Amikacin: Uses, Resistance, and Prospects for Inhibition
Abstract
:1. A Brief History of Aminoglycoside Antibiotics
2. Mechanism of Action and Side Effects
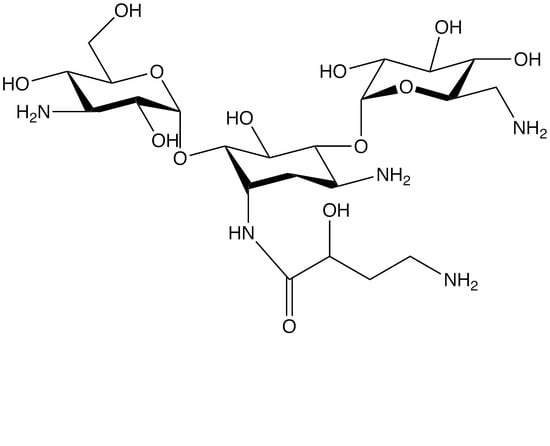
3. Amikacin
3.1. AAC(6′)-I Enzymes of Gram-Positive Bacteria
3.2. AAC(6′)-I Enzymes of Gram-Negative Bacteria
3.3. Inhibition of Amikacin-Resistance Mediated by AAC(6′)-Ib
4. Final Remarks
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Vakulenko, S.B.; Mobashery, S. Versatility of aminoglycosides and prospects for their future. Clin. Microbiol. Rev. 2003, 16, 430–450. [Google Scholar] [CrossRef] [PubMed]
- Kotra, L.P.; Haddad, J.; Mobashery, S. Aminoglycosides: Perspectives on mechanisms of action and resistance and strategies to counter resistance. Antimicrob. Agents Chemother. 2000, 44, 3249–3256. [Google Scholar] [CrossRef] [PubMed]
- Houghton, J.L.; Green, K.D.; Chen, W.; Garneau-Tsodikova, S. The future of aminoglycosides: The end or renaissance? ChemBioChem 2010, 11, 880–902. [Google Scholar] [CrossRef] [PubMed]
- Serio, A.; Magalaes, M.; Blanchard, J.S.; Connolly, L. Aminoglycosides: Mechanisms of action and resistance. In Antimicrobial Drug Resistance; Mayers, D., Sobel, J., Ouellette, M., Kaye, K., Marchaim, D., Eds.; Springer: Cham, Switzerland, 2017. [Google Scholar]
- Pullens, B.; van Benthem, P.P. Intratympanic gentamicin for Meniere’s disease or syndrome. Cochrane Database Syst. Rev. 2011. [Google Scholar] [CrossRef]
- Richardson, R.; Smart, M.; Tracey-White, D.; Webster, A.R.; Moosajee, M. Mechanism and evidence of nonsense suppression therapy for genetic eye disorders. Exp. Eye Res. 2017, 155, 24–37. [Google Scholar] [CrossRef] [PubMed]
- Keeling, K.M.; Wang, D.; Conard, S.E.; Bedwell, D.M. Suppression of premature termination codons as a therapeutic approach. Crit. Rev. Biochem. Mol. Biol. 2012, 47, 444–463. [Google Scholar] [CrossRef] [PubMed]
- James, P.D.; Raut, S.; Rivard, G.E.; Poon, M.C.; Warner, M.; McKenna, S.; Leggo, J.; Lillicrap, D. Aminoglycoside suppression of nonsense mutations in severe hemophilia. Blood 2005, 106, 3043–3048. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, R.; Waldsich, C.; Wank, H. Modulation of RNA function by aminoglycoside antibiotics. EMBO J. 2000, 19, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Veyssier, P.; Bryskier, A. Aminocyclitol aminoglycosides. In Antimicrobial Agents; Bryskier, A., Ed.; ASM Press: Washington, DC, USA, 2005; pp. 453–469. [Google Scholar]
- Davies, J.E. Aminoglycosides: Ancient and modern. J. Antibiot. 2006, 59, 529–532. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.; Metzger, H.J.; Schatz, A.; Waksman, S.A. Control of gram-negative bacteria in experimental animals by streptomycin. Science 1944, 100, 103–105. [Google Scholar] [CrossRef] [PubMed]
- Waksman, S.A.; Lechevalier, H.A. Neomycin, a new antibiotic active against streptomycin-resistant bacteria, including tuberculosis organisms. Science 1949, 109, 305–307. [Google Scholar] [CrossRef] [PubMed]
- Umezawa, H.; Tazaki, T.; Okami, Y.; Fukuyama, S. Studies on streptothricin group substances. On streptothricin A and streptothricin B. J. Antibiot. 1949, 3, 232–235. [Google Scholar] [CrossRef]
- Umezawa, H. Kanamycin: Its discovery. Ann. N. Y. Acad. Sci. 1958, 76, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, M.J.; Luedemann, G.M.; Oden, E.M.; Wagman, G.H. Gentamicin, a new broad-spectrum antibiotic complex. Antimicrob. Agents Chemother. 1963, 161, 1–7. [Google Scholar] [PubMed]
- Weinstein, M.J.; Luedemann, G.M.; Oden, E.M.; Wagman, G.H.; Rosselet, J.P.; Marquez, J.A.; Coniglio, C.T.; Charney, W.; Herzog, H.L.; Black, J. Gentamicin, a new antibiotic complex from Micromonospora. J. Med. Chem. 1963, 6, 463–464. [Google Scholar] [CrossRef] [PubMed]
- Higgins, C.E.; Kastner, R.E. Nebramycin, a new broad-spectrum antibiotic complex. II. Description of Streptomyces tenebrarius. Antimicrob. Agents Chemother. 1967, 7, 324–331. [Google Scholar] [PubMed]
- Chandrika, N.T.; Garneau-Tsodikova, S. A review of patents (2011–2015) towards combating resistance to and toxicity of aminoglycosides. MedChemComm 2016, 7, 50–68. [Google Scholar] [CrossRef] [PubMed]
- Davidson, R.N.; den Boer, M.; Ritmeijer, K. Paromomycin. Trans. R. Soc. Trop. Med. Hyg. 2009, 103, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Fosso, M.; AlFindee, M.N.; Zhang, Q.; Nziko Vde, P.; Kawasaki, Y.; Shrestha, S.K.; Bearss, J.; Gregory, R.; Takemoto, J.Y.; Chang, C.W. Structure-activity relationships for antibacterial to antifungal conversion of kanamycin to amphiphilic analogues. J. Org. Chem. 2015, 80, 4398–4411. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, S.K.; Fosso, M.Y.; Green, K.D.; Garneau-Tsodikova, S. Amphiphilic tobramycin analogues as antibacterial and antifungal agents. Antimicrob. Agents Chemother. 2015, 59, 4861–4869. [Google Scholar] [CrossRef] [PubMed]
- Tolmasky, M.E. Aminoglycoside-modifying enzymes: Characteristics, localization, and dissemination. In Enzyme-Mediated Resistance to Antibiotics: Mechanisms, Dissemination, and Prospects for Inhibition; Bonomo, R.A., Tolmasky, M.E., Eds.; ASM Press: Washington, DC, USA, 2007; pp. 35–52. [Google Scholar]
- Yao, J.; Moellering, R. Antibacterial agents. In Manual of Clinical Microbiology; Murray, P., Baron, E., Jorgensen, J., Landry, M., Pfaller, M., Eds.; American Society for Microbiology Press: Washington, DC, USA, 2007; Volume 1, pp. 1077–1113. [Google Scholar]
- Park, S.R.; Park, J.W.; Ban, Y.H.; Sohng, J.K.; Yoon, Y.J. 2-Deoxystreptamine-containing aminoglycoside antibiotics: Recent advances in the characterization and manipulation of their biosynthetic pathways. Nat. Prod. Rep. 2013, 30, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, M.S.; Tolmasky, M.E. Aminoglycoside modifying enzymes. Drug Resist. Updat. 2010, 13, 151–171. [Google Scholar] [CrossRef] [PubMed]
- Shaw, K.J.; Rather, P.N.; Hare, R.S.; Miller, G.H. Molecular genetics of aminoglycoside resistance genes and familial relationships of the aminoglycoside-modifying enzymes. Microbiol. Rev. 1993, 57, 138–163. [Google Scholar] [PubMed]
- Umezawa, H.; Kondo, S. Mechanisms of resistance to amino-glycoside antibiotics. In Aminoglycoside Antibiotics; Umezawa, H., Hooper, H., Eds.; Handbook of Experimental Pharmacology; Springer: Berlin/Heidelberg, Germany; New York, NY, USA, 1982; Volume 62, pp. 267–292. [Google Scholar]
- Garneau-Tsodikova, S.; Labby, K.J. Mechanisms of resistance to aminoglycoside antibiotics: Overview and perspectives. MedChemComm 2016, 7, 11–27. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Nishino, K.; Roberts, M.C.; Tolmasky, M.; Aminov, R.I.; Zhang, L. Mechanisms of antibiotic resistance. Front. Microbiol. 2015, 6, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Umezawa, H.; Okanishi, M.; Utahara, R.; Maeda, K.; Kondo, S. Isolation and structure of kanamycin inactivated by a cell free system of kanamycin-resistant E. coli. J. Antibiot. 1967, 20, 136–141. [Google Scholar] [PubMed]
- Favrot, L.; Blanchard, J.S.; Vergnolle, O. Bacterial GCN5-related N-acetyltransferases: From resistance to regulation. Biochemistry 2016, 55, 989–1002. [Google Scholar] [CrossRef] [PubMed]
- Salah Ud-Din, A.I.; Tikhomirova, A.; Roujeinikova, A. Structure and functional diversity of GCN5-related N-acetyltransferases (GNAT). Int. J. Mol. Sci. 2016, 17, 1018. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, M.S.; Nikolaidis, N.; Tolmasky, M.E. Rise and dissemination of aminoglycoside resistance: The aac(6′)-Ib paradigm. Front. Microbiol. 2013, 4, 121. [Google Scholar] [CrossRef] [PubMed]
- Kondo, S.; Hotta, K. Semisynthetic aminoglycoside antibiotics: Development and enzymatic modifications. J. Infect. Chemother. 1999, 5, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Oizumi, K.; Ariji, F.; Kumano, N.; Oka, S.; Konno, K. Action mechanism of 3′,4′-dideoxykanamycin B (DKB) on Klebsiella pneumoniae. Sci. Rep. Res. Inst. Tohoku Univ. Med. 1974, 21, 47–53. [Google Scholar] [PubMed]
- Umezawa, H.; Umezawa, S.; Tsuchiya, T.; Okazaki, Y. 3′,4′-dideoxy-kanamycin B active against kanamycin-resistant Escherichia coli and Pseudomonas aeruginosa. J. Antibiot. 1971, 24, 485–487. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, H.; Naito, T.; Nakagawa, S.; Fujisawa, K.I. BB-K8, a new semisynthetic aminoglycoside antibiotic. J. Antibiot. 1972, 25, 695–708. [Google Scholar] [CrossRef] [PubMed]
- Tolmasky, M.E.; Chamorro, R.M.; Crosa, J.H.; Marini, P.M. Transposon-mediated amikacin resistance in Klebsiella pneumoniae. Antimicrob. Agents Chemother. 1988, 32, 1416–1420. [Google Scholar] [CrossRef] [PubMed]
- Tolmasky, M.E.; Crosa, J.H. Tn1331, a novel multiresistance transposon encoding resistance to amikacin and ampicillin in Klebsiella pneumoniae. Antimicrob. Agents Chemother. 1987, 31, 1955–1960. [Google Scholar] [CrossRef] [PubMed]
- Tolmasky, M.E.; Roberts, M.; Woloj, M.; Crosa, J.H. Molecular cloning of amikacin resistance determinants from a Klebsiella pneumoniae plasmid. Antimicrob. Agents Chemother. 1986, 30, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Woloj, M.; Tolmasky, M.E.; Roberts, M.C.; Crosa, J.H. Plasmid-encoded amikacin resistance in multiresistant strains of Klebsiella pneumoniae isolated from neonates with meningitis. Antimicrob. Agents Chemother. 1986, 29, 315–319. [Google Scholar] [CrossRef] [PubMed]
- Tolmasky, M.E. Bacterial resistance to aminoglycosides and β-lactams: The Tn1331 transposon paradigm. Front. Biosci. 2000, 5, D20–D29. [Google Scholar] [CrossRef] [PubMed]
- Mangia, A.; Giobbio, V.; Ornato, G. Novel Process for the Synthesis of Amikacin. U.S. Patent 4,902,790, 20 February 1990. [Google Scholar]
- Hanessian, S.; Patil, G. Aminoglycoside antibiotics—A method for selective N-acylation based on the temporary protection of amino alcohol functions as copper chelates. Tetrahedron Lett. 1978, 19, 1035–1038. [Google Scholar] [CrossRef]
- Kahlmeter, G. Netilmicin: Clinical pharmacokinetics and aspects on dosage schedules. An overview. Scand. J. Infect. Dis. 1980, 12 (Suppl. 23), 74–81. [Google Scholar]
- Nagabhushan, T.L.; Cooper, A.B.; Tsai, H.; Daniels, P.J.; Miller, G.H. The syntheses and biological properties of 1-N-(S-4-amino-2-hydroxybutyryl)-gentamicin B and 1-N-(S-3-amino-2-hydroxypropionyl)-gentamicin B. J. Antibiot. 1978, 31, 681–687. [Google Scholar] [CrossRef] [PubMed]
- Kondo, S. Development of arbekacin and synthesis of new derivatives stable to enzymatic modifications by methicillin-resistant Staphylococcus aureus. Jpn. J. Antibiot. 1994, 47, 561–574. [Google Scholar] [PubMed]
- Labby, K.J.; Garneau-Tsodikova, S. Strategies to overcome the action of aminoglycoside-modifying enzymes for treating resistant bacterial infections. Future Med. Chem. 2013, 5, 1285–1309. [Google Scholar] [CrossRef] [PubMed]
- Park, J.W.; Ban, Y.H.; Nam, S.J.; Cha, S.S.; Yoon, Y.J. Biosynthetic pathways of aminoglycosides and their engineering. Curr. Opin. Biotechnol. 2017, 48, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Chandrika, N.T.; Green, K.; Houghton, J.L.; Garneau-Tsodikova, S. Synthesis and biological activity of mono- and di-N-acylated aminoglycosides. ACS Med. Chem. Lett. 2015, 6, 1134–1139. [Google Scholar] [CrossRef] [PubMed]
- Jackson, J.; Chen, C.; Buising, K. Aminoglycosides: How should we use them in the 21st century? Curr. Opin. Infect. Dis. 2013, 26, 516–525. [Google Scholar] [CrossRef] [PubMed]
- Dozzo, P.; Moser, H.E. New aminoglycoside antibiotics. Expert Opin. Ther. Pat. 2010, 20, 1321–1341. [Google Scholar] [CrossRef] [PubMed]
- Vong, K.; Auclair, K. Understanding and overcoming aminoglycoside resistance caused by N-6′-acetyltransferase. MedChemComm 2012, 3, 397–407. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Ye, X.S. Development of aminoglycoside antibiotics effective against resistant bacterial strains. Curr. Top. Med. Chem. 2010, 10, 1898–1926. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, L.; Das, I.; Desire, J.; Sautrey, G.; Barros, R.S.V.; El Khoury, M.; Mingeot-Leclercq, M.P.; Decout, J.L. New broad-spectrum antibacterial amphiphilic aminoglycosides active against resistant bacteria: From neamine derivatives to smaller neosamine analogues. J. Med. Chem. 2016, 59, 9350–9369. [Google Scholar] [CrossRef] [PubMed]
- Fair, R.J.; McCoy, L.S.; Hensler, M.E.; Aguilar, B.; Nizet, V.; Tor, Y. Singly modified amikacin and tobramycin derivatives show increased rRNA A-site binding and higher potency against resistant bacteria. ChemMedChem 2014, 9, 2164–2171. [Google Scholar] [CrossRef] [PubMed]
- You, X.F.; Li, C.R.; Yang, X.Y.; Yuan, M.; Zhang, W.X.; Lou, R.H.; Wang, Y.M.; Li, G.Q.; Chen, H.Z.; Song, D.Q.; et al. In Vivo antibacterial activity of vertilmicin, a new aminoglycoside antibiotic. Antimicrob. Agents Chemother. 2009, 53, 4525–4528. [Google Scholar] [CrossRef] [PubMed]
- Aggen, J.B.; Armstrong, E.S.; Goldblum, A.A.; Dozzo, P.; Linsell, M.S.; Gliedt, M.J.; Hildebrandt, D.J.; Feeney, L.A.; Kubo, A.; Matias, R.D.; et al. Synthesis and spectrum of the neoglycoside ACHN-490. Antimicrob. Agents Chemother. 2010, 54, 4636–4642. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, E.S.; Miller, G.H. Combating evolution with intelligent design: The neoglycoside ACHN-490. Curr. Opin. Microbiol. 2010, 13, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Avial, I.; Pena, I.; Picazo, J.J.; Rodriguez-Avial, C.; Culebras, E. In Vitro activity of the next-generation aminoglycoside plazomicin alone and in combination with colistin, meropenem, fosfomycin or tigecycline against carbapenemase-producing Enterobacteriaceae strains. Int. J. Antimicrob. Agents 2015, 46, 616–621. [Google Scholar] [CrossRef] [PubMed]
- Wright, H.; Bonomo, R.A.; Paterson, D.L. New agents for the treatment of infections with Gram-negative bacteria: Restoring the miracle or false dawn? Clin. Microbiol. Infect. 2017, 23, 704–712. [Google Scholar] [CrossRef] [PubMed]
- Arrington, D. Achaogen submits Plazomicin New Drug Application (NDA) to the U.S. FDA for Treatment of Complicated Urinary Tract Infections and Bloodstream Infections. Available online: http://investors.achaogen.com/releasedetail.cfm?releaseid=1045559 (accessed on 2 November 2017).
- Galani, I.; Souli, M.; Daikos, G.L.; Chrysouli, Z.; Poulakou, G.; Psichogiou, M.; Panagea, T.; Argyropoulou, A.; Stefanou, I.; Plakias, G.; et al. Activity of plazomicin (ACHN-490) against MDR clinical isolates of Klebsiella pneumoniae, Escherichia coli, and Enterobacter spp. from Athens, Greece. J. Chemother. 2012, 24, 191–194. [Google Scholar] [CrossRef] [PubMed]
- Denervaud-Tendon, V.; Poirel, L.; Connolly, L.E.; Krause, K.M.; Nordmann, P. Plazomicin activity against polymyxin-resistant Enterobacteriaceae, including MCR-1-producing isolates. J. Antimicrob. Chemother. 2017, 72, 2787–2791. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Kashikar, A.; Bush, K. In Vitro activity of plazomicin against β-lactamase-producing carbapenem-resistant Enterobacteriaceae (CRE). J. Antimicrob. Chemother. 2017, 72, 2792–2795. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Salguero, C.; Rodriguez-Avial, I.; Picazo, J.J.; Culebras, E. Can plazomicin alone or in combination be a therapeutic option against carbapenem-resistant Acinetobacter baumannii? Antimicrob. Agents Chemother. 2015, 59, 5959–5966. [Google Scholar] [CrossRef] [PubMed]
- Walkty, A.; Adam, H.; Baxter, M.; Denisuik, A.; Lagace-Wiens, P.; Karlowsky, J.A.; Hoban, D.J.; Zhanel, G.G. In Vitro activity of plazomicin against 5015 gram-negative and gram-positive clinical isolates obtained from patients in canadian hospitals as part of the CANWARD study, 2011–2012. Antimicrob. Agents Chemother. 2014, 58, 2554–2563. [Google Scholar] [CrossRef] [PubMed]
- Lopez Diaz, M.C.; Rios, E.; Rodriguez-Avial, I.; Simaluiza, R.J.; Picazo, J.J.; Culebras, E. In-Vitro activity of several antimicrobial agents against methicillin-resistant Staphylococcus aureus (MRSA) isolates expressing aminoglycoside-modifying enzymes: Potency of plazomicin alone and in combination with other agents. Int. J. Antimicrob. Agents 2017, 50, 191–196. [Google Scholar] [CrossRef] [PubMed]
- The Royal Pharmaceutical Society of Great Britain, British National Formulary; BMJ Group, RCPCH Publications Ltd.: London, UK; The Royal Pharmaceutical Society of Great Britain: London, UK, 2017.
- Vanhoof, R.; Sonck, P.; Hannecart-Pokorni, E. The role of lipopolysaccharide anionic binding sites in aminoglycoside uptake in Stenotrophomonas (Xanthomonas) maltophilia. J. Antimicrob. Chemother. 1995, 35, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Muir, M.E.; van Heeswyck, R.S.; Wallace, B.J. Effect of growth rate on streptomycin accumulation by Escherichia coli and Bacillus megaterium. J. Gen. Microbiol. 1984, 130, 2015–2022. [Google Scholar] [CrossRef] [PubMed]
- Nichols, W.W.; Young, S.N. Respiration-dependent uptake of dihydrostreptomycin by Escherichia coli. Its irreversible nature and lack of evidence for a uniport process. Biochem. J. 1985, 228, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Bryan, L.; van der Elzen, H. Effects of membrane-energy mutations and cations on streptomycin and gentamicin accumulation by bacteria: A model for entry of streptomycin and gentamicin in susceptible and resistant bacteria. Antimicrob. Agents Chemother. 1977, 12, 163–177. [Google Scholar] [CrossRef] [PubMed]
- Hurwitz, C.; Braun, C.B.; Rosano, C.L. Role of ribosome recycling in uptake of dihydrostreptomycin by sensitive and resistant Escherichia coli. Biochim. Biophys. Acta 1981, 652, 168–176. [Google Scholar] [CrossRef]
- Davis, B.D. Non-specific membrane permeability and aminoglycoside action. J. Antimicrob. Chemother. 1989, 24, 77–78. [Google Scholar] [CrossRef] [PubMed]
- Nichols, W.W. The enigma of streptomycin transport. J. Antimicrob. Chemother. 1989, 23, 673–676. [Google Scholar] [CrossRef] [PubMed]
- Nichols, W.W.; Dorrington, S.M.; Slack, M.P.; Walmsley, H.L. Inhibition of tobramycin diffusion by binding to alginate. Antimicrob. Agents Chemother. 1988, 32, 518–523. [Google Scholar] [CrossRef] [PubMed]
- Taber, H.W.; Mueller, J.P.; Miller, P.F.; Arrow, A.S. Bacterial uptake of aminoglycoside antibiotics. Microbiol. Rev. 1987, 51, 439–457. [Google Scholar] [PubMed]
- Bakker, E.P. Aminoglycoside and aminocyclitol antibiotics: Hygromycin B is an atypical bactericidal compound that exerts effects on cells of Escherichia coli characteristics for bacteriostatic aminocyclitols. J. Gen. Microbiol. 1992, 138, 563–569. [Google Scholar] [CrossRef] [PubMed]
- Busse, H.J.; Wostmann, C.; Bakker, E.P. The bactericidal action of streptomycin: Membrane permeabilization caused by the insertion of mistranslated proteins into the cytoplasmic membrane of Escherichia coli and subsequent caging of the antibiotic inside the cells due to degradation of these proteins. J. Gen. Microbiol. 1992, 138, 551–561. [Google Scholar] [PubMed]
- Davis, B.D. Mechanism of bactericidal action of aminoglycosides. Microbiol. Rev. 1987, 51, 341–350. [Google Scholar] [PubMed]
- Magnet, S.; Blanchard, J.S. Molecular insights into aminoglycoside action and resistance. Chem. Rev. 2005, 105, 477–498. [Google Scholar] [CrossRef] [PubMed]
- Degtyareva, N.N.; Gong, C.; Story, S.; Levinson, N.S.; Oyelere, A.K.; Green, K.D.; Garneau-Tsodikova, S.; Arya, D.P. Antimicrobial activity, AME resistance, and A-site binding studies of anthraquinone-neomycin conjugates. ACS Infect. Dis. 2017, 3, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Jana, S.; Deb, J.K. Molecular targets for design of novel inhibitors to circumvent aminoglycoside resistance. Curr. Drug Targets 2005, 6, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Jana, S.; Deb, J.K. Molecular understanding of aminoglycoside action and resistance. Appl. Microbiol. Biotechnol. 2006, 70, 140–150. [Google Scholar] [CrossRef] [PubMed]
- McCoy, L.S.; Xie, Y.; Tor, Y. Antibiotics that target protein synthesis. Wiley Interdiscip. Rev. RNA 2011, 2, 209–232. [Google Scholar] [CrossRef] [PubMed]
- Foster, C.; Champney, W.S. Characterization of a 30S ribosomal subunit assembly intermediate found in Escherichia coli cells growing with neomycin or paromomycin. Arch. Microbiol. 2008, 189, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Mehta, R.; Champney, W.S. Neomycin and paromomycin inhibit 30S ribosomal subunit assembly in Staphylococcus aureus. Curr. Microbiol. 2003, 47, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Belousoff, M.J.; Graham, B.; Spiccia, L.; Tor, Y. Cleavage of RNA oligonucleotides by aminoglycosides. Org. Biomol. Chem. 2009, 7, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Vourekas, A.; Stamatopoulou, V.; Toumpeki, C.; Tsitlaidou, M.; Drainas, D. Insights into functional modulation of catalytic RNA activity. IUBMB Life 2008, 60, 669–683. [Google Scholar] [CrossRef] [PubMed]
- Bao, Y.; Herrin, D.L. Mg2+ mimicry in the promotion of group I ribozyme activities by aminoglycoside antibiotics. Biochem. Biophys. Res. Commun. 2006, 344, 1246–1252. [Google Scholar] [CrossRef] [PubMed]
- Mikkelsen, N.E.; Brannvall, M.; Virtanen, A.; Kirsebom, L.A. Inhibition of RNase P RNA cleavage by aminoglycosides. Proc. Natl. Acad. Sci. USA 1999, 96, 6155–6160. [Google Scholar] [CrossRef] [PubMed]
- Kawamoto, S.A.; Sudhahar, C.G.; Hatfield, C.L.; Sun, J.; Behrman, E.J.; Gopalan, V. Studies on the mechanism of inhibition of bacterial ribonuclease P by aminoglycoside derivatives. Nucleic Acids Res. 2008, 36, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Goh, E.B.; Yim, G.; Tsui, W.; McClure, J.; Surette, M.G.; Davies, J. Transcriptional modulation of bacterial gene expression by subinhibitory concentrations of antibiotics. Proc. Natl. Acad. Sci. USA 2002, 99, 17025–17030. [Google Scholar] [CrossRef] [PubMed]
- Possoz, C.; Newmark, J.; Sorto, N.; Sherratt, D.J.; Tolmasky, M.E. Sublethal concentrations of the aminoglycoside amikacin interfere with cell division without affecting chromosome dynamics. Antimicrob. Agents Chemother. 2007, 51, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Radigan, E.A.; Gilchrist, N.A.; Miller, M.A. Management of aminoglycosides in the intensive care unit. J. Intensive Care Med. 2010, 25, 327–342. [Google Scholar] [CrossRef] [PubMed]
- Paradelis, A.G.; Triantaphyllidis, C.; Giala, M.M. Neuromuscular blocking activity of aminoglycoside antibiotics. Methods Find. Exp. Clin. Pharmacol. 1980, 2, 45–51. [Google Scholar] [PubMed]
- Singh, Y.N.; Marshall, I.G.; Harvey, A.L. Some effects of the aminoglycoside antibiotic amikacin on neuromuscular and autonomic transmission. Br. J. Anaesth. 1978, 50, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Wargo, K.A.; Edwards, J.D. Aminoglycoside-induced nephrotoxicity. J. Pharm. Pract. 2014, 27, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Leis, J.A.; Rutka, J.A.; Gold, W.L. Aminoglycoside-induced ototoxicity. CMAJ 2015, 187, E52. [Google Scholar] [CrossRef] [PubMed]
- Prayle, A.; Watson, A.; Fortnum, H.; Smyth, A. Side effects of aminoglycosides on the kidney, ear and balance in cystic fibrosis. Thorax 2010, 65, 654–658. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, T.; Teranishi, M.; Hibi, T.; Kobayashi, M.; Umemura, M. Vestibular and cochlear toxicity of aminoglycosides—A review. Acta Otolaryngol. 2000, 120, 904–911. [Google Scholar] [PubMed]
- Lanvers-Kaminsky, C.; Zehnhoff-Dinnesen, A.A.; Parfitt, R.; Ciarimboli, G. Drug-induced ototoxicity: Mechanisms, pharmacogenetics, and protective strategies. Clin. Pharmacol. Ther. 2017, 101, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Guthrie, O.W. Aminoglycoside induced ototoxicity. Toxicology 2008, 249, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Sha, S.H.; Qiu, J.H.; Schacht, J. Aspirin to prevent gentamicin-induced hearing loss. N. Engl. J. Med. 2006, 354, 1856–1857. [Google Scholar] [CrossRef] [PubMed]
- Feldman, L.; Efrati, S.; Eviatar, E.; Abramsohn, R.; Yarovoy, I.; Gersch, E.; Averbukh, Z.; Weissgarten, J. Gentamicin-induced ototoxicity in hemodialysis patients is ameliorated by N-acetylcysteine. Kidney Int. 2007, 72, 359–363. [Google Scholar] [CrossRef] [PubMed]
- Kirkwood, N.K.; O’Reilly, M.; Derudas, M.; Kenyon, E.J.; Huckvale, R.; van Netten, S.M.; Ward, S.E.; Richardson, G.P.; Kros, C.J. d-Tubocurarine and berbamine: Alkaloids that are permeant blockers of the hair cell’s mechano-electrical transducer channel and protect from aminoglycoside toxicity. Front. Cell. Neurosci. 2017, 11, 262. [Google Scholar] [CrossRef] [PubMed]
- Mingeot-Leclercq, M.P.; Tulkens, P.M. Aminoglycosides: Nephrotoxicity. Antimicrob. Agents Chemother. 1999, 43, 1003–1012. [Google Scholar] [PubMed]
- McWilliam, S.J.; Antoine, D.J.; Smyth, R.L.; Pirmohamed, M. Aminoglycoside-induced nephrotoxicity in children. Pediatr. Nephrol. 2017, 32, 2015–2025. [Google Scholar] [CrossRef] [PubMed]
- Vicente-Vicente, L.; Casanova, A.G.; Hernandez-Sanchez, M.T.; Pescador, M.; Lopez-Hernandez, F.J.; Morales, A.I. A systematic meta-analysis on the efficacy of pre-clinically tested nephroprotectants at preventing aminoglycoside nephrotoxicity. Toxicology 2017, 377, 14–24. [Google Scholar] [CrossRef] [PubMed]
- Gerding, D.N.; Larson, T.A.; Hughes, R.A.; Weiler, M.; Shanholtzer, C.; Peterson, L.R. Aminoglycoside resistance and aminoglycoside usage: Ten years of experience in one hospital. Antimicrob. Agents Chemother. 1991, 35, 1284–1290. [Google Scholar] [CrossRef] [PubMed]
- Gad, G.F.; Mohamed, H.A.; Ashour, H.M. Aminoglycoside resistance rates, phenotypes, and mechanisms of Gram-negative bacteria from infected patients in upper Egypt. PLoS ONE 2011, 6, e17224. [Google Scholar] [CrossRef] [PubMed]
- Marsot, A.; Guilhaumou, R.; Riff, C.; Blin, O. Amikacin in critically ill patients: A review of population pharmacokinetic studies. Clin. Pharmacokinet. 2017, 56, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Pacifici, G.; Marchini, G. Clinical pharmacokinetics of amikacin in neonates. Int. J. Pediatr. 2017, 5, 4407–4428. [Google Scholar]
- Yu, V.L.; Rhame, F.S.; Pesanti, E.L.; Axline, S.G. Amikacin therapy. Use against infections caused by gentamicin- and tobramycin-resistant organisms. JAMA 1977, 238, 943–947. [Google Scholar] [CrossRef] [PubMed]
- Sklaver, A.R.; Greenman, R.L.; Hoffman, T.A. Amikacin therapy of gram-negative bacteremia and meningitis. Treatment in diseases due to multiple resistant bacilli. Arch. Intern. Med. 1978, 138, 713–716. [Google Scholar] [CrossRef] [PubMed]
- Ristuccia, A.M.; Cunha, B.A. An overview of amikacin. Ther. Drug Monit. 1985, 7, 12–25. [Google Scholar] [CrossRef] [PubMed]
- Tamma, P.D.; Cosgrove, S.E.; Maragakis, L.L. Combination therapy for treatment of infections with gram-negative bacteria. Clin. Microbiol. Rev. 2012, 25, 450–470. [Google Scholar] [CrossRef] [PubMed]
- Ambrosioni, J.; Lew, D.; Garbino, J. Nocardiosis: Updated clinical review and experience at a tertiary center. Infection 2010, 38, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.M. Mycobacterial endocarditis: A comprehensive review. Rev. Bras. Cir. Cardiovasc. 2015, 30, 93–103. [Google Scholar] [CrossRef] [PubMed]
- Caminero, J.A.; Sotgiu, G.; Zumla, A.; Migliori, G.B. Best drug treatment for multidrug-resistant and extensively drug-resistant tuberculosis. Lancet Infect. Dis. 2010, 10, 621–629. [Google Scholar] [CrossRef]
- White, B.P.; Lomaestro, B.; Pai, M.P. Optimizing the initial amikacin dosage in adults. Antimicrob. Agents Chemother. 2015, 59, 7094–7096. [Google Scholar] [CrossRef] [PubMed]
- MacDougall, C.; Chambers, H. Aminogylcosides. In The Pharmacological Basis of Therapeutics; Brunton, L., Chamber, B., Knollman, B., Eds.; Mc Graw Hill: New York, NY, USA, 2011; pp. 1507–1517. [Google Scholar]
- Sherwin, C.M.; Svahn, S.; Van der Linden, A.; Broadbent, R.S.; Medlicott, N.J.; Reith, D.M. Individualised dosing of amikacin in neonates: A pharmacokinetic/pharmacodynamic analysis. Eur. J. Clin. Pharmacol. 2009, 65, 705–713. [Google Scholar] [CrossRef] [PubMed]
- Siddiqi, A.; Khan, D.A.; Khan, F.A.; Razzaq, A. Therapeutic drug monitoring of amikacin in preterm and term infants. Singap. Med. J. 2009, 50, 486–489. [Google Scholar]
- Tayman, C.; El-Attug, M.N.; Adams, E.; Van Schepdael, A.; Debeer, A.; Allegaert, K.; Smits, A. Quantification of amikacin in bronchial epithelial lining fluid in neonates. Antimicrob. Agents Chemother. 2011, 55, 3990–3993. [Google Scholar] [CrossRef] [PubMed]
- Kondo, J.; Francois, B.; Russell, R.J.; Murray, J.B.; Westhof, E. Crystal structure of the bacterial ribosomal decoding site complexed with amikacin containing the γ-amino-α-hydroxybutyryl (haba) group. Biochimie 2006, 88, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Russell, R.J.; Murray, J.B.; Lentzen, G.; Haddad, J.; Mobashery, S. The complex of a designer antibiotic with a model aminoacyl site of the 30S ribosomal subunit revealed by X-ray crystallography. J. Am. Chem. Soc. 2003, 125, 3410–3411. [Google Scholar] [CrossRef] [PubMed]
- Quon, B.S.; Goss, C.H.; Ramsey, B.W. Inhaled antibiotics for lower airway infections. Ann. Am. Thorac. Soc. 2014, 11, 425–434. [Google Scholar] [CrossRef] [PubMed]
- Sime, F.B.; Johnson, A.; Whalley, S.; Santoyo-Castelazo, A.; Montgomery, A.B.; Walters, K.A.; Lipman, J.; Hope, W.W.; Roberts, J.A. Pharmacodynamics of aerosolized fosfomycin and amikacin against resistant clinical isolates of Pseudomonas aeruginosa and Klebsiella pneumoniae in a hollow-fiber infection model: Experimental basis for combination therapy. Antimicrob. Agents Chemother. 2017, 61, e01763-16. [Google Scholar] [CrossRef] [PubMed]
- Hassan, N.A.; Awdallah, F.F.; Abbassi, M.M.; Sabry, N.A. Nebulized versus IV amikacin as adjunctive antibiotic for hospital and ventilator-acquired pneumonia postcardiac surgeries: A randomized controlled trial. Crit. Care Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- Yagi, K.; Ishii, M.; Namkoong, H.; Asami, T.; Iketani, O.; Asakura, T.; Suzuki, S.; Sugiura, H.; Yamada, Y.; Nishimura, T.; et al. The efficacy, safety, and feasibility of inhaled amikacin for the treatment of difficult-to-treat non-tuberculous mycobacterial lung diseases. BMC Infect. Dis. 2017, 17, 558. [Google Scholar] [CrossRef] [PubMed]
- Ghannam, D.E.; Rodriguez, G.H.; Raad, I.I.; Safdar, A. Inhaled aminoglycosides in cancer patients with ventilator-associated Gram-negative bacterial pneumonia: Safety and feasibility in the era of escalating drug resistance. Eur. J. Clin. Microbiol. Infect. Dis. 2009, 28, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Davis, K.K.; Kao, P.N.; Jacobs, S.S.; Ruoss, S.J. Aerosolized amikacin for treatment of pulmonary Mycobacterium avium infections: An observational case series. BMC Pulm. Med. 2007, 7, 2. [Google Scholar] [CrossRef] [PubMed]
- Olivier, K.N.; Shaw, P.A.; Glaser, T.S.; Bhattacharyya, D.; Fleshner, M.; Brewer, C.C.; Zalewski, C.K.; Folio, L.R.; Siegelman, J.R.; Shallom, S.; et al. Inhaled amikacin for treatment of refractory pulmonary nontuberculous mycobacterial disease. Ann. Am. Thorac. Soc. 2014, 11, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Malinin, V.; Neville, M.; Eagle, G.; Gupta, R.; Perkins, W.R. Pulmonary deposition and elimination of liposomal amikacin for inhalation and effect on macrophage function after administration in rats. Antimicrob. Agents Chemother. 2016, 60, 6540–6549. [Google Scholar] [CrossRef] [PubMed]
- Tsimogianni, A.; Alexandropoulos, P.; Chantziara, V.; Vassi, A.; Micha, G.; Lagiou, F.; Chinou, E.; Michaloudis, G.; Georgiou, S. Intrathecal or intraventricular administration of colistin, vancomycin and amikacin for central nervous system infections in neurosurgical patients in an intensive care unit. Int. J. Antimicrob. Agents 2017, 49, 389–390. [Google Scholar] [CrossRef] [PubMed]
- Berning, S.E.; Cherry, T.A.; Iseman, M.D. Novel treatment of meningitis caused by multidrug-resistant Mycobacterium tuberculosis with intrathecal levofloxacin and amikacin: Case report. Clin. Infect. Dis. 2001, 32, 643–646. [Google Scholar] [CrossRef] [PubMed]
- Nicolau, D.P.; Freeman, C.D.; Belliveau, P.P.; Nightingale, C.H.; Ross, J.W.; Quintiliani, R. Experience with a once-daily aminoglycoside program administered to 2184 adult patients. Antimicrob. Agents Chemother. 1995, 39, 650–655. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Sohn, Y.M.; Ko, J.Y.; Lee, S.Y.; Jhun, B.W.; Park, H.Y.; Jeon, K.; Kim, D.H.; Kim, S.Y.; Choi, J.E.; et al. Once-daily dosing of amikacin for treatment of Mycobacterium abscessus lung disease. Int. J. Tuberc. Lung Dis. 2017, 21, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Sima, M.; Hartinger, J.; Cikankova, T.; Slanar, O. Estimation of once-daily amikacin dose in critically ill adults. J. Chemother. 2017, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Tulkens, P.M. Pharmacokinetic and toxicological evaluation of a once-daily regimen versus conventional schedules of netilmicin and amikacin. J. Antimicrob. Chemother. 1991, 27 (Suppl. C), 49–61. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, A.; Thomson, A.H.; Brown, N.M.; Semple, Y.; Sluman, C.; MacGowan, A.; Lovering, A.M.; Wiffen, P.J. Amikacin use and therapeutic drug monitoring in adults: Do dose regimens and drug exposures affect either outcome or adverse events? A systematic review. J. Antimicrob. Chemother. 2016, 71, 2754–2759. [Google Scholar] [CrossRef] [PubMed]
- Bleyzac, N.; Varnier, V.; Labaune, J.M.; Corvaisier, S.; Maire, P.; Jelliffe, R.W.; Putet, G.; Aulagner, G. Population pharmacokinetics of amikacin at birth and interindividual variability in renal maturation. Eur. J. Clin. Pharmacol. 2001, 57, 499–504. [Google Scholar] [PubMed]
- Labaune, J.M.; Bleyzac, N.; Maire, P.; Jelliffe, R.W.; Boutroy, M.J.; Aulagner, G.; Putet, G. Once-a-day individualized amikacin dosing for suspected infection at birth based on population pharmacokinetic models. Biol. Neonate 2001, 80, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.B.; McCraken, G.H., Jr.; Trujillo, H.; Mohs, E. Amikacin in newborn infants: Comparative pharmacology with kanamycin and clinical efficacy in 45 neonates with bacterial diseases. Antimicrob. Agents Chemother. 1976, 10, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, A.; Karamat, K.A.; Butt, T. Neonatal sepsis: High antibiotic resistance of the bacterial pathogens in a neonatal intensive care unit in Karachi. J. Pak. Med. Assoc. 2002, 52, 348–350. [Google Scholar] [PubMed]
- Hughes, K.M.; Johnson, P.N.; Anderson, M.P.; Sekar, K.C.; Welliver, R.C.; Miller, J.L. Comparison of amikacin pharmacokinetics in neonates following implementation of a new dosage protocol. J. Pediatr. Pharmacol. Ther. 2017, 22, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Friedland, I.R.; Funk, E.; Khoosal, M.; Klugman, K.P. Increased resistance to amikacin in a neonatal unit following intensive amikacin usage. Antimicrob. Agents Chemother. 1992, 36, 1596–1600. [Google Scholar] [CrossRef] [PubMed]
- Schiffelers, R.; Storm, G.; Bakker-Woudenberg, I. Liposome-encapsulated aminoglycosides in pre-clinical and clinical studies. J. Antimicrob. Chemother. 2001, 48, 333–344. [Google Scholar] [CrossRef] [PubMed]
- Krieger, J.; Childs, S.; Klimberg, I. Urinary tract infection treatment using liposomal amikacin (MiKasome). In Proceedings of the Ninth European Congress of Clinical Microbiology and Infectious Diseases, Berlin, Germany, 21–24 March 1999; Elsevier: Amsterdam, The Netherlands, 1999; Volume 5S3, p. 136. [Google Scholar]
- Xiong, Y.Q.; Kupferwasser, L.I.; Zack, P.M.; Bayer, A.S. Comparative efficacies of liposomal amikacin (MiKasome) plus oxacillin versus conventional amikacin plus oxacillin in experimental endocarditis induced by Staphylococcus aureus: Microbiological and echocardiographic analyses. Antimicrob. Agents Chemother. 1999, 43, 1737–1742. [Google Scholar] [PubMed]
- Leitzke, S.; Bucke, W.; Borner, K.; Muller, R.; Hahn, H.; Ehlers, S. Rationale for and efficacy of prolonged-interval treatment using liposome-encapsulated amikacin in experimental Mycobacterium avium infection. Antimicrob. Agents Chemother. 1998, 42, 459–461. [Google Scholar] [PubMed]
- Duzgunes, N.; Perumal, V.K.; Kesavalu, L.; Goldstein, J.A.; Debs, R.J.; Gangadharam, P.R. Enhanced effect of liposome-encapsulated amikacin on Mycobacterium avium-M. intracellulare complex infection in beige mice. Antimicrob. Agents Chemother. 1988, 32, 1404–1411. [Google Scholar] [CrossRef] [PubMed]
- Schiffelers, R.M.; Storm, G.; Ten Kate, M.T.; Bakker-Woudenberg, I.A. Therapeutic efficacy of liposome-encapsulated gentamicin in rat Klebsiella pneumoniae pneumonia in relation to impaired host defense and low bacterial susceptibility to gentamicin. Antimicrob. Agents Chemother. 2001, 45, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Price, K.E.; DeFuria, M.D.; Pursiano, T.A. Amikacin, an aminoglycoside with marked activity against antibiotic-resistant clinical isolates. J. Infect. Dis. 1976, 134, S249–S261. [Google Scholar] [CrossRef] [PubMed]
- Price, K.E.; Pursiano, T.A.; DeFuria, M.D. Activity of BB-K8 (amikacin) against clinical isolates resistant to one or more aminoglycoside antibiotics. Antimicrob. Agents Chemother. 1974, 5, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Miller, G.H.; Sabatelli, F.J.; Hare, R.S.; Glupczynski, Y.; Mackey, P.; Shlaes, D.; Shimizu, K.; Shaw, K.J. The most frequent aminoglycoside resistance mechanisms—Changes with time and geographic area: A reflection of aminoglycoside usage patterns? Clin. Infect. Dis. 1997, 24 (Suppl. 1), S46–S62. [Google Scholar] [CrossRef] [PubMed]
- Jacoby, G.A. Properties of an R plasmid in Pseudomonas aeruginosa producing amikacin (BB-K8), butirosin, kanamycin, tobramycin, and sisomicin resistance. Antimicrob. Agents Chemother. 1974, 6, 807–810. [Google Scholar] [CrossRef] [PubMed]
- Novick, R.P.; Clowes, R.C.; Cohen, S.N.; Curtiss, R.; Datta, N.; Falkow, S. Uniform nomenclature for bacterial plasmids: A proposal. Bacteriol. Rev. 1976, 40, 168–189. [Google Scholar] [PubMed]
- Kawabe, H.; Kondo, S.; Umezawa, H.; Mitsuhashi, S. R factor-mediated aminoglycoside antibiotic resistance in Pseudomonas aeruginosa: A new aminoglycoside 6′-N-acetyltransferase. Antimicrob. Agents Chemother. 1975, 7, 494–499. [Google Scholar] [CrossRef] [PubMed]
- Kawabe, H.; Naito, T.; Mitsuhashi, S. Acetylation of amikacin, a new semisynthetic antibiotic, by Pseudomonas aeruginosa carrying an R factor. Antimicrob. Agents Chemother. 1975, 7, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Hull, R.; Klinger, J.D.; Moody, E.E. Isolation and characterization of mutants of Escherichia coli K12 resistant to the new aminoglycoside antibiotic, amikacin. J. Gen. Microbiol. 1976, 94, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Perlin, M.H.; Lerner, S.A. Amikacin resistance associated with a plasmid-borne aminoglycoside phosphotransferase in Escherichia coli. Antimicrob. Agents Chemother. 1979, 16, 598–604. [Google Scholar] [CrossRef] [PubMed]
- Perlin, M.H.; Lerner, S.A. High-level amikacin resistance in Escherichia coli due to phosphorylation and impaired aminoglycoside uptake. Antimicrob. Agents Chemother. 1986, 29, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Bongaerts, G.P.; Kaptijn, G.M. Aminoglycoside phosphotransferase-II-mediated amikacin resistance in Escherichia coli. Antimicrob. Agents Chemother. 1981, 20, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Coombe, R.G.; George, A.M. New plasmid-mediated aminoglycoside adenylyltransferase of broad substrate range that adenylylates amikacin. Antimicrob. Agents Chemother. 1981, 20, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Murray, B.E.; Moellering, R.C., Jr. In-vivo acquisition of two different types of aminoglycoside resistance by a single strain of Klebsiella pneumoniae causing severe infection. Ann. Intern. Med. 1982, 96, 176–180. [Google Scholar] [CrossRef] [PubMed]
- Cook, L.N.; Davis, R.S.; Stover, B.H. Outbreak of amikacin-resistant Enterobacteriaceae in an intensive care nursery. Pediatrics 1980, 65, 264–268. [Google Scholar] [PubMed]
- Prammananan, T.; Sander, P.; Brown, B.A.; Frischkorn, K.; Onyi, G.O.; Zhang, Y.; Bottger, E.C.; Wallace, R.J., Jr. A single 16S ribosomal RNA substitution is responsible for resistance to amikacin and other 2-deoxystreptamine aminoglycosides in Mycobacterium abscessus and Mycobacterium chelonae. J. Infect. Dis. 1998, 177, 1573–1581. [Google Scholar] [CrossRef] [PubMed]
- Jugheli, L.; Bzekalava, N.; de Rijk, P.; Fissette, K.; Portaels, F.; Rigouts, L. High level of cross-resistance between kanamycin, amikacin, and capreomycin among Mycobacterium tuberculosis isolates from Georgia and a close relation with mutations in the rrs gene. Antimicrob. Agents Chemother. 2009, 53, 5064–5068. [Google Scholar] [CrossRef] [PubMed]
- Sirgel, F.A.; Tait, M.; Warren, R.M.; Streicher, E.M.; Bottger, E.C.; van Helden, P.D.; Gey van Pittius, N.C.; Coetzee, G.; Hoosain, E.Y.; Chabula-Nxiweni, M.; et al. Mutations in the rrs A1401G gene and phenotypic resistance to amikacin and capreomycin in Mycobacterium tuberculosis. Microb. Drug Resist. 2012, 18, 193–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Du, Q.; Dai, G.; Long, Q.; Yu, X.; Dong, L.; Huang, H.; Xie, J. Mycobacterium tuberculosis rrs A1401G mutation correlates with high-level resistance to kanamycin, amikacin, and capreomycin in clinical isolates from mainland China. Diagn. Microbiol. Infect. Dis. 2013, 77, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Kambli, P.; Ajbani, K.; Nikam, C.; Sadani, M.; Shetty, A.; Udwadia, Z.; Georghiou, S.B.; Rodwell, T.C.; Catanzaro, A.; Rodrigues, C. Correlating rrs and eis promoter mutations in clinical isolates of Mycobacterium tuberculosis with phenotypic susceptibility levels to the second-line injectables. Int. J. Mycobacteriol. 2016, 5, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Tsodikov, O.V.; Green, K.D.; Garneau-Tsodikova, S. A random sequential mechanism of aminoglycoside acetylation by Mycobacterium tuberculosis Eis protein. PLoS ONE 2014, 9, e92370. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Biswas, T.; Porter, V.R.; Tsodikov, O.V.; Garneau-Tsodikova, S. Unusual regioversatility of acetyltransferase Eis, a cause of drug resistance in XDR-TB. Proc. Natl. Acad. Sci. USA 2011, 108, 9804–9808. [Google Scholar] [CrossRef] [PubMed]
- Casin, I.; Hanau-Bercot, B.; Podglajen, I.; Vahaboglu, H.; Collatz, E. Salmonella enterica serovar Typhimurium bla(PER-1)-carrying plasmid pSTI1 encodes an extended-spectrum aminoglycoside 6′-N-acetyltransferase of type Ib. Antimicrob. Agents Chemother. 2003, 47, 697–703. [Google Scholar] [CrossRef] [PubMed]
- Robicsek, A.; Strahilevitz, J.; Jacoby, G.A.; Macielag, M.; Abbanat, D.; Park, C.H.; Bush, K.; Hooper, D.C. Fluoroquinolone-modifying enzyme: A new adaptation of a common aminoglycoside acetyltransferase. Nat. Med. 2006, 12, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Fisher, J.F.; Mobashery, S. The bifunctional enzymes of antibiotic resistance. Curr. Opin. Microbiol. 2009, 12, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Centron, D.; Roy, P.H. Presence of a group II intron in a multiresistant Serratia marcescens strain that harbors three integrons and a novel gene fusion. Antimicrob. Agents Chemother. 2002, 46, 1402–1409. [Google Scholar] [CrossRef] [PubMed]
- Boehr, D.D.; Daigle, D.M.; Wright, G.D. Domain-domain interactions in the aminoglycoside antibiotic resistance enzyme AAC(6′)-APH(2″). Biochemistry 2004, 43, 9846–9855. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, J.J.; Gilmore, K.S.; Courvalin, P. Nucleotide sequence analysis of the gene specifying the bifunctional 6′-aminoglycoside acetyltransferase 2″-aminoglycoside phosphotransferase enzyme in Streptococcus faecalis and identification and cloning of gene regions specifying the two activities. J. Bacteriol. 1986, 167, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Culebras, E.; Martinez, J.L. Aminoglycoside resistance mediated by the bifunctional enzyme 6′-N-aminoglycoside acetyltransferase-2″-O-aminoglycoside phosphotransferase. Front. Biosci. 1999, 4, D1–D8. [Google Scholar] [CrossRef] [PubMed]
- Dubois, V.; Poirel, L.; Marie, C.; Arpin, C.; Nordmann, P.; Quentin, C. Molecular characterization of a novel class 1 integron containing bla(GES-1) and a fused product of aac(3)-Ib/aac(6″)-Ib″ gene cassettes in Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2002, 46, 638–645. [Google Scholar] [CrossRef] [PubMed]
- Mendes, R.; Toleman, M.; Ribeiro, J.; Sader, H.; Jones, R.; Walsh, T. Integron carrying a novel metallo-β-lactamase gene, blaIMP-16, and a fused form of aminoglycoside-resistance gene aac(6′)-30/aac(6′)-Ib′: Report from the SENTRY antimicrobial surveillance program. Antimicrob. Agents Chemother. 2004, 48, 4693–4702. [Google Scholar] [CrossRef] [PubMed]
- Li, C.R.; Yang, X.Y.; Lou, R.H.; Zhang, W.X.; Wang, Y.M.; Yuan, M.; Li, Y.; Chen, H.Z.; Hong, B.; Sun, C.H.; et al. In vitro antibacterial activity of vertilmicin and its susceptibility to modifications by the recombinant AAC6′-APH2″ enzyme. Antimicrob. Agents Chemother. 2008, 52, 3875–3882. [Google Scholar] [CrossRef] [PubMed]
- Costa, Y.; Galimand, M.; Leclercq, R.; Duval, J.; Courvalin, P. Characterization of the chromosomal aac(6′)-Ii gene specific for Enterococcus faecium. Antimicrob. Agents Chemother. 1993, 37, 1896–1903. [Google Scholar] [CrossRef] [PubMed]
- Chow, J.W.; Kak, V.; You, I.; Kao, S.J.; Petrin, J.; Clewell, D.B.; Lerner, S.A.; Miller, G.H.; Shaw, K.J. Aminoglycoside resistance genes aph(2″)-Ib and aac(6′)-Im detected together in strains of both Escherichia coli and Enterococcus faecium. Antimicrob. Agents Chemother. 2001, 45, 2691–2694. [Google Scholar] [CrossRef] [PubMed]
- Rouch, D.A.; Byrne, M.E.; Kong, Y.C.; Skurray, R.A. The aacA-aphD gentamicin and kanamycin resistance determinant of Tn4001 from Staphylococcus aureus: Expression and nucleotide sequence analysis. J. Gen. Microbiol. 1987, 133, 3039–3052. [Google Scholar] [CrossRef] [PubMed]
- Zarrilli, R.; Tripodi, M.F.; Di Popolo, A.; Fortunato, R.; Bagattini, M.; Crispino, M.; Florio, A.; Triassi, M.; Utili, R. Molecular epidemiology of high-level aminoglycoside-resistant enterococci isolated from patients in a university hospital in southern Italy. J. Antimicrob. Chemother. 2005, 56, 827–835. [Google Scholar] [CrossRef] [PubMed]
- Holbrook, S.Y.; Garneau-Tsodikova, S. Expanding aminoglycoside resistance enzyme regiospecificity by mutation and truncation. Biochemistry 2016, 55, 5726–5737. [Google Scholar] [CrossRef] [PubMed]
- Sadowy, E.; Sienko, A.; Gawryszewska, I.; Bojarska, A.; Malinowska, K.; Hryniewicz, W. High abundance and diversity of antimicrobial resistance determinants among early vancomycin-resistant Enterococcus faecium in Poland. Eur. J. Clin. Microbiol. Infect. Dis. 2013, 32, 1193–1203. [Google Scholar] [CrossRef] [PubMed]
- Chow, V.C.; Hawkey, P.M.; Chan, E.W.; Chin, M.L.; Au, T.K.; Fung, D.K.; Chan, R.C. High-level gentamicin resistance mediated by a Tn4001-like transposon in seven nonclonal hospital isolates of Streptococcus pasteurianus. Antimicrob. Agents Chemother. 2007, 51, 2508–2513. [Google Scholar] [CrossRef] [PubMed]
- Lyon, B.R.; Gillespie, M.T.; Byrne, M.E.; May, J.W.; Skurray, R.A. Plasmid-mediated resistance to gentamicin in Staphylococcus aureus: The involvement of a transposon. J. Med. Microbiol. 1987, 23, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, M.T.; Lyon, B.R.; Messerotti, L.J.; Skurray, R.A. Chromosome- and plasmid-mediated gentamicin resistance in Staphylococcus aureus encoded by Tn4001. J. Med. Microbiol. 1987, 24, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Hodel-Christian, S.L.; Murray, B.E. Characterization of the gentamicin resistance transposon Tn5281 from Enterococcus faecalis and comparison to staphylococcal transposons Tn4001 and Tn4031. Antimicrob. Agents Chemother. 1991, 35, 1147–1152. [Google Scholar] [CrossRef] [PubMed]
- Thomas, W.D., Jr.; Archer, G.L. Mobility of gentamicin resistance genes from staphylococci isolated in the United States: Identification of Tn4031, a gentamicin resistance transposon from Staphylococcus epidermidis. Antimicrob. Agents Chemother. 1989, 33, 1335–1341. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, S.J.; Huang, Y.; Berghuis, A.M. Antibiotic binding drives catalytic activation of aminoglycoside kinase APH(2″)-Ia. Structure 2016, 24, 935–945. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.A.; Toth, M.; Bhattacharya, M.; Frase, H.; Vakulenko, S.B. Structure of the phosphotransferase domain of the bifunctional aminoglycoside-resistance enzyme AAC(6′)-Ie-APH(2″)-Ia. Acta Crystallogr. D Biol. Crystallogr. 2014, 70, 1561–1571. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.A.; Toth, M.; Weiss, T.M.; Frase, H.; Vakulenko, S.B. Structure of the bifunctional aminoglycoside-resistance enzyme AAC(6′)-Ie-APH(2″)-Ia revealed by crystallographic and small-angle X-ray scattering analysis. Acta Crystallogr. D Biol. Crystallogr. 2014, 70, 2754–2764. [Google Scholar] [CrossRef] [PubMed]
- Burk, D.L.; Ghuman, N.; Wybenga-Groot, L.E.; Berghuis, A.M. X-ray structure of the AAC(6′)-Ii antibiotic resistance enzyme at 1.8 A resolution; examination of oligomeric arrangements in GNAT superfamily members. Protein Sci. 2003, 12, 426–437. [Google Scholar] [CrossRef] [PubMed]
- Burk, D.L.; Xiong, B.; Breitbach, C.; Berghuis, A.M. Structures of aminoglycoside acetyltransferase AAC(6′)-Ii in a novel crystal form: Structural and normal-mode analyses. Acta Crystallogr. D Biol. Crystallogr. 2005, 61, 1273–1279. [Google Scholar] [CrossRef] [PubMed]
- Draker, K.A.; Northrop, D.B.; Wright, G.D. Kinetic mechanism of the GCN5-related chromosomal aminoglycoside acetyltransferase AAC(6′)-Ii from Enterococcus faecium: Evidence of dimer subunit cooperativity. Biochemistry 2003, 42, 6565–6574. [Google Scholar] [CrossRef] [PubMed]
- Boucher, H.W.; Talbot, G.H.; Bradley, J.S.; Edwards, J.E.; Gilbert, D.; Rice, L.B.; Scheld, M.; Spellberg, B.; Bartlett, J. Bad bugs, no drugs: No ESKAPE! An update from the Infectious Diseases Society of America. Clin. Infect. Dis. 2009, 48, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Pourreza, A.; Witherspoon, M.; Fox, J.; Newmark, J.; Bui, D.; Tolmasky, M.E. Mutagenesis analysis of a conserved region involved in acetyl coenzyme A binding in the aminoglycoside 6′-N-acetyltransferase type Ib encoded by plasmid pJHCMW1. Antimicrob. Agents Chemother. 2005, 49, 2979–2982. [Google Scholar] [CrossRef] [PubMed]
- Rice, L.B.; Carias, L.L.; Hutton, R.A.; Rudin, S.D.; Endimiani, A.; Bonomo, R.A. The KQ element, a complex genetic region conferring transferable resistance to carbapenems, aminoglycosides, and fluoroquinolones in Klebsiella pneumoniae. Antimicrob. Agents Chemother. 2008, 52, 3427–3429. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, M.S.; Traglia, G.M.; Lin, D.L.; Tran, T.; Tolmasky, M.E. Plasmid-mediated antibiotic resistance and virulence in Gram-negatives: The Klebsiella pneumoniae paradigm. Microbiol. Spectr. 2014, 2, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, E.; Saenz, Y.; Zarazaga, M.; Rocha-Gracia, R.; Martinez-Martinez, L.; Arlet, G.; Torres, C. qnr, aac(6′)-Ib-cr and qepA genes in Escherichia coli and Klebsiella spp.: Genetic environments and plasmid and chromosomal location. J. Antimicrob. Chemother. 2012, 67, 886–897. [Google Scholar] [CrossRef] [PubMed]
- Arivett, B.A.; Fiester, S.E.; Ream, D.C.; Centron, D.; Ramirez, M.S.; Tolmasky, M.E.; Actis, L.A. Draft genome of the multidrug-resistant Acinetobacter baumannii strain A155 clinical isolate. Genome Announc. 2015, 3, e00212–e00215. [Google Scholar] [CrossRef] [PubMed]
- Poirel, L.; Cabanne, L.; Collet, L.; Nordmann, P. Class II transposon-borne structure harboring metallo-β-lactamase gene blaVIM-2 in Pseudomonas putida. Antimicrob. Agents Chemother. 2006, 50, 2889–2891. [Google Scholar] [CrossRef] [PubMed]
- Chamorro, R.M.; Actis, L.A.; Crosa, J.H.; Tolmasky, M.E. Dissemination of plasmid-mediated amikacin resistance among pathogenic Klebsiella pneumoniae. Medicina 1990, 50, 543–547. [Google Scholar] [PubMed]
- Woodford, N.; Carattoli, A.; Karisik, E.; Underwood, A.; Ellington, M.J.; Livermore, D.M. Complete nucleotide sequences of plasmids pEK204, pEK499, and pEK516, encoding CTX-M enzymes in three major Escherichia coli lineages from the United Kingdom, all belonging to the international O25:H4-ST131 clone. Antimicrob. Agents Chemother. 2009, 53, 4472–4482. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Chavda, K.D.; Al Laham, N.; Melano, R.G.; Jacobs, M.R.; Bonomo, R.A.; Kreiswirth, B.N. Complete nucleotide sequence of a blaKPC-harboring IncI2 plasmid and its dissemination in New Jersey and New York hospitals. Antimicrob. Agents Chemother. 2013, 57, 5019–5025. [Google Scholar] [CrossRef] [PubMed]
- Gillings, M.R. Class 1 integrons as invasive species. Curr. Opin. Microbiol. 2017, 38, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Escudero, J.A.; Loot, C.; Nivina, A.; Mazel, D. The integron: Adaptation on demand. Microbiol. Spectr. 2015, 3. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, M.S.; Parenteau, T.R.; Centron, D.; Tolmasky, M.E. Functional characterization of Tn1331 gene cassettes. J. Antimicrob. Chemother. 2008, 62, 669–673. [Google Scholar] [CrossRef] [PubMed]
- Zong, Z.; Partridge, S.R.; Iredell, J.R. A blaVEB-1 variant, blaVEB-6, associated with repeated elements in a complex genetic structure. Antimicrob. Agents Chemother. 2009, 53, 1693–1697. [Google Scholar] [CrossRef] [PubMed]
- Van Nhieu, G.T.; Collatz, E. Primary structure of an aminoglycoside 6′-N-acetyltransferase AAC(6′)-4, fused in vivo with the signal peptide of the Tn3-encoded β-lactamase. J. Bacteriol. 1987, 169, 5708–5714. [Google Scholar] [CrossRef]
- Van Nhieu, G.T.; Goldstein, F.W.; Pinto, M.E.; Acar, J.F.; Collatz, E. Transfer of amikacin resistance by closely related plasmids in members of the family Enterobacteriaceae isolated in Chile. Antimicrob. Agents Chemother. 1986, 29, 833–837. [Google Scholar] [CrossRef] [PubMed]
- Nobuta, K.; Tolmasky, M.E.; Crosa, L.M.; Crosa, J.H. Sequencing and expression of the 6′-N-acetyltransferase gene of transposon Tn1331 from Klebsiella pneumoniae. J. Bacteriol. 1988, 170, 3769–3773. [Google Scholar] [CrossRef] [PubMed]
- Sarno, R.; McGillivary, G.; Sherratt, D.J.; Actis, L.A.; Tolmasky, M.E. Complete nucleotide sequence of Klebsiella pneumoniae multiresistance plasmid pJHCMW1. Antimicrob. Agents Chemother. 2002, 46, 3422–3427. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Lamothe, R.; Tran, T.; Meas, D.; Lee, L.; Li, A.M.; Sherratt, D.J.; Tolmasky, M.E. High-copy bacterial plasmids diffuse in the nucleoid-free space, replicate stochastically and are randomly partitioned at cell division. Nucleic Acids Res. 2014, 42, 1042–1051. [Google Scholar] [CrossRef] [PubMed]
- Trigueros, S.; Tran, T.; Sorto, N.; Newmark, J.; Colloms, S.D.; Sherratt, D.J.; Tolmasky, M.E. mwr Xer site-specific recombination is hypersensitive to DNA supercoiling. Nucleic Acids Res. 2009, 37, 3580–3587. [Google Scholar] [CrossRef] [PubMed]
- Quiroga, M.P.; Orman, B.; Errecalde, L.; Kaufman, S.; Centron, D. Characterization of Tn6238 with a new allele of aac(6′)-Ib-cr. Antimicrob. Agents Chemother. 2015, 59, 2893–2897. [Google Scholar] [CrossRef] [PubMed]
- Warburg, G.; Hidalgo-Grass, C.; Partridge, S.R.; Tolmasky, M.E.; Temper, V.; Moses, A.E.; Block, C.; Strahilevitz, J. A carbapenem-resistant Klebsiella pneumoniae epidemic clone in Jerusalem: Sequence type 512 carrying a plasmid encoding aac(6′)-Ib. J. Antimicrob. Chemother. 2012, 67, 898–901. [Google Scholar] [CrossRef] [PubMed]
- He, S.; Chandler, M.; Varani, A.M.; Hickman, A.B.; Dekker, J.P.; Dyda, F. Mechanisms of evolution in high-consequence drug resistance plasmids. MBio 2016, 7, e01987-16. [Google Scholar] [CrossRef] [PubMed]
- He, S.; Hickman, A.B.; Varani, A.M.; Siguier, P.; Chandler, M.; Dekker, J.P.; Dyda, F. Insertion sequence IS26 reorganizes plasmids in clinically isolated multidrug-resistant bacteria by replicative transposition. MBio 2015, 6, e00762. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Mathema, B.; Chavda, K.D.; DeLeo, F.R.; Bonomo, R.A.; Kreiswirth, B.N. Carbapenemase-producing Klebsiella pneumoniae: Molecular and genetic decoding. Trends Microbiol. 2014, 22, 686–696. [Google Scholar] [CrossRef] [PubMed]
- Chavda, K.D.; Chen, L.; Jacobs, M.R.; Bonomo, R.A.; Kreiswirth, B.N. Molecular diversity and plasmid analysis of KPC-producing Escherichia coli. Antimicrob. Agents Chemother. 2016, 60, 4073–4081. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Deng, H.; Li, L.; Chen, M.Y.; Fang, L.X.; Yang, Q.E.; Liu, Y.H.; Liao, X.P. Complete nucleotide sequence of cfr-carrying IncX4 plasmid pSD11 from Escherichia coli. Antimicrob. Agents Chemother. 2015, 59, 738–741. [Google Scholar] [CrossRef] [PubMed]
- Deleo, F.R.; Chen, L.; Porcella, S.F.; Martens, C.A.; Kobayashi, S.D.; Porter, A.R.; Chavda, K.D.; Jacobs, M.R.; Mathema, B.; Olsen, R.J.; et al. Molecular dissection of the evolution of carbapenem-resistant multilocus sequence type 258 Klebsiella pneumoniae. Proc. Natl. Acad. Sci. USA 2014, 111, 4988–4993. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, S.; Mondal, A.; Mitra, S.; Basu, S. Acinetobacter baumannii transfers the blaNDM-1 gene via outer membrane vesicles. J. Antimicrob. Chemother. 2017, 72, 2201–2207. [Google Scholar] [CrossRef] [PubMed]
- Rumbo, C.; Fernandez-Moreira, E.; Merino, M.; Poza, M.; Mendez, J.A.; Soares, N.C.; Mosquera, A.; Chaves, F.; Bou, G. Horizontal transfer of the OXA-24 carbapenemase gene via outer membrane vesicles: A new mechanism of dissemination of carbapenem resistance genes in Acinetobacter baumannii. Antimicrob. Agents Chemother. 2011, 55, 3084–3090. [Google Scholar] [CrossRef] [PubMed]
- Yaron, S.; Kolling, G.L.; Simon, L.; Matthews, K.R. Vesicle-mediated transfer of virulence genes from Escherichia coli O157:H7 to other enteric bacteria. Appl. Environ. Microbiol. 2000, 66, 4414–4420. [Google Scholar] [CrossRef] [PubMed]
- Saberi, F.; Kamali, M.; Najafi, A.; Yazdanparast, A.; Moghaddam, M.M. Natural antisense RNAs as mRNA regulatory elements in bacteria: A review on function and applications. Cell. Mol. Biol. Lett. 2016, 21, 6. [Google Scholar] [CrossRef] [PubMed]
- Thomason, M.K.; Storz, G. Bacterial antisense RNAs: How many are there, and what are they doing? Annu. Rev. Genet. 2010, 44, 167–188. [Google Scholar] [CrossRef] [PubMed]
- Waldbeser, L.S.; Tolmasky, M.E.; Actis, L.A.; Crosa, J.H. Mechanisms for negative regulation by iron of the fatA outer membrane protein gene expression in Vibrio anguillarum 775. J. Biol. Chem. 1993, 268, 10433–10439. [Google Scholar] [PubMed]
- Tolmasky, M.E.; Actis, L.A.; Crosa, J.H. Plasmid DNA replication. In Encyclopedia of Industrial Biotechnology: Bioprocess, Bioseparation, and Cell Technology; Flickinger, M., Ed.; John Wiley and Sons, Inc.: New York, NY, USA, 2010; Volume 6, pp. 3931–3953. [Google Scholar]
- Brantl, S. Plasmid Replication Control by Antisense RNAs. In Plasmids: Biology and Impact in Biotiechnology and Discovery; Tolmasky, M.E., Alonso, J., Eds.; ASM Press: Washignton, DC, USA, 2015; pp. 83–104. [Google Scholar]
- Goyal, N.; Narayanaswami, P. Making sense of antisense oligonucleotides: A narrative review. Muscle Nerve 2017. [Google Scholar] [CrossRef] [PubMed]
- Woodford, N.; Wareham, D.W. Tackling antibiotic resistance: A dose of common antisense? J. Antimicrob. Chemother. 2009, 63, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, L.C.; Sperling-Petersen, H.U.; Mortensen, K.K. Hitting bacteria at the heart of the central dogma: Sequence-specific inhibition. Microb. Cell Fact. 2007, 6, 24. [Google Scholar] [CrossRef] [PubMed]
- Davies-Sala, C.; Soler-Bistue, A.; Bonomo, R.A.; Zorreguieta, A.; Tolmasky, M.E. External guide sequence technology: A path to development of novel antimicrobial therapeutics. Ann. N. Y. Acad. Sci. 2015, 1354, 98–110. [Google Scholar] [CrossRef] [PubMed]
- Dinan, A.M.; Loftus, B.J. (Non-)translational medicine: Targeting bacterial RNA. Front. Genet. 2013, 4, 230. [Google Scholar] [CrossRef] [PubMed]
- Sully, E.K.; Geller, B.L. Antisense antimicrobial therapeutics. Curr. Opin. Microbiol. 2016, 33, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Sarno, R.; Ha, H.; Weinsetel, N.; Tolmasky, M.E. Inhibition of aminoglycoside 6′-N-acetyltransferase type Ib-mediated amikacin resistance by antisense oligodeoxynucleotides. Antimicrob. Agents Chemother. 2003, 47, 3296–3304. [Google Scholar] [CrossRef] [PubMed]
- Lopez, C.; Arivett, B.A.; Actis, L.A.; Tolmasky, M.E. Inhibition of AAC(6′)-Ib-mediated resistance to amikacin in Acinetobacter baumannii by an antisense peptide-conjugated 2’,4’-bridged nucleic acid-NC-DNA hybrid oligomer. Antimicrob. Agents Chemother. 2015, 59, 5798–5803. [Google Scholar] [CrossRef] [PubMed]
- Lundblad, E.W.; Altman, S. Inhibition of gene expression by RNase P. New Biotechnol. 2010, 27, 212–221. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.; Jani, S.; Sala, C.D.; Soler-Bistue, A.J.; Zorreguieta, A.; Tolmasky, M.E. Assessment of configurations and chemistries of bridged nucleic acids-containing oligomers as external guide sequences: A methodology for inhibition of expression of antibiotic resistance genes. Biol. Methods Protoc. 2016, 1. [Google Scholar] [CrossRef] [PubMed]
- Soler Bistue, A.J.; Ha, H.; Sarno, R.; Don, M.; Zorreguieta, A.; Tolmasky, M.E. External guide sequences targeting the aac(6′)-Ib mRNA induce inhibition of amikacin resistance. Antimicrob. Agents Chemother. 2007, 51, 1918–1925. [Google Scholar] [CrossRef] [PubMed]
- Bistue, A.J.S.; Martin, F.A.; Vozza, N.; Ha, H.; Joaquin, J.C.; Zorreguieta, A.; Tolmasky, M.E. Inhibition of aac(6′)-Ib-mediated amikacin resistance by nuclease-resistant external guide sequences in bacteria. Proc. Natl. Acad. Sci. USA 2009, 106, 13230–13235. [Google Scholar] [CrossRef] [PubMed]
- Tolmasky, M.E. Strategies to prolong the useful life of existing antibiotics and help overcoming the antibiotic resistance crisis. In Frontiers in Clinical Drug Research-Anti Infectives; Atta-ur-Rhaman, Ed.; Bentham Books: Sharjah, UAE, 2017; Volume 1, pp. 1–27. [Google Scholar]
- Lombes, T.; Begis, G.; Maurice, F.; Turcaud, S.; Lecourt, T.; Dardel, F.; Micouin, L. NMR-guided fragment-based approach for the design of AAC(6′)-Ib ligands. ChemBioChem 2008, 9, 1368–1371. [Google Scholar] [CrossRef] [PubMed]
- Friesner, R.A.; Banks, J.L.; Murphy, R.B.; Halgren, T.A.; Klicic, J.J.; Mainz, D.T.; Repasky, M.P.; Knoll, E.H.; Shelley, M.; Perry, J.K.; et al. Glide: A new approach for rapid, accurate docking and scoring. 1. Method and assessment of docking accuracy. J. Med. Chem. 2004, 47, 1739–1749. [Google Scholar] [CrossRef] [PubMed]
- Halgren, T.A.; Murphy, R.B.; Friesner, R.A.; Beard, H.S.; Frye, L.L.; Pollard, W.T.; Banks, J.L. Glide: A new approach for rapid, accurate docking and scoring. 2. Enrichment factors in database screening. J. Med. Chem. 2004, 47, 1750–1759. [Google Scholar] [CrossRef] [PubMed]
- Trott, O.; Olson, A.J. AutoDock Vina: Improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J. Comput. Chem. 2010, 31, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Chiem, K.; Jani, S.; Fuentes, B.; Lin, D.L.; Rasche, M.E.; Tolmasky, M.E. Identification of an inhibitor of the aminoglycoside 6′-N-acetyltransferase type Ib [AAC(6′)-Ib] by glide molecular docking. MedChemComm 2016, 7, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Lin, D.L.; Tran, T.; Adams, C.; Alam, J.Y.; Herron, S.R.; Tolmasky, M.E. Inhibitors of the aminoglycoside 6′-N-acetyltransferase type Ib [AAC(6′)-Ib] identified by in silico molecular docking. Bioorg. Med. Chem. Lett. 2013, 23, 5694–5698. [Google Scholar] [CrossRef] [PubMed]
- Green, K.D.; Chen, W.; Garneau-Tsodikova, S. Identification and characterization of inhibitors of the aminoglycoside resistance acetyltransferase Eis from Mycobacterium tuberculosis. ChemMedChem 2012, 7, 73–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garzan, A.; Willby, M.J.; Green, K.D.; Gajadeera, C.S.; Hou, C.; Tsodikov, O.V.; Posey, J.E.; Garneau-Tsodikova, S. Sulfonamide-based Inhibitors of aminoglycoside acetyltransferase Eis abolish resistance to kanamycin in Mycobacterium tuberculosis. J. Med. Chem. 2016, 59, 10619–10628. [Google Scholar] [CrossRef] [PubMed]
- Garzan, A.; Willby, M.J.; Ngo, H.X.; Gajadeera, C.S.; Green, K.D.; Holbrook, S.Y.; Hou, C.; Posey, J.E.; Tsodikov, O.V.; Garneau-Tsodikova, S. Combating enhanced intracellular survival (Eis)-mediated kanamycin resistance of Mycobacterium tuberculosis by novel pyrrolo[1,5-a]pyrazine-based Eis inhibitors. ACS Infect. Dis. 2017, 3, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Garzan, A.; Willby, M.J.; Green, K.D.; Tsodikov, O.V.; Posey, J.E.; Garneau-Tsodikova, S. Discovery and optimization of two Eis inhibitor families as kanamycin adjuvants against drug-resistant M. tuberculosis. ACS Med. Chem. Lett. 2016, 7, 1219–1221. [Google Scholar] [CrossRef] [PubMed]
- Chiem, K.; Fuentes, B.A.; Lin, D.L.; Tran, T.; Jackson, A.; Ramirez, M.S.; Tolmasky, M.E. Inhibition of aminoglycoside 6′-N-acetyltransferase type Ib-mediated amikacin resistance in Klebsiella pneumoniae by zinc and copper pyrithione. Antimicrob. Agents Chemother. 2015, 59, 5851–5853. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Green, K.D.; Johnson, B.R.; Garneau-Tsodikova, S. Inhibition of aminoglycoside acetyltransferase resistance enzymes by metal salts. Antimicrob. Agents Chemother. 2015, 59, 4148–4156. [Google Scholar] [CrossRef] [PubMed]
- Lin, D.L.; Tran, T.; Alam, J.Y.; Herron, S.R.; Ramirez, M.S.; Tolmasky, M.E. Inhibition of aminoglycoside 6′-N-acetyltransferase type Ib by zinc: Reversal of amikacin resistance in Acinetobacter baumannii and Escherichia coli by a zinc ionophore. Antimicrob. Agents Chemother. 2014, 58, 4238–4241. [Google Scholar] [CrossRef] [PubMed]
- Barnham, K.J.; Bush, A.I. Biological metals and metal-targeting compounds in major neurodegenerative diseases. Chem. Soc. Rev. 2014, 43, 6727–6749. [Google Scholar] [CrossRef] [PubMed]
- Bareggi, S.R.; Cornelli, U. Clioquinol: Review of its mechanisms of action and clinical uses in neurodegenerative disorders. CNS Neurosci. Ther. 2012, 18, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Chiem, K.; Hue, F.; Magallon, J.; Tolmasky, M.E. Inhibition of aminoglycoside 6′-N-acetyltransferase type Ib-mediated amikacin resistance by zinc complexed to clioquinol, an ionophore active against tumors and neurodegenerative diseases. Int. J. Antimicrob. Agents 2017. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, K.; Hayashi, I.; Kouda, S.; Kato, F.; Fujiwara, T.; Kayama, S.; Hirakawa, H.; Itaha, H.; Ohge, H.; Gotoh, N.; et al. Identification and characterization of a novel aac(6′)-Iag associated with the blaIMP-1-integron in a multidrug-resistant Pseudomonas aeruginosa. PLoS ONE 2013, 8, e70557. [Google Scholar] [CrossRef] [PubMed]
- Xiong, J.; Hawkey, P.; Roy, P.H. Novel Class 1 Integrons on Large Plasmids in Multiresistant Pseudomonas aeruginosa Isolated from a Multicenter Survey in Guangzhou, PRC. Available online: https://www.ncbi.nlm.nih.gov/nuccore/208436664 (accessed on 11 November 2017).
- Tada, T.; Miyoshi-Akiyama, T.; Shimada, K.; Shimojima, M.; Kirikae, T. Novel 6′-N-aminoglycoside acetyltransferase AAC(6′)-Iaj from a clinical isolate of Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2013, 57, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Tada, T.; Miyoshi-Akiyama, T.; Dahal, R.K.; Mishra, S.K.; Shimada, K.; Ohara, H.; Kirikae, T.; Pokhrel, B.M. Identification of a novel 6′-N-aminoglycoside acetyltransferase, AAC(6′)-Iak, from a multidrug-resistant clinical isolate of Stenotrophomonas maltophilia. Antimicrob. Agents Chemother. 2014, 58, 6324–6327. [Google Scholar] [CrossRef] [PubMed]
- Tada, T.; Miyoshi-Akiyama, T.; Shimada, K.; Dahal, R.K.; Mishra, S.K.; Ohara, H.; Kirikae, T.; Pokhrel, B.M. A novel 6′-N-aminoglycoside acetyltransferase, AAC(6′)-Ial, from a clinical isolate of Serratia marcescens. Microb. Drug Resist. 2016, 22, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Jin, W.; Wachino, J.; Kimura, K.; Yamada, K.; Arakawa, Y. New plasmid-mediated aminoglycoside 6′-N-acetyltransferase, AAC(6′)-Ian, and ESBL, TLA-3, from a Serratia marcescens clinical isolate. J. Antimicrob. Chemother. 2015, 70, 1331–1337. [Google Scholar] [CrossRef] [PubMed]




| Enzyme | Genetic Location | Accession Number | Host | Reference |
|---|---|---|---|---|
| AAC(6′)-Iag | Integron (In124)-Plasmid | AB472901 | P. aeruginosa | [270] |
| AAC(6′)-Iai | Integron | EU886977 | P. aeruginosa | [271] |
| AAC(6′)-Iaj | Integron (In151)-Chromosome | AB709942 | P. aeruginosa | [272] |
| AAC(6′)-Iak | Chromosome | AB894482 | Stenotrophomonas maltophilia | [273] |
| AAC(6′)-Ial | Chromosome | AB894481 | S. marcescens | [274] |
| AAC(6′)-Ian | Plasmid | AP014611 | S. marcescens | [275] |
| AAC(6′)-Iap 2 | AB979699 | S. marcescens | [274] |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramirez, M.S.; Tolmasky, M.E. Amikacin: Uses, Resistance, and Prospects for Inhibition. Molecules 2017, 22, 2267. https://doi.org/10.3390/molecules22122267
Ramirez MS, Tolmasky ME. Amikacin: Uses, Resistance, and Prospects for Inhibition. Molecules. 2017; 22(12):2267. https://doi.org/10.3390/molecules22122267
Chicago/Turabian StyleRamirez, Maria S., and Marcelo E. Tolmasky. 2017. "Amikacin: Uses, Resistance, and Prospects for Inhibition" Molecules 22, no. 12: 2267. https://doi.org/10.3390/molecules22122267
APA StyleRamirez, M. S., & Tolmasky, M. E. (2017). Amikacin: Uses, Resistance, and Prospects for Inhibition. Molecules, 22(12), 2267. https://doi.org/10.3390/molecules22122267