Cell-Based Therapy for Urethral Regeneration: A Narrative Review and Future Perspectives
Abstract
:1. Introduction
2. Non-Stem Cell-Based Regenerative Therapy
2.1. Epithelial Cells
2.2. Mesothelial Cells
2.3. Smooth Muscle Cells
2.4. Endothelial Cells
3. Stem Cell-Based Regenerative Therapy
3.1. Pluripotent Stem Cells
3.2. Bone Marrow-Derived Stem Cells
3.3. Adipose-Derived Stem Cells
3.4. Urine-Derived Stem Cells
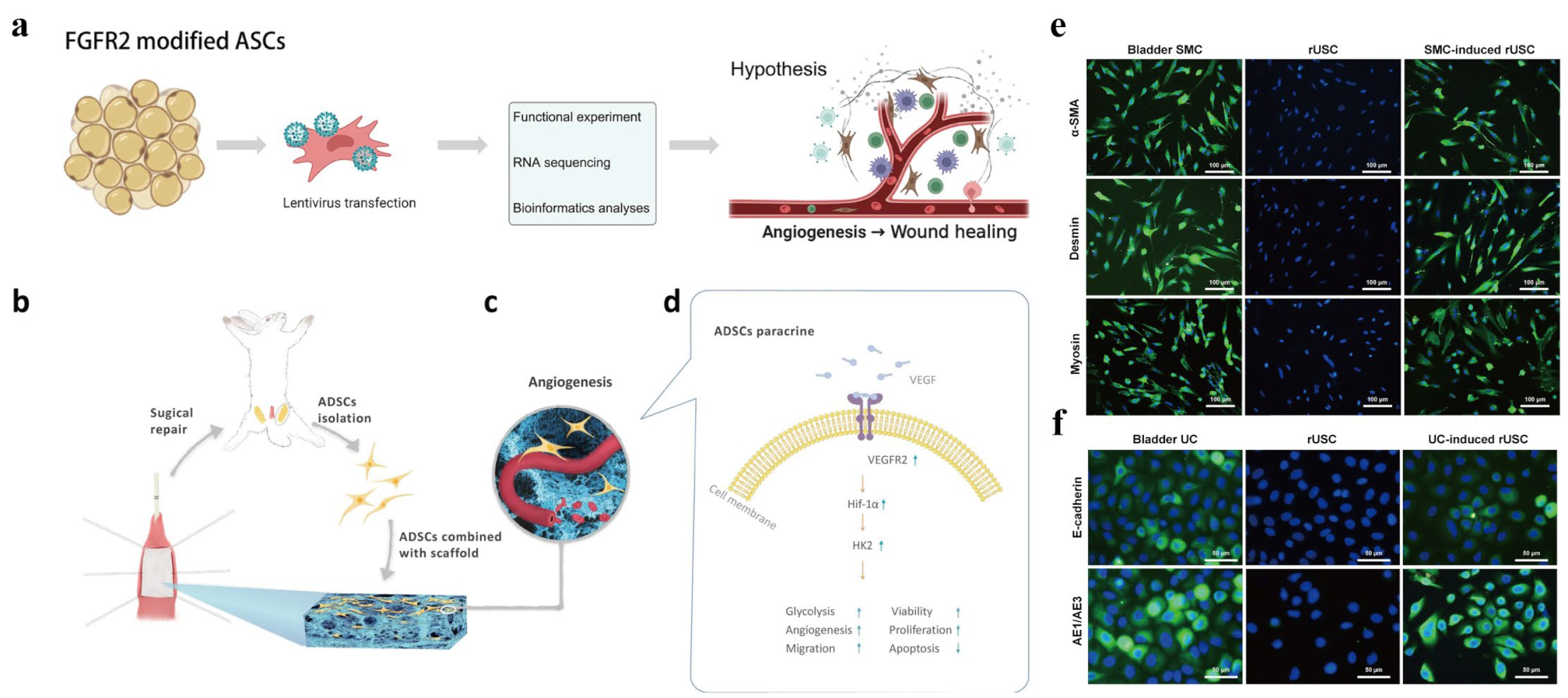
3.5. Other Stem Cell Types
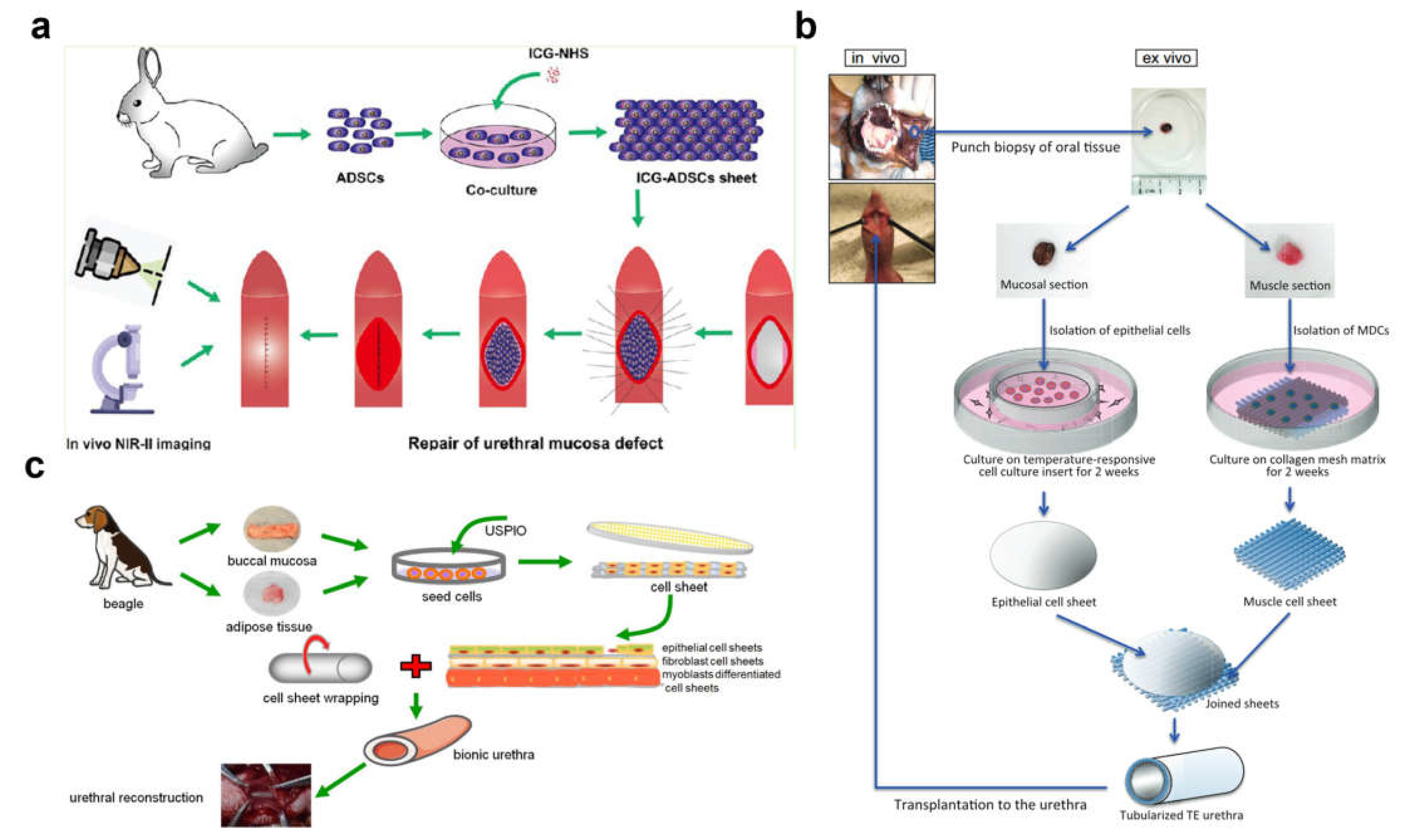
4. Cell Sheet Technology
5. Clinical Studies
6. Future Perspectives
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mundy, A.R.; Andrich, D.E. Urethral strictures. BJU Int. 2011, 107, 6–26. [Google Scholar] [CrossRef] [PubMed]
- Simsek, A.; Bullock, A.J.; Roman, S.; Chapple, C.R.; Macneil, S. Developing improved tissue-engineered buccal mucosa grafts for urethral reconstruction. Can. Urol. Assoc. J. 2018, 12, E234–E242. [Google Scholar] [CrossRef] [PubMed]
- Santucci, R.A.; Joyce, G.F.; Wise, M. Male Urethral Stricture Disease. J. Urol. 2007, 177, 1667–1674. [Google Scholar] [CrossRef] [PubMed]
- Davis, N.F.; Quinlan, M.R.; Bhatt, N.R.; Browne, C.; MacCraith, E.; Manecksha, R.; Walsh, M.T.; Thornhill, J.A.; Mulvin, D. Incidence, Cost, Complications and Clinical Outcomes of Iatrogenic Urethral Catheterization Injuries: A Prospective Multi-Institutional Study. J. Urol. 2016, 196, 1473–1477. [Google Scholar] [CrossRef] [PubMed]
- Marshall, S.D.; Raup, V.T.; Brandes, S.B. Dorsal inlay buccal mucosal graft (Asopa) urethroplasty for anterior urethral stricture. Transl. Androl. Urol. 2015, 4, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Atala, A.; Danilevskiy, M.; Lyundup, A.; Glybochko, P.; Butnaru, D.; Vinarov, A.; Yoo, J.J. The potential role of tissue-engineered urethral substitution: Clinical and preclinical studies. J. Tissue Eng. Regen. Med. 2017, 11, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Lumen, N.; Vierstraete-Verlinde, S.; Oosterlinck, W.; Hoebeke, P.; Palminteri, E.; Goes, C.; Maes, H.; Spinoit, A.F. Buccal Versus Lingual Mucosa Graft in Anterior Urethroplasty: A Prospective Comparison of Surgical Outcome and Donor Site Morbidity. J. Urol. 2016, 195, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Atala, A. Engineering organs. Curr. Opin. Biotechnol. 2009, 20, 575–592. [Google Scholar] [CrossRef]
- Liu, Y.; Bharadwaj, S.; Lee, S.J.; Atala, A.; Zhang, Y. Optimization of a natural collagen scaffold to aid cell-matrix penetration for urologic tissue engineering. Biomaterials 2009, 30, 3865–3873. [Google Scholar] [CrossRef]
- Dorin, R.P.; Pohl, H.G.; De Filippo, R.E.; Yoo, J.J.; Atala, A. Tubularized urethral replacement with unseeded matrices: What is the maximum distance for normal tissue regeneration? World J. Urol. 2008, 26, 323–326. [Google Scholar] [CrossRef]
- Farzamfar, S.; Elia, E.; Chabaud, S.; Naji, M.; Bolduc, S. Prospects and Challenges of Electrospun Cell and Drug Delivery Vehicles to Correct Urethral Stricture. Int. J. Mol. Sci. 2022, 23, 10519. [Google Scholar] [CrossRef] [PubMed]
- Xue, J.D.; Gao, J.; Fu, Q.; Feng, C.; Xie, H. Seeding cell approach for tissue-engineered urethral reconstruction in animal study: A systematic review and meta-analysis. Exp. Biol. Med. 2016, 241, 1416–1428. [Google Scholar] [CrossRef] [PubMed]
- Fu, Q.; Cao, Y.L. Tissue engineering and stem cell application of urethroplasty: From bench to bedside. Urology 2012, 79, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Orabi, H.; AbouShwareb, T.; Zhang, Y.; Yoo, J.J.; Atala, A. Cell-seeded tubularized scaffolds for reconstruction of long urethral defects: A preclinical study. Eur. Urol. 2013, 63, 531–538. [Google Scholar] [CrossRef]
- Chan, Y.Y.; Bury, M.I.; Yura, E.M.; Hofer, M.D.; Cheng, E.Y.; Sharma, A.K. The current state of tissue engineering in the management of hypospadias. Nat. Rev. Urol. 2020, 17, 162–175. [Google Scholar] [CrossRef] [PubMed]
- Sievert, K.D.; Daum, L.; Maurer, S.; Toomey, P.; Vaegler, M.; Aufderklamm, S.; Amend, B. Urethroplasty performed with an autologous urothelium-vegetated collagen fleece to treat urethral stricture in the minipig model. World J. Urol. 2020, 38, 2123–2131. [Google Scholar] [CrossRef] [PubMed]
- De Graaf, P.; van der Linde, E.M.; Rosier, P.; Izeta, A.; Sievert, K.D.; Bosch, J.; de Kort, L.M.O. Systematic Review to Compare Urothelium Differentiation with Urethral Epithelium Differentiation in Fetal Development, as a Basis for Tissue Engineering of the Male Urethra. Tissue Eng. Part. B Rev. 2017, 23, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Fu, M.; Li, F.; Fu, W.; Zhao, Z.; Xia, H.; Niu, Y. Tissue-engineered PLLA/gelatine nanofibrous scaffold promoting the phenotypic expression of epithelial and smooth muscle cells for urethral reconstruction. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 111, 110810. [Google Scholar] [CrossRef]
- Wang, F.; Liu, T.; Yang, L.; Zhang, G.; Liu, H.; Yi, X.; Yang, X.; Lin, T.Y.; Qin, W.; Yuan, J. Urethral reconstruction with tissue-engineered human amniotic scaffold in rabbit urethral injury models. Med. Sci. Monit. 2014, 20, 2430–2438. [Google Scholar] [CrossRef]
- Fossum, M.; Gustafson, C.J.; Nordenskjöld, A.; Kratz, G. Isolation and in vitro cultivation of human urothelial cells from bladder washings of adult patients and children. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2003, 37, 41–45. [Google Scholar] [CrossRef]
- Amesty, M.V.; Chamorro, C.I.; López-Pereira, P.; Martínez-Urrutia, M.J.; Sanz, B.; Rivas, S.; Lobato, R.; Fossum, M. Creation of Tissue-Engineered Urethras for Large Urethral Defect Repair in a Rabbit Experimental Model. Front. Pediatr. 2021, 9, 691131. [Google Scholar] [CrossRef] [PubMed]
- Xuan, Z.; Zachar, V.; Pennisi, C.P. Sources, Selection, and Microenvironmental Preconditioning of Cells for Urethral Tissue Engineering. Int. J. Mol. Sci. 2022, 23, 14074. [Google Scholar] [CrossRef] [PubMed]
- Kimball, J.R.; Nittayananta, W.; Klausner, M.; Chung, W.O.; Dale, B.A. Antimicrobial barrier of an in vitro oral epithelial model. Arch. Oral. Biol. 2006, 51, 775–783. [Google Scholar] [CrossRef] [PubMed]
- Corradini, F.; Zattoni, M.; Barbagli, G.; Bianchi, G.; Giovanardi, M.; Serafini, C.; Genna, V.G.; Ribbene, A.; Balò, S.; Fidanza, F.; et al. Comparative Assessment of Cultures from Oral and Urethral Stem Cells for Urethral Regeneration. Curr. Stem Cell Res. Ther. 2016, 11, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.W.; Lv, X.G.; Li, Z.; Song, L.J.; Feng, C.; Xie, M.K.; Li, C.; Li, H.B.; Wang, J.H.; Zhu, W.D.; et al. Urethral reconstruction with a 3D porous bacterial cellulose scaffold seeded with lingual keratinocytes in a rabbit model. Biomed. Mater. 2015, 10, 055005. [Google Scholar] [CrossRef] [PubMed]
- Lv, X.; Feng, C.; Liu, Y.; Peng, X.; Chen, S.; Xiao, D.; Wang, H.; Li, Z.; Xu, Y.; Lu, M. A smart bilayered scaffold supporting keratinocytes and muscle cells in micro/nano-scale for urethral reconstruction. Theranostics 2018, 8, 3153–3163. [Google Scholar] [CrossRef] [PubMed]
- Ram-Liebig, G.; Barbagli, G.; Heidenreich, A.; Fahlenkamp, D.; Romano, G.; Rebmann, U.; Standhaft, D.; van Ahlen, H.; Schakaki, S.; Balsmeyer, U.; et al. Results of Use of Tissue-Engineered Autologous Oral Mucosa Graft for Urethral Reconstruction: A Multicenter, Prospective, Observational Trial. EBioMedicine 2017, 23, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Fu, Q.; Deng, C.L.; Liu, W.; Cao, Y.L. Urethral replacement using epidermal cell-seeded tubular acellular bladder collagen matrix. BJU Int. 2007, 99, 1162–1165. [Google Scholar] [CrossRef]
- Rogovaya, O.S.; Fayzulin, A.K.; Vasiliev, A.V.; Kononov, A.V.; Terskikh, V.V. Reconstruction of rabbit urethral epithelium with skin keratinocytes. Acta Nat. 2015, 7, 70–77. [Google Scholar] [CrossRef]
- Zhang, D.; Hou, J.; Gu, Y.; Shao, J.; Zhou, S.; Zhuang, J.; Song, L.; Wang, X. Cryopreserved skin epithelial cell sheet combined with acellular amniotic membrane as an off-the-shelf scaffold for urethral regeneration. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 122, 111926. [Google Scholar] [CrossRef]
- Dauleh, S.; Santeramo, I.; Fielding, C.; Ward, K.; Herrmann, A.; Murray, P.; Wilm, B. Characterisation of Cultured Mesothelial Cells Derived from the Murine Adult Omentum. PLoS ONE 2016, 11, e0158997. [Google Scholar] [CrossRef] [PubMed]
- Nanni, L.; Vallasciani, S.; Fadda, G.; Perrelli, L. Free peritoneal grafts for patch urethroplasty in male rabbits. J. Urol. 2001, 165, 578–580. [Google Scholar] [CrossRef] [PubMed]
- Kajbafzadeh, A.M.; Arshadi, H.; Payabvash, S.; Salmasi, A.H.; Najjaran-Tousi, V.; Sahebpor, A.R. Proximal hypospadias with severe chordee: Single stage repair using corporeal tunica vaginalis free graft. J. Urol. 2007, 178, 1036–1042, discussion 1042. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Xu, Z.; Zhao, Y.; Yan, L.; Zhou, Z.; Gu, G. Urethral Reconstruction Using Mesothelial Cell-Seeded Autogenous Granulation Tissue Tube: An Experimental Study in Male Rabbits. Biomed. Res. Int. 2017, 2017, 1850256. [Google Scholar] [CrossRef]
- Wang, C.; Chen, C.; Guo, M.; Li, B.; Han, F.; Chen, W. Stretchable collagen-coated polyurethane-urea hydrogel seeded with bladder smooth muscle cells for urethral defect repair in a rabbit model. J. Mater. Sci. Mater. Med. 2019, 30, 135. [Google Scholar] [CrossRef] [PubMed]
- Lv, X.; Yang, J.; Feng, C.; Li, Z.; Chen, S.; Xie, M.; Huang, J.; Li, H.; Wang, H.; Xu, Y. Bacterial Cellulose-Based Biomimetic Nanofibrous Scaffold with Muscle Cells for Hollow Organ Tissue Engineering. ACS Biomater. Sci. Eng. 2016, 2, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Niu, Y.; Liu, G.; Fu, M.; Chen, C.; Fu, W.; Zhang, Z.; Xia, H.; Stadler, F.J. Designing a multifaceted bio-interface nanofiber tissue-engineered tubular scaffold graft to promote neo-vascularization for urethral regeneration. J. Mater. Chem. B 2020, 8, 1748–1758. [Google Scholar] [CrossRef]
- Niu, Y.; Liu, G.; Chen, C.; Fu, M.; Fu, W.; Zhao, Z.; Xia, H.; Stadler, F.J. Urethral reconstruction using an amphiphilic tissue-engineered autologous polyurethane nanofiber scaffold with rapid vascularization function. Biomater. Sci. 2020, 8, 2164–2174. [Google Scholar] [CrossRef]
- Bouhout, S.; Chabaud, S.; Bolduc, S. Organ-specific matrix self-assembled by mesenchymal cells improves the normal urothelial differentiation in vitro. World J. Urol. 2016, 34, 121–130. [Google Scholar] [CrossRef]
- De Filippo, R.E.; Kornitzer, B.S.; Yoo, J.J.; Atala, A. Penile urethra replacement with autologous cell-seeded tubularized collagen matrices. J. Tissue Eng. Regen. Med. 2015, 9, 257–264. [Google Scholar] [CrossRef]
- Heller, M.; Frerick-Ochs, E.V.; Bauer, H.K.; Schiegnitz, E.; Flesch, D.; Brieger, J.; Stein, R.; Al-Nawas, B.; Brochhausen, C.; Thüroff, J.W.; et al. Tissue engineered pre-vascularized buccal mucosa equivalents utilizing a primary triculture of epithelial cells, endothelial cells and fibroblasts. Biomaterials 2016, 77, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.K.; Cheng, E.Y. Growth factor and small molecule influence on urological tissue regeneration utilizing cell seeded scaffolds. Adv. Drug Deliv. Rev. 2015, 82–83, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Caplan, A.I.; Correa, D. The MSC: An injury drugstore. Cell Stem Cell 2011, 9, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Beegle, J.; Lakatos, K.; Kalomoiris, S.; Stewart, H.; Isseroff, R.R.; Nolta, J.A.; Fierro, F.A. Hypoxic preconditioning of mesenchymal stromal cells induces metabolic changes, enhances survival, and promotes cell retention in vivo. Stem Cells 2015, 33, 1818–1828. [Google Scholar] [CrossRef]
- Clément, F.; Grockowiak, E.; Zylbersztejn, F.; Fossard, G.; Gobert, S.; Maguer-Satta, V. Stem cell manipulation, gene therapy and the risk of cancer stem cell emergence. Stem Cell Investig. 2017, 4, 67. [Google Scholar] [CrossRef] [PubMed]
- Pederzoli, F.; Joice, G.; Salonia, A.; Bivalacqua, T.J.; Sopko, N.A. Regenerative and engineered options for urethroplasty. Nat. Rev. Urol. 2019, 16, 453–464. [Google Scholar] [CrossRef]
- Blank, R.S.; Swartz, E.A.; Thompson, M.M.; Olson, E.N.; Owens, G.K. A retinoic acid-induced clonal cell line derived from multipotential P19 embryonal carcinoma cells expresses smooth muscle characteristics. Circ. Res. 1995, 76, 742–749. [Google Scholar] [CrossRef] [PubMed]
- Oottamasathien, S.; Wang, Y.; Williams, K.; Franco, O.E.; Wills, M.L.; Thomas, J.C.; Saba, K.; Sharif-Afshar, A.R.; Makari, J.H.; Bhowmick, N.A.; et al. Directed differentiation of embryonic stem cells into bladder tissue. Dev. Biol. 2007, 304, 556–566. [Google Scholar] [CrossRef]
- Suzuki, K.; Koyanagi-Aoi, M.; Uehara, K.; Hinata, N.; Fujisawa, M.; Aoi, T. Directed differentiation of human induced pluripotent stem cells into mature stratified bladder urothelium. Sci. Rep. 2019, 9, 10506. [Google Scholar] [CrossRef]
- Demirel, B.D.; Bıçakcı, Ü.; Rızalar, R.; Alpaslan Pınarlı, F.; Aydın, O. Histopathological effects of mesenchymal stem cells in rats with bladder and posterior urethral injuries. Turk. J. Med. Sci. 2017, 47, 1912–1919. [Google Scholar] [CrossRef]
- Zhang, Y.; Lin, H.K.; Frimberger, D.; Epstein, R.B.; Kropp, B.P. Growth of bone marrow stromal cells on small intestinal submucosa: An alternative cell source for tissue engineered bladder. BJU Int. 2005, 96, 1120–1125. [Google Scholar] [CrossRef] [PubMed]
- Yudintceva, N.M.; Nashchekina, Y.A.; Mikhailova, N.A.; Vinogradova, T.I.; Yablonsky, P.K.; Gorelova, A.A.; Muraviov, A.N.; Gorelov, A.V.; Samusenko, I.A.; Nikolaev, B.P.; et al. Urethroplasty with a bilayered poly-D,L-lactide-co-ε-caprolactone scaffold seeded with allogenic mesenchymal stem cells. J. Biomed. Mater. Res. B Appl. Biomater. 2020, 108, 1010–1021. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.S.; Bury, M.I.; Fuller, N.J.; Sturm, R.M.; Ahmad, N.; Sharma, A.K. Bone Marrow Stem/Progenitor Cells Attenuate the Inflammatory Milieu Following Substitution Urethroplasty. Sci. Rep. 2016, 6, 35638. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zheng, S.; Zhang, X.; Dai, P.; Gao, Y.; Nan, L.; Zhang, Y. Transplantation of Amniotic Scaffold-Seeded Mesenchymal Stem Cells and/or Endothelial Progenitor Cells From Bone Marrow to Efficiently Repair 3-cm Circumferential Urethral Defect in Model Dogs. Tissue Eng. Part A 2018, 24, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Katz, A.J.; Llull, R.; Hedrick, M.H.; Futrell, J.W. Emerging approaches to the tissue engineering of fat. Clin. Plast. Surg. 1999, 26, 587–603. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Xu, Y.; Fu, Q.; Li, C. Effects of multiple agents on epithelial differentiation of rabbit adipose-derived stem cells in 3D culture. Tissue Eng. Part A 2012, 18, 1760–1770. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Xu, M.X.; Zhou, Z.; Zhang, K.; Zhou, J.; Zhao, Y.; Wang, Z.; Lu, M.J. The differentiation of human adipose-derived stem cells towards a urothelium-like phenotype in vitro and the dynamic temporal changes of related cytokines by both paracrine and autocrine signal regulation. PLoS ONE 2014, 9, e95583. [Google Scholar] [CrossRef]
- Zhang, M.; Peng, Y.; Zhou, Z.; Zhou, J.; Wang, Z.; Lu, M. Differentiation of human adipose-derived stem cells co-cultured with urothelium cell line toward a urothelium-like phenotype in a nude murine model. Urology 2013, 81, 465.e15–465.e22. [Google Scholar] [CrossRef]
- Li, H.; Xu, Y.; Xie, H.; Li, C.; Song, L.; Feng, C.; Zhang, Q.; Xie, M.; Wang, Y.; Lv, X. Epithelial-differentiated adipose-derived stem cells seeded bladder acellular matrix grafts for urethral reconstruction: An animal model. Tissue Eng. Part A 2014, 20, 774–784. [Google Scholar] [CrossRef]
- Fu, Q.; Deng, C.L.; Zhao, R.Y.; Wang, Y.; Cao, Y. The effect of mechanical extension stimulation combined with epithelial cell sorting on outcomes of implanted tissue-engineered muscular urethras. Biomaterials 2014, 35, 105–112. [Google Scholar] [CrossRef]
- Zhang, R.; Jack, G.S.; Rao, N.; Zuk, P.; Ignarro, L.J.; Wu, B.; Rodríguez, L.V. Nuclear fusion-independent smooth muscle differentiation of human adipose-derived stem cells induced by a smooth muscle environment. Stem Cells 2012, 30, 481–490. [Google Scholar] [CrossRef]
- Castiglione, F.; Dewulf, K.; Hakim, L.; Weyne, E.; Montorsi, F.; Russo, A.; Boeri, L.; Bivalacqua, T.J.; De Ridder, D.; Joniau, S.; et al. Adipose-derived Stem Cells Counteract Urethral Stricture Formation in Rats. Eur. Urol. 2016, 70, 1032–1041. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; He, Y.; Li, J. MicroRNA-21: A central regulator of fibrotic diseases via various targets. Curr. Pharm. Des. 2015, 21, 2236–2242. [Google Scholar] [CrossRef] [PubMed]
- Meng, F.; Henson, R.; Wehbe-Janek, H.; Ghoshal, K.; Jacob, S.T.; Patel, T. MicroRNA-21 regulates expression of the PTEN tumor suppressor gene in human hepatocellular cancer. Gastroenterology 2007, 133, 647–658. [Google Scholar] [CrossRef] [PubMed]
- Feng, Z.; Chen, H.; Fu, T.; Zhang, L.; Liu, Y. miR-21 modification enhances the performance of adipose tissue-derived mesenchymal stem cells for counteracting urethral stricture formation. J. Cell. Mol. Med. 2018, 22, 5607–5616. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.C.; Wu, Y.P.; Li, X.D.; Chen, S.H.; Ye, X.J.; Xue, X.Y.; Xu, N. TNF-α-induced exosomal miR-146a mediates mesenchymal stem cell-dependent suppression of urethral stricture. J. Cell. Physiol. 2019, 234, 23243–23255. [Google Scholar] [CrossRef] [PubMed]
- Zhong, H.; Shen, Y.; Zhao, D.; Yan, G.; Wu, C.; Huang, G.; Liu, Z.; Zhai, J.; Han, Q. Cell-Seeded Acellular Artery for Reconstruction of Long Urethral Defects in a Canine Model. Stem Cells Int. 2021, 2021, 8854479. [Google Scholar] [CrossRef]
- Tian, B.; Song, L.; Liang, T.; Li, Z.; Ye, X.; Fu, Q.; Li, Y. Repair of urethral defects by an adipose mesenchymal stem cell-porous silk fibroin material. Mol. Med. Rep. 2018, 18, 209–215. [Google Scholar] [CrossRef]
- Yang, M.; Zhang, Y.; Fang, C.; Song, L.; Wang, Y.; Lu, L.; Yang, R.; Bu, Z.; Liang, X.; Zhang, K.; et al. Urine-Microenvironment-Initiated Composite Hydrogel Patch Reconfiguration Propels Scarless Memory Repair and Reinvigoration of the Urethra. Adv. Mater. 2022, 34, e2109522. [Google Scholar] [CrossRef]
- Qazi, T.H.; Mooney, D.J.; Duda, G.N.; Geissler, S. Biomaterials that promote cell-cell interactions enhance the paracrine function of MSCs. Biomaterials 2017, 140, 103–114. [Google Scholar] [CrossRef]
- Przybyt, E.; Krenning, G.; Brinker, M.G.; Harmsen, M.C. Adipose stromal cells primed with hypoxia and inflammation enhance cardiomyocyte proliferation rate in vitro through STAT3 and Erk1/2. J. Transl. Med. 2013, 11, 39. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Kim, S.M.; Sung, J.H. Cellular and molecular stimulation of adipose-derived stem cells under hypoxia. Cell Biol. Int. 2014, 38, 553–562. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Yang, J.; Ji, X.; Wang, Z.; Dai, C.; Li, S.; Li, X.; Xie, Y.; Zheng, Y.; Lin, J.; et al. Clinical application of a double-modified sulfated bacterial cellulose scaffold material loaded with FGFR2-modified adipose-derived stem cells in urethral reconstruction. Stem Cell Res. Ther. 2022, 13, 463. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Wen, Y.; Zhang, Z.; Wang, H.; Warrington, J.A.; Polan, M.L. Menstrual phase-dependent gene expression differences in periurethral vaginal tissue from women with stress incontinence. Am. J. Obstet. Gynecol. 2003, 189, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Gobet, R.; Bleakley, J.; Cisek, L.; Kaefer, M.; Moses, M.A.; Fernandez, C.A.; Peters, C.A. Fetal partial urethral obstruction causes renal fibrosis and is associated with proteolytic imbalance. J. Urol. 1999, 162, 854–860. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Wen, Y.; Wang, H.; Polan, M.L. Differences in estrogen modulation of tissue inhibitor of matrix metalloproteinase-1 and matrix metalloproteinase-1 expression in cultured fibroblasts from continent and incontinent women. Am. J. Obstet. Gynecol. 2003, 189, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Sa, Y.; Wang, L.; Shu, H.; Gu, J. Post-transcriptional suppression of TIMP-1 in epithelial-differentiated adipose-derived stem cells seeded bladder acellular matrix grafts reduces urethral scar formation. Artif. Cells Nanomed. Biotechnol. 2018, 46, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Xie, M.K.; Xu, H.; Wei, Z.W.; Yao, H.J.; Wang, Z.; Zheng, D.C. Hypoxia-preconditioned adipose-derived stem cells combined with scaffold promote urethral reconstruction by upregulation of angiogenesis and glycolysis. Stem Cell Res. Ther. 2020, 11, 535. [Google Scholar] [CrossRef]
- Riis, S.; Hansen, A.C.; Johansen, L.; Lund, K.; Pedersen, C.; Pitsa, A.; Hyldig, K.; Zachar, V.; Fink, T.; Pennisi, C.P. Fabrication and characterization of extracellular matrix scaffolds obtained from adipose-derived stem cells. Methods 2020, 171, 68–76. [Google Scholar] [CrossRef]
- Orabi, H.; Bouhout, S.; Morissette, A.; Rousseau, A.; Chabaud, S.; Bolduc, S. Tissue engineering of urinary bladder and urethra: Advances from bench to patients. Sci. World J. 2013, 2013, 154564. [Google Scholar] [CrossRef]
- Anisimova, N.Y.; Kiselevsky, M.V.; Sukhorukova, I.V.; Shvindina, N.V.; Shtansky, D.V. Fabrication method, structure, mechanical, and biological properties of decellularized extracellular matrix for replacement of wide bone tissue defects. J. Mech. Behav. Biomed. Mater. 2015, 49, 255–268. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Wang, Y.; Zhang, K.; Cao, N.; Yang, R.; Huang, J.; Zhao, W.; Rahman, M.; Liao, H.; Fu, Q. The Fabrication and Evaluation of a Potential Biomaterial Produced with Stem Cell Sheet Technology for Future Regenerative Medicine. Stem Cells Int. 2020, 2020, 9567362. [Google Scholar] [CrossRef] [PubMed]
- Bharadwaj, S.; Liu, G.; Shi, Y.; Wu, R.; Yang, B.; He, T.; Fan, Y.; Lu, X.; Zhou, X.; Liu, H.; et al. Multipotential differentiation of human urine-derived stem cells: Potential for therapeutic applications in urology. Stem Cells. 2013, 31, 1840–1856. [Google Scholar] [CrossRef]
- Zhang, D.; Wei, G.; Li, P.; Zhou, X.; Zhang, Y. Urine-derived stem cells: A novel and versatile progenitor source for cell-based therapy and regenerative medicine. Genes Dis. 2014, 1, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Liu, Y.; Bharadwaj, S.; Atala, A.; Zhang, Y. Human urine-derived stem cells seeded in a modified 3D porous small intestinal submucosa scaffold for urethral tissue engineering. Biomaterials 2011, 32, 1317–1326. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Chen, B.; Deng, J.; Zhuang, G.; Wu, S.; Liu, G.; Deng, C.; Yang, G.; Qiu, X.; Wei, P.; et al. Characterization of rabbit urine-derived stem cells for potential application in lower urinary tract tissue regeneration. Cell Tissue Res. 2018, 374, 303–315. [Google Scholar] [CrossRef]
- Liu, Y.; Ma, W.; Liu, B.; Wang, Y.; Chu, J.; Xiong, G.; Shen, L.; Long, C.; Lin, T.; He, D.; et al. Urethral reconstruction with autologous urine-derived stem cells seeded in three-dimensional porous small intestinal submucosa in a rabbit model. Stem Cell Res. Ther. 2017, 8, 63. [Google Scholar] [CrossRef]
- Lang, R.; Liu, G.; Shi, Y.; Bharadwaj, S.; Leng, X.; Zhou, X.; Liu, H.; Atala, A.; Zhang, Y. Self-renewal and differentiation capacity of urine-derived stem cells after urine preservation for 24 hours. PLoS ONE 2013, 8, e53980. [Google Scholar] [CrossRef]
- Wan, Q.; Xiong, G.; Liu, G.; Shupe, T.D.; Wei, G.; Zhang, D.; Liang, D.; Lu, X.; Atala, A.; Zhang, Y. Urothelium with barrier function differentiated from human urine-derived stem cells for potential use in urinary tract reconstruction. Stem Cell Res. Ther. 2018, 9, 304. [Google Scholar] [CrossRef]
- Kirton, J.P.; Xu, Q. Endothelial precursors in vascular repair. Microvasc. Res. 2010, 79, 193–199. [Google Scholar] [CrossRef]
- Li, Y.; Wu, J.; Feng, F.; Men, C.; Yang, D.; Gao, Z.; Zhu, Z.; Cui, Y.; Zhao, H. A Preclinical Study of Cell-seeded Tubularized Scaffolds Specially Secreting LL37 for Reconstruction of Long Urethral Defects. Anticancer Res. 2017, 37, 4295–4301. [Google Scholar] [CrossRef] [PubMed]
- De Coppi, P.; Bartsch, G., Jr.; Siddiqui, M.M.; Xu, T.; Santos, C.C.; Perin, L.; Mostoslavsky, G.; Serre, A.C.; Snyder, E.Y.; Yoo, J.J.; et al. Isolation of amniotic stem cell lines with potential for therapy. Nat. Biotechnol. 2007, 25, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.H.; Kang, J.J.; Kang, H.G.; Chung, S.S. Urothelial differentiation of human amniotic fluid stem cells by urothelium specific conditioned medium. Cell Biol. Int. 2014, 38, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Prado, S.; Muiños-López, E.; Hermida-Gómez, T.; Cicione, C.; Rendal-Vázquez, M.E.; Fuentes-Boquete, I.; de Toro, F.J.; Blanco, F.J. Human amniotic membrane as an alternative source of stem cells for regenerative medicine. Differentiation 2011, 81, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Seo, M.S.; Park, S.B.; Kim, H.S.; Kang, J.G.; Chae, J.S.; Kang, K.S. Isolation and characterization of equine amniotic membrane-derived mesenchymal stem cells. J. Vet. Sci. 2013, 14, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Alviano, F.; Fossati, V.; Marchionni, C.; Arpinati, M.; Bonsi, L.; Franchina, M.; Lanzoni, G.; Cantoni, S.; Cavallini, C.; Bianchi, F.; et al. Term Amniotic membrane is a high throughput source for multipotent Mesenchymal Stem Cells with the ability to differentiate into endothelial cells in vitro. BMC Dev. Biol. 2007, 7, 11. [Google Scholar] [CrossRef] [PubMed]
- Lv, X.; Guo, Q.; Han, F.; Chen, C.; Ling, C.; Chen, W.; Li, B. Electrospun Poly(l-lactide)/Poly(ethylene glycol) Scaffolds Seeded with Human Amniotic Mesenchymal Stem Cells for Urethral Epithelium Repair. Int. J. Mol. Sci. 2016, 17, 1262. [Google Scholar] [CrossRef] [PubMed]
- Tan, Q.; Le, H.; Tang, C.; Zhang, M.; Yang, W.; Hong, Y.; Wang, X. Tailor-made natural and synthetic grafts for precise urethral reconstruction. J. Nanobiotechnol. 2022, 20, 392. [Google Scholar] [CrossRef]
- Kajbafzadeh, A.M.; Abbasioun, R.; Sabetkish, S.; Sabetkish, N.; Rahmani, P.; Tavakkolitabassi, K.; Arshadi, H. Future Prospects for Human Tissue Engineered Urethra Transplantation: Decellularization and Recellularization-Based Urethra Regeneration. Ann. Biomed. Eng. 2017, 45, 1795–1806. [Google Scholar] [CrossRef]
- Liang, Y.; Yang, C.; Ye, F.; Cheng, Z.; Li, W.; Hu, Y.; Hu, J.; Zou, L.; Jiang, H. Repair of the Urethral Mucosa Defect Model Using Adipose-Derived Stem Cell Sheets and Monitoring the Fate of Indocyanine Green-Labeled Sheets by Near Infrared-II. ACS Biomater. Sci. Eng. 2022, 8, 4909–4920. [Google Scholar] [CrossRef]
- Mikami, H.; Kuwahara, G.; Nakamura, N.; Yamato, M.; Tanaka, M.; Kodama, S. Two-layer tissue engineered urethra using oral epithelial and muscle derived cells. J. Urol. 2012, 187, 1882–1889. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Yang, R.; Zou, Q.; Zhang, K.; Yin, T.; Zhao, W.; Shapter, J.G.; Gao, G.; Fu, Q. Fabrication of Tissue-Engineered Bionic Urethra Using Cell Sheet Technology and Labeling By Ultrasmall Superparamagnetic Iron Oxide for Full-Thickness Urethral Reconstruction. Theranostics 2017, 7, 2509–2523. [Google Scholar] [CrossRef] [PubMed]
- Rashidbenam, Z.; Jasman, M.H.; Tan, G.H.; Goh, E.H.; Fam, X.I.; Ho, C.C.K.; Zainuddin, Z.M.; Rajan, R.; Rani, R.A.; Nor, F.M.; et al. Fabrication of Adipose-Derived Stem Cell-Based Self-Assembled Scaffold under Hypoxia and Mechanical Stimulation for Urethral Tissue Engineering. Int. J. Mol. Sci. 2021, 22, 3350. [Google Scholar] [CrossRef] [PubMed]
- Bhargava, S.; Chapple, C.R. Buccal mucosal urethroplasty: Is it the new gold standard? BJU Int. 2004, 93, 1191–1193. [Google Scholar] [CrossRef] [PubMed]
- Barbagli, G.; Kulkarni, S.B.; Fossati, N.; Larcher, A.; Sansalone, S.; Guazzoni, G.; Romano, G.; Pankaj, J.M.; Dell’Acqua, V.; Lazzeri, M. Long-term followup and deterioration rate of anterior substitution urethroplasty. J. Urol. 2014, 192, 808–813. [Google Scholar] [CrossRef] [PubMed]
- Al Taweel, W.; Seyam, R. Visual Internal Urethrotomy for Adult Male Urethral Stricture Has Poor Long-Term Results. Adv. Urol. 2015, 2015, 656459. [Google Scholar] [CrossRef] [PubMed]
- Scott, K.A.; Li, G.; Manwaring, J.; Nikolavsky, D.A.; Fudym, Y.; Caza, T.; Badar, Z.; Taylor, N.; Bratslavsky, G.; Kotula, L.; et al. Liquid buccal mucosa graft endoscopic urethroplasty: A validation animal study. World J. Urol. 2020, 38, 2139–2145. [Google Scholar] [CrossRef]
- Vaddi, S.P.; Reddy, V.B.; Abraham, S.J. Buccal epithelium Expanded and Encapsulated in Scaffold-Hybrid Approach to Urethral Stricture (BEES-HAUS) procedure: A novel cell therapy-based pilot study. Int. J. Urol. 2019, 26, 253–257. [Google Scholar] [CrossRef]
- Horiguchi, A.; Ojima, K.; Shinchi, M.; Kushibiki, T.; Mayumi, Y.; Miyai, K.; Katoh, S.; Takeda, M.; Iwasaki, M.; Prakash, V.S.; et al. Successful engraftment of epithelial cells derived from autologous rabbit buccal mucosal tissue, encapsulated in a polymer scaffold in a rabbit model of a urethral stricture, transplanted using the transurethral approach. Regen. Ther. 2021, 18, 127–132. [Google Scholar] [CrossRef]
- Horiguchi, A.; Shinchi, M.; Ojima, K.; Hirano, Y.; Kushibiki, T.; Mayumi, Y.; Miyai, K.; Miura, I.; Iwasaki, M.; Suryaprakash, V.; et al. Engraftment of Transplanted Buccal Epithelial Cells onto the Urethrotomy Site, Proven Immunohistochemically in Rabbit Model; a Feat to Prevent Urethral Stricture Recurrence. Stem Cell Rev. Rep. 2023, 19, 275–278. [Google Scholar] [CrossRef]
- Kulkarni, S.B.; Pathak, H.; Khanna, S.; Choubey, S. A prospective, multi-center, open-label, single-arm phase 2b study of autologous adult live cultured buccal epithelial cells (AALBEC) in the treatment of bulbar urethral stricture. World J. Urol. 2021, 39, 2081–2087. [Google Scholar] [CrossRef] [PubMed]
- Barbagli, G.; Sansalone, S.; Djinovic, R.; Romano, G.; Lazzeri, M. Current controversies in reconstructive surgery of the anterior urethra: A clinical overview. Int. Braz. J. Urol. 2012, 38, 307–316, discussion 316. [Google Scholar] [CrossRef] [PubMed]
- Lumen, N.; Oosterlinck, W.; Hoebeke, P. Urethral reconstruction using buccal mucosa or penile skin grafts: Systematic review and meta-analysis. Urol. Int. 2012, 89, 387–394. [Google Scholar] [CrossRef] [PubMed]
- Bhargava, S.; Patterson, J.M.; Inman, R.D.; MacNeil, S.; Chapple, C.R. Tissue-engineered buccal mucosa urethroplasty-clinical outcomes. Eur. Urol. 2008, 53, 1263–1269. [Google Scholar] [CrossRef] [PubMed]
- Lazzeri, M.; Barbagli, G.; Fahlenkamp, D.; Romano, G.; Balsmeyer, U.; Knispel, H.; Spiegeler, M.E.; Stuerzebecher, B.; Ram-Liebig, G. MP9-04 preclinical and clinical examination of tissue-engineered graft for urethral reconstruction (mukocell) with regard to its safety. J. Urol. 2014, 191, e122–e123. [Google Scholar] [CrossRef]
- Barbagli, G.; Akbarov, I.; Heidenreich, A.; Zugor, V.; Olianas, R.; Aragona, M.; Romano, G.; Balsmeyer, U.; Fahlenkamp, D.; Rebmann, U.; et al. Anterior Urethroplasty Using a New Tissue Engineered Oral Mucosa Graft: Surgical Techniques and Outcomes. J. Urol. 2018, 200, 448–456. [Google Scholar] [CrossRef] [PubMed]
- Barbagli, G.; Heidenreich, A.; Zugor, V.; Karapanos, L.; Lazzeri, M. Urothelial or oral mucosa cells for tissue-engineered urethroplasty: A critical revision of the clinical outcome. Asian J. Urol. 2020, 7, 18–23. [Google Scholar] [CrossRef]
- Roh, J.D.; Sawh-Martinez, R.; Brennan, M.P.; Jay, S.M.; Devine, L.; Rao, D.A.; Yi, T.; Mirensky, T.L.; Nalbandian, A.; Udelsman, B.; et al. Tissue-engineered vascular grafts transform into mature blood vessels via an inflammation-mediated process of vascular remodeling. Proc. Natl. Acad. Sci. USA 2010, 107, 4669–4674. [Google Scholar] [CrossRef]
- Hibino, N.; Villalona, G.; Pietris, N.; Duncan, D.R.; Schoffner, A.; Roh, J.D.; Yi, T.; Dobrucki, L.W.; Mejias, D.; Sawh-Martinez, R.; et al. Tissue-engineered vascular grafts form neovessels that arise from regeneration of the adjacent blood vessel. FASEB J. 2011, 25, 2731–2739. [Google Scholar] [CrossRef]
- Ankrum, J.A.; Ong, J.F.; Karp, J.M. Mesenchymal stem cells: Immune evasive, not immune privileged. Nat. Biotechnol. 2014, 32, 252–260. [Google Scholar] [CrossRef]
- Davis, N.F.; Cunnane, E.M.; Mulvihill, J.J.; Quinlan, M.R.; Bolton, D.M.; Walsh, M.T.; Jack, G.S. The Role of Stem Cells for Reconstructing the Lower Urinary Tracts. Curr. Stem Cell Res. Ther. 2018, 13, 458–465. [Google Scholar] [CrossRef]
- Kang, H.S.; Choi, S.H.; Kim, B.S.; Choi, J.Y.; Park, G.B.; Kwon, T.G.; Chun, S.Y. Advanced Properties of Urine Derived Stem Cells Compared to Adipose Tissue Derived Stem Cells in Terms of Cell Proliferation, Immune Modulation and Multi Differentiation. J. Korean Med. Sci. 2015, 30, 1764–1776. [Google Scholar] [CrossRef]
| Cell Type | Source | Function in Urethral Regeneration | References |
|---|---|---|---|
| Mucosal epithelial cells | Bladder mucosa | Support epithelial integrity, stratification, and continuity with normal urothelium; reduce potential rejection reactions; and improve the biocompatibility of the graft material. | [16,18,19,21] |
| Oral mucosa | Promotion of urethral epithelial regeneration; participation in the construction of tissue-engineered buccal mucosa (TEBM). | [2,25,26,27] | |
| Skin/foreskin | Form a thick barrier to isolate urine. | [19,30] | |
| Mesothelial cells | Peritoneal/vaginal endothelial | Act as a substitute for epithelial cells. | [34] |
| Smooth muscle cells | Bladder | Promote earlier, more mature regeneration of urethral smooth muscle; enhance the mechanical properties of grafts; and support the epithelial–mesenchymal interactions required for normal maturation of the urothelium. | [14,22,26,35,36,37,38,39,40] |
| Endothelial cells | Foreskin | Promote tissue angiogenesis and graft vascularization. | [41] |
| Cell Type | Source | Function in Urethral Regeneration | References |
|---|---|---|---|
| Pluripotent stem cells | Human embryos | Differentiate to any cell type in the urethra. | [47,48,49] |
| Reprogrammed cells from adult tissues | |||
| BMDSCs | Bone marrow | Differentiate into urothelial cells and bladder SMCs; reduce fibrosis and inflammation; and interact with other cells to further promote tissue regeneration. | [50,51,52,53,54] |
| ADSCs | Adipose tissue | Differentiate into urothelial cells and SMCs; prevent fibrosis and reduce scarring; promote regeneration of vascular and smooth muscle tissues; and reduce the inflammatory response. Paracrine function promotes regeneration. | [56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,77,78] |
| UDSCs | Urine | Differentiate into urothelial cells, SMCs, and endothelial cells; promote regeneration of vascular and smooth muscle tissues; secrete various growth factors; and promote vascularization. | [83,84,85,86,87,88,89] |
| EPCs | Venous blood and bone marrow | Involved in vascular remodeling and angiogenesis. | [54,90,91] |
| hAFSCs | Amniotic fluid | Differentiate into urothelial cells. | [92,93] |
| AMSCs | Amniotic membrane | Promotes regeneration of the urethral epithelium. | [97] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, Y.; Zhao, W.; Yang, M.; Fang, W.; Gao, G.; Wang, Y.; Fu, Q. Cell-Based Therapy for Urethral Regeneration: A Narrative Review and Future Perspectives. Biomedicines 2023, 11, 2366. https://doi.org/10.3390/biomedicines11092366
Jin Y, Zhao W, Yang M, Fang W, Gao G, Wang Y, Fu Q. Cell-Based Therapy for Urethral Regeneration: A Narrative Review and Future Perspectives. Biomedicines. 2023; 11(9):2366. https://doi.org/10.3390/biomedicines11092366
Chicago/Turabian StyleJin, Yangwang, Weixin Zhao, Ming Yang, Wenzhuo Fang, Guo Gao, Ying Wang, and Qiang Fu. 2023. "Cell-Based Therapy for Urethral Regeneration: A Narrative Review and Future Perspectives" Biomedicines 11, no. 9: 2366. https://doi.org/10.3390/biomedicines11092366






