Motor Vehicle Collision Involvement among Persons with Hemianopia and Quadrantanopia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| CI | Confidence interval |
| CVA | Cerebrovascular accident |
| DSST | Digit symbol substitution test |
| MMSE | Mini-mental status examination |
| MVC | Motor vehicle collision |
| N | Number |
| NA | Not applicable |
| OU | Oculus uterque for both eyes |
| RR | Rate ratio |
| SD | Standard deviation |
| UAB | University of Alabama at Birmingham |
References
- Zhang, X.; Kedar, S.; Lynn, M.; Newman, N.; Biousse, V. Homonymous hemianopias clinical-anatomic correlations in 904 cases. Neurology 2006, 66, 906–910. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Kedar, S.; Lynn, M.J.; Newman, N.J.; Biousse, V. Homonymous hemianopia in stroke. J. Neuro-Ophthalmol. 2006, 26, 180–183. [Google Scholar] [CrossRef] [PubMed]
- Gilhotra, J.S.; Mitchell, P.; Healey, P.R.; Cumming, R.G.; Currie, J. Homonymous visual field defects and stroke in an older population. Stroke 2002, 33, 2417–2420. [Google Scholar] [CrossRef] [PubMed]
- Warren, M. Pilot study on activities of daily living limitations in adults with hemianopsia. Am. J. Occup. Ther. 2009, 63, 626–633. [Google Scholar] [CrossRef] [PubMed]
- Parker, W.T.; McGwin, G., Jr.; Wood, J.M.; Elgin, J.; Vaphiades, M.S.; Kline, L.B.; Owsley, C. Self-reported driving difficulty by persons with hemianopia and quadrantanopia. Curr. Eye Res. 2011, 36, 270–277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- International Council of Ophthalmology. Vision Requirements for Driving Safety: Appendices 1 and 2; International Council of Ophthalmology: San Paulo, Brazil, 2006. [Google Scholar]
- Owsley, C.; McGwin, G., Jr. Vision and driving. Vis. Res. 2010, 50, 2348–2361. [Google Scholar] [CrossRef] [PubMed]
- Racette, L.; Casson, E. The impact of visual field loss on driving performance: Evidence from on-road driving assessments. Optom. Vis. Sci. 2005, 82, 668–674. [Google Scholar] [CrossRef] [PubMed]
- Wood, J.M.; McGwin, G., Jr.; Elgin, J.; Vaphiades, M.S.; Braswell, R.A.; DeCarlo, D.K.; Kline, L.B.; Meek, G.C.; Searcey, K.; Owsley, C. On-road driving performance by persons with hemianopia and quadrantanopia. Investig. Ophthalmol. Vis. Sci. 2009, 50, 577–585. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elgin, J.; McGwin, G.; Wood, J.M.; Vaphiades, M.S.; Braswell, R.A.; DeCarlo, D.K.; Kline, L.B.; Owsley, C. Evaluation of on-road driving in people with hemianopia and quadrantanopia. Am. J. Occup. Ther. 2010, 64, 268–278. [Google Scholar] [CrossRef] [PubMed]
- Wood, J.M.; McGwin, G., Jr.; Elgin, J.; Vaphiades, M.S.; Braswell, R.A.; DeCarlo, D.K.; Kline, L.B.; Owsley, C. Hemianopic and quadrantanopic field loss, eye and head movements, and driving. Investig. Ophthalmol. Vis. Sci. 2011, 52, 1220–1225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kasneci, E.; Sippel, K.; Aehling, K.; Heister, M.; Rosenstiel, W.; Schiefer, U.; Papageorgiou, E. Driving with binocular visual field loss? A study on a supervised on-road parcours with simultaneous eye and head tracking. PLoS ONE 2014, 9, e87470. [Google Scholar] [CrossRef] [PubMed]
- Szlyk, J.P.; Brigell, M.; Seiple, W. Effects of age and hemianopic visual field loss on driving. Optom. Vis. Sci. 1993, 70, 1031–1037. [Google Scholar] [CrossRef] [PubMed]
- Bowers, A.R.; Mandel, A.J.; Goldstein, R.B.; Peli, E. Driving with hemianopia, i: Detection performance in a driving simulator. Investig. Ophthalmol. Vis. Sci. 2009, 50, 5137–5147. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, E.; Hardiess, G.; Mallot, H.A.; Schiefer, U. Gaze patterns predicting successful collision avoidance in patients with homonymous visual field defects. Vis. Res. 2012, 65, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Kübler, T.C.; Kasneci, E.; Rosenstiel, W.; Schiefer, U.; Nagel, K.; Papageorgiou, E. Stress-indicators and Exploratory gaze for the analysis of hazard perception in patients with visual field loss. Transp. Res. Part F: Traffic Psychol. Behav. 2014, 24, 231–243. [Google Scholar]
- Kübler, T.C.; Kasneci, E.; Rosenstiel, W.; Aehling, K.; Heister, M.; Nagel, K.; Schiefer, U.; Papageorgiou, E. Driving with homonymous visual field defects: Driving performance and compensatory gaze movements. J. Eye Mov. Res. 2015, 8. [Google Scholar] [CrossRef]
- Smith, M.; Mole, C.D.; Kountouriotis, G.K.; Chisholm, C.; Bhakta, B.; Wilkie, R.M. Driving with homonymous visual field loss: Does visual search performance predict hazard detection? Br. J. Occup. Ther. 2015, 78, 85–95. [Google Scholar] [CrossRef]
- Bowers, A.R.; Alberti, C.F.; Hwang, A.D.; Goldstein, R.; Peli, E. Pilot Study of Gaze Scanning and Intersection Detection Failures by Drivers with Hemianopia. In Proceedings of the 8th International Driving Symposium on Human Factors in Driver Assessment, Training, and Vehicle Design, Salt Lake City, UT, USA, 22–25 June 2015.
- Martin, T.; Riley, M.E.; Kelly, K.N.; Hayhoe, M.; Huxlin, K.R. Visually-guided behavior of homonymous hemianopes in a naturalistic task. Vis. Res. 2007, 47, 3434–3446. [Google Scholar] [CrossRef] [PubMed]
- Hardiess, G.; Papageorgiou, E.; Schiefer, U.; Mallot, H.A. Functional compensation of visual field deficits in hemianopic patients under the influence of different task demands. Vis. Res. 2010, 50, 1158–1172. [Google Scholar] [CrossRef] [PubMed]
- Halligan, P.W.; Cockburn, J.; Wilson, B.A. The behavioural assessment of visual neglect. Neuropsychol. Rehabil. 1991, 1, 5–32. [Google Scholar] [CrossRef]
- Owsley, C.; Ball, K.; McGwin, G., Jr.; Sloane, M.E.; Roenker, D.L.; White, M.F.; Overley, E.T. Visual processing impairment and risk of motor vehicle crash among older adults. JAMA 1998, 279, 1083–1088. [Google Scholar] [CrossRef] [PubMed]
- Owsley, C.; Stalvey, B.; Wells, J.; Sloane, M.E. Older drivers and cataract: Driving habits and crash risk. J. Gerontol. A Biol. Sci. Med. Sci. 1999, 54A, M203–M211. [Google Scholar] [CrossRef]
- Folstein, M.; Folstein, S.; McHugh, P. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Ferris, F.L.; Kassoff, A.; Bresnick, G.H.; Bailey, I. New visual acuity charts for clinical research. Am. J. Ophthalmol. 1982, 94, 91–96. [Google Scholar] [CrossRef]
- Pelli, D.; Robson, J.; Wilkins, A. The design of a new letter chart for measuring contrast sensitivity. Clin. Vis. Sci. 1988, 2, 187–199. [Google Scholar]
- Elliott, D.; Bullimore, M.; Bailey, I. Improving the reliability of the pelli-robson contrast sensitivity test. Clin. Vis. Sci. 1991, 6, 471–475. [Google Scholar]
- Reitan, R.M. The relationship of the trail making test to organic brain damage. J. Consult. Psychol. 1955, 19, 393–394. [Google Scholar] [CrossRef] [PubMed]
- Wechsler, D. Wechsler Adult Intelligence Scale-Revised; Psychological Corporation: San Antonio, TX, USA, 1981. [Google Scholar]
- Schulte, T.; Strasburger, H.; Müller-Oehring, E.M.; Kasten, E.; Sabel, B.A. Automobile driving performance of brain-injured patients with visual field defects. Am. J. Phys. Med. Rehabil. 1999, 78, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Bowers, A.R.; Mandel, A.J.; Goldstein, R.B.; Peli, E. Driving with hemianopia, ii: Lane position and steering in a driving simulator. Investig. Ophthalmol. Vis. Sci. 2010, 51, 6605–6613. [Google Scholar] [CrossRef] [PubMed]
- National Highway Traffic Safety Administration. Medical conditions and driver crash risk: Do license restrictions affect public safety? Ann. Emerg. Med. 2000, 36, 164–165. [Google Scholar]
- Ragland, D.R.; Satariano, W.A.; MacLeod, K.E. Driving cessation and increased depressive symptoms. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 399–403. [Google Scholar] [CrossRef] [PubMed]
- De Haan, G.A.; Melis-Dankers, B.J.; Brouwer, W.H.; Bredewoud, R.A.; Tucha, O.; Heutink, J. Car driving performance in hemianopia: An on-road driving studycar driving in hemianopia. Investig. Ophthalmol. Vis. Sci. 2014, 55, 6482–6489. [Google Scholar] [CrossRef] [PubMed]
- Bahnemann, M.; Hamel, J.; De Beukelaer, S.; Ohl, S.; Kehrer, S.; Audebert, H.; Kraft, A.; Brandt, S.A. Compensatory eye and head movements of patients with homonymous hemianopia in the naturalistic setting of a driving simulation. J. Neurol. 2015, 262, 316–325. [Google Scholar] [CrossRef] [PubMed]
| Participants with Field Loss N = 27 | Participants with Normal Fields N = 27 | |||
|---|---|---|---|---|
| Hemianopia N = 20 | Quadrantanopia N = 7 | Combined N = 27 | ||
| Age, years, mean (sd) | 50.5 (19.6) | 50.7 (18.5) | 50.5 (19.0) | 50.4 (18.3) |
| Gender, % | ||||
| Male | 60.0 | 71.4 * | 63.0* | 29.6 |
| Race, % | ||||
| African American | 10.0 | 0.0 | 7.4 | 14.8 |
| White, non-Hispanic | 85.0 | 100.0 | 89.9 | 85.2 |
| Other | 5.0 | 0.0 | 3.7 | 0.0 |
| # Chronic medical conditions, mean (sd) | 5.6 * (3.3) | 4.3 (1.3) | 5.2 * (2.9) | 2.1 (1.5) |
| # Current medications, mean (sd) | 5.2 * (4.1) | 4.6 (3.7) | 5.0 * (3.9) | 2.2 (2.1) |
| Visual acuity, OU, logMAR, mean (sd) | 0.07 * (0.30) | −0.02 (0.35) | 0.04 * (0.31) | −0.17 (0.22) |
| Contrast sensitivity, OU, log sensitivity, mean (sd) | 1.75 (0.17) | 1.81 (0.13) | 1.76 * (0.16) | 1.85 (0.10) |
| MMSE score, mean (sd) | 28.4 (1.6) | 28.7 (0.8) | 28.4 * (1.5) | 29.2 (1.2) |
| Estimated weekly mileage, mean (sd) | 177.4 (133.7) | 182.1 (111.3) | 178.6 * (126.2) | 296.7 (215.3) |
| Time since injury, years, mean (sd) | 8.0 (13.4) | 11.4 (20.5) | 9.0 (15.2) | NA |
| Participants with Field Loss N = 27 | Participants with Normal Fields N = 27 | |||
|---|---|---|---|---|
| Hemianopia N = 20 | Quadrantanopia N = 7 | Combined N = 27 | ||
| Motor vehicle collisions | ||||
| All | 15 | 4 | 19 | 21 |
| At-fault | 10 | 2 | 12 | 10 |
| Person-years | 134.6 | 45.8 | 180.4 | 238.4 |
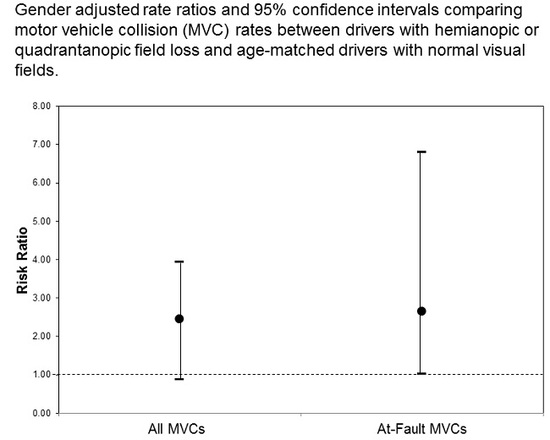
| All MVC RR (95% CI) | 1.61 (0.65-3.96) | 0.37 (0.08–1.70) | 1.10 (0.51–2.36) | --- |
| At-fault MVC RR (95% CI) | 3.13 (0.78–12.46) | 0.83 (0.04–17.72) | 2.50 (0.76–8.21) | --- |
| Person-miles | 1,098,917 | 419,296 | 1,518,213 | 3,678,181 |
| All MVC RR (95% CI) | 2.43 (1.05–5.62) | 0.87 (0.20–3.73) | 2.45 (0.89–3.95) | --- |
| At-fault MVC RR (95% CI) | 2.69 (1.00–7.30) | 2.31 (0.17–31.22) | 2.64 (1.03–6.80) | --- |
© 2016 by the author; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
McGwin Jr., G.; Wood, J.; Huisingh, C.; Owsley, C. Motor Vehicle Collision Involvement among Persons with Hemianopia and Quadrantanopia. Geriatrics 2016, 1, 19. https://doi.org/10.3390/geriatrics1030019
McGwin Jr. G, Wood J, Huisingh C, Owsley C. Motor Vehicle Collision Involvement among Persons with Hemianopia and Quadrantanopia. Geriatrics. 2016; 1(3):19. https://doi.org/10.3390/geriatrics1030019
Chicago/Turabian StyleMcGwin Jr., Gerald, Joanne Wood, Carrie Huisingh, and Cynthia Owsley. 2016. "Motor Vehicle Collision Involvement among Persons with Hemianopia and Quadrantanopia" Geriatrics 1, no. 3: 19. https://doi.org/10.3390/geriatrics1030019