Medically Serious and Non-Serious Suicide Attempts in Persons Aged 70 and Above
Abstract
:1. Introduction
2. Methods
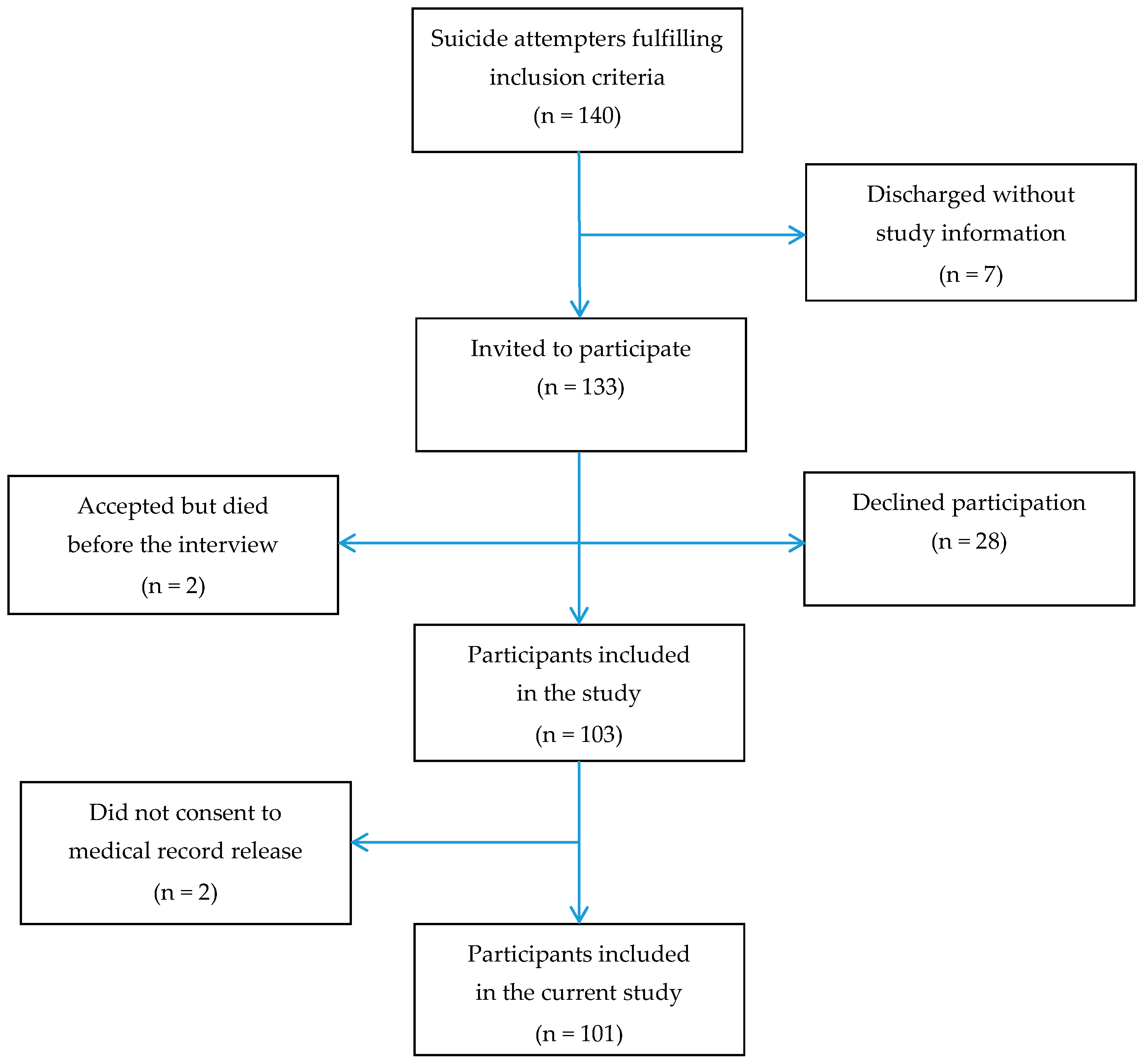
2.1. Participants
2.2. Procedures
2.3. Diagnostics and Classification of Attempts
2.4. Classification of Suicide Attempts
2.5. Statistics
2.6. Ethics
3. Results
3.1. Suicide Methods and Medical Severity
3.2. Psychosocial and Clinical Characteristics in Persons with MSSA vs. NMSSA
3.3. Reasons for Attempting Suicide in Persons with MSSA vs. NMSSA
3.4. Regression Models
4. Discussion
4.1. Findings
4.2. Methodological Considerations
4.3. Implications
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Fedyszyn, I.E.; Erlangsen, A.; Hjorthøj, C.; Madsen, T.; Nordentoft, M. Repeated suicide attempts and suicide among individuals with a first emergency department contact for attempted suicide: A prospective, nationwide, danish register-based study. J. Clin. Psychiatry 2016, 77, 832–840. [Google Scholar] [CrossRef] [PubMed]
- Beautrais, A.L. Suicides and serious suicide attempts: Two populations or one? Psychol. Med. 2001, 31, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Beautrais, A.L.; Joyce, P.R.; Mulder, R.T. Personality traits and cognitive styles as risk factors for serious suicide attempts among young people. Suicide Life Threat. Behav. 1999, 29, 37–47. [Google Scholar] [PubMed]
- Horesh, N.; Levi, Y.; Apter, A. Medically serious versus non-serious suicide attempts: Relationships of lethality and intent to clinical and interpersonal characteristics. J. Affect. Disord. 2012, 136, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Giner, L.; Jaussent, I.; Olié, E.; Béziat, S.; Guillaume, S.; Baca-Garcia, E.; Lopez-Castroman, J.; Courtet, P. Violent and serious suicide attempters: One step closer to suicide? J. Clin. Psychiatry 2014, 75, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Levi-Belz, Y.; Beautrais, A. Serious Suicide Attempts. Crisis 2016. [Google Scholar] [CrossRef] [PubMed]
- Vanyukov, P.M.; Szanto, K.; Hallquist, M.; Moitra, M.; Dombrovski, A.Y. Perceived burdensomeness is associated with low-lethality suicide attempts, dysfunctional interpersonal style, and younger rather than older age. Int. J. Geriatr. Psychiatry 2016. [Google Scholar] [CrossRef] [PubMed]
- Fässberg, M.M.; Cheung, G.; Canetto, S.S.; Erlangsen, A.; Lapierre, S.; Lindner, R.; Draper, B.; Gallo, J.J.; Wong, C.; Wu, J.; et al. A systematic review of physical illness, functional disability, and suicidal behaviour among older adults. Aging Ment. Health 2015, 20, 166–194. [Google Scholar] [CrossRef] [PubMed]
- Van Orden, K.A.; Wiktorsson, S.; Duberstein, P.; Berg, A.I.; Fässberg, M.M.; Waern, M. Reasons for attempted suicide in later life. Am. J. Geriatr. Psychiatry 2015, 23, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Wiktorsson, S.; Runeson, B.; Skoog, I.; Östling, S.; Waern, M. Attempted suicide in the elderly: Characteristics of suicide attempters 70 years and older and a general population comparison group. Am. J. Geriatr. Psychiatry 2010, 18, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.; Davis, R.J.; Frederick, J.C.; Perlin, S.; Pokorny, A.D.; Schulman, R.E.; Seiden, R.H.; Wittlin, B. Classification and Nomenclature. In Suicide Prevention in the Seventies; Resnick, H.L.P., Hathorne, B.C., Eds.; US Government Printing Office: Washington, DC, USA, 1972; pp. 7–12. [Google Scholar]
- Gottfries, G.G.; Noltorp, S.; Norgaard, N. Experience with a Swedish version of the Geriatric Depression Scale in primary care centres. Int. J. Geriatr. Psychiatry 1997, 12, 1029–1034. [Google Scholar] [CrossRef]
- Yesavage, J.A.; Brink, T.L.; Rose, T.L.; Lum, O.; Huang, V.; Adey, M.; Leirer, V.O. Development and validation of a geriatric depression screening scale: A preliminary report. J. Psychiatric Res. 1982, 17, 37–49. [Google Scholar] [CrossRef]
- Tyrer, P.; Owen, R.T.; Cicchetti, D.V. The brief scale for anxiety: A subdivision of the comprehensive psychopathological rating scale. J. Neurol. Neurosurg. Psychiatry 1984, 47, 970–975. [Google Scholar] [CrossRef] [PubMed]
- Asberg, M.; Montgomery, S.A.; Perris, C.; Schalling, D.; Sedvall, G. A comprehensive psychopathological rating scale. Acta Psychiatr. Scand. 1978, 57, 5–27. [Google Scholar] [CrossRef]
- Folstein, M.F.; Robins, L.N.; Helzer, J.E. The Mini-Mental State Examination. Arch. Gen. Psychiatry 1983, 40, 812. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.D.; Paradis, C.F.; Houck, P.R.; Mazumdar, S.; Stack, J.A.; Rifai, A.H.; Mulsant, B.; Reynolds, C.F., 3rd. Rating chronic medical illness burden in geropsychiatric practice and research: Application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992, 41, 237–248. [Google Scholar] [CrossRef]
- Waern, M.; Rubenowitz, E.; Runeson, B.; Skoog, I.; Wilhelmson, K.; Allebeck, P. Burden of illness and suicide in elderly people: Case-control study. BMJ 2002, 324, 1355. [Google Scholar] [CrossRef] [PubMed]
- Wiktorsson, S.; Berg, A.I.; Wilhelmson, K.; Mellqvist Fässberg, M.; Van Orden, K.; Duberstein, P.; Waern, M. Assessing the role of physical illness in young old and older old suicide attempters. Int. J. Geriatr. Psychiatry 2015, 31, 771–774. [Google Scholar] [CrossRef] [PubMed]
- Antonovsky, A. Unraveling The Mystery of Health—How People Manage Stress and Stay Well; Jossey-Bass Publishers: San Francisco, CA, USA, 1987. [Google Scholar]
- Mellqvist, M.; Wiktorsson, S.; Joas, E.; Ostling, S.; Skoog, I.; Waern, M. Sense of coherence in elderly suicide attempters: The impact of social and health-related factors. Int. Psychogeriatr. 2011, 23, 986–993. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, DSM-IV; American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar]
- Morin, J.; Wiktorsson, S.; Marlow, T.; Olesen, P.J.; Skoog, I.; Waern, M. Alcohol use disorder in elderly suicide attempters: A comparison study. Am. J. Geriatr. Psychiatry 2013, 21, 196–203. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, -Revised (DSM-III-R); American Psychiatric Association: Washington, DC, USA, 1987. [Google Scholar]
- Skoog, I.; Skoog, I.; Nilsson, L.; Palmertz, B.; Andreasson, L.A.; Svanborg, A. A population-based study of dementia in 85-year-olds. N. Engl. J. Med. 1993, 328, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Conwell, Y.; Rotenberg, M.; Caine, E.D. Completed suicide at age 50 and over. J. Am. Geriatr. Soc. 1990, 38, 640–644. [Google Scholar] [CrossRef] [PubMed]
- Trakhtenbrot, R.; Gvion, Y.; Levi-Belz, Y.; Horesh, N.; Fischel, T.; Weiser, M.; Treves, I.; Apter, A. Predictive value of psychological characteristics and suicide history on medical lethality of suicide attempts: A follow-up study of hospitalized patients. J. Affect. Disord. 2016, 199, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Gvion, Y.; Horresh, N.; Levi-Belz, Y.; Fischel, T.; Treves, I.; Weiser, M.; David, H.S.; Stein-Reizer, O.; Apter, A. Aggression–impulsivity, mental pain, and communication difficulties in medically serious and medically non-serious suicide attempters. Compr. Psychiatry 2014, 55, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Olsson, P.; Wiktorsson, S.; Sacuiu, S.; Marlow, T.; Östling, S.; Fässberg, M.M.; Skoog, I.; Waern, M. Cognitive function in older suicide attempters and a population-based comparison group. J. Geriatr. Psychiatry Neurol. 2016, 29, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Mukaetova-Ladinska, E.B. Current and Future Perspectives of Liaison Psychiatry Services: Relevance for Older People’s Care. Geriatrics 2016, 1, 7. [Google Scholar] [CrossRef]
- Gysin-Maillart, A.; Schwab, S.; Soravia, L.; Megert, M.; Michel, K. A novel brief therapy for patients who attempt suicide: A 24-months follow-up randomized controlled study of the attempted suicide short intervention program (ASSIP). PLoS Med. 2016, 13, e1001968. [Google Scholar] [CrossRef] [PubMed]
| Suicide Methods | Medically Serious Attempt | Total | |
|---|---|---|---|
| No (n = 73); n (%) | Yes (n = 28); n (%) | (n = 101); n (%) | |
| Non-Violent Methods (Overdose/Poisoning) | |||
| Sedatives and hypnotics | |||
| Bensodiazepines | 23 (31.5) | 9 (32.1) | 32 (31.6) |
| Zopiclone | 12 (16.4) | 4 (14.2) | 16 (15.8) |
| Zolpidem | 13 (17.8) | 2 (7.1) | 15 (14.8) |
| Others | 6 (8.2) | 3 (10.7) | 9 (8.9) |
| Antidepressants | 7 (9.6) | 1 (3.6) | 8 (7.9) |
| Antipsychotics | 1 (1.4) | 2 (7.1) | 3 (2.9) |
| Lithium | 0 (-) | 1 (3.6) | 1 (0.9) |
| Analgesics | 1(1.4) | 2 (7.1) | 3 (2.9) |
| Opioids | 4 (5.5) | 4 (14.3) | 8 (7.9) |
| Paracetamol | 3 (4.1) | 2 (7.1) | 5 (4.9) |
| Other substances | 14 (19.2) | 3 (10.7) | 17 (16.8) |
| Violent methods | |||
| Drowning | 2 (2.7) | 0 (-) | 2 (1.9) |
| Hanging | 1 (1.4) | 4 (14.3) | 5 (5.0) |
| Strangling | 7 (9.6) | 0 (-) | 7 (6.9) |
| Suffocation | 1 (1.4) | 0 (-) | 1 (0.9) |
| Cutting | 5 (6.8) | 6 (21.4) | 11 (10.9) |
| Characteristics | Medically Serious Attempts | Test Result 1 p-Value | |
|---|---|---|---|
| No (n = 73); n (%) | Yes (n = 28); n (%) | ||
| Psychosocial Characteristics | |||
| Living alone | 52 (71.2) | 16 (57.1) | 0.236 |
| Married/living with a partner | 21 (28.8) | 12 (42.9) | 0.236 |
| Education, mandatory only | 40 (54.8) | 17 (60.7) | 0.658 |
| Loneliness | 41 (56.2) | 17 (60.7) | 0.823 |
| Family history of suicide | 6 (8.2) | 4 (14.3) | 0.458 |
| Clinical Characteristics | |||
| Major depression | 46 (63.0) | 21 (75.0) | 0.348 |
| Minor depression | 19 (26.0) | 7 (12.5) | 1.000 |
| Alcohol use disorder | 22 (30.1) | 5 (17.9) | 0.315 |
| Dementia | 4 (5.5) | 4 (14.3) | 0.212 |
| Serious physical illness | 42 (57.5) | 21 (75.0) | 0.116 |
| History of psychiatric treatment | 41 (56.2) | 18 (64.3) | 0.506 |
| Previous suicide attempt(s) | 26 (35.6) | 10 (35.7) | 1.000 |
| Antidepressant prescription | 39 (53.4) | 21 (75) | 0.070 |
| Hopelessness 2 | 39 (56.5) | 15 (55.6) | 0.932 |
| Rating Scales | Mean (SD 3) | Mean (SD) | Test Result 4 |
| Geriatric Depression Scale, (n = 96) | 9.5 (2.7) | 9.9 (2.8) | t = −0.76, df = 94, p = 0.447 |
| Brief Scale of Anxiety, (n = 97) | 8.6 (5.3) | 11.4 (6.3) | t = −2.27, df = 95, p = 0.025 |
| Sense of Coherence, (n = 87) | 131.3 (20.8) | 123.9 (26.9) | t = 1.31, df = 85, p = 0.193 |
| Cumulative illness rating scale, (n = 101) | 9.6 (4.4) | 9.1 (3.2) | t = 0.63, df = 99, p = 0.532 |
| MMSE 5, (n = 96) | 26.0 (3.5) | 23.7 (4.3) | t = 2.70, df = 94, p = 0.008 |
| Reasons | Medically Serious Attempts | Test Result 2 p-Value | |
|---|---|---|---|
| No 1 (n = 72); n (%) | Yes (n = 28); n (%) | ||
| Social problems | 6 (8.3) | 7 (25.0) | 0.043 |
| Being a burden to others | 9 (12.5) | 4 (14.3) | 0.753 |
| Functioning and autonomy | 13 (18.1) | 11 (39.3) | 0.037 |
| Somatic problems and pain | 12 (16.7) | 4 (14.3) | 1.000 |
| Psychological problems | 16 (22.2) | 8 (28.6) | 0.603 |
| Lack of meaning | 6 (8.3) | 2 (7.1) | 1.000 |
| Escape | 19 (26.4) | 10 (35.7) | 0.462 |
| Wanted to die or sleep 3 | 13 (18.1) | 0 (0) | 0.017 |
| No memory or understanding | 11 (15.3) | 3 (10.7) | 0.752 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wiktorsson, S.; Olsson, P.; Waern, M. Medically Serious and Non-Serious Suicide Attempts in Persons Aged 70 and Above. Geriatrics 2016, 1, 23. https://doi.org/10.3390/geriatrics1030023
Wiktorsson S, Olsson P, Waern M. Medically Serious and Non-Serious Suicide Attempts in Persons Aged 70 and Above. Geriatrics. 2016; 1(3):23. https://doi.org/10.3390/geriatrics1030023
Chicago/Turabian StyleWiktorsson, Stefan, Petter Olsson, and Margda Waern. 2016. "Medically Serious and Non-Serious Suicide Attempts in Persons Aged 70 and Above" Geriatrics 1, no. 3: 23. https://doi.org/10.3390/geriatrics1030023






