How Nanotechnology and Biomedical Engineering Are Supporting the Identification of Predictive Biomarkers in Neuro-Oncology
Abstract
:1. Introduction
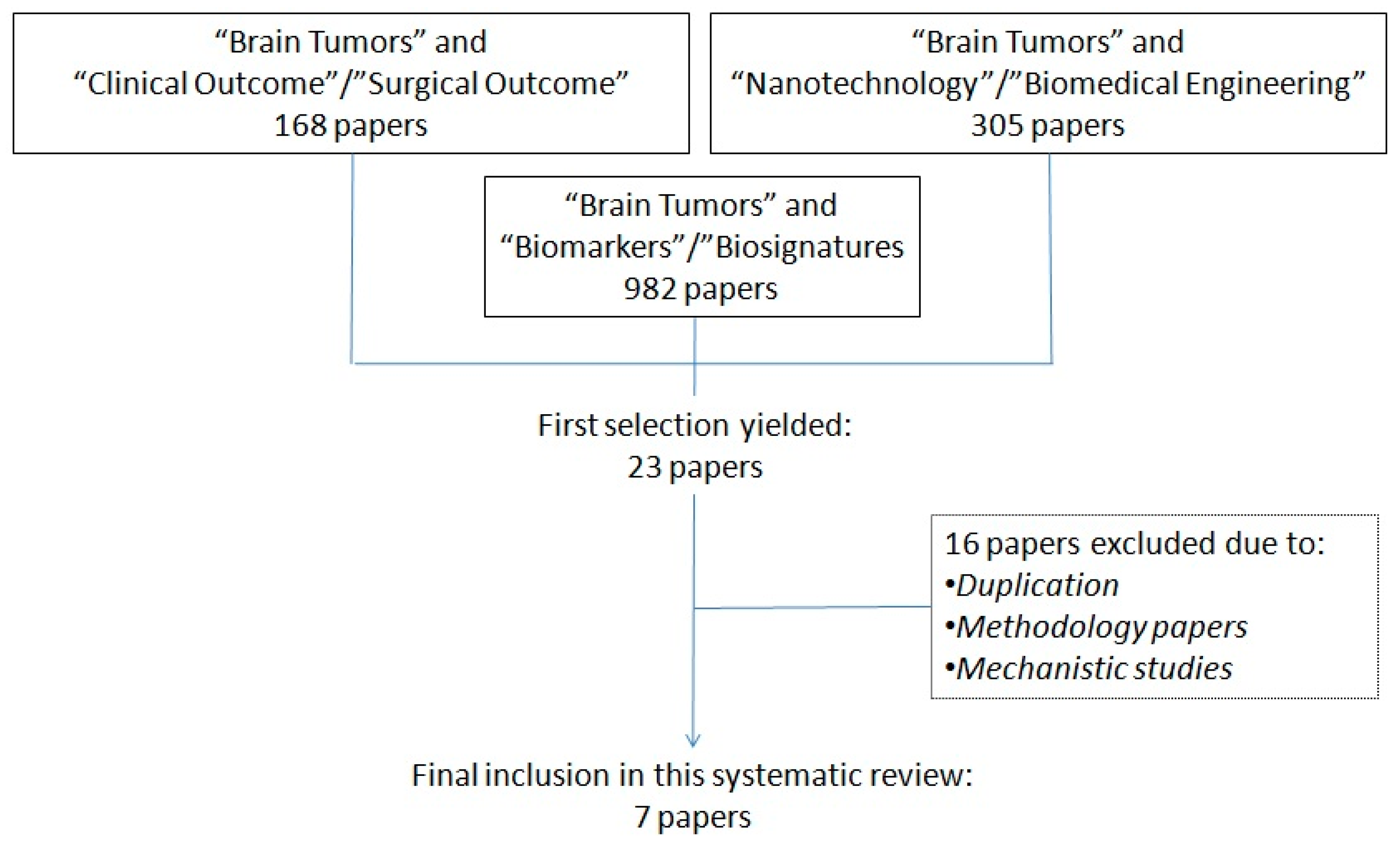
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Prentice, R.L. Surrogate and mediating endpoints: Current status and future directions. J. Natl. Cancer Inst. 2009, 101, 216–217. [Google Scholar] [CrossRef] [PubMed]
- Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: Preferred definitions and conceptual framework. Clin. Pharmacol. Ther. 2001, 69, 89–95. [Google Scholar]
- FDA-NIH Biomarker Working Group. BEST (Biomarkers, EndpointS, and Other Tools) Resource; Food and Drug Administration: Silver Spring, MD, USA, 2016.
- Chau, C.H.; Rixe, O.; McLeod, H.; Figg, W.D. Validation of analytic methods for biomarkers used in drug development. Clin. Cancer Res. 2008, 14, 5967–5976. [Google Scholar] [CrossRef] [PubMed]
- Yates, L.R.; Seoane, J.; Le Tourneau, C.; Siu, L.L.; Marais, R.; Michiels, S.; Soria, J.C.; Campbell, P.; Normanno, N.; Scarpa, A.; et al. The European Society for Medical Oncology (ESMO) Precision Medicine Glossary. Ann. Oncol. 2018, 29, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Margolin-Miller, Y.; Yanichkin, N.; Shichrur, K.; Toledano, H.; Ohali, A.; Tzaridis, T.; Michowitz, S.; Fichman-Horn, S.; Feinmesser, M.; Pfister, S.M.; et al. Prognostic relevance of miR-124-3p and its target TP53INP1 in pediatric ependymoma. Genes Chromosom. Cancer 2017, 56, 639–650. [Google Scholar] [CrossRef] [PubMed]
- Schliesser, M.G.; Claus, R.; Hielscher, T.; Grimm, C.; Weichenhan, D.; Blaes, J.; Wiestler, B.; Hau, P.; Schramm, J.; Sahm, F.; et al. Prognostic relevance of miRNA-155 methylation in anaplastic glioma. Oncotarget 2016, 7, 82028–82045. [Google Scholar] [CrossRef] [PubMed]
- Tang, H.; Liu, Q.; Liu, X.; Ye, F.; Xie, X.; Xie, X.; Wu, M. Plasma miR-185 as a predictive biomarker for prognosis of malignant glioma. J. Cancer Res. Ther. 2015, 11, 630–634. [Google Scholar] [PubMed]
- Steponaitis, G.; Skiriutė, D.; Kazlauskas, A.; Golubickaitė, I.; Stakaitis, R.; Tamašauskas, A.; Vaitkienė, P. High CHI3L1 expression is associated with glioma patient survival. Diagn. Pathol. 2016, 11, 42. [Google Scholar] [CrossRef] [PubMed]
- Vaitkienė, P.; Skiriutė, D.; Steponaitis, G.; Skauminas, K.; Tamašauskas, A.; Kazlauskas, A. High level of Sema3C is associated with glioma malignancy. Diagn. Pathol. 2015, 10, 58. [Google Scholar] [CrossRef] [PubMed]
- Freitag, D.; McLean, A.L.; Simon, M.; Koch, A.; Grube, S.; Walter, J.; Kalff, R.; Ewald, C. NANOG overexpression and its correlation with stem cell and differentiation markers in meningiomas of different WHO grades. Mol. Carcinog. 2017, 56, 1953–1964. [Google Scholar] [CrossRef] [PubMed]
- Kickingereder, P.; Sahm, F.; Radbruch, A.; Wick, W.; Heiland, S.; Deimling, A.; Bendszus, M.; Wiestler, B. IDH mutation status is associated with a distinct hypoxia/angiogenesis transcriptome signature which is non-invasively predictable with rCBV imaging in human glioma. Sci. Rep. 2015, 5, 16238. [Google Scholar] [CrossRef] [PubMed]
- Weller, M.; Tabatabai, G.; Kästner, B.; Felsberg, J.; Steinbach, J.P.; Wick, A.; Schnell, O.; Hau, P.; Herrlinger, U.; Sabel, M.C.; et al. MGMT Promoter Methylation Is a Strong Prognostic Biomarker for Benefit from Dose-Intensified Temozolomide Rechallenge in Progressive Glioblastoma: The Director Trial. Clin. Cancer Res. 2015, 21, 2057–2064. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.N.; Ullah, N.; Hussein, D.; Saini, K.S. Current and emerging biomarkers in tumors of the central nervous system: Possible diagnostic, prognostic and therapeutic applications. Semin. Cancer Biol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Tabatabai, G.; Weller, M. Glioblastoma stem cells. Cell Tissue Res. 2011, 343, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Nikiforova, M.N.; Hamilton, R.L. Molecular diagnostics of gliomas. Arch. Pathol. Lab. Med. 2011, 135, 558–568. [Google Scholar] [PubMed]
- Weiler, M.; Wick, W. Molecular predictors of outcome in low-grade glioma. Curr. Opin. Neurol. 2012, 25, 767–773. [Google Scholar] [CrossRef] [PubMed]
- Ilhan-Mutlu, A.; Wagner, L.; Preusser, M. Circulating biomarkers of CNS tumors: An update. Biomark. Med. 2013, 7, 267–285. [Google Scholar] [CrossRef] [PubMed]
- Weller, M.; Nabors, L.B.; Gorlia, T.; Leske, H.; Rushing, E.; Bady, P.; Hicking, C.; Perry, J.; Hong, Y.K.; Roth, P.; et al. Cilengitide in newly diagnosed glioblastoma: Biomarker expression and outcome. Oncotarget 2016, 7, 15018–15032. [Google Scholar] [CrossRef] [PubMed]
- Ebrahimi, A.; Skardelly, M.; Bonzheim, I.; Ott, I.; Mühleisen, H.; Eckert, F.; Tabatabai, G.; Schittenhelm, J. ATRX immunostaining predicts IDH and H3F3A status in gliomas. Acta Neuropathol. Commun. 2016, 4, 60. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.W.; Pajtler, K.W.; Worst, B.C.; Pfister, S.M.; Wechsler-Reya, R.J. Molecular mechanisms and therapeutic targets in pediatric brain tumors. Sci. Signal. 2017, 10, 470. [Google Scholar] [CrossRef] [PubMed]
- Capper, D.; von Deimling, A.; Brandes, A.A.; Carpentier, A.F.; Kesari, S.; Sepulveda-Sanchez, J.M.; Wheeler, H.R.; Chinot, O.; Cher, L.; Steinbach, J.P.; et al. Biomarker and Histopathology Evaluation of Patients with Recurrent Glioblastoma Treated with Galunisertib, Lomustine, or the Combination of Galunisertib and Lomustine. Int. J. Mol. Sci. 2017, 18, 995. [Google Scholar] [CrossRef] [PubMed]
- Kaidar-Person, O.; Meattini, I.; Jain, P.; Bult, P.; Simone, N.; Kindts, I.; Steffens, R.; Weltens, C.; Navarria, P.; Belkacemi, Y.; et al. Discrepancies between biomarkers of primary breast cancer and subsequent brain metastases: An international multicenter study. Breast Cancer Res. Treat. 2017, 167, 479–483. [Google Scholar] [CrossRef] [PubMed]
- Cagney, D.N.; Sul, J.; Huang, R.Y.; Ligon, K.L.; Wen, P.Y.; Alexander, B.M. The FDA NIH Biomarkers, EndpointS, and other Tools (BEST) Resource in Neuro-Oncology. Neuro Oncol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Krutzik, P.O.; Irish, J.M.; Nolan, G.P.; Perez, O.D. Analysis of protein phosphorylation and cellular signaling events by flow cytometry: Techniques and clinical applications. Clin. Immunol. 2004, 110, 206–221. [Google Scholar] [CrossRef] [PubMed]
- Ganau, L.; Ligarotti, G.K.I.; Ganau, M. Predicting complexity of tumor removal and postoperative outcome in patients with high-grade gliomas. Neurosurg. Rev. 2018, 41, 371–373. [Google Scholar] [CrossRef] [PubMed]
- Talacchi, A.; Turazzi, S.; Locatelli, F.; Sala, F.; Beltramello, A.; Alessandrini, F.; Manganotti, P.; Lanteri, P.; Gambin, R.; Ganau, M.; et al. Surgical treatment of high-grade gliomas in motor areas. The impact of different supportive technologies: A 171-patient series. J. Neurooncol. 2010, 100, 417–426. [Google Scholar] [CrossRef] [PubMed]
- Ganau, M.; Bosco, A.; Palma, A.; Corvaglia, S.; Parisse, P.; Fruk, L.; Beltrami, A.P.; Cesselli, D.; Casalis, L.; Scoles, G. A DNA-based nano-immunoassay for the label-free detection of glial fibrillary acidic protein in multicell lysates. Nanomedicine 2015, 11, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Ganau, L.; Paris, M.; Ligarotti, G.K.; Ganau, M. Management of Gliomas: Overview of the Latest Technological Advancements and Related Behavioral Drawbacks. Behav. Neurol. 2015, 2015, 862634. [Google Scholar] [CrossRef] [PubMed]
- Ben-Porath, I.; Thomson, M.W.; Carey, V.J.; Ge, R.; Bell, G.W.; Regev, A.; Weinberg, R.A. An embryonic stem cell-like gene expression signature in poorly differentiated aggressive human tumors. Nat. Genet. 2008, 40, 499–507. [Google Scholar] [CrossRef] [PubMed]
- Niu, C.S.; Li, D.X.; Liu, Y.H.; Fu, X.M.; Tang, S.F.; Li, J. Expression of NANOG in human gliomas and its relationship with undifferentiated glioma cells. Oncol. Rep. 2011, 26, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Soni, P.; Qayoom, S.; Husain, N.; Kumar, P.; Chandra, A.; Ojha, B.K.; Gupta, R.K. CD24 and Nanog expression in Stem Cells in Glioblastoma: Correlation with Response to Chemoradiation and Overall Survival. Asian Pac. J. Cancer Prev. 2017, 18, 2215–2219. [Google Scholar] [PubMed]
- Sun, W.; Julie Li, Y.S.; Huang, H.D.; Shyy, J.Y.; Chien, S. microRNA: A master regulator of cellular processes for bioengineering systems. Annu. Rev. Biomed. Eng. 2010, 12, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Ganau, M.; Syrmos, N.; Paris, M.; Ganau, L.; Ligarotti, G.K.I.; Moghaddamjou, A.; Chibbaro, S.; Soddu, A.; Prisco, L. Current and Future Applications of Biomedical Engineering for Proteomic Profiling: Predictive Biomarkers in Neuro-Traumatology. Medicines 2018, 5, 19. [Google Scholar] [CrossRef] [PubMed]
- Tetreault, L.; Palubiski, L.M.; Kryshtalskyj, M.; Idler, R.K.; Martin, A.R.; Ganau, M.; Wilson, J.R.; Kotter, M.; Fehlings, M.G. Significant Predictors of Outcome Following Surgery for the Treatment of Degenerative Cervical Myelopathy: A Systematic Review of the Literature. Neurosurg. Clin. 2018, 29, 115–127. [Google Scholar] [CrossRef] [PubMed]
- Cho, W.C. Nasopharyngeal carcinoma: Molecular biomarker discovery and progress. Mol. Cancer 2007, 6, 1. [Google Scholar] [CrossRef] [PubMed]
- Cho, W.C. Potentially useful biomarkers for the diagnosis, treatment and prognosis of lung cancer. Biomed. Pharmacother. 2007, 61, 515–519. [Google Scholar] [PubMed]
- Ganau, M. Tackling gliomas with nanoformulated antineoplastic drugs: Suitability of hyaluronic acid nanoparticles. Clin. Transl. Oncol. 2014, 16, 220–223. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Zhang, F.; Wang, Y.; Sun, X.; Choi, K.Y.; Liu, D.; Choi, J.S.; Shin, T.H.; Cheon, J.; Niu, G.; et al. Design considerations of iron-based nanoclusters for noninvasive tracking of mesenchymal stem cell homing. ACS Nano 2014, 8, 4403–4414. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, J.; Varallyay, C.G.; Dosa, E.; Gahramanov, S.; Hamilton, B.; Rooney, W.D.; Muldoon, L.L.; Neuwelt, E.A. Superparamagnetic iron oxide nanoparticles: Diagnostic magnetic resonance imaging and potential therapeutic applications in neurooncology and central nervous system inflammatory pathologies, a review. J. Cereb. Blood Flow Metab. 2010, 30, 15–35. [Google Scholar] [CrossRef] [PubMed]
- Ganau, M.; Syrmos, N.C.; D’Arco, F.; Ganau, L.; Chibbaro, S.; Prisco, L.; Ligarotti, G.K.I.; Ambu, R.; Soddu, A. Enhancing contrast agents and radiotracers performance through hyaluronic acid-coating in neuroradiology and nuclear medicine. Hell. J. Nucl. Med. 2017, 20, 166–168. [Google Scholar] [PubMed]
- Huang, H.; Lovell, J.F. Advanced Functional Nanomaterials for Theranostics. Adv. Funct. Mater. 2017, 27, 1603524. [Google Scholar] [CrossRef] [PubMed]
- Ganau, L.; Prisco, L.; Ligarotti, G.K.I.; Ambu, R.; Ganau, M. Understanding the pathological basis of neurological diseases through diagnostic platforms based on innovations in biomedical engineering: New concepts and theranostics perspectives. Medicines 2018, 5, 22. [Google Scholar]
- Ganau, M.; Prisco, L.; Pescador, D.; Ganau, L. Challenging New Targets for CNS-HIV Infection. Front. Neurol. 2012, 3, 43. [Google Scholar] [CrossRef] [PubMed]
- Muthu, M.S.; Leong, D.T.; Mei, L.; Feng, S.S. Nanotheranostics—Application and further development of nanomedicine strategies for advanced theranostics. Theranostics 2014, 4, 660–677. [Google Scholar] [CrossRef] [PubMed]
- Ganau, M.; Holly, L.T.; Mizuno, J.; Fehlings, M.G. Future Directions and New Technologies for the Management of Degenerative Cervical Myelopathy. Neurosurg. Clin. 2018, 29, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Ganau, M.; Foroni, R.I.; Gerosa, M.; Zivelonghi, E.; Longhi, M.; Nicolato, A. Radiosurgical options in neuro-oncology: A review on current tenets and future opportunities. Part I: Therapeutic strategies. Tumori 2014, 100, 459–465. [Google Scholar] [PubMed]
- Ganau, M.; Foroni, R.I.; Gerosa, M.; Ricciardi, G.K.; Longhi, M.; Nicolato, A. Radiosurgical options in neuro-oncology: A review on current tenets and future opportunities. Part II: Adjuvant radiobiological tools. Tumori 2015, 101, 57–63. [Google Scholar] [CrossRef] [PubMed]
| Methodologies and References | Tumor Histology | Findings |
|---|---|---|
| MicroRNA | ||
| Margolin-Miller, Y.; et al., 2017 [7] | Pediatric Ependymoma (WHO Class II–III) | Following miR-array expression analysis, 9 miRNAs that correlated with relapse of disease were further validated by quantitative real-time PCR in a cohort of 67 patients. Eventually, miR-124-3p emerged as an independent prognostic factor of relapse. Negative levels of the miR-124-3p target (protein TP53INP1) also correlated with a poor outcome. |
| Schliesser, M.G.; et al., 2016 [8] | Anaplastic Glioma (WHO Class III) | Out of 12 putative miRNA promoter regions identified from unbiased DNA methylation screens, miR-155 promoter methylation and miR-155 expression were demonstrated to have the strongest negative correlation with patient survival. MiR-155 also conferred resistance towards alkylating temozolomide and radiotherapy as consequence of nuclear factor (NF)κB activation. |
| Tang, H.; et al., 2015 [9] | Glioma (WHO Class III–IV) Meningioma, Pituitary Adenoma and Acoustic Schwannoma (WHO Class I–II) | Plasma levels of miR-185 results significantly altered in glioma patients compared to normal controls; of note, low plasma levels seems to correlate with poor survival. Of note, miR-185 levels do not appear observably changed in patients with other brain tumors, such as meningioma, acoustic schwannoma, or pituitary adenoma. Furthermore, in Grade IV gliomas treated with surgical excision and chemo-radiotherapy, the plasma levels of miR-185 almost returned to normal levels. |
| Methodologies and References | Tumor Histology | Findings |
|---|---|---|
| mRNA | ||
| Steponaitis, G.; et al., 2016 [10] | Glioma (WHO Class I–IV) | CHI3L1 expression was assessed with quantitative real-time PCR in a cohort of 98 patients: mRNA expression of CHI3L1 was evidently higher in glioblastoma than in lower-grade glioma tissues. However, patients with high CHI3L1 expression had a shorter overall survival regardless of their histology (high-grade as well as lower-grade gliomas). |
| Vaitkienė, P.; et al., 2015 [11] | Glioma (WHO Class I–IV) | Protein and mRNA levels of semaphorin 3C (Sema3C), a protein involved in tumorigenesis and metastasis were studied in a cohort of 84 patients. Protein levels markedly increased in grade IV gliomas compared to grade I–III astrocytomas and were significantly associated with the shorter overall survival of patients. Sema3C mRNA levels showed no association with either grade of glioma or patient survival. |
| Methodologies and References | Tumor Histology | Findings |
|---|---|---|
| Multiplexing and Immunoassays | ||
| Freitag, D; et al., 2017 [12] | Meningioma (WHO Class I–III) | The overexpression of NANOG, a key regulator of pluripotency and malignant behavior, was studied by single-cell immunoassay in a cohort of 33 patients. While low-grade meningiomas expressed 1% NANOG+ cells, the rate rose to 2% in grade II/III meningiomas. Of note, NANOG+ cells also expressed other markers of pluripotency (i.e., SOX2 and OCT4), thus being demonstrated to act as “stem cell-like” cells with an impact on tumorigenesis and progression. |
| Methodologies and References | Tumor Histology | Findings |
|---|---|---|
| Biosignature—MicroRNA plus MRI features | ||
| Kickingereder, P.; et al., 2015 [13] | Glioma (WHO Class II–III) | A genotype/imaging phenotype correlation analysis with relative cerebral blood volume (rCBV) MRI, a robust and non-invasive estimate of tumor angiogenesis, showed in a cohort of 73 patients that a one-unit increase in rCBV corresponds to a two-thirds decrease in the odds of an IDH mutation and correctly predicts IDH mutation status in 88% of patients. Given the role of IDH gene in hypoxia-inducible-factor 1-alpha (HIF1A), a driving force in hypoxia-initiated angiogenesis, this study demonstrated that IDH mutation status, and the associated distinct angiogenesis transcriptome signature, can be non-invasively predicted with rCBV imaging. |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ganau, M.; Paris, M.; Syrmos, N.; Ganau, L.; Ligarotti, G.K.I.; Moghaddamjou, A.; Prisco, L.; Ambu, R.; Chibbaro, S. How Nanotechnology and Biomedical Engineering Are Supporting the Identification of Predictive Biomarkers in Neuro-Oncology. Medicines 2018, 5, 23. https://doi.org/10.3390/medicines5010023
Ganau M, Paris M, Syrmos N, Ganau L, Ligarotti GKI, Moghaddamjou A, Prisco L, Ambu R, Chibbaro S. How Nanotechnology and Biomedical Engineering Are Supporting the Identification of Predictive Biomarkers in Neuro-Oncology. Medicines. 2018; 5(1):23. https://doi.org/10.3390/medicines5010023
Chicago/Turabian StyleGanau, Mario, Marco Paris, Nikolaos Syrmos, Laura Ganau, Gianfranco K.I. Ligarotti, Ali Moghaddamjou, Lara Prisco, Rossano Ambu, and Salvatore Chibbaro. 2018. "How Nanotechnology and Biomedical Engineering Are Supporting the Identification of Predictive Biomarkers in Neuro-Oncology" Medicines 5, no. 1: 23. https://doi.org/10.3390/medicines5010023