International Differences in Outpatient Pain Management: A Survey of Sickle Cell Disease
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Outpatient
3.2. Outpatient Quantity
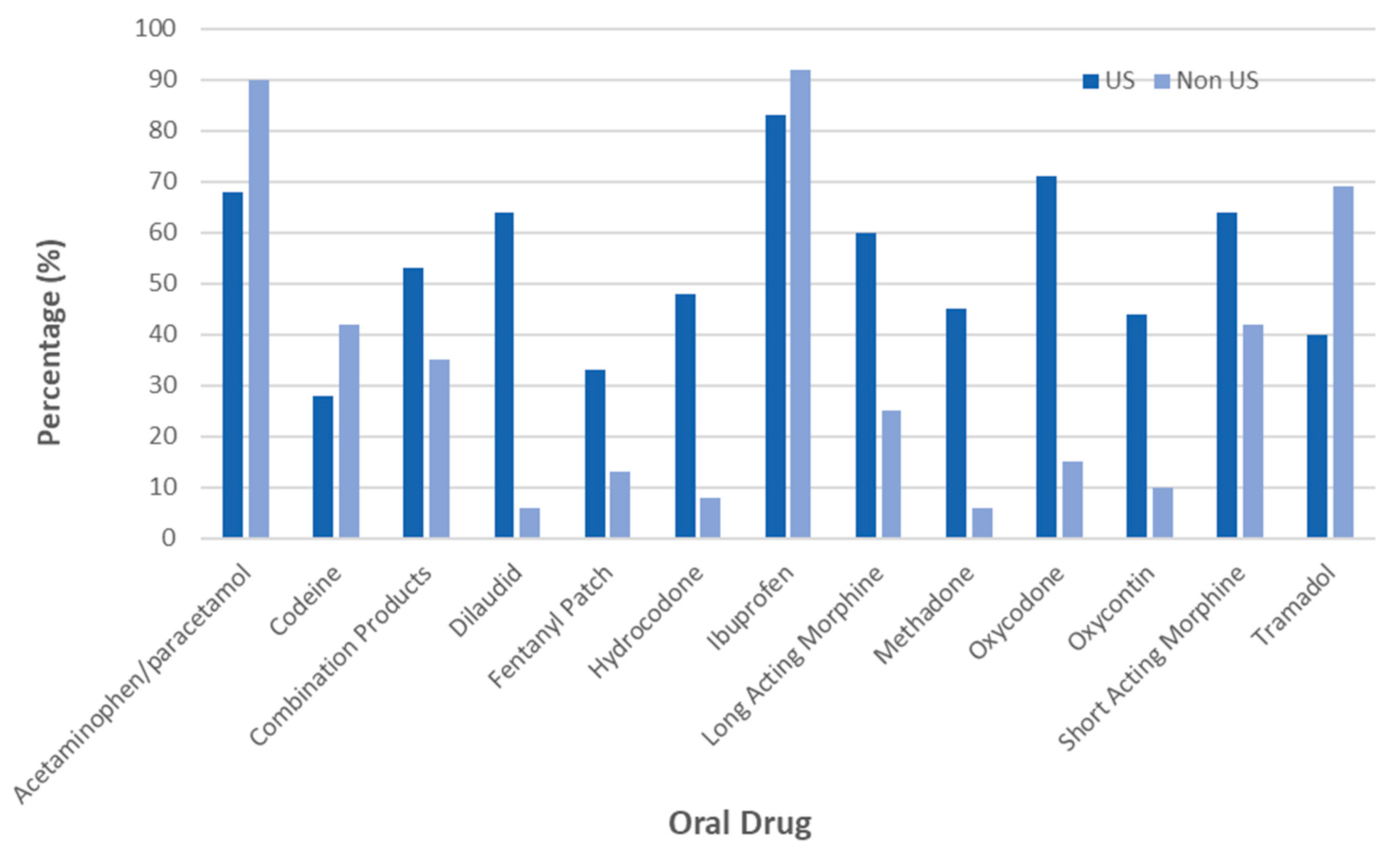
3.3. Outpatient Pain Medication Type
3.4. Inpatient
3.5. Opioid Misuse/Abuse
3.6. Disease-Modifying Therapy
3.7. Pediatric vs. Adult Providers
4. Discussion
Author Contributions
Funding
Conflicts of Interest
Appendix A
References
- Brousseau, D.C.; Owens, P.L.; Mosso, A.L.; Panepinto, J.A.; Steiner, C.A. Acute care utilization and rehospitalizations for sickle cell disease. JAMA 2010, 303, 1288–1294. [Google Scholar] [CrossRef]
- Platt, O.S.; Thorington, B.D.; Brambilla, D.J.; Milner, P.F.; Rosse, W.F.; Vichinsky, E.; Kinney, T.R. Pain in sickle cell disease. Rates and risk factors. N. Engl. J. Med. 1991, 325, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Kauf, T.L.; Coates, T.D.; Huazhi, L.; Mody-Patel, N.; Hartzema, A.G. The cost of health care for children and adults with sickle cell disease. Am. J. Hematol. 2009, 84, 323–327. [Google Scholar] [CrossRef] [PubMed]
- Lanzkron, S.; Carroll, C.P.; Haywood, C. The burden of emergency department use in sickle cell disease: an analysis of the national emergency database sample department. Am. J. Hematol. 2010, 85, 797–799. [Google Scholar] [CrossRef] [PubMed]
- Dampier, C.; Ely, E.; Brodecki, D.; Oneal, P. Home management of pain in sickle cell disease: A daily diary study in children and adolescents. J. Pediatr. Hematol. Oncol. 2002, 24, 643–647. [Google Scholar] [CrossRef] [PubMed]
- National Lung, Heart and Blood Institute. Evidence Based Management of Sickle Cell Disease: Expert Panel Report; National Heart, Lung, and Blood Institute: Bethesda, MD, USA; US Department of Health and Human Services: Washington, DC, USA, 2014.
- Sickle Cell Society. Standards for the Clinical Care of Adults with Sickle Cell Disease in the UK, 2nd ed.; University of York Design and Print: Heslington, UK, 2018. [Google Scholar]
- Food and Drug Administration. American Society of Hematology-Sickle Cell Disease Clinical Endpoints Workshop; Food and Drug Administration: Rockville, MD, USA, 2018. [Google Scholar]
- Pack-Mabien, A.; Labbe, E.; Herbert, D.; Haynes, J., Jr. Nurses’ attitudes and practices in sickle cell pain management. Appl. Nurs. Res. 2001, 14, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Bulgin, D.; Tabe, P.; Jenerette, C. Stigma of sickle cell disease: A systematic review. Issues Ment. Health Nurs. 2018, 39, 675–686. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, L.J.; Dampier, C.D.; Jacox, A.; Odesina, V.; Phoenix, D.; Shapiro, B. Guideline for the Management of Acute and Chronic Pain in Sickle Cell Disease; American Pain Society Clinical Practice Guidelines Series, No. 1; American Pain Society: Glenview, IL, USA, 1999. [Google Scholar]
- Mathias, M.D.; McCavit, T.L. Timing of opioid administration as a quality indicator for pain crises in sickle cell disease. Pediatrics 2015, 135, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Smith, W.R.; McClish, D.K.; Dahman, B.A.; Levenson, J.L.; Aisiku, I.P. Daily home opioid use in adults with sickle cell disease: The PiSCES project. J. Opioid Manag. 2015, 11, 243–253. [Google Scholar] [CrossRef] [PubMed]
- Smith, W.R.; Penberthy, L.T.; Bovbjerg, V.E.; McClish, D.K.; Roberts, J.D.; Dahman, B.; Roseff, S.D. Daily assessment of pain in adults with sickle cell disease. Ann. Intern. Med. 2008, 148, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Ballas, S.K.; Bauserman, R.L.; McCarthy, W.F.; Castro, O.L.; Smith, W.R.; Waclawiw, M.A. Hydroxyurea and acute painful crises in sickle cell anemia: Effects on hospital length of stay and opioid utilization during hospitalization, outpatient, acute care contacts and at home. J. Pain Symptom Manag. 2010, 60, 870–883. [Google Scholar] [CrossRef] [PubMed]
- Heeney, M.M.; Hoppe, C.C.; Abboud, M.R.; Inusa, B.; Kanter, J.; Ogutu, B.; Zamoryakhin, D. A multinational trial of prasugrel for sickle cell vaso-occlusive events. N. Engl. J. Med. 2016, 374, 625–635. [Google Scholar] [CrossRef] [PubMed]
- Kanter, J.; Heath, L.E.; Knorr, J.; Agbenyega, E.T.; Colombatti, R.; Dampier, C.; Jakubowski, J.A. Novel findings from the multinational DOVE study on geographic and age-related differences in pain perception and analgesic usage in children with sickle cell anaemia. Br. J. Haematol. 2018, 184, 1058–1061. [Google Scholar] [CrossRef] [PubMed]
- Kunnumpurath, S.; Julien, N.; Kodumudi, G.; Kunnumpurath, A.; Kodumudi, V.; Vadivelu, N. Global supply and demand of opioids for pain management. Curr. Pain Headache Rep. 2018, 22, 34. [Google Scholar] [CrossRef] [PubMed]
- Yi, P.; Pryzbylkowski, P. Opioid Induced Hyperalgesia. Pain Med. 2015, 16, S32–S36. [Google Scholar] [CrossRef] [PubMed]
- Silverman, S.M. Opioid induced hyperalgesia: Clinical implications for the pain practitioner. Pain Physician 2009, 12, 679–684. [Google Scholar] [PubMed]
- Camilleri, M.; Lembo, A.; Katzka, D.A. Opioids in gastroenterology: Treating adverse effects and creating therapeutic benefits. Clin. Gastroenterol Hepatol 2017, 15, 1338–1349. [Google Scholar] [CrossRef] [PubMed]
- Trescot, A.M.; Helm, S.; Hansen, H.; Benya-min, R.; Adlaka, R.; Patel, S.; Manchikanti, L. Opioids in the management of chronic non-cancer pain: An update of American Society of Interventional Pain Physicians’ (ASIPP) guidelines. Pain Physician 2008, 11, S5–S62. [Google Scholar] [PubMed]
- World Health Organization: Information Sheet on Opioid Abuse. Available online: http://www.who.int/substance_abuse/information-sheet/en/ (accessed on 16 February 2019).
- Key Substance Use and Mental Health Indicators in the United States. Results from the 2016 National Survey on Drug Use and Health; Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2017. [Google Scholar]
- Ballas, S.; Kanter, J.; Agadoa, I.; Howard, R.; Wade, S.; Noxon, V.; Dampier, C. Opioid Utilization Patterns in the United States with Sickle Cell Disease. Am. J. Hematol. 2018, 93, E345–E347. [Google Scholar] [CrossRef] [PubMed]
- Smith, W. Treating pain in sickle cell disease with opioids: Clinical advances, ethical pitfalls. J. Law Med. Ethics 2014, 42, 139–146. [Google Scholar] [CrossRef] [PubMed]

| Type of Physician | N (%) |
|---|---|
| Pediatric Hematologist/Oncologist | 54 (42.5%) |
| Adult Hematologist/Oncologist | 44 (34.7%) |
| Internal Medicine | 4 (3.2%) |
| ER Physician | 9 (7.1%) |
| Family Medicine | 3 (2.4%) |
| Other | 13 (10.2%) |
| Regions | N (%) |
| United States | 75 (59) |
| Europe | 25 (19.7%) |
| Africa | 12 (9.4%) |
| South America | 7 (5.5%) |
| Caribbean | 3 (2.4%) |
| Other | 5 (3.9%) |
| Question | Response | Peds *US n (%) | Peds non-US n (%) | Other US n (%) | Other Non-US n (%) | Total US n (%) | Total Non-US n (%) | US vs. Non-US Unadjusted p-Value | US vs. Non-US Adjusted † p-Value |
|---|---|---|---|---|---|---|---|---|---|
| Do you prescribe opioids? | Yes | 35 (100.0) | 17 (68.0) | 35 (89.7) | 21 (77.8) | 70 (94.6) | 38 (73.1) | p < 0.0007 | p < 0.05 |
| No | 0 (0.0) | 8 (32.0) | 4 (10.3) | 6 (22.2) | 4 (5.4) | 14 (26.9) | |||
| How comfortable are you prescribing opioids? | Very Comfortable | 32 (91.4) | 9 (36.0) | 22 (56.4) | 10 (37.0) | 54 (73.0) | 19 (36.5) | p < 0.0005 | p < 0.0001 |
| Somewhat Comfortable | 3 (8.6) | 16 (64.0) | 14 (35.9) | 13 (48.2) | 17 (23.0) | 29 (55.8) | |||
| Somewhat Uncomfortable | 0 (0.0) | 0 (0.0) | 1 (2.6) | 3 (11.1) | 1 (1.4) | 3 (5.8) | |||
| Very Uncomfortable | 0 (0.0) | 0 (0.0) | 2 (5.1) | 1 (3.7) | 2 (2.7) | 1 (1.9) | |||
| How many doses do you prescribe at one time? | <10 | 4 (11.8) | 11 (57.9) | 8 (23.5) | 16 (69.6) | 12 (17.7) | 27 (64.3) | p < 0.0001 | p < 0.0001 |
| 10–30 | 19 (55.9) | 8 (42.1) | 8 (23.5) | 5 (21.7) | 27 (40.0) | 13 (31.0) | |||
| 30–60 | 10 (29.4) | 0 (0.0) | 8 (23.5) | 1 (4.4) | 18 (26.5) | 1(2.4) | |||
| 60–90 | 0 (0.0) | 0 (0.0) | 5 (14.7) | 1 (4.4) | 5 (7.4) | 1 (2.4) | |||
| >90 | 1 (2.9) | 0 (0.0) | 5 (14.7) | 0 (0.0) | 6 (8.8) | 0 (0.0) | |||
| Prescription tracker database? | Yes | 27 (77.1) | 9 (36.0) | 30 (79.0) | 9 (36.0) | 57 (78.0) | 18 (36.0) | p < 0.0001 | p < 0.0001 |
| No | 8 (22.9) | 16 (64.0) | 8 (21.1) | 16 (64.0) | 16 (22.0) | 32 (64.0) | |||
| How often are you concerned for misuse? | Never | 4 (11.4) | 11 (44.0) | 0 (0.0) | 4 (14.8) | 4 (5.4) | 15 (28.9) | p < 0.0002 | p < 0.05 |
| Not very often | 30 (85.7) | 12 (48.0) | 29 (74.4) | 17 (63.0) | 59 (79.7) | 29 (55.8) | |||
| Somewhat often | 1 (2.9) | 1 (4.0) | 9 (23.1) | 5 (18.5) | 10 (13.5) | 6 (11.5) | |||
| Very Often | 0 (0.0) | 1 (4.0) | 1 (2.6) | 1 (3.7) | 1 (1.4) | 2 (3.9) | |||
| How often are you concerned for abuse? | Never | 1 (2.9) | 5 (20.8) | 0 (0.0) | 1 (3.7) | 1 (1.4) | 6 (11.8) | p < 0.05 | p = 0.15 |
| Not very often | 29 (82.9) | 15 (62.5) | 20 (51.3) | 16 (59.3) | 49 (66.2) | 31 (60.8) | |||
| Somewhat often | 4 (11.4) | 2 (8.3) | 15 (38.5) | 6 (22.2) | 19 (25.7) | 8 (15.7) | |||
| Very Often | 1 (2.9) | 2 (8.3) | 4 (10.3) | 4 (14.8) | 5 (6.8) | 6 (11.8) | |||
| Do you do urine drug screens? | Yes | 7 (21.2) | 1 (4.4) | 23 (60.5) | 1 (3.7) | 30 (42.2) | 2 (4.0) | p < 0.0001 | p < 0.0001 |
| THERAPY | Total N (%) | Peds US N (%) | Peds Non-US N (%) | Other * US N (%) | Other * Non-US N (%) | Total US N (%) | Total Non-US N (%) | US vs. Non-US Unadjusted p-Value | US vs. Non-US Adjusted † p-Value |
|---|---|---|---|---|---|---|---|---|---|
| Providers that Prescribe Hydroxyurea | |||||||||
| Yes | 115 (92.7) | 35 (100.0) | 25 (100.0) | 29 (76.3) | 26 (100.0) | 64 (87.7) | 51 (100.0) | p < 0.01 | p < 0.01 |
| Estimated Percentage of Patients Taking Hydroxyurea | |||||||||
| <10% | 8 (7.1) | 0 (0.0) | 1 (4.2) | 1 (3.5) | 6 (23.1) | 1 (1.6) | 7 (14.0) | p < 0.01 | p < 0.01 |
| 10–30% | 20 (17.9) | 5 (15.2) | 4 (16.7) | 1 (3.5) | 10 (38.5) | 6 (9.7) | 14 (28.0) | ||
| 30–50% | 28 (25) | 5 (15.2) | 6 (25.0) | 13 (44.8) | 4 (15.4) | 18 (29.0) | 10 (20.0) | ||
| 50–80% | 40 (35.7) | 17 (51.5) | 5 (20.8) | 12 (41.4) | 6 (23.1) | 29 (46.8) | 11 (22.0) | ||
| 80–100% | 16 (14.3) | 6 (18.2) | 8 (33.3) | 2 (6.9) | 0 (0.0) | 8 (13.0) | 8 (16.0) | ||
| On Chronic Transfusions | |||||||||
| <10% | 68 (54) | 17 (48.6) | 16 (64.0) | 21 (53.9) | 14 (51.9) | 31 (51.4) | 30 (57.7) | p = 0.19 | p = 0.63 |
| 10–30% | 51 (40.5) | 18 (51.4) | 5 (20.0) | 16 (41.0) | 12 (44.4) | 34 (46.0) | 17 (32.7) | ||
| 30–50% | 5 (4) | 0 (0.0) | 3 (12.0) | 1 (2.6) | 1 (3.7) | 1 (1.4) | 4 (7.7) | ||
| 50–80% | 2 (1.6) | 0 (0.0) | 1 (4.0) | 1 (2.6) | 0 (0.0) | 1 (1.4) | 1 (1.9) | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Amin, N.; Nietert, P.; Kanter, J. International Differences in Outpatient Pain Management: A Survey of Sickle Cell Disease. J. Clin. Med. 2019, 8, 2136. https://doi.org/10.3390/jcm8122136
El-Amin N, Nietert P, Kanter J. International Differences in Outpatient Pain Management: A Survey of Sickle Cell Disease. Journal of Clinical Medicine. 2019; 8(12):2136. https://doi.org/10.3390/jcm8122136
Chicago/Turabian StyleEl-Amin, Nadirah, Paul Nietert, and Julie Kanter. 2019. "International Differences in Outpatient Pain Management: A Survey of Sickle Cell Disease" Journal of Clinical Medicine 8, no. 12: 2136. https://doi.org/10.3390/jcm8122136
APA StyleEl-Amin, N., Nietert, P., & Kanter, J. (2019). International Differences in Outpatient Pain Management: A Survey of Sickle Cell Disease. Journal of Clinical Medicine, 8(12), 2136. https://doi.org/10.3390/jcm8122136





