Clinical and Radiological Deterioration in a Case of Creutzfeldt–Jakob Disease following SARS-CoV-2 Infection: Hints to Accelerated Age-Dependent Neurodegeneration
Abstract
:1. Introduction
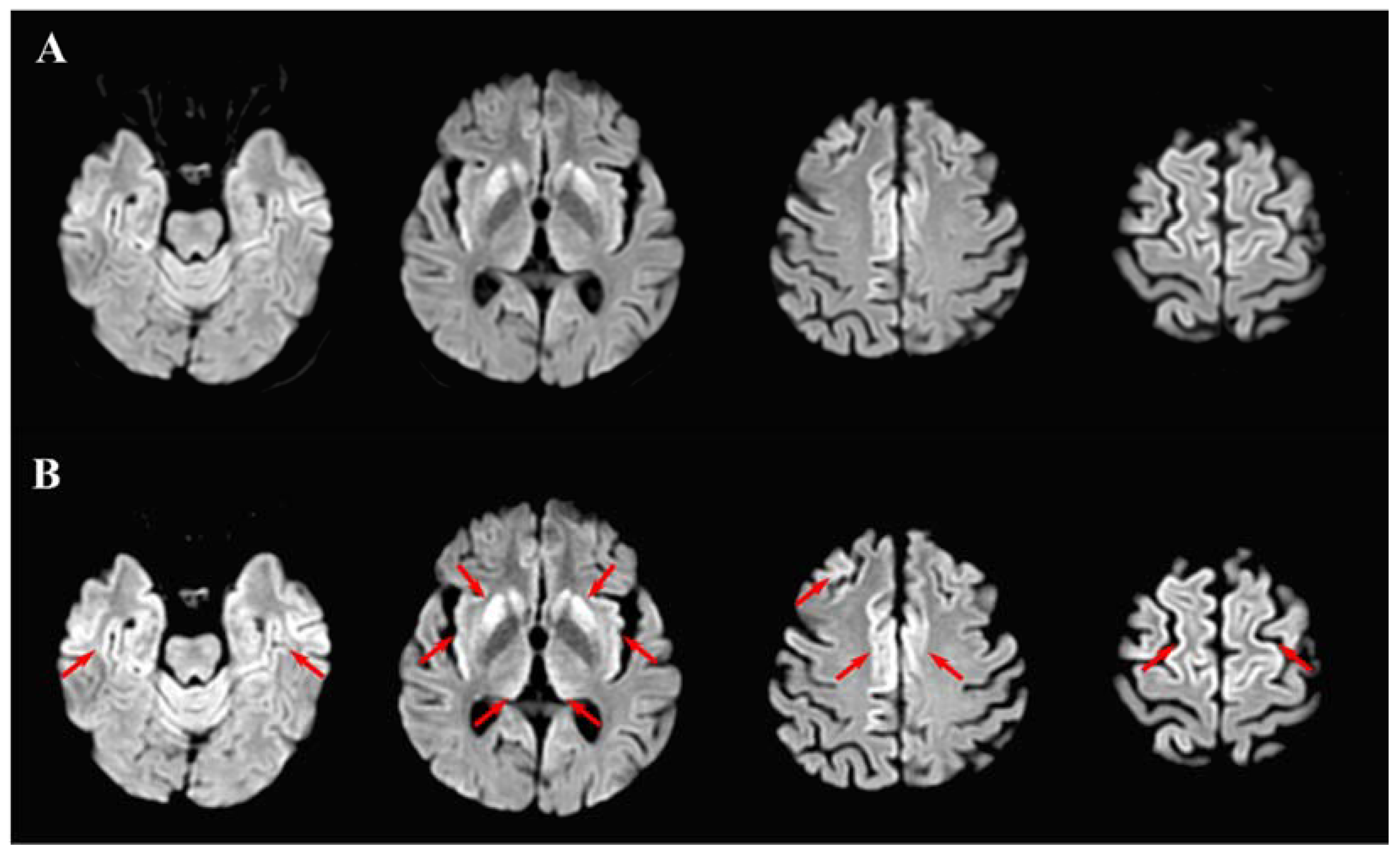
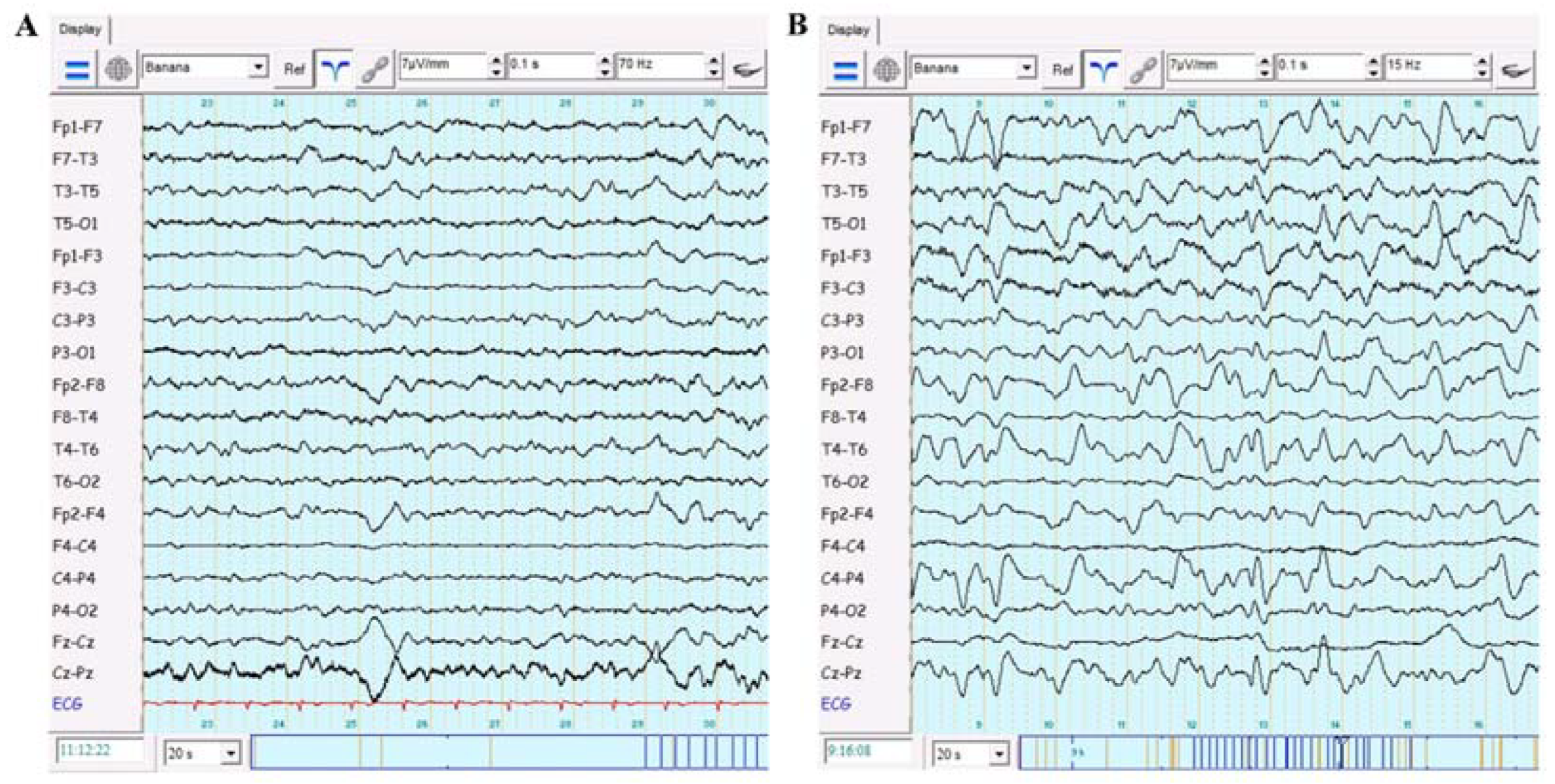
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sikorska, B.; Knight, R.; Ironside, J.W.; Liberski, P.P. Creutzfeldt-Jakob disease. Neurodegener. Dis. 2012, 724, 76–90. [Google Scholar]
- Iwasaki, Y. Creutzfeldt-Jakob disease. Neuropathology 2017, 37, 174–188. [Google Scholar] [CrossRef]
- Ladogana, A.; Kovacs, G.G. Genetic Creutzfeldt–Jakob disease. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2018; Volume 153, pp. 219–242. [Google Scholar]
- Zerr, I.; Parchi, P. Sporadic Creutzfeldt–Jakob disease. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2018; Volume 153, pp. 155–174. [Google Scholar]
- Zerr, I.; Kallenberg, K.; Summers, D.; Romero, C.; Taratuto, A.; Heinemann, U.; Breithaupt, M.; Varges, D.; Meissner, B.; Ladogana, A. Updated clinical diagnostic criteria for sporadic Creutzfeldt-Jakob disease. Brain 2009, 132, 2659–2668. [Google Scholar] [CrossRef] [Green Version]
- Hermann, P.; Appleby, B.; Brandel, J.-P.; Caughey, B.; Collins, S.; Geschwind, M.D.; Green, A.; Haïk, S.; Kovacs, G.G.; Ladogana, A. Biomarkers and diagnostic guidelines for sporadic Creutzfeldt-Jakob disease. Lancet Neurol. 2021, 20, 235–246. [Google Scholar] [CrossRef]
- Barnett, F.; McLEAN, G. Care management of Creutzfeldt–Jakob disease within the United Kingdom. J. Nurs. Manag. 2005, 13, 111–118. [Google Scholar] [CrossRef]
- Amore, S.; Puppo, E.; Melara, J.; Terracciano, E.; Gentili, S.; Liotta, G. Impact of COVID-19 on older adults and role of long-term care facilities during early stages of epidemic in Italy. Sci. Rep. 2021, 11, 12530. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines; National Institutes of Health: Bethesda, MD, USA, 2020.
- Guan, W.-j.; Ni, Z.-y.; Hu, Y.; Liang, W.-h.; Ou, C.-q.; He, J.-x.; Liu, L.; Shan, H.; Lei, C.-l.; Hui, D.S. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Ciolac, D.; Crivorucica, I.; Zota, E.; Gorincioi, N.; Efremova, D.; Manea, D.; Crivorucica, V.; Ciocanu, M.; Groppa, S.A. Extensive cerebellar involvement and cognitive impairment in COVID-19-associated acute necrotizing encephalopathy. Ther. Adv. Neurol. Disord. 2021, 14, 1756286420985175. [Google Scholar] [CrossRef] [PubMed]
- Groppa, S.A.; Ciolac, D.; Duarte, C.; Garcia, C.; Gasnaș, D.; Leahu, P.; Efremova, D.; Gasnaș, A.; Bălănuță, T.; Mîrzac, D.; et al. Molecular Mechanisms of SARS-CoV-2/COVID-19 Pathogenicity on the Central Nervous System: Bridging Experimental Probes to Clinical Evidence and Therapeutic Interventions; Springer International Publishing: Cham, Switzerland, 2021; pp. 1–27. [Google Scholar]
- Ciolac, D.; Crivorucica, I.; Zota, E.; Manea, D.; Efremova, D.; Gușanu, L.; Crivorucica, V.; Ciocanu, M.; Groppa, S.A. Gray Matter-Restricted Whole Spinal Cord Involvement in a Young Woman with SARS-CoV-2 Infection. J. Magn. Reson. Imaging 2005, 1–3. [Google Scholar] [CrossRef]
- Ulinici, M.; Covantev, S.; Wingfield-Digby, J.; Beloukas, A.; Mathioudakis, A.G.; Corlateanu, A. Screening, Diagnostic and Prognostic Tests for COVID-19: A Comprehensive Review. Life 2021, 11, 561. [Google Scholar] [CrossRef] [PubMed]
- Bek, L.M.; Berentschot, J.C.; Hellemons, M.E.; Huijts, S.M.; Aerts, J.G.; van Bommel, J.; van Genderen, M.E.; Gommers, D.A.; Ribbers, G.M.; Heijenbrok-Kal, M.H. CO-FLOW: COvid-19 Follow-up care paths and Long-term Outcomes Within the Dutch health care system: Study protocol of a multicenter prospective cohort study following patients 2 years after hospital discharge. BMC Health Serv. Res. 2021, 21, 847. [Google Scholar] [CrossRef]
- Mabbott, N.A.; Bradford, B.M.; Pal, R.; Young, R.; Donaldson, D.S. The effects of immune system modulation on prion disease susceptibility and pathogenesis. Int. J. Mol. Sci. 2020, 21, 7299. [Google Scholar] [CrossRef] [PubMed]
- Nasiri, E.; Naseri, A.; Yazdchi, M.; Talebi, M. Is there a link between COVID-19 and Creutzfeldt-Jakob Disease? A Case Report. J. Res. Clin. Med. 2021, 9, 26. [Google Scholar] [CrossRef]
- Young, M.J.; O’Hare, M.; Matiello, M.; Schmahmann, J.D. Creutzfeldt-Jakob disease in a man with COVID-19: SARS-CoV-2-accelerated neurodegeneration? Brain Behav. Immun. 2020, 89, 601–603. [Google Scholar] [CrossRef]
- Rodriguez, M.; Soler, Y.; Perry, M.; Reynolds, J.L.; El-Hage, N. Impact of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the nervous system: Implications of COVID-19 in neurodegeneration. Front. Neurol. 2020, 11, 583459. [Google Scholar] [CrossRef] [PubMed]
- Heneka, M.T.; Golenbock, D.; Latz, E.; Morgan, D.; Brown, R. Immediate and long-term consequences of COVID-19 infections for the development of neurological disease. Alzheimer’s Res. Ther. 2020, 12, 69. [Google Scholar] [CrossRef] [PubMed]
- Cohen, M.E.; Eichel, R.; Steiner-Birmanns, B.; Janah, A.; Ioshpa, M.; Bar-Shalom, R.; Paul, J.J.; Gaber, H.; Skrahina, V.; Bornstein, N.M. A case of probable Parkinson’s disease after SARS-CoV-2 infection. Lancet Neurol. 2020, 19, 804–805. [Google Scholar] [CrossRef]
- Salari, M.; Etemadifar, M. Can COVID-19 accelerate neurodegeneration? Clin. Case Rep. 2021, 9, e04433. [Google Scholar] [CrossRef]
- Jang, J.-W.; Park, S.Y.; Park, Y.H.; Kim, J.E.; Kim, S. Symptomatic aggravation after corticosteroid pulse therapy in definite sporadic Creutzfeldt-Jakob disease with the feature of Hashimoto’s encephalopathy. BMC Neurol. 2014, 14, 179. [Google Scholar] [CrossRef] [Green Version]
- Septyaningtrias, D.E.; Susilowati, R. Neurological involvement of COVID-19: From neuroinvasion and neuroimmune crosstalk to long-term consequences. Rev. Neurosci. 2021, 32, 427–442. [Google Scholar] [CrossRef]
- Espíndola, O.M.; Gomes, Y.C.; Brandão, C.O.; Torres, R.C.; Siqueira, M.; Soares, C.N.; Lima, M.A.S.; Leite, A.C.C.; Venturotti, C.O.; Carvalho, A.J.C. Inflammatory Cytokine Patterns Associated with Neurological Diseases in Coronavirus Disease 2019. Ann. Neurol. 2021, 89, 1041–1045. [Google Scholar] [CrossRef] [PubMed]
- Najjar, S.; Najjar, A.; Chong, D.J.; Pramanik, B.K.; Kirsch, C.; Kuzniecky, R.I.; Pacia, S.V.; Azhar, S. Central nervous system complications associated with SARS-CoV-2 infection: Integrative concepts of pathophysiology and case reports. J. Neuroinflammation 2020, 17, 231. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Makarava, N.; Chang, J.C.-Y.; Molesworth, K.; Baskakov, I.V. Region-specific glial homeostatic signature in prion diseases is replaced by a uniform neuroinflammation signature, common for brain regions and prion strains with different cell tropism. Neurobiol. Dis. 2020, 137, 104783. [Google Scholar] [CrossRef] [PubMed]
- Llorens, F.; Thüne, K.; Sikorska, B.; Schmitz, M.; Tahir, W.; Fernández-Borges, N.; Cramm, M.; Gotzmann, N.; Carmona, M.; Streichenberger, N. Altered Ca2+ homeostasis induces Calpain-Cathepsin axis activation in sporadic Creutzfeldt-Jakob disease. Acta Neuropathol. Commun. 2017, 5, 35. [Google Scholar] [CrossRef]
- Duarte, C.; Akkaoui, J.; Ho, A.; Garcia, C.; Yamada, C.; Movila, A. Age-dependent effects of the recombinant spike protein/SARS-CoV-2 on the M–CSF–and IL-34-differentiated macrophages in vitro. Biochem. Biophys. Res. Commun. 2021, 546, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Ramani, A.; Müller, L.; Ostermann, P.N.; Gabriel, E.; Abida-Islam, P.; Müller-Schiffmann, A.; Mariappan, A.; Goureau, O.; Gruell, H.; Walker, A. SARS-CoV-2 targets neurons of 3D human brain organoids. EMBO J. 2020, 39, e106230. [Google Scholar] [CrossRef] [PubMed]
- Tavassoly, O.; Safavi, F.; Tavassoly, I. Seeding Brain Protein Aggregation by SARS-CoV-2 as a Possible Long-Term Complication of COVID-19 Infection. ACS Chem. Neurosci. 2020, 11, 3704–3706. [Google Scholar] [CrossRef]
| Parameter | Range | COVID-19 ICU | Neurology Ward | ICU | |||||
|---|---|---|---|---|---|---|---|---|---|
| Day 1 (Admission) | Day 5 | Day 10 | Day 1 | Day 4 (Neurological Aggravation) | Day 8 | Day 1 | Day 3 (Death) | ||
| HGB | 120–140 g/L | 126 | 132 | 116 | 114 | 124 | 105 | 116 | 118 |
| RBC | 3.7–4.7 × 1012/L | 4.1 | 4.7 | 3.9 | 3.6 | 4.4 | 3.2 | 3.9 | 4 |
| PLT | 150–400 × 109/L | 209 | 186 | 222 | 207 | 296 | 119 | 275 | 239 |
| WBC | 4–9 × 109/L | 4.9 | 12.4 | 20.6 | 27.5 | 17.6 | 19.7 | 27.3 | 25.2 |
| NEUT | 47–72 (%) | 49 | 75 | 77 | 84 | 63 | 60 | 45 | 23 |
| LY | 19–37 (%) | 32 | 5 | 15 | 3 | 22 | 15 | 6 | 15 |
| Parameter | Range | COVID-19 ICU | Neurology Ward | ICU | |||||
|---|---|---|---|---|---|---|---|---|---|
| Day 1 (Admission) | Day 5 | Day 10 | Day 1 | Day 4 (Neurological Aggravation) | Day 8 | Day 1 | Day 3 (Death) | ||
| CRP | <6 (mg/mL) | 48 | 32 | 66 | - | 46 | - | 48 | - |
| Fibrinogen | 2–4 (g/L) | 5.3 | 5.7 | 6.9 | 6.4 | 5.3 | 4.1 | 6 | 4.8 |
| D-dimer | 0–0.5 mg/mL | 1.02 | 1.64 | - | - | 1.8 | - | 1.72 | - |
| Procalcitonin | <0.05 ng/mL | 0.1 | 0.1 | - | - | 0.25 | - | 4 | - |
| ESR | 2–15 mm/h | 40 | 51 | 26 | 24 | 22 | 17 | 19 | 21 |
| Parameter | Range | COVID-19 ICU | Neurology Ward | ICU | |||||
|---|---|---|---|---|---|---|---|---|---|
| Day 1 (Admission) | Day 5 | Day 10 | Day 1 | Day 4 (Neurological Aggravation) | Day 8 | Day 1 | Day 3 (Death) | ||
| AST | <40 U/L | 51 | 30 | 20 | 94 | 41 | 38 | 42 | 44 |
| ALT | <41 U/L | 50 | 73 | 132 | 77 | 72 | 43 | 34 | 39 |
| Glucose | 3.3–5.5 mmol/L | 5.2 | 6.9 | 4.8 | 7.2 | 3.9 | 5.4 | 6.3 | 6 |
| BUN | 2.5–8.3 mmol/L | 6.7 | 8.5 | 7.4 | 16.5 | 7.9 | 4.7 | 8.8 | 8.5 |
| Creatinine | 44–88 mmol/L | 77 | 64 | 87 | 77 | 58 | 35 | 59 | 70 |
| Protein | 64–83 g/L | 82 | 64 | 52 | 48 | 52 | 47 | 50 | 52 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciolac, D.; Racila, R.; Duarte, C.; Vasilieva, M.; Manea, D.; Gorincioi, N.; Condrea, A.; Crivorucica, I.; Zota, E.; Efremova, D.; et al. Clinical and Radiological Deterioration in a Case of Creutzfeldt–Jakob Disease following SARS-CoV-2 Infection: Hints to Accelerated Age-Dependent Neurodegeneration. Biomedicines 2021, 9, 1730. https://doi.org/10.3390/biomedicines9111730
Ciolac D, Racila R, Duarte C, Vasilieva M, Manea D, Gorincioi N, Condrea A, Crivorucica I, Zota E, Efremova D, et al. Clinical and Radiological Deterioration in a Case of Creutzfeldt–Jakob Disease following SARS-CoV-2 Infection: Hints to Accelerated Age-Dependent Neurodegeneration. Biomedicines. 2021; 9(11):1730. https://doi.org/10.3390/biomedicines9111730
Chicago/Turabian StyleCiolac, Dumitru, Renata Racila, Carolina Duarte, Maria Vasilieva, Diana Manea, Nadejda Gorincioi, Alexandra Condrea, Igor Crivorucica, Eremei Zota, Daniela Efremova, and et al. 2021. "Clinical and Radiological Deterioration in a Case of Creutzfeldt–Jakob Disease following SARS-CoV-2 Infection: Hints to Accelerated Age-Dependent Neurodegeneration" Biomedicines 9, no. 11: 1730. https://doi.org/10.3390/biomedicines9111730






