Feature Papers in Obesity, Type 2 Diabetes and Metabolic Syndrome
Share This Topical Collection
Editor
 Prof. Dr. Manfredi Tesauro
Prof. Dr. Manfredi Tesauro
 Prof. Dr. Manfredi Tesauro
Prof. Dr. Manfredi Tesauro
E-Mail
Website
Collection Editor
U.O.C. of Internal Medicine—Center of Hypertension and Nephrology Unit, Department of Systems Medicine, University of Rome Tor Vergata, Rome, Italy
Interests: endothelial dysfunction; obesity; insulin resistance; diabetic nephropathy; metabolic syndrome; adipokines
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
The Topical Collection “Feature Papers in Obesity, Type 2 Diabetes and Metabolic Syndrome” will comprise important contributions by scholars and the Editorial Board members of the section Endocrinology and Metabolism Research in Biomedicines in the field of the emerging mechanisms underlying vascular and metabolic complications in diabetes and obesity. Both molecular and clinical studies are encouraged. Their broad expertise will result in a comprehensive array of the latest findings in this field, and, thus, we encourage submissions of high-quality research papers or review articles.
Contributions that explore different aspects ranging from adipokins, gastrointestinal peptides, visceral adipose tissue, perivascular adipose tissue, oxidative stress, vascular dysfunction in obesity and diabetes, free fatty acids (FFA), insulin resistance, ceramides, exercise/diet and new therapeutic targets for obesity, and type 2 diabetes are appropriate topics for this Special Issue. We look forward to your submissions on the above-listed research areas of cell biology and pathology.
Dr. Manfredi Tesauro
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Biomedicines is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript.
The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs).
Submitted papers should be well formatted and use good English. Authors may use MDPI's
English editing service prior to publication or during author revisions.
Published Papers (9 papers)
Open AccessArticle
Ethnic Variations in the Levels of Bone Biomarkers (Osteoprostegerin, Receptor Activator of Nuclear Factor Kappa-Β Ligand and Glycoprotein Non-Metastatic Melanoma Protein B) in People with Type 2 Diabetes
by
Preethi Cherian, Irina Al-Khairi, Mohamed Abu-Farha, Tahani Alramah, Ahmed N. Albatineh, Doha Alhomaidah, Fayez Safadi, Hamad Ali, Muhammad Abdul-Ghani, Jaakko Tuomilehto, Heikki A. Koistinen, Fahd Al-Mulla and Jehad Abubaker
Viewed by 407
Abstract
The global incidence of Type 2 diabetes (T2D) is on the rise, fueled by factors such as obesity, sedentary lifestyles, socio-economic factors, and ethnic backgrounds. T2D is a multifaceted condition often associated with various health complications, including adverse effects on bone health. This
[...] Read more.
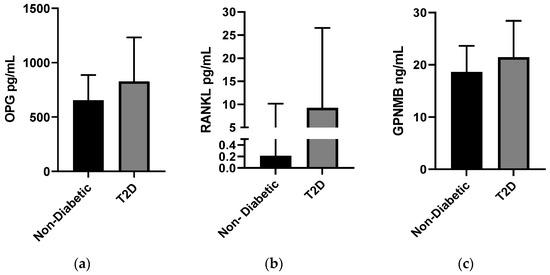
The global incidence of Type 2 diabetes (T2D) is on the rise, fueled by factors such as obesity, sedentary lifestyles, socio-economic factors, and ethnic backgrounds. T2D is a multifaceted condition often associated with various health complications, including adverse effects on bone health. This study aims to assess key biomarkers linked to bone health and remodeling—Osteoprotegerin (OPG), Receptor Activator of Nuclear Factor Kappa-Β Ligand (RANKL), and Glycoprotein Non-Metastatic Melanoma Protein B (GPNMB)—among individuals with diabetes while exploring the impact of ethnicity on these biomarkers. A cross-sectional analysis was conducted on a cohort of 2083 individuals from diverse ethnic backgrounds residing in Kuwait. The results indicate significantly elevated levels of these markers in individuals with T2D compared to non-diabetic counterparts, with OPG at 826.47 (405.8) pg/mL, RANKL at 9.25 (17.3) pg/mL, and GPNMB at 21.44 (7) ng/mL versus 653.75 (231.7) pg/mL, 0.21 (9.94) pg/mL, and 18.65 (5) ng/mL in non-diabetic individuals, respectively. Notably, this elevation was consistent across Arab and Asian populations, except for lower levels of RANKL observed in Arabs with T2D. Furthermore, a positive and significant correlation between OPG and GPNMB was observed regardless of ethnicity or diabetes status, with the strongest correlation (r = 0.473,
p < 0.001) found among Arab individuals with T2D. Similarly, a positive and significant correlation between GPNMB and RANKL was noted among Asian individuals with T2D (r = 0.401,
p = 0.001). Interestingly, a significant inverse correlation was detected between OPG and RANKL in non-diabetic Arab individuals. These findings highlight dysregulation in bone remodeling markers among individuals with T2D and emphasize the importance of considering ethnic variations in T2D-related complications. The performance of further studies is warranted to understand the underlying mechanisms and develop interventions based on ethnicity for personalized treatment approaches.
Full article
►▼
Show Figures
Open AccessArticle
Hepcidin Reduction during Testosterone Therapy in Men with Type 2 Diabetes: A Randomized, Double-Blinded, Placebo-Controlled Study
by
Line Velling Magnussen, Louise Helskov Jørgensen, Dorte Glintborg and Marianne Skovsager Andersen
Viewed by 903
Abstract
High hepcidin is linked to low-grade inflammation and lower iron levels. The consequences of testosterone replacement therapy (TRT) on inflammation and the risk of cardiovascular disease (CVD) are undetermined. We investigate the effect of TRT on the inflammatory cardiovascular risk markers hepcidin-iron, fibroblast
[...] Read more.
High hepcidin is linked to low-grade inflammation and lower iron levels. The consequences of testosterone replacement therapy (TRT) on inflammation and the risk of cardiovascular disease (CVD) are undetermined. We investigate the effect of TRT on the inflammatory cardiovascular risk markers hepcidin-iron, fibroblast growth factor 23 (FGF23)-phosphate-klotho, and calprotectin pathways. Methods: A randomized, placebo-controlled, double-blinded study at an academic tertiary-care medical center. Interventions were testosterone gel (TRT,
n = 20) or placebo gel (
n = 19) for 24 weeks. We included 39 men (50–70 years) with type 2 diabetes (T2D) on metformin monotherapy with bioavailable testosterone levels <7.3 nmol/L. Body composition was assessed with DXA- and MRI-scans; the main study outcomes were serum hepcidin-iron, FGF23, phosphate, klotho, and calprotectin. Results: Hepcidin levels decreased during TRT (β = −9.5 ng/mL,
p < 0.001), lean body mass (β = 1.9 kg,
p = 0.001) increased, and total fat mass (β = −1.3 kg,
p = 0.009) decreased compared to placebo. Delta hepcidin was not associated with changes in lean body mass or fat mass. Iron and the pathways of FGF23-phosphate-klotho and calprotectin were unchanged during TRT. Conclusions: During TRT, the reduction in hepcidin was not associated with circulating iron levels, lean body mass, or fat mass; these findings suggested a direct anti-inflammatory effect of TRT and no indirect effect mediated through these factors.
Full article
Open AccessArticle
Genetic Correlates as a Predictor of Bariatric Surgery Outcomes after 1 Year
by
Panayotis K. Thanos, Colin Hanna, Abrianna Mihalkovic, Aaron Hoffman, Alan Posner, John Butsch, Kenneth Blum, Lesley Georger, Lucy D. Mastrandrea and Teresa Quattrin
Cited by 1 | Viewed by 1330
Abstract
This study analyzed genetic risk assessments in patients undergoing bariatric surgery to serve as a predictive factor for weight loss parameters 1 year after the operation. Thirty (30) patients were assessed for Genetic Addiction Risk Severity (GARS), which analyzes neurogenetic polymorphisms involved in
[...] Read more.
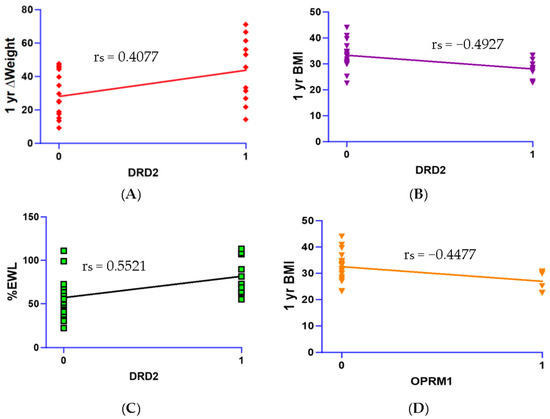
This study analyzed genetic risk assessments in patients undergoing bariatric surgery to serve as a predictive factor for weight loss parameters 1 year after the operation. Thirty (30) patients were assessed for Genetic Addiction Risk Severity (GARS), which analyzes neurogenetic polymorphisms involved in addiction and reward deficiency. Genetic and psychosocial data collected before the operation were correlated with weight loss data, including changes in weight, body mass index (BMI), and percent of expected weight loss (%EWL). Results examined correlations between individual gene risk alleles, 1-year body weight data, and psychosocial trait scores. Spearman’s correlations revealed that the
OPRM1 (rs1799971) gene polymorphism had significant negative correlation with 1-year weight (r
s = −0.4477,
p < 0.01) and BMI (r
s = −0.4477,
p < 0.05). In addition, the
DRD2 risk allele (rs1800497) was correlated negatively with BMI at 1 year (r
s = −0.4927,
p < 0.05), indicating that one risk allele copy was associated with lower BMI. However, this allele was positively correlated with both ∆Weight (r
s = 0.4077,
p < 0.05) and %EWL (r
s = 0.5521,
p < 0.05) at 1 year post-surgery. Moreover, the overall GARS score was correlated with %EWL (r
s = 0.4236,
p < 0.05), ∆Weight (r
s = 0.3971,
p < 0.05) and ∆BMI (r
s = 0.3778,
p < 0.05). Lastly, Food Cravings Questionnaire (FCQ) scores were negatively correlated with %EWL (r
s = −0.4320,
p < 0.05) and ∆Weight at 1 year post-surgery (r
s = −0.4294,
p < 0.05). This suggests that individuals with a higher genetic addiction risk are more responsive to weight loss treatment, especially in the case of the
DRD2 polymorphism. These results should translate clinically to improve positivity and attitude related to weight management by those individuals born with the risk alleles (rs1800497; rs1799971).
Full article
►▼
Show Figures
Open AccessArticle
Body Mass Index and Its Influence on Chronic Low Back Pain in the Spanish Population: A Secondary Analysis from the European Health Survey (2020)
by
María Orosia Lucha-López, César Hidalgo-García, Sofía Monti-Ballano, Sergio Márquez-Gonzalvo, Loreto Ferrández-Laliena, Julián Müller-Thyssen-Uriarte and Ana Carmen Lucha-López
Viewed by 1260
Abstract
Risk factors such as obesity and a sedentary lifestyle contribute to the development of chronic low back pain. Purpose: To describe how body mass index (BMI) influences the prevalence of chronic low back pain in the general Spanish population and assess this influence
[...] Read more.
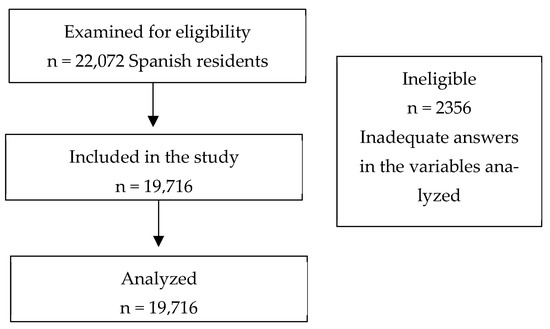
Risk factors such as obesity and a sedentary lifestyle contribute to the development of chronic low back pain. Purpose: To describe how body mass index (BMI) influences the prevalence of chronic low back pain in the general Spanish population and assess this influence given other factors as sex, age, physical occupational demands, and recreational physical activity. Methods: An analytical cross-sectional design was performed based on secondary data from the European Health Survey in Spain (2020). Data on age, gender, physical occupational demands, physical activity, BMI, and presence of chronic low back pain were extracted. Results: A total of 19,716 (52.2% women) subjects with a median age of 53 years old were analyzed. Of these, 18.3% had chronic low back pain, 39% were overweight, and 16.1% were obese. The adjusted generalized linear model showed that being obese increased the odds of chronic low back pain by 1.719 times (
p < 0.001). Being a woman increased the odds by 1.683 times (
p < 0.001). Performing occupational tasks requiring high physical demands increased the odds by 1.403 times (
p < 0.001). Performing physical activity in leisure time several times a week decreased the odds by 0.598 times (
p < 0.001). For every additional year of age, the odds of chronic low back pain increased by 3.3% (
p < 0.001). Conclusions: Obesity is related with the presence of chronic low back pain in the general Spanish population. This association persists, being the more relevant factor, after adjusting the association of BMI and chronic low back pain with other factors such as sex, age, physical occupational demands, and recreational physical activity.
Full article
►▼
Show Figures
Open AccessCase Report
An Uncommon Cause of Recurrent Presyncope, Dizziness, and Tachycardia: A Case Report of Diffuse, Adult-Onset Nesidioblastosis/Non-Insulinoma Pancreatogenous Hypoglycemia Syndrome (NIPHS)
by
Martin Philipp Dieterle, Ayman Husari, Sophie Nicole Prozmann, Hendrik Wiethoff, Albrecht Stenzinger, Manuel Röhrich, Uwe Pfeiffer, Wolfgang Rüdiger Kießling, Helena Engel, Harald Sourij, Thorsten Steinberg, Pascal Tomakidi, Stefan Kopf and Julia Szendroedi
Cited by 1 | Viewed by 1419
Abstract
Neurovegetative and autonomic symptoms are common presentations of various diseases, ranging from psychosomatic to severe organic disorders. A 23-year-old man presented with a history of recurrent presyncope, dizziness, and tachycardia. Repeated diagnostic work-up in various clinical settings could not identify any definite cause
[...] Read more.
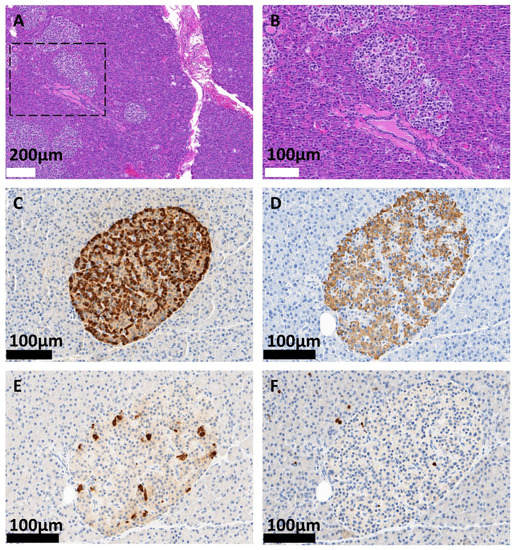
Neurovegetative and autonomic symptoms are common presentations of various diseases, ranging from psychosomatic to severe organic disorders. A 23-year-old man presented with a history of recurrent presyncope, dizziness, and tachycardia. Repeated diagnostic work-up in various clinical settings could not identify any definite cause for approximately eight years. However, the incidental detection of postprandial and exercise-induced hypoglycemia was suggestive of an insulin-related disorder. A 72 h plasma glucose fasting test revealed endogenous hyperinsulinism. Upon imaging studies, no tumor mass potentially indicating insulinoma could be detected.
68Ga-DOTA-Exendin-4 PET/CT showed diffuse tracer enrichment throughout the whole pancreas. A subtotal pancreatectomy was performed, and the diagnosis of diffuse, adult-onset nesidioblastosis was established histopathologically. This corresponds to the clinical findings of a functional β-cell disorder, also known as non-insulinoma pancreatogenous hypoglycemia syndrome (NIPHS). After nine months, the symptoms recurred, making complete pancreatectomy necessary. Postoperative laboratory evaluation exhibited no residual endogenous C-peptide production. This case illustrates the diagnostic challenges in patients presenting with unspecific, neurovegetative and autonomic symptoms with a severe and rare underlying cause.
Full article
►▼
Show Figures
Open AccessReview
Diffuse, Adult-Onset Nesidioblastosis/Non-Insulinoma Pancreatogenous Hypoglycemia Syndrome (NIPHS): Review of the Literature of a Rare Cause of Hyperinsulinemic Hypoglycemia
by
Martin Philipp Dieterle, Ayman Husari, Sophie Nicole Prozmann, Hendrik Wiethoff, Albrecht Stenzinger, Manuel Röhrich, Uwe Pfeiffer, Wolfgang Rüdiger Kießling, Helena Engel, Harald Sourij, Thorsten Steinberg, Pascal Tomakidi, Stefan Kopf and Julia Szendroedi
Cited by 3 | Viewed by 3220
Abstract
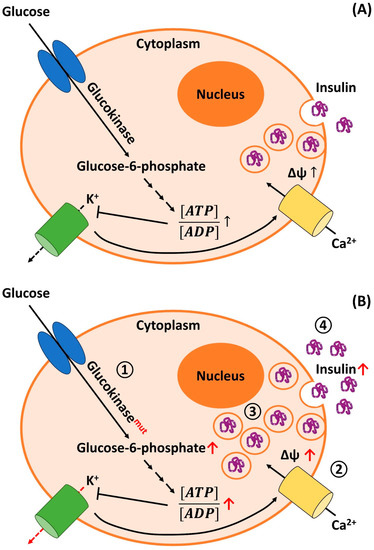
Differential diagnosis of hypoglycemia in the non-diabetic adult patient is complex and comprises various diseases, including endogenous hyperinsulinism caused by functional β-cell disorders. The latter is also designated as nesidioblastosis or non-insulinoma pancreatogenous hypoglycemia syndrome (NIPHS). Clinically, this rare disease presents with unspecific
[...] Read more.
Differential diagnosis of hypoglycemia in the non-diabetic adult patient is complex and comprises various diseases, including endogenous hyperinsulinism caused by functional β-cell disorders. The latter is also designated as nesidioblastosis or non-insulinoma pancreatogenous hypoglycemia syndrome (NIPHS). Clinically, this rare disease presents with unspecific adrenergic and neuroglycopenic symptoms and is, therefore, often overlooked. A combination of careful clinical assessment, oral glucose tolerance testing, 72 h fasting, sectional and functional imaging, and invasive insulin measurements can lead to the correct diagnosis. Due to a lack of a pathophysiological understanding of the condition, conservative treatment options are limited and mostly ineffective. Therefore, nearly all patients currently undergo surgical resection of parts or the entire pancreas. Consequently, apart from faster diagnosis, more elaborate and less invasive treatment options are needed to relieve the patients from the dangerous and devastating symptoms. Based on a case of a 23-year-old man presenting with this disease in our department, we performed an extensive review of the medical literature dealing with this condition and herein presented a comprehensive discussion of this interesting disease, including all aspects from epidemiology to therapy.
Full article
►▼
Show Figures
Open AccessReview
Role of Melatonin in the Onset of Metabolic Syndrome in Women
by
Vania Miloucheva Peneva, Dora Dimitrova Terzieva and Mitko Dimitrov Mitkov
Cited by 1 | Viewed by 1495
Abstract
Metabolic syndrome (MetS) is a constellation of several associated cardiometabolic risk factors that increase the risk of developing type 2 diabetes mellitus (T2DM), cardiovascular diseases, and mortality. The role of hormonal factors in the development of MetS is assumed. In women, an insulin-resistant
[...] Read more.
Metabolic syndrome (MetS) is a constellation of several associated cardiometabolic risk factors that increase the risk of developing type 2 diabetes mellitus (T2DM), cardiovascular diseases, and mortality. The role of hormonal factors in the development of MetS is assumed. In women, an insulin-resistant state that is associated with polycystic ovarian syndrome and increased deposition of intra-abdominal adipose tissue promotes the development of MetS and increases cardiovascular risk. The neuroendocrine hormone melatonin is secreted mainly at night under the regulatory action of the suprachiasmatic nucleus in the hypothalamus. Melatonin secretion is influenced by exogenous factors such as light and seasons and endogenous factors such as age, sex, and body weight. At present, the role of melatonin in metabolic disorders in humans is not fully understood. In this review, we set out to analyze the relationship of melatonin with the main features of MetS in women. Data from experimental and clinical studies on the role of melatonin in glucose metabolism and on the involvement of melatonin in lipid disturbances in MetS are reviewed. The complex influence of melatonin on hypertension is discussed. The changes in melatonin, leptin, and ghrelin and their relation to various metabolic processes and vascular dysfunction are discussed.
Full article
Open AccessArticle
A High-Quality Diet, as Measured by the DASH Score, Is Associated with a Lower Risk of Metabolic Syndrome and Visceral Obesity
by
Klaudia Konikowska, Wojciech Bombała, Andrzej Szuba, Dorota Różańska and Bożena Regulska-Ilow
Cited by 4 | Viewed by 2284
Abstract
The current study was designed to examine the relationship between diet quality, as measured by the Dietary Approaches to Stop Hypertension (DASH) score, and the prevalence of metabolic syndrome (MetS) and its components. The study was cross-sectional in design and enrolled 535 people,
[...] Read more.
The current study was designed to examine the relationship between diet quality, as measured by the Dietary Approaches to Stop Hypertension (DASH) score, and the prevalence of metabolic syndrome (MetS) and its components. The study was cross-sectional in design and enrolled 535 people, including 215 with MetS and 320 without MetS. Using a validated food frequency questionnaire, the DASH diet quality score was counted. The mean age of the MetS group and control subjects was 58.48 ± 14.65 and 58.33 ± 9.26 years, respectively. The study showed that the MetS group had a significantly lower mean total DASH score than the control group (23.13 ± 5.44 vs. 24.62 ± 5.07,
p = 0.0023). In addition, it was found that an increase in the total DASH score was associated with a lower risk of MetS (odds ratio [OR] = 0.95, 95% confidence interval [CI] = 0.91–0.99,
p = 0.009). In the correlation analysis of the total population, a better-quality diet (higher DASH score) was positively correlated with high-density lipoprotein cholesterol (HDL-c), and negatively correlated with triglyceride (TG) concentration and waist circumference. It was also found that an increase in the total DASH score was associated with a lower risk of abdominal obesity (OR = 0.93, 95% CI = 0.88–0.99,
p = 0.017). The results from the analyzed data highlight the potential benefits of following a healthy diet such as DASH.
Full article
Open AccessArticle
Evaluation of Lipid Peroxidation in the Saliva of Diabetes Mellitus Type 2 Patients with Periodontal Disease
by
Jelena Mirnic, Milanko Djuric, Tanja Veljovic, Ivana Gusic, Jasmina Katanic, Karolina Vukoje, Bojana Ramic, Ana Tadic and Snezana Brkic
Cited by 3 | Viewed by 1232
Abstract
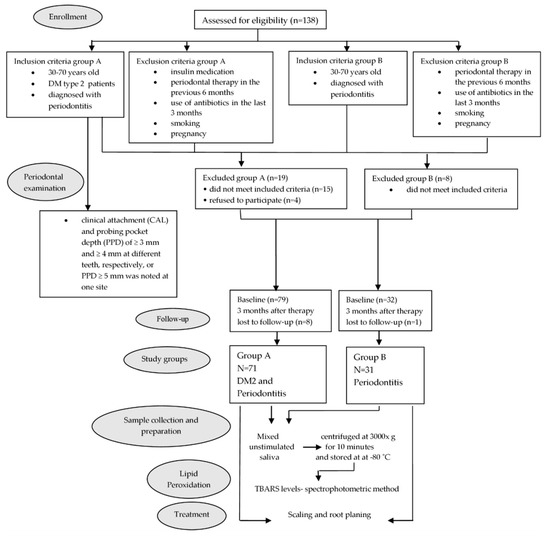
As oxidative stress has been implicated in the pathogenesis of diabetes mellitus and periodontitis, it may serve as a link between these conditions. Therefore, as a part of the present study, salivary lipid peroxidation (LP) in periodontitis patients with and without diabetes mellitus
[...] Read more.
As oxidative stress has been implicated in the pathogenesis of diabetes mellitus and periodontitis, it may serve as a link between these conditions. Therefore, as a part of the present study, salivary lipid peroxidation (LP) in periodontitis patients with and without diabetes mellitus type 2 (DM2) was evaluated, along with the periodontal therapy effectiveness. The study sample comprised of 71 DM2 patients with periodontitis and 31 systemically healthy controls suffering from periodontitis of comparable severity. In all participants, periodontal indices—plaque index (PI), gingival index (GI), papilla bleeding index (PBI), probing pocket depth (PPD), and clinical attachment level (CAL)—were recorded, and salivary LP was measured using a spectrophotometric method prior to treatment initiation and three months post-treatment. At baseline, mean salivary LP in DM2 patients was higher than that measured for the control group, but the difference did not reach statistical significance (
p > 0.05), whereas a positive significant correlation was found between PPD and LP in both groups. Three months after nonsurgical periodontal therapy, clinical periodontal parameters and salivary LP levels were significantly reduced in both groups (
p < 0.05). These findings indicate that the improvement in clinical periodontal status following nonsurgical periodontal therapy is accompanied by a significant decrease in salivary LP in DM2 patients, suggesting that periodontitis, rather than diabetes, is the primary driver of the elevated salivary LP in this group.
Full article
►▼
Show Figures