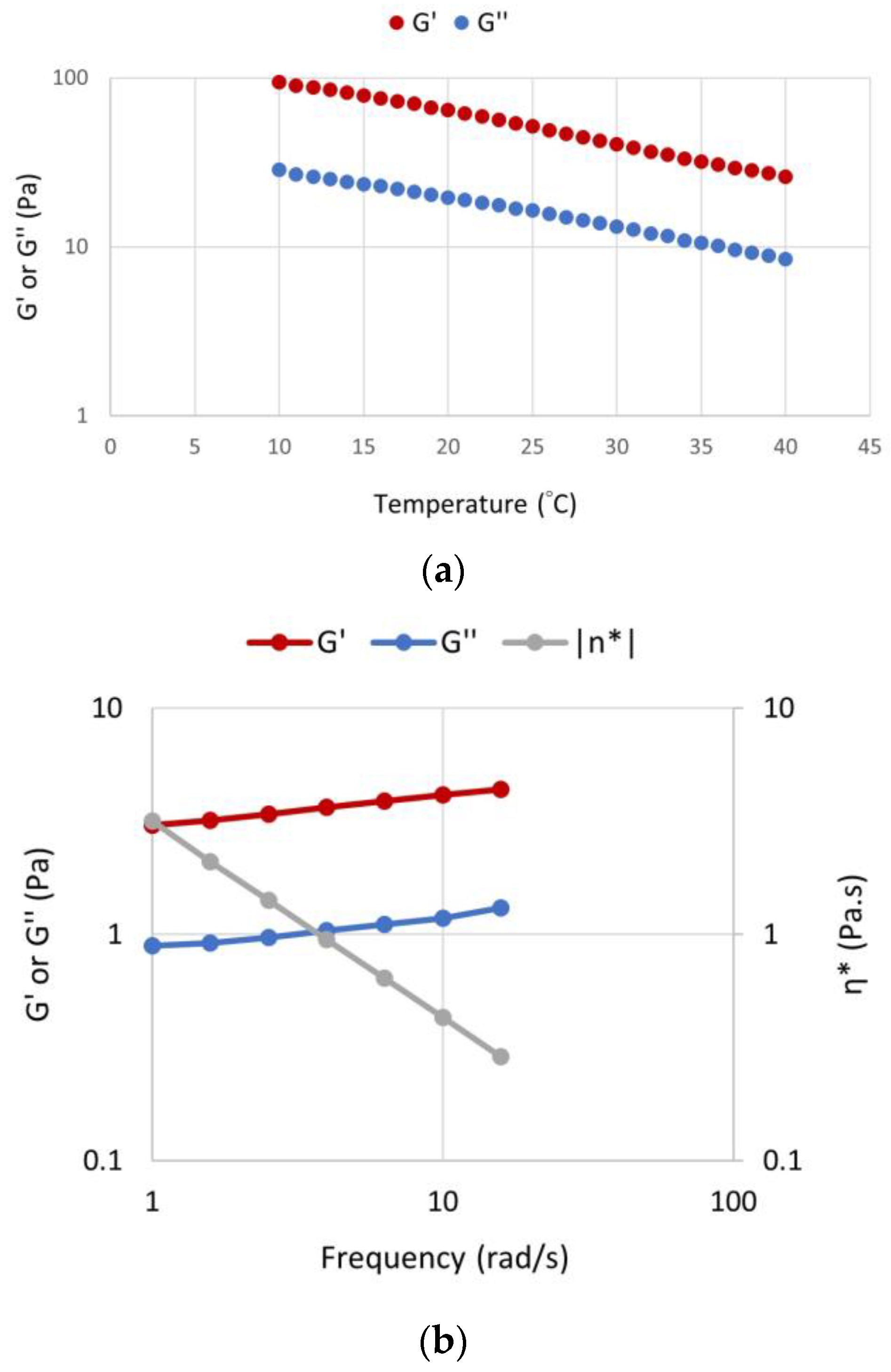
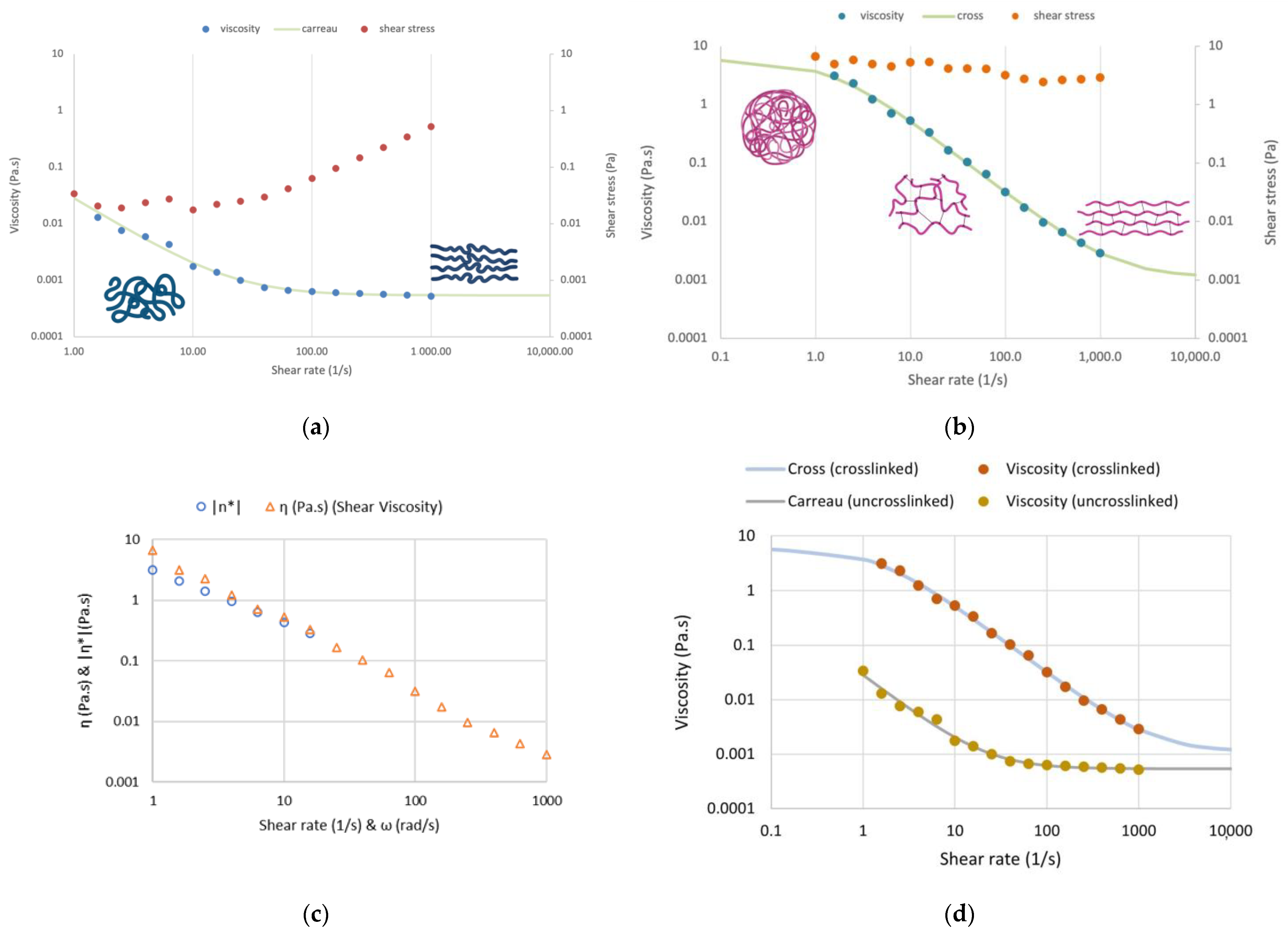
3.2. Rheological Characterization
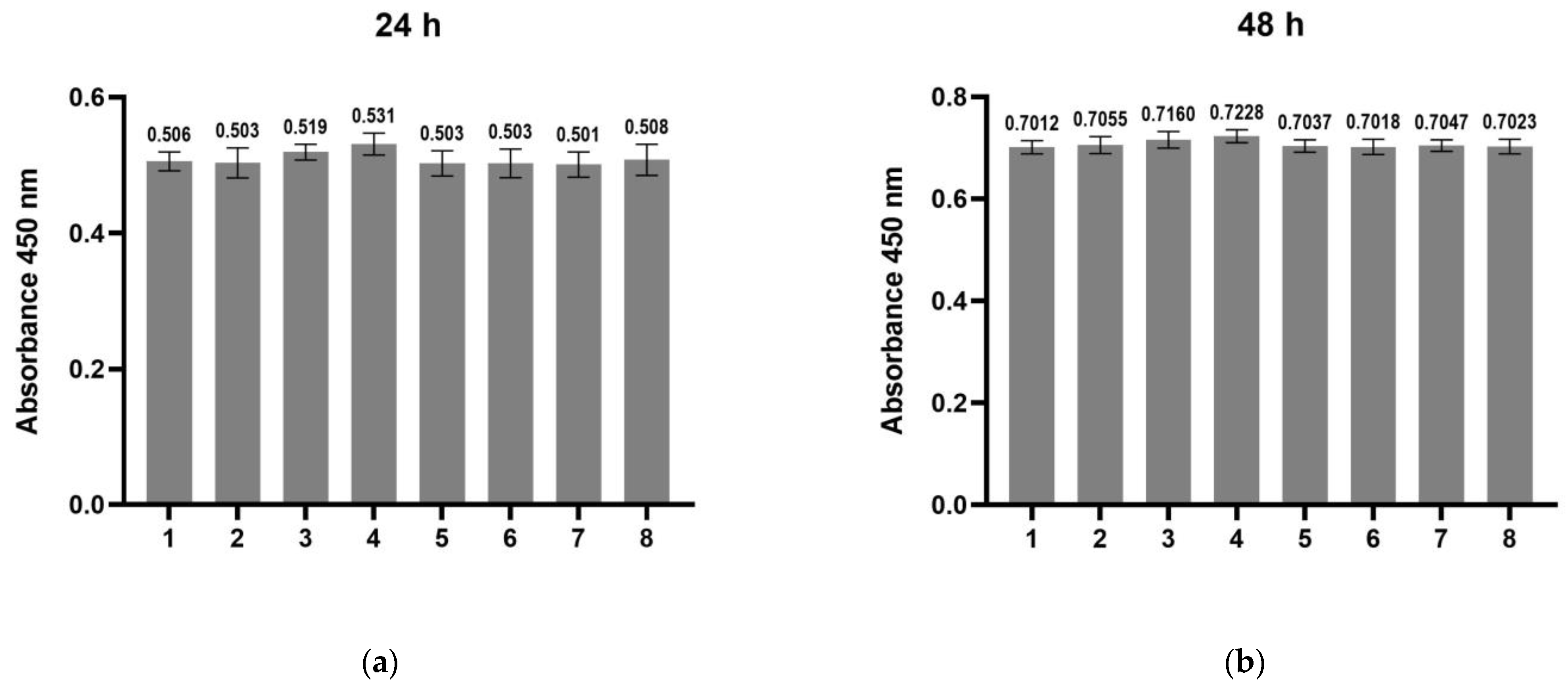
3.3. Assessment of Cytotoxicity of the Scaffolds on hDPSCs and of Their Effect on Cell Proliferation
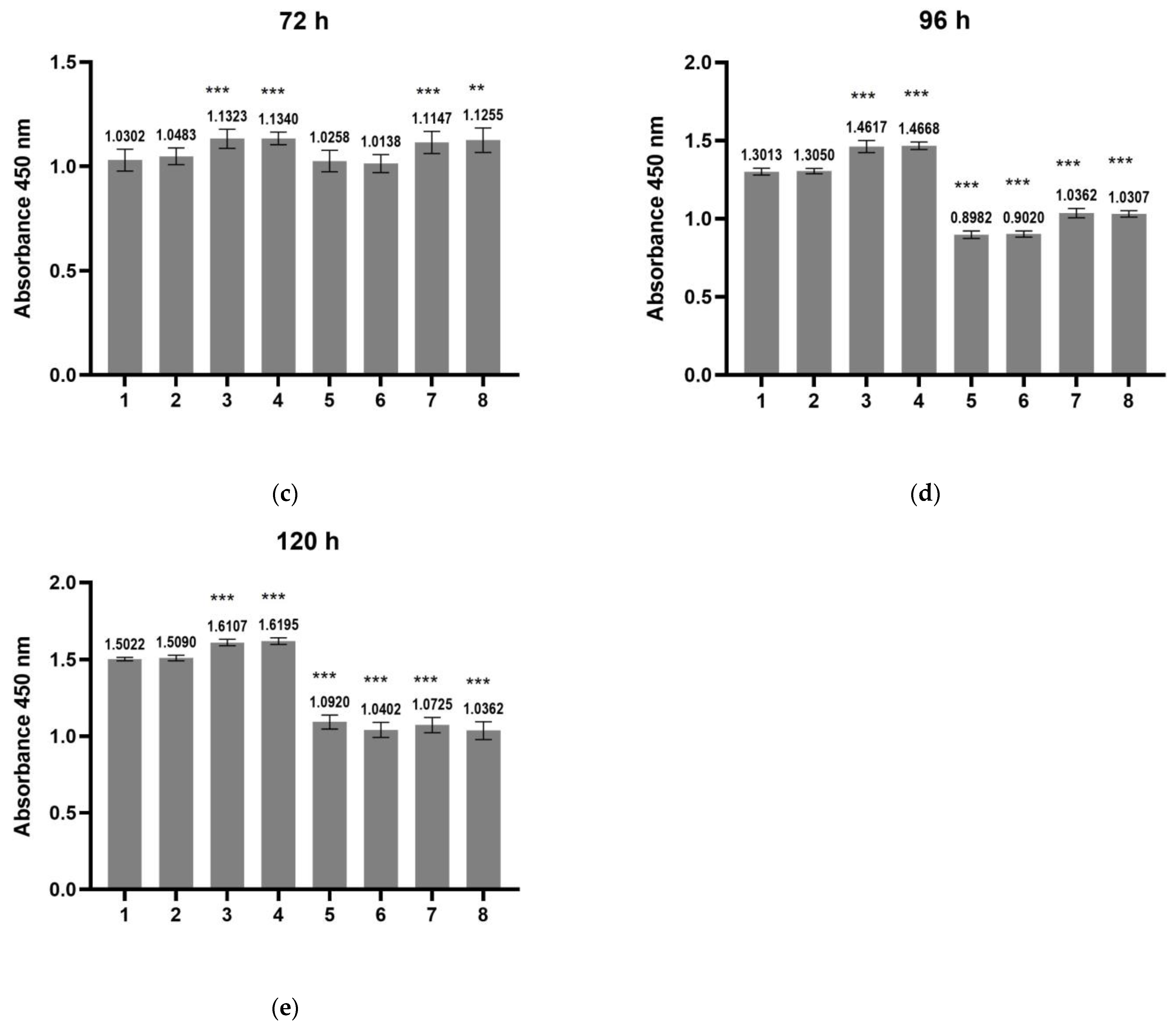
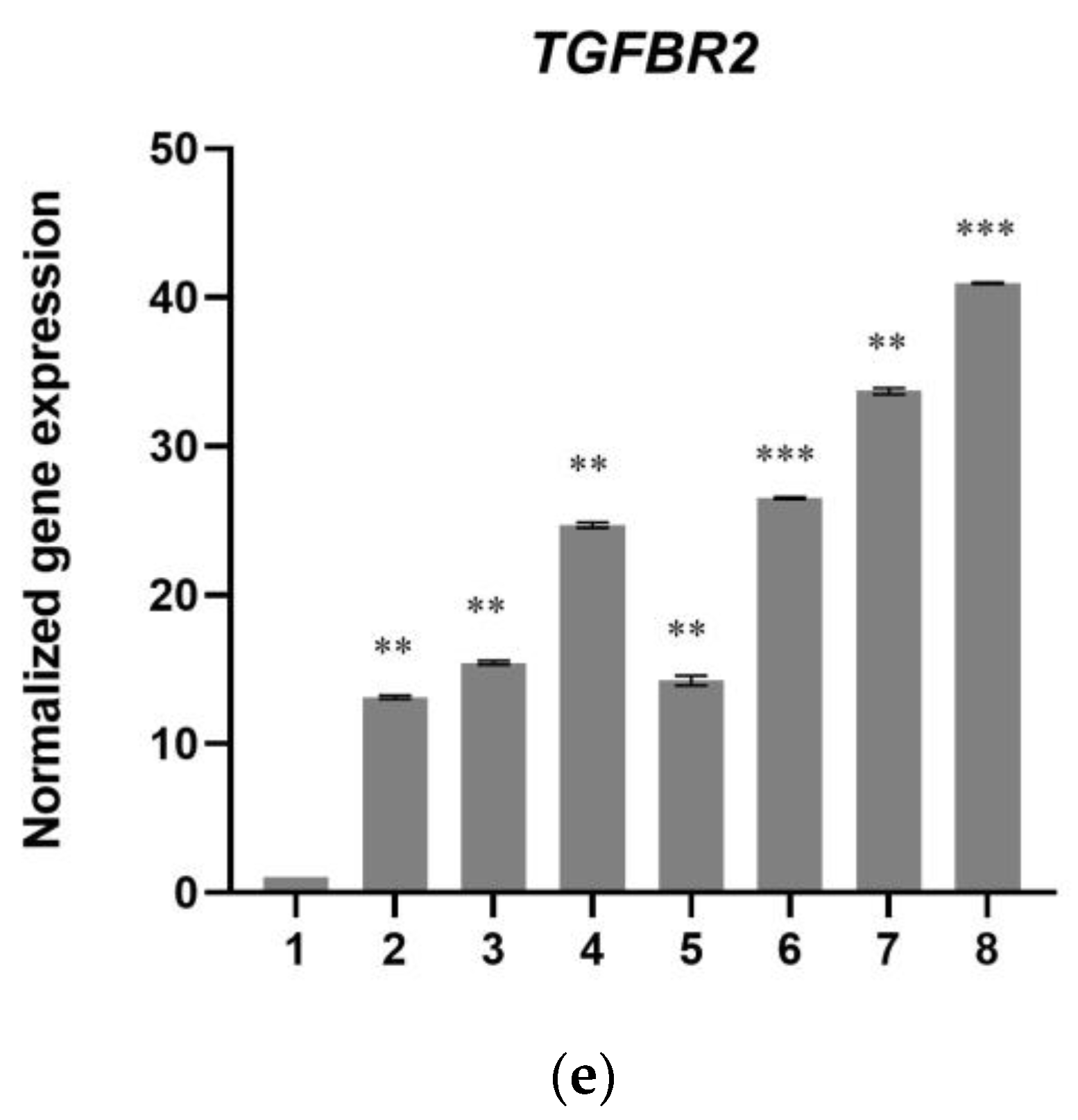
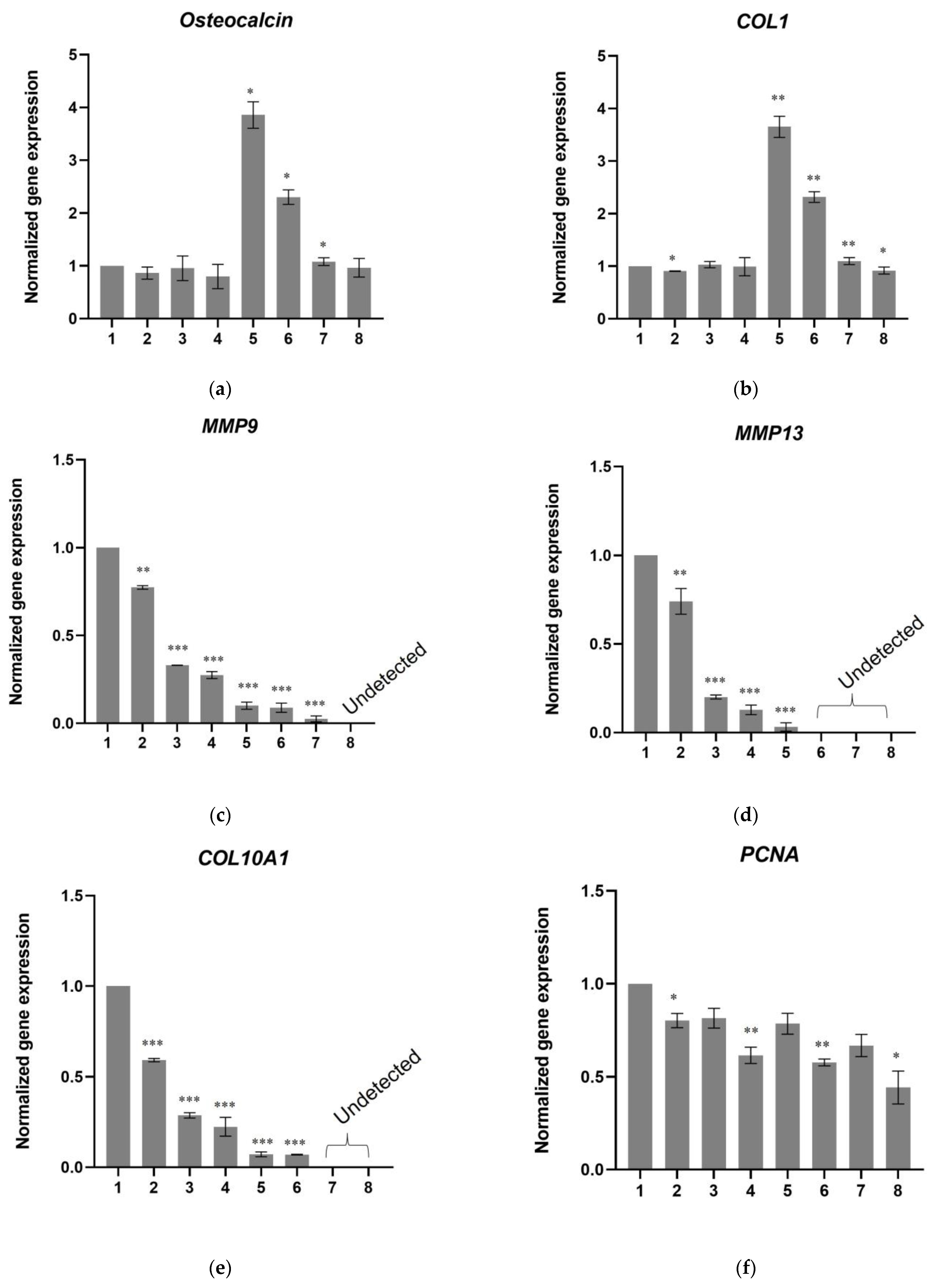
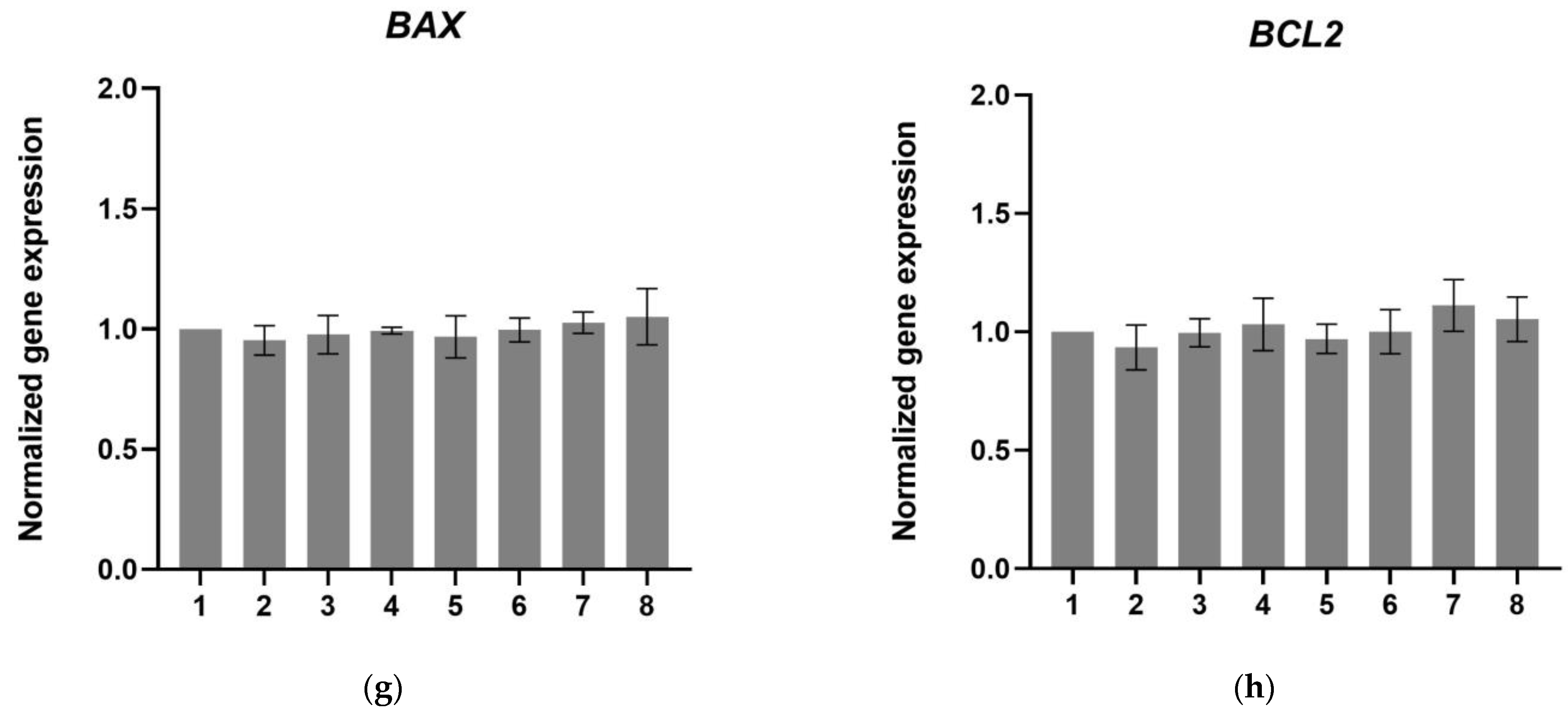
3.4. A Scaffold That Contains the Active TGF-β1 Peptide “ΥΥVGRKPK” Induces Chondrogenesis in hDPSCs
4. Discussion
5. Conclusions
6. Future Prospects
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Huey, D.J.; Hu, J.C.; Athanasiou, K.A. Unlike Bone, Cartilage Regeneration Remains Elusive. Science 2012, 338, 917–921. [Google Scholar] [CrossRef] [Green Version]
- Sophia Fox, A.J.; Bedi, A.; Rodeo, S.A. The Basic Science of Articular Cartilage: Structure, Composition, and Function. Sports Health 2009, 1, 461–468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arden, N.; Nevitt, M.C. Osteoarthritis: Epidemiology. Best Pract. Res. Clin. Rheumatol. 2006, 20, 3–25. [Google Scholar] [CrossRef] [PubMed]
- Luna, M. The Influence of the Gut Microbiome on Bone and Joint Disease; Cornell University: Ithaca, NY, USA, 2020. [Google Scholar]
- Gloria, A.; De Santis, R.; Ambrosio, L. Polymer-Based Composite Scaffolds for Tissue Engineering. J. Appl. Biomater. Biomech. 2010, 8, 57–67. [Google Scholar] [PubMed]
- Fernández-Colino, A.; Arias, F.J.; Alonso, M.; Rodríguez-Cabello, J.C. Self-Organized ECM-Mimetic Model Based on an Amphiphilic Multiblock Silk-Elastin-Like Corecombinamer with a Concomitant Dual Physical Gelation Process. Biomacromolecules 2014, 15, 3781–3793. [Google Scholar] [CrossRef]
- Machado, R.; Da Costa, A.; Sencadas, V.; Garcia-Arévalo, C.; Costa, C.M.; Padrão, J.; Gomes, A.; Lanceros-Méndez, S.; Rodríguez-Cabello, J.C.; Casal, M. Electrospun Silk-Elastin-like Fibre Mats for Tissue Engineering Applications. Biomed. Mater. 2013, 8, 065009. [Google Scholar] [CrossRef]
- Cipriani, F.; Krüger, M.; De Torre, I.G.; Sierra, L.Q.; Rodrigo, M.A.; Kock, L.; Rodriguez-Cabello, J.C. Cartilage Regeneration in Preannealed Silk Elastin-Like Co-Recombinamers Injectable Hydrogel Embedded with Mature Chondrocytes in an Ex Vivo Culture Platform. Biomacromolecules 2018, 19, 4333–4347. [Google Scholar] [CrossRef]
- Huang, W.; Rollett, A.; Kaplan, D.L. Silk-Elastin-like Protein Biomaterials for the Controlled Delivery of Therapeutics. Expert Opin. Drug Deliv. 2015, 12, 779–791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Girotti, A.; Fernández-Colino, A.; López, I.M.; Rodríguez-Cabello, J.C.; Arias, F.J. Elastin-like Recombinamers: Biosynthetic Strategies and Biotechnological Applications. Biotechnol. J. 2011, 6, 1174–1186. [Google Scholar] [CrossRef]
- Ivarsson, M.; Prenkert, M.; Cheema, A.; Wretenberg, P.; Andjelkov, N. Mussel Adhesive Protein as a Promising Alternative to Fibrin for Scaffold Fixation during Cartilage Repair Surgery. Cartilage 2021, 13, 663S–671S. [Google Scholar] [CrossRef]
- Lin, Q.; Gourdon, D.; Sun, C.; Holten-Andersen, N.; Anderson, T.H.; Waite, J.H.; Israelachvili, J.N. Adhesion Mechanisms of the Mussel Foot Proteins Mfp-1 and Mfp-3. Proc. Natl. Acad. Sci. USA 2007, 104, 3782–3786. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.X.; Liu, P.; Ding, W.; Meng, Q.B.; Su, D.H.; Zhang, Q.C.; Lian, R.X.; Yu, B.Q.; Zhao, M.D.; Dong, J.; et al. Injectable Mussel-Inspired Highly Adhesive Hydrogel with Exosomes for Endogenous Cell Recruitment and Cartilage Defect Regeneration. Biomaterials 2021, 278, 121169. [Google Scholar] [CrossRef] [PubMed]
- Fulkerson, J.P.; Norton, L.A.; Gronowicz, G.; Picciano, P.; Massicotte, J.M.; Nissen, C.W. Attachment of Epiphyseal Cartilage Cells and 17/28 Rat Osteosarcoma Osteoblasts Using Mussel Adhesive Protein. J. Orthop. Res. 1990, 8, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Schedlich, L.J.; Young, T.F.; Firth, S.M.; Baxter, R.C. Insulin-like Growth Factor-Binding Protein (IGFBP)-3 and IGFBP-5 Share a Common Nuclear Transport Pathway in T47D Human Breast Carcinoma Cells. J. Biol. Chem. 1998, 273, 18347–18352. [Google Scholar] [CrossRef] [Green Version]
- Hong, J.M.; Kim, B.J.; Shim, J.H.; Kang, K.S.; Kim, K.J.; Rhie, J.W.; Cha, H.J.; Cho, D.W. Enhancement of Bone Regeneration through Facile Surface Functionalization of Solid Freeform Fabrication-Based Three-Dimensional Scaffolds Using Mussel Adhesive Proteins. Acta Biomater. 2012, 8, 2578–2586. [Google Scholar] [CrossRef]
- Mantsou, A.; Papachristou, E.; Keramidas, P.; Lamprou, P.; Pavlidis, A.; Papi, R.M.; Dimitriou, K.; Aggeli, A.; Choli-Papadopoulou, T. A Novel Drastic Peptide Genetically Adapted to Biomimetic Scaffolds “Delivers” Osteogenic Signals to Human Mesenchymal Stem Cells. Nanomaterials 2023, 13, 1236. [Google Scholar] [CrossRef]
- Pitou, M.; Papachristou, E.; Papi, R.; Bratsios, D.; Kefala, G.-M.; Tsagkarakou, A.; Leonidas, D.; Aggeli, A.; Papadopoulos, G.; Choli-Papadopoulou, T. In Vitro Chondrogenesis Induction by Short Peptides of the Carboxy-Terminal Domain of Transforming Growth Factor Β1. Int. J. Mol. Sci. 2023. [Google Scholar]
- Martín, L.; Alonso, M.; Girotti, A.; Arias, F.J.; Rodríguez-Cabello, J.C. Synthesis and Characterization of Macroporous Thermosensitive Hydrogels from Recombinant Elastin-Like Polymers. Biomacromolecules 2009, 10, 3015–3022. [Google Scholar] [CrossRef]
- Bakopoulou, A.; Leyhausen, G.; Volk, J.; Papachristou, E.; Koidis, P.; Geurtsen, W. Wnt/β-Catenin Signaling Regulates Dental Pulp Stem Cells’ Responses to Pulp Injury by Resinous Monomers. Dent. Mater. 2015, 31, 542–555. [Google Scholar] [CrossRef]
- Adolphe, M.; Thenet-Gauci, S.; Demignot, S. Chondrocyte Culture: A Target System to Evaluate. In In Vitro Methods in Pharmaceutical Research; Castell, J.V., Gómez-Lechón, M.J., Eds.; Elsevier: Amsterdam, The Netherlands, 1997; pp. 181–207. [Google Scholar]
- Whitcomb, K. Determining the Linear Viscoelastic Region in Oscillatory Measurements. Available online: https://www.tainstruments.com/pdf/literature/RH107.pdf (accessed on 22 February 2023).
- Ding, Z.; Cheng, W.; Mia, M.S.; Lu, Q. Silk Biomaterials for Bone Tissue Engineering. Macromol. Biosci. 2021, 21, 2100153. [Google Scholar] [CrossRef]
- Bhattacharjee, P.; Kundu, B.; Naskar, D.; Kim, H.W.; Maiti, T.K.; Bhattacharya, D.; Kundu, S.C. Silk Scaffolds in Bone Tissue Engineering: An Overview. Acta Biomater. 2017, 63, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.J.; Choi, Y.S.; Cha, H.J. Reinforced Multifunctionalized Nanofibrous Scaffolds Using Mussel Adhesive Proteins. Angew. Chemie Int. Ed. 2012, 51, 675–678. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Zhang, Q.; Li, H.; Wei, Q.; Zhao, X.; Chen, F. Elastin-like Polypeptide Modified Silk Fibroin Porous Scaffold Promotes Osteochondral Repair. Bioact. Mater. 2021, 6, 589–601. [Google Scholar] [CrossRef] [PubMed]
- Karageorgiou, V.; Tomkins, M.; Fajardo, R.; Meinel, L.; Snyder, B.; Wade, K.; Chen, J.; Vunjak-Novakovic, G.; Kaplan, D.L. Porous Silk Fibroin 3-D Scaffolds for Delivery of Bone Morphogenetic Protein-2 in Vitro and in Vivo. J. Biomed. Mater. Res. Part A 2006, 78, 324–334. [Google Scholar] [CrossRef] [PubMed]
- Docheva, D.; Popov, C.; Mutschler, W.; Schieker, M. Human Mesenchymal Stem Cells in Contact with Their Environment: Surface Characteristics and the Integrin System. J. Cell. Mol. Med. 2007, 11, 21–38. [Google Scholar] [CrossRef] [PubMed]
- Verrecchio, A.; Germann, M.W.; Schick, B.P.; Kung, B.; Twardowski, T.; San Antonio, J.D. Design of Peptides with High Affinities for Heparin and Endothelial Cell Proteoglycans. J. Biol. Chem. 2000, 275, 7701–7707. [Google Scholar] [CrossRef] [Green Version]
- Song, J.J.; Aswad, R.; Kanaan, R.A.; Rico, M.C.; Owen, T.A.; Barbe, M.F.; Safadi, F.F.; Popoff, S.N. Connective Tissue Growth Factor (CTGF) Acts as a Downstream Mediator of TGF-Β1 to Induce Mesenchymal Cell Condensation. J. Cell. Physiol. 2007, 210, 398–410. [Google Scholar] [CrossRef]
- Tuli, R.; Tuli, S.; Nandi, S.; Huang, X.; Manner, P.A.; Hozack, W.J.; Danielson, K.G.; Hall, D.J.; Tuan, R.S. Transforming Growth Factor-β-Mediated Chondrogenesis of Human Mesenchymal Progenitor Cells Involves N-Cadherin and Mitogen-Activated Protein Kinase and Wnt Signaling Cross-Talk. J. Biol. Chem. 2003, 278, 41227–41236. [Google Scholar] [CrossRef] [Green Version]
- Akiyama, H.; Lefebvre, V. Unraveling the Transcriptional Regulatory Machinery in Chondrogenesis. J. Bone Miner. Metab. 2011, 29, 390–395. [Google Scholar] [CrossRef] [Green Version]
- Long, F.; Ornitz, D.M. Development of the Endochondral Skeleton. Cold Spring Harb. Perspect. Biol. 2013, 5, a008334. [Google Scholar] [CrossRef] [Green Version]
- Wang, W.; Rigueur, D.; Lyons, K.M. TGFβ Signaling in Cartilage Development and Maintenance. Birth Defects Res. Part C Embryo Today Rev. 2014, 102, 37–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strzalka, W.; Ziemienowicz, A. Proliferating Cell Nuclear Antigen (PCNA): A Key Factor in DNA Replication and Cell Cycle Regulation. Ann. Bot. 2011, 107, 1127–1140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bologna-Molina, R.; Mosqueda-Taylor, A.; Molina-Frechero, N.; Mori-Estevez, A.; Sanchez-Acuna, G. Comparison of the Value of PCNA and Ki-67 as Markers of Cell Proliferation in Ameloblastic Tumors. Med. Oral Patol. Oral y Cir. Bucal 2013, 18, e174–e179. [Google Scholar] [CrossRef] [PubMed]









| Polypeptides | Scaffold-TGFβ1 | Scaffold without Peptides |
|---|---|---|
| TGF-β1 peptide-(ELP10-Silk2-Mussel15)2-Mussel-6xHis | + | - |
| (ELP5-RGD peptide-ELP5-Silk2-Mussel15)2-Mussel-6xHis | + | + |
| Laminin peptide-(ELP10-Silk2-Mussel15)2-Mussel-6xHis | + | + |
| Heparin-binding peptide-(ELP10-Silk2-Mussel15)2-Mussel-6xHis | + | + |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mantsou, A.; Papachristou, E.; Keramidas, P.; Lamprou, P.; Pitou, M.; Papi, R.M.; Dimitriou, K.; Aggeli, A.; Choli-Papadopoulou, T. Fabrication of a Smart Fibrous Biomaterial That Harbors an Active TGF-β1 Peptide: A Promising Approach for Cartilage Regeneration. Biomedicines 2023, 11, 1890. https://doi.org/10.3390/biomedicines11071890
Mantsou A, Papachristou E, Keramidas P, Lamprou P, Pitou M, Papi RM, Dimitriou K, Aggeli A, Choli-Papadopoulou T. Fabrication of a Smart Fibrous Biomaterial That Harbors an Active TGF-β1 Peptide: A Promising Approach for Cartilage Regeneration. Biomedicines. 2023; 11(7):1890. https://doi.org/10.3390/biomedicines11071890
Chicago/Turabian StyleMantsou, Aglaia, Eleni Papachristou, Panagiotis Keramidas, Paraskevas Lamprou, Maria Pitou, Rigini M. Papi, Katerina Dimitriou, Amalia Aggeli, and Theodora Choli-Papadopoulou. 2023. "Fabrication of a Smart Fibrous Biomaterial That Harbors an Active TGF-β1 Peptide: A Promising Approach for Cartilage Regeneration" Biomedicines 11, no. 7: 1890. https://doi.org/10.3390/biomedicines11071890






