Liquid Dynamics in the Upper Respiratory–Digestive System with Contracting Pharynx Motions and Varying Epiglottis Angles
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
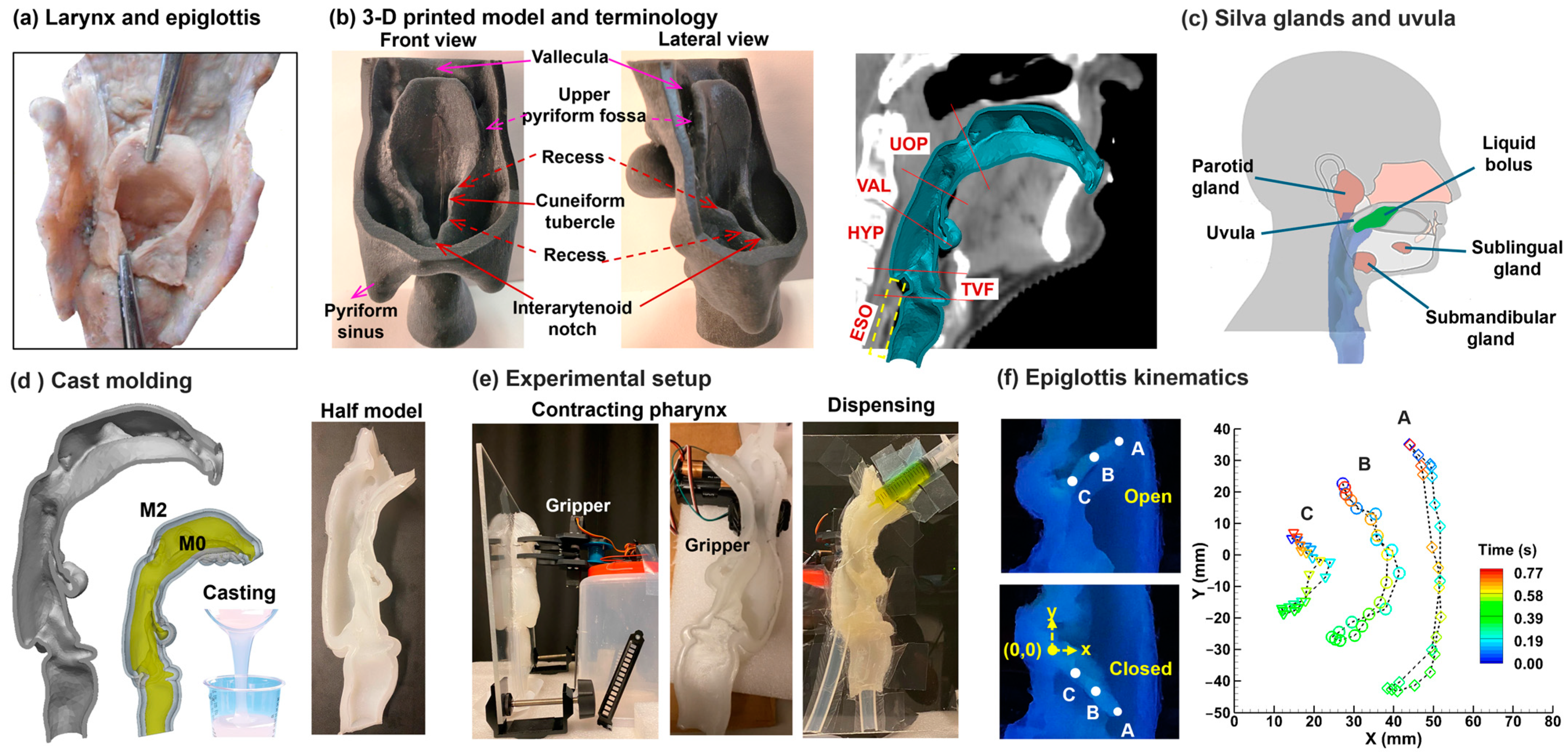
2.2. Pharynx–Epiglottis Geometry and Cast
2.3. Experimental Setup and Procedures
2.3.1. Control of Dynamic Structures
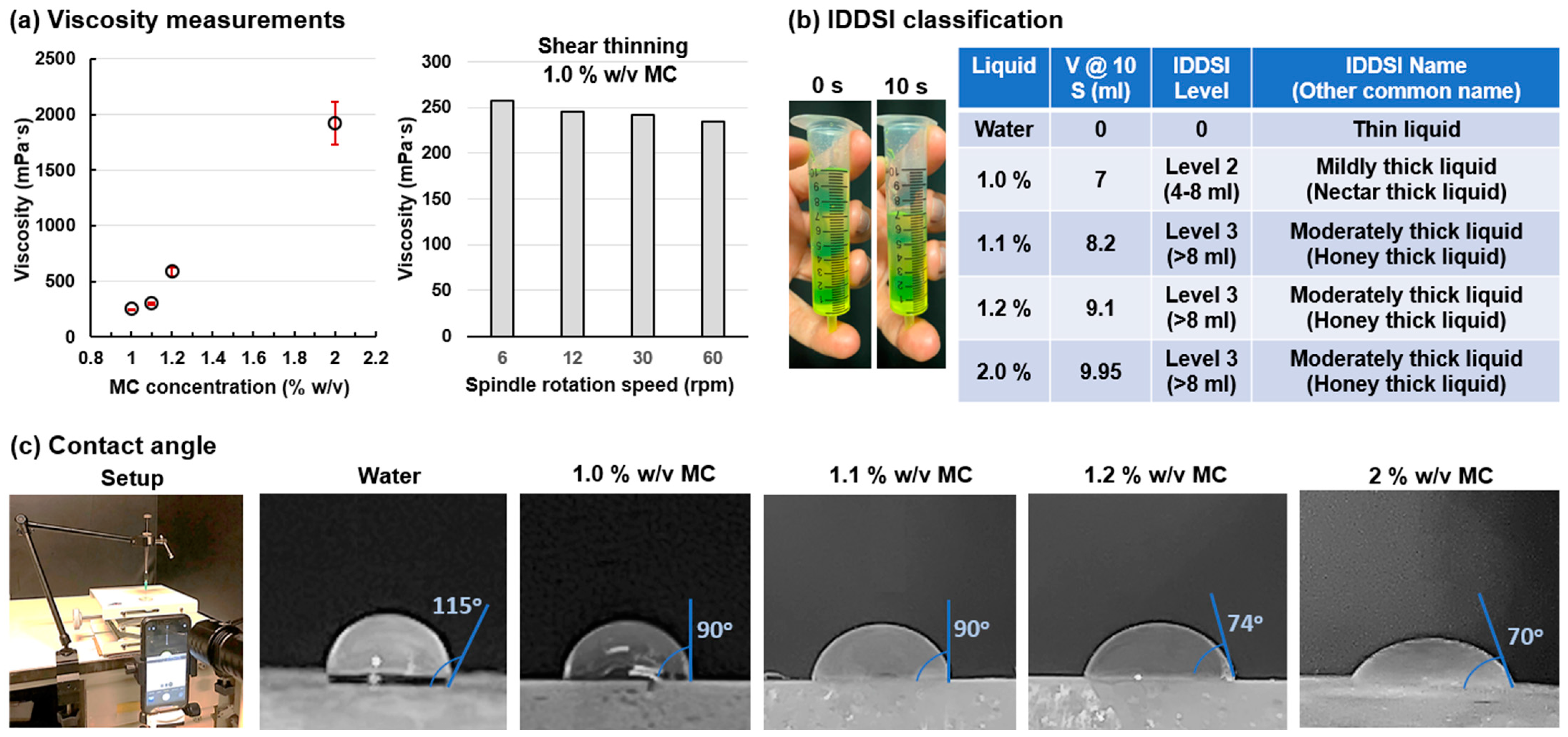
2.3.2. Liquid Selection and Property Measurements
2.3.3. Visualization and Recording
3. Results
3.1. Liquid Physical Property Measurement
3.2. Liquid Flow Dynamics with Contracting Pharynx and Flapping Epiglottis
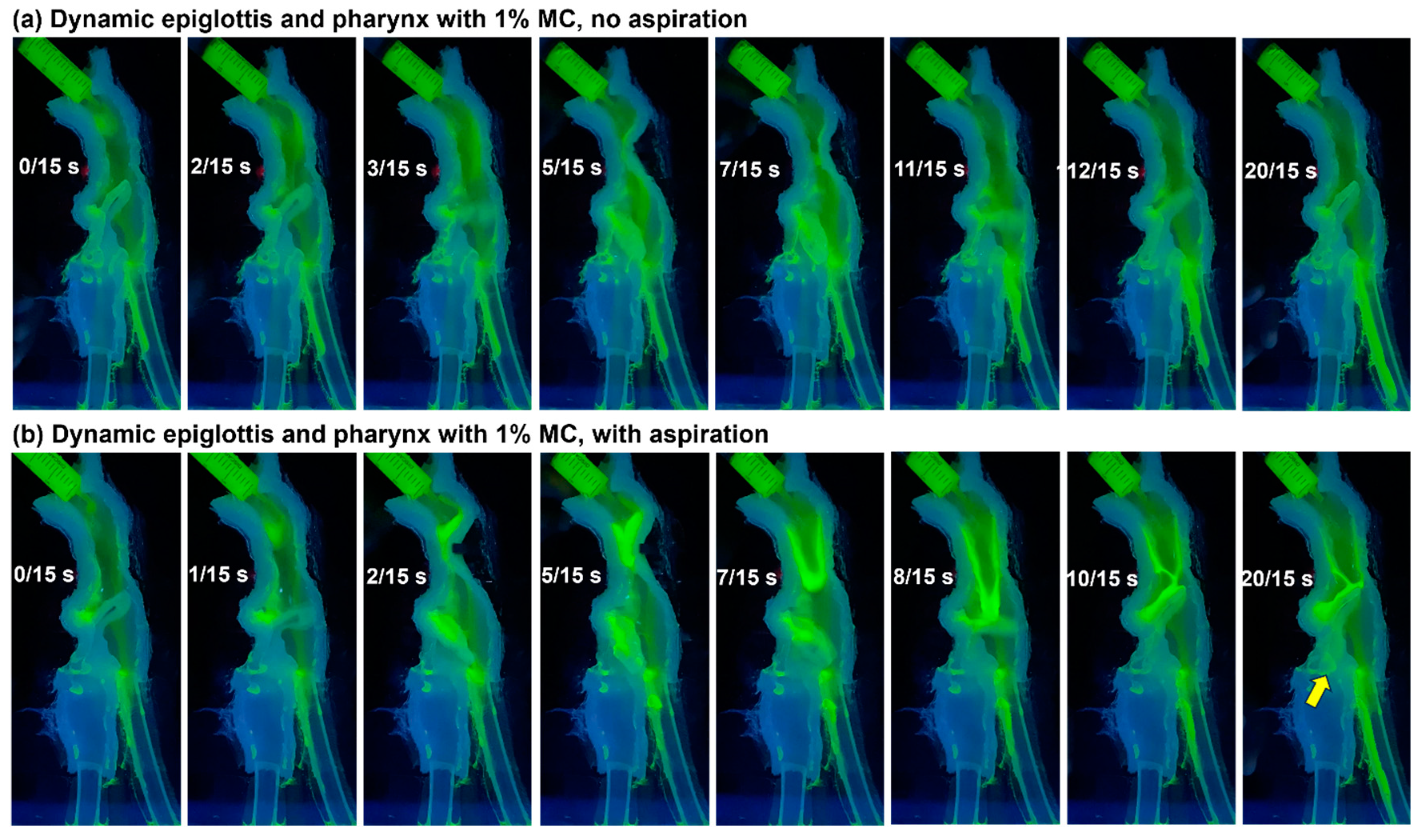
3.2.1. MC Solution of 1% w/v
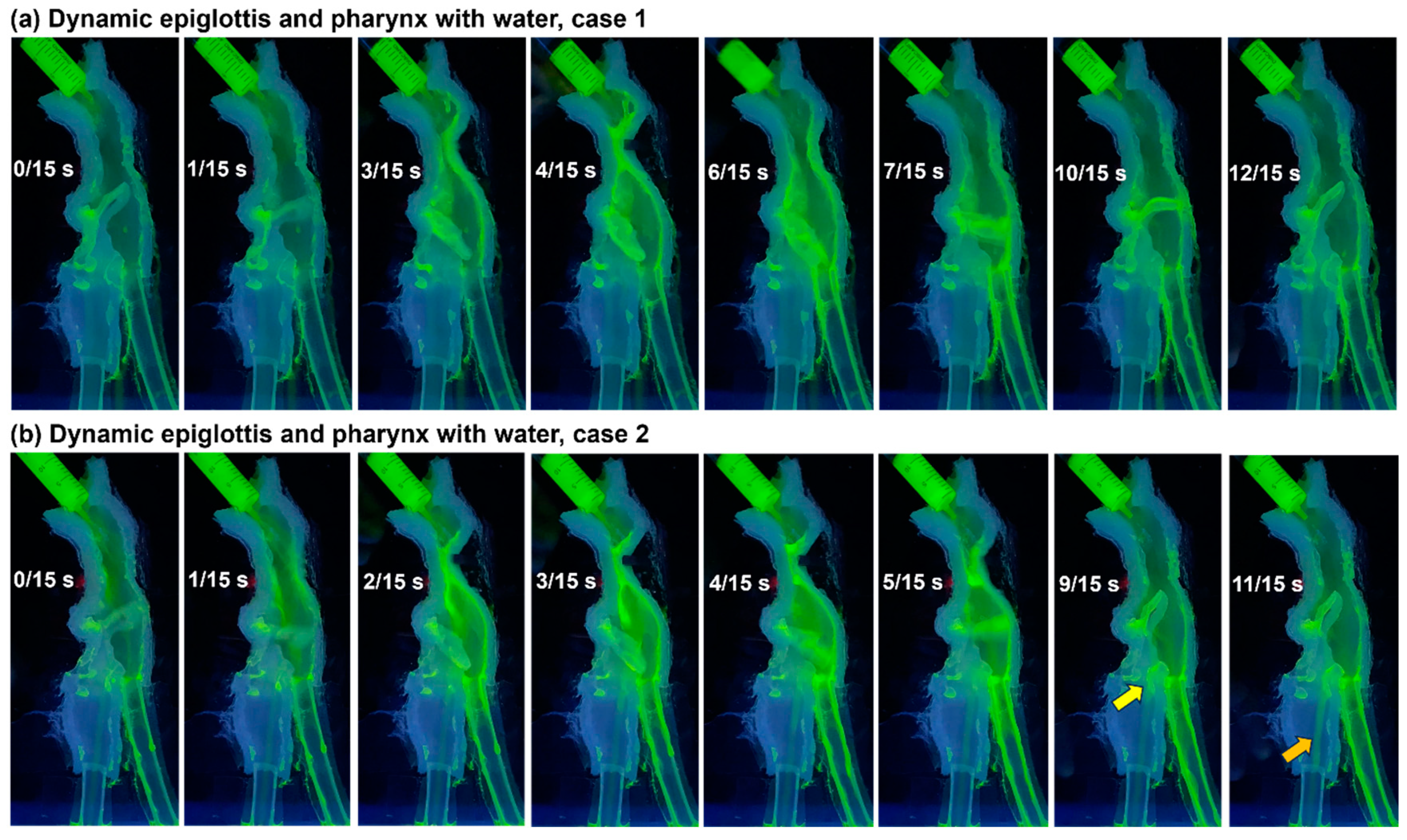
3.2.2. Water
3.3. Liquid Flow Dynamics with Flapping Epiglottis Only
3.3.1. MC Solution of 1% w/v
3.3.2. Water
3.4. Liquid Flow Dynamics with Stationary Epiglottis at Varying Angles
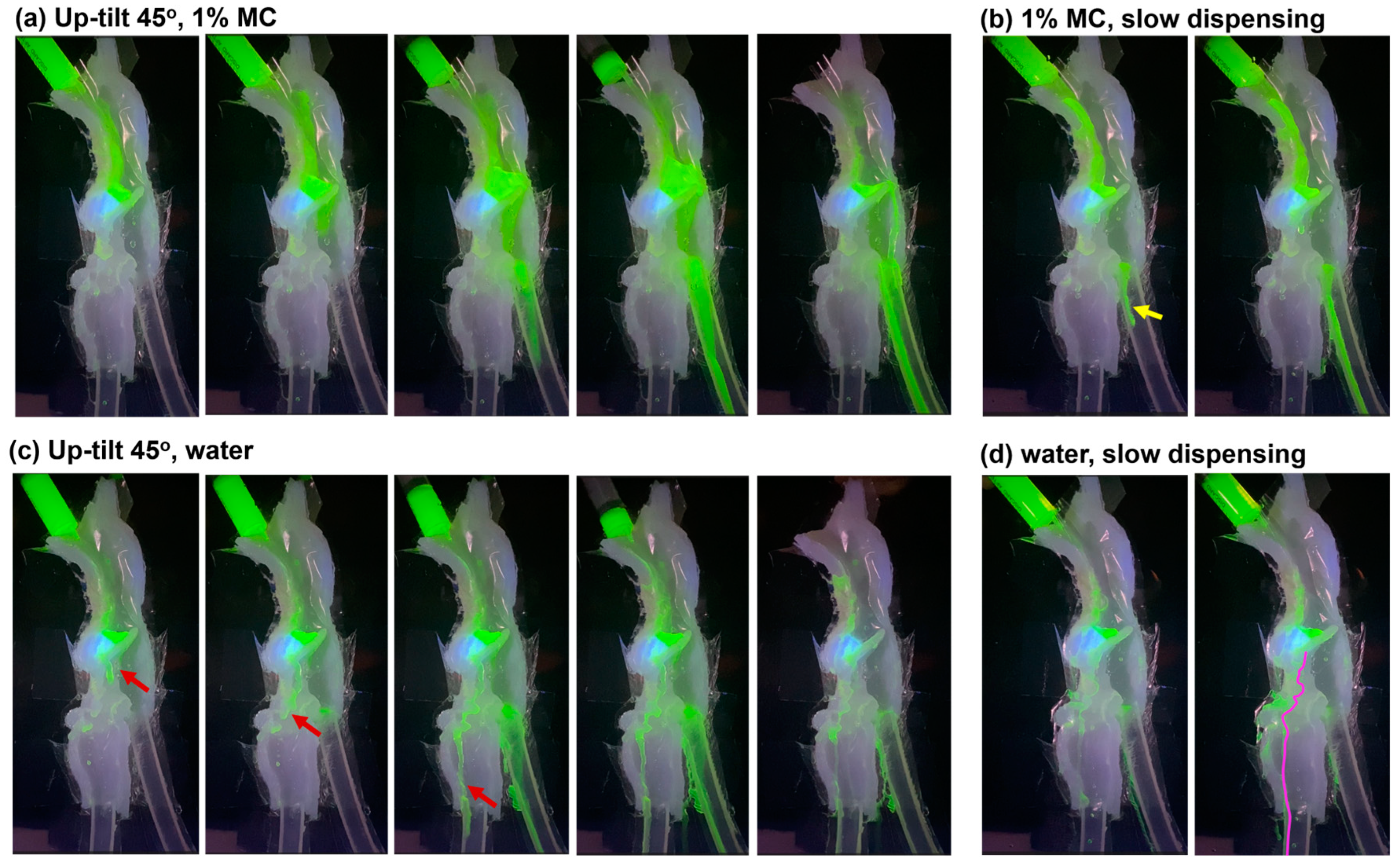
3.4.1. Up-Tilt 45°, 1% w/v MC
3.4.2. Up-Tilt 45°, Water
3.4.3. Horizontal (0°), Water
3.4.4. Down-Tilt 45°, Water
4. Discussion
4.1. Liquid Flow Patterns with Higher Aspiration Risks
4.2. Frequent Aspirations with Slow Water Dispensing and Implications
4.3. Limitations and Future Studies
5. Conclusions
- Water poses a higher aspiration risk than the 1% w/v methylcellulose (MC) solution for all scenarios considered.
- The dynamic pharynx and epiglottis caused a delayed esophageal entry and vallecular residual for the MC solution.
- Dispensing liquid too slowly increased the aspiration risk for water, but not for the MC solution.
- An incomplete inversion of the epiglottis, such as a horizontal or 45° downward tilt, increases the risk of aspirating water.
- Three frequent aspiration locations were observed, including the epiglottis base for capillary flows, the cuneiform tubercular recesses for off-edge flows, and the interarytenoid notch for flows accumulated in the pyriform fossa.
- Future studies are needed to verify the observed aspiration mechanisms in models with increasing levels of physiological realism.
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shaw, S.M.; Martino, R. The normal swallow: Muscular and neurophysiological control. Otolaryngol. Clin. N. Am. 2013, 46, 937–956. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, K.; Palmer, J.B. Anatomy and physiology of feeding and swallowing: Normal and abnormal. Phys. Med. Rehabil. Clin. N. Am. 2008, 19, 691–707. [Google Scholar] [CrossRef] [PubMed]
- Ding, P.; Tufano, R.P.; German, R.Z. Anatomical anomalies of the laryngeal branches of the vagus nerve in pigs (Sus scrofa). Lab. Anim. 2012, 46, 338–340. [Google Scholar] [CrossRef]
- Niederman, M.S.; Cilloniz, C. Aspiration pneumonia. Rev. Esp. Quimioter. 2022, 35 (Suppl. S1), 73–77. [Google Scholar] [CrossRef] [PubMed]
- Košutova, P.; Mikolka, P. Aspiration syndromes and associated lung injury: Incidence, pathophysiology and management. Physiol. Res. 2021, 70, S567–S583. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, T.T.; Mylotte, J.M. Nursing home-acquired pneumonia. Clin. Infect. Dis. 2002, 35, 1205–1211. [Google Scholar]
- Gupte, T.; Knack, A.; Cramer, J.D. Mortality from aspiration pneumonia: Incidence, trends, and risk factors. Dysphagia 2022, 37, 1493–1500. [Google Scholar] [CrossRef] [PubMed]
- Caplan, Z.U.S. Older Population Grew from 2010 to 2020 at Fastest Rate Since 1880 to 1890. Available online: https://www.census.gov/library/stories/2023/05/2020-census-united-states-older-population-grew.html (accessed on 15 January 2024).
- Sasegbon, A.; Hamdy, S. The anatomy and physiology of normal and abnormal swallowing in oropharyngeal dysphagia. Neurogastroenterol. Motil. 2017, 29, e13100. [Google Scholar] [CrossRef] [PubMed]
- Skarbinski, K.F.; Glennon, E. Dysphagia: A review. Nurse Pract. 2020, 45, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, J.M.; Codipilly, D.C.; Wilfahrt, R.P. Dysphagia: Evaluation and collaborative management. Am. Fam. Physician 2021, 103, 97–106. [Google Scholar]
- Iorgulescu, G. Saliva between normal and pathological. Important factors in determining systemic and oral health. J. Med. Life 2009, 2, 303–307. [Google Scholar] [PubMed]
- Jensen, S.B.; Vissink, A.; Limesand, K.H.; Reyland, M.E. Salivary Gland Hypofunction and Xerostomia in Head and Neck Radiation Patients. J. Natl. Cancer Inst. Monogr. 2019, 2019, lgz016. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.Z.; Ando, H.; Unno, S.; Kitagawa, J. Targeting chemosensory ion channels in peripheral swallowing-related regions for the management of oropharyngeal dysphagia. Int. J. Mol. Sci. 2020, 21, 6214. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, P.; Plowman, E.K.; Steele, C.M. Differences in pharyngeal swallow event timing: Healthy aging, Parkinson disease, and amyotrophic lateral sclerosis. Laryngoscope Investig. Otolaryngol. 2023, 8, 466–477. [Google Scholar] [CrossRef] [PubMed]
- Takizawa, C.; Gemmell, E.; Kenworthy, J.; Speyer, R. A systematic review of the prevalence of oropharyngeal dysphagia in stroke, Parkinson’s disease, Alzheimer’s disease, head injury, and pneumonia. Dysphagia 2016, 31, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Mayerl, C.J.; Gould, F.D.H.; Adjerid, K.; Edmonds, C.; German, R.Z. The pathway from anatomy and physiology to diagnosis: A developmental perspective on swallowing and dysphagia. Dysphagia 2023, 38, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, M.A.; Gillespie, M.B.; Ishman, S.L.; Ishii, L.E.; Brody, R.; Cohen, E.; Dhar, S.I.; Hutcheson, K.; Jefferson, G.; Johnson, F.; et al. Expert consensus statement: Management of dysphagia in head and neck cancer patients. Otolaryngol. Head Neck Surg. 2023, 168, 571–592. [Google Scholar] [CrossRef] [PubMed]
- Labeit, B.; Michou, E.; Hamdy, S.; Trapl-Grundschober, M.; Suntrup-Krueger, S.; Muhle, P.; Bath, P.M.; Dziewas, R. The assessment of dysphagia after stroke: State of the art and future directions. Lancet Neurol. 2023, 22, 858–870. [Google Scholar] [CrossRef] [PubMed]
- Mira, A.; Gonçalves, R.; Rodrigues, I.T. Dysphagia in Alzheimer’s disease: A systematic review. Dement. Neuropsychol. 2022, 16, 261–269. [Google Scholar] [CrossRef]
- Umemoto, G.; Furuya, H. Management of dysphagia in patients with parkinson’s disease and related disorders. Intern Med. 2020, 59, 7–14. [Google Scholar] [CrossRef]
- Goyal, R.; Mashimo, H. Physiology of oral, pharyngeal, and esophageal motility. GI Motility Online 2006. [Google Scholar] [CrossRef]
- Ding, P.; Fung, G.S.; Lin, M.; Holman, S.D.; German, R.Z. The effect of bilateral superior laryngeal nerve lesion on swallowing: A novel method to quantitate aspirated volume and pharyngeal threshold in videofluoroscopy. Dysphagia 2015, 30, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Xi, J.; Han, P.; Wongwiset, N.; Pontius, J.; Dong, H. Computational analysis of a flapping uvula on aerodynamics and pharyngeal wall collapsibility in sleep apnea. J. Biomech. 2019, 94, 88–98. [Google Scholar] [CrossRef]
- Xi, J.; Wang, Z.; Talaat, K.; Glide-Hurst, C.; Dong, H. Numerical study of dynamic glottis and tidal breathing on respiratory sounds in a human upper airway model. Sleep Breath. 2018, 22, 463–479. [Google Scholar] [CrossRef] [PubMed]
- Si, X.; Talaat, M.; Xi, J. SARS CoV-2 virus-laden droplets coughed from deep lungs: Numerical quantification in a single-path whole respiratory tract geometry. Phys. Fluids 2021, 33, 023306. [Google Scholar]
- Mizunuma, H.; Sonomura, M.; Shimokasa, K. Numerical simulation of pharyngeal bolus flow influenced by bolus viscosity and apparent slip. J. Texture Stud. 2020, 51, 742–754. [Google Scholar] [CrossRef] [PubMed]
- Xi, J.; Kim, J.; Si, X.; Corley, R.A.; Zhou, Y. Modeling of inertial depositions in scaled models of rat and human nasal airways: Towards in vitro regional dosimetry in small animals. J. Aerosol Sci. 2015, 99, 78–93. [Google Scholar] [CrossRef]
- Xi, J.; Talaat, M.; Si, X.A.; Han, P.; Dong, H.; Zheng, S. Alveolar size effects on nanoparticle deposition in rhythmically expanding-contracting terminal alveolar models. Comput. Biol. Med. 2020, 121, 103791. [Google Scholar] [CrossRef]
- Kikuchi, T.; Michiwaki, Y.; Azegami, H. Identification of muscle activities involved in hyoid bone movement during swallowing using computer simulation. Comput. Methods Biomech. Biomed. Eng. Imaging Vis. 2023, 11, 1791–1802. [Google Scholar] [CrossRef]
- Nakamura, T.; Kita, Y.; Fujimoto, J.; Ayuzawa, K.; Ozawa, H. Hyoid bone movement during swallowing and mechanism of pharyngeal residue in patients with profound intellectual and multiple disabilities. Int. J. Pediatr. Otorhinolaryngol. 2021, 149, 110849. [Google Scholar] [CrossRef]
- Hashimoto, T.; Urabe, M.; Chee-Sheng, F.; Murakoshi, A.; Kikuchi, T.; Michiwaki, Y.; Koike, T. Development of a musculoskeletal model of hyolaryngeal elements for understanding pharyngeal swallowing mechanics. Appl. Sci. 2020, 10, 6276. [Google Scholar] [CrossRef]
- Li, Q.; Minagi, Y.; Ono, T.; Chen, Y.; Hori, K.; Fujiwara, S.; Maeda, Y. The biomechanical coordination during oropharyngeal swallowing: An evaluation with a non-invasive sensing system. Sci. Rep. 2017, 7, 15165. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, V.; de Loubens, C.; Thomas, C.; Panouillé, M.; Magnin, A.; Souchon, I. An experimental model to investigate the biomechanical determinants of pharyngeal mucosa coating during swallowing. J. Biomech. 2018, 72, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Stading, M.; Waqas, M.Q.; Holmberg, F.; Wiklund, J.; Kotze, R.; Ekberg, O. A device that models human swallowing. Dysphagia 2019, 34, 615–626. [Google Scholar] [CrossRef]
- Fujiso, Y.; Perrin, N.; van der Giessen, J.; Vrana, N.E.; Neveu, F.; Woisard, V. Swall-E: A robotic in-vitro simulation of human swallowing. PLoS ONE 2018, 13, e0208193. [Google Scholar] [CrossRef] [PubMed]
- Xi, J.; Wang, Z.; Si, X.A.; Zhou, Y. Nasal dilation effects on olfactory deposition in unilateral and bi-directional deliveries: In vitro tests and numerical modeling. Eur. J. Pharm. Sci. 2018, 118, 113–123. [Google Scholar] [CrossRef] [PubMed]
- Printza, A.; Boziki, M.; Triaridis, S.; Kiousi, V.; Arnaoutoglou, M.; Constantinidis, J.; Grigoriadis, N. Tongue strength, dysphagia questionnaire, pharyngeal secretions and FEES findings in dysphagia management in amyotrophic lateral sclerosis. Auris Nasus Larynx 2021, 48, 672–682. [Google Scholar] [CrossRef] [PubMed]
- Murphy, E.R.; Thompson, R.; Osman, K.L.; Haxton, C.; Brothers, M.; Lee, L.; Warncke, K.; Smith, C.L.; Keilholz, A.N.; Hamad, A.; et al. A strength endurance exercise paradigm mitigates deficits in hypoglossal-tongue axis function, strength, and structure in a rodent model of hypoglossal motor neuron degeneration. Front. Neurosci. 2022, 16, 869592. [Google Scholar] [CrossRef] [PubMed]
- Rutili, V.; Nieri, M.; Franceschi, D.; Pierleoni, F.; Giuntini, V.; Franchi, L. Comparison of rapid versus slow maxillary expansion on patient-reported outcome measures in growing patients: A systematic review and meta-analysis. Prog. Orthod. 2022, 23, 47. [Google Scholar] [CrossRef]
- Corley, R.A.; Kabilan, S.; Kuprat, A.P.; Carson, J.P.; Jacob, R.E.; Minard, K.R.; Teeguarden, J.G.; Timchalk, C.; Pipavath, S.; Glenny, R.; et al. Comparative risks of aldehyde constituents in cigarette smoke using transient computational fluid dynamics/physiologically based pharmacokinetic models of the rat and human respiratory tracts. Toxicol. Sci. 2015, 146, 65–88. [Google Scholar] [CrossRef]
- Corley, R.A.; Kabilan, S.; Kuprat, A.P.; Carson, J.P.; Minard, K.R.; Jacob, R.E.; Timchalk, C.; Glenny, R.; Pipavath, S.; Cox, T.; et al. Comparative computational modeling of airflows and vapor dosimetry in the respiratory tracts of rat, monkey, and human. Toxicol. Sci. 2012, 128, 500–516. [Google Scholar] [CrossRef]
- Wikiwand. Epiglottic Vallecula, From Wikipedia, the Free Encyclopedia. Available online: https://www.wikiwand.com/en/Epiglottic_vallecula (accessed on 15 January 2024).
- Materials, A. Silicone Rubber: Room Temperature Vulcanising (RTV) Rubbers. Available online: https://www.azom.com/article.aspx?ArticleID=920 (accessed on 4 January 2024).
- Ismael-Mohammed, K.; Bolivar-Prados, M.; Laguna, L.; Clavé, P. Measuring the rheological and textural properties of thick Purees used to manage patients with swallowing disorders. Nutrients 2023, 15, 3767. [Google Scholar] [CrossRef] [PubMed]
- Bolivar-Prados, M.; Hayakawa, Y.; Tomsen, N.; Arreola, V.; Nascimento, W.; Riera, S.; Kawakami, S.; Miyaji, K.; Takeda, Y.; Kayashita, J.; et al. Shear-viscosity-dependent effect of a gum-based thickening product on the safety of swallowing in older patients with severe oropharyngeal dysphagia. Nutrients 2023, 15, 3279. [Google Scholar] [CrossRef] [PubMed]
- Newman, R.; Vilardell, N.; Clavé, P.; Speyer, R. Effect of Bolus Viscosity on the Safety and Efficacy of Swallowing and the Kinematics of the Swallow Response in Patients with Oropharyngeal Dysphagia: White Paper by the European Society for Swallowing Disorders (ESSD). Dysphagia 2016, 31, 232–249. [Google Scholar] [CrossRef] [PubMed]
- Molfenter, S.M.; Steele, C.M. The relationship between residue and aspiration on the subsequent swallow: An application of the normalized residue ratio scale. Dysphagia 2013, 28, 494–500. [Google Scholar] [CrossRef] [PubMed]
- Mao, S.; Sabry, A.; Khalifa, Y.; Coyle, J.L.; Sejdic, E. Estimation of laryngeal closure duration during swallowing without invasive X-rays. Future Gener. Comput. Syst. 2021, 115, 610–618. [Google Scholar] [CrossRef] [PubMed]
- Gallegos, C.; Turcanu, M.; Assegehegn, G.; Brito-de la Fuente, E. Rheological issues on oropharyngeal dysphagia. Dysphagia 2023, 38, 558–585. [Google Scholar] [CrossRef] [PubMed]
- Forbes, J.; Humbert, I. Impact of the chin-down posture on temporal measures of patients with dysphagia: A pilot study. Am. J. Speech Lang. Pathol. 2021, 30, 1049–1060. [Google Scholar] [CrossRef] [PubMed]
- Pearson, W.G., Jr.; Molfenter, S.M.; Smith, Z.M.; Steele, C.M. Image-based measurement of post-swallow residue: The normalized residue ratio scale. Dysphagia 2013, 28, 167–177. [Google Scholar] [CrossRef]
- Meng, Y.; Rao, M.A.; Datta, A.K. Computer simulation of the pharyngeal bolus transport of Newtonian and non-Newtonian fluids. Food Bioprod. Process. 2005, 83, 297–305. [Google Scholar] [CrossRef]
- Michiwaki, Y.; Kamiya, T.; Kikuchi, T.; Toyama, Y.; Takai, M.; Hanyu, K.; Inoue, M.; Yahiro, N.; Koshizuka, S. Realistic computer simulation of bolus flow during swallowing. Food Hydrocoll. 2020, 108, 106040. [Google Scholar] [CrossRef]
- Nicosia, M.A.; Robbins, J.A. The fluid mechanics of bolus ejection from the oral cavity. J. Biomech. 2001, 34, 1537–1544. [Google Scholar] [CrossRef] [PubMed]
- Ohta, J.; Ishida, S.; Kawase, T.; Katori, Y.; Imai, Y. A computational fluid dynamics simulation of liquid swallowing by impaired pharyngeal motion: Bolus pathway and pharyngeal residue. Neurogastroenterol. Motil. 2019, 317, G784–G792. [Google Scholar] [CrossRef]
- Irvine, L.E.; Yang, Z.; Kezirian, E.J.; Nimni, M.E.; Han, B. Hyoepiglottic ligament collagen and elastin fiber composition and changes associated with aging. Laryngoscope 2018, 128, 1245–1248. [Google Scholar] [CrossRef] [PubMed]


| Constricting Pharynx and Flapping Epiglottis | Flapping Epiglottis Only | Epiglottis Up-Tilt 45° | Epiglottis 0° | Epiglottis Down-Tilt 45° | |
|---|---|---|---|---|---|
| 1% w/v MC | Figure 3a *, S1 Figure 3b * | Figure 5a *, S3 | Figure 6a * Figure 6b (slow) | NA | NA |
| Water | Figure 4a * Figure 4b *, S2 | Figure 5b *, S4 | Figure 6c * Figure 6d (slow) | Figure 7a Figure 7b (slow) | Figure 7c (Normal and slow) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seifelnasr, A.; Si, X.; Ding, P.; Xi, J. Liquid Dynamics in the Upper Respiratory–Digestive System with Contracting Pharynx Motions and Varying Epiglottis Angles. Liquids 2024, 4, 415-431. https://doi.org/10.3390/liquids4020022
Seifelnasr A, Si X, Ding P, Xi J. Liquid Dynamics in the Upper Respiratory–Digestive System with Contracting Pharynx Motions and Varying Epiglottis Angles. Liquids. 2024; 4(2):415-431. https://doi.org/10.3390/liquids4020022
Chicago/Turabian StyleSeifelnasr, Amr, Xiuhua Si, Peng Ding, and Jinxiang Xi. 2024. "Liquid Dynamics in the Upper Respiratory–Digestive System with Contracting Pharynx Motions and Varying Epiglottis Angles" Liquids 4, no. 2: 415-431. https://doi.org/10.3390/liquids4020022
APA StyleSeifelnasr, A., Si, X., Ding, P., & Xi, J. (2024). Liquid Dynamics in the Upper Respiratory–Digestive System with Contracting Pharynx Motions and Varying Epiglottis Angles. Liquids, 4(2), 415-431. https://doi.org/10.3390/liquids4020022







