Association of Combined Metals and PFAS with Cardiovascular Disease Risk
Abstract
:1. Introduction
1.1. Cardiovascular Disease a Public Health Issue of Concern
1.2. Metals Adversely Affect Cardiovascular Health
1.3. PFASs Adversely Affect Cardiovascular Health
1.4. Mixed Exposures Better Model Environmental Effects on Cardiovascular Health
2. Materials and Methods
2.1. Sampling Strategy and Description Participants
2.2. Quantifying PFAS and Metals
2.3. Measuring Cardiovascular Variables
2.3.1. Cardiovascular Indexes
2.3.2. Framingham Risk Score
2.4. Statistical Analysis
2.4.1. Descriptive Statistics
2.4.2. Multivariable Linear Regression
2.4.3. Bayesian Kernel Machine Regression (BKMR)
3. Results
3.1. Characteristics of the Sample Population
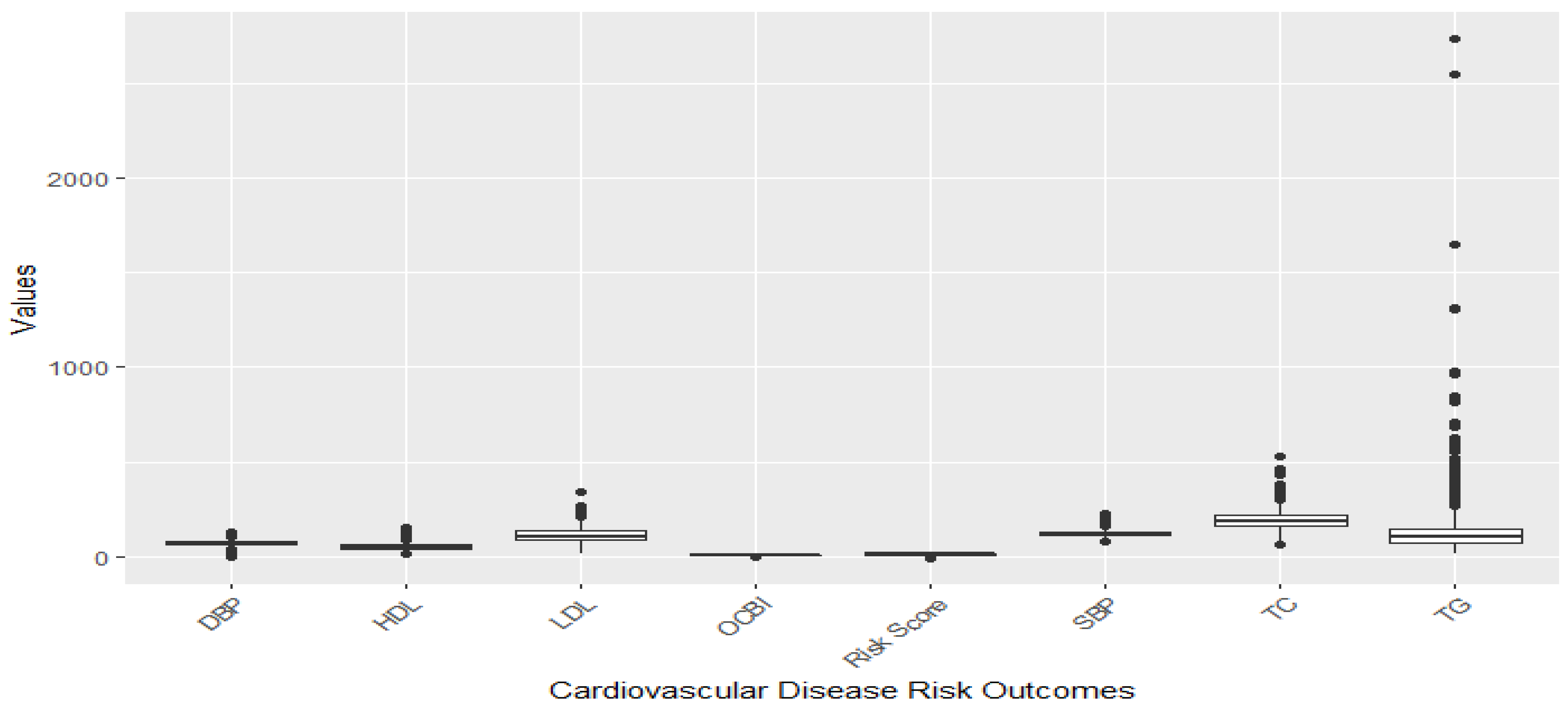
3.2. Distribution of Exposure and Study Variables
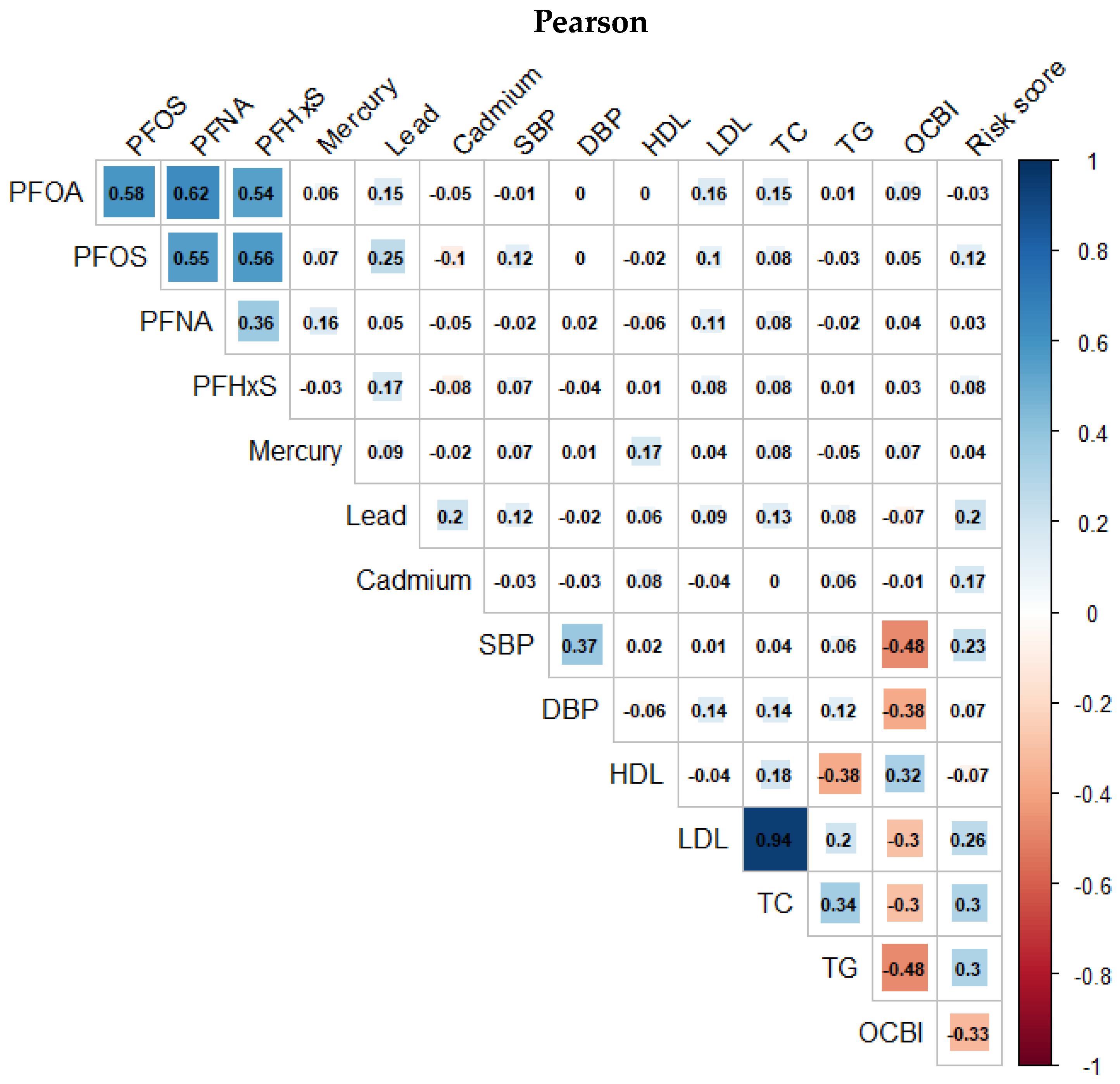
3.3. Correlation between Pollution Variables and Cardiovascular-Related Variables
3.4. Association between Pollution Variables and Cardiovascular-Related Variables
3.5. Association between Pollution Variables and Framingham Risk Score
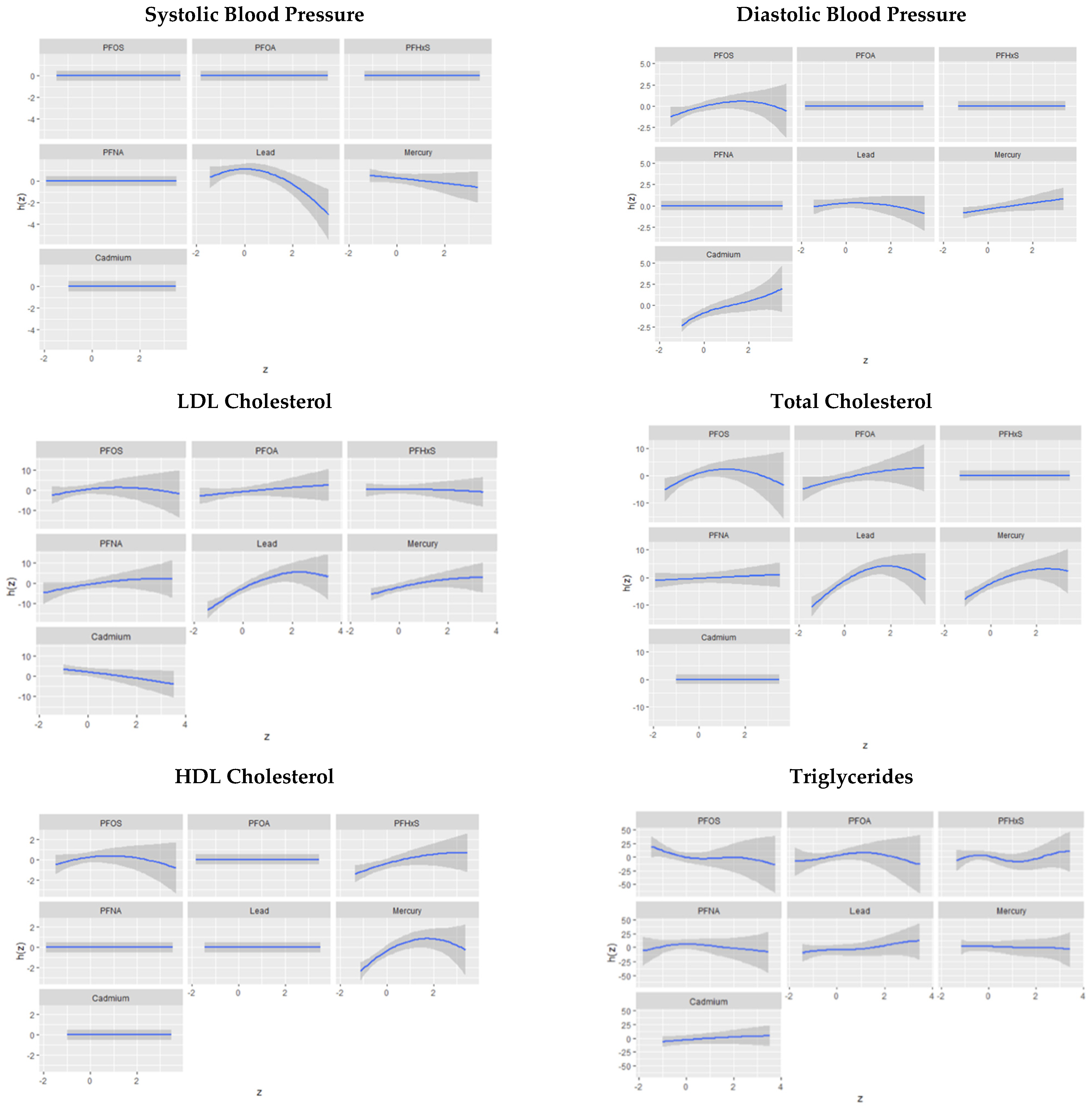
3.6. BKMR Analysis
3.6.1. Univariate Association of PFASs and Metals with Systolic and Diastolic Blood Pressure
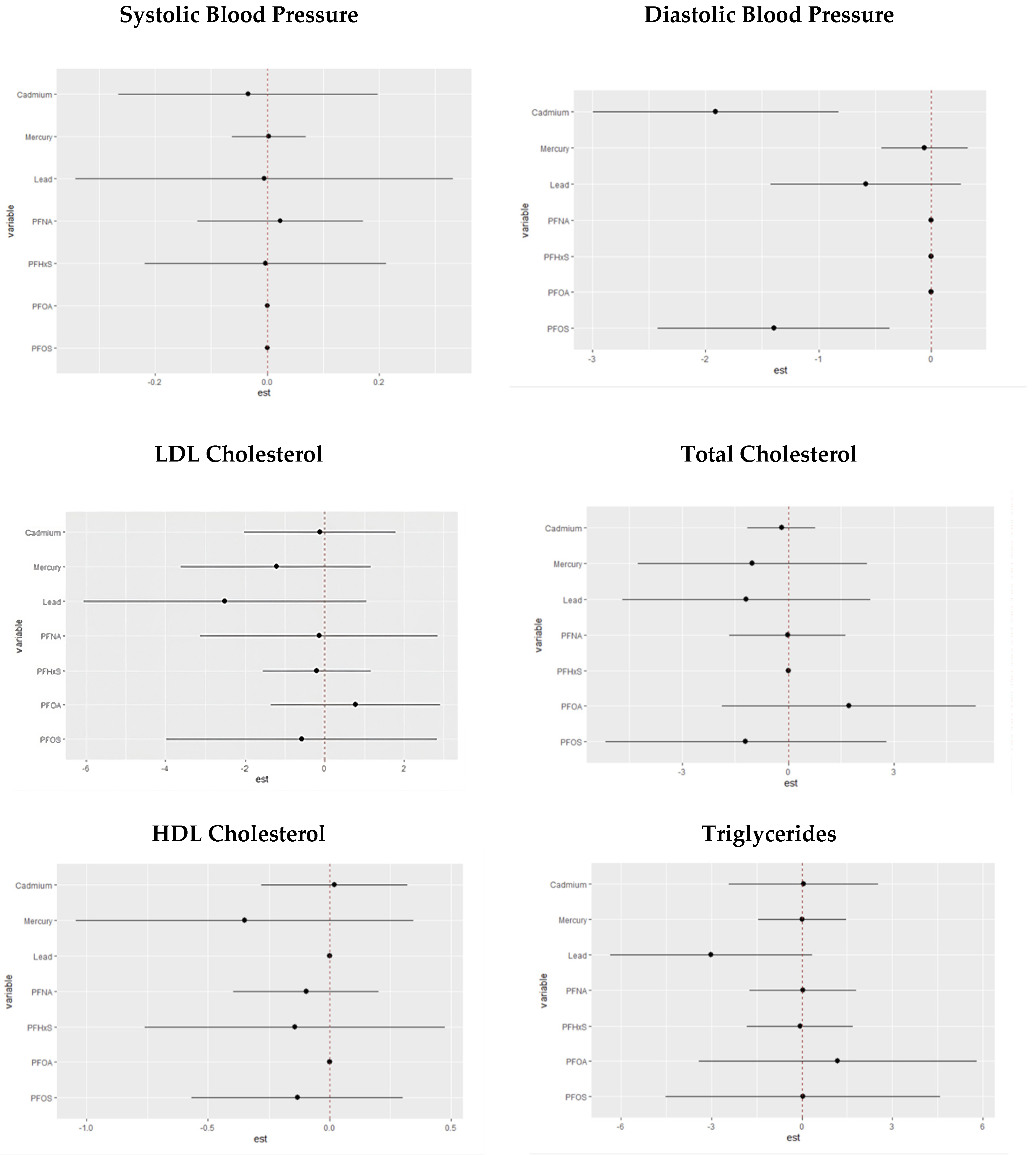
3.6.2. Single-Variable Effects of PFASs and Metals on Individual Cardiovascular-Related Markers
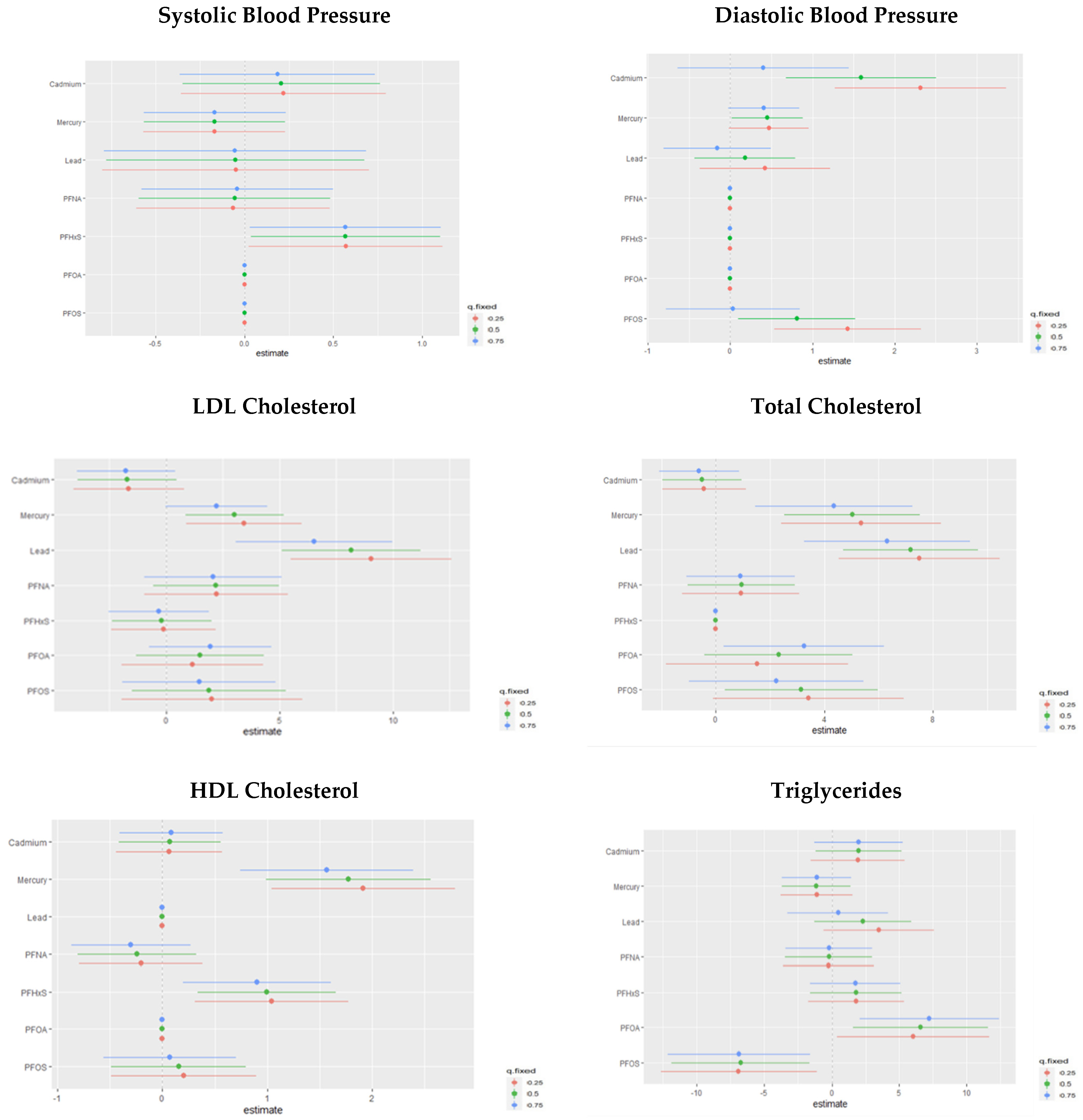
3.7. Single-Variable Interaction Terms of PFASs and Metals on Individual CVD-Related Markers
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Framingham Risk Scor
| Criteria 1: Age by Gender. | ||
| Female | ||
| Framingham Risk Score by Gender | Age | Point |
| Female | ≥20 & ≤34 | −7 |
| 35 & ≤39 | −3 | |
| 40 & ≤44 | 0 | |
| 45 & ≤49 | 3 | |
| 50 & ≤54 | 6 | |
| 55 & ≤59 | 8 | |
| 60 & ≤64 | 10 | |
| 65 & ≤69 | 12 | |
| 70 & ≤74 | 14 | |
| 75 & ≤79 | 16 | |
| Male | ||
| Male | ≥20 & ≤34 | −9 |
| 35 & ≤39 | −4 | |
| 40 & ≤44 | 0 | |
| 45 & ≤49 | 3 | |
| 50 & ≤54 | 6 | |
| 55 & ≤59 | 8 | |
| 60 & ≤64 | 10 | |
| 65 & ≤69 | 11 | |
| 70 & ≤74 | 12 | |
| 75 & ≤79 | 13 | |
| Criteria 2: Age and Total Cholesterol by Gender. | |||
| Female | |||
| Framingham Risk Score by Gender | Age | Total Cholesterol | Point |
| Female | ≥20 & ≤39 | <160 | 0 |
| ≥20 & ≤39 | ≥160 & <200 | 4 | |
| ≥20 & ≤39 | ≥200 & <240 | 8 | |
| ≥20 & ≤39 | ≥240 & <280 | 11 | |
| ≥20 & ≤39 | ≥280 | 13 | |
| 40 & ≤49 | <160 | 0 | |
| 40 & ≤49 | ≥160 & <200 | 3 | |
| 40 & ≤49 | ≥200 & <240 | 6 | |
| 40 & ≤49 | ≥240 & <280 | 8 | |
| 40 & ≤49 | ≥280 | 10 | |
| 50 & ≤59 | <160 | 0 | |
| 50 & ≤59 | ≥160 & <200 | 2 | |
| 50 & ≤59 | ≥200 & <240 | 4 | |
| 50 & ≤59 | ≥240 & <280 | 5 | |
| 50 & ≤59 | ≥280 | 7 | |
| 60 & ≤69 | <160 | 0 | |
| 60 & ≤69 | ≥160 & <200 | 1 | |
| 60 & ≤69 | ≥200 & <240 | 2 | |
| 60 & ≤69 | ≥240 & <280 | 3 | |
| 60 & ≤69 | ≥280 | 4 | |
| 70 & ≤79 | <160 | 0 | |
| 70 & ≤79 | ≥160 & <200 | 1 | |
| 70 & ≤79 | ≥200 & <240 | 2 | |
| 70 & ≤79 | ≥240 & <280 | 3 | |
| 70 & ≤79 | ≥280 | 4 | |
| Male | |||
| Framingham Risk Score by Gender | Age | Total Cholesterol | Point |
| Male | ≥20 & ≤39 | <160 | 0 |
| ≥20 & ≤39 | ≥160 & <200 | 4 | |
| ≥20 & ≤39 | ≥200 & <240 | 7 | |
| ≥20 & ≤39 | ≥240 & <280 | 9 | |
| ≥20 & ≤39 | ≥280 | 8 | |
| 40 & ≤49 | < 160 | 0 | |
| 40 & ≤49 | ≥160 & <200 | 3 | |
| 40 & ≤49 | ≥200 & <240 | 5 | |
| 40 & ≤49 | ≥240 & <280 | 6 | |
| 40 & ≤49 | ≥280 | 8 | |
| 50 & ≤59 | <160 | 0 | |
| 50 & ≤59 | ≥160 & <200 | 2 | |
| 50 & ≤59 | ≥200 & <240 | 3 | |
| 50 & ≤59 | ≥240 & <280 | 4 | |
| 50 & ≤59 | ≥280 | 5 | |
| 60 & ≤69 | <160 | 0 | |
| 60 & ≤69 | ≥160 & <200 | 1 | |
| 60 & ≤69 | ≥200 & <240 | 1 | |
| 60 & ≤69 | ≥240 & <280 | 2 | |
| 60 & ≤69 | ≥280 | 3 | |
| 70 & ≤79 | <160 | 0 | |
| 70 & ≤79 | ≥160 & <200 | 0 | |
| 70 & ≤79 | ≥200 & <240 | 0 | |
| 70 & ≤79 | ≥240 & <280 | 1 | |
| 70 & ≤79 | ≥280 | 1 | |
| Criteria 3: Smoker. | |||
|---|---|---|---|
| Female | |||
| Framingham Risk Score by Gender | Smoker | Age | Point |
| Female | Yes | 20 & Age ≤ 39 | 9 |
| Yes | 40 & Age ≤ 49 | 7 | |
| Yes | 50 & Age ≤ 59 | 4 | |
| Yes | 60 & Age ≤ 69 | 2 | |
| Yes | 70 & Age ≤ 79 | 1 | |
| No | 0 | ||
| Male | |||
| Male | Yes | 20 & Age ≤ 39 | 8 |
| Yes | 40 & Age ≤ 49 | 5 | |
| Yes | 50 & Age ≤ 59 | 3 | |
| Yes | 60 & Age ≤ 69 | 1 | |
| Yes | 70 & Age ≤ 79 | 1 | |
| No | 0 | ||
| Criteria 4: HDL. | ||
| Female | ||
| Framingham Risk Score by Gender | HDL | Point |
| HDL ≥ 60 | −1 | |
| HDL ≥ 50 | 0 | |
| HDL ≥ 40 | 1 | |
| HDL < 40 | 2 | |
| Male | ||
| Male | HDL ≥ 60 | −1 |
| HDL ≥ 50 | 0 | |
| HDL ≥ 40 | 1 | |
| HDL < 40 | 2 | |
| Criteria 5: The participant has Systolic Blood Pressure and Treatment status. | |||
| Female | |||
| Framingham Risk Score by Gender | Treatment Status | Systolic Blood Pressure | Point |
| Female | Treated | <120 | 0 |
| Treated | ≥120 & <130 | 3 | |
| Treated | 130 & <140 | 4 | |
| Treated | 140 & <160 | 5 | |
| Treated | ≥160 | 6 | |
| Untreated | <120 | 0 | |
| Untreated | ≥120 & <130 | 1 | |
| Untreated | 130 & <140 | 2 | |
| Untreated | 140 & <160 | 3 | |
| Untreated | ≥160 | 4 | |
| Male | |||
| Male | Treated | <120 | 0 |
| Treated | ≥120 & <130 | 1 | |
| Treated | 130 & <140 | 2 | |
| Treated | 140 & <160 | 2 | |
| Treated | ≥160 | 3 | |
| Untreated | <120 | 0 | |
| Untreated | ≥120 & <130 | 0 | |
| Untreated | 130 & <140 | 2 | |
| Untreated | 140 & <160 | 2 | |
| Untreated | ≥160 | 3 | |
| Note: Women: The following point totals are related to different 10-year risks in %. Under 9 points: <1%; 9–12 points: 1%; 13–14 points: 2%; 15 points: 3%; 16 points: 4%; 17 points: 5%; 18 points: 6%; 19 points: 8%; 20 points: 11%; 21 = 14%, 22 = 17%, 23 = 22%, 24 = 27%, and >25= over 30%. Men: The following point totals are related to different 10-year risk in %. Less than 1 point: <1%; 1–4 points: 1%; 5–6 points: 2%; 7 points: 3%; 8 points: 4%; 9 points: 5%; 10 points: 6%; 11 points: 8%; 12 points: 10%; 13 points: 12%; 14 points: 16%; 15 points: 20%; 16 points: 25%; 17 points or more: over 30%. | |||
References
- Deaton, C.; Froelicher, E.S.; Wu, L.H.; Ho, C.; Shishani, K.; Jaarsma, T. The global burden of cardiovascular disease. Eur. J. Cardiovasc. Nurs. 2011, 10, S5–S13. [Google Scholar] [CrossRef] [PubMed]
- Labarthe, D.R.; Dunbar, S.B. Global cardiovascular health promotion and disease prevention: 2011 and beyond. Circulation 2012, 125, 2667–2676. [Google Scholar] [CrossRef] [PubMed]
- Berner-Rodoreda, A.; Kanyama, C.; Supady, A.; Bärnighausen, T. Cardiovascular Diseases. In Global Health Essentials; Springer: Berlin/Heidelberg, Germany, 2023; pp. 157–162. [Google Scholar]
- Kelishadi, R.; Poursafa, P. A review on the genetic, environmental, and lifestyle aspects of the early-life origins of cardiovascular disease. Curr. Probl. Pediatr. Adolesc. Health Care 2014, 44, 54–72. [Google Scholar] [CrossRef] [PubMed]
- Alissa, E.M.; Ferns, G.A. Heavy metal poisoning and cardiovascular disease. J. Toxicol. 2011, 2011, 870125. [Google Scholar] [CrossRef] [PubMed]
- Sevim, Ç.; Doğan, E.; Comakli, S. Cardiovascular disease and toxic metals. Curr. Opin. Toxicol. 2020, 19, 88–92. [Google Scholar] [CrossRef]
- Navas-Acien, A.; Guallar, E.; Silbergeld, E.K.; Rothenberg, S.J. Lead exposure and cardiovascular disease—A systematic review. Environ. Health Perspect. 2007, 115, 472–482. [Google Scholar] [CrossRef]
- Yim, G.; Wang, Y.; Howe, C.G.; Romano, M.E. Exposure to metal mixtures in association with cardiovascular risk factors and outcomes: A scoping review. Toxics 2022, 10, 116. [Google Scholar] [CrossRef]
- Kacholi, D.S.; Sahu, M. Levels and health risk assessment of heavy metals in soil, water, and vegetables of Dar es Salaam, Tanzania. J. Chem. 2018, 2018, 1402674. [Google Scholar] [CrossRef]
- Obeng-Gyasi, E.; Tarver, W.; Obeng-Gyasi, S. Allostatic Load and Breast Cancer: A Systematic Review of the Literature. Curr. Breast Cancer Rep. 2022, 14, 180–191. [Google Scholar] [CrossRef]
- Zeng, J.; Han, G.; Yang, K. Assessment and sources of heavy metals in suspended particulate matter in a tropical catchment, northeast Thailand. J. Clean. Prod. 2020, 265, 121898. [Google Scholar] [CrossRef]
- Li, C.; Zhou, K.; Qin, W.; Tian, C.; Qi, M.; Yan, X.; Han, W. A review on heavy metals contamination in soil: Effects, sources, and remediation techniques. Soil Sediment Contam. Int. J. 2019, 28, 380–394. [Google Scholar] [CrossRef]
- Dorne, J.-L.; Kass, G.; Bordajandi, L.R.; Amzal, B.; Bertelsen, U.; Castoldi, A.F.; Heppner, C.; Eskola, M.; Fabiansson, S.; Ferrari, P. Human risk assessment of heavy metals: Principles and applications. Met. Ions Life Sci. 2011, 8, 27–60. [Google Scholar] [PubMed]
- Wen, X.; Li, T.; Xu, X. Cadmium exposure in US adults, research based on the National Health and Nutrition Examination Survey from 1988 to 2018. Environ. Sci. Pollut. Res. 2022, 29, 22293–22305. [Google Scholar] [CrossRef] [PubMed]
- Pirkle, J.L.; Brody, D.J.; Gunter, E.W.; Kramer, R.A.; Paschal, D.C.; Flegal, K.M.; Matte, T.D. The decline in blood lead levels in the United States: The National Health and Nutrition Examination Surveys (NHANES). JAMA 1994, 272, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Lanphear, B.P.; Rauch, S.; Auinger, P.; Allen, R.W.; Hornung, R.W. Low-level lead exposure and mortality in US adults: A population-based cohort study. Lancet Public Health 2018, 3, e177–e184. [Google Scholar] [CrossRef] [PubMed]
- Lustberg, M.; Silbergeld, E. Blood lead levels and mortality. Arch. Intern. Med. 2002, 162, 2443–2449. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Aro, A.; Payton, M.; Korrick, S.; Sparrow, D.; Weiss, S.T.; Rotnitzky, A. The relationship of bone and blood lead to hypertension: The Normative Aging Study. JAMA 1996, 275, 1171–1176. [Google Scholar] [CrossRef]
- Nash, D.; Magder, L.; Lustberg, M.; Sherwin, R.W.; Rubin, R.J.; Kaufmann, R.B.; Silbergeld, E.K. Blood lead, blood pressure, and hypertension in perimenopausal and postmenopausal women. JAMA 2003, 289, 1523–1532. [Google Scholar] [CrossRef]
- Vaziri, N.D. Mechanisms of lead-induced hypertension and cardiovascular disease. Am. J. Physiol.-Heart Circ. Physiol. 2008, 295, H454–H465. [Google Scholar] [CrossRef]
- Peters, J.L.; Perlstein, T.S.; Perry, M.J.; McNeely, E.; Weuve, J. Cadmium exposure in association with history of stroke and heart failure. Environ. Res. 2010, 110, 199–206. [Google Scholar] [CrossRef]
- Everett, C.J.; Frithsen, I.L. Association of urinary cadmium and myocardial infarction. Environ. Res. 2008, 106, 284–286. [Google Scholar] [CrossRef] [PubMed]
- Navas-Acien, A.; Silbergeld, E.K.; Sharrett, A.R.; Calderon-Aranda, E.; Selvin, E.; Guallar, E. Metals in urine and peripheral arterial disease. Environ. Health Perspect. 2005, 113, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Obeng-Gyasi, E. Chronic cadmium exposure and cardiovascular disease in adults. J. Environ. Sci. Health Part A 2020, 55, 726–729. [Google Scholar] [CrossRef] [PubMed]
- Houston, M.C. Role of mercury toxicity in hypertension, cardiovascular disease, and stroke. J. Clin. Hypertens. 2011, 13, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Magos, L. Physiology and toxicology of mercury. Met. Ions Biol. Syst. 1997, 34, 321–370. [Google Scholar] [PubMed]
- Wiggers, G.A.; Peçanha, F.M.; Briones, A.M.; Perez-Giron, J.V.; Miguel, M.; Vassallo, D.V.; Cachofeiro, V.; Alonso, M.J.; Salaices, M. Low mercury concentrations cause oxidative stress and endothelial dysfunction in conductance and resistance arteries. Am. J. Physiol. Circ. Physiol. 2008, 295, H1033–H1043. [Google Scholar] [CrossRef]
- Kobal, A.B.; Horvat, M.; Prezelj, M.; Briški, A.S.; Krsnik, M.; Dizdarevič, T.; Mazej, D.; Falnoga, I.; Stibilj, V.; Arnerič, N.; et al. The impact of long-term past exposure to elemental mercury on antioxidative capacity and lipid peroxidation in mercury miners. J. Trace Elements Med. Biol. 2004, 17, 261–274. [Google Scholar] [CrossRef]
- Wierzbicki, R.; Prażanowski, M.; Michalska, M.; Krajewska, U.; Mielicki, W.P. Disorders in blood coagulation in humans occupationally exposed to mercuric vapors. J. Trace Elements Exp. Med. 2002, 15, 21–29. [Google Scholar] [CrossRef]
- Kishimoto, T.; Oguri, T.; Abe, M.; Kajitani, H.; Tada, M. Inhibitory effect of methylmercury on migration and tube formation by cultured human vascular endothelial cells. Arch. Toxicol. 1995, 69, 357–361. [Google Scholar] [CrossRef]
- Eom, S.-Y.; Choi, S.-H.; Ahn, S.-J.; Kim, D.-K.; Kim, D.-W.; Lim, J.-A.; Choi, B.-S.; Shin, H.-J.; Yun, S.-W.; Yoon, H.-J.; et al. Reference levels of blood mercury and association with metabolic syndrome in Korean adults. Int. Arch. Occup. Environ. Health 2014, 87, 501–513. [Google Scholar] [CrossRef]
- Lind, P.M.; Lind, L. Are persistent organic pollutants linked to lipid abnormalities, atherosclerosis and cardiovascular disease? A review. J. Lipid Atheroscler. 2020, 9, 334. [Google Scholar] [CrossRef] [PubMed]
- Meneguzzi, A.; Fava, C.; Castelli, M.; Minuz, P. Exposure to perfluoroalkyl chemicals and cardiovascular disease: Experimental and epidemiological evidence. Front. Endocrinol. 2021, 12, 850. [Google Scholar] [CrossRef] [PubMed]
- de Hollander, A.E.; Melse, J.M.; Lebret, E.; Kramers, P.G.J.E. An aggregate public health indicator to represent the impact of multiple environmental exposures. Epidemiology 1999, 10, 606–617. [Google Scholar] [CrossRef] [PubMed]
- Centers-For-Disease-Control-and-Prevention. Laboratory Procedure Manual. Available online: https://wwwn.cdc.gov/nchs/data/nhanes/2015-2016/labmethods/PFAS_I_MET.pdf (accessed on 30 November 2023).
- Babekir, A.; Mostafa, S.; Obeng-Gyasi, E. The Association of Toxoplasma gondii IgG and Cardiovascular Biomarkers. Int. J. Environ. Res. Public Health 2021, 18, 4908. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.W.; D’Agostino, R.B.; Levy, D.; Belanger, A.M.; Silbershatz, H.; Kannel, W.B. Prediction of coronary heart disease using risk factor categories. Circulation 1998, 97, 1837–1847. [Google Scholar] [CrossRef] [PubMed]
- Bobb, J.F.; Valeri, L.; Claus Henn, B.; Christiani, D.C.; Wright, R.O.; Mazumdar, M.; Godleski, J.J.; Coull, B.A. Bayesian kernel machine regression for estimating the health effects of multi-pollutant mixtures. Biostatistics 2015, 16, 493–508. [Google Scholar] [CrossRef]
- Bobb, J.F.; Claus Henn, B.; Valeri, L.; Coull, B.A. Statistical software for analyzing the health effects of multiple concurrent exposures via Bayesian kernel machine regression. Environ. Health 2018, 17, 67. [Google Scholar] [CrossRef]
- Bobb, J.F. Example Using the Bkmr R Package with Simulated Data from the NIEHS Mixtures Workshop. Available online: https://jenfb.github.io/bkmr/SimData1 (accessed on 30 November 2023).
- Lakatta, E.G. Age-associated cardiovascular changes in health: Impact on cardiovascular disease in older persons. Heart Fail. Rev. 2002, 7, 29–49. [Google Scholar] [CrossRef]
- Sniderman, A.D.; Furberg, C.D. Age as a modifiable risk factor for cardiovascular disease. Lancet 2008, 371, 1547–1549. [Google Scholar] [CrossRef]
- Butter, M.E. Are women more vulnerable to environmental pollution? J. Hum. Ecol. 2006, 20, 221–226. [Google Scholar] [CrossRef]
- Byrne, C.; Divekar, S.D.; Storchan, G.B.; Parodi, D.A.; Martin, M.B. Cadmium—A metallohormone? Toxicol. Appl. Pharmacol. 2009, 238, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Obeng-Gyasi, E.; Armijos, R.X.; Weigel, M.M.; Filippelli, G.M.; Sayegh, M.A. Cardiovascular-related outcomes in US adults exposed to lead. Int. J. Environ. Res. Public Health 2018, 15, 759. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.; Jiao, J.; Zhuang, P.; Chen, X.; Wang, J.; Zhang, Y. Serum polyfluoroalkyl chemicals are associated with risk of cardiovascular diseases in national US population. Environ. Int. 2018, 119, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Victor, V.M.; Rocha, M.; Sola, E.; Banuls, C.; Garcia-Malpartida, K.; Hernandez-Mijares, A. Oxidative stress, endothelial dysfunction and atherosclerosis. Curr. Pharm. Des. 2009, 15, 2988–3002. [Google Scholar] [CrossRef] [PubMed]
- Lahera, V.; Goicoechea, M.; Garcia de Vinuesa, S.; Miana, M.; Heras, N.d.l.; Cachofeiro, V.; Luno, J. Endothelial dysfunction, oxidative stress and inflammation in atherosclerosis: Beneficial effects of statins. Curr. Med. Chem. 2007, 14, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Qu, Y.; Lv, Y.; Ji, S.; Ding, L.; Zhao, F.; Zhu, Y.; Zhang, W.; Hu, X.; Lu, Y.; Li, Y. Effect of exposures to mixtures of lead and various metals on hypertension, pre-hypertension, and blood pressure: A cross-sectional study from the China National Human Biomonitoring. Environ. Pollut. 2022, 299, 118864. [Google Scholar] [CrossRef]



| Cardiovascular Biomarker | Biomarker Value Assigned Index Value (1) | Biomarker Value Assigned Index Value (0) |
|---|---|---|
| Diastolic blood pressure (DBP) | ≤80 | >80 |
| Systolic blood pressure (SBP) | ≤120 | >120 |
| High-density lipoprotein (HDL) | ≥50 mg/dL | <50 mg/dL |
| Triglycerides (TG) | ≤199 mg/dL | >199 mg/dL |
| C-reactive protein (CRP) | ≤1 mg/dL | >1 mg/dL |
| Gamma glutamyl transferase (GGT) | ≤40 U/L | >40 U/L |
| Total cholesterol (TC) | <200 mg/dL | >200 mg/dL |
| Glucose (FG) | <100 mg/dL | >100 mg/dL |
| Overall biomarker index | Sum of eight biomarker indicator values | |
| Characteristics | |
|---|---|
| N | 6237 |
| Age: mean (SD) | 43.0 (5.23) |
| Gender | |
| Female | 51.3% |
| Male | 48.7% |
| Education | |
| Less than high school | 18.10% |
| High school or equivalent | 21.35% |
| Some college/associate degree | 30.41% |
| Bachelor’s degree or higher | 30.13% |
| Race/ethnicity | |
| Black | 10.84% |
| White | 67.75% |
| Hispanic | 14.16% |
| Other | 7.25% |
| Household Income | |
| <25,000 | 31.72% |
| 25,000–55,000 | 42.53% |
| 55,000–75,000 | 19.72% |
| 75,000+ | 6.02% |
| Marital Status | |
| Married or Living with a partner | 62.8% |
| Single | 37.2% |
| Overall | Male | Female | p Value | |
|---|---|---|---|---|
| N | 6237 | 3100 | 3137 | |
| PFOA | 3.69 (1.32) | 4.15 (3.20) | 3.26 (2.38) | <0.0001 |
| PFOS | 12.84 (22.40) | 15.35 (15.11) | 10.46 (10.28) | <0.0001 |
| PFNA | 1.39 (0.48) | 1.48 (1.50) | 1.30 (1.20) | 0.0000 |
| PFHxS | 2.5 (1.68) | 3.13 (3.98) | 1.92 (2.48) | <0.0001 |
| Mercury | 1.51 (1.79) | 1.65 (1.99) | 1.38 (3.08) | 0.0067 |
| Lead | 1.47 (0.59) | 1.72 (1.91) | 1.23 (1.70) | <0.0001 |
| Cadmium | 0.48 (0.03) | 0.45 (0.57) | 0.51 (0.61) | 0.0012 |
| Systolic Blood Pressure | 121.62 (17.69) | 121.65 (15.10) | 118.13 (18.03) | <0.0001 |
| Diastolic Blood Pressure | 69.05 (12.90) | 70.24 (13.14) | 68.00 (12.33) | <0.0001 |
| Total Cholesterol | 197.90 (42.80) | 187.98 (42.41) | 195.48 (41.90) | <0.0001 |
| Triglycerides | 132.08 (69.00) | 140.99 (131.08) | 115.49 (90.20) | 0.0002 |
| LDL cholesterol | 118.8 (37.50) | 113.17 (37.53) | 115.17 (35.42) | 0.2988 |
| HDL Cholesterol | 52.63 (15.58) | 47.39 (13.22) | 57.23 (16.26) | <0.0001 |
| OCBI | 5.7 (1.40) | 4.71 (1.67) | 5.11 (1.65) | <0.0001 |
| Framingham Risk Score | 9.24 (6.32) | 8.08 (6.15) | 10.34 (6.36) | <0.0001 |
| (A) | ||||||||
| Stratum | Systolic Blood Pressure | Diastolic Blood Pressure | LDL Cholesterol | Total Cholesterol | ||||
| Term | Coefficient Estimates (95% CI) | p-Value | Coefficient Estimates (95% CI) | p-Value | Coefficient Estimates (95% CI) | p-Value | Coefficient Estimates (95% CI) | p-Value |
| N | 3513 | 3523 | 1747 | 3648 | ||||
| Intercept | 95.63 (3.99, 5.00) | <0.0001 | 54.57 (49.9, 59.23) | <0.0001 | 62.84 (49.9, 75.74) | <0.0001 | 139.48 (127.03, 151.73) | <0.0001 |
| PFOS | – | – | – | – | – | – | – | – |
| PFNA | – | – | – | – | – | – | – | – |
| PFOA | – | – | – | – | – | – | – | – |
| PFHxS | −4.46 (−8.56, −0.37) | 0.0338 | – | – | – | – | – | – |
| Mercury | – | – | – | – | 11.57 (5.31, 17.83) | 0.0007 | 4.36 (4.74, 13.07) | 0.0001 |
| Cadmium | 8.72 (2.22, 15.21) | 0.0106 | 10.67 (3.56, 17.80) | 0.0047 | – | – | – | – |
| Lead | – | – | 2.62 (0.24, 5.00) | 0.0321 | 10.53 (3.83, 17.83) | 0.0031 | 8.49 (4.37, 12.61) | 0.0002 |
| Age | 0.32 (0.28, 0.36) | <0.0001 | 0.08 (0.52, 0.11) | <0.0001 | 0.29 (0.14, 0.46) | 0.0006 | 0.42 (0.31, 0.54) | <0.0001 |
| BMI | 0.30 (0.24,−0.37) | <0.0001 | 0.26 (0.20, 0.31) | <0.0001 | 0.61 (0.33, 0.90) | 0.0001 | 0.49 (0.25, 0.73) | 0.0002 |
| Gender Male | 4.31 (3.16, 5.46) | <0.0001 | 3.37 (1.04, 3.69) | 0.0010 | – | – | −9.65 (−13.12, −6.19) | <0.0001 |
| PFOS:PFOA | – | – | – | – | – | – | – | – |
| PFOS:PFNA | – | – | – | – | – | – | – | – |
| PFOA:PFNA | – | – | – | – | – | – | – | – |
| PFOS:PFHxS | 0.38 (0.02, 0.75) | 0.0398 | ||||||
| PFOA:PFHxS | – | – | – | – | 3.19 (0.28, 6.10) | 0.032 | 1.72 (0.03, 3.41) | 0.045 |
| PFNA:PFHxS | – | – | – | – | – | – | – | – |
| Mercury:Cadmium | – | – | – | – | – | – | – | – |
| Mercury:Lead | – | – | – | – | – | – | −3.43 (−6.41, −0.44) | 0.026 |
| Cadmium:Lead | −6.16 (−11.37, −0.94) | 0.0225 | −7.60 (−12.04, −2.81) | 0.0030 | ||||
| PFOS:PFOA:PFNA | – | – | – | – | – | – | – | – |
| PFOS:PFOA:PFHxS | – | – | −0.05 (−0.10, −0.00) | 0.0465 | – | – | – | – |
| PFOS:PFNA:PFHxS | – | – | – | – | – | – | – | – |
| PFOA:PFNA:PFHxS | – | – | – | – | – | – | – | – |
| Mercury:Cadmium:Lead | – | – | – | – | – | – | – | – |
| PFOS:PFOA:PFNA:PFHxS | – | – | – | – | – | – | – | – |
| 0.27 | 0.00 | 0.15 | 0.13 | |||||
| (B) | ||||||||
| Stratum | HDL Cholesterol | Triglycerides | OCBI | |||||
| Term | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | ||
| N | 3648 | 1747 | 3651 | |||||
| Intercept | 63.79 (58.58, 68.99) | <0.0001 | 40.60 (17.06, 64.13) | 0.0013 | 7.25 (6.41, 7.91) | <0.0001 | ||
| PFOS | – | – | −4.17 (−6.78, −1.57) | 0.0026 | – | – | ||
| PFNA | – | – | – | – | – | – | ||
| PFOA | – | – | – | – | – | – | ||
| PFHxS | 3.7 (0.51, 6.93) | 0.0246 | – | – | – | – | ||
| Mercury | 2.36 (0.91, 3.81) | 0.0024 | – | – | – | – | ||
| Cadmium | – | – | 28.6 (5.92, 51.28) | 0.0150 | −1.12 (−1.78, −0.36) | 0.0032 | ||
| Lead | – | – | – | – | – | – | ||
| Age | 0.04 (0.02, 0.07)) | 0.0013 | 0.61 (0.39, 0.83) | <0.0001 | −0.01 (−0.02, −0.01) | <0.0001 | ||
| BMI | −0.58 (−0.65, −0.52) | <0.0001 | 1.74 (1.34, 2.14) | <0.0001 | −0.05 (−0.06, −0.05) | <0.0001 | ||
| Gender Male | −8.65 (−9.83, −7.47) | <0.0001 | – | – | −0.49 (−6.64, −0.32) | <0.0001 | ||
| PFOS:PFOA | – | – | 0.93 (0.31, 1.54) | 0.0044 | – | – | ||
| PFOS:PFNA | – | – | – | – | −0.18 (−0.42, 0.11) | 0.0482 | ||
| PFOA:PFNA | – | – | – | – | – | – | ||
| PFOS:PFHxS | – | – | 1.33 | 0.0149 | ||||
| PFOA:PFHxS | −1.52 (−2.72, −0.32) | 0.0149 | (0.28, 2.39) | – | – | – | ||
| PFNA:PFHxS | – | – | – | – | – | – | ||
| Mercury:Cadmium | – | – | – | – | 0.84 (0.07, 1.53) | 0.0250 | ||
| Mercury:Lead | – | – | – | – | – | – | ||
| Cadmium:Lead | – | – | ||||||
| PFOS:PFOA:PFNA | – | – | – | – | – | – | ||
| PFOS:PFOA:PFHxS | 0.10 (0.00, 0.19) | 0.0486 | −0.38 (−0.64, −0.12) | 0.0149 | – | – | ||
| PFOS:PFNA:PFHxS | – | – | – | – | – | – | ||
| PFOA:PFNA:PFHxS | – | – | – | – | – | – | ||
| Mercury:Cadmium: Lead | – | – | – | – | – | – | ||
| PFOS:PFOA:PFNA:PFHxS | – | – | – | – | – | – | ||
| 0.30 | 0.18 | 0.13 | ||||||
| Stratum | Male (N = 962) | Female (N = 741) | ||
|---|---|---|---|---|
| Term | Coefficient Estimates (95% CI) | p-Value | Coefficient Estimates (95% CI) | p-Value |
| Intercept | – | – | −3.61 (−6.99, −0.25) | 0.0362 |
| PFOS | – | – | – | – |
| PFNA | – | – | – | – |
| PFOA | −0.70 (−2.60, −0.80) | 0.0005 | – | – |
| PFHxS | – | – | – | – |
| Mercury | – | – | – | – |
| Cadmium | 3.02 (1.78, 4.25) | <0.0001 | 4.35 (2.40, 6.29) | <0.0001 |
| Lead | 1.56 (1.00, 2.12) | <0.0001 | 1.75 (1.00, 2.50) | <0.0001 |
| BMI | 0.25 (−0.65, −0.52) | <0.0001 | 0.21 (0.14, 0.27) | <0.0001 |
| PFOS:PFOA | 0.05 (0.01, 0.09) | 0.0112 | −0.07 (−0.13, −0.01) | 0.0295 |
| PFOS:PFNA | – | – | – | – |
| PFOA:PFNA | – | – | – | – |
| PFOS:PFHxS | – | – | – | – |
| PFOA:PFHxS | – | 0.0149 | 0.47 (0.02, 0.92) | 0.393 |
| PFNA:PFHxS | – | – | – | – |
| Mercury:Cadmium | – | – | – | – |
| Mercury:Lead | – | – | – | – |
| Cadmium:Lead | – | – | ||
| PFOS:PFOA:PFNA | – | – | 0.04 (0.00, 0.07) | 0.0689 |
| PFOS:PFOA:PFHxS | – | – | – | – |
| PFOS:PFNA:PFHxS | – | – | – | – |
| PFOA:PFNA:PFHxS | – | – | – | – |
| Mercury:Cadmium: Lead | – | – | – | – |
| PFOS:PFOA:PFNA:PFHxS | – | – | – | – |
| 0.15 | 0.20 | |||
| Adjusted for BMI | ||||
| BKMR Models Showing PIP for Exposure to PFAS and Metal and by Health Outcome | ||||||
|---|---|---|---|---|---|---|
| Systolic Blood Pressure | Diastolic Blood Pressure | LDL Cholesterol | Total Cholesterol | HDL Cholesterol | Triglycerides | |
| N | 3515 | 3515 | 1690 | 3515 | 3515 | 1690 |
| PFOS | 0.0000 | 0.9548 | 0.4340 | 0.5724 | 0.0220 | 0.3026 |
| PFOA | 0.0000 | 0.0000 | 0.0790 | 0.3984 | 0.0000 | 0.4552 |
| PFHxS | 0.0062 | 0.0000 | 0.0298 | 0.0000 | 0.1038 | 0.0264 |
| PFNA | 0.0046 | 0.0000 | 0.3986 | 0.0240 | 0.0068 | 0.0392 |
| Lead | 0.1840 | 0.0000 | 0.9960 | 1.000 | 0.0000 | 0.1668 |
| Mercury | 0.0014 | 0.1044 | 0.2444 | 0.9736 | 0.9722 | 0.0222 |
| Group | Group PIP | Cond PIP | |
|---|---|---|---|
| PFOS | 1 | 0.910 | 1.0000 |
| PFOA | 1 | 0.910 | 0.0000 |
| PFHxS | 1 | 0.910 | 0.0000 |
| PFNA | 1 | 0.910 | 0.0000 |
| Lead | 2 | 0.994 | 0.0805 |
| Mercury | 2 | 0.994 | 0.0000 |
| Cadmium | 2 | 0.994 | 0.9195 |
| Group | Group PIP | Cond PIP | |
|---|---|---|---|
| PFOS | 1 | 0.050 | 0.0400 |
| PFOA | 1 | 0.050 | 0.1200 |
| PFHxS | 1 | 0.050 | 0.1600 |
| PFNA | 1 | 0.050 | 0.6800 |
| Lead | 2 | 0.368 | 0.9945 |
| Mercury | 2 | 0.368 | 0.0000 |
| Cadmium | 2 | 0.368 | 0.0054 |
| Group | Group PIP | Cond PIP | |
|---|---|---|---|
| PFOS | 1 | 0.988 | 0.9089 |
| PFOA | 1 | 0.988 | 0.0162 |
| PFHxS | 1 | 0.988 | 0.0000 |
| PFNA | 1 | 0.988 | 0.0749 |
| Lead | 2 | 1.000 | 1.0000 |
| Mercury | 2 | 1.000 | 0.0000 |
| Cadmium | 2 | 1.000 | 0.0054 |
| Notes | |||
| Group | Group PIP | Cond PIP | |
|---|---|---|---|
| PFOS | 1 | 0.202 | 0.1782 |
| PFOA | 1 | 0.202 | 0.0000 |
| PFHxS | 1 | 0.202 | 0.8218 |
| PFNA | 1 | 0.202 | 0.0000 |
| Lead | 2 | 1.000 | 0.0000 |
| Mercury | 2 | 1.000 | 1.0000 |
| Cadmium | 2 | 1.000 | 0.0000 |
| Notes | |||
| Group | Group PIP | Cond PIP | |
|---|---|---|---|
| PFOS | 1 | 0.962 | 0.0000 |
| PFOA | 1 | 0.962 | 0.0187 |
| PFHxS | 1 | 0.962 | 0.0000 |
| PFNA | 1 | 0.962 | 0.9812 |
| Lead | 2 | 1.000 | 1.0000 |
| Mercury | 2 | 1.000 | 0.0000 |
| Cadmium | 2 | 1.000 | 0.0000 |
| Notes | |||
| Hierarchical BKMR Results for Triglycerides | |||
|---|---|---|---|
| Group | Group PIP | Cond PIP | |
| PFOS | 1 | 0.410 | 0.0000 |
| PFOA | 1 | 0.410 | 0.6390 |
| PFHxS | 1 | 0.410 | 0.0829 |
| PFNA | 1 | 0.410 | 0.2780 |
| Lead | 2 | 0.694 | 0.2478 |
| Mercury | 2 | 0.694 | 0.2075 |
| Cadmium | 2 | 0.694 | 0.5447 |
| Notes | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boafo, Y.S.; Mostafa, S.; Obeng-Gyasi, E. Association of Combined Metals and PFAS with Cardiovascular Disease Risk. Toxics 2023, 11, 979. https://doi.org/10.3390/toxics11120979
Boafo YS, Mostafa S, Obeng-Gyasi E. Association of Combined Metals and PFAS with Cardiovascular Disease Risk. Toxics. 2023; 11(12):979. https://doi.org/10.3390/toxics11120979
Chicago/Turabian StyleBoafo, Yvonne S., Sayed Mostafa, and Emmanuel Obeng-Gyasi. 2023. "Association of Combined Metals and PFAS with Cardiovascular Disease Risk" Toxics 11, no. 12: 979. https://doi.org/10.3390/toxics11120979






