Establishing Smoke-Free Homes in the Indigenous Populations of Australia, New Zealand, Canada and the United States: A Systematic Literature Review
Abstract
:1. Introduction
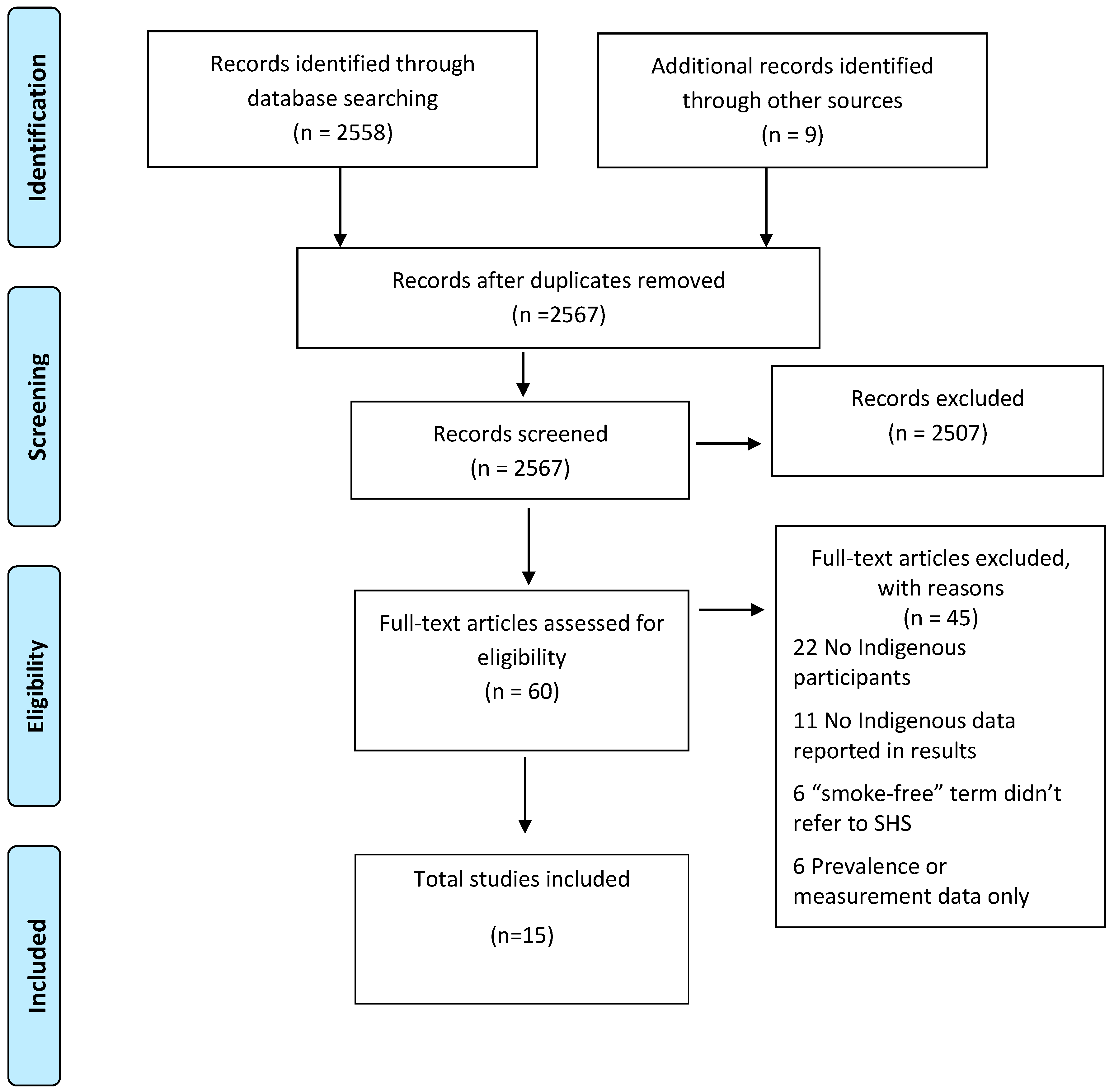
2. Methods
2.1. Search Terms
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Data Extraction and Synthesis
3. Results
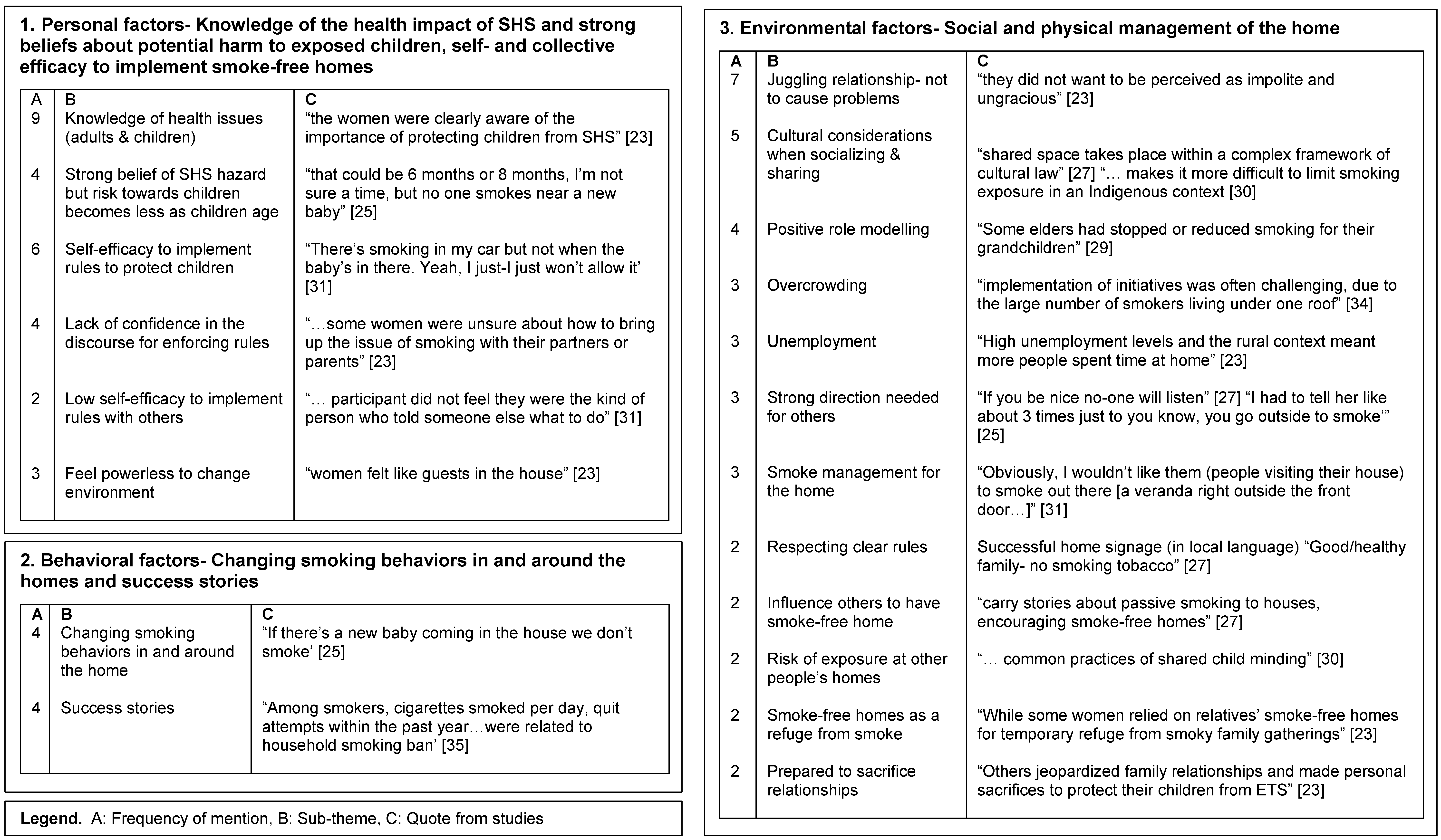
3.1. Personal Factors—Knowledge of the Health Impact of SHS, Strong Beliefs about Potential Harm to Exposed Children and Self-Efficacy and Collective Efficacy to Manage Smoke-Free Homes
Self- and Collective Efficacy
3.2. Behavioral Factors—Changing Smoking Behaviors in and around the Home and Success Stories
3.2.1. Changing Smoking Behaviors in and around the Home
3.2.2. Success Stories
3.3. Environmental Factors—Social and Physical Management of the Home
3.3.1. Relationships
3.3.2. Communicating Smoke-Free Rules
3.3.3. Role Modelling
3.3.4. Physical Management of SHS in the Home
3.3.5. Socio-Economic Issues
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- U.S. Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, GA, USA, 2006.
- Thomas, D.; Stevens, M. Aboriginal and Torres Strait Islander smoke-free homes, 2002 to 2008. Aust. N. Z. J. Public Health 2014, 38, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. The Health of New Zealand Adults 2011/2012: Key Findings of the New Zealand Health Survey; Ministry of Health: Wellington, New Zealand, 2012.
- Singh, G.; Siahpush, M.; Kogan, M.D. Disparities in children’s exposure to environmental tobacco smoke in the United States, 2007. Pediatrics 2010, 126, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Gionet, L.; Roshanafshar, S. Select Health Indicators of First Nations People Living off Reserve, Metis and Inuit. Available online: http://www.statcan.gc.ca/pub/82-624-x/2013001/article/11763-eng.pdf (accessed on 8 August 2017).
- Reid, J.; Hammond, D.; Rynard, V.; Burkalter, R. Tobacco Use in Canada: Patterns and Trends, 2015 Edition; Propel Centre for Population Health Impact University of Waterloo: Waterloo, ON, Canada, 2015. [Google Scholar]
- Ministry of Health. Annual Update of Key Results 2015/2016: New Zealand Health Survey; Ministry of Health: Wellington, New Zealand, 2016.
- Australian Bureau of Statistics. Australian Aboriginal and Torres Strait Islander Health Survey: First Results, Australia, 2012–2013. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/mf/4727.0.55.001 (accessed on 8 August 2017).
- Reading, C.L.; Wien, F. Health Inequalities and Social Determinants of Aboriginal Peoples’ Health; National Collaborating Centre for Aboriginal Health: Prince George, BC, Canada, 2009. [Google Scholar]
- Jamal, A.; Homa, D.; O’Connor, E.; Babb, S.; Caraballo, R.; Singh, T.; Hu, S.; King, B. Current cigarette smoking among adults—United States, 2005–2014. MMWR Morb. Mortal. Wkly. Rep. 2015, 64, 1233–1240. [Google Scholar] [CrossRef] [PubMed]
- Kunitz, S.J. Disease and Social Diversity: The European Impact on the Health of Non-Europeans; Oxford University Press: New York, NY, USA, 1996. [Google Scholar]
- Borland, R.; Yong, H.; Cummings, K.; Hyland, A.; Anderson, S.; Fong, G. Determinants and consequences of smoke-free homes: Findings from the International Tobacco Control (ITC) Four Country Survey. Tob. Control 2006, 15, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Gilpin, E.A.; White, M.M.; Farkas, A.J.; Pierce, J.P. Home smoking restrictions: Which smokers have them and how they are associated with smoking behavior. Nicotine Tob. Res. 1999, 1, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Berg, C.J.; An, L.C.; Kirch, M.; Guo, H.; Thomas, J.L.; Patten, C.A.; Ahluwalia, J.S.; West, R. Failure to report attempts to quit smoking. Addict. Behav. 2010, 35, 900–904. [Google Scholar] [CrossRef] [PubMed]
- Emory, K.; Saquib, N.; Gilpin, E.A.; Pierce, J.P. The association between home smoking restrictions and youth smoking behaviour: A review. Tob. Control 2010, 19, 495–506. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Social Learning Theory; Prentice-Hall: Englewood Cliffs, NJ, USA, 1977. [Google Scholar]
- Bandura, A. Social cognitive theory in cultural context. Appl. Psychol. 2002, 51, 269–290. [Google Scholar] [CrossRef]
- Cragg, L.; Davies, M.; Macdowall, W. Health Promotion Theory; McGraw-Hill Education: Maidenhead, UK, 2013. [Google Scholar]
- Borland, R. Theories of Behavior Change in Relation to Environmental Tobacco Smoke Control to Protect Children. 1999. Available online: http://www.who.int/tobacco/media/en/borland.pdf (accessed on 8 August 2017).
- Johnston, V.; Walker, N.; Thomas, D.P.; Glover, M.; Chang, A.B.; Bullen, C.; Morris, P.; Brown, N.; Vander Hoorn, S.; Borland, R.; et al. The study protocol for a randomized controlled trial of a family-centred tobacco control program about environmental tobacco smoke (ETS) to reduce respiratory illness in Indigenous infants. BMC Public Health 2010, 10, 114. [Google Scholar] [CrossRef] [PubMed]
- Kegler, M.; Escoffery, C.; Groff, A.; Butler, S.; Foreman, A. A qualitative study of how families decide to adopt household smoking restrictions. Fam. Community Health 2007, 30, 328–341. [Google Scholar] [CrossRef] [PubMed]
- Glover, M.; Paynter, J.; Wong, G.; Scragg, R.; Nosa, V.; Freeman, B. Parental attitudes towards the uptake of smoking by children. Health Promot. J. Aust. 2006, 17, 128–133. [Google Scholar]
- Bottorff, J.L.; Johnson, J.L.; Carey, J.; Hutchinson, P.; Sullivan, D.; Mowatt, R.; Wardman, D. A family affair: Aboriginal women’s efforts to limit second-hand smoke exposure at home. Can. J. Public Health 2010, 101, 32–35. [Google Scholar] [PubMed]
- Glover, M.; Kira, A.; Faletau, J. Smoke, smoking and cessation: The views of children with respiratory illness. J. Asthma 2013, 50, 722–728. [Google Scholar] [CrossRef] [PubMed]
- Gould, G.; Munn, J.; Avuri, S.; Hoff, S.; Cadet-James, Y.; McEwen, A.; Clough, A. “Nobody smokes in the house if there’s a new baby in it”: Aboriginal perspectives on tobacco smoking in pregnancy and in the household in regional NSW Australia. Women Birth 2013, 26, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Johnston, V.; Thomas, D.P.; McDonnell, J.; Andrews, R.M. Maternal smoking and smoking in the household during pregnancy and postpartum: Findings from an Indigenous cohort in the Northern Territory. Med. J. Aust. 2011, 194, 556–559. [Google Scholar] [PubMed]
- Robertson, J.; Pointing, B.S.; Stevenson, L.; Clough, A.R. “We made the rule, we have to stick to it”: Towards effective management of environmental tobacco smoke in remote Australian Aboriginal communities. Int. J. Environ. Res. Public Health 2013, 10, 4944–4966. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, L.C.; Bohanna, I.; Robertson, J.A.; Clough, A.R. Aboriginal people in remote communities in Arnhem land (Northern Territory) restrict their smoking in some environments: Implications for developing and implementing interventions to reduce exposure to environmental tobacco smoke. Drug Alcohol Rev. 2013, 32, 627–630. [Google Scholar] [CrossRef] [PubMed]
- Varcoe, C.; Bottorff, J.L.; Carey, J.; Sullivan, D.; Williams, W. Wisdom and influence of elders: Possibilities for health promotion and decreasing tobacco exposure in First Nations communities. Can. J. Public Health 2010, 101, 154–158. [Google Scholar] [PubMed]
- Wood, L.; France, K.; Hunt, K.; Eades, S.; Slack-Smith, L. Indigenous women and smoking during pregnancy: Knowledge, cultural contexts and barriers to cessation. Soc. Sci. Med. 2008, 66, 2378–2389. [Google Scholar] [CrossRef] [PubMed]
- Glover, M.; Kira, A.; Johnston, V.; Walker, N.; Brown, N.; Thomas, D. Australian and New Zealand Indigenous mothers’ report respect for smoking bans in homes. Women Birth 2015, 28, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Arjunan, P.; Poder, N.; Welsh, K.; Bellear, L.; Heathcote, J.; Wright, D.; Millen, E.; Spinks, M.; Williams, M.; Wen, L.M. Smoking among Aboriginal adults in Sydney, Australia. Health Promot. J. Aust. 2016, 27, 66–69. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, J.; Milne, K.; Wilson, N. Secondhand smoke in New Zealand homes and cars: Exposure, attitudes, and behaviours in 2004. N. Z. Med. J. 2005, 118, U1782. [Google Scholar] [PubMed]
- Johnston, V.; Thomas, D.P. Smoking behaviours in a remote Australian Indigenous community: The influence of family and other factors. Soc. Sci. Med. 2008, 67, 1708–1716. [Google Scholar] [CrossRef] [PubMed]
- Kegler, M.C.; Malcoe, L.H. Smoking restrictions in the home and car among rural Native American and white families with young children. Prev. Med. 2002, 35, 334–342. [Google Scholar] [CrossRef] [PubMed]
- Walker, N.; Johnston, V.; Glover, M.; Bullen, C.; Trenholme, A.; Chang, A.; Morris, P.; Segan, C.; Brown, N.; Fenton, B.D. Effect of a family-centered, secondhand smoke intervention to reduce respiratory illness in Indigenous infants in Australia and New Zealand: A randomized controlled trial. Nicotine Tob. Res. 2015, 17, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Keleher, H.; Murphy, B.; MacDougall, C. Understanding Health Promotion; Oxford University Press: Oxford, UK, 2007. [Google Scholar]
- Hovell, M.F.; Zakarian, J.M.; Wahlgren, D.R.; Matt, G.E. Reducing children’s exposure to environmental tobacco smoke: The empirical evidence and directions for future research. Tob. Control 2000, 9, ii40–ii47. [Google Scholar] [CrossRef] [PubMed]
- Passey, M.E.; Longman, J.M.; Robinson, J.; Wiggers, J.; Jones, L.L. Smoke-free homes: What are the barriers, motivators and enablers? A qualitative systematic review and thematic synthesis. BMJ Open 2016, 6, e010260. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Health promotion from the perspective of social cognitive theory. Psychol. Health 1998, 13, 623–649. [Google Scholar] [CrossRef]
- Mungabbareena Aboriginal Corporation and Women’ Health Goulburn North East. Using a Health Promotion Framework with an ‘Aboriginal Lens’. 2008. Available online: http://www.whealth.com.au/mtww/documents/MTWW_Health-Promotion-Framework.pdf (accessed on 14 September 2017).
| Study (First Author, Year) [Ref] | Location of Study by Country and Region as Described by Authors | Method | Sample | Total Participants N | Indigenous Participants N | Focus of Study |
|---|---|---|---|---|---|---|
| Arjunan et al., 2016 [32] | Australia Sydney | Quantitative—survey of Aboriginal community members | Community members | 663 | 663 | Associated factors with smoking, cessation behaviors and attitudes towards smoke-free homes. Indigenous specific focus |
| Bottorff et al., 2010 [23] | Canada Reserve | Qualitative—focus groups | Pregnant women, key informants, elders, youth | 63 | 63 | Explore what influences smoking bans in the home. Indigenous specific focus |
| Gillespie et al., 2005 [33] | New Zealand National | Quantitative—population telephone survey | Women, men | 2731 | 924 | Assess passive smoking exposure in homes and cars, and describe attitudes and behaviors towards smoke-free settings. Mixed ethnic population |
| Glover et al., 2006 [22] | New Zealand Auckland | Qualitative—focus groups and in-depth interviews | Parents and caregivers | 61 | 6 | Investigate parental attitudes and behaviors regarding their children’s uptake of smoking. Indigenous specific focus |
| Glover et al., 2013 [24] | New Zealand Auckland, Wellington | Qualitative—focus groups and in-depth interviews | Children | 41 | 27 | Describe attitudes of children with respiratory illness towards passive smoking, smoking and parental cessation. Mixed population |
| Glover et al., 2015 [31] | Australia & New Zealand Darwin & Auckland | Qualitative—semi-structured interviews nested within a randomized controlled trial | Mothers | 26 | 26 | Understand smoke-free rules around infants. Indigenous specific focus—Maori and Aboriginal |
| Gould et al., 2013 [25] | Australia Regional New South Wales | Qualitative—focus groups | Pregnant women, partners/family | 18 | 18 | Describe women’s and family-members’ attitudes and experiences of prenatal tobacco smoking and household smoking. Indigenous specific focus |
| Johnston & Thomas 2008 [34] | Australia Remote Northern Territory | Qualitative—semi-structured interviews | Community members, health staff | 38 | 29 | Understand motivators of smoking uptake, routine smoking behavior and motivators and issues related to quitting. Indigenous specific focus |
| Johnston et al., 2011 [26] | Australia Darwin & Remote Northern Territory | Quantitative—cross-sectional survey | Post-partum women | 215 | 215 | Describe trends in maternal smoking and smoking in the home. Indigenous specific focus |
| Kegler et al., 2002 [35] | United States Rural | Quantitative—in-home survey | Parents/ caregivers | 380 | 167 | Understand household and car smoking restrictions in low-income, rural Native American and White households with young children. Native American and white parents or guardians participated. |
| Robertson et al., 2013 [27] | Australia Remote Northern Territory | Multi-methods—community surveys, focus groups and in-depth interviews | Key informants, community members, health staff | 400 | 400 | Describe a grass-roots response to passive smoking in the community setting. Indigenous specific focus |
| Stevenson et al., 2013 [28] | Australia Remote Northern Territory | Quantitative—community survey | Community members | 258 | 258 | Comparison of those who restrict smoking in the home, car and workplace, and those who do not. Indigenous specific focus |
| Varcoe et al., 2010 [29] | Canada Rural reserve | Qualitative—individual, group interviews | Key informants | 66 | 66 | Describe influences on smoking practices and SHS exposure with a focus on pregnancy and children. Indigenous specific |
| Walker et al., 2015 [36] | Australia & New Zealand Darwin/Greater Darwin & Manukau region | Quantitative—data collection in participant homes | Mother/infant dyads | 228 | 228 | Evaluate a smoke-free intervention with acute respiratory related visits to a health care provider in the infant’s first year of life as the main outcome measure. Indigenous specific focus—Both Maori and Aboriginal |
| Wood et al., 2008 [30] | Australia Perth | Qualitative—focus groups and in-depth interviews | Pregnant women & health workers | 50 | 50 | Investigate the cultural context of tobacco smoking relating to smoking in pregnancy. Indigenous specific focus |
| SCT | Themes | Recommendations for Policy and Practice |
|---|---|---|
| Personal factors | Knowledge of the health impact of SHS and strong beliefs about potential harm to exposed to children Self and collective efficacy to implement smoke-free homes | Strategies to support families transfer knowledge of the importance of SFH into practice by supporting individuals and families develop a discourse to help with the decision-making process for implementing smoke-free homes Health promotion messages co-developed with Indigenous communities can be positively framed as family and community interventions. |
| Behavioral factors | Smoking behaviors in and round the home Success stories | Identifying change agents and leaders in the community to role model and promote smoke-free home behaviors Narrative and video-based media to promote success stories |
| Environmental factors | Social and physical management of the home | Understanding decision-making processes, and the power structure of relationships within family homes may improve the development of smoke-free home intervention strategies Future qualitative and quantitative research could explore the how to build self and collective efficacy in the decision-making processes for implementing smoke-free homes in Indigenous community setting, rather than focusing only on the individual smoker |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stevenson, L.; Campbell, S.; Bohanna, I.; Gould, G.S.; Robertson, J.; Clough, A.R. Establishing Smoke-Free Homes in the Indigenous Populations of Australia, New Zealand, Canada and the United States: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2017, 14, 1382. https://doi.org/10.3390/ijerph14111382
Stevenson L, Campbell S, Bohanna I, Gould GS, Robertson J, Clough AR. Establishing Smoke-Free Homes in the Indigenous Populations of Australia, New Zealand, Canada and the United States: A Systematic Literature Review. International Journal of Environmental Research and Public Health. 2017; 14(11):1382. https://doi.org/10.3390/ijerph14111382
Chicago/Turabian StyleStevenson, Leah, Sandy Campbell, India Bohanna, Gillian S. Gould, Jan Robertson, and Alan R. Clough. 2017. "Establishing Smoke-Free Homes in the Indigenous Populations of Australia, New Zealand, Canada and the United States: A Systematic Literature Review" International Journal of Environmental Research and Public Health 14, no. 11: 1382. https://doi.org/10.3390/ijerph14111382
APA StyleStevenson, L., Campbell, S., Bohanna, I., Gould, G. S., Robertson, J., & Clough, A. R. (2017). Establishing Smoke-Free Homes in the Indigenous Populations of Australia, New Zealand, Canada and the United States: A Systematic Literature Review. International Journal of Environmental Research and Public Health, 14(11), 1382. https://doi.org/10.3390/ijerph14111382





