Breast Cancer—Therapeutic Challenges, Research Strategies and Novel Diagnostics
A topical collection in Cancers (ISSN 2072-6694). This collection belongs to the section "Cancer Therapy".
Viewed by 42053Editor
Topical Collection Information
Dear Colleagues,
Thanks to the breast cancer research of recent decades, effective methods and strategies have been established, allowing the mortality rates of breast cancer patients to decrease more and more.
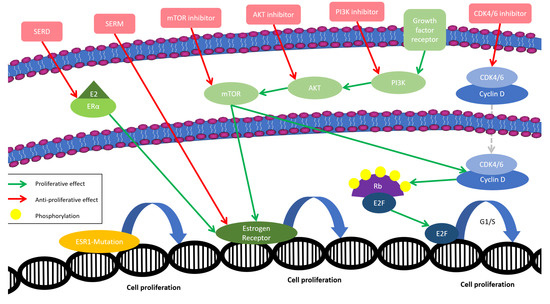
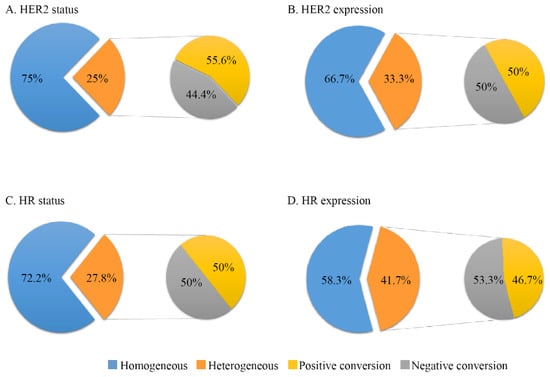
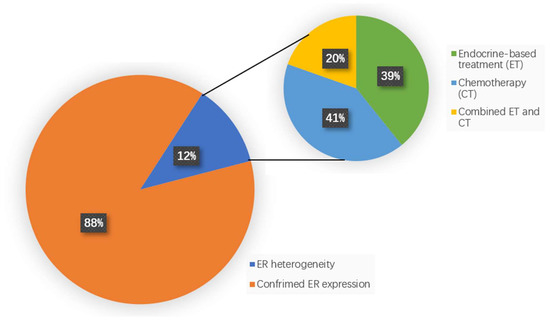
Compared with other subtypes, triple-negative breast cancer remains one of the most aggressive cancers. However, modern therapeutics, such as immune checkpoint inhibitors and antibody–drug conjugates, are currently changing the treatment landscape of this disease. In HER2-positive breast cancer patients, who had once been patients with an extremely poor prognosis, targeted therapies have reduced mortality rates immensely. Research has gone so far that, even decades after the discovery of the HER2 receptor, its differentiation to zero, low or positive has gained importance, as this is another target option for specific novel treatments. Additionally, when it comes to hormone-receptor-positive breast cancer, it is the class of CDK4/6 inhibitors that—after almost half a century of single-endocrine treatment—has changed usual treatment patterns, and was the first to be successfully combined even in the early therapy stage.
Despite all these advancements, we still face many challenges in breast cancer research.
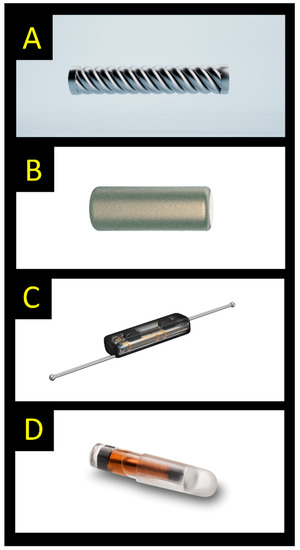
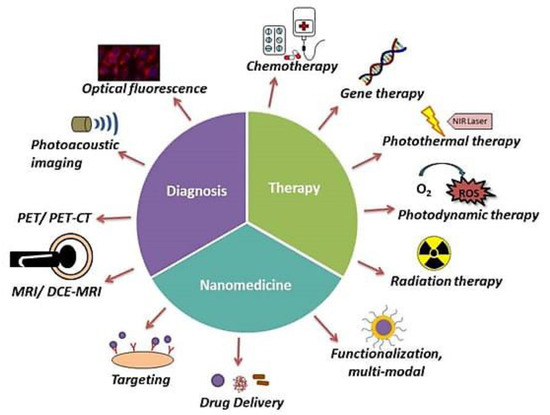
On a molecular basis, the role of intrinsic subtypes, certain biomarkers or mutations is still not clear for treatment and surveillance. Novel drugs, including those mentioned above, are often associated with a different spectrum of adverse events than that seen for conventional therapies, accordingly having an impact on patients’ compliance behaviors. In breast cancer surgery, in some cases, the question remains of whether to escalate or to deescalate. Additionally, with regard to diagnostics, in a digitalized world, artificial intelligence, home-based tools and therapy monitoring options are of high importance, especially after conditions seen during the COVID-19 pandemic and supply problems.
The aim is to gather original research articles and reviews demonstrating therapeutic challenges, research strategies and novel diagnostics in breast cancer.
Dr. Naiba Nabieva
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cancers is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2900 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- breast cancer
- chemotherapy
- targeted therapy
- breast surgery
- irradiation
- adherence
- compliance
- side effects
- digital health solution
Planned Papers
The below list represents only planned manuscripts. Some of these manuscripts have not been received by the Editorial Office yet. Papers submitted to MDPI journals are subject to peer-review.
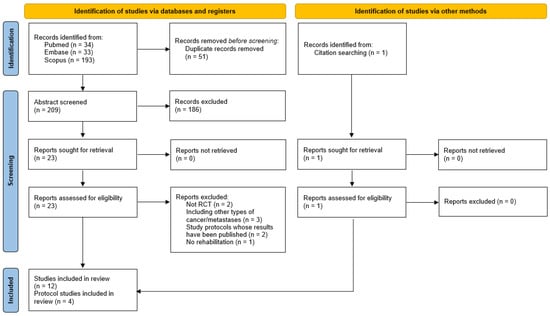
Title: Cognitive impairment and rehabilitation in breast cancer patients treated with endocrine therapies.
Authors: Pierfranco Conte
Affiliation: Università degli Studi di Padova, Padua, Italy
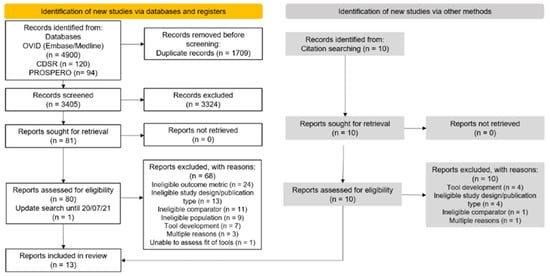
Title: Breast preservation after local recurrence of breast cancer: Comparison of length and quality of life (QoL) between breast conserving surgery with intraoperative radiotherapy (TARGIT-IORT) versus mastectomy
Authors: Kolberg
Affiliation: Clincs of Bottrop