Potential Influence of Aspirin on Neopterin and Tryptophan Levels in Patients with a Delirium
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Procedures
2.3. Biochemical Measurements
2.4. Statistical Analyses
3. Results
3.1. Participant Characteristics
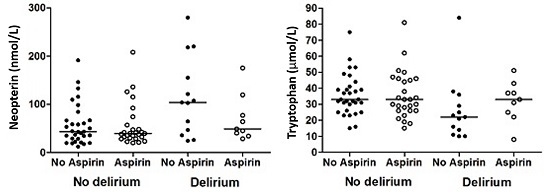
3.2. Analysis of Biochemical Parameters
4. Discussion
Limitations and Strengths
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Inouye, S.K.; Westendorp, R.G.; Saczynski, J.S. Delirium in elderly people. Lancet 2014, 383, 911–922. [Google Scholar] [CrossRef]
- Witlox, J.; Eurelings, L.S.; de Jonghe, J.F.; Kalisvaart, K.J.; Eikelenboom, P.; van Gool, W.A. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: A meta-analysis. JAMA 2010, 304, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Egberts, A.; Wijnbeld, E.H.; Fekkes, D.; van der Ploeg, M.A.; Ziere, G.; Hooijkaas, H.; van der Cammen, T.J.; Mattace-Raso, F.U. Neopterin: A potential biomarker for delirium in elderly patients. Dement. Geriatr. Cogn. Disord. 2015, 39, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Murr, C.; Widner, B.; Wirleitner, B.; Fuchs, D. Neopterin as a marker for immune system activation. Curr. Drug Metab. 2002, 3, 175–187. [Google Scholar] [CrossRef] [PubMed]
- Berdowska, A.; Zwirska-Korczala, K. Neopterin measurement in clinical diagnosis. J. Clin. Pharm. Ther. 2001, 26, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Egberts, A.; Fekkes, D.; Wijnbeld, E.H.A.; van der Ploeg, M.A.; van Saase, J.L.C.M.; Ziere, G.; van der Cammen, T.J.M.; Mattace-Raso, F.U.S. Disturbed serotonergic neurotransmission and oxidative stress in elderly patients with a delirium. Dement. Geriatr. Cogn. Disord. Extra 2015, 5, 450–458. [Google Scholar] [CrossRef] [PubMed]
- Schroecksnadel, K.; Winkler, C.; Wirleitner, B.; Schennach, H.; Fuchs, D. Aspirin down-regulates tryptophan degradation in stimulated human peripheral blood mononuclear cells in vitro. Clin. Exp. Immunol. 2005, 140, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Schuurmans, M.J.; Shortridge-Baggett, L.M.; Duursma, S.A. The delirium observation screening scale: A screening instrument for delirium. Res. Theory Nurs. Pract. 2003, 17, 31–50. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manuel of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- McDowell, I.; Newell, C. Measuring Health: A Guide to Rating Scales and Questionnaires; Oxford University Press: New York, NY, USA, 1996. [Google Scholar]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The barthel index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Dendukuri, N.; McCusker, J.; Belzile, E. The identification of seniors at risk screening tool: Further evidence of concurrent and predictive validity. J. Am. Geriatr. Soc. 2004, 52, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Laich, A.; Neurauter, G.; Wirleitner, B.; Fuchs, D. Degradation of serum neopterin during daylight exposure. Clin. Chim. Acta 2002, 322, 175–178. [Google Scholar] [CrossRef]
- Fekkes, D. Automated analysis of primary amino acids in plasma by high-performance liquid chromatography. Methods Mol. Biol. 2012, 828, 183–200. [Google Scholar] [PubMed]
- Van Gool, A.R.; Fekkes, D.; Kruit, W.H.; Mulder, P.G.; Ten Hagen, T.L.; Bannink, M.; Maes, M.; Eggermont, A.M. Serum amino acids, biopterin and neopterin during long-term immunotherapy with interferon-alpha in high-risk melanoma patients. Psychiatry Res. 2003, 119, 125–132. [Google Scholar] [CrossRef]
- Neurauter, G.; Wirleitner, B.; Laich, A.; Schennach, H.; Weiss, G.; Fuchs, D. Atorvastatin suppresses interferon-γ-induced neopterin formation and tryptophan degradation in human peripheral blood mononuclear cells and in monocytic cell lines. Clin. Exp. Immunol. 2003, 131, 264–267. [Google Scholar] [CrossRef] [PubMed]
- King, N.J.; Thomas, S.R. Molecules in focus: Indoleamine 2,3-dioxygenase. Int. J. Biochem. Cell Biol. 2007, 39, 2167–2172. [Google Scholar] [CrossRef] [PubMed]
- Weyand, C.M.; Kaiser, M.; Yang, H.; Younge, B.; Goronzy, J.J. Therapeutic effects of acetylsalicylic acid in giant cell arteritis. Arthritis Rheum. 2002, 46, 457–466. [Google Scholar] [CrossRef] [PubMed]
- Forrest, C.M.; Mackay, G.M.; Oxford, L.; Stoy, N.; Stone, T.W.; Darlington, L.G. Kynurenine pathway metabolism in patients with osteoporosis after 2 years of drug treatment. Clin. Exp. Pharmacol. Physiol. 2006, 33, 1078–1087. [Google Scholar] [CrossRef] [PubMed]
- Clegg, A.; Young, J.B. Which medications to avoid in people at risk of delirium: A systematic review. Age Ageing 2011, 40, 23–29. [Google Scholar] [CrossRef] [PubMed]

| Variable | No Delirium (n = 58) | Delirium (n = 22) | p-Value |
|---|---|---|---|
| Gender male | 28 (48.3) | 9 (40.9) | 0.555 * |
| Age in years | 80.4 ± 7.5 | 85.8 ± 4.1 | 0.002 ‡ |
| MMSE || | 25.0 (22.0–28.0) | 20.0 (17.3–24.3) | 0.000 † |
| Katz ADL score ¶ | 0.0 (0.0–3.0) | 3.5 (1.0–11.3) | 0.013 † |
| OARS-IADL score # | 5.0 (0.0–10.0) | 10.0 (3.0–14.0) | 0.037 † |
| Barthel Index ** | 18.0 (13.0–20.0) | 16.0 (9.0–19.0) | 0.050 † |
| ISAR score †† | 4.0 (2.5–6.0) | 6.0 (5.0–7.0) | 0.000 † |
| Charlson Comorbidity Index ‡‡ | 2.00 (1.00–3.00) | 2.00 (1.00–3.25) | 0.202 † |
| eGFR (mL/min) | 64.3 ± 25.3 | 48.0 ± 24.7 | 0.011 ‡ |
| Aspirin at admission | 27 (46.6) | 9 (40.9) | 0.651 * |
| Type of aspirin: | |||
| Acetylsalicylic acid | 12 (44.4) | 5 (55.6) | |
| Carbasalate calcium | 15 (55.6) | 4 (44.4) | |
| Beta-blockers | 17 (29.3) | 6 (27.3) | 0.857 * |
| Diuretics | 22 (37.9) | 7 (31.8) | 0.612 * |
| ACE inhibitors | 14 (24.1) | 6 (27.3) | 0.772 * |
| Angiotensin II receptor antagonists | 8 (13.8) | 2 (9.1) | 0.719 § |
| Calcium channel blockers | 13 (22.4) | 3 (13.6) | 0.536 § |
| Nitrates | 5 (8.6) | 1 (4.5) | 1.000 § |
| Statins | 27 (46.6) | 3 (13.6) | 0.007 * |
| Dipyridamole | 5 (8.6) | 0 (0.0) | 0.315 § |
| No Delirium | No Aspirin (n = 31) | Aspirin (n = 27) | p-Value |
|---|---|---|---|
| Model 1 | 45.8 (36.2–57.9) | 44.9 (34.9–57.8) | 0.908 |
| Model 2 | 47.0 (37.8–58.3) | 43.6 (34.5–55.0) | 0.645 |
| Delirium | No Aspirin (n = 13) | Aspirin (n = 9) | p-Value |
| Model 1 | 88.3 (57.7–135.2) | 59.3 (35.6–98.9) | 0.228 |
| Model 2 | 77.8 (52.4–115.6) | 71.1 (43.8–115.6) | 0.779 |
| No Delirium | No Aspirin (n = 31) | Aspirin (n = 27) | p-Value |
|---|---|---|---|
| Model 1 | 33.8 (29.6–38.6) | 33.1 (28.7–38.2) | 0.835 |
| Model 2 | 33.1 (29.2–37.6) | 33.9 (29.6–38.8) | 0.816 |
| Delirium | No Aspirin (n = 13) | Aspirin (n = 9) | p-Value |
| Model 1 | 21.6 (15.4–30.3) | 28.8 (19.2–43.2) | 0.269 |
| Model 2 | 22.4 (16.2–30.9) | 27.3 (18.4–40.5) | 0.439 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Egberts, A.; Fekkes, D.; Ziere, G.; Van der Cammen, T.J.M.; Mattace-Raso, F.U.S. Potential Influence of Aspirin on Neopterin and Tryptophan Levels in Patients with a Delirium. Geriatrics 2016, 1, 10. https://doi.org/10.3390/geriatrics1020010
Egberts A, Fekkes D, Ziere G, Van der Cammen TJM, Mattace-Raso FUS. Potential Influence of Aspirin on Neopterin and Tryptophan Levels in Patients with a Delirium. Geriatrics. 2016; 1(2):10. https://doi.org/10.3390/geriatrics1020010
Chicago/Turabian StyleEgberts, Angelique, Durk Fekkes, Gijsbertus Ziere, Tischa J. M. Van der Cammen, and Francesco U. S. Mattace-Raso. 2016. "Potential Influence of Aspirin on Neopterin and Tryptophan Levels in Patients with a Delirium" Geriatrics 1, no. 2: 10. https://doi.org/10.3390/geriatrics1020010