Interventions Targeting Bottle and Formula Feeding in the Prevention and Treatment of Early Childhood Caries, Overweight and Obesity: An Integrative Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Questions
- What interventions, trials or programs have been undertaken to support best-practice formula feeding or bottle cessation in infants and children, focusing on either oral health or weight-related outcomes?
- What are the impacts of these interventions on formula feeding practice, bottle cessation, oral health and/or child weight outcomes?
2.2. Eligibility Criteria
2.3. Information Sources
2.4. Search Strategy
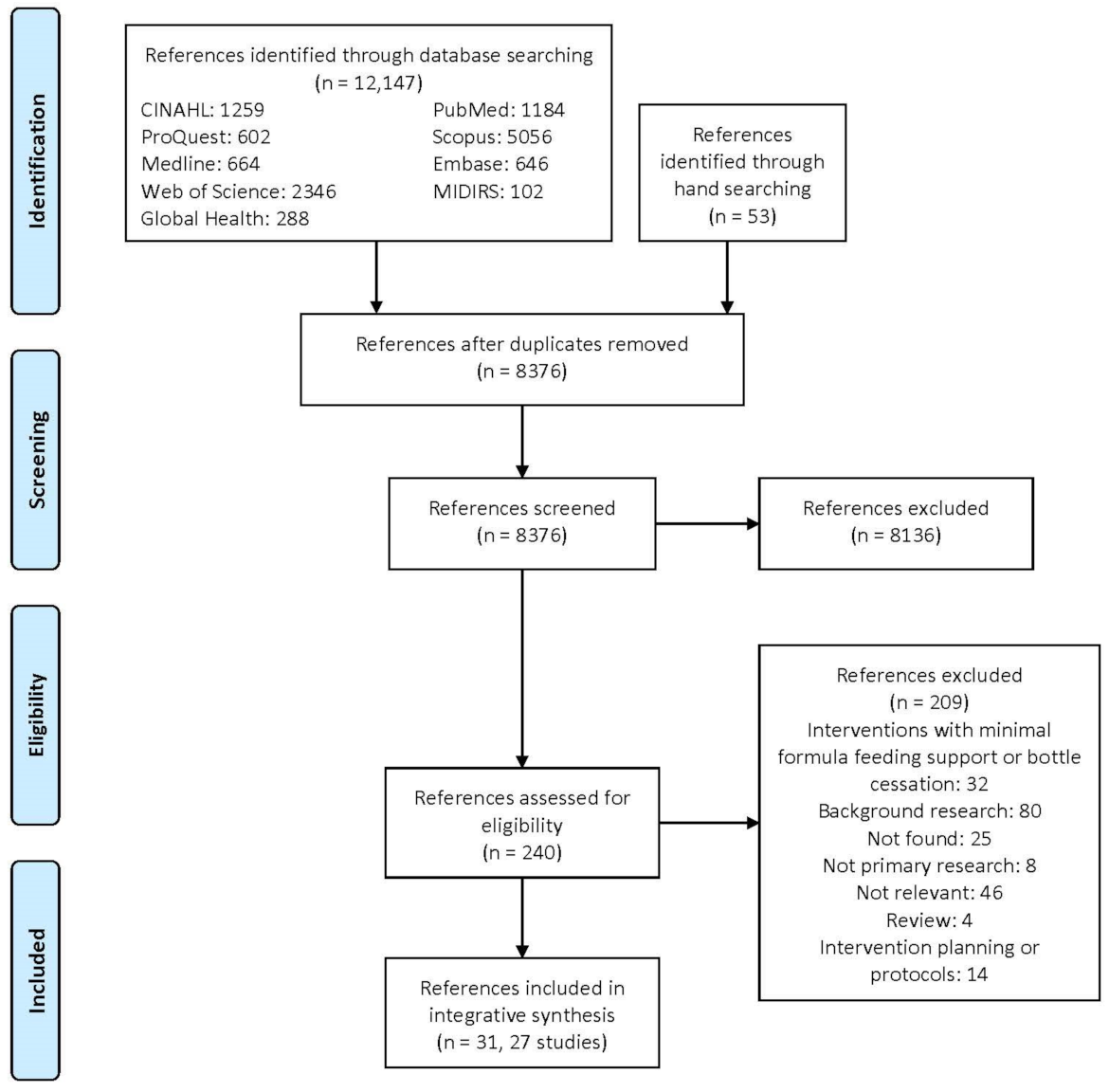
2.5. Study Selection
2.6. Data Extraction and Synthesis
2.7. Quality Assessment
3. Results
3.1. Included Studies
3.2. Participants
3.3. Interventions
3.3.1. Setting and Interventionists
3.3.2. Intervention Content: Education
3.3.3. Intervention Content: Resource Distribution
3.3.4. Intervention Design and Stakeholder Engagement
3.4. Study Outcomes
3.4.1. Weight or Anthropometry
3.4.2. Dental Caries Prevalence
3.4.3. Carer Knowledge and Awareness
3.4.4. Bottle and Cup Use
3.4.5. Cariogenic Dietary Behaviours
3.4.6. Obesogenic Dietary Behaviours
3.4.7. Healthcare Professional Practice
3.5. Critical Appraisal
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Ending Childhood Dental Caries: WHO Implementation Manual; World Health Organisation: Geneva, Switzerland, 2019. [Google Scholar]
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.L.; Marcenes, W. Global Burden of Untreated Caries: A Systematic Review and Metaregression. J. Dent. Res. 2015, 94, 650–658. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Smith, A.G.C.; Bernabé, E.; Fleming, T.D.; Reynolds, A.E.; Vos, T.; Murray, C.J.L.; Marcenes, W. Global, Regional, and National Prevalence, Incidence, and Disability-Adjusted Life Years for Oral Conditions for 195 Countries, 1990–2015: A Systematic Analysis for the Global Burden of Diseases, Injuries, and Risk Factors. J. Dent. Res. 2017, 96, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Casamassimo, P.S.; Thikkurissy, S.; Edelstein, B.L.; Maiorini, E. Beyond the dmft: The Human and Economic Cost of Early Childhood Caries. J. Am. Dent. Assoc. 2009, 140, 650–657. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- George, A.; Sousa, M.S.; Kong, A.C.; Blinkhorn, A.; Patterson Norrie, T.; Foster, J.; Dahlen, H.G.; Ajwani, S.; Johnson, M. Effectiveness of preventive dental programs offered to mothers by non-dental professionals to control early childhood dental caries: A review. BMC Oral Health 2019, 19, 172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anil, S.; Anand, P.S. Early Childhood Caries: Prevalence, Risk Factors, and Prevention. Front. Pediatr. 2017, 5, 157. [Google Scholar] [CrossRef] [Green Version]
- Broadbent, J.M.; Thomson, W.M.; Poulton, R. Trajectory patterns of dental caries experience in the permanent dentition to the fourth decade of life. J. Dent Res 2008, 87, 69–72. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 30 October 2020).
- Lucas, K.; James, P.; Choh, A.C.; Lee, M.; Czerwinski, S.A.; Demerath, E.W.; Johnson, W. The positive association of infant weight gain with adulthood body mass index has strengthened over time in the Fels Longitudinal Study. Pediatr. Obes. 2018, 13, 476–484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Druet, C.; Stettler, N.; Sharp, S.; Simmons, R.K.; Cooper, C.; Smith, G.D.; Ekelund, U.; Lévy-Marchal, C.; Jarvelin, M.R.; Kuh, D.; et al. Prediction of childhood obesity by infancy weight gain: An individual-level meta-analysis. Paediatr. Perinat. Epidemiol. 2012, 26, 19–26. [Google Scholar] [CrossRef]
- Daniels, S.R.; Arnett, D.K.; Eckel, R.H.; Gidding, S.S.; Hayman, L.L.; Kumanyika, S.; Robinson, T.N.; Scott, B.J.; St Jeor, S.; Williams, C.L. Overweight in Children and Adolescents. Circulation 2005, 111, 1999–2012. [Google Scholar] [CrossRef] [Green Version]
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 95–107. [Google Scholar] [CrossRef] [Green Version]
- Manohar, N.; Hayen, A.; Fahey, P.; Arora, A. Obesity and dental caries in early childhood: A systematic review and meta-analyses. Obes. Rev. 2020, 21, e12960. [Google Scholar] [CrossRef]
- Vadiakas, G. Case definition, aetiology and risk assessment of early childhood caries (ECC): A revisited review. Eur. J. Paediatr. Dent. 2008, 9, 114–125. [Google Scholar] [CrossRef]
- Brecher, E.A.; Lewis, C.W. Infant Oral Health. Pediatr. Clin. N. Am. 2018, 65, 909–921. [Google Scholar] [CrossRef]
- Appleton, J.; Russell, C.G.; Laws, R.; Fowler, C.; Campbell, K.; Denney-Wilson, E. Infant formula feeding practices associated with rapid weight gain: A systematic review. Matern. Child Nutr. 2018, 14, e12602. [Google Scholar] [CrossRef] [Green Version]
- Ripa, L.W. Nursing caries: A comprehensive review. Pediatr. Dent. 1988, 10, 268–282. [Google Scholar] [PubMed]
- Gooze, R.A.; Anderson, S.E.; Whitaker, R.C. Prolonged bottle use and obesity at 5.5 years of age in US children. J. Pediatr. 2011, 159, 431–436. [Google Scholar] [CrossRef]
- Bonuck, K.; Kahn, R.; Schechter, C. Is late bottle-weaning associated with overweight in young children? Analysis of NHANES III data. Clin. Pediatr. 2004, 43, 535–540. [Google Scholar] [CrossRef]
- Angelopoulou, M.V.; Beinlich, M.; Crain, A. Early Childhood Caries and Weight Status: A Systematic Review and Meta-Analysis. Pediatr. Dent. 2019, 41, 261–272. [Google Scholar]
- World Health Organization. WHO Expert Consultation on Public Health Intervention against Early Childhood Caries; WHO/NMH/PND/17.1; World Health Organisation: Geneva, Switzerland, 2017. [Google Scholar]
- Abou El Fadl, R.; Blair, M.; Hassounah, S. Integrating Maternal and Children’s Oral Health Promotion into Nursing and Midwifery Practice—A Systematic Review. PLoS ONE 2016, 11, e0166760. [Google Scholar] [CrossRef] [PubMed]
- Taylor, E.; Marino, D.; Thacker, S.; DiMarco, M.; Huff, M.; Biordi, D. Expanding oral health preventative services for young children: A successful interprofessional model. J. Allied Health 2014, 43, e5–e9. [Google Scholar] [PubMed]
- Pollock, A.; Berge, E. How to do a systematic review. Int. J. Stroke 2017, 13, 138–156. [Google Scholar] [CrossRef]
- Murdoch University. Systematic Reviews—Research Guide: Using PICO or PICo. Available online: https://libguides.murdoch.edu.au/systematic (accessed on 30 November 2020).
- Cooper, C.; Booth, A.; Varley-Campbell, J.; Britten, N.; Garside, R. Defining the process to literature searching in systematic reviews: A literature review of guidance and supporting studies. BMC Med. Res. Methodol. 2018, 18, 85. [Google Scholar] [CrossRef]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlet, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; et al. Mixed Methods Appraisal Tool (MMAT) Version 2018: User Guide; McGill University: Montréal, QC, Canada, 2018. [Google Scholar]
- Bonuck, K.; Avraham, S.B.; Lo, Y.; Kahn, R.; Hyden, C. Bottle-weaning intervention and toddler overweight. J. Pediatr. 2014, 164, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Kahn, R.; Bonuck, K.; Trombley, M. Randomized controlled trial of bottle weaning intervention: A pilot study. Clin. Pediatr. 2007, 46, 163–174. [Google Scholar] [CrossRef]
- Weber-Gasparoni, K.; Reeve, J.; Ghosheh, N.; Warren, J.J.; Drake, D.R.; Kramer, K.W.; Dawson, D.V. An effective psychoeducational intervention for early childhood caries prevention: Part I. Pediatr. Dent. 2013, 35, 241–246. [Google Scholar] [PubMed]
- Weber-Gasparoni, K.; Warren, J.J.; Reeve, J.; Drake, D.R.; Kramer, K.W.O.; Marshall, T.A.; Dawson, D.V. An effective psychoeducational intervention for early childhood caries prevention: Part II. Pediatr. Dent. 2013, 35, 247–251. [Google Scholar]
- Kavanagh, K.F.; Cohen, R.J.; Heinig, M.J.; Dewey, K.G. Educational Intervention to Modify Bottle-feeding Behaviors among Formula-feeding Mothers in the WIC Program: Impact on Infant Formula Intake and Weight Gain. J. Nutr. Educ. Behav. 2008, 40, 244–250. [Google Scholar] [CrossRef]
- Ventura, A.K.; Silva Garcia, K.; Meza, M.; Rodriguez, E.; Martinez, C.E.; Whaley, S.E. Promoting Responsive Bottle-Feeding Within WIC: Evaluation of a Policy, Systems, and Environmental Change Approach. J. Acad. Nutr. Diet. 2021, in press. [Google Scholar] [CrossRef]
- Lawrence, H.P.; Romanetz, M.; Rutherford, L.; Cappel, L.; Binguis, D.; Rogers, J.B. Effects of a community-based prenatal nutrition program on the oral health of Aboriginal preschool children in northern Ontario. Probe 2004, 38, 172–188. [Google Scholar]
- Schroth, R.J.; Edwards, J.M.; Brothwell, D.J.; Yakiwchuk, C.A.; Bertone, M.F.; Mellon, B.; Ward, J.; Ellis, M.; Hai-Santiago, K.; Lawrence, H.P.; et al. Evaluating the impact of a community developed collaborative project for the prevention of early childhood caries: The Healthy Smile Happy Child project. Rural Remote Health 2015, 15, 3566. [Google Scholar] [CrossRef] [PubMed]
- Bruerd, B.; Jones, C. Preventing baby bottle tooth decay: Eight-year results. Public Health Rep. 1996, 111, 63–65. [Google Scholar]
- Bruerd, B.; Kinney, M.B.; Bothwell, E. Preventing baby bottle tooth decay in American Indian and Alaska native communities: A model for planning. Public Health Rep. 1989, 104, 631–640. [Google Scholar] [PubMed]
- Jamieson, L.; Smithers, L.; Hedges, J.; Mills, H.; Kapellas, K.; Ha, D.; Do, L.; Ju, X. Follow-up of an Intervention to Reduce Dental Caries in Indigenous Australian Children: A Secondary Analysis of a Randomized Clinical Trial. JAMA Netw. Open 2019, 2, e1915611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jamieson, L.; Smithers, L.; Hedges, J.; Parker, E.; Mills, H.; Kapellas, K.; Lawrence, H.P.; Broughton, J.R.; Ju, X. Dental Disease Outcomes Following a 2-Year Oral Health Promotion Program for Australian Aboriginal Children and Their Families: A 2-Arm Parallel, Single-blind, Randomised Controlled Trial. EClinicalMedicine 2018, 1, 43–50. [Google Scholar] [CrossRef] [Green Version]
- Smithers, L.G.; Lynch, J.; Hedges, J.; Jamieson, L.M. Diet and anthropometry at 2 years of age following an oral health promotion programme for Australian Aboriginal children and their carers: A randomised controlled trial. Br. J. Nutr. 2017, 118, 1061–1069. [Google Scholar] [CrossRef] [Green Version]
- Kowash, M.B.; Pinfield, A.; Smith, J.; Curzon, M.E. Effectiveness on oral health of a long-term health education programme for mothers with young children. Br. Dent. J. 2000, 188, 201–205. [Google Scholar] [CrossRef] [Green Version]
- Braun, P.A.; Widmer-Racich, K.; Sevick, C.; Starzyk, E.J.; Mauritson, K.; Hambidge, S.J. Effectiveness on Early Childhood Caries of an Oral Health Promotion Program for Medical Providers. Am. J. Public Health 2017, 107 (Suppl. S1), S97–S103. [Google Scholar] [CrossRef] [PubMed]
- Davies, G.M.; Duxbury, J.T.; Boothman, N.J.; Davies, R.M.; Blinkhorn, A.S. A staged intervention dental health promotion programme to reduce early childhood caries. Community Dent. Health 2005, 22, 118–122. [Google Scholar]
- Hamilton, F.A.; Davis, K.E.; Blinkhorn, A.S. An oral health promotion programme for nursing caries. Int. J. Paediatr. Dent. 1999, 9, 195–200. [Google Scholar] [CrossRef]
- Joury, E.; Alghadban, M.; Elias, K.; Bedi, R. Impact of providing free preventive dental products without health workers’ counselling on infants’ tooth-brushing and bottle-feeding termination practices: A randomised controlled trial. Community Dent. Health 2016, 33, 213–217. [Google Scholar] [CrossRef]
- Harrison, R.L.; Wong, T. An oral health promotion program for an urban minority population of preschool children. Community Dent. Oral Epidemiol. 2003, 31, 392–399. [Google Scholar] [CrossRef]
- Hoeft, K.S.; Barker, J.C.; Shiboski, S.; Pantoja-Guzman, E.; Hiatt, R.A. Effectiveness evaluation of Contra Caries Oral Health Education Program for improving Spanish-speaking parents’ preventive oral health knowledge and behaviors for their young children. Community Dent. Oral Epidemiol. 2016, 44, 564–576. [Google Scholar] [CrossRef] [Green Version]
- Karasz, A.; Margulis, K.; Badner, V.; Bonuck, K. Reducing Oral Health Risks in South Asian Immigrant Children: A Pilot Study. N. Y. State Dent. J. 2018, 84, 28–33. [Google Scholar]
- Vichayanrat, T.; Steckler, A.; Tanasugarn, C.; Lexomboon, D. The evaluation of a multi-level oral health intervention to improve oral health practices among caregivers of preschool children. Southeast Asian J. Trop. Med. Public Health 2012, 43, 526–539. [Google Scholar] [PubMed]
- Lakshman, R.; Sharp, S.J.; Whittle, F.; Schiff, A.; Hardeman, W.; Irvine, L.; Wilson, E.; Griffin, S.J.; Ong, K.K. Randomised controlled trial of a theory-based behavioural intervention to reduce formula milk intake. Arch. Dis. Child. 2018, 103, 1054–1060. [Google Scholar] [CrossRef]
- Borghese-Lang, T.; Morrison, L.; Ogle, A.; Wright, A. Successful bottle feeding of the young infant. J. Pediatr. Health Care 2003, 17, 94–101. [Google Scholar] [CrossRef]
- Boonrusmee, S.; Cheamsanit, S. Telephone-based counselling helped parents to wean children off bottles at two years of age. Acta Paediatr. 2021, 110, 718–719. [Google Scholar] [CrossRef]
- Franco, S.; Theriot, J.; Greenwell, A. The influence of early counselling on weaning from a bottle. Community Dent. Health 2008, 25, 115–118. [Google Scholar] [CrossRef]
- Maguire, J.L.; Birken, C.S.; Jacobson, S.; Peer, M.; Taylor, C.; Khambalia, A.; Mekky, M.; Thorpe, K.E.; Parkin, P. Office-based intervention to reduce bottle use among toddlers: TARget kids! Pragmatic, randomized trial. Pediatrics 2010, 126, e343–e350. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.K.; Faniyan, A.; Chan Yuen, J.; Myers, T.; Fleck, M.; Burgess, J.; Williams, K.; Wijeratne, R.; Webster, R.; Cox, J.; et al. Changes in Oral Health Behaviors Associated With a Nursing Intervention in Primary Care. Glob. Pediatr. Health 2019, 6, 1–12. [Google Scholar] [CrossRef]
- Koelen, M.A.; Hielkema-De Meij, J.E.; Van Der Sanden-Stoelinga, M.S.E. ‘Bottle it up—take a cup!’ The fight against nursing caries in the Netherlands: The campaign and its results. Int. J. Health Promot. Educ. 2000, 38, 47–53. [Google Scholar] [CrossRef]
- Sgan-Cohen, H.D.; Mansbach, I.K.; Haver, D.; Gofin, R. Community-oriented oral health promotion for infants in Jerusalem: Evaluation of a program trial. J. Public Health Dent. 2001, 61, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Strippel, H. Effectiveness of structured comprehensive paediatric oral health education for parents of children less than two years of age in Germany. Community Dent. Health 2010, 27, 74–80. [Google Scholar] [CrossRef]
- National Health Service UK. Health Visitor. Available online: https://www.healthcareers.nhs.uk/explore-roles/public-health/roles-public-health/health-visitor (accessed on 22 October 2020).
- Winnipeg Regional Health Authority. Early Childhood Tooth Decay. Available online: https://wrha.mb.ca/oral-health/early-childhood-tooth-decay/ (accessed on 22 October 2020).
- Hyden, C.; Kahn, R.; Bonuck, K. Bottle-weaning intervention tools: The “how” and “why” of a WIC-based educational flipchart, parent brochure, and website. Health Promot. Pract. 2013, 14, 75–80. [Google Scholar] [CrossRef] [PubMed]
- van der Sanden-Stoelinga, M.S.; Koelen, M.A.; Hielkema-de Meij, J.E. The making of a nation-wide campaign fighting the nursing caries. Int. J. Dent. Hyg. 2003, 1, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Lakshman, R.; Landsbaugh, J.R.; Schiff, A.; Cohn, S.; Griffin, S.; Ong, K.K. Developing a programme for healthy growth and nutrition during infancy: Understanding user perspectives. Child: Care Health Dev. 2012, 38, 675–682. [Google Scholar] [CrossRef]
- Hoeft, K.S.; Rios, S.M.; Guzman, E.P.; Barker, J.C. Using community participation to assess acceptability of “Contra Caries”, a theory-based, promotora-led oral health education program for rural Latino parents: A mixed methods study. BMC Oral Health 2015, 15, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Matvienko-Sikar, K.; Griffin, C.; Kelly, C.; Heary, C.; Lillholm Pico Pedersen, M.; McGrath, N.; Toomey, E.; Harrington, J.; Hennessy, M.; Queally, M.; et al. A core outcome set for trials of infant-feeding interventions to prevent childhood obesity. Int. J. Obes. 2020, 44, 2035–2043. [Google Scholar] [CrossRef]
- Lamont, T.; Schwendicke, F.; Innes, N. Why we need a core outcome set for trials of interventions for prevention and management of caries. Evid. Based Dent. 2015, 16, 66–68. [Google Scholar] [CrossRef]
- Kelly, M.P.; Barker, M. Why is changing health-related behaviour so difficult? Public Health 2016, 136, 109–116. [Google Scholar] [CrossRef] [Green Version]
- Teixeira, P.J.; Marques, M.M. Health Behavior Change for Obesity Management. Obes. Facts 2017, 10, 666–673. [Google Scholar] [CrossRef]
- Freeman, R.; Stevens, A. Nursing caries and buying time: An emerging theory of prolonged bottle feeding. Community Dent. Oral Epidemiol. 2008, 36, 425–433. [Google Scholar] [CrossRef] [PubMed]
- Kuswara, K.; Laws, R.; Kremer, P.; Hesketh, K.D.; Campbell, K.J. The infant feeding practices of Chinese immigrant mothers in Australia: A qualitative exploration. Appetite 2016, 105, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Karasz, A.; Patel, V.; Ranasinghe, S.; Chaudhuri, K.; McKee, D. Preventing caries in young children of immigrant Bangladeshi families in New York: Perspectives of mothers and paediatricians. Community Dent. Health 2014, 31, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Rehayem, A.; Taki, S.; Brown, N.; Denney-Wilson, E. Infant feeding beliefs and practices of Arabic mothers in Australia. Women Birth 2019, 33, e391–e399. [Google Scholar] [CrossRef] [PubMed]
- Hunter-Adams, J.; Myer, L.; Rother, H.-A. Perceptions related to breastfeeding and the early introduction of complementary foods amongst migrants in Cape Town, South Africa. Int. Breastfeed. J. 2016, 11, 29. [Google Scholar] [CrossRef] [Green Version]
- Wandel, M.; Terragni, L.; Nguyen, C.; Lyngstad, J.; Amundsen, M.; de Paoli, M. Breastfeeding among Somali mothers living in Norway: Attitudes, practices and challenges. Women Birth 2016, 29, 487–493. [Google Scholar] [CrossRef]
- Beck, A.; Takayama, J.; Halpern-Felsher, B.; Badiner, N.; Barker, J. Understanding How Latino Parents Choose Beverages to Serve to Infants and Toddlers. Matern. Child Health J. 2014, 18, 1308–1315. [Google Scholar] [CrossRef]
- Arora, A.; Lucas, D.; To, M.; Chimoriya, R.; Bhole, S.; Tadakamadla, S.K.; Crall, J.J. How Do Mothers Living in Socially Deprived Communities Perceive Oral Health of Young Children? A Qualitative Study. Int. J. Environ. Res. Public Health 2021, 18, 3521. [Google Scholar] [CrossRef]
- Chestnutt, I.G.; Murdoch, C.; Robson, K.F. Parents and carers’ choice of drinks for infants and toddlers, in areas of social and economic disadvantage. Community Dent. Health 2003, 20, 139–145. [Google Scholar]
- Borrelli, B.; Tooley, E.M.; Scott-Sheldon, L.A.J. Motivational Interviewing for Parent-child Health Interventions: A Systematic Review and Meta-Analysis. Pediatr. Dent. 2015, 37, 254–265. [Google Scholar] [PubMed]
- Harris, R.; Gamboa, A.; Dailey, Y.; Ashcroft, A. One-to-one dietary interventions undertaken in a dental setting to change dietary behaviour. Cochrane Database Syst. Rev. 2012, 2012, Cd006540. [Google Scholar] [CrossRef]
- Henshaw, M.M.; Borrelli, B.; Gregorich, S.E.; Heaton, B.; Tooley, E.M.; Santo, W.; Cheng, N.F.; Rasmussen, M.; Helman, S.; Shain, S.; et al. Randomized Trial of Motivational Interviewing to Prevent Early Childhood Caries in Public Housing. JDR Clin. Trans. Res. 2018, 3, 353–365. [Google Scholar] [CrossRef] [Green Version]
- John Buhler Research Centre. Healthy Smile Happy Child: The Manitoba Partnership for the Prevention of Early Childhood Tooth Decay; John Buhler Research Centre: Winnipeg, MB, Canada, 2017. [Google Scholar]
- Cidro, J.; Zahayko, L.; Lawrence, H.P.; Folster, S.; McGregor, M.; McKay, K. Breast feeding practices as cultural interventions for early childhood caries in Cree communities. BMC Oral Health 2015, 15, 49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NSW Ministry of Health. Early Childhood Oral Health Guidelines for Child Health Professionals; NSW Health: Sydney, Australia, 2014. [Google Scholar]
- Maher, L.; Phelan, C.; Lawrence, G.; Torvaldsen, S.; Dawson, A.; Wright, C. The Early Childhood Oral Health Program: Promoting prevention and timely intervention of early childhood caries in NSW through shared care. Health Promot. J. Austr. 2012, 23, 171–176. [Google Scholar] [CrossRef]
- Ajwani, S.; Sousa, M.S.; Villarosa, A.C.; Bhole, S.; Johnson, M.; Dahlen, H.G.; Hoolsema, J.; Blinkhorn, A.; Srinivas, R.; Yaacoub, A.; et al. Process evaluation of the midwifery initiated oral health-dental service program: Perceptions of dental professionals. Health Promot. J. Austr. 2019, 30, 333–343. [Google Scholar] [CrossRef] [PubMed]
- Dahlen, H.G.; Johnson, M.; Hoolsema, J.; Norrie, T.P.; Ajwani, S.; Blinkhorn, A.; Bhole, S.; Ellis, S.; Srinivas, R.; Yaacoub, A.; et al. Process evaluation of the midwifery initiated oral health-dental service program: Perceptions of midwives in Greater Western Sydney, Australia. Women Birth 2019, 32, e159–e165. [Google Scholar] [CrossRef]
- George, A.; Villarosa, A.; Patterson Norrie, T.; Hoolsema, J.; Dahlen, H.; Ajwani, S.; Bhole, S.; Blinkhorn, A.; Srinivas, R.; Yaacoub, A.; et al. Process evaluation of the midwifery initiated oral health-dental service program: Perceptions of pregnant women. Aust. Dent. J. 2019, 64, 55–65. [Google Scholar] [CrossRef] [Green Version]
- Centre for Oral Health Outcomes and Research Translation. COHORT Research Report, 2015–2020; Western Sydney University, South Western Sydney Local Health District, Nepean Blue Mountains Local Health District, Ingham Institute for Applied Medical Research: Liverpool, Australia, 2020. [Google Scholar]
- Dental Health Services Victoria. Healthy Families, Healthy Smiles. Available online: https://www.dhsv.org.au/oral-health-programs/hfhs (accessed on 8 February 2021).
- Fitzgerald, L.; Peace, J. Healthy Tums, Healthy Gums: An oral health and nutrition collaboration. In Proceedings of the 12th National Rural Health Conference, Adelaide, Australia, 7–10 April 2013. [Google Scholar]
- Karasz, A.; Bonuck, K. Reducing pediatric caries and obesity risk in South Asian immigrants: Randomized controlled trial of common health/risk factor approach. BMC Public Health 2018, 18, 680. [Google Scholar] [CrossRef] [Green Version]
- Chomitz, V.R.; Park, H.J.; Koch-Weser, S.; Chui, K.K.H.; Sun, L.; Malone, M.E.; Palmer, C.; Loo, C.Y.; Must, A. Modifying dietary risk behaviors to prevent obesity and dental caries in very young children: Results of the Baby Steps to Health pediatric dental pilot. J. Public Health Dent. 2019, 79, 207–214. [Google Scholar] [CrossRef]
- Cheng, H.; Eames-Brown, R.; Tutt, A.; Laws, R.; Blight, V.; McKenzie, A.; Rossiter, C.; Campbell, K.; Sim, K.; Fowler, C.; et al. Promoting healthy weight for all young children: A mixed methods study of child and family health nurses’ perceptions of barriers and how to overcome them. BMC Nurs. 2020, 19, 84. [Google Scholar] [CrossRef] [PubMed]
| Reference. Country | Aim | Study Type; Period | IG and CG Sample | IG and CG Description | Key Findings |
|---|---|---|---|---|---|
| Bonuck et al. 2014. USA. | To evaluate the impact of a WIC-based counselling intervention on bottle use and WFL. | RCT; 2008–2011. | Infants aged 11–13 months, consuming > 2 bottles of milk or juice daily, in USA WIC program. IG: n = 149 at baseline; 49 after 12 months. CG: n = 150 at baseline; 55 after 12 months. | IG: Resources distributed: pamphlet, sippy cup. Education, during 12 months. WIC visit: healthy weight, ECC, iron deficiency, based on precaution adoption process model. CG: Regular WIC care. | At 24 months: NS difference in risk of overweight (WFL > 85th percentile). NS difference in mean daily number of bottles used; mean daily number of sippy cups used; prevalence of any bottle use, prevalence of any sippy cup use; mean fluid intake from bottles; mean fluid intake from sippy cups. |
| Borghese-Lang et al. 2003. USA. | To develop an informational handout on FF and assess parental evaluation of its usefulness. | Quasi-experimental trial; April–May 2002. | Exclusively FF infants from birth to 4 months. IG: 31 handouts distributed; 22 parents followed up by telephone. CG: N/A. | IG: Development of information handout on successful formula feeding, with 5.5 grade reading level, and distributed to parents at well-baby visits. CG: N/A | 19 (86%) read handout. 18 (of 19) increased understanding of bottle feeding after reading handout. |
| Boonrusmee et al. 2021. Thailand. | To evaluate a novel telephone-based intervention on bottle cessation. | RCT; January 2018–March 2019. | Bottle-fed children, 21–24 months, attending routine well-child visit. IG: 51; 46 completers. CG: 51; 46 completers. | IG: Telephone call at 3 and 6 weeks after receiving routine outpatient advice: motivational interviewing on bottle cessation, individual counselling to support weaning. CG: Routine outpatient advice on bottle cessation. | At 8 weeks: Increased bottle cessation: 41.3% vs. 17.4%, p = 0.022. |
| Braun et al. 2017. USA. | To assess an oral health promotion intervention for medical providers’ impact on ECC in children aged 36–42 months. | Quasi-experimental trial; 2009–2015. | 8 Denver Health federally qualified health centres—89% of paediatric patients living below federal poverty line. IG: n = 1646 in 2011, receiving fluoride varnish application; n = 1708 in 2015. CG: 2009 pre-intervention cohort. n = 1501, receiving fluoride varnish application. | IG: ECC risk assessment and fluoride varnish, from 6 months to 3 years. Resources distributed: oral health kit with toothbrush, toothpaste. Education: bottle cessation, water intake, limit snacking. Self-management goal sheet handout. CG: Pre-intervention usual care. | Post-program evaluation of children from 2009 (pre-intervention), 2011 (mid-intervention) and 2015 cohorts. At 36–42 months: Decreased ECC: 46.5%, 57.6% and 37.3%, p < 0.001. Increased bottle cessation: use of bottles in 7.9%, 8.1% and 2%, p = 0.03. Decreased use of non-water sippy cups in bed: 87.1%, 76.0% and 78.4%, p = 0.005. NS difference in non-water bottle use in bed; bottle cessation at bedtime. Increased snacking between meals: 59.9%, 64.8% and 75.2%, p = 0.01. |
| Bruerd et al. 1989. Bruerd et al. 1996. USA. | To prevent baby bottle tooth decay in 12 First Nations American communities, by 50% over 5 years. | Experimental community program; 1986–1989, with follow-up in 1994. | First Nations American communities. IG: 2 × 4 pilot sites, at high and medium intensity, intensity varied on training of interventionists. n = 928 screened in 1985; 932 screened in 1989. CG: 4 pilot sites, at low intensity. n = 455 screened in 1985; 640 screened in 1989. | IG: Community championship for parent education. Resources distributed: counselling booklets, two-handled cups, posters, stickers. Education: bottle cessation and cup use by 1 year age. Media and advertising. CG: Site coordinators received educational materials but no training. | After 4 years in 1989: 33%, 18% and 27% reduction in prevalence of ECC in high-, medium- and low-intensity intervention sites (p < 0.001 each). Overall, 25% reduction in ECC across all sites (p < 0.001). At 4 years follow-up in 1994 (after funding cessation in 1990), compared with 1986 baseline: - 25% reduction in ECC across all sites (p < 0.001). - 38% reduction in ECC, in 5 sites with ongoing program (p < 0.001). - 13% reduction in ECC, in 7 sites who ceased program in 1989 (NS, p-value NR). |
| Cheng et al. 2019. USA. | To modify oral health behaviours after a nursing intervention targeted at children with ECC risk. | Retrospective longitudinal study, intervention and annual training in 2010–2015, clinical records April 2013–June 2015 evaluated. | Children, 9 months to 4.9 years age, with ≥2 documented ECC risk assessments, attending well-child visits across two urban clinics. n = 2097. | IG: Fluoride varnish applied. Education targeted to risk factors, using flipchart: caries aetiology, sugar content, bottle/sippy cup use, teeth brushing instructions with adult supervision. Resources distributed: toothbrushes and toothpaste. CG: N/A, pre-intervention care. | From visit 1 (baseline) to visits 2 and 3 (follow-up): ~33% children with non-water bottle/sippy cup use in bed at visits 1, 2 and 3. NS increase in SSB intake, p = 0.05: - 1–2 serves/day, 37.2% vs. 41.6% and 43% - ≥3 serves/day, 11.5% vs. 15.6% and 15.7%. NS difference in frequency of ECC: 3.5% vs. 4.7% and 3.5%, p = 0.413. |
| Davies et al. 2005. UK. | To assess the effects of a multi-stage dental health promotion programme in reducing ECC. | Cluster RCT; 1999–2003. | 8 month infants, attending health development checks, in socially deprived inner-city area without fluoridated water. IG: randomly sampled children from a Primary Care Group. n = 649 → 79 respondents at 21 months; 190 at 3–4 years assessment. CG: randomly sampled children. n = 558 → 89 respondents at 21 months; 148 at 3–4 years assessment. | IG: Resources distributed: toothpaste, toothbrush, education leaflet, trainer cup. Education: bottle cessation, cup use, safe drinks, teeth brushing instructions. Intervention at 8 months, 12–15 months, 18 months, 26 months and 32 months of age. CG: Usual care and standard development checks. | At 21 months: Increased bottle cessation: 33% in IG vs. 18% in CG, p = 0.04. Increased limited bottle use only at bedtime, by bottle-using children: 43% in IG vs. 62% in CG, p = 0.02. Decreased cup use for only drinking unsafe (cariogenic) drinks: 13% in IG vs. 30% in CG, p = 0.02. NR difference in non-cariogenic drink use in bottles; trainer cup use at 21 months; cup use for combined cariogenic and non-cariogenic drinks. At 3 to 4 years: Decreased prevalence of ECC at <3 years age: 16.6% in IG vs. 23.5% in CG, p = 0.003. Decreased prevalence of ECC at ≥3 years age: 28.7% in IG vs. 39.2% in CG, p = 0.001. |
| Franco et al. 2008. USA. | To evaluate the effectiveness of intensive counselling on bottle cessation. | RCT; September 1999-June 2002. | 4 month infants, predominantly AA, attending well-child visit. IG: n = 67 parent/infant dyads at 12 months. CG: n = 65 parent/infant dyads at 12 months. | IG: Education at 4 months, 6 months, 9 months and 12 months: bottle cessation, transition to cup use at 9 months. CG: Education: brief counselling on cup use at 6 months, bottle cessation at 9 months and 12 months. | At 12–24 months: NS difference in prevalence of ECC; bottle cessation. Increased knowledge of bottle cessation by 12 months age: 49% of IG parents vs. 68% of CG parents, p = 0.049. |
| Hamilton et al. 1999. UK. | To evaluate an oral health promotion programme provided by HV, directed at mothers of 8 month infants. | Quasi-experimental trial; cross-sectional surveys with historical CG Nov 1996 and IG Nov 1997. | Mothers of ~1 year children, seen by HVs from a community healthcare centre in a deprived inner-city area. IG: n = 182 mothers, randomly selected from Child Health Register. CG: n = 170 mothers, randomly selected. | IG: Resources distributed at 8 month well-child visit: feeder cup, toothbrush, toothpaste. Education: information handout, re: safe drinks for infants, sugar-free medication, dental registration. CG: N/A, pre-trial usual care. | Increased mothers recall HVs talking about using feeder cup instead of bottle: 93% post-trial vs. 54% pre-trial, p < 0.001. Increased mothers recall HVs talking about limiting sugary food and drink: 91% post-trial vs. 62% pre-trial, p < 0.001. |
| Harrison et al. 2003. Canada. | To design, implement and evaluate an oral health promotion program for inner-city Vietnamese preschool children. | Community program; 1994–2001 (approx.). | Vietnamese mothers with infants attending well-child visits. IG: mothers-child dyads followed up after counselling clinic; n = 25, 1994; n = 25, 1998; n = 17, 2001. CG: children of a similar age from neighbouring Vietnamese community. n = 14 baseline, n = 9 comparison children. | IG: Education, during 2 month, 4 month, 6 month, 12 month and 18 month well-child check: avoid bottle use in bed, teeth cleaning, transition to cup use. Resource distribution: toothbrush, training cup. Community outreach. CG: No intervention. | At 1996 follow-up clinic, at children 18 months age: For IG children, compared to baseline and comparison children: - decreased daytime bottle use: 6.3% vs. 83.3% and 55.6%, p < 0.05. - decreased bottle use in bed: 13.3% vs. 69.2% and 55.6%, p < 0.05. For IG cohorts at 1994 baseline and 1998 and 2001 follow-up: - decreased daytime bottle use: 81.8%, 0% and 11.8%, p < 0.05. - decreased bottle use in bed: 66.7%, 12.0% and 11.8%, p < 0.05. - cessation of bottle use by 2 years: 13%, 83.3% and 88.2%, p < 0.05. |
| Hoeft et al. 2016. USA. | To determine program effectiveness of parents’ oral health knowledge and behaviours for their young children. | Quasi-experimental trial; August-December 2011, final survey follow-up March 2012. | Low-income Spanish-speaking parents/carers of children aged 0–5 years. IG: n = 105 enrolments, with n = 95 post-intervention and n = 79 3 months post-intervention. CG: N/A. | IG: Education: caries aetiology, toothbrushing behaviours, reducing sugar intake, snacking and bottle use, dental visits. Behaviour management and goal setting on tooth brushing. CG: N/A. | 13 children using a bottle at baseline, with 3 children ceasing bottle use by 3 months post-intervention. Increased children having limited (<1/day) sweet drink intake: 33% baseline vs. 77% post-Intervention, p = 0.0082. NS long-term difference: 77% post-intervention vs. 63% 3 months post-intervention, p = 0.1306. NS difference in limited (<1/day) sweet food intake, across baseline, post-intervention and 3 months post-intervention. Increased oral health knowledge (scored out of 16): 12.8 ± 1.6 baseline vs. 15.2 ± 0.7 post-intervention, p < 0.0001. NS difference in oral health knowledge post-intervention and 3 months post-intervention. Includes: increased correct response that sippy cup for milk consumption at bedtime is bad for children’s teeth: 66% baseline vs. 96% post-intervention. |
| Joury et al. 2016. Syria. | To investigate the impact of an integrated oral health promotion intervention, within a national immunisation programme, on tooth-brushing and bottle-feeding termination practices. | Pilot RCT: 2 parallel CGs, 1 IG; March-May 2013. | Mothers of 1 year old infants, attending an infant vaccination clinic. IG: n = 32. CG 1: n = 30. CG 2: n = 30. | IG: Resource distribution: trainer cup, toothbrush, toothpaste. Education: information pamphlet on bottle cessation, cup use, tooth brushing. CG 1: Oral health information pamphlet. CG 2: No intervention. | 100% infants bottle feeding at baseline. Increased bottle cessation at 1 month follow-up: 18.8% bottle use in IG vs. 69.2% in CG 1 and 93.8% in CG 2, p < 0.001. |
| Kahn et al. 2007. USA. (Pilot study to Bonuck et al. 2014). | To pilot test a standardised protocol for bottle cessation by parents in WIC program. | Pilot RCT; dates NR. | Infants aged 18–30 months, who consumed >3 bottles daily, attending WIC program. IG: n = 18 retained at follow-up. CG: n = 21 retained at follow-up. | IG: Education: parental style, parent’s feelings about bottle use, bottle cessation protocol, usual WIC care. Resources distributed: sippy cup. CG: Usual WIC care. | Decreased daily bottle use: 0.9 in IG vs. 2.2 in CG, p < 0.05. NS difference in bottle cessation; type of beverage consumed in bottles (milk, juice, sweet beverages). |
| Karasz et al. 2018. (Pilot study to Karasz et al. 2018) USA. | To pilot the acceptability and feasibility of an oral health prevention program, conducted by community health workers, for South Asian children at high risk of ECC. | Pilot RCT; dates NR. | Bangladeshi immigrant mothers with a 6–18 month infant. IG: n = 38, 31 at follow-up. CG: n = 21, 21 at follow-up. | IG: Enhanced usual care: 2 home visits, 3 follow-up phone calls after 3 months, 6 months, 9 months. Motivational interviewing and education: oral health education, set goals on change on bottle feeding, develop action plan. CG: Enhanced usual care. Education: oral health pamphlet, 5 min oral health counselling, referral to local dentists. | Decreased total and nap/night-time bottle intake in IG vs. CG, p-value NR, p-value significant. NS decrease in total bottles with added solids/sweeteners; SSBs; sweets. 150% increase in bottle use in CG from baseline; 36% decrease in IG from baseline. |
| Kavanagh et al. 2008. USA. | To evaluate whether education about infant satiety cues would alter FF practices and infant formula intake and weight gain. | RCT; dates NR. | Carers of exclusively FF infants aged 3–10 weeks, attending WIC. IG: n = 44, 19 completed final data collection. CG: n = 57, 21 completed final data collection. | IG: Education, replacing usual WIC class: infant feeding, avoid preparation of excessive formula, awareness of infant satiety, discouraging use of >6 oz formula bottles. CG: General guidance on infant feeding. | At 20–27 weeks: Increased adjusted mean weight: 7214 g in IG vs. 6758 g in CG, p = 0.006. Increased weight gain per week: 195.3 in IG vs. 156.1 g in CG, p = 0.008. Increased adjusted mean length: 64.2 cm in IG vs. 63.3 cm in CG, p = 0.02. Increased length gain per week: 0.70 cm in IG vs. 0.63 cm in CG, p = 0.045. NS difference in final formula intake (mL/24 h), change in formula intake from baseline to end of study, % of bottles emptied at baseline and end of study and % of >6 oz bottles offered at baseline and end of study. |
| Koelen et al. 2000. The Netherlands. | To evaluate the effect of an ECC prevention, implemented a nationwide scale, on increasing knowledge and awareness in HCPs; motivate caries prevention discussions from HCPs to parents; increase parental awareness of prolonged bottle use and increase transition from bottle to cup at 9 months. | Quasi-experimental national trial; May 1995–1997. | Parents of 0–4 year children, specifically in 9–18 month range. IG: n = 60 local child health centres contacted for post-program evaluation → 40 centres, 73 HCPs and 102 parents (53 participating in pre-program evaluation) participated. CG: n = 20 local child health centres contacted for pre-program evaluation → 16 centres, 22 HCPs and 135 parents participated. | IG: Campaign in primary, secondary and tertiary services. Resources distributed for interventionists and parents: colouring and message sheets; visual resources; tear-off pads. Education by dental hygienists and oral health workers. CG: N/A. | At 1.5-year program evaluation: Increased discussion by HCPs on transitioning from bottle to cup: 27% post-program vs. 15% pre-program. No change in discussion of ECC by HCPs: ~75% pre- and post-program. Decreased HCPs that warn against incorrect bottle use: 24% post-program vs. 75% pre-program. Increased parental awareness of ECC: 78% post-program vs. 60% pre-program, p < 0.05. Decreased parental use of bottles: 88% vs. 64% of new parents, p < 0.001. Decreased frequency of bottle use, post-program compared to pre-program: - 1/day, 34% vs. 6% - 2/ day, 31% vs. 21% - 3/day, 11% vs. 33% - >3/day, 23% vs. 39%, p < 0.001. Increased frequency of switching from bottle to cup before 12 months: 88% post-program vs. 72% pre-program, p < 0.1 (NB: p-value as reported by authors). |
| Kowash et al. 2000. UK. | To determine the effect of dental health education on caries incidence in infants, through regular home visits by trained dental health educators over a period of 3 years. | Quasi-experimental trial with cohort design of interventions of varying intensity; dates NR. | Mothers with children born between Jan and September 1995, residing in a deprived area with high caries prevalence. IG A: n = 60. IG B: n = 59. IG C: n = 60. IG D: n = 40. CG: n = 55. | IG: Intervention A or B: dental health education, focused on diet or oral hygiene. Intervention C: Intervention A + B. Intervention A–C: 15 min dental health education at HV every 3 months from 0–2 years, then twice/year for 1 year. Intervention D: Intervention C, but only one year home visit. Education: replace bottle with cup, tooth brushing, regular dental attendance. CG: No intervention. | At 3 years: CG children with more frequent consumption of sweets, p < 0.001, c.f. all IG: - 33% in CG, vs. 9% in IG A, 0% in IG B, 2% in IG C and 8% in IG D, with >1/day sweet consumption - 5% in CG, vs. 58% in IG A, 64% in IG B, 45% in IG C and 50% in IG D, with 1/week sweet consumption Decreased ECC prevalence: 2 (4%) in IG A vs. 18 (33%) in CG, p < 0.001. IG children with more frequent limited sweet consumption, after meals only, or on weekends only: 33% in CG, vs. 75% in IG A, 70% in IG B, 63% in IG C and 62% in IG D, p-value NR. |
| Lakshman et al. 2018. UK. | To assess the efficacy of a theory-based behavioural intervention to prevent RWG in FF infants. | RCT; March 2011–June 2015. | Healthy, full-term infants FF within 14 weeks of birth. IG: n = 340 at baseline, 293 at 12 mo. CG: n = 329 at baseline, 293 at 12 mo. | IG: 3 face-to-face and 2 phone contact visits with nurse facilitator until infant 6 months. Education: reduce formula intake; use responsive feeding; monitor growth. Action planning, goal setting and coping planning. CG: Other FF education: equipment sterilisation, formula preparation, parenting, sleep. | At 6 months: Reduced milk intake: 836.1 mL/day in IG vs. 895.9 mL/day in CG. Difference = −59.7 (−91.1 to −28.3), p-value NR. At 12 months: NS mean change in weight SDS; BMI SDS; RWG prevalence. |
| Lawrence et al. 2004. Canada. | To evaluate the effectiveness of the dental hygiene-coordinated prenatal nutrition program, delivered by community-based nutrition educators, on dental health and child feeding habits; child oral health status; and early childhood obesity. | Cross-sectional longitudinal evaluation of community program; launched mid−1996. | Carers of infants born in June 1996-Feburary 1999, in the First Nations reserve. IG: n = 230 in 2001, 215 responses; n = 367 in 2002, 217 responses. CG: n = 241 in 2001, 182 responses; n = 338 in 2002, 158 responses. | Resources distributed: two-handled cup, toothbrush, dental information sheets. Education, in prenatal program: nutrition and dental prevention. Community campaign. IG: 4 ‘high intensity’ sites with ≥70% distribution of program’s oral health promotion materials to mothers. CG: 4 ‘low intensity’ sites, with ≤10% distribution of program’s oral health promotion materials to mothers. | At 2–5 years, comparing high-intensity sites to low-intensity sites in 2001 and 2002: Increased oral health knowledge (including topics on bottle use for child soothing; SSB, formula or milk damaging children’s teeth; and ad libitum bottle feeding of older children) in high-intensity group in 2001 (p < 0.001) and 2002 (p < 0.05), c.f to low-intensity group. Decreased rate of ever bottle feeding, 78.4% and 80.1% vs. 86% and 88.6%, p < 0.05; however, NS difference in rates of breastfeeding. NS difference in age of bottle-feeding initiation; number of sugary snacks eaten per day; use of sugar/honey-dipped baby pacifiers; age of bottle cessation; continued bottle use at 2–5 years. Increased bottle use outside of meals by high-intensity group: during nap time, p = 0.01; and bedtime, p = 0.018, in 2001. Decreased bottle use outside of meals by high-intensity group: ‘always’ during child crying, 15.9% vs. 31.2%, p = 0.009, in 2002. NS difference in BMI weight categories in 2001. Increased normal weight children, 54.5% vs. 40.5%; decreased ‘at risk of overweightness’ children (BMI ≥ 85th to <95th), 16.2% vs. 24.7; and decreased overweightness children (≥95th BMI), 25.8% vs. 31.8%, p = 0.023, in high-intensity vs. low-intensity group in 2002. For 2001 respondents: Similar prevalence of ECC at 2 years and 3 years age; decreased ECC at 4 years age: 49.1% in high-intensity vs. 67.8% in low-intensity group, p < 0.05. For 2002 respondents; Trend towards decreasing unregulated bottle sipping by child during the day in high-intensity vs. low-intensity group, p = 0.052. Cariogenic fluid use in bottles similar, with decreased sugar-sweetened cariogenic fluid use in bottles, in high-intensity vs. low-intensity group: cow’s milk, 28.1% vs. 14.3%; condensed milk (sweetened evaporated milk), 23.3% vs. 48.6%; formula, 25.3% vs. 18.6%; fruit juice, 12.3% vs. 8.6%; sweetened water/tea, 8.2% vs. 7.1%, overall, p = 0.001. High, but decreased, addition of sugar or sweetener to bottles, 34.5% in high-intensity vs. 55.4% low-intensity group, p < 0.001. NS difference in current or ongoing two-handled cup use. Earlier initiation of two-handled cup: 13.9 ± 0.6 months vs. 15.7 ± 0.7 months, p = 0.048. |
| Maguire et al. 2010. Canada. | To determine education for parents of 9 month infants can reduce bottle use and anaemia at 2 years of age. | RCT; 2006–2007. | Healthy 9 month infants, attending routine paediatrician health visit. IG: n = 129, 126 at 15 mo, 102 followed up at 2 years. CG: n = 122, 99 followed up at 2 years. | IG: Education, during 9 month visit: iron-deficiency anaemia risk, tooth decay, limit milk talk. Repeat education at 15 month if child still using cup. Resources distributed: sippy cup, bottle cessation protocol. CG: Standardised nutrition counselling: iron-rich first foods, solid food feeding, food safety, limit fruit juice. | At 2 years: Decreased bottle use during day: 15% in IG vs. 40% in CG, p = 0.0004. Decreased bottle use in bed: 3% in IG vs. 10% in CG, p = 0.05. Earlier cup use: median 9 months in IG vs. 12 months in CG, p = 0.001. Earlier bottle cessation: median 12 months in IG vs. 16 months in CG, p = 0.004. NS difference in daily milk and juice intake. |
| Jamieson et al. 2018. Jamieson et al. 2019. Smithers et al. 2017. Australia. | To investigate whether a culturally appropriate multi-faceted oral health promotion intervention reduced Aboriginal children’s intake of sugars from discretionary foods at 2 years of age. | Parallel RCT; February 2011–May 2012. | South Australian mothers, pregnant or giving birth to a baby with Aboriginal Australian ethnicity within 6 weeks. IG: n = 223 mothers, 224 infants—159 received intervention; 148 children followed up at 2 years. n = 225 mothers, 230 infants—165 received intervention; 145 children followed up at 2 years. | IG: Motivational interviewing and education at pregnancy, 6 months, 12 months and 18 months infant age, with home visits: oral health, diet, dental treatment, fluoride varnish, caries aetiology from sugary foods and drinks, reduce sugary and cariogenic foods, no SSBs in bottles at night. Goal planning for addressing barriers. CG: Delayed intervention, at 24 months, 30 months and 36 months child age. | At 2 years: Increased infant weight z-score: 0.9 in IG vs. 0.6 in CG, p = 0.019. Decreased infant height z-score: −0.2 in IG vs. −0.5 in CG, p = 0.028. NS difference in BMI z-score; prevalence of overweight or obesity; % energy intake from sugar in discretionary foods; % energy intake from discretionary foods. Decreased ECC prevalence: 19.7% in IG vs. 23.6% in CG, p < 0.0001. At 5 years: NS difference in ECC prevalence. |
| Schroth et al. 2015. Canada. | To determine the effectiveness of the Healthy Smile Happy Child community project on promoting early childhood oral health. To assess changes in carer knowledge, attitudes, and behaviours relating to early childhood oral health, and the burden of ECC and severe ECC. | Serial cross-sectional evaluation of a community program; 1999 start. | 4 First Nation communities in Manitoba, Canada: one remote, one rural, two urban. IG: n = 319 children evaluated. CG: n = 408 children evaluated pre-program. | IG: Community capacity building. Embed oral health promotion in community activity, child and family programs and services. Health promotion education: child comforting without bottle, water intake, bottle cessation and cup transition, avoid cariogenic drinks, no bottle propping, no sweeteners on pacifiers; with development of teaching tools and resources. CG: N/A. | After 5 years: Increased disagreement to ‘frequently giving my child fruit juice or drink is OK for their teeth’: 70.9% at follow-up vs. 48.3% pre-program, p < 0.0001. Decreased agreement to ‘frequently giving my child milk or formula is OK for their teeth’: 67.1% at follow-up vs. 74.3% pre-program, p = 0.015. NS change in disagreement to ‘frequently giving my child soda is OK for their teeth’: 97.2% at follow-up vs. 94.3% pre-program. Increased disagreement to ‘as my baby gets older, they should use a bottle whenever they want’: 72.1% at follow-up vs. 61.8% pre-program, p = 0.0022. Increased disagreement to ‘it is OK to put my baby to bed with a bottle’: 79% at follow-up vs. 70.3% pre-program, p = 0.0073. Increased agreement to ‘bottle feeding after my child is one year old is bad for their teeth’: 78.1% at follow-up vs. 62% pre-program, p < 0.01. Increased disagreement to ‘babies who do not have bottles will cry more’: 64% at follow-up vs. 54.3% pre-program, p = 0.014. NS difference in bottle feeding prevalence. Increased sippy cup use: 93% at follow-up vs. 77.8% pre-program, p = 0.0001. NS difference in ECC prevalence. Significant difference in ECC prevalence across 4 community sites, p = 0.0012: increased ECC in rural and remote communities, c.f. to one urban community. Trend towards decreased severe ECC prevalence: 38.6% at follow-up vs. 45% pre-program, p = 0.08. Significant difference in severe ECC prevalence across 4 community sites, p = 0.0052: increased ECC in rural and remote communities, c.f. to one urban community. |
| Sgan-Cohen et al. 2001. Israel. | To measure the effect of a community health education program on reported infants’ bottle-feeding practices and toothbrushing behaviour, with or without distribution of toothpaste and toothbrushes. | Quasi-experimental 2 × 2 comparison study; dates NR. | Mother and child health centres, providing services to 6–12 months infants. Stratified by religion profile: secular-moderately religious mixed or predominantly Orthodox. IG 1: health education & resource distribution, n = 268. IG 2: health education, n = 187. CG 1: usual care & resource distribution, n = 133. CG 2: usual care, n = 139. | IG: Education at each visit, between 0–2 years: decrease SSB frequency, cup transition, tooth cleaning, avoid added sugar, avoid bottle use as pacifier or sleeping with bottle, dental attendance, dental pamphlet. Resource distribution: toothpaste, toothbrush, at baseline, 2 months and 4 months visit. CG: Usual care, with or without resource distribution. | Use of bottle feeding decreased from age 6–12 months to 12–18 months; however, adding sugar to bottles increased. NS difference in use of bottles with added sugar during meals at 6 months, 10.2% in IG vs. 6.3% in CG, p = 0.06. However, this increased from 1.5% in IG vs. 1.3% in CG at baseline, p < 0.001. Less use of bottle with added sugar between meals at 6 months, 42.4% in IG vs. 47.3% in CG, p = 0.06. However, this increased from 20.6% in IG vs. 20.9% in CG at baseline, p < 0.001. NS difference in use of bottles during meals; bottles between meals; bottles during sleep; bottles with added sugar during sleep. |
| Strippel et al. 2010. Germany. | To examine the effectiveness of expanding and improving oral health education in a clinical setting. | Prospective controlled trial; July–Dec 2001. | Parents of ~6 week (IG 1) or ~24 month (IG 2) children, attending routine paediatric examination. IG 1: n = 1015. IG 2: n = 1025. CG: age-matched children in northern Germany. CG 1: n = 1181. CG 2: n = 989. | IG 1: Education at 6 weeks and 7 months: breastfeeding, bottle feeding, tooth eruption, oral hygiene, fluoride supplements, nursing bottle use. IG 2: Education at 24 months: caries prevention, oral hygiene, nursing bottle use, drinks in bottles, fluoride supplement. Education to cover 7–8 oral prevention topics, with 15 min education. CG: Conventional oral health education. | For IG 1 (aged 7 months): NS difference in bottle use in bed at night. Decreased bottle use at daytime: ‘never’, 33% in IG vs. 24% in CG; daily, 32% in IG vs. 41% in CG, p < 0.001. Decreased ‘sometimes or always’ adding sugar to pureed baby food: 24% in IG vs. 32% in CG, p < 0.001. Increased oral prevention topics addressed by clinicians: 3.3 ± 2.1 topics vs. 1.9 ± 1.7, p < 0.001. For IG 2 (aged 24 months): NS difference in bottle use at daytime and in bed; ongoing nursing bottle use; frequency in cariogenic food at daytime and in bed; frequency in cariogenic beverage use in bed; knowledge of cariogenic foods and juice. Decreased frequent cariogenic beverage use at daytime: 61% in IG vs. 66% in CG, p = 0.013. Increased oral prevention topics addressed by clinicians: 4.2 ± 2.2 topics vs. 2.4 ± 1.7, p < 0.001. |
| Ventura et al. 2021. USA. | To assess effect of policy, systems and environmental change strategies to promote responsive bottle feeding on RWG risk. | Cluster-RCT. May-August 2019 recruitment; 2020 follow-up interrupted by COVID-19 pandemic. | Mothers with new-born infants in USA WIC program. IG: 124 mother–infant dyads. CG: 122 mother–infant dyads. | IG: Policy, systems and environmental change of WIC program. Retooling of infant feeding assessment to be inclusive of responsive bottle feeding; development of assessment tools, counselling probes resources; responsive bottle-feeding online education and text message support; rebranding of infant feeding helpline. CG: Usual care, including timely and tailored breastfeeding support; breastfeeding support resources (helpline, online education, responsive text message support). | At 6 months: Decreased RWG: OR: 0.36 (0.16–0.81), p = 0.014. NS difference in exclusive bottle feeding: 65% in IG vs. 65% in CG. NS difference in mixed breast milk and formula feeding: 16% in IG vs. 13% in CG. NS difference in responsive feeding style; pressuring feeding style; encouragement of bottle emptying; percentage of daily feeding from a bottle. |
| Vichayanrat et al. 2012. Thailand. | To report effect of a multi-level oral health intervention pilot on carer’s oral health practices. | Pilot quasi-experimental trial; dates NR. | Carers of healthy 6–36 months children in 4 sub-districts across 2 provincial districts. IG: 62 carer-child dyads. CG: 52 carer-child dyads. | IG: Community mobilisation. Oral health home visits every 3 months. Improved oral health education, including tooth brushing, bottle feeding, controlling cariogenic intake, and services delivered during child vaccination. CG: Routine health services and toothbrushes from local health centres. | NS difference in prevalence of caries; children falling asleep with bottle; sweetened milk, juice or soda in bottles; consumption of all snacks, in IG and CG. Increased carer knowledge on not putting juice in bottles: 66.1% in IG vs. 34.6% in CG, p = 0.001. |
| Weber-Gasparo, Reeve, et al. 2013. Weber-Gasparo, Warren, et al. 2013. USA. | To compare whether a videotaped message, informed by the self-determination theory, leads to greater changes in oral health knowledge and behavioural intentions to prevent childhood caries. | RCT; dates NR. | Mothers with child aged 12–49 months, in USA WIC program. IG: n = 283; 155 completed 1 month follow-up QNR; 181 completed the 6 month follow-up visit. CG: n = 132; 78 completed 1 month follow-up QNR; 86 completed the 6 month follow-up visit. | IG: Education: 15 min video on oral health, informed by self-determination theory re: caries aetiology, oral hygiene, diet and caries risk, early caries identification. CG: Neutral-language paper brochure, with same dental content. | At 6 months follow-up: NS difference in ECC prevalence; sippy cup use at night with non-water drinks; sippy cup use at daytime with sugary drinks; sugary drinks consumed between meals; daily intake of >6 oz 100% fruit juice; daily intake of >2 cariogenic snacks; intake of 100% juice; intake of drinks with added sugar; intake of all sugary drinks (added sugar drinks and 100% fruit juice), in IG and CG. Increased maternal oral health knowledge (including bottle use in bed, cariogenic foods and drinks) from baseline: 5.17 ± 3.90 in IG vs. 3.11 ± 4.25 in CG, p < 0.001. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, H.; Chen, R.; Milosevic, M.; Rossiter, C.; Arora, A.; Denney-Wilson, E. Interventions Targeting Bottle and Formula Feeding in the Prevention and Treatment of Early Childhood Caries, Overweight and Obesity: An Integrative Review. Int. J. Environ. Res. Public Health 2021, 18, 12304. https://doi.org/10.3390/ijerph182312304
Cheng H, Chen R, Milosevic M, Rossiter C, Arora A, Denney-Wilson E. Interventions Targeting Bottle and Formula Feeding in the Prevention and Treatment of Early Childhood Caries, Overweight and Obesity: An Integrative Review. International Journal of Environmental Research and Public Health. 2021; 18(23):12304. https://doi.org/10.3390/ijerph182312304
Chicago/Turabian StyleCheng, Heilok, Rebecca Chen, Maxim Milosevic, Chris Rossiter, Amit Arora, and Elizabeth Denney-Wilson. 2021. "Interventions Targeting Bottle and Formula Feeding in the Prevention and Treatment of Early Childhood Caries, Overweight and Obesity: An Integrative Review" International Journal of Environmental Research and Public Health 18, no. 23: 12304. https://doi.org/10.3390/ijerph182312304








