3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing
Abstract
:1. Introduction
2. Current State of Technology
2.1. A Rationale for Digital Manufacturing and 3D Printing in Dentistry
2.2. History of 3D Printing
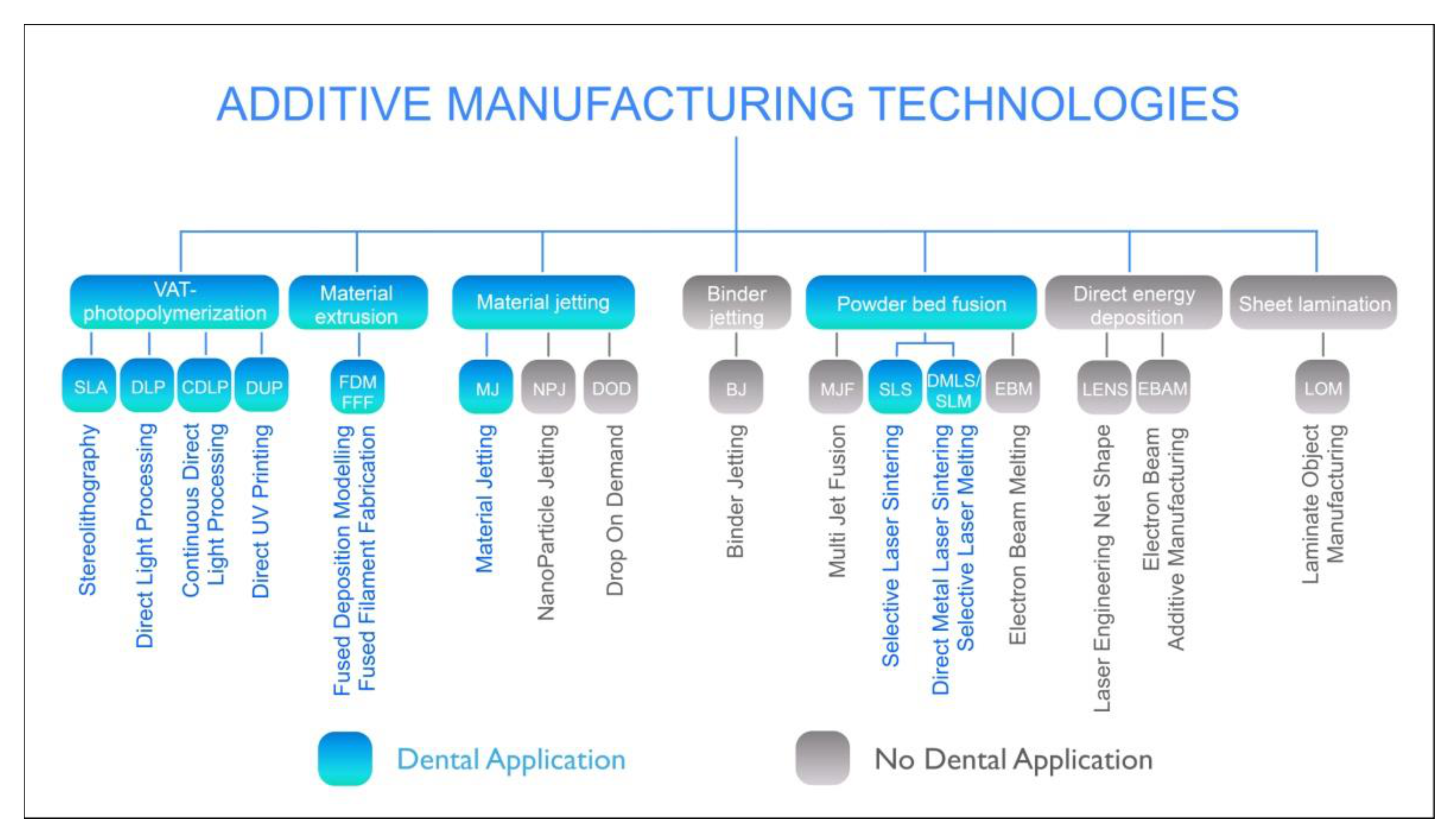
2.3. Nomenclature and Classification of Additive CAD/CAM-Based Manufacturing
- Vat photopolymerization (VPP)
- Material extrusion (MEX)
- Material jetting (MJT)
- Binder jetting (BJT)
- Powder-bed fusion (PBF)
- Directed energy deposition (DED)
- Sheet lamination (SHL)
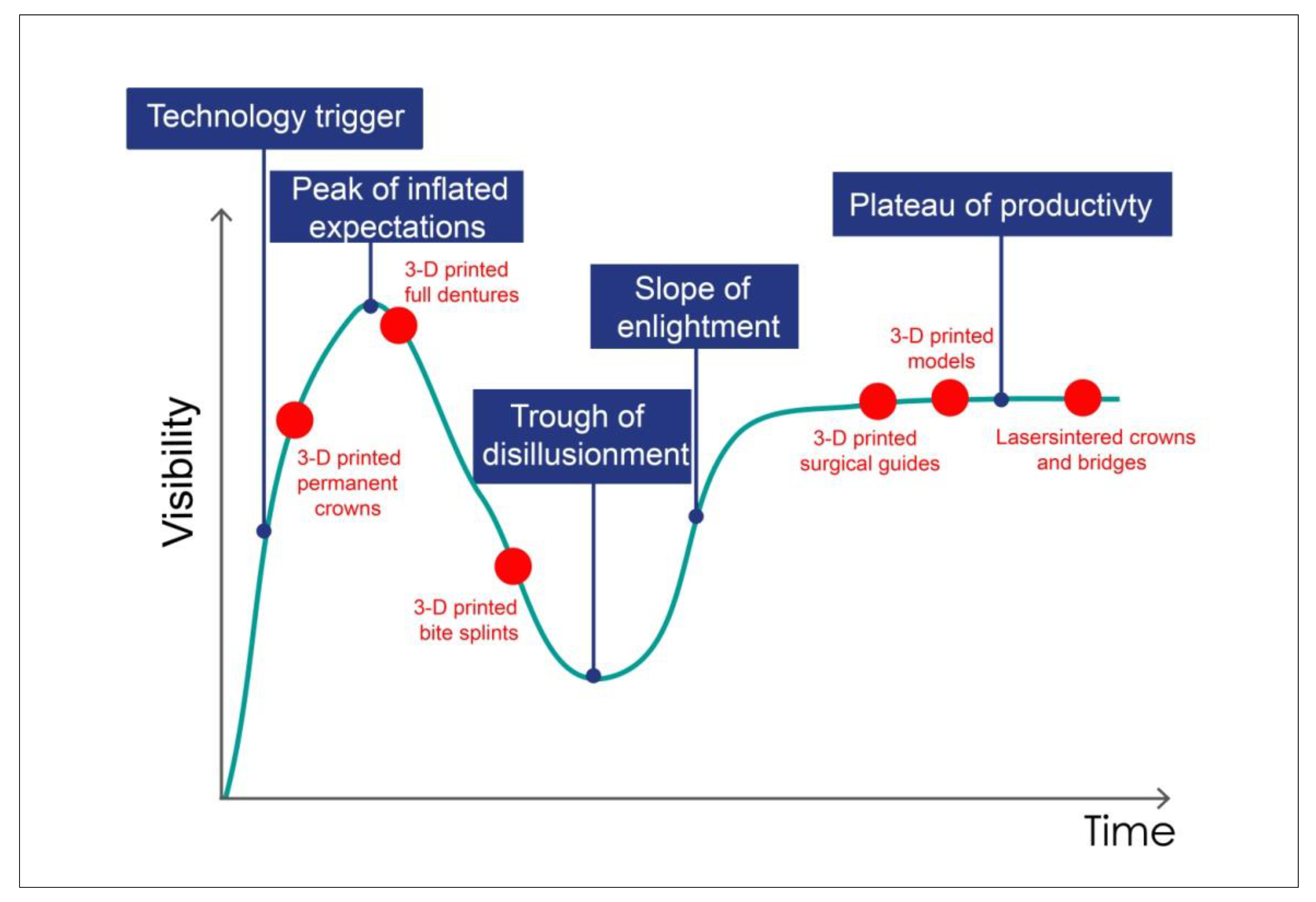
3. The Status Quo of Dental 3D Printing
Common Processes in Dental 3D Printing
4. Dental Indications and Applications of 3D Printing
4.1. Additive Manufacturing and Metals
4.1.1. Laser Sintering of Crowns and Bridges Made from Non-Precious Alloys
4.1.2. Laser Sintering of Clasp-Retained Cast-Metal Frameworks
- The required initial clasp withdrawal forces were attained by the cast and laser-sintered clasps alike. After artificial aging, the laser-sintered clasps exhibited no decrease in retention force.
- Pores and flaws were smaller and more evenly distributed overall in the laser-sintered clasps compared to the cast clasps.
- Laser-sintered clasps performed significantly better in the long term than cast clasps, with more than twice the latter’s survival rates. One reason could be the superior structural quality of the laser-sintered clasps.
4.1.3. Hybrid Manufacturing
4.2. Additive Manufacturing and Polymers
4.2.1. Stereolithography Using a Laser Source (SLA)
4.2.2. Digital Light Processing (DLP)
Resolution of DLP Printers
- Using a DMD chip with higher resolution (e.g., 4K resolution)
- Two DLP projectors with HD resolution connected in parallel
- Moving DLP projectors (W2P Engineering, Vienna, Austria)
- Prodways MovingLight technology (Prodways Group, Paris, France)
DLP Printer Build Process Optimization
- Fixed intervals
- Force Feedback technology (Rapid Shape, Heimsheim, Germany)
- Vat deflection feedback system (VDFS; W2P, Vienna, Austria)
- Continuous direct light processing (CDLP; Carbon3D, Redwood City, CA, USA)
4.2.3. Material Jetting (MJT)
4.2.4. Useful Indications for AM of Polymers
- Model fabrication based on intraoral scan data
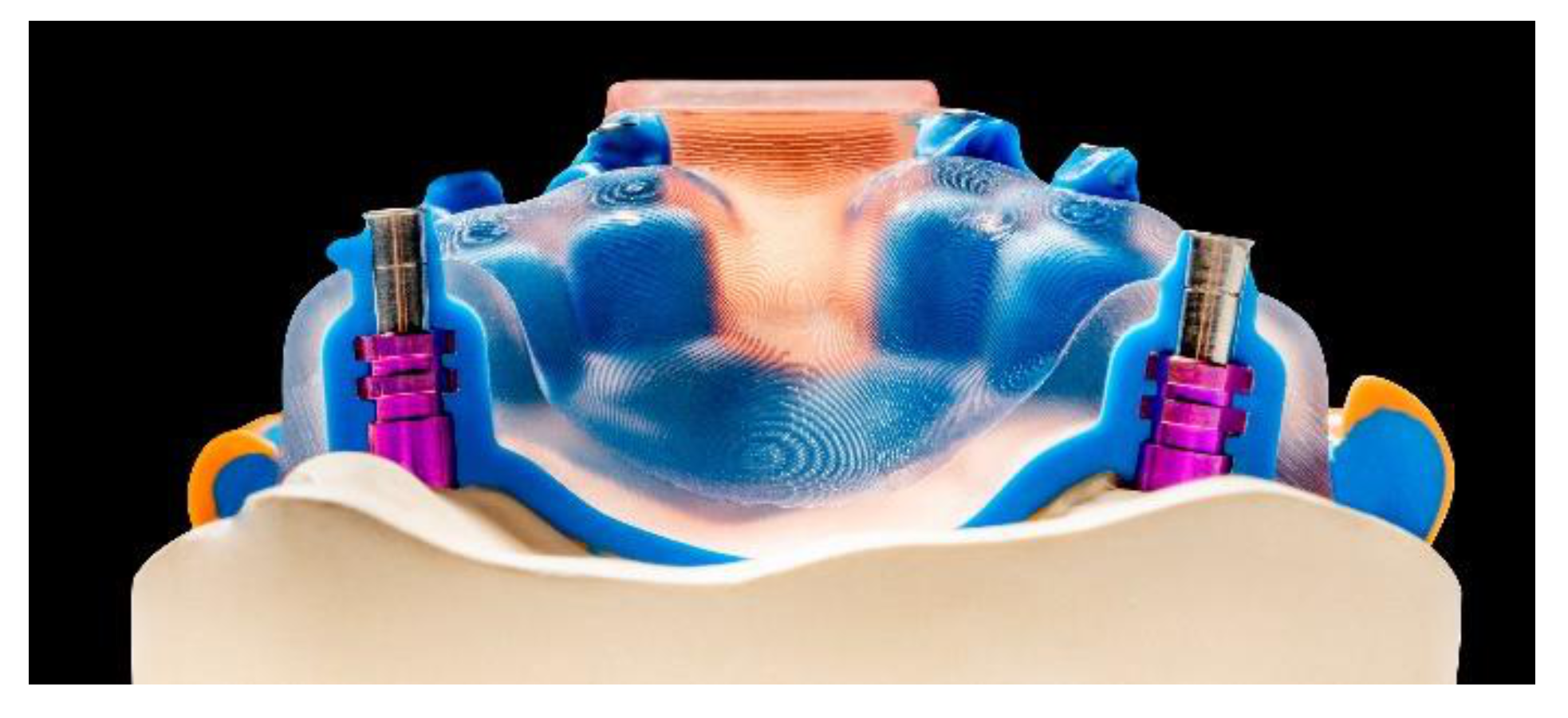
- Templates (drilling stents) for guided implant surgery
- Custom impression trays
- Production of occlusal splints
- Production of realistic training models
- Production of graphic 3D models (3D Medical Print, Lenzing, Austria)
- VarseoSmile Crown plus–3D printing of permanent single-tooth restorations (Bego, Bremen, Germany)
4.3. Additive Manufacturing and Ceramics
- Trix print process by Dekema (Freilassing, Germany)
- IPS e.max Digital Press Design–Wax Tree by Ivoclar Vivadent (Schaan, Liechtenstein)
- SLA process, e.g., 3DCeram (Limoges, France)
- DLP process, e.g., LCM (lithography-based ceramic manufacturing, LCM) by Lithoz (Vienna, Austria)
- Material extrusion (fused-filament fabrication, FFF; paste-extrusion modeling, PEM)
- Material jetting/nanoparticle jetting, e.g., XJET (Rehovot, Israel)
- Binder jetting, e.g., 3D Systems (Rock Hill, SC, USA)
- SLS process (research project at the Department for Dental Prosthetics of the University of Munich, the Friedrich Baur Institute for Biomaterials at Bayreuth, Germany, and Concept Laser at Lichtenfels, Germany)
- LOM process (laminated object layering)
4.3.1. Indirect 3D Printing of Ceramics Example: Dekema Trix Print
4.3.2. Direct 3D Printing of Ceramics Example: LCM Technology
- Immersing the crown in the staining solution
- Custom painting of the crown using a brush and staining solution
- A combination of the two
4.3.3. Multi-Material 3D Printing of Ceramics
- Two materials in a single layer
- A denser material combined with a second porous material
- Two-phase or multi-phase materials with gradual variations in composition
- Gradual variations in both density and composition
5. Limitations of 3D-Printing
6. Outlook
Author Contributions
Funding
Conflicts of Interest
References
- Schweiger, J.; Edelhoff, D.; Güth, J.F. Update digitale Zahnheilkunde 2020—Aktuelle Möglichkeiten und Limitationen. Bayerisches Zahnärzte Blatt 2020, 57, 42–52. [Google Scholar]
- Schweiger, J.; Güth, J.F. Neue Entwicklungen in der additiven und subtraktiven Fertigung Teamwork. J. Cont. Dent. Educ. 2020, 23, 82–90. [Google Scholar]
- Betriebe—Beschäftigte—Auszubildende im Zahntechniker-Handwerk. Available online: https://www.vdzi.de/statistik.html. (accessed on 10 December 2020).
- Campbell, S.D.; Cooper, L.; Craddock, H.; Hyde, T.P.; Nattress, B.; Pavitt, S.H.; Seymour, D.W. Removable partial dentures: The clinical need for innovation. J. Prosthet. Dent. 2017, 118, 273–280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jordan, R.A.; Micheelis, W. Fünfte Deutsche Mundgesundheitsstudie (DMS V); Deutscher Zahnärzte: Köln, Germany, 2016. [Google Scholar]
- Van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Horn, T.J.; Harryson, O.L.A. Overview of current additive manufacturing technologies and selected applications. Sci. Prog. 2012, 95, 255–282. [Google Scholar] [CrossRef] [PubMed]
- Dawood, A.; Marti, B.; Sauret Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Caviezel, C.; Grünwald, R.; Ehrenberg-Silies, S.; Kind, S.; Jetzke, T.; Bovenschulte, M. Additive Fertigungsverfahren (3D-Druck)—Innovationsanalyse; TAB Arbeitsbereicht: Berlin, Germany, 2017. [Google Scholar]
- Kessler, A.; Hickel, R.; Reymus, M. 3D Printing in Dentistry—State of the Art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Kieschnick, A.; Schweiger, J.; Edelhoff, D.; Güth, J.F. Status Präsens 2020: Additive CAD/CAM-Gestützte Fertigungstechnologien im Zahntechnischen Labor. Available online: https://www.researchgate.net/publication/341990852_Status_Prasens_2020_Additive_CADCAM-gestutzte_Fertigungstechnologien_im_zahntechnischen_Labor#fullTextFileContent. (accessed on 10 December 2020).
- Hull, C.W. Apparatus for Production of Three-Dimensional Objects by Stereolithography. U.S. Patent 4,575,330, 8 August 1984. [Google Scholar]
- Crump, S. Apparatus and Method for Creating Three-Dimensional Objects. U.S. Patent 5,121,329, 5 September 1989. [Google Scholar]
- Kollenberg, W. Keramik und Multimaterial 3D-Druck. Keram. Z. 2014, 66, 233–236. [Google Scholar] [CrossRef]
- ISO/ASTM. Additive Manufacturing—General Principles—Terminology. Beuth 2017, 52900. [Google Scholar] [CrossRef]
- ISO/ASTM. Additive Manufacturing—General Principles—Part 2: Overview of Process Categories and Feedstock. Beuth 2016, 17296-2. [Google Scholar] [CrossRef]
- Gartner Hype Cycle. Available online: https://www.gartner.com/en/research/methodologies/gartner-hype-cycle (accessed on 10 December 2020).
- Dolabdjian, H.; Strietzel, R. Verfahren zur Herstellung von Zahnersatz und dentalen Hilfsteilen. European Patent Application 1 021 997 B2, 26 July 2000. [Google Scholar]
- Revilla-León, M.; Meyer, M.J.; Özcan, M. Metal additive manufacturing technologies. Int. J. Comput. Dent. 2019, 22, 55–67. [Google Scholar]
- Fischer, J.; Stawarczyk, B.; Trottmann, A.; Hämmerle, C.H.F. Festigkeit lasergesinterter Brückengerüste aus einer CoCr-legierung. Quintessenz Zahntech. 2008, 34, 140–149. [Google Scholar]
- Rudolph, M.; Setz, J. Ein CAD/CAM-System mit aufbauender Lasertechnologie. Quintessenz Zahntech. 2007, 33, 582–587. [Google Scholar]
- Quante, K.; Ludwig, K.; Kern, M. Marginal and internal fit of metal-ceramic crowns abricated with a new laser melting technology. Dent. Mater. 2008, 24, 1311–1355. [Google Scholar] [CrossRef]
- Xu, D.; Xiang, N.; Wie, B. The marginal fit of selective laser melting-fabricated metal crowns: An in vitro study. J. Prosth. Dent. 2014, 112, 1437–1440. [Google Scholar] [CrossRef]
- Huang, Z.; Zhang, L.; Zhu, J.; Zhang, X. Clinical marginal and internal fitt of metal ceramic crowns fabricated with a selective laser melting technolog. J. Prosth. Dent. 2015, 113, 623–627. [Google Scholar] [CrossRef]
- Lövgren, N.; Roxner, R.; Klemendz, S.; Larsson, C. Effect of production method on surface roughness, marginal and internal fit, and retention of cobalt-chromium single crowns. J Prosth Dent 2017, 118, 95–101. [Google Scholar] [CrossRef] [Green Version]
- Lehmann, K.M.; Hellwig, E.; Wenz, H.J. Zahnärztliche Propädeutik; Deutscher Zahnärzte: Köln, Germany, 2015. [Google Scholar]
- Stark, H. Ist die Modellgussprothese adäquater Zahnersatz für den älteren Menschen? Quintessenz 2005, 56, 367–373. [Google Scholar]
- Roach, F.E. Principles and essentials of bar clasp partial dentures. J. Am. Dent. Assoc. 1930, 17, 124–138. [Google Scholar]
- Schweiger, J.; Kieschnick, A. CAD/CAM in der digitalen Zahnheilkunde; Teamwork Media: Fuchstal, Germany, 2017. [Google Scholar]
- Alifui-Segbaya, F.; Williams, R.J.; George, R. Additive manufacturing: A novel method for fabricating cobalt-chromium removable partial denture frameworks. Eur. J. Prosthodont Restor. Dent. 2017, 25, 73–78. [Google Scholar]
- Laverty, D.P.; Thomas, M.B.M.; Clark, P.; Addy, L.D. The use of 3D metal printing (direct metal laser sintering) in removable prosthodontics. Dent. Update 2016, 43, 826–835. [Google Scholar] [CrossRef] [PubMed]
- Lima, J.M.; Anami, L.C.; Araujo, R.M.; Pavanelli, C.A. Removable partial dentures: Use of rapid prototyping. J. Prosthodont. 2014, 23, 588–591. [Google Scholar] [CrossRef] [PubMed]
- Tregermann, I.; Renne, W.; Kelly, A.; Wilson, D. Evaluation of removable partial denture frameworks fabricated using 3 differnet techniques. J. Prosthet. Dent. 2019, 122, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Van Zeghbroeck, L.; Boons, E. Evaluation of technicians working time in the fabrication of removable partial dentures: Cad/Cam versus tradition. In Proceedings of the 14th Biennial Meeting of the International College of Prosthodontics, Waikoloa Village, HI, USA, 7–12 September 2011; p. 63. [Google Scholar]
- Schweiger, J.; Güth, J.F.; Erdelt, K.J.; Edelhoff, D.; Schubert, O. Internal porosities, retentive force, and survival of cobalt-chromium alloy clasps fabricated by selective laser sintering. J. Prosthodont. Res. 2019, 64, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Torii, M.; Nakata, T.; Takahashi, K.; Kawamura, N.; Shimpo, H.; Ohkubo, C. Fitness and retentive force of cobalt-chromium alloy clasps fabricates with repeated laser sintering and milling. J. Prosthodont. Res. 2018, 62, 342–346. [Google Scholar] [CrossRef]
- Nakata, T.; Shimpo, H.; Okhubo, C. Clasp fabrication using one-process molding by repeated laser sintering and high-speed milling. J. Prosth. Research 2017, 61, 276–282. [Google Scholar] [CrossRef]
- Revilla-León, M.; Öczan, M. Additive manufacturing technologies used for processing polymers: Current status and potential application in prosthetic dentistry. J Prosthodont. 2019, 28, 146–158. [Google Scholar] [CrossRef] [Green Version]
- Jokusch, J.; Öczan, M. Additive manufacturing of dental polymers: An overview on processes, materials and applications. Dent. Mater. J. 2020, 39, 345–354. [Google Scholar] [CrossRef] [Green Version]
- Quan, H.; Zhang, T.; Xu, H.; Luo, S.; Nie, J.; Zhu, X. Photo-curing 3D-Printing technique and its challenges. Bioact. Mater. 2020, 22, 110–115. [Google Scholar] [CrossRef]
- Dietrich, C.A.; Ender, A.; Baumgartner, S.; Mehl, A. A validation study of reconstructes rapid prototyping models produces by two technologies. Angle Orthod. 2017, 87, 782–787. [Google Scholar] [CrossRef] [Green Version]
- Brown, G.B.; Currier, G.F.; Kadioglu, O.; Kierl, J.P. Accuracy of 3-dimensional printed dental models reconstructed from digital intraoral impressions. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 733–739. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.Y.; Shin, Y.S.; Jund, H.D.; Hwang, C.J.; Baik, H.S.; Cha, J.Y. Precision and trueness of dental models manufactured with different 3-dimensional printing technologies. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 144–153. [Google Scholar] [CrossRef] [Green Version]
- Emir, F.; Ayyildiz, S. Accuracy evaluation of complete-arch models manufactured by three different 3D printing technologies: A three-dimensional analysis. J. Prosthodont. Res. 2021. [Google Scholar] [CrossRef]
- Rungrojwittayakul, O.; Kann, J.Y.; Shiozaki, K.; Swamidass, R.S.; Goodacre, B.J.; Goodacre, C.J.; Lozada, J.L. Accuracy of 3D-printed models created by two technolgies of printers with different designs of model base. J. Prosthodont. 2020, 29, 124–128. [Google Scholar] [CrossRef]
- Etemad-Shahidi, Y.; Qallandar, O.B.; Evenden, J.; Alifui-Segbaya, F.; Ahmed, K.E. Accuracy of 3-Dimensionally printed full-arch dental models: A systematic review. J. Clin. Med. 2020, 9, 3357. [Google Scholar] [CrossRef]
- Kallweit, D.; Mönch, W.; Zappe, H. Kontrolliert kippen: Silizium-Mikrospiegel mit integriertem optischen Feedback. Photonik 2006, 4, 62–65. [Google Scholar]
- Viereck, V.; Li, Q.; Jäkel, A.; Hillmer, H. Großflächige Anwendung von optischen MEMS: Mikospiegel-Arrays zur Tageslichtlenkung. Photonik 2009, 2, 28–29. [Google Scholar]
- DLP® 0.47-inch 4K UHD HSSI Digital Micromirror Device (DMD). Available online: https://www.ti.com/product/DLP471TP (accessed on 10 December 2020).
- The 3D Printing Standard in Speed, Reliability and Workflow Integration. Available online: https://www.rapidshape.de/images/kataloge/Dental_Katalog_EN.pdf#page=11 (accessed on 4 May 2021).
- Professionelle Desktop 3D-Drucker. Available online: https://www.way2production.at/produkte (accessed on 10 December 2020).
- Allanic, A.L. Production of a Volume Object by Lithography, Having Improved Spatial Resolution. European Patent Application 2 943 329 B1, 8 November 2015. [Google Scholar]
- ProMaker LD20 Dental Plus. Compact High Precision 3d Printer. Available online: https://www.prodways.com/en/industrial-3d-printers/promaker-ld20-dental-plus/ (accessed on 10 December 2020).
- Schultheiss, A. Mehr Qualität, mehr Produktivität: Professioneller 3D-Druck im Dentallabor. Zahntechnik Magazin 2018. Available online: https://www.ztm-aktuell.de/marktplatz/industrie-report/story/mehr-Qualitaet-mehr-produktivitaet-professioneller-3d-druck-im-dentallabor_670.html (accessed on 10 December 2020).
- Stadlmann, K. Anlage zum schichtweisen Aufbau eines Körpers und Entformvorrichtung hierfür. AT 51 4496 B1, 2015.
- Stadlmann, K. System for Layered Construction of a Body and Tray therefore. U.S. Patent US 10,414,091 B2, 2017. [Google Scholar]
- DeSimone, J.M.; Ermoshkin, A.; Ermoshkin, N.; Samulski, E.T. Continuous Liquid Interphase Printing. U.S. Patent US 9,205,601 B2, 8 December 2015. [Google Scholar]
- Tumbletone, J.R.; Shirvanyants, D.; Ermoshkin, N.; Janusziewicz, R.; Johnson, A.R.; Kelly, D.; Chen, K.; Pinschmidt, R.; Rolland, J.P.; Ermoshkin, A.; et al. Additive manufacturing. Continuous liquid interface production of 3D objects. Science 2015, 347, 1349–1352. [Google Scholar] [CrossRef]
- Schweiger, J.; Edelhoff, D.; Stimmelmayr, M.; Güth, J.F.; Beuer, F. Automatisierte Fertigung von mehrschichtigem Frontzahnersatz mithilfe digitaler Dentinkerne. Quintessenz Zahntech. 2014, 40, 1248–1266. [Google Scholar]
- Schweiger, J.; Edelhoff, D.; Stimmelmayr, M.; Güth, J.F.; Beuer, F. Automated production of multilayer anterior restorations with digitally produced dentin cores. Quintessence Dent. Tech. 2015, 38, 207–220. [Google Scholar]
- Schweiger, J.; Trimpl, J.; Schwerin, C.; Güth, J.F.; Edelhoff, D. Biomaterials update—Additive manufacturing: Applications in dentistry based on materials selection. Quintessence Dent. Tech. 2019, 42, 50–69. [Google Scholar]
- Schweiger, J.; Edelhoff, D.; Schubert, O.; Trimpl, J.; Erdelt, K.J.; Güth, J.F. Digitale Modellherstellung—eine Übersicht. Quintessenz Zahntech. 2019, 45, 41–61. [Google Scholar]
- Güth, J.F.; Schubert, O.; Nold, E.; Trimpl, J.; Schweiger, J. Teamdisziplin-3D-Planung und Navigation in der Implantologie. Bayerischer Zahnärzte Blatt 2018, 55, 50–56. [Google Scholar]
- Wöstmann, B.; Powers, M. Präzisionsabformungen—Ein Leitfaden für Theorie und Praxis; 3M ESPE: Seefeld, Germany, 2016. [Google Scholar]
- Wedekind, L.; Güth, J.-F.; Schweiger, J.; Kollmuss, M.; Reichl, F.-X.; Edelhoff, D.; Högg, C. Elution behavior of a 3D-printed, milled and conventional resin-based occlusal splint material. Dent. Mater. 2021, 37, 701–710. [Google Scholar] [CrossRef]
- Lutz, A.-M.; Hampe, R.; Roos, M.; Lümkemann, N.; Eichberger, M.; Stawarczyk, B. Fracture resistance and 2-body wear of 3-dimensional–printed occlusal devices. J. Prosthet. Dent. 2019, 121, 166–172. [Google Scholar] [CrossRef]
- Berli, C.; Thieringer, F.M.; Sharma, N.; Müller, J.A.; Dedem, P.; Fischer, J.; Rohr, N. Comparing the mechanical properties of pressed, milled, and 3D-printed resins for occlusal devices. J. Prosthet. Dent. 2020, 124, 780–786. [Google Scholar] [CrossRef]
- Reymus, M.; Hickel, R.; Kunz, A. Accuracy of CAD/CAM-fabricated bite splints: Milling vs. 3D printing. Clin. Oral Investig. 2020, 24, 4607–4615. [Google Scholar]
- Reymus, M.; Fotiadou, C.; Kessler, A.; Heck, K.; Hickel, R.; Diegritz, C. 3D printed replicas for endodontic education. Int. Endod. J. 2019, 52, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Meglioli, M.; Naveau, A.; Macaluso, G.M.; Catros, S. 3D printed bone models in oral and cranio-maxillofacial surgery: A systematic review. 3D Print. Med. 2020, 6, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Schweiger, J.; Edelhoff, D.; Güth, J.F. Update digitale Fertigung 2020—neueste Entwicklungen in der additiven und subtraktiven Fertigung. Dent. Dialogue 2020, 21, 36–51. [Google Scholar]
- Schweiger, J.; Beuer, F.; Stimmelmayr, M.; Edelhoff, D.; Magne, P.; Güth, J.F. Histo-anatomic 3D printing of dental structures. Br. Dent. J. 2016, 221, 555–560. [Google Scholar] [CrossRef]
- Schweiger, J. Method, Apparatur and Computer Program for Producing a Dental Prosthesis. U.S. Patent US8,775,131,B2, 8 July 2014. [Google Scholar]
- Schweiger, J. Method, Apparatur and Computer Program for Producing a Dental Prosthesis. European Patent Application 2 363 094 B1, 10 July 2013. [Google Scholar]
- Wissenschaftliche Untersuchungen zu VarseoSmile Crown Plus. Available online: http://www.bego.com/de/3d-druck/materialien/varseosmile-crown-plus/wissenschaftliche-untersuchungen (accessed on 10 December 2020).
- Schweiger, J.; Bomze, D.; Schwentenwein, M. 3D-Printing of Zirconia—What is the future? Curr. Oral Health Rep. 2019, 6, 339–343. [Google Scholar] [CrossRef]
- Geier, S.; Potestio, I. 3D-printing: From multi-material to functionally-graded ceramic. Ceram. Appl. 2020, 8, 32–35. [Google Scholar]
- Kessler, A.; Reichl, F.-X.; Folwaczny, M.; Högg, C. Monomer release from surgical guide resins manufactured with different 3D printing devices. Dent. Mater. 2020, 36, 1486–1492. [Google Scholar] [CrossRef]
- Prpić, V.; Schauperl, Z.; Ćatić, A.; Dulčić, N.; Čimić, S. Comparison of mechanical properties of 3D-printed, CAD/CAM, and conventional denture base materials. J. Prosthodont. 2020, 29, 524–528. [Google Scholar] [CrossRef]
- Wemken, G.; Burkhardt, F.; Spies, B.C.; Kleinvogel, L.; Adali, U.; Sterzenbach, G.; Beuer, F.; Wesemann, C. Bond strength of conventional, subtractive, and additive manufactured denture bases to soft and hard relining materials. Dent. Mater. 2021, 37, 928–938. [Google Scholar] [CrossRef]
- Unkovskiy, A.; Schmidt, F.; Beuer, F.; Li, P.; Spintzyk, S.; Fernandez, P.K. Stereolithography vs. direct light processing for rapid manufacturing of complete denture bases: An in vitro accuracy analysis. J. Clin. Med. 2021, 10, 1070. [Google Scholar] [CrossRef]
- Anadioti, E.; Musharbash, L.; Blatz, M.B.; Papavasiliou, G.; Kamposiora, P. 3D printed complete removable dental prostheses: A narrative review. BMC Oral Health 2020, 20, 1–9. [Google Scholar] [CrossRef]















| Filament-Based 3D Printing | Light-Based 3D Printing | Material Jetting | |||
|---|---|---|---|---|---|
| FDM/FFF | SLA | DUP | DLP | MJT | |
| Speed | medium | medium | medium | high | high |
| Resolution | low | high | medium | high | high |
| Size | scalable | scalable | scalable | scalable | scalable |
| Process reliability | medium | medium | low | high | high |
| Cost | low | medium | low | medium to high | high |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schweiger, J.; Edelhoff, D.; Güth, J.-F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J. Clin. Med. 2021, 10, 2010. https://doi.org/10.3390/jcm10092010
Schweiger J, Edelhoff D, Güth J-F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. Journal of Clinical Medicine. 2021; 10(9):2010. https://doi.org/10.3390/jcm10092010
Chicago/Turabian StyleSchweiger, Josef, Daniel Edelhoff, and Jan-Frederik Güth. 2021. "3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing" Journal of Clinical Medicine 10, no. 9: 2010. https://doi.org/10.3390/jcm10092010
APA StyleSchweiger, J., Edelhoff, D., & Güth, J.-F. (2021). 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. Journal of Clinical Medicine, 10(9), 2010. https://doi.org/10.3390/jcm10092010






