Pediatric Adapted Liking Survey (PALS) with Tailored Nutrition Education Messages: Application to a Middle School Setting
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Characteristics of the Student
2.4. Behavioral Screening and Tailored Message Program
2.5. Feasibility Measures (Acceptability and Usefulness)
2.6. Data Analysis
3. Results
3.1. Descriptive Results
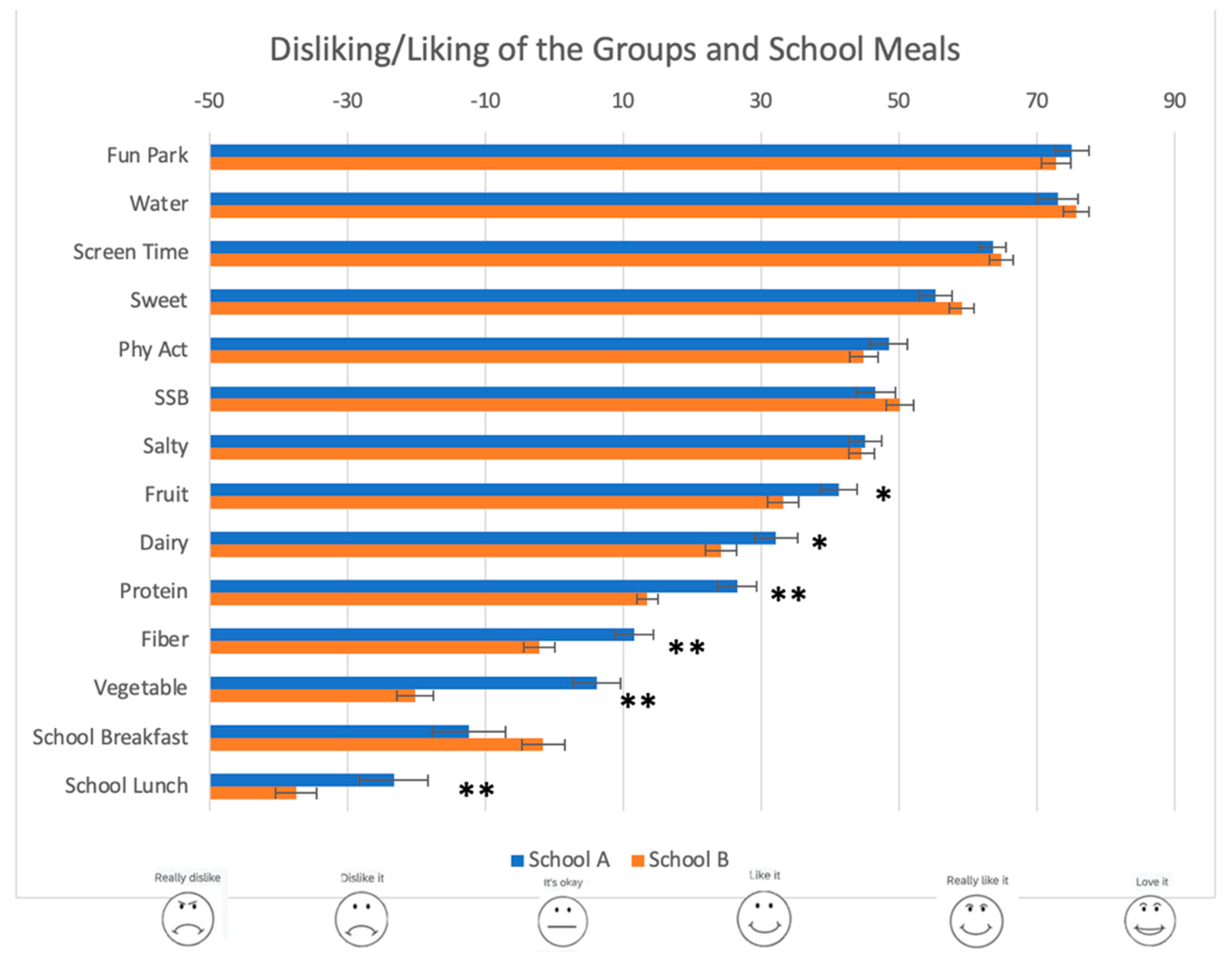
3.2. Description of the PALS Responses
3.3. Survey Acceptability and Usefulness
3.4. Tailored Messaging Program
3.5. Willingness for Behavior Change.
3.6. Message Evaluation
4. Discussions
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- International Food Information Council. 2020 Food & Health Survey. Available online: https://foodinsight.org/wp-content/uploads/2020/06/IFIC-Food-and-Health-Survey-2020.pdf (accessed on 22 January 2021).
- Sick, J.; Hojer, R.; Olsen, A. Children’s Self-Reported Reasons for Accepting and Rejecting Foods. Nutrients 2019, 11, 2455. [Google Scholar] [CrossRef] [Green Version]
- Marijn Stok, F.; Renner, B.; Allan, J.; Boeing, H.; Ensenauer, R.; Issanchou, S.; Kiesswetter, E.; Lien, N.; Mazzocchi, M.; Monsivais, P.; et al. Dietary Behavior: An Interdisciplinary Conceptual Analysis and Taxonomy. Front. Psychol. 2018, 9, 1689. [Google Scholar] [CrossRef] [Green Version]
- Tuorila, H.; Huotilainen, A.; Lähteenmäki, L.; Ollila, S.; Tuomi-Nurmi, S.; Urala, N. Comparison of affective rating scales and their relationship to variables reflecting food consumption. Food Qual. Pref. 2008, 19, 51–61. [Google Scholar] [CrossRef]
- Sharafi, M.; Perrachio, H.; Scarmo, S.; Huedo-Medina, T.B.; Mayne, S.T.; Cartmel, B.; Duffy, V.B. Preschool-Adapted Liking Survey (PALS): A brief and valid method to assess dietary quality of preschoolers. Child. Obes. 2015, 11, 530–540. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.; Johnson, S.; Oldman, S.; Duffy, V. Pediatric-adapted liking survey: Feasible and reliable dietary screening in clinical practice. Caries Res. 2018, 53, 153–159. [Google Scholar] [CrossRef]
- Chau, S.; Oldman, S.; Smith, S.R.; Lin, C.A.; Ali, S.; Duffy, V.B. Online behavioral screener with tailored obesity prevention messages: Application to a pediatric clinical setting. Nutrients 2021, 13, 223. [Google Scholar] [CrossRef] [PubMed]
- Vosburgh, K.; Smith, S.R.; Oldman, S.; Huedo-Medina, T.; Duffy, V.B. Pediatric-Adapted Liking Survey (PALS): A Diet and Activity Screener in Pediatric Care. Nutrients 2019, 11, 1641. [Google Scholar] [CrossRef] [Green Version]
- Haegele, J.A.; Foley, J.T.; Healy, S.; Paller, A. Prevalence of overweight among youth with chronic conditions in the United States: An update from the 2016 National Survey of Children’s Health. Pediatr. Obes. 2020, 15, e12595. [Google Scholar] [CrossRef]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity among Adults and Youth: United States, 2015–2016; National Center for Health Statistics: Hyattsville, MD, USA, 2017.
- Ogden, C.L.; Carroll, M.D.; Fakhouri, T.H.; Hales, C.M.; Fryar, C.D.; Li, X.; Freedman, D.S. Prevalence of Obesity Among Youths by Household Income and Education Level of Head of Household—United States 2011–2014. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 186–189. [Google Scholar] [CrossRef]
- Au, L.E.; Zhu, S.M.; Nhan, L.A.; Plank, K.R.; Frongillo, E.A.; Laraia, B.A.; Gurzo, K.; Ritchie, L.D. Household Food Insecurity is Associated with Higher Adiposity among US Schoolchildren Ages 10–15 Years: The Healthy Communities Study. J. Nutr. 2019, 149, 1642–1650. [Google Scholar] [CrossRef]
- WHO. What Is a Health Promoting School? Available online: https://www.who.int/school_youth_health/gshi/hps/en/ (accessed on 12 January 2021).
- Hung, L.S.; Tidwell, D.K.; Hall, M.E.; Lee, M.L.; Briley, C.A.; Hunt, B.P. A meta-analysis of school-based obesity prevention programs demonstrates limited efficacy of decreasing childhood obesity. Nutr. Res. 2015, 35, 229–240. [Google Scholar] [CrossRef]
- Liu, Z.; Xu, H.M.; Wen, L.M.; Peng, Y.Z.; Lin, L.Z.; Zhou, S.; Li, W.H.; Wang, H.J. A systematic review and meta-analysis of the overall effects of school-based obesity prevention interventions and effect differences by intervention components. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 95. [Google Scholar] [CrossRef]
- National Institutes of Health. 2020–2030 Strategic Plan for NIH Nutrition Research. Available online: https://dpcpsi.nih.gov/onr/strategic-plan (accessed on 22 January 2021).
- Burgermaster, M.; Contento, I.; Koch, P.; Mamykina, L. Behavior change is not one size fits all: Psychosocial phenotypes of childhood obesity prevention intervention participants. Transl. Behav. Med. 2018, 8, 799–807. [Google Scholar] [CrossRef] [PubMed]
- Celis-Morales, C.; Livingstone, K.M.; Marsaux, C.F.; Macready, A.L.; Fallaize, R.; O’Donovan, C.B.; Woolhead, C.; Forster, H.; Walsh, M.C.; Navas-Carretero, S.; et al. Effect of personalized nutrition on health-related behaviour change: Evidence from the Food4Me European randomized controlled trial. Int. J. Epidemiol. 2017, 46, 578–588. [Google Scholar] [CrossRef] [Green Version]
- Jilani, H.; Pohlabeln, H.; De Henauw, S.; Eiben, G.; Hunsberger, M.; Molnar, D.; Moreno, L.A.; Pala, V.; Russo, P.; Solea, A.; et al. Relative Validity of a Food and Beverage Preference Questionnaire to Characterize Taste Phenotypes in Children Adolescents and Adults. Nutrients 2019, 11, 1453. [Google Scholar] [CrossRef] [Green Version]
- Prochaska, J.O.; Velicer, W.F. The transtheoretical model of health behavior change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef]
- Wright, J.A.; Whiteley, J.A.; Laforge, R.G.; Adams, W.G.; Berry, D.; Friedman, R.H. Validation of 5 stage-of-change measures for parental support of healthy eating and activity. J. Nutr. Educ. Behav. 2015, 47, 134–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C.; et al. How we design feasibility studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paruthi, S.; Brooks, L.J.; D’Ambrosio, C.; Hall, W.A.; Kotagal, S.; Lloyd, R.M.; Malow, B.A.; Maski, K.; Nichols, C.; Quan, S.F.; et al. Consensus Statement of the American Academy of Sleep Medicine on the Recommended Amount of Sleep for Healthy Children: Methodology and Discussion. J. Clin. Sleep Med. 2016, 12, 1549–1561. [Google Scholar] [CrossRef] [PubMed]
- Drake, C.; Nickel, C.; Burduvali, E.; Roth, T.; Jefferson, C.; Pietro, B. The pediatric daytime sleepiness scale (PDSS): Sleep habits and school outcomes in middle-school children. Sleep 2003, 26, 455–458. [Google Scholar]
- Tambalis, K.D.; Panagiotakos, D.B.; Psarra, G.; Sidossis, L.S. Insufficient Sleep Duration Is Associated with Dietary Habits, Screen Time, and Obesity in Children. J. Clin. Sleep Med. 2018, 14, 1689–1696. [Google Scholar] [CrossRef] [Green Version]
- Wingood, G.M.; DiClemente, R.J. The ADAPT-ITT model: A novel method of adapting evidence-based HIV Interventions. J. Acquir. Immune Defic. Syndr. 2008, 47 (Suppl. 1), S40–S46. [Google Scholar] [CrossRef]
- Golem, D.L.; Martin-Biggers, J.T.; Koenings, M.M.; Davis, K.F.; Byrd-Bredbenner, C. An integrative review of sleep for nutrition professionals. Adv. Nutr. 2014, 5, 742–759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bartoshuk, L.M.; Duffy, V.B.; Hayes, J.E.; Moskowitz, H.R.; Snyder, D.J. Psychophysics of sweet and fat perception in obesity: Problems, solutions and new perspectives. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2006, 361, 1137–1148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meyer, C.; Barbosa, D.G.; Junior, G.J.F.; Andrade, R.D.; Silva, D.A.S.; Pelegrini, A.; Gomes Felden, E.P. Proposal of cutoff points for pediatric daytime sleepiness scale to identify excessive daytime sleepiness. Chronobiol. Int. 2018, 35, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Kral, T.V.E.; Chittams, J.; Moore, R.H. Relationship between food insecurity, child weight status, and parent-reported child eating and snacking behaviors. J. Spec. Pediatr. Nurs. 2017, 22, e12177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, S.S.; Gentzke, A.; Jamal, A.; Homa, D.; Neff, L. Feasibility of Administering an Electronic Version of the National Youth Tobacco Survey in a Classroom Setting. Prev. Chronic Dis. 2020, 17, E20. [Google Scholar] [CrossRef] [PubMed]
- Smigelskas, K.; Lukoseviciute, J.; Vaiciunas, T.; Mozuraityte, K.; Ivanaviciute, U.; Mileviciute, I.; Zemaitaityte, M. Measurement of Health and Social Behaviors in Schoolchildren: Randomized Study Comparing Paper Versus Electronic Mode. Zdr. Varst. 2019, 58, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Pont, S.J.; Puhl, R.; Cook, S.R.; Slusser, W.; Section On, O.; Obesity, S. Stigma Experienced by Children and Adolescents With Obesity. Pediatrics 2017, 140, e20173034. [Google Scholar] [CrossRef] [Green Version]
- Petty, R.T.; Cacioppo, J.T. Attitudes and Persuasion: Classic and Contemporary Approaches; Westview Press: Boulder, CO, USA, 1996. [Google Scholar]
- Armitage, C.J. Is there utility in the transtheoretical model? Br. J. Health Psychol. 2009, 14, 195–210. [Google Scholar] [CrossRef]
- Oldman, S. Improving Diet & Physical Activity Behaviors through Tailored mHealth Messages: Application to Childhood Obesity Prevention in a Pediatric Emergency Department. Master’s Thesis, University of Connecticut, Mansfield, CO, USA, 2018. [Google Scholar]
- DHHS/USDA. Dietary Guidelines 2015–2020. Available online: https://health.gov/our-work/food-nutrition/previous-dietary-guidelines/2015 (accessed on 9 March 2021).
- Lund, A.M. Measuring Usability with the USE Questionnaire. Usability Interface 2001, 8, 3–6. [Google Scholar]
- Karner, H. A Feasible and Tailored Nutrition Education Intervention for Middle-Schoolers: Coordination with School Nutrition Program and Preliminary Outcomes. Master’s Thesis, University of Connecticut, Mansfield, CO, USA, 2019. [Google Scholar]
- Bawajeeh, A.O.; Albar, S.A.; Zhang, H.; Zulyniak, M.A.; Evans, C.E.L.; Cade, J.E. Impact of Taste on Food Choices in Adolescence-Systematic Review and Meta-Analysis. Nutrients 2020, 12, 1985. [Google Scholar] [CrossRef]
- Estay, K.; Pan, S.; Zhong, F.; Capitaine, C.; Guinard, J.X. A cross-cultural analysis of children’s vegetable preferences. Appetite 2019, 142, 104346. [Google Scholar] [CrossRef]
- Duffy, V.B.; Hayes, J.E.; Sharafi, M. Interactions between retronasal olfaction and taste influence vegetable liking and consumption: A psychophysical investigation. J. Agric. Food Res. 2020, 2, 100044. [Google Scholar] [CrossRef]
- Rageliene, T.; Gronhoj, A. Preadolescents’ healthy eating behavior: Peeping through the social norms approach. BMC Public Health 2020, 20, 1268. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, S.R.; Angka, S.; Olsen, K.; Tolver, A.; Olsen, A. Repeated exposure to vegetable-enriched snack bars may increase children’s liking for the bars—But not for the vegetables. Appetite 2019, 140, 1–9. [Google Scholar] [CrossRef]
- van der Horst, K.; Mathias, K.C.; Prieto Patron, A.; Allirot, X. Art on a Plate: A Pilot Evaluation of an International Initiative Designed to Promote Consumption of Fruits and Vegetables by Children. J. Nutr. Educ. Behav. 2019, 51, 919–925. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Appleton, K.M.; Barrie, E.; Samuel, T.J. Modelling positive consequences: Increased vegetable intakes following modelled enjoyment versus modelled intake. Appetite 2019, 140, 76–81. [Google Scholar] [CrossRef]
- Zhao, C.; Panizza, C.; Fox, K.; Boushey, C.J.; Byker Shanks, C.; Ahmed, S.; Chen, S.; Serrano, E.L.; Zee, J.; Fialkowski, M.K.; et al. Plate Waste in School Lunch: Barriers, Motivators, and Perspectives of SNAP-Eligible Early Adolescents in the US. J. Nutr. Educ. Behav. 2019, 51, 967–975. [Google Scholar] [CrossRef] [Green Version]
- Bohnen, N.I.; Muller, M.L.; Kotagal, V.; Koeppe, R.A.; Kilbourn, M.A.; Albin, R.L.; Frey, K.A. Olfactory dysfunction, central cholinergic integrity and cognitive impairment in Parkinson’s disease. Brain 2010, 133, 1747–1754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cullen, K.W.; Chen, T.A. The contribution of the USDA school breakfast and lunch program meals to student daily dietary intake. Prev. Med. Rep. 2017, 5, 82–85. [Google Scholar] [CrossRef]
- USDA. New Meal Pattern Requirements and Nutrition Standards, National School Lunch and School Breakfast Programs. Available online: http://www.fns.usda.gov/sites/default/files/LAC_03-06-12_0.pdf (accessed on 21 January 2021).
- Turner, L.; Chaloupka, F.J. Perceived reactions of elementary school students to changes in school lunches after implementation of the United States Department of Agriculture’s new meals standards: Minimal backlash, but rural and socioeconomic disparities exist. Child. Obes. 2014, 10, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Terry-McElrath, Y.M.; Turner, L.; Colabianchi, N.; O’Malley, P.M.; Chaloupka, F.J.; Johnston, L.D. Student Reactions during the First Year of Updated School Lunch Nutrition Standards—A BTG Research Brief; Bridging the Gap Program, Institute for Social Research, University of Michigan: Ann Arbor, MI, USA, 2014. [Google Scholar]
- Hamdi, N.; Ellison, B.; McCaffrey, J.; Metcalfe, J.J.; Hoffman, A.; Haywood, P.; Prescott, M.P. Implementation of a Multi-Component School Lunch Environmental Change Intervention to Improve Child Fruit and Vegetable Intake: A Mixed-Methods Study. Int. J. Environ. Res. Public Health 2020, 17, 3971. [Google Scholar] [CrossRef]
- Guenther, P.M.; Kirkpatrick, S.I.; Reedy, J.; Krebs-Smith, S.M.; Buckman, D.W.; Dodd, K.W.; Casavale, K.O.; Carroll, R.J. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J. Nutr. 2014, 144, 399–407. [Google Scholar] [CrossRef] [Green Version]
- Malheiros, L.E.A.; da Costa, B.G.G.; Lopes, M.V.V.; Chaput, J.P.; Silva, K.S. Association between physical activity, screen time activities, diet patterns and daytime sleepiness in a sample of Brazilian adolescents. Sleep Med. 2020, 78, 1–6. [Google Scholar] [CrossRef]
- Landry, M.J.; van den Berg, A.E.; Asigbee, F.M.; Vandyousefi, S.; Ghaddar, R.; Davis, J.N. Child-Report of Food Insecurity Is Associated with Diet Quality in Children. Nutrients 2019, 11, 1574. [Google Scholar] [CrossRef] [Green Version]
- Huang, K.Y.; Cheng, S.; Theise, R. School contexts as social determinants of child health: Current practices and implications for future public health practice. Public Health Rep. 2013, 128 (Suppl. 3), 21–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joffer, J.; Jerden, L.; Ohman, A.; Flacking, R. Exploring self-rated health among adolescents: A think-aloud study. BMC Public Health 2016, 16, 156. [Google Scholar] [CrossRef]
- Wickström, A.; Zeiler, K. The performativity of surveys: Teenagers’ meaning-making of the ‘Health Behavior in School-aged Children Survey’ in Sweden. Child. Soc. 2021. [Google Scholar] [CrossRef]
- Holmberg, C.; Larsson, C.; Korp, P.; Lindgren, E.C.; Jonsson, L.; Froberg, A.; Chaplin, J.E.; Berg, C. Empowering aspects for healthy food and physical activity habits: adolescents’ experiences of a school-based intervention in a disadvantaged urban community. Int. J. Qual. Stud. Health Well-Being 2018, 13, 1487759. [Google Scholar] [CrossRef]
- Schmid, K.L.; Rivers, S.E.; Latimer, A.E.; Salovey, P. Targeting or tailoring? Mark. Health Serv. 2008, 28, 32–37. [Google Scholar]
- Shaver, E.R.; McGlumphy, K.C.; Gill, A.K.; Hasson, R.E. Application of the Transtheoretical Model to Physical Activity and Exercise Behaviors in African-American Adolescents. Am. J. Health Behav. 2019, 43, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Perez-Cueto, F.J.A.; Giboreau, A.; Mavridis, I.; Hartwell, H. The Promotion of Eating Behaviour Change through Digital Interventions. Int. J. Environ. Res. Public Health 2020, 17, 7488. [Google Scholar] [CrossRef] [PubMed]
- Bahreynian, M.; Salehi, M.; Khoshhali, M.; Kelishadi, R. Impact of text message-based intervention for weight control and health-promoting lifestyle behaviors of overweight and obese children. J. Educ. Health Promot. 2020, 9, 108. [Google Scholar] [CrossRef]
- Murimi, M.W.; Nguyen, B.; Moyeda-Carabaza, A.F.; Lee, H.J.; Park, O.H. Factors that contribute to effective online nutrition education interventions: A systematic review. Nutr. Rev. 2019, 77, 663–690. [Google Scholar] [CrossRef]
- Schneider, M.; DeBar, L.; Calingo, A.; Hall, W.; Hindes, K.; Sleigh, A.; Thompson, D.; Volpe, S.L.; Zeveloff, A.; Pham, T.; et al. The effect of a communications campaign on middle school students’ nutrition and physical activity: Results of the healthy study. J. Health Commun. 2013, 18, 649–667. [Google Scholar] [CrossRef] [Green Version]
- DeBar, L.L.; Schneider, M.; Ford, E.G.; Hernandez, A.E.; Showell, B.; Drews, K.L.; Moe, E.L.; Gillis, B.; Jessup, A.N.; Stadler, D.D.; et al. Social marketing-based communications to integrate and support the HEALTHY study intervention. Int. J. Obes. (Lond.) 2009, 33 (Suppl. 4), S52–S59. [Google Scholar] [CrossRef] [Green Version]
- Santarossa, S.; Woodruff, S.J. #LancerHealth: Using Twitter and Instagram as a tool in a campus wide health promotion initiative. J. Public Health Res. 2018, 7, 1166. [Google Scholar] [CrossRef] [Green Version]
- O’Keefe, L. Identifying Food Insecurity: Two-Question Screening Tool Has 97% Sensitivity. AAP News 2015. Available online: https://www.aappublications.org/news/2015/10/22/FoodSecurity102315 (accessed on 22 January 2021).
- Banna, J.; Richards, R.; Jones, B.; Anderson, A.K.; Reicks, M.; Cluskey, M.; Gunther, C.; Hongu, N.K.; Lora, K.; Misner, S.; et al. Describing Independent Eating Occasions among Low-Income Adolescents. Int. J. Environ. Res. Public Health 2020, 17, 981. [Google Scholar] [CrossRef] [Green Version]


| Phase | Methodology |
|---|---|
| 1. Assessment |
|
| 2. Decision |
|
| 3. Administration |
|
| 4. Production |
|
| 5. Topical Experts |
|
| 6. Integration |
|
| 7. Testing |
|
| % of Participants: School A (N = 195) | % of Participants: School B (N = 310) | ||
|---|---|---|---|
| Age | Ten Eleven Twelve Thirteen Fourteen Other | 0 10.5 80.0 8.5 1.0 0 | 1.3 34.8 34.2 24.2 3.9 1.3 |
| Gender | Male Female Other | 51 49 N/A | 48 49 3 |
| Race/Ethnicity | White Black/African Am. Hispanic/Latino Asian American Indian Other Pacific Islander Multiple Declines to Answer/ Don’t know/Not sure | 22.5 34.0 10.0 2.0 0.5 0.5 21.5 6.0 3.0 | 9.7 21.0 40.6 9.0 0.3 0 12.9 2.6 3.9 |
| How do you feel today? | Smile rating Neutral Frown rating | 68 22 10 | 68 24 9 |
| Food Insecurity † | Food Secure Food Insecure | 61 39 | 56 44 |
| Sleep ‡ | Insufficient Sleep Sufficient Sleep | 43 57 | 55 45 |
| Food Secure N = 283 | Food Insecure N = 209 | |
|---|---|---|
| Sedentary | 63.77 ± 1.65 | 64.69 ± 1.92 |
| Sweet | 55.94 ± 1.85 | 59.55 ± 2.15 |
| Phys Act | 50.47 ± 2.05 | 40.70 ± 2.38 |
| Sugar Sweetened Beverages | 47.96 ± 2.14 | 49.29 ± 2.49 |
| Salty | 43.10 ± 1.93 | 46.66 ± 2.23 |
| Fruit | 37.56 ± 2.27 | 34.42 ± 2.64 |
| Dairy | 27.16 ± 2.40 | 27.27 ± 2.79 |
| Protein | 19.14 ± 1.93 | 17.47 ± 2.24 |
| Fiber | 2.00 ± 2.31 | 4.10 ± 2.68 |
| Vegetable | −9.11 ± 2.90 | −12.3 ± 3.32 |
| HBI ‡ | −5.16 ± 2.19 | −9.00 ± 2.55 |
| School A | School B | |||
|---|---|---|---|---|
| Food Secure | Food Insecure | Food Secure | Food Insecure | |
| Only Reinforcing | 11.8 | 14.9 | 5.8 | 5.8 |
| Only Motivating | 47.4 | 45.6 | 56.9 | 46.8 |
| Both Types of Messages | 40.8 | 39.5 | 37.3 | 47.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hildrey, R.; Karner, H.; Serrao, J.; Lin, C.A.; Shanley, E.; Duffy, V.B. Pediatric Adapted Liking Survey (PALS) with Tailored Nutrition Education Messages: Application to a Middle School Setting. Foods 2021, 10, 579. https://doi.org/10.3390/foods10030579
Hildrey R, Karner H, Serrao J, Lin CA, Shanley E, Duffy VB. Pediatric Adapted Liking Survey (PALS) with Tailored Nutrition Education Messages: Application to a Middle School Setting. Foods. 2021; 10(3):579. https://doi.org/10.3390/foods10030579
Chicago/Turabian StyleHildrey, Rachel, Heidi Karner, Jessica Serrao, Carolyn A. Lin, Ellen Shanley, and Valerie B. Duffy. 2021. "Pediatric Adapted Liking Survey (PALS) with Tailored Nutrition Education Messages: Application to a Middle School Setting" Foods 10, no. 3: 579. https://doi.org/10.3390/foods10030579
APA StyleHildrey, R., Karner, H., Serrao, J., Lin, C. A., Shanley, E., & Duffy, V. B. (2021). Pediatric Adapted Liking Survey (PALS) with Tailored Nutrition Education Messages: Application to a Middle School Setting. Foods, 10(3), 579. https://doi.org/10.3390/foods10030579








