Traditional Uses, Botany, Phytochemistry, Pharmacology, Pharmacokinetics and Toxicology of Xanthium strumarium L.: A Review
Abstract
:1. Introduction
2. Traditional Usages
3. Botany
4. Phytochemistry
4.1. Sesquiterpenoids and Triterpenoids
4.2. Phenylpropenoids
4.3. Lignanoids and Coumarins
4.4. Steroids
4.5. Glycosides
4.6. Flavonoids
4.7. Thiazides
4.8. Other Compounds
5. Pharmacology
5.1. Anti-AR Effect
5.2. Anti-Tumor Effect
5.3. Anti-Inflammatory and Analgesic Effects
5.4. Insecticide and Antiparasitic Effects
5.5. Antioxidant Effect
5.6. Antibacterial and Antifungal Effects
5.7. Antidiabetic Effect
5.8. Antilipidemic Effect
5.9. Antiviral Activity
5.10. Other Pharmacological Effects
5.11. Summary of Pharmacologic Effects
6. Pharmacokinetics
7. Toxicity
8. Future Perspectives and Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| WEX | water extracts of fruit of Xanthium strumarium |
| MEX | methanol extracts of fruits of X. strumarium |
| EEXA | ethanol extracts of aerial parts of X. strumarium |
| EEXS | ethanol extracts of stems of X. strumarium |
| WFEEX | water fraction of ethanol extracts of fruits of X. strumarium |
| NFEEX | n-butanol fraction of ethanol extracts of fruits of X. strumarium |
| MEXA | methanol extracts of aerial parts of X. strumarium |
| HEXA | hydroalcoholic extracts of aerial parts of X. strumarium |
| EAFEEX | ethylacetate fraction of ethanol extracts of fruits of X. strumarium |
| CFEEXA | chloroform fraction of ethanol extracts of aerial parts of X. strumarium |
| CEXR | chloroform extracts of roots of X. strumarium |
| MEXR | methanol extracts of roots of X. strumarium |
| EAFMEX | ethylacetate fraction of methanol extracts of fruits of X. strumarium |
| DFEEXA | dichloromethane fraction of ethanol extracts of aerial parts of X. strumarium |
| EEX | ethanol extracts of fruits of X. strumarium |
| MEXL | methanol extracts of leaves of X. strumarium |
| WEXL | water extracts of leaveas of X. strumarium |
| EEXL | ethanol extracts of leaves of X. strumarium |
| EEXL | ethanol extracts of leaves of X. strumarium |
| PEEXW | petroleum ether extracts of whole plant of X. strumarium |
| MEXS | methanol extracts of stems of X. strumarium |
| EEXR | ethanol extracts of roots of X. strumarium |
| EOX | essential oil of fruits of Xanthium strumarium |
| EOXL | essential oil of leaves of Xanthium strumarium |
| WEXFT | water extract of flowering twigs of Xanthium strumarium |
| CFMEXL | chloroform fraction of methanol extracts of leaves of X. strumarium |
| MEXW | methanol extracts of whole plant of X. strumarium |
| HEEXB | hydro-ethanol extracts of burs of X. strumarium |
| HEEXA | hydro-ethanol extracts of aerial parts of X. strumarium |
| EFEEX | ethylacetate fraction of ethanol extracts of X. strumarium |
References
- Kamboj, A.; Saluja, A.K. Phytopharmacological review of Xanthium strumarium L. (Cocklebur). Int. J. Green Pharm. 2010, 4, 129–139. [Google Scholar] [CrossRef]
- Chinese Pharmacopoeia Commission. Pharmacopoeia of the People’s Republic of China Part I; People’s Medical Publishing House: Beijing, China, 1963; p. 130. (In Chinese) [Google Scholar]
- Amin, S.; Barkatullah; Khan, H. Pharmacology of Xanthium species. A review. J. Phytopharmacol. 2016, 5, 126–127. [Google Scholar]
- Zhuang, Y.S.; Hu, J.; Cai, H.; Qin, K.M.; Yang, B.; Liu, X.; Cai, B.C. advanced study on chemical constituents and pharmaceutical activities of Xanthium strumarium. J. Nanjing Univ. Tradit. Chin. Med. 2017, 33, 428–432. (In Chinese) [Google Scholar]
- Chinese Pharmacopoeia Commission. Pharmacopoeia of the People’s Republic of China Part I; People’s Medical Publishing House: Beijing, China, 2015; p. 162. (In Chinese) [Google Scholar]
- Nanjing University of Traditional Chinese Medicine. Traditional Chinese Medicine Dictionary; Shanghai Science and Technology Press: Shanghai, China, 1986; p. 1071. (In Chinese) [Google Scholar]
- Chopra, R.N.; Nayar, S.L.; Chopra, I.C. Glossary of Indian Medicinal Plants; Council of Scientific and Industrial Research: New Delhi, India, 1986; p. 259. [Google Scholar]
- Islam, M.R.; Uddin, M.Z.; Rahman, M.S.; Tutul, E.; Rahman, M.Z.; Hassan, M.A.; Faiz, M.A.; Hossain, M.; Hussain, M.; Rashid, M.A. Ethnobotanical, phytochemical and toxicological studies of Xanthium strumarium L. Bangladesh Med. Res. Counc. Bull. 2009, 35, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Chang, F.; Hanna, M.A.; Zhang, D.J.; Li, H.; Zhou, Q.; Song, B.A.; Yang, S. Production of biodiesel from non-edible herbaceous vegetable oil: Xanthium sibiricum Patr. Bioresour. Technol. 2013, 140, 435–438. [Google Scholar] [CrossRef] [PubMed]
- Rozina; Asif, S.; Ahmad, M.; Zafar, M.; Ali, N. Prospects and potential of fatty acid methyl esters of some non-edible seed oils for use as biodiesel in Pakistan. Renew. Sustain. Energy Rev. 2017, 74, 687–702. [Google Scholar] [CrossRef]
- Chinese Flora Commission. Flora of China; Science Publishing House: Beijing, China, 1975; p. 325. (In Chinese) [Google Scholar]
- State Administration of Traditional Chinese Medicine. Chinese Materia Medica; Shanghai Science and Technology Press: Shanghai, China, 1998; pp. 1010–1013. (In Chinese) [Google Scholar]
- Shi, Y.S.; Liu, Y.B.; Ma, S.G.; Li, Y.; Qu, J.; Li, L.; Yuan, S.P.; Hou, Q.; Li, Y.H.; Jiang, J.D.; et al. Bioactive Sesquiterpenes and Lignans from the Fruits of Xanthium sibiricum. J. Nat. Prod. 2015, 78, 1526–1535. [Google Scholar] [CrossRef] [PubMed]
- Han, T.; Zhang, H.; Li, H.l.; Zhang, Q.H.; Zheng, H.C.; Qin, L.P. Composition of supercritical fluid extracts of some Xanthium species from China. Chem. Nat. Compd. 2008, 6, 814–816. [Google Scholar] [CrossRef]
- Winters, T.E.; Theodore, A.; Geissman, D.S. Sesquiterpene lactones of Xanthium species. Xanthanol and isoxanthanol, and correlation of xanthinin with ivalbin. J. Org. Chem. 1969, 34, 153–155. [Google Scholar] [CrossRef]
- McMillan, C.; Chavez, P.I.; Mabry, T.J. Sesquiterpene lactones of Xanthium strumarium in a texas population and in experimental hybrids. Biochem. Syst. Ecol. 1975, 3, 137–141. [Google Scholar] [CrossRef]
- Ahn, J.W.; No, Z.; Ryu, S.Y.; Zee, O.P. Isolation of cytotoxic compounds from the leaves of Xanthium strumarium L. Nat. Prod. Sci. 1995, 1, 1–4. [Google Scholar]
- Karmakar, U.K.; Ishikawa, N.; Toume, K.; Arai, M.A.; Sadhu, S.K.; Ahmed, F.; Ishibashi, M. Sesquiterpenes with TRAIL-resistance overcoming activity from Xanthium strumarium. Bioorg. Med. Chem. 2015, 23, 4746–4754. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.S.; Li, L.; Liu, Y.B.; Ma, S.G.; Li, Y.; Qu, J.; Liu, Q.; Shen, Z.F.; Chen, X.G.; Yu, S.S. A new thiophene and two new monoterpenoids from Xanthium sibiricum. J. Asian Nat. Prod. Res. 2015, 17, 1039–1047. [Google Scholar] [CrossRef] [PubMed]
- Malik, M.S.; Sangwan, N.K.; Dhindsa, K.S. Xanthanolides from Xanthium strumarium. Phytochemistry 1992, 32, 206–207. [Google Scholar] [CrossRef]
- Hu, D.Y.; Yang, S.Y.; Yuan, C.S.; Han, G.T.; Shen, H.M. Isolation and identification of chemical constituents in Xanthium sibiricum. Chin. Tradit. Herbal Drugs 2012, 43, 640–644. (In Chinese) [Google Scholar]
- Mahmoud, A.A. Xanthanolides and xanthane epoxide derivatives from Xanthium strumarium. Planta Med. 1998, 64, 724–727. [Google Scholar] [CrossRef] [PubMed]
- Saxena, V.K.; Mondal, S.K. A xanthanolide from Xanthium strumarium. Phytochemistry 1994, 35, 1080–1082. [Google Scholar] [CrossRef]
- Chen, J.; Wang, R.; Shi, Y.P. Chemical constituents from Xanthii Fructus. Chin. Tradit. Herbal Drugs 2013, 44, 1717–1720. (In Chinese) [Google Scholar]
- Wang, L.; Wang, J.; Li, F.; Liu, X.; Chen, B.; Tang, Y.X.; Wang, M.K. Cytotoxic sesquiterpene lactones from aerial parts of Xanthium sibiricum. Planta Med. 2013, 79, 661–665. [Google Scholar] [CrossRef]
- Jiang, H.; Yang, L.; Xing, X.D.; Yan, M.L.; Guo, X.Y.; Su, X.L.; Sun, Y.P.; Yang, B.Y.; Wang, Q.H.; Kuang, H.X. Chemical constituents of terpenoids from Xanthium strumarium. Chin. Tradit. Pat. Med. 2018, 40, 2461–2466. [Google Scholar]
- Cui, W.P. Chemical Constituents from Three Medicinal Plants and Their Bioactivities. Ph.D. Thesis, East China Normal University, Shanghai, China, 2013. (In Chinese). [Google Scholar]
- Ingawale, A.S.; Sadiq, M.B.; Nguyen, L.T.; Ngan, T.B. Optimization of extraction conditions and assessment of antioxidant, α-glucosidase inhibitory and antimicrobial activities of Xanthium strumarium L. fruits. Biocatal. Agric. Biotechnol. 2018, 14, 40–47. [Google Scholar] [CrossRef]
- Wahab, A.; Sultana, A.; Khan, K.M.; Irshad, A.; Ambreen, N.; Ali, M.; Bilal, M. Chemical investigation of Xanthium strumarium Linn and biological activity of its different fractions. J. Pharm. Res. 2012, 5, 1984–1987. [Google Scholar]
- Li, N.; Zhang, W.Z. Studies on Chemical Constituents of Xanthium sibiricum Patrin ex Widder. J. Qiqihar Univ. 2016, 32, 51–53. (In Chinese) [Google Scholar]
- Sultana, A. Phytochemical Studies on the Chemical Constituents of Xanthium strumarium Linn., Synthesis in addition Bioactivities of 2, 3-Diaminonaphthalenimidazole Derivatives and Amides of Piperic Acid. Ph.D. Thesis, Federal Urdu University of Arts, Science and Technology, Karachi, Pakistan, 2014. [Google Scholar]
- Kaur, M.; Kamboj, A.; Rathour, A.; Saluja, A.K. Isolation and Characterization of Constituents from the Leaves of Xanthium strumarium and their Evaluation for Antioxidant and Antimicrobial Potential. Nat. Prod. Chem. Res. 2015, 3, 168–173. [Google Scholar] [CrossRef]
- Agata, I.; Goto, S.; Hatano, T.; Nishibe, S.; Okuda, T. 1, 3, 5-tri-O-caffeoylquinic acid from Xanthium strumarium. Phytochemistry 1993, 33, 508–509. [Google Scholar] [CrossRef]
- Hwang, S.H.; Wang, Z.Q.; Yoon, H.N.; Lim, S.S. Xanthium strumarium as an Inhibitor of α-Glucosidase, Protein Tyrosine Phosphatase 1β, Protein Glycation and ABTS+ for Diabetic and Its Complication. Molecules 2016, 21, 1241. [Google Scholar] [CrossRef]
- Han, T.; Li, H.L.; Hu, Y.; Zhang, Q.Y.; Huang, B.K.; Zheng, H.C.; Rahman, K.; Qin, L.P. Phenolic acids in Fructus Xanthii and determination of contents of total phenolic acids in different species and populations of Xanthium in China. J. Chin. Intergr. Med. 2006, 4, 194–198. (In Chinese) [Google Scholar] [CrossRef]
- Tian, J.; Xia, Y.F.; Fang, K.H. Simultaneous determination of eight phenolic acids in Xanthium sibiricum by HPLC. Chin. Tradit. Pat. Med. 2013, 36, 1623–1626. (In Chinese) [Google Scholar]
- Yuan, H.E. Study on the Chemical Constituents of Herba Commelinae and Fructus Xanthii. Master’s Thesis, Jinan University, Guangzhou, China, 2014. (In Chinese). [Google Scholar]
- Cheng, Z.; Wang, L.; Chen, B.; Li, F.; Wang, M.K. Chemical Constituents from Fructus Xanthii. Chin. J. Appl. Environ. Biol. 2011, 17, 350–352. (In Chinese) [Google Scholar] [CrossRef]
- Kan, S.Q.; Chen, G.Y.; Han, C.R.; Chen, Z.; Song, X.M.; Ren, M.; Jiang, H. Chemical constituents from the roots of Xanthium sibiricum. Nat. Prod. Res. 2011, 25, 1243–1249. [Google Scholar] [CrossRef]
- Jiang, H.; Yang, L.; Ma, G.X.; Xing, X.D.; Yan, M.L.; Zhang, Y.Y.; Wang, Q.H.; Yang, B.Y.; Kuang, H.X.; Xu, X.D. New phenylpropanoid derivatives from the fruits of Xanthium sibiricum and their anti-inflammatory activity. Fitoterapia 2017, 117, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Yang, L.; Liu, C.; Hou, H.; Wang, Q.; Wang, Z.; Yang, B.; Kuang, H. Four new glycosides from the fruit of Xanthium sibiricum Patr. Molecules 2013, 18, 12464–12473. [Google Scholar] [CrossRef] [PubMed]
- Yin, R.H.; Bai, X.; Feng, T.; Dong, Z.J.; Li, Z.H.; Liu, J.K. Two new compounds from Xanthium strumarium. J. Asian Nat. Prod. Res. 2016, 18, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Han, T.; Li, H.L.; Zhang, Q.Y.; Zheng, H.C.; Qin, L.P. New thiazinediones and other components from Xanthium strumarium. Chem. Nat. Compd. 2006, 42, 567–570. [Google Scholar] [CrossRef]
- Pandey, D.P.; Rather, M.A. Isolation and Identification of Phytochemicals from Xanthium strumarium. Int. J. ChemTech Res. 2012, 4, 266–271. [Google Scholar]
- Jiang, H.; Yang, L.; Xing, X.D.; Zhang, Y.Y.; Yan, M.L.; Yang, B.Y.; Wang, Q.H.; Kuang, H.X. Chemical constituents from fruits of Xanthium sibiricum. Chin. Tradit. Herbal Drugs 2017, 48, 47–51. (In Chinese) [Google Scholar]
- Qiu, Y.L.; Dai, Y.H.; Wang, D.; Cui, Z. Chemical constituents in the fruits of Xanthium sibiricum. Chin. J. Med. Chem. 2010, 20, 214–216. (In Chinese) [Google Scholar]
- Yoon, H.N.; Lee, M.Y.; Kim, J.K.; Suh, H.W.; Lim, S.S. Aldose Reductase Inhibitory Compounds from Xanthium strumarium. Arch. Pharmacal. Res. 2013, 36, 1090–1095. [Google Scholar] [CrossRef]
- Jiang, H.; Yang, L.; Xing, X.D.; Yan, M.L.; Guo, X.Y.; Su, X.L.; Sun, Y.P.; Yang, B.Y.; Wang, Q.H.; Kuang, H.X. Study on lignans from Xanthii Fructus. Chin. J. Chin. Mater. Med 2018, 43, 2097–2103. (In Chinese) [Google Scholar]
- Wang, S.X.; Ren, L.J.; Sun, Z.R.; Pei, Y.H.; Zhu, T.R. Toxic Constituents in Seeds of Xanthium mongolicum. Chin. J. Med. Chem. 1983, 14, 529–531. (In Chinese) [Google Scholar]
- Craig, J.C.; Mole, M.L.; Billets, S.; El-Feraly, F. Isolation and identification of the hypoglycemic agent, carboxyatracrylate from Xanthium strumarium. Phytochemistry 1976, 15, 1178. [Google Scholar] [CrossRef]
- Jiang, H.; Zhang, Y.Y.; Zhang, Y.; Yang, L.; Wang, Q.H.; Kuang, H.X. Isolation and Identification of Chemical Constituents from the Fruit of Xanthium Sibiricum Patr. Inf. Tradit. Chin. Med. 2016, 33, 8–10. (In Chinese) [Google Scholar]
- Ma, Y.T.; Huang, M.C.; Hsu, F.L.; Chang, H.F. Thiazinedione from xanthium strumarium. Phytochemistry 1998, 48, 1083–1085. [Google Scholar] [CrossRef]
- Lee, C.L.; Huang, P.C.; Hsieh, P.W.; Hwang, T.L.; Hou, Y.Y.; Chang, F.R.; Wu, Y.C. (-)-Xanthienopyran, a new inhibitor of superoxide anion generation by activated neutrophils, and further constituents of the seeds of Xanthium strumarium. Planta Med. 2008, 74, 1276–1279. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.H.; Yu, J.G.; Sun, L.; Guo, B.L.; Li, D.Y. Studies on Chemical Constituents of Xanthium sibiricum. Chin. J. Chin. Mater. Med. 2005, 30, 1027–1028. (In Chinese) [Google Scholar]
- Vasas, A.; Hohmann, J. Xanthane sesquiterpenoids: Structure, synthesis and biological activity. Nat. Prod. Rep. 2011, 28, 824–842. [Google Scholar] [CrossRef] [PubMed]
- Seaman, F.C. Sesquiterpene lactones as taxonomic characters in the asteraceae. Bot. Rev. 1982, 48, 121–594. [Google Scholar] [CrossRef]
- Hong, Y.; Han, Y.Q.; Xia, L.Z.; Gui, J.; Chen, X.; Sun, Y.H. Simultaneous Determination of Nine Phenolic Acid Components in Xanthii Fructus. Chin. Pharm. J. 2013, 13, 1109–1112. (In Chinese) [Google Scholar]
- Jiang, H.; Yang, L.; Xing, X.; Yan, M.; Guo, X.; Yang, B.; Wang, Q.; Kuang, H. HPLC-PDA Combined with Chemometrics for Quantitation of Active Components and Quality Assessment of Raw and Processed Fruits of Xanthium strumarium L. Molecules 2018, 23, 243. [Google Scholar] [CrossRef] [PubMed]
- Song, Z.Y.; Zhang, L.Y.; Xie, M.Z.; Li, Z.H.; Guo, W.W. Toxic Constituents and Pharmacological Effect of Xanthium sibiricum. Acta Pharm. Sin. 1962, 9, 678–683. (In Chinese) [Google Scholar]
- Duo, R.; Chen, Y.; Liu, Y.H.; Huang, Z.F.; Liu, Y.H.; Yi, J.H. Influence of processing on contents of carboxyatractyloside and atractyloside in Xanthii Fructus. Chin. Tradit. Pat. Med. 2013, 35, 353–356. (In Chinese) [Google Scholar]
- Hong, S.H.; Jeong, H.J.; Kim, H.M. Inhibitory effects of Xanthii Fructus extract on mast cell-mediated allergic reaction in murine model. J. Ethnopharmacol. 2003, 88, 229–234. [Google Scholar] [CrossRef]
- Hong, S.H.; Oh, M.J.; Lee, E.J.; Park, J.H.; Kim, N.H.; Rhee, H.K.; Kim, H.M.; Jung, S.K. Processed Xanthii Fructus increases cell viability of mast cell line, RBL-2H3. Orient. Pharm. Exp. Med. 2004, 4, 60–64. [Google Scholar]
- Zhao, Y.; Yang, H.; Zheng, Y.B.; Wong, Y.O.; Leung, P.C. The Effects of Fructus Xanthii Extract on Cytokine Release from Human Mast Cell Line (HMC-1) and Peripheral Blood Mononuclear Cells. Immunopharmacol. Immunotoxicol. 2008, 30, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Yan, G.H.; Jin, G.Y.; Li, G.Z.; Cui, C.A.; Quan, G.H.; Jin, D.S.; Jin, D.Z. The possible mechanism of inhibitory effect of xanthium strumarium on mast cells activated by compound 48/80. Prog. Anat. Sci. 2010, 16, 164–166. (In Chinese) [Google Scholar]
- Peng, W.; Ming, Q.L.; Han, P.; Zhang, Q.Y.; Jiang, Y.P.; Zheng, C.J.; Han, Y.; Qin, L.P. Anti-allergic rhinitis effect of caffeoylxanthiazonoside isolated from fruits of Xanthium strumarium L. in rodent animals. Phytomedicine 2014, 21, 824–829. [Google Scholar] [CrossRef]
- Tao, L.; Fan, F.T.; Liu, Y.P.; Li, W.D.; Zhang, L.; Ruan, J.S.; Shen, C.S.; Sheng, X.B.; Zhu, Z.J.; Wang, A.Y.; et al. Concerted suppression of STAT3 and GSK3β is involved in growth inhibition of non-small cell lung cancer by Xanthatin. PLoS ONE 2013, 8, e81945. [Google Scholar] [CrossRef]
- Tao, L.; Sheng, X.; Zhang, L.; Li, W.; Wei, Z.; Zhu, P.; Zhang, F.; Wang, A.; Woodgett, J.R.; Lu, Y. Xanthatin anti-tumor cytotoxicity is mediated via glycogen synthase kinase-3β and β-catenin. Biochem. Pharmacol. 2016, 115, 18–27. [Google Scholar] [CrossRef]
- Tao, L.; Cao, Y.; Wei, Z.; Jia, Q.; Yu, S.; Zhong, J.; Wang, A.; Woodgett, J.R.; Lu, Y. Xanthatin triggers Chk1-mediated DNA damage response and destabilizes Cdc25C via lysosomal degradation in lung cancer cells. Toxicol. Appl. Pharmacol. 2017, 337, 85–94. [Google Scholar] [CrossRef]
- Kim, Y.S.; Kim, J.S.; Park, S.H.; Choi, S.U.; Lee, C.O.; Kim, S.K.; Kim, Y.K.; Kim, S.H.; Ryu, S.Y. Two cytotoxic sesquiterpene lactones from the leaves of Xanthium strumarium and their in vitro inhibitory activity on farnesyltransferase. Planta Med. 2003, 69, 375–377. [Google Scholar] [CrossRef]
- Ferrer, J.P.; Zampini, I.C.; Cuello, A.S.; Francisco, M.; Romero, A.; Valdivia, D.; Gonzalez, M.; Carlos, S.; Lamar, A.S.; Isla, M.I. Cytotoxic Compounds from Aerial Organs of Xanthium strumarium. Nat. Prod. Commun. 2016, 11, 371–374. [Google Scholar] [PubMed]
- Ramírez-Erosa, I.; Huang, Y.; Hickie, R.A.; Sutherland, R.G.; Barl, B. Xanthatin and xanthinosin from the burs of Xanthium strumarium L. as potential anticancer agents. Can. J. Physiol. Pharmacol. 2007, 85, 1160–1172. [Google Scholar] [CrossRef] [PubMed]
- Takeda, S.; Matsuo, K.; Yaji, K.; Okajima-Miyazaki, S.; Harada, M.; Miyoshi, H.; Okamoto, Y.; Amamoto, T.; Shindo, M.; Omiecinski, C.J.; et al. (-)-Xanthatin selectively induces GADD45γ and stimulates caspase-independent cell death in human breast cancer MDA-MB-231 cells. Chem. Res. Toxicol. 2011, 24, 855–865. [Google Scholar] [CrossRef] [PubMed]
- Takeda, S.; Noguchi, M.; Matsuo, K.; Yamaguchi, Y.; Kudo, T.; Nishimura, H.; Okamoto, Y.; Amamoto, T.; Shindo, M.; Omiecinski, C.J.; et al. (-)-Xanthatin up-regulation of the GADD45γ tumor suppressor gene in MDA-MB-231 breast cancer cells: Role of topoisomerase IIα inhibition and reactive oxygen species. Toxicology 2013, 305, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Takeda, S.; Nishimura, H.; Koyachi, K.; Matsumoto, K.; Yoshida, K.; Okamoto, Y.; Amamoto, T.; Shindo, M.; Aramaki, H. (-)-Xanthatin induces the prolonged expression of c-Fos through an N-acetyl-l-cysteine (NAC)-sensitive mechanism in human breast cancer MDA-MB-231 cells. J. Toxicol. Sci. 2013, 38, 547–557. [Google Scholar] [CrossRef] [PubMed]
- Vaishnav, K.; George, L.B.; Highland, H.N. Induction of cell death through alteration of antioxidant activity in HeLa cervical cancer cells by Xanthium strumarium L. extract. IOSR J. Pharm. Biol. Sci. 2015, 10, 33–42. [Google Scholar]
- Liu, R.; Shi, D.; Zhang, J.; Li, X.; Han, X.; Yao, X.; Fang, J. Xanthatin Promotes Apoptosis via Inhibiting Thioredoxin Reductase and Eliciting Oxidative Stress. Mol. Pharm. 2018, 15, 3285–3296. [Google Scholar] [CrossRef]
- Bui, V.B.; Liu, S.T.; Zhu, J.J.; Xiong, J.; Zhao, Y.; Yang, G.X.; Xia, G.; Hu, J.F. Sesquiterpene lactones from the aerial parts of Xanthium sibiricum and their cytotoxic effects on human cancer cell lines. Phytochem. Lett. 2012, 5, 685–689. [Google Scholar] [CrossRef]
- Zhang, L.; Tao, L.; Ruan, J.; Li, W.; Wu, Y.; Yan, L.; Zhang, F.; Fan, F.; Zheng, S.; Wang, A.; et al. Xanthatin induces G2/M cell cycle arrest and apoptosis in human gastric carcinoma MKN-45 cells. Planta Med. 2012, 78, 890–895. [Google Scholar] [CrossRef]
- Jiang, H.; Ma, G.X.; Yang, L.; Xing, X.D.; Yan, M.L.; Zhang, Y.Y.; Wang, Q.H.; Kuang, H.X.; Xu, X.D. Rearranged ent-kauranoid glycosides from the fruits of Xanthium strumarium and their antiproliferative activity. Phytochem. Lett. 2016, 18, 192–196. [Google Scholar] [CrossRef]
- Al-Mekhlafi, F.A.; Abutaha, N.; Mashaly, A.M.A.; Nasr, F.A.; Ibrahim, K.E.; Wadaan, M.A. Biological activity of Xanthium strumarium seed extracts on different cancer cell lines and Aedes caspius, Culex pipiens (Diptera: Culicidae). Saudi, J. Biol. Sci. 2017, 24, 817–821. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Min, Y.S.; Park, K.C.; Kim, D.S. Inhibition of melanogenesis by Xanthium strumarium L. Biosci. Biotechnol. Biochem. 2012, 76, 767–771. [Google Scholar] [CrossRef] [PubMed]
- Li, W.D.; Wu, Y.; Zhang, L.; Yan, L.G.; Yin, F.Z.; Ruan, J.S.; Chen, Z.P.; Yang, G.M.; Yan, C.P.; Zhao, D.; et al. Characterization of xanthatin: Anticancer properties and mechanisms of inhibited murine melanoma in vitro and in vivo. Phytomedicine 2013, 20, 865–873. [Google Scholar] [CrossRef] [PubMed]
- Roussakis, C.; Chinou, I.; Vayas, C.; Harvala, C.; Verbist, J.F. Cytotoxic activity of xanthatin and the crude extracts of Xanthium strumarium. Planta Med. 1994, 60, 473–474. [Google Scholar] [CrossRef] [PubMed]
- Nibret, E.; Youns, M.; Krauth-Siegel, R.L.; Wink, M. Biological activities of xanthatin from Xanthium strumarium leaves. Phytother. Res. 2011, 25, 1883–1890. [Google Scholar] [CrossRef] [PubMed]
- Pan, J.H.; Wang, Y.L.; Xie, M.R.; Yu, F.R. Inhibitory effect of xanthium extract on S180 cells growth and the impact on immune functions in tumor-bearing mice. Chin. J. Clin. Res. 2013, 26, 317–319. (In Chinese) [Google Scholar]
- Ishwarya, S.; Singh, M.K. Evaluation of antioxidant and invitro cytotoxicity of crude fractions from the roots of Xanthiuim strumarium. Int. J. Pharmtech Res. 2010, 2, 2219–2223. [Google Scholar]
- An, H.J.; Jeong, H.J.; Lee, E.H.; Kim, Y.K.; Hwang, W.J.; Yoo, S.J. Xanthii Fructus Inhibits Inflammatory Responses in LPS-Stimulated Mouse Peritoneal Macrophages. Inflammation 2004, 28, 263–270. [Google Scholar] [CrossRef]
- Kim, I.T.; Park, Y.M.; Won, J.H.; Jung, H.J.; Park, H.J.; Choi, J.W.; Lee, K.T. Methanol extract of Xanthium strumarium L. possesses anti-inflammatory and anti-nociceptive activities. Biol. Pharm. Bull. 2005, 28, 94–100. [Google Scholar] [CrossRef]
- Yoon, J.H.; Lim, H.J.; Lee, H.J.; Kim, H.D.; Jeon, R.; Ryu, J.H. Inhibition of lipopolysaccharide-induced inducible nitric oxide synthase and cyclooxygenase-2 expression by xanthanolides isolated from Xanthium strumarium. Bioorg. Med. Chem. Lett. 2008, 18, 2179–2182. [Google Scholar] [CrossRef]
- Khuda, F.; Iqbal, Z.; Khan, A.; Shah, Z.Y.; Ahmad, L.; Nasir, F.; Hassan, M.; Shah, I.; Shah, W.A. Evaluation of anti-inflammatory activity of selected medicinal plants of Khyber Pakhtunkhwa, Pakistan. Pak. J. Pharm. Sci. 2014, 27, 365–368. [Google Scholar] [PubMed]
- Ju, A.; Cho, Y.C.; Cho, S. Methanol extracts of Xanthium sibiricum roots inhibit inflammatory responses via the inhibition of nuclear factor-κB (NF-κB) and signal transducer and activator of transcription 3 (STAT3) in murine macrophages. J. Ethnopharmacol. 2015, 174, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Yeom, M.; Kim, J.H.; Min, J.H.; Hwang, M.K.; Jung, H.S.; Sohn, Y. Xanthii Fructus inhibits inflammatory responses in LPS-stimulated RAW 264.7 macrophages through suppressing NF-κB and JNK/p38 MAPK. J. Ethnopharmacol. 2015, 176, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Hossen, M.J.; Kim, M.Y.; Cho, J.Y. MAPK/AP-1-Targeted Anti-Inflammatory Activities of Xanthium strumarium. Am. J. Chin. Med. 2016, 44, 1111–1125. [Google Scholar] [CrossRef] [PubMed]
- Hossen, M.J.; Cho, J.Y.; Kim, D. PDK1 in NF-κB signaling is a target of Xanthium strumarium methanolic extract-mediated anti-inflammatory activities. J. Ethnopharmacol. 2016, 190, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.H.; Wang, B.S.; Chiu, C.S.; Amagaya, S.; Hsieh, W.T.; Huang, S.S.; Shie, P.H.; Huang, G.J. Antioxidant, antinociceptive, and anti-inflammatory activities of Xanthii Fructus extract. J. Ethnopharmacol. 2011, 135, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Han, T.; Li, H.L.; Zhang, Q.Y.; Han, P.; Zheng, H.C.; Rahman, K.; Qin, L.P. Bioactivity-guided fractionation for anti-inflammatory and analgesic properties and constituents of Xanthium strumarium L. Phytomedicine 2007, 14, 825–829. [Google Scholar] [CrossRef]
- Park, J.H.; Kim, M.S.; Jeong, G.S.; Yoon, J. Xanthii Fructus extract inhibits TNF-α/IFN-γ-induced Th2-chemokines production via blockade of NF-κB, STAT1 and p38-MAPK activation in human epidermal keratinocytes. J. Ethnopharmacol. 2015, 171, 85–93. [Google Scholar] [CrossRef]
- Hasan, T.; Das, B.K.; Qibria, T.; Morshed, M.A.; Uddin, M.A. Phytochemical Screening and Evaluation of Analgesic Activity of Xanthium Srtumarium L. Asian. J. Biochem. Pharm. Res. 2011, 1, 2231–2560. [Google Scholar]
- Talakal, T.S.; Dwivedi, S.K.; Sharma, S.R. In vitro and in vivo antitrypanosomal activity of Xanthium strumarium leaves. J. Ethnopharmacol. 1995, 49, 141–145. [Google Scholar] [CrossRef]
- Gökçe, A.; Isaacs, R.; Whalon, M.E. Ovicidal, larvicidal and anti-ovipositional activities of Bifora radians and other plant extracts on the grape berry moth Paralobesia viteana (Clemens). J. Pest. Sci. 2011, 84, 487–493. [Google Scholar] [CrossRef]
- Chandel, S.; Bagai, U. Screening of Cytotoxicity and Antiplasmodial Activity of Xanthium strumarium L. Res. J. Pharm. Biol. Chem. Sci. 2012, 3, 625–631. [Google Scholar]
- Roy, B.; Amin, M.R.; Jalal, S.; Kwon, Y.J.; Suh, S.J. Evaluation of common cocklebur Xanthium strumarium leaf extract as post-harvest grain protectant of black gram against pulse beetle Callosobruchus chinensis (Coleoptera: Bruchidae) and isolation of crude compound. Entomol. Res. 2014, 44, 254–261. [Google Scholar] [CrossRef]
- Kepenekci, I.; Saglam, H.D. Extracts of some indigenous plants affecting hatching and mortality in the root-knot nematode [Meloidogyne javanica (Treub) Chitwood]. Egypt. J. Pest Control 2015, 25, 39–44. [Google Scholar]
- Kumar, K.K.S.; Rajkapoor, B. Effect of Xanthium strumarium L. Extracts on Antioxidant Enzymes Levels in Rat Brain after Induction of Epilepsy. Pharmacologyonline 2010, 2, 883–888. [Google Scholar]
- Narendiran, S.; Mohanambal, E.; Kumar, P.S.; Shankar, M.; Kuttimani, T.; Vijayakumar, B. Study of anti-diabetic and anti-oxidant activities of methanolic extract of Xanthium strumarium (Linn.) stems on diabetic rats. J. Pharm. Res. 2011, 4, 3728–3732. [Google Scholar]
- Sridharamurthy, N.B.; Yogananda, R.; Srinivas, U. In-vitro Antioxidant and Antilipidemic Activities of Xanthium strumarium L. Curr. Trends Biotechnol. Pharm. 2011, 5, 1362–1371. [Google Scholar]
- Kamboj, A.; Atri, P.; Saluja, A.K. Phytochemical Screening, In-vitro Evaluation of Antioxidant and Free Radical Scavenging Activity of Leaves, Stems and Roots of Xanthium strumarium L., (Compositae). Br. J. Pharm. Res. 2014, 4, 1–22. [Google Scholar] [CrossRef]
- Ghahari1, S.; Alinezhad, H.; Nematzadeh, G.A.; Tajbakhsh, M.; Baharfar, R. Biochemical Composition, Antioxidant and Biological Activities of the Essential Oil and Fruit Extract of Xanthium strumarium Linn. From Northern Iran. J. Agric. Sci. Technol. 2017, 19, 1603–1616. [Google Scholar]
- Mehta, P.; Chopra, S.; Mehta, A. Antimicrobial properties of some plant extracts against bacteria. Folia Microbiol. 1983, 28, 467–469. [Google Scholar] [CrossRef]
- Sato, Y.; Oketani, H.; Yamada, T.; Singyouchi, K.; Ohtsubo, T.; Kihara, M.; Shibata, H.; Higuti, T. A xanthanolide with potent antibacterial activity against methicillin-resistant Staphylococcus aureus. J. Pharm. Pharmacol. 1997, 49, 1042–1044. [Google Scholar] [CrossRef] [PubMed]
- Srinivas, P.; Rajashekar, V. Phytochemical Screening and in vitro Antimicrobial Investigation of the Methanolic Extract of Xanthium strumarium Leaf. Int. J. Drug Dev. Res. 2011, 3, 286–293. [Google Scholar]
- Chen, W.H.; Liu, W.J.; Wang, Y.; Song, X.P.; Chen, G.Y. A new naphthoquinone and other antibacterial constituents from the roots of Xanthium sibiricum. Nat. Prod. Res. 2015, 29, 739–744. [Google Scholar] [CrossRef] [PubMed]
- Devkota, A.; Das, R.K. Antibacterial activities of Xanthium strumarium L. J. Nat. Hist. Mus. 2015, 29, 70–77. [Google Scholar] [CrossRef]
- Sharifi-Rad, J.; Hoseini-Alfatemi, S.M.; Sharifi-Rad, M.; Sharifi-Rad, M.; Iriti, M.; Sharifi-Rad, M.; Sharifi-Rad, R.; Raeisi, S. Phytochemical compositions and biological activities of essential oil from Xanthium strumarium L. Molecules 2015, 20, 7034–7047. [Google Scholar] [CrossRef] [PubMed]
- Sharifi-Rad, J.; Soufi, L.; Ayatollahi, S.A.; Iriti, M.; Sharifi-Rad, M.; Varoni, E.M.; Shahri, F.; Esposito, S.; Kuhestani, K.; Sharifi-Rad, M. Anti-bacterial effect of essential oil from Xanthium strumarium against shiga toxin-producing Escherichia coli. Cell. Mol. Biol. 2016, 62, 69–74. [Google Scholar] [PubMed]
- Wang, W.; Jiang, H.; Zhiwei, W.U.; Qian, J.; Wang, X.; Jinxiu, X.U. Study on the bacteriostatic effects of 7 kinds of chinese herbal medicines such as ophiopogon japonicus and comb. Agric. Sci. Technol. 2016, 17, 2560. [Google Scholar]
- Kim, D.K.; Shim, C.K.; Bae, D.W.; Kawk, Y.S.; Yang, M.S.; Kim, H.K. Identification and Biological Characteristics of an Antifungal Compound Extracted from Cocklebur (Xanthium strumarium) against Phytophthora drechsleri. Plant Pathol. J. 2002, 18, 288–292. [Google Scholar] [CrossRef]
- Yanar, Y.; Kadioğlu, L.; Gökçe, A.; Demirtaş, D.; Gören, N.; Çam, H.; Whalon, M. In vitro antifungal activities of 26 plant extracts on mycelial growth of Phytophthora infestans (Mont.) de Bary. Afr. J. Biotechnol. 2011, 10, 2625–2629. [Google Scholar]
- Parveen, Z.; Mazhar, S.; Siddique, S.; Manzoor, A.; Ali, Z. Chemical Composition and Antifungal Activity of Essential Oil from Xanthium strumarium L. Leaves. Indian J. Pharm. Sci. 2017, 79, 316–321. [Google Scholar] [CrossRef]
- Kupiecki, F.P.; Ogzewalla, C.D.; Schell, F.M. Isolation and characterization of a hypoglycemic agent from Xanthium strumarium. J. Pharm. Sci. 1974, 63, 1166–1167. [Google Scholar] [CrossRef] [PubMed]
- Hsu, F.L.; Chen, Y.C.; Cheng, J.T. Caffeic acid as active principle from the fruit of Xanthium strumarium to lower plasma glucose in diabetic rats. Planta Med. 2000, 66, 228–230. [Google Scholar] [CrossRef]
- Khuda, F.; Iqbal, Z.; Khan, A.; Zakiullah; Shah, Y.; Khan, A. Report: Screening of selected medicinal plants for their enzyme inhibitory potential—A validation of their ethnopharmacological uses. Pak. J. Pharm. Sci. 2014, 27, 593–596. [Google Scholar] [PubMed]
- Li, X.M.; Yang, M.X.; Li, Z.P.; Xue, M.; ShangGuan, Z.S.; Ou, Z.M.; Liu, M.; Liu, S.H.; Yang, S.Y.; Li, X.J. Fructus xanthii improves lipid homeostasis in the epididymal adipose tissue of rats fed a high-fat diet. Mol. Med. Rep. 2016, 13, 787–795. [Google Scholar] [CrossRef] [PubMed]
- Li, T.X.; Shen, J.Y.; Li, M.; Wang, G.R. Effects of Fructus Xanthii on Blood Glucose and Lipid in Diabetic Mice before and after Processing. Lishizhen Med. Mater. Med. Res. 2017, 28, 608–609. (In Chinese) [Google Scholar]
- Liu, Y.; Wu, Z.M.; Lan, P. Experimental Study on Effect of Fructus Xanthii Extract on Duck Hepatitis B Virus. Lishizhen Med. Mater. Med. Res. 2009, 20, 1776–1777. (In Chinese) [Google Scholar]
- Wang, Y.H.; Li, T.H.; Wu, B.Q.; Liu, H.; Shi, Y.F.; Feng, D.Y. Protective effects of caffeoylxanthiazonoside isolated from fruits of Xanthium strumarium on sepsis mice. Pharm. Biol. 2015, 53, 1367–1371. [Google Scholar] [CrossRef] [PubMed]
- Li, X.M.; Li, Z.P.; Xue, M.; Ou, Z.M.; Liu, M.; Yang, M.X.; Liu, S.H.; Yang, S.Y.; Li, X.J. Fructus Xanthii Attenuates Hepatic Steatosis in Rats Fed on High-Fat Diet. PLoS ONE 2013, 8, e61499. [Google Scholar] [CrossRef]
- Lin, B.; Zhao, Y.; Han, P.; Yue, W.; Ma, X.Q.; Rahman, K.; Zheng, C.J.; Qin, L.P.; Han, T. Anti-arthritic activity of xanthium strumarium L. extract on complete freund’s adjuvant induced arthritis in rats. J. Ethnopharmacol. 2014, 155, 248–255. [Google Scholar] [CrossRef]
- Afsar, S.K.; Kumar, K.R.; Raveesha, P.; Sree, K. Evaluation of Anti-pyretic Activity of Methanolic Whole Plant Extract of Xanthium strumarium Against Yeast Induced Pyrexia Model in Wistar Rats. J. Pharm. Res. 2012, 5, 5277–5279. [Google Scholar]
- Kumar, K.K.S.; Rajkapoor, B. Evaluation of Anti-epileptic Activity of Xanthium strumarium L. Pharmacologyonline 2010, 2, 850–855. [Google Scholar]
- Panigrahi, P.N.; Dey, S.; Sahoo, M.; Choudhary, S.S.; Mahajan, S. Alteration in oxidative/nitrosative imbalance, histochemical expression of osteopontin and antiurolithiatic efficacy of xanthium strumarium (L.) in ethylene glycol induced urolithiasis. Biomed. Pharmacother. 2016, 84, 1524–1532. [Google Scholar] [CrossRef] [PubMed]
- Kandhare, A.D.; Kumar, V.S.; Adil, M.; Rajmane, A.R.; Ghosh, P.; Bodhankar, S.L. Investigation of gastro protective activity of Xanthium strumarium L. by modulation of cellular and biochemical marker. Orient. Pharm. Exp. Med. 2012, 12, 287–299. [Google Scholar] [CrossRef]
- Yang, B.; Wang, F.; Cao, H.; Liu, G.; Zhang, Y.; Yan, P.; Li, B. Caffeoylxanthiazonoside exerts cardioprotective effects during chronic heart failure via inhibition of inflammatory responses in cardiac cells. Exp. Ther. Med. 2017, 14, 4224–4230. [Google Scholar] [CrossRef] [PubMed]
- Yan, C.P.; Li, H.; Wu, Y.; Xie, D.H.; Weng, Z.B.; Cai, B.C.; Liu, X.; Li, W.D.; Chen, Z.P. Determination of xanthatin by ultra high performance liquid chromatography coupled with triple quadrupole mass spectrometry: Application to pharmacokinetic study of xanthatin in rat plasma. J. Chromatogr. B 2014, 974–978, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.L. The Detection of atractyIoside in Fructus Xanthii and the Pharmacokinetic of Atractyloside in Rat. Master’s Thesis, Guangzhou University of Chinese Medicine, Guangzhou, China, 2013. (In Chinese). [Google Scholar]
- Shen, J.Y. Comparative Study of Pharmacodynamics and Pharmacokinetics before and after Processing Xanthii Fructus. Master’s Thesis, Hubei University of Traditional Chinese Medicine, Wuhan, China, 2016. (In Chinese). [Google Scholar]
- Witte, S.T.; Osweiler, G.D.; Stahr, H.M.; Mobley, G. Cocklebur toxicosis in cattle associated with the consumption of mature Xanthium strumarium. J. Vet. Diagn. Investig. 1990, 2, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Wang, J.X.; Zhang, L.; Huang, J.K.; Yang, X.H. Comprehensive evaluation and risk control measures of Xanthii Fructus. Chin. J. Chin. Mater. Med. 2017, 42, 4079–4085. (In Chinese) [Google Scholar]
- Li, J.; Gao, T.; Xie, Z.Q.; Tang, Y. The Toxicity Comparison Experiment of the Extractions from Fructus Xanthii. Lishizhen Med. Mater. Med. Res. 2005, 16, 484–487. (In Chinese) [Google Scholar]
- Yan, L.C.; Zhang, T.T.; Zhao, J.N.; Song, J.; Hua, H.; Li, L. Comparative study on acute toxicity of four extracts from Xanthii Fructus in mice. Chin. J. Chin. Mater. Med. 2012, 37, 2228–2231. (In Chinese) [Google Scholar]
- Fu, S.; Guan, J.H. Experimental Study on the Toxicity and Efficacy of Siegesbeckiae and Cocklebur. World J. Integr. Tradit. West. Med. 2015, 10, 493–496. (In Chinese) [Google Scholar]
- Stuart, B.P.; Cole, R.J.; Gosser, H.S. Cocklebur (xanthium strumarium L. var. strumarium) intoxication in swine: Review and redefinition of the toxic principle. Vet. Pathol. 1981, 18, 368–383. [Google Scholar]
- Wang, Y.; Han, T.; Xue, L.M.; Han, P.; Zhang, Q.Y.; Huang, B.K.; Zhang, H.; Ming, Q.L.; Peng, W.; Qin, L.P. Hepatotoxicity of kaurene glycosides from Xanthium strumarium L. fruits in mice. Die Pharm. 2011, 66, 445–449. [Google Scholar]
- Stewart, M.J.; Steenkamp, V. The Biochemistry and Toxicity of Atractyloside: A Review. Ther. Drug Monit. 2000, 22, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Liu, S.M.; Liu, Y.; Mou, H. Toxic effects of ethylacetate, n-butanol, and water extracts from alcohol extractions of cocklebur fruit on liver in rats. Advers. Drug React. J. 2010, 12, 17–20. (In Chinese) [Google Scholar]
- Cao, M.; Wu, B.; Ma, D.; Bai, Y.; Liu, S.M. Metabolomics study on Fructus Xanthii-induced hepatotoxicity in rats. Advers. Drug React. J. 2011, 13, 287–293. (In Chinese) [Google Scholar]
- Xue, L.M.; Zhang, Q.Y.; Han, P.; Jiang, Y.P.; Yan, R.D.; Wang, Y.; Rahman, K.; Jia, M.; Han, T.; Qin, L.P. Hepatotoxic constituents and toxicological mechanism of Xanthium strumarium L. fruits. J. Ethnopharmacol. 2014, 152, 272–282. [Google Scholar] [CrossRef] [PubMed]
- Zeng, J.; Tang, S.W.; Liu, Y.H.; Wang, Y.Q.; Hua, Y.; Zhao, J.N. Experimental Study on Liver Toxicity of Raw and Stir-fried Xanthium sibiricum Based on Sensitive Biomarkers. Pharm. Clin. Chin. Mater. Med. 2018, 34, 122–125. (In Chinese) [Google Scholar]
- Mandal, S.C.; Dhara, A.K.; Kumar, C.K.A.; Maiti, B.C. Neuropharmacological Activity of Xanthium Strumarium Linn. Extract. J. Herbs Spices Med. Plants 2001, 8, 69–77. [Google Scholar] [CrossRef]
- Yin, J.; Li, D.; Hu, W.; Meng, Q. Effects of glycyrrhizic acid on cocklebur-induced hepatotoxicity in rat and human hepatocytes. Phytother. Res. 2008, 22, 395–400. [Google Scholar] [CrossRef]
- Yu, J.; Song, M.Z.; Wang, J.; Li, Y.F.; Lin, P.; Que, L.; Bao, Z. In vitro cytotoxicity and in vivo acute and chronic toxicity of Xanthii Fructus and its processed product. Biomed. Res. Int. 2013, 2013, 1–12. [Google Scholar]
- Piloto Ferrer, J.; Cozzi, R.; Cornetta, T.; Stano, P.; Fiore, M.; Degrassi, F.; De Salvia, R.; Remigio, A.; Francisco, M.; Quiñones, O.; et al. Xanthium strumarium L. Extracts Produce DNA Damage Mediated by Cytotoxicity in In vitro Assays but Does Not Induce Micronucleus in Mice. Biomed. Res. Int. 2014, 2014, 575197. [Google Scholar] [CrossRef] [PubMed]
- Su, T.; Cheng, B.C.; Fu, X.Q.; Li, T.; Guo, H.; Cao, H.H.; Kwan, H.Y.; Tse, A.K.W.; Yu, H.; Cao, H.; et al. Comparison of the toxicities, bioactivities and chemical profiles of raw and processed Xanthii Fructus. BMC Complement. Altern. Med. 2016, 16, 24. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.Q.; Hou, H.R.; Liu, K.C.; Wang, X.M.; Peng, W.B.; Han, L.W.; Wang, X.; Chen, W.Y. Toxicity of Fructus Xanthii extract to the growth and motion behavior of zebrafish embryos. Shandong SCI 2014, 27, 10–13. (In Chinese) [Google Scholar]













| Preparation Name | Main Compositions | Traditional and Clinical Uses | References |
|---|---|---|---|
| Li Bi Tablets | Xanthii Fructus, Scutellariae Radix, Magno1iae Flos, Menthae Haplocalycis Herba, Angelicae Dahuricae Radix, Asari Radix Et Rhizoma, Taraxaci Herba | Curing common cold with nasal obstruction, nasosinusitis, turbid nasal discharge | “Chinese Pharmacopoeia (2010)” a |
| Shuang Xin Bi Dou Yan Ke Li | Xanthii Fructus, Magno1iae Flos, Angelicae Dahuricae Radix, Asari Radix Et Rhizoma, Lonicerae Japonicae Flos, Lonicerae Japonicae Cau1is, Taraxaci Herba, Glycyrrhizae Radix Et Rhizoma, Platycodonis Radix, Chrysanthemi Flos, Scutellariae Radix, Paeoniae Radix Rubra, Coicis Semen, Rehmanniae Radix | Treating nasosinusitis | “Guo Jia Zhong Cheng Yao Biao Zhun” b |
| Xiao Er Bi Yan Tablets | Xanthii Fructus, Ligustici Rhizoma Et Radix, Saposhnikoviae Radix, Angelicae Dahuricae Radix, Polygoni Tinctorii Folium, Taraxaci Herba, Cimicifugae Rhizoma, Glycyrrhizae Radix Et Rhizoma | Curing chronic rhinitis of child | “Zhong Yao Cheng Fang Zhi Ji”c |
| Yu Yuan Wan | Xanthii Fructus, Scutellariae Radix, Gardeniae Fructus, Scrophulariae Radix, Magno1iae Flos, Ophiopogonis Radix, Lycii Cortex, Paeoniae Radix Rubra, Forsythiae Fructus, Angelicae Dahuricae Radix, Menthae Haplocalycis Herb, Schizonepetae Herba, Glycyrrhizae Radix Et Rhizoma, Platycodonis Radix | Treating redness and swelling of the nostrils, swelling and pain in throat | “Zhong Yao Cheng Fang Zhi Ji”c |
| Yi Xuan Ning Jiao Nang | Xanthii Fructus, Chrysanthemi Flos, Arisaema Cum Bile, Scutellariae Radix, Bambusae Caulis in Taenias, Ostreae Concha, Crataegi Fructus, Citri Reticulatae Pericarpium, Paeoniae Radix Alba Poria, Lycii Fructus | Treating hyperactivity of liver-yang, vertigo due to deficiency of Qi and blood | “Xin Yao Zhuan Zheng Biao Zhun” d |
| Qing Re Zhi Ke Ke Li | Xanthii Fructus, Scutellariae Radix, Fritillariae Thunbergii Bulbus, Paridis Rhizoma, Commelinae Herba, Anemarrhenae Rhizoma, Gypsum Fibrosum, Citri Reticulatae Pericarpium, Aurantii Fructus, Armeniacae Semen Amarum, Platycodonis Radix | Curing cough, phlegm, fever, pharyngalgia, thirst, chest tightness, dry stool, yellow urine due to pulmonary retention of phlegmopyrexia; acute bronchitis, acute exacerbation of chronic bronchitis | “Xin Yao Zhuan Zheng Biao Zhun” d |
| Di Tong Bi Yan Liquid | Xanthii Fructus, Taraxaci Herba, Asari Radix Et Rhizoma, Scutellariae Radix, Ephedrae Herba, Acori Tatarinowii Rhizoma, Angelicae Dahuricae Radix, Magno1iae Flos | Curing common cold with nasal obstruction, chronic rhinitis, allergic rhinitis, nasosinusitis | “Zhong Yao Cheng Fang Zhi Ji” c |
| Di Tong Bi Yan Liquid Pen Wu Ji | Xanthii Fructus, Scutellariae Radix, Taraxaci Herba, Ephedrae Herba, Magno1iae Flos, Angelicae Dahuricae Radix, Asari Radix Et Rhizoma, Acori Tatarinowii Rhizoma | Curing common cold with nasal obstruction, chronic rhinitis, allergic rhinitis, nasosinusitis | “Xin Yao Zhuan Zheng Biao Zhun” d |
| Fu Yang Chong Ji | Xanthii Fructus, Chuanxiong Rhizoma, Carthami Flos, Kochiae Fructus | Treating pruritus, eczema, urticaria | “Zhong Yao Cheng Fang Zhi Ji” c |
| Dan Xiang Bi Yan Tablets | Xanthii Fructus, Pogostemonis Herba, Angelicae Dahuricae Radix, Centipedae Herba, Schizonepetae Herba, Lonicerae Japonicae Flos, Chrysanthemi Indici Flos | Curing chronic simple rhinitis, allergic rhinitis, acute and chronic rhinitis, and nasosinusitis | “Zhong Yao Cheng Fang Zhi Ji” c |
| Nao Ning Tablets | Xanthii Fructus, Polygonati Rhizoma, Epimedii Folium, Ophiopogonis Radix, Ginseng Radix Et Rhizoma Rubra, Polygalae Radix, Ziziphi Spinosae Semen, Schisandrae Chinensis Fructus, Lycii Fructus, Cervi Cornu Pantotrichum, Testudinis Carapax Et Plastrum, Poria, Jujubae Fructus, Rehmanniae Radix Praeparata, Cervi Cornus Colla | Curing neurasthenia, forgetfulness and insomnia, dizziness and palpitation, weariness of body, weak health and spontaneous perspiration, impotence and spermatorrhea | “Zhong Yao Cheng Fang Zhi Ji” c |
| Nao Ning Su Tablets | Xanthii Fructus, Polygonati Rhizoma, Lycii Fructus, Poria, Epimedii Folium, Polygalae Radix, Jujubae Fructus, Schisandrae Chinensis Fructus, Ziziphi Spinosae Semen, Ophiopogonis Radix, Testudinis Carapax Et Plastrum, Cervi Cornu Pantotrichum, Cervi Cornus Colla, Rehmanniae Radix Praeparata, Ginseng Radix Et Rhizoma | Curing neurasthenia, forgetfulness and insomnia, dizziness and palpitation, weariness of body, weak health and spontaneous perspiration, impotence and spermatorrhea | “Zhong Yao Cheng Fang Zhi Ji” c |
| Qin Zhi Bi Yan Tang Jiang | Xanthii Fructus, Scutellariae Radix, Angelicae Dahuricae Radix, Ephedrae Herba, Magno1iae Flos, Centipedae Herba, Menthae Haplocalycis Herba | Treating acute rhinitis | “Chinese Pharmacopoeia (2015)” a |
| Cang Yi Di Bi You | Xanthii Fructus, Angelicae Dahuricae Radix, Borneolum Syntheticum | Curing nasosinusitis, nasal obstruction and runny nose | “Zhong Yao Cheng Fang Zhi Ji”c |
| Cang Xin Qi Wu Ji | Xanthii Fructus, Magno1iae Flos, Asari Radix Et Rhizoma, Angelicae Dahuricae Radix, Coptidis Rhizoma | Curing nasal obstruction, rhinocnesmus, sneeze, allergic rhinitis, acute and chronic rhinitis | “Guo Jia Zhong Cheng Yao Biao Zhun” b |
| Xin Yi Bi Yan Pills | Xanthii Fructus, Magno1iae Flos, Menthae Haplocalycis Herba, Perillae Folium, Glycyrrhizae Radix Et Rhizoma, Pogostemonis Herba, Centipedae Herba, Isatidis Radix, Angelicae Dahuricae Radix, Saposhnikoviae Radix, Houttuyniae Herba, Chrysanthemi Flos | Treating allergic rhinitis, chronic rhinitis, nervous headache, cold and rhinorrhea, nasal obstruction | “Zhong Yao Cheng Fang Zhi Ji” c |
| Xin Qin Chong Ji | Xanthii Fructus, Asari Radix Et Rhizoma, Scutellariae Radix, Schizonepetae Herba, Saposhnikoviae Radix, Angelicae Dahuricae Radix, Astragali Radix, Atractylodis Macrocephalae Rhizoma, Cinnamomi Ramulus, Acori Tatarinowii Rhizoma | Curing allergic rhinitis due to deficiency of lung qi | “Zhong Yao Cheng Fang Zhi Ji” c |
| Xin Qin Tablets | Xanthii Fructus, Asari Radix Et Rhizoma, Scutellariae Radix, Schizonepetae Herba, Saposhnikoviae Radix, Angelicae Dahuricae Radix, Astragali Radix, Atractylodis Macrocephalae Rhizoma, Cinnamomi Ramulus | Curing allergic rhinitis, deficiency of lung qi, exogenous pathogenic wind | “Xin Yao Zhuan Zheng Biao Zhun” d |
| Xin Qin Ke Li | Xanthii Fructus, Asari Radix Et Rhizoma, Scutellariae Radix, Schizonepetae Herba, Saposhnikoviae Radix, Angelicae Dahuricae Radix, Astragali Radix, Atractylodis Macrocephalae Rhizoma, Cinnamomi Ramulus, Acori Tatarinowii Rhizoma | Curing rhinocnesmus, sneeze, rhinorrhea, cold, allergic rhinitis | “Chinese Pharmacopoeia (2010)” a |
| Tong Qiao Bi Yan Tablets | Xanthii Fructus, Saposhnikoviae Radix, Astragali Radix, Magno1iae Flos, Atractylodis Macrocephalae Rhizoma, Menthae Haplocalycis Herba | Curing nasal obstruction, rhinorrhea, rhinocnesmus, forehead headache, chronic rhinitis, allergic rhinitis, nasosinusitis | “Chinese Pharmacopoeia (2010)” a |
| Tong Qiao Bi Yan Jiao Nang | Xanthii Fructus, Saposhnikoviae Radix, Astragali Radix, Magno1iae Flos, Atractylodis Macrocephalae Rhizoma, Menthae Haplocalycis Herba | Curing nasal obstruction, rhinorrhea, rhinocnesmus, forehead headache, chronic rhinitis, allergic rhinitis, nasosinusitis | “Xin Yao Zhuan Zheng Biao Zhun” d |
| Tong Qiao Bi Yan Ke Li | Xanthii Fructus, Astragali Radix, Magno1iae Flos, Menthae Haplocalycis Herba, Saposhnikoviae Radix, Angelicae Dahuricae Radix, Atractylodis Macrocephalae Rhizoma | Curing nasal obstruction, rhinocnesmus, rhinorrhea, forehead headache, chronic rhinitis, allergic rhinitis, nasosinusitis | “Chinese Pharmacopoeia (2015)” a |
| Fang Zhi Bi Yan Tablets | Xanthii Fructus, Chrysanthemi Indici Flos, Centipedae Herba, Angelicae Dahuricae Radix, Saposhnikoviae Radix, Ecliptae Herba, Paeoniae Radix Alba, Arisaema Cum Bile, Glycyrrhizae Radix Et Rhizoma, Tribuli Fructus | Curing sneeze, nasal obstruction, headache, allergic rhinitis, nasosinusitis | “Zhong Yao Cheng Fang Zhi Ji”c |
| Bi Yan Qing Du Ji | Xanthii Fructus, Chrysanthemi Indici Flos, Paridis Rhizoma, Zanthoxyli Radix, Prunellae Spica, Gentianae Radix Et Rhizoma, Codonopsis Radix | Treating chronic inflammation of nasopharynx, swelling and pain in throat | “Zhong Yao Cheng Fang Zhi Ji”c |
| Bi Yan Qing Du Ke Li | Xanthii Fructus, Chrysanthemi Indici Flos, Paridis Rhizoma, Zanthoxyli Radix, Prunellae Spica, Gentianae Radix Et Rhizoma, Codonopsis Radix | Treating chronic inflammation of nasopharynx | “Chinese Pharmacopoeia (2015)” a |
| Bi Yuan Pills | Xanthii Fructus, Magno1iae Flos, Lonicerae Japonicae Flos, Rubiae Radix Et Rhizoma, Chrysanthemi Indici Flos | Curing nasal obstruction, nasosinusitis, ventilation lack, rhinorrhea, anosmia, headache, pain of superciliary ridge | “Chinese Pharmacopoeia (2010)” a |
| Bi Yuan He Ji | Xanthii Fructus, Magno1iae Flos, Lonicerae Japonicae Flos, Rubiae Radix Et Rhizoma, Chrysanthemi Indici Flos | Curing nasal obstruction, nasosinusitis, ventilation lack, rhinorrhea, anosmia, headache, pain of superciliary ridge | “Xin Yao Zhuan Zheng Biao Zhun” d |
| Bi Yuan Tablets | Xanthii Fructus, Magno1iae Flos, Lonicerae Japonicae Flos, Rubiae Radix Et Rhizoma, Chrysanthemi Indici Flos | Curing chronic rhinitis, nasosinusitis | “Zhong Yao Cheng Fang Zhi Ji”c |
| Bi Yuan Shu Kou Fu Ye | Xanthii Fructus, Magno1iae Flos, Menthae Haplocalycis Herba, Angelicae Dahuricae Radix, Scutellariae Radix, Gardeniae Fructus, Bupleuri Radix, Asari Radix Et Rhizoma, Chuanxiong Rhizoma, Astragali Radix, Clematidis Armandii Caulis, Platycodonis Radix, Poria | Curing rhinitis, nasosinusitis | “Chinese Pharmacopoeia (2010)” a |
| Bi Yuan Shu Jiao Nang | Xanthii Fructus, Magno1iae Flos, Menthae Haplocalycis Herba, Angelicae Dahuricae Radix, Scutellariae Radix, Gardeniae Fructus, Bupleuri Radix, Asari Radix Et Rhizoma, Chuanxiong Rhizoma, Astragali Radix, Clematidis Armandii Caulis, Platycodonis Radix, Poria | Curing rhinitis, nasosinusitis | “Chinese Pharmacopoeia (2010)” a |
| Bi Yuan Tong Qiao Ke Li | Xanthii Fructus, Magno1iae Flos, Ephedrae Herba, Angelicae Dahuricae Radix, Menthae Haplocalycis Herba, Ligustici Rhizoma Et Radix, Scutellariae Radix, Forsythiae Fructus, Chrysanthemi Indici Flos, Trichosanthis Radix, Rehmanniae Radix, Salviae Miltiorrhizae Radix Et Rhizoma, Poria, Glycyrrhizae Radix Et Rhizoma | Curing acute nasosinusitis, nasal obstruction, headache, fever | “Chinese Pharmacopoeia (2015)” a |
| Bi Yan Ling Pills | Xanthii Fructus, Magno1iae Flos, Angelicae Dahuricae Radix, Asari Radix Et Rhizoma, Scutellariae Radix, Menthae Haplocalycis Herba, Fritillariae Cirrhosae Bulbus, Sojae Semen Praeparatum | Curing nasosinusitis, nasal obstruction, chronic rhinitis | “Zhong Yao Cheng Fang Zhi Ji” c |
| Bi Yan Ling Tablets | Xanthii Fructus, Magno1iae Flos, Angelicae Dahuricae Radix, Asari Radix Et Rhizoma, Scutellariae Radix, Fritillariae Cirrhosae Bulbus, Sojae Semen Praeparatum | Treating chronic nasosinusitis, rhinitis, nasal obstruction and headache, anosmia | “Zhong Yao Cheng Fang Zhi Ji” c |
| Bi Yan Tablets | Xanthii Fructus, Magno1iae Flos, Saposhnikoviae Radix, Forsythiae Fructus, Chrysanthemi Indici Flos, Schisandrae Chinensis Fructus, Platycodonis Radix, Angelicae Dahuricae Radix, Anemarrhenae Rhizoma, Schizonepetae Herba, Glycyrrhizae Radix Et Rhizoma, Phellodendri Chinensis Cortex, Ephedrae Herba, Asari Radix Et Rhizoma | Treating acute and chronic rhinitis, nasal obstruction, rhinorrhea, fever, headache | “Chinese Pharmacopoeia (2010)” a |
| Bi Yan Tang Jiang | Xanthii Fructus, Scutellariae Radix, Angelicae Dahuricae Radix, Ephedrae Herba, Magno1iae Flos, Centipedae Herba, Menthae Haplocalycis Herba | Treating acute rhinitis | “Zhong Yao Cheng Fang Zhi Ji” c |
| Bi Dou Yan Kou Fu Yan | Xanthii Fructus, Magno1iae Flos, Menthae Haplocalycis Herba, Platycodonis Radix, Bupleuri Radix, Angelicae Dahuricae Radix, Chuanxiong Rhizoma, Scutellariae Radix, Gardeniae Fructus, Poria, Clematidis Armandii Caulis, Astragali Radix | Curing nasal obstruction due to wind-heat affecting lung, acute and chronic rhinitis, nasosinusitis | “Chinese Pharmacopoeia (2010)” a |
| Bi Shu Shi Tablets | Xanthii Fructus, Chrysanthemi Indici Flos, Centipedae Herba, Angelicae Dahuricae Radix, Saposhnikoviae Radix, Ecliptae Herba, Paeoniae Radix Alba, Arisaema Cum Bile, Glycyrrhizae Radix Et Rhizoma, Tribuli Fructus | Curing sneeze, rhinorrhea, nasal obstruction, headache, allergic rhinitis, chronic nasosinusitis | “Zhong Yao Cheng Fang Zhi Ji” c |
| Bi Tong Pills | Xanthii Fructus, Magno1iae Flos, Angelicae Dahuricae Radix, Centipedae Herba, Menthae Haplocalycis Herba, Scutellariae Radix, Glycyrrhizae Radix Et Rhizoma | Curing affection of exogenous wind-heat, chronic rhinitis | “Zhong Yao Cheng Fang Zhi Ji” c |
| Classification | No. | Chemical Component | Part of Plant | Reference |
|---|---|---|---|---|
| Sesquiterpenoids | 1 | sibirolide A | Fruits | [13] |
| 2 | sibirolide B | Fruits | [13] | |
| 3 | norxanthantolide A | Fruits | [13] | |
| 4 | norxanthantolide B | Fruits | [13] | |
| 5 | norxanthantolide C | Fruits | [13] | |
| 6 | norxanthantolide D | Fruits | [13] | |
| 7 | norxanthantolide E | Fruits | [13] | |
| 8 | norxanthantolide F | Fruits | [13] | |
| 9 | 1β-hydroxyl-5α-chloro-8-epi-xanthatin | Aerial parts | [14] | |
| 10 | 11α,13-dihydro-8-epi-xanthatin | Aerial parts | [14] | |
| Sesquiterpenoids | 11 | xanthinin | Leaves | [15] |
| 12 | xanthumin | Leaves | [15] | |
| 13 | xanthanol | Leaves | [15] | |
| 14 | xanthanol Acetate | Leaves | [15] | |
| 15 | isoxanthanol | Leaves | [15] | |
| 16 | xanthumanol | Leaves | [16] | |
| 17 | deacetoxylxanthumin | Leaves | [16] | |
| 18 | xanthatin | Leaves | [16] | |
| 19 | xanthinosin | Leaves | [16] | |
| 20 | tomentosin | Leaves | [16] | |
| 21 | 8-epi-tomentosin | Leaves | [17] | |
| 22 | 11α,13-dihydroxanthuminol | Leaves | [18] | |
| 23 | desacetylxanthanol | Leaves | [18] | |
| 24 | (2E,4E,1’S,2’R,4’S,6’R)-dihydrophaseic acid | Fruits | [19] | |
| 25 | 8-epi-xanthatin | Aerial parts | [20] | |
| 26 | 2-hydroxy xanthinosin | Aerial parts | [21] | |
| 27 | lasidiol p-methoxybenzoate | Leaves | [18] | |
| 28 | 1β, 4β, 4α,5α-diepoxyxanth-11(13)-en-12-oic acid | Aerial parts | [22] | |
| 29 | 11α,13-dihydroxanthatin | Aerial parts | [22] | |
| 30 | 4β,5β-epoxyxanthatin-1α,4α-endoperoxide | Aerial parts | [22] | |
| 31 | 4-epi-xanthanol | Aerial parts | [22] | |
| 32 | 4-epi-isoxanthanol | Aerial parts | [22] | |
| 33 | 4-oxo-bedfordia acid | Aerial parts | [22] | |
| 34 | 2-hydroxytomentosin | Aerial parts | [20] | |
| 35 | 2-hydroxytomentosin-1β,5β-epoxide | Aerial parts | [20] | |
| 36 | xanthnon | Aerial parts | [21] | |
| 37 | 6β,9β-dihydroxy-8-epi-xanthatin | Leaves | [23] | |
| 38 | inusoniolide | Aerial parts | [21] | |
| 39 | (3S,5R,6S,7E)-5,6-epoxy-3-hydroxy-7-megastigmene-9-one | Fruits | [24] | |
| 40 | pungiolide E | Aerial parts | [25] | |
| 41 | pungiolide A | Aerial parts | [25] | |
| 42 | pungiolide D | Aerial parts | [25] | |
| 43 | 5-azuleneacetic acid | Aerial parts | [21] | |
| 44 | dihydrophaseic acid sodium salt 4’-O-β-d-glucopyranoside | Fruits | [26] | |
| 45 | (3S,5R,6R,7E,9S)-megastigman-7ene-3,5,6,9-tetrol-3-O-β-d-glucopyranoside | Aerial parts | [27] | |
| Triterpenoids | 46 | betulinic acid | Roots | [28] |
| 47 | betulin | Roots | [28] | |
| 48 | erythrodiol | Roots | [28] | |
| 49 | lup-20(29)-en-3β-ol | Aerial parts | [27] | |
| Triterpenoids | 50 | lupenyl acetate | Aerial parts | [29] |
| 51 | lupeol acetate | Whole plants | [30] | |
| 52 | β-amyrin | Aerial parts | [31] | |
| 53 | oleanolic acid | Aerial parts | [31] | |
| 54 | α-amyrin | Leaves | [32] | |
| Phenylpropenoids | 55 | 1,3,5-tri-O-caffeoylquinic acid | Fruits | [33] |
| 56 | 3,5-di-O-caffeoylquinic acid | Fruits | [33] | |
| 57 | neochlorogenic acid methyl ester | Fruits | [34] | |
| 58 | 1,3-di-O-caffeoylquinic acid | Fruits | [34] | |
| 59 | methyl-3,5-di-O-caffeoylquinic acid | Fruits | [34] | |
| 60 | chlorogenic acid | Fruits | [35] | |
| 61 | 1,4-di-O-caffeoylquinic acid | Fruits | [35] | |
| 62 | 4,5-di-O-caffeoylquinic acid | Fruits | [35] | |
| 63 | 5-O-caffeoylquinic acid | Fruits | [35] | |
| 64 | 1,5-di-O-caffeoylquinic acid | Fruits | [36] | |
| 65 | 3,4-di-caffeoylquinic acid methyl ester | Fruits | [37] | |
| 66 | 3,5-di-caffeoylquinic acid methyl ester | Fruits | [37] | |
| 67 | 4-O-caffeoyl quinic acid methyl ester | Fruits | [38] | |
| 68 | N-trans-feruloyl tyramine | Roots | [39] | |
| 69 | 9,9’-O-di-(E)-feruloyl-(-)-secoisolariciresinol | Roots | [39] | |
| 70 | xanthiumnolic A | Fruits | [40] | |
| 71 | xanthiumnolic C | Fruits | [40] | |
| 72 | 2,3-dihydroxy-1-(4-hydroxy-3-methoxyphenyl)-propan-1-one | Fruits | [41] | |
| 73 | threo-guaiacylglycerol-8-O-4’- (coniferyl alcohol) ether | Fruits | [42] | |
| 74 | erythro-guaiacylglycerol-8-O-4’-(coniferyl alcohol) ether | Fruits | [42] | |
| 75 | threo-1-phenyl-(4-hydroxy-3-methoxy)-2-phenyl-(4’’-hydroxy-3’’-methoxy)-1,3-propanediol | Fruits | [42] | |
| 76 | (1S,2R)-1,2-bis(4-hydroxy-3-methoxyphenyl)-1,3-propanediol | Fruits | [42] | |
| 77 | threo-guaiacylglycerol-β-coniferyl aldehyde ether | Fruits | [42] | |
| 78 | erythro-guaiacylglycerol-β-coniferyl aldehyde ether | Fruits | [42] | |
| 79 | xanthiumnolic D | Fruits | [40] | |
| 80 | xanthiumnolic E | Fruits | [40] | |
| 81 | ferulic acid | Fruits | [43] | |
| 82 | caffeic acid | Fruits | [36] | |
| 83 | protocatechuic acid | Fruits | [19] | |
| 84 | isovanillic acid | Whole plants | [30] | |
| 85 | 7-(4-hydroxy-3-methoxyphenyl)-1-phenylhept-4-en-3-one | Roots | [28] | |
| Phenylpropenoids | 86 | xanthiazone-(2-O-caffeoyl)-β-d-glucopyranoside | Whole plants | [44] |
| 87 | rel-(2α,3β)-7-O-methylcedrusin | Fruits | [42] | |
| 88 | caffeic acid choline ester | Fruits | [38] | |
| 89 | icariside D1 | Fruits | [45] | |
| 90 | 3-methoxy-4-hydroxy-transcinnamaldehyde | Fruits | [24] | |
| 91 | methylchlorogenate | Fruits | [46] | |
| 92 | icariside F2 | Fruits | [45] | |
| 93 | arbutin | Fruits | [45] | |
| 94 | coniferine | Fruits | [45] | |
| 95 | 3-hydoxy-1-(4-hydroxy-phenyl)-propan-1-one | Fruits | [47] | |
| 96 | ω-hydroxypropioguaiacone | Fruits | [45] | |
| 97 | caffeic acid ethyl ester | Fruits | [19] | |
| 98 | 4-hydroxy-3-methoxycinnamaldehyde | Fruits | [37] | |
| 99 | p-hydroxybenzaldehyde | Fruits | [24] | |
| Lignanoids | 100 | xanthiumnolic B | Fruits | [40] |
| 101 | (-)-1-O-β-d-glucopyranosyl-2-{2-methoxy-4-[1-(E)-propen-3-ol]phenoxyl}-propane-3-ol | Fruits | [48] | |
| 102 | leptolepisol D | Fruits | [48] | |
| 103 | dihydrodehydrodiconiferyl alcohol | Fruits | [48] | |
| 104 | chushizisin E | Fruits | [48] | |
| 105 | (-)-(2R)-1-O-β-d-glucopyranosyl-2-{2-methoxy-4-[(E)formylviny1]phenoxyl}propane-3-ol | Fruits | [48] | |
| 106 | (-)-7R,8S-dehydrodiconiferyl alcohol | Fruits | [48] | |
| 107 | (-)-simulanol | Fruits | [48] | |
| 108 | 2-(4-hydroxy-3-methoxyphenyl)-3-(2-hydroxy-5-methoxyphenyl)-3-oxo-1-propanol | Fruits | [48] | |
| 109 | diospyrosin | Fruits | [48] | |
| 110 | dehydrodiconiferyl alcohol | Fruits | [48] | |
| 111 | balanophonin A | Fruits | [48] | |
| 112 | threo-dihydroxydehydrodiconiferyl alcohol | Fruits | [48] | |
| Lignanoids | 113 | 1-(4-hydroxy-3-methoxy)-phenyl-2-[4-(1,2,3-trihydroxypropyl)-2-methoxy]-phenoxy-1,3-propandiol | Fruits | [48] |
| 114 | 7R,8S-dihydrodehydrodiconiferyl alcohol 4-O-β-d-glucopyranoside | Fruits | [48] | |
| 115 | syringaresinol | Roots | [39] | |
| 116 | fructusol A | Fruits | [42] | |
| 117 | balanophonin | Fruits | [24] | |
| 118 | 4-oxopinoresinol | Roots | [28] | |
| 119 | pinoresinol | Fruits | [24] | |
| Coumarins | 120 | jatrocin B | Roots | [39] |
| Coumarins | 121 | cleomiscosin A | Roots | [39] |
| 122 | cleomiscosin C | Roots | [39] | |
| 123 | scopoletin | Roots | [39] | |
| Steroids | 124 | stigmast-4-en-β-ol-3-one | Roots | [39] |
| 125 | β-sitostenone | Roots | [39] | |
| 126 | β-sitosterol | Fruits, Leaves | [39] | |
| 127 | daucosterol | Fruits | [39] | |
| 128 | 5α,8α-epidioxy-22E-ergosta-6,22-dien-3β-ol | Roots | [39] | |
| 129 | 6β-hydroxy-stigmast-4,22-dien-3-one | Roots | [28] | |
| 130 | 6β-hydroxy-stigmast-4-en-3-one | Roots | [28] | |
| 131 | 3-oxo-△(4,5)-sitostenone | Roots | [28] | |
| 132 | β-daucosterol | Roots | [28] | |
| 133 | β-stigmasterol | Roots | [28] | |
| 134 | 7-ketositosterol | Roots | [28] | |
| 135 | stigmasterol | Aerial parts | [31] | |
| 136 | β-sitosterol-3-O-β-d-glucopyranoside | Aerial parts | [31] | |
| 137 | ergosterol | Whole plants | [30] | |
| 138 | taraxasteryl acetate | Whole plants | [30] | |
| 139 | 7α-hydroxy-β-sitosterol (stigmast-5-ene-3β,7α-diol) | Fruits | [24] | |
| 140 | stigmast-4-ene-3β,6α-diol | Fruits | [24] | |
| 141 | 14-methyl-12,13-dehydro-sitosterol-heptadeconate | Leaves | [32] | |
| Glycosides | 142 | atractyloside | Fruits | [49] |
| 143 | carboxyatractyloside | Burrs | [50] | |
| 144 | 3β-norpinan-2-one 3-O-β-d-apiofuranosyl-(1→6)-β-d-glucopyranoside | Fruits | [41] | |
| 145 | (6Z)-3-hydroxymethyl-7-methylocta-1,6-dien-3-ol 8-O-β-d-glucopyranoside | Fruits | [41] | |
| 146 | (6E)-3-hydroxymethyl-7-methylocta-1,6-dien-3-ol 8-O-β-d-glucopyranoside | Fruits | [41] | |
| 147 | 7-[(β-d-apiofuranosyl-(1→6)-β-d-glucopyranosyl)oxymethy]-8,8-dimethyl-4,8-dihydrobenzo[1,4]thiazine-3,5-dione | Fruits | [41] | |
| 148 | 3’,4’-dedisulphated-atractyloside | Fruits | [46] | |
| 149 | 2-methyl-3-buten-2-ol-β-d-ap-iofuranosyl-(1→6)-β-d-glucopyranoside | Fruits | [51] | |
| 150 | everlastoside C | Fruits | [51] | |
| Flavonoids | 151 | ononin | Fruits | [43] |
| 152 | quercetin | Fruits | [37] | |
| 153 | allopatuletin | Fruits | [37] | |
| 154 | patuletin-3-glucuronide | Fruits | [34] | |
| Flavonoids | 155 | quercetin-3-O-glucuronide | Fruits | [34] |
| 156 | formononetin | Fruits | [43] | |
| Tihiazdes | 157 | xanthiazone | Fruits | [36] |
| 158 | 2-hydroxy-xanthiazone | Fruits | [42] | |
| 159 | 7-hydroxymethyl-8,8-dimethyl-4,8-dihydrobenzol[1,4]thiazine-3,5-dione-11-O-β-d-glucopyranoside | Fruits | [43] | |
| 160 | 2-hydroxy-7-hydroxymethyl-8,8-dimethyl-4,8-dihydrobenzol[1,4]thiazine-3,5-dione-11-O-β-d-glucopyranoside | Fruits | [43] | |
| 161 | 7-Hydroxymethyl-8,8-dimethyl-4,8-dihydrobenzol[1,4]thiazine-3,5-dione-(2-O-caffeoyl)-β-d-glucopyranoside | Fruits | [52] | |
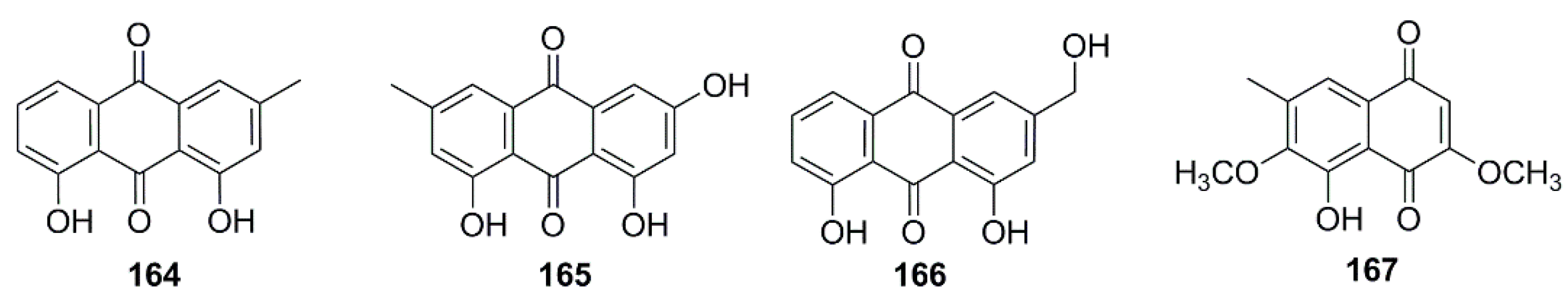
| Anthraquinones & naphthoquinones | 162 | xanthialdehyde | Fruits | [53] |
| 163 | chrysophanic acid | Fruits | [54] | |
| 164 | emodin | Fruits | [54] | |
| 165 | aloe emodin | Fruits | [54] | |
| 166 | 5-hydroxy-3,6-dimethoxy-7-methyl-1,4-naphthalenedione | Roots | [28] | |
| Other compounds | 167 | 5-methyluracil | Roots | [39] |
| 168 | uracil | Roots | [39] | |
| 169 | sibiricumthionol | Fruits | [19] | |
| 170 | indole-3-carbaldehyde | Fruits | [45] | |
| 171 | N-(1’-d-deoxyxylitolyl)-6,7-dimethyl-1,4-dihydro-2,3-quinoxalinedione | Fruits | [38] | |
| 172 | nonadecanoic acid | Roots | [39] | |
| 173 | hexadecanoic acid | Leaves | [32] |
| Effects | Detail | Extracts/Compounds | Concentration/Dose | In Vivo/In vitro | Reference |
|---|---|---|---|---|---|
| Anti-AR effects | Inhibiting C 48/80-induced systemic anaphylaxis | WEX | Mice, 0.01–1 g/kg (p.o.) | in vivo | [61,62] |
| Inhibiting histamine and TNF-α released from RPMC | WEX | RPMC, 0.01–1 mg/mL | in vitro | [63] | |
| Modulating the HMC-1- and PBMNC-mediated inflammatory and immunological reactions | WEX | HMC-1, PBMNC, 0.25–1 mg/mL | in vitro | [63] | |
| Inhibiting histamine and cAMP released from RPMC | MEX | RPMC, 20–500 μg/mL | in vitro | [64] | |
| Ameliorate the nasal symptoms of OVA induced AR rats via anti-allergic; down-regulating IgE; anti-inflammatory and analgesic properties | CXT | Rats, 5, 10, 20 mg/kg (p.o.) | in vivo | [65] | |
| Anti-tumor effects | Lung cancer | ||||
| Growth inhibition by suppression of STAT3, GSK3β and β-catenin | xanthatin | Cell lines of A549, H1975, H1299, H1650 & HCC827, 1–40 μM | in vitro | [66,67,68] | |
| Triggering Chk1-mediated DNA damage and destabilization of Cdc25C via lysosomal degradation | xanthatin | ||||
| Cytotoxic effects on A549 cell | 8-epi-xanthatin | IC50 = 1.1 μg/mL | in vitro | [17] | |
| 8-epi-xanthatin epoxide | IC50 = 3.0 μM | in vitro | [69] | ||
| xanthatin | IC50 = 1.3 μg/mL | in vitro | [17] | ||
| 8-epi-xanthatin-1α, 5α-epoxide | IC50 = 9.5 μM | in vitro | [25] | ||
| 1β-hydroxyl-5α-chloro-8-epi-xanthatin | IC50 = 20.7 μM | in vitro | [25] | ||
| EEXA | IC50 = 52.2 μg/mL | in vitro | [70] | ||
| Breast cancer | |||||
| Cytotoxic effects on MDA-MB-231 cells | xanthatin | IC50 = 13.9 μg/mL | in vitro | [71] | |
| Cytotoxic effects on MDA-MB-231 cells | xanthinosin | IC50 = 4.8 μg/mL | in vitro | [71] | |
| Inhibiting cell growth via inducing caspase independent cell death | xanthatin | MDA-MB-231 cells, 5–25 μM | in vitro | [72] | |
| Anti-tumor effects | Up-regulating GADD45 γ tumor suppressor gene; inducing the prolonged expression of c-Fos via N-acetyl-l-cysteine-sensitive mechanism | xanthatin | MDA-MB-231 cells, 2.5–10 μM | in vitro | [73,74] |
| Cytotoxic effects on MFC7 cells | EEXA | IC50 = 70.6 μg/mL | in vitro | [70] | |
| Cervical cancer | |||||
| Altering the antioxidant levels | WEX | Hela cells, 12.5–50 μg/mL | in vitro | [75] | |
| Promoting apoptosis via inhibiting thioredoxin reductase and eliciting oxidative stress | xanthatin | Hela cells, 5–20 µM | in vitro | [76] | |
| Colon cancer | |||||
| Cytotoxic effects on HCT-15 cells | xanthatin | ED50 = 1.1 μg/mL | in vitro | [17] | |
| 8-epi-xanthatin | ED50 = 0.1 μg/mL | in vitro | [17] | ||
| Cytotoxic effects on WiDr cells | xanthatin | IC50 = 6.15 μg/mL | in vitro | [71] | |
| xanthinosin | IC50 = 2.65 μg/mL | in vitro | [71] | ||
| Cytotoxic effects on BGC-823 cells | eremophil-1(10),11(13)-dien-12,8β-olide | IC50 = 13.22 µM | in vitro | [77] | |
| 8-epi-xanthatin-1β,5β-epoxide | IC50 = 2.43 µM | in vitro | [77] | ||
| tomentosin | IC50 = 4.54 µM | in vitro | [77] | ||
| Cytotoxic effects on KE-97 cells | eremophil-1(10),11(13)-dien-12,8β-olide | IC50 = 4.41 µM | in vitro | [77] | |
| 8-epi-xanthatin-1β,5β-epoxide | IC50 = 1.44 µM | in vitro | [77] | ||
| tomentosin | IC50 = 3.47 µM | in vitro | [77] | ||
| Inducing G2/M cell cycle arrest and apoptosis | xanthatin | MKN-45 Cells, 3.9–18.6 µM | in vitro | [75] | |
| Potentiating both extrinsic and intrinsic TRAIL-mediated apoptosis pathways and also decreased the level of cell survival protein Bcl-2 | xanthinosin | AGS cells, 8 µM | in vitro | [18] | |
| lasidiol p-methoxybenzoate | AGS cells, 16 µM | in vitro | [18] | ||
| Cytotoxic effects on CT26 cells | EEXA | IC50 = 58.9 μg/mL | in vitro | [70] | |
| CFEEXA | IC50 = 25.3 μg/mL | in vitro | [70] | ||
| Cytotoxic effects on AGS cells | fructusnoid C | IC50 = 7.6 µM | in vitro | [79] | |
| Liver cancer | |||||
| Cytotoxic effects on SNU387 cells | 1β-hydroxyl-5α-chloro-8-epi-xanthatin | IC50 =5.1 µM | in vitro | [25] | |
| Cytotoxic effects on HepG2 cells | MEX | LC50 = 112.9 μg/mL | in vitro | [80] | |
| EAFMEX | LC50 = 68.739 μg/mL | in vitro | [80] | ||
| Induction of apoptosis via inhibiting thioredoxin reductase and eliciting oxidative stress | xanthatin | HepG2 cells, 5–40 μM | in vitro | [76] | |
| Meningioma | |||||
| Cytotoxic effects on SK-MEL-2 cells | xanthatin | ED50 = 0.5 μg/mL | in vitro | [17] | |
| 8-epi-xanthatin | ED50 = 0.2 μg/mL | in vitro | [17] | ||
| Inhibiting melanin synthesis through downregulation of tyrosinase via GSK3β phosphorylation | EEXS | Mel-Ab cells, 1–50 µg/mL | in vitro | [81] | |
| Inhibiting cell proliferation associated with activation of Wnt/β-catenin pathway and inhibition of angiogenesis | xanthatin | B16-F10 cells, 2.5–40μM | in vitro | [82] | |
| Mice, 0.1–0.4 mg/10 g(i.p.) | in vivo | [82] | |||
| Anti-tumor effects | Leukemia | ||||
| Cytotoxic effects on P-388 cells | DFEEXA | IC50 = 1.64 μg/mL | in vitro | [83] | |
| Cytotoxic effects on HL-60 cells | xanthatin | IC50 = 52.50 µg/mL | in vitro | [84] | |
| Cytotoxic effects on Jurkat cells | MEX | LC50 = 50.18 µg/mL | in vitro | [80] | |
| EAFMEX | LC50 = 48.73 µg/mL | in vitro | [80] | ||
| Other tumors | |||||
| Cytotoxic effects on XF-498 cells | xanthatin | ED50 = 1.7 μg/mL | in vitro | [17] | |
| 8-epi-xanthatin | ED50 = 1.3 μg/mL | in vitro | [17] | ||
| Cytotoxic effects on S180 cells | WEX | Mice, 5–20 g/kg | in vivo | [85] | |
| Cytotoxic effects on HEP-2 cells | CEXR | 12.5–100 µg/mL | in vitro | [86] | |
| MEXR | 12.5–100 µg/mL | in vitro | [86] | ||
| Anti-inflammatory and analgesic effects | Anti-inflammatory | ||||
| Inhibitting LPS-stimulated inflammatory | WEX | 10, 100 and 1000 µg/mL | in vitro | [87] | |
| Inhibitting LPS-stimulated inflammatory | MEX | 30, 60 and 90 mg/mL | in vitro | [88] | |
| xanthatin and xanthinosin | IC50 = 0.47 and 11.2 μM | in vitro | [89] | ||
| MEXL | IC50 = 87 μg/mL | in vitro | [90] | ||
| MEXR | 50–400 μg/mL | in vitro | [91] | ||
| WEX | 0.5, 1 and 2 mg/mL | in vitro | [92] | ||
| MEX | 0–300 μg/mL | in vitro | [93] | ||
| MEXA | 0–300 μg/mL | in vitro | [94] | ||
| xanthiumnolic E | IC50 = 8.73 μM. | in vitro | [26] | ||
| Inhibiting carrageenan induced hind paw edema | MEX | 100, 200 mg/kg/d (p.o.) | in vivo | [88] | |
| WEX | 0.1, 0.5 and 1.0 g/kg, (p.o.) | in vitro | [95] | ||
| MEXL | 100, 200 and 400 mg/kg body weight. | in vivo | [90] | ||
| Inhibiting croton-oil-induced ear edema | NFEEX | Mice, 0.5, 0.75 and 1.0 mg/ear | in vivo | [96] | |
| Inhibiting both PGE 2 synthesis and 5-lipoxygenase activity | xanthatin | 100 and 97 mg/mL, respectively | in vitro | [84] | |
| Inhibiting production of TARC/CCL17 and MDC/CCL22 induced by TNF-α/IFN-γ | EEX | 10 μg/mL | in vitro | [97] | |
| Analgesic effect | |||||
| Ameliorating HCl/EtOH-induced gastritis lesions | MEXA | 50 and 200 mg/kg (p.o.) | in vivo | [94] | |
| Analgesic effect on acetic acid-induced abdominal constriction test and a hot plate test | MEX | 100, 200 mg/kg/d (p.o.) | in vivo | [88] | |
| Reducing the number of writhings induced by acetic acid | NFEEX | Mice, 100,200 and 400 mg/kg body wt. | in vivo | [96] | |
| Analgesic effect on writhing and formalin tests | WXF | 0.1, 0.5 and 1.0 g/kg, (p.o.) | in vivo | [95] | |
| Analgesic effect on hot plate test, acetic acid induced writhing test and formalin test | EEX | 250 and 500 mg/kg body weight | in vivo | [98] | |
| Insecticide and antiparasitic effects | Antiplasmodial activity against T. evansi | EEXL | 5, 50, 500 and 1000 µg/mL | in vitro | [99] |
| 100, 300 and 1000 mg/kg (i.p.) | in vivo | [99] | |||
| Insecticidal effects against T. b. brucei | xanthatin | IC50 = 2.63 µg/mL | in vitro | [84] | |
| Anti-insect effects towards P. viteana | MEX | LC50 = 11.02 (w/w) | in vitro | [100] | |
| Insecticide and antiparasitic effects | Antiplasmodial activity against P. berghei | EEXL | IC50 = 4 µg/mL | in vitro | [101] |
| Insecticidal properties against C. chinensis | WEXL | 1%, 2% and 4% concentration | in vitro | [102] | |
| Anti-nematode activity against Meloidogyne javanica | EEX | 3%, 6% and 12% concentration | in vitro | [103] | |
| Insecticidal effects against A. caspius, C. pipiens | MEX | LC50 = 531.07 and 502.32 μg/mL, respectively | in vitro | [80] | |
| Antioxidant effects | Scavenging DPPH | CEXR and MEXR | LC50 = 10.28 and 40.40 µg/mL | in vitro | [86] |
| WEX | 0.05–0.2 mg/mL | in vitro | [95] | ||
| EEXR and CEXR | IC50 = 29.81 and 24.85 µg/mL | in vitro | [106] | ||
| EEXL | IC50 = 85 µg/mL | in vitro | [107] | ||
| Scavenging DPPH | hexadecanoic acid; α- amyrin; 14-methyl-12, 13-dehydro-sitosterol-heptadeconate | IC50 = 106.4, 64.16 and 76.18 µg/mL | in vitro | [32] | |
| Scavenging DPPH | EOX | 138.87 μg/mL | in vitro | [108] | |
| MEX | Not mentioned | in vitro | [28] | ||
| Scavenging nitric oxide | EEXR and CEXR | IC50 = 395.20 and 415.80 µg/mL | in vitro | [106] | |
| EEXL | IC50 = 72 µg/mL | in vitro | [107] | ||
| Scavenging hydrogen peroxide | EEXR and CEXR | IC50 = 10.18 and 9.23 µg/mL | in vitro | [106] | |
| EEXL | IC50 = 62 µg/mL | in vitro | [107] | ||
| Increasing of superoxide dismutase, glutathione peroxidase, glutathione reductase and catalase contents | PEEXW | 250 and 500 mg/kg body weight (p.o for 20 days) | in vivo | [104] | |
| Liposome protection | WEX | 0.05–0.2 mg/mL | in vitro | [95] | |
| Scavenging ABTS | WEX | 0.05–0.2 mg/mL | in vitro | [95] | |
| Reducing activity | WEX | 0.05–0.2 mg/mL | in vitro | [95] | |
| Increasing of SOD, CAT, GSH and GPx contents | MEXS | 100 and 200 mg/kg (p.o., for 10 days) | in vivo | [105] | |
| Superoxide anion | EEXR and CEXR | IC50 = 495.30 and 418.30 µg/mL | in vitro | [106] | |
| Scavenging hydroxyl radicals | hexadecanoic acid; α- amyrin; 14-methyl-12, 13-dehydro-sitosterol-heptadeconate | IC50 = 127.4, 83.96 and 84.4 µg/mL | in vitro | [32] | |
| FRAP antioxidant activity | MEX | Not mentioned | in vitro | [28] | |
| Antibacterial and antifungal effects | Antibacterial | ||||
| Inhibitory effects against V. cholerae | WEXFT | Not mentioned | in vitro | [109] | |
| Inhibitory effects against S. epidermidis, B. cereus, K. pneumoniae, P. aeruginosa and S. fyphi | xanthatin | MIC = 31.3, 62.5, 31.3, 125 and 125 µg/mL | in vitro | [110] | |
| Inhibitory effects against K. pneumoniae, P. vulgaris, P. Aeruginosa, P. putida, S. typhimurium, B. cereus, B. subtilis, S. epidermidis | MEXL | 500 and 100 mg/mL | in vitro | [111] | |
| Inhibitory effects against E. coli | β-sitosterol and β-daucosterol | MIC = 0.17 and 0.35 µg/mL | in vitro | [112] | |
| Inhibitory effects towards K. pneumonia, P. mirabilis, E. coli, B. subtilis, E. faecalis, S. aureus | MEXL | 50, 100, 150, 200 and 250 mg/mL, respectively | in vitro | [113] | |
| WEXL | |||||
| Antibacterial and antifungal effects | Inhibitory effects against S. aureus, B. subtilis, K. pneumoniae and P. aeruginosa | EOXL | MIC = 0.5, 1.3, 4.8 and 20.5 µg/mL, respectively | in vitro | [114] |
| Inhibitory effects against Shiga toxin-producing E. coli | EOXL | 30, 60 and 120 mg/mL | in vitro | [115] | |
| Inhibitory effects against S. aureus and E. coli | WEX | MIC = 31.25 and 7.81 mg/mL, respectively | in vitro | [116] | |
| Inhibitory effects against R. toxicus, S. aureus and P. S. syringae | EOX | MIC = 25, 50 and 50 µg/mL, respectively | in vitro | [108] | |
| Antifungal | |||||
| Inhibitory effects against P. drechsleri | deacetylxanthumin | MIC = 12.5 µg/mL | in vitro | [117] | |
| Inhibitory effects against P. infestans | MEX | MIC = 2.0% w/v | in vitro | [118] | |
| Inhibitory effects against C. albicans and A. niger | EOXL | MIC = 55.2 and 34.3 µg/mL, respectively | in vitro | [114] | |
| Inhibitory effects against P. oryzae and F. oxysporum | EOX | MIC = 12.5 and 50 µg/mL, respectively | in vitro | [108] | |
| Inhibitory effects against A. niger, A. flavus, F. oxysporum, F. solani, A. alternata and P. digitatum | EOXL | MIC = 8 µg/mL and MFC = 8 µg/mL | in vitro | [119] | |
| Antidiabetic effects | Exhibiting potent hypoglycemic activity | WEX | 15 and 30 mg/kg (i.p.) | in vivo | [120] |
| Decreasing the plasma glucose in diabetic rats | caffeic acid | 0.5–3 mg/kg (i.v.) | in vivo | [121] | |
| Decreasing the blood glucose and HbA1C level and increase the level of insulin | MEXS | 100 and 200 mg/kg (p.o., for 30 days) | in vivo | [105] | |
| Inhibitory effect against rAR and rhAR | methyl-3,5-di-O-caffeoylquinate | IC50 = 0.30 and 0.67 µM, respectively | in vivo | [47] | |
| Inhibitory effect against α-glucosidase | CFMEXL | IC50 = 72 µg/mL | in vitro | [122] | |
| Inhibitory effect against α-glucosidase | MEX | IC50 = 15.25 µg/mL | in vivo | [28] | |
| Antilipidemic effects | Decreasing plasma cholesterol, triglyceride, LDL, and VLDL and increasing plasma HDL levels | CEXR and EEXR | 200 and 400 mg/kg (p.o.) | in vivo | [106] |
| Improving lipid homeostasis | WEX | 570 and 1140 mg/kg (p.o., for 6 weeks) | in vivo | [123] | |
| Decreasing blood glucose, TC, TG, LDLC levels and increasing HDLC levels. | WEX | 3.7 and 11.11 g/kg (p.o., for 4 weeks) | in vivo | [124] | |
| Antiviral activity | Antiviral activity against duck hepatitis B virus | WEX | 0.01, 0.1 and 1 g/kg (i.g., for 10 days) | in vivo | [125] |
| Antiviral activity against Influenza A virus | norxanthantolide F | IC50 = 6.4 µM | in vitro | [13] | |
| 2-desoxy-6-epi-parthemollin | IC50 = 8.6 µM | in vitro | [13] | ||
| xanthatin | IC50 = 8.4 µM | in vitro | [13] | ||
| threo-guaiacylglycerol-8′-vanillic acid ether | IC50 = 8.4 µM | in vitro | [13] | ||
| caffeic acid ethyl ester | IC50 = 3.7 µM | in vitro | [13] | ||
| Other pharmacological effects | Anti-septic activity | CXT | 10, 20 and 40 mg/kg(i.p.) | in vivo | [126] |
| Attenuating hepatic steatosis | WEX | 570 and 1140 mg/kg (p.o., for 6 weeks) | in vivo | [127] | |
| Anti-arthritic effect | EEX | 75 and 300 mg/kg (p.o.) | in vivo | [128] | |
| Other pharmacological effects | Anti-pyretic activity | MEXW | 200 and 400 mg/kg (p.o.) | in vivo | [129] |
| Anti-epileptic activity | PEEXW | 250 and 500 mg/kg (p.o., for 20 days) | in vivo | [130] | |
| Antiurolithiatic effect | HEEXB | 500 mg/kg (p.o.) | in vivo | [131] | |
| Antiulcer effect | EEXL | 200 and 400 mg/kg | in vivo | [132] | |
| Cardioprotective effect | CXT | 10, 20 and 40 mg/kg (p.o.) | in vivo | [133] | |
| Extracts/Compounds | Animal/Subjects | LD50/Toxic Dose Range | Toxic Reactions | Reference |
|---|---|---|---|---|
| WEX | mice | LD50 = 201.14 g/kg (i.g., crude herb mass equivalent) | Death | [139] |
| WEX | mice | LD50 = 167.60 g/kg (i.g., crude herb mass equivalent) | Death | [140] |
| EEX | mice | LD50 = 275.41 g/kg (i.g., crude herb mass equivalent) | Death | [140] |
| WEX | mice | LD50 = 194.15g/kg (i.g., crude herb mass equivalent) | Death | [141] |
| carboxyatractyloside | swine | 10–100 mg (i.v.) | Death | [142] |
| atractyloside | mice | 50–200 mg/kg (i.p.) | Increasing contents of ALT, AST, ALP, MDA in mice serum | [143] |
| carbxyatractyloside | mice | 50–150 mg/kg (i.p.) | Increasing contents of ALT, AST, ALP, MDA in mice serum | [143] |
| NFEEX | mice | 0.06, 0.3, 0.7 g/kg (i.g., for 28 days) | Weight loss, enlarged hepatic cell space, karyolysis and inflammatory cell infiltration | [145] |
| WFEEX | mice | 0.06, 0.3, 0.7 g/kg (i.g., for 28 days) | Weight loss, enlarged hepatic cell space, karyolysis, and inflammatory cell infiltration | [145] |
| WEX | mice | 21.0 g/kg (i.g., for 28 days) | Weight loss and increase of ALT, AST in mice serum | [146] |
| WEX | mice | 7.5, 15.0 and 30.0 g/kg (i.g., for 5 days) | Increasing contents of VLDL/LDL, β-HB, glutamate, choline, acetate, glucose in serum | [147] |
| WEX | mice | 16.7 g/kg (i.g., for 7 days) | Increasing contents of GLDH, α-GST and decreasing miRNA-122 | [148] |
| MEXA | mice | 100, 200, 300 mg/kg | Depressing the action of central nervous system | [149] |
| atractyloside | rat hepatocytes | 0.01–0.05 g/L | Reducing cell viability and intracellular GSH content | [150] |
| atractyloside, carbxyatractyloside | L-02 cells, BRL cells | 100 μmol/L for 48 h | Inhibiting cell proliferation, improving LDH activity | [147] |
| WEX | HK-2 cells | 100 μg/mL | Inhibiting cell proliferation | [151] |
| HEEXA | CHO cells | 25–100 μg/mL | Inducing DNA damage | [152] |
| EFEEX | MIHA cells | IC50 = 231.1 μg/ml | Decreasing viability of cell | [153] |
| WEX | zebrafish | 15 μg/mL | Decreasing hatch rate | [154] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, W.; Fan, L.; Peng, C.; Zhang, Q.; Wang, L.; Li, L.; Wang, J.; Zhang, D.; Peng, W.; Wu, C. Traditional Uses, Botany, Phytochemistry, Pharmacology, Pharmacokinetics and Toxicology of Xanthium strumarium L.: A Review. Molecules 2019, 24, 359. https://doi.org/10.3390/molecules24020359
Fan W, Fan L, Peng C, Zhang Q, Wang L, Li L, Wang J, Zhang D, Peng W, Wu C. Traditional Uses, Botany, Phytochemistry, Pharmacology, Pharmacokinetics and Toxicology of Xanthium strumarium L.: A Review. Molecules. 2019; 24(2):359. https://doi.org/10.3390/molecules24020359
Chicago/Turabian StyleFan, Wenxiang, Linhong Fan, Chengyi Peng, Qing Zhang, Li Wang, Lin Li, Jiaolong Wang, Dayong Zhang, Wei Peng, and Chunjie Wu. 2019. "Traditional Uses, Botany, Phytochemistry, Pharmacology, Pharmacokinetics and Toxicology of Xanthium strumarium L.: A Review" Molecules 24, no. 2: 359. https://doi.org/10.3390/molecules24020359
APA StyleFan, W., Fan, L., Peng, C., Zhang, Q., Wang, L., Li, L., Wang, J., Zhang, D., Peng, W., & Wu, C. (2019). Traditional Uses, Botany, Phytochemistry, Pharmacology, Pharmacokinetics and Toxicology of Xanthium strumarium L.: A Review. Molecules, 24(2), 359. https://doi.org/10.3390/molecules24020359





