Herbal Composition LI73014F2 Alleviates Articular Cartilage Damage and Inflammatory Response in Monosodium Iodoacetate-Induced Osteoarthritis in Rats
Abstract
:1. Introduction
2. Results
2.1. Composition of LI73014F2
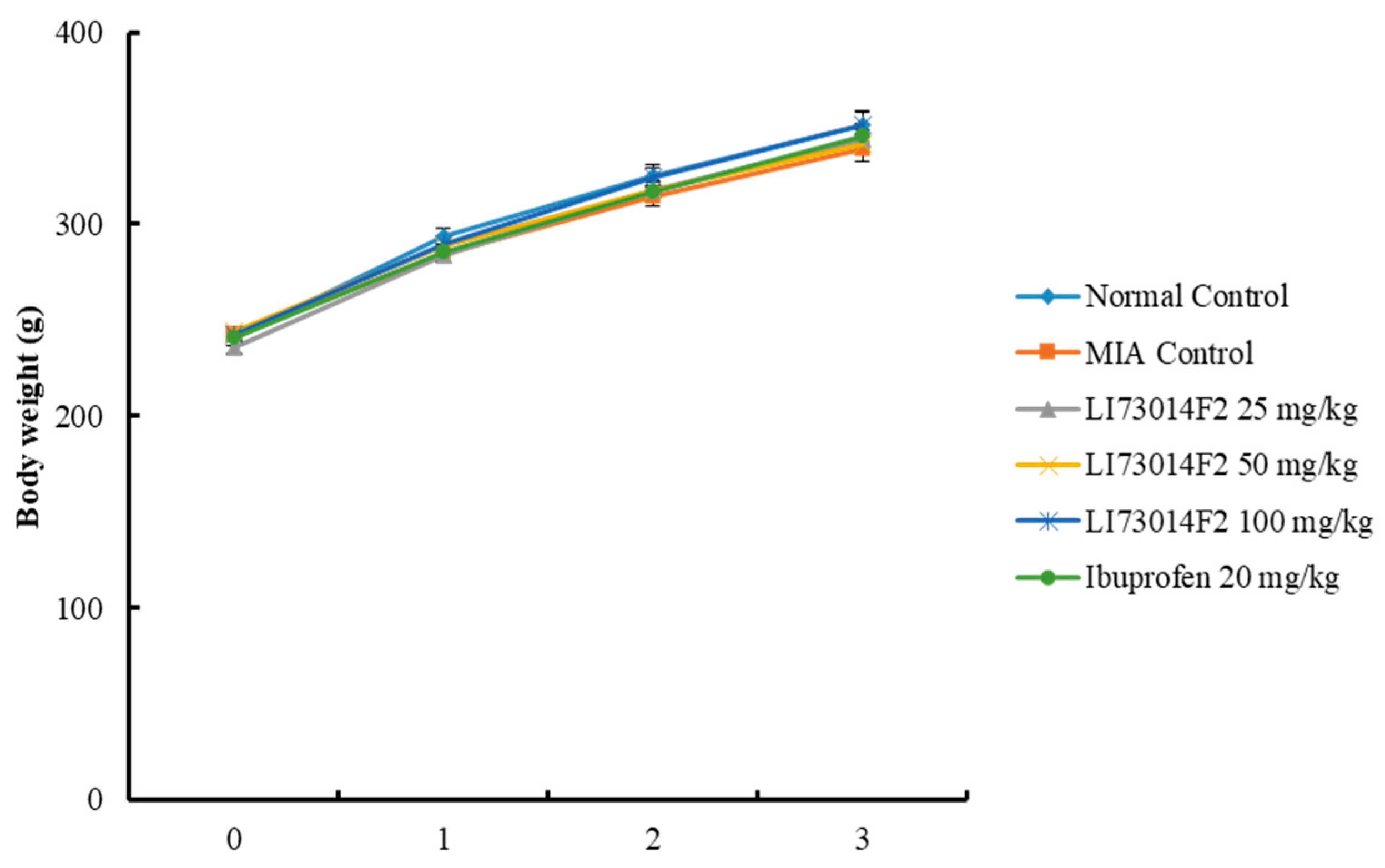
2.2. Effects of LI73014F2 on Changes in Body Weight in Monosodium Iodoacetate (MIA)-Induced Osteoarthritis in Rats
2.3. Effects of LI73014F2 on the Hind Paw Weight-Bearing Distribution for 21 Days in MIA-Induced Osteoarthritis in Rats
2.4. Effects of LI73014F2 on Arthritis Index (AI) for 21 Days in MIA-Induced Osteoarthritis in Rats
2.5. Effects of LI73014F2 on Synovial Fluid Levels of Inflammatory Factors in MIA-Induced Osteoarthritis in Rats
2.6. Effects of LI73014F2 on the Expression Levels of Inflammation-Related Proteins in Articular Cartilage
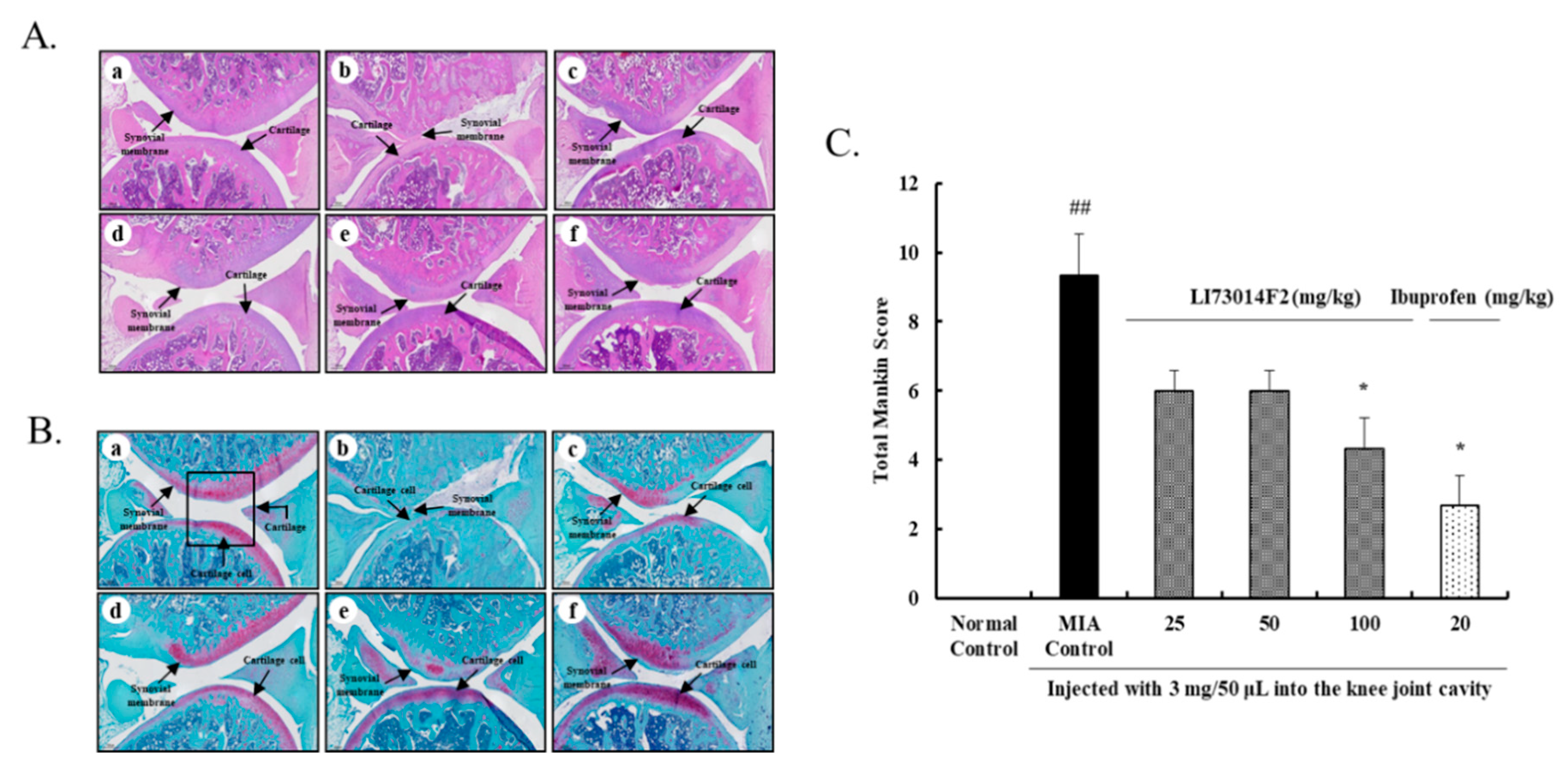
2.7. Effects of LI73014F2 on Histological Evaluation of Joint Activity in MIA-Induced Osteoarthritis in Rats
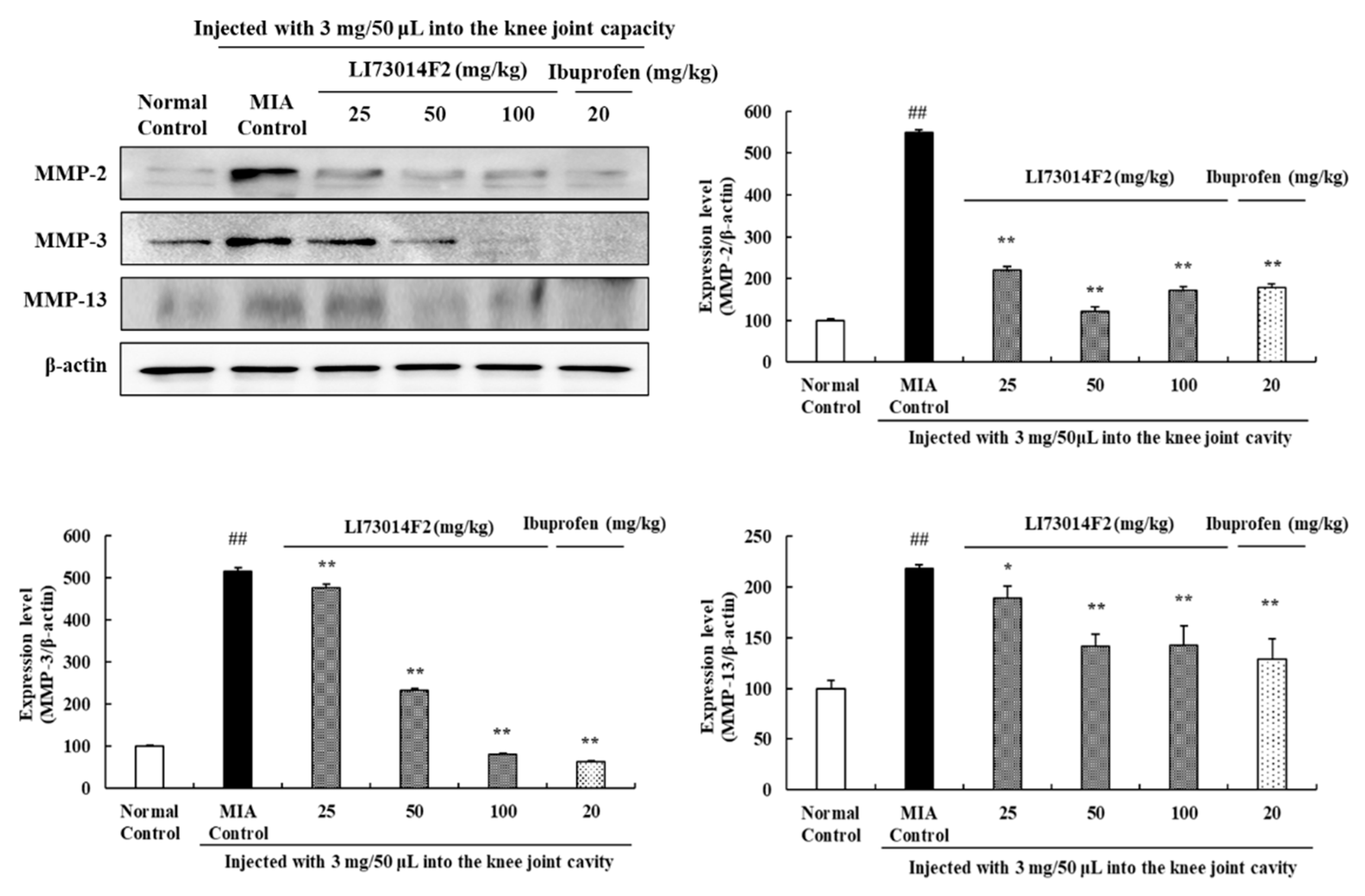
2.8. Effects of LI73014F2 on Expression Levels of MMPs in Articular Cartilage
3. Discussion
4. Materials and Methods
4.1. Sample Preparation and Component Analysis
4.2. Animals
4.3. MIA-Induced OA and Drug Administration
4.4. Progression of OA and Hind Paw Weight-Bearing Distribution
4.5. Synovial Fluid Analysis
4.6. Joint Histological Examination
4.7. Western Blotting
4.8. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Nakata, K.; Hanai, T.; Take, Y.; Osada, T.; Tsuchiya, T.; Shima, D.; Fujimoto, Y. Disease-modifying effects of COX-2 selective inhibitors and non-selective NSAIDs in osteoarthritis: A systematic review. Osteoarthr. Cartil. 2018, 26, 1263–1273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwon, J.Y.; Lee, S.H.; Na, H.-S.; Jung, K.; Choi, J.; Cho, K.H.; Lee, C.-Y.; Kim, S.J.; Park, S.-H.; Shin, D.-Y.; et al. Kartogenin inhibits pain behavior, chondrocyte inflammation, and attenuates osteoarthritis progression in mice through induction of IL-10. Sci. Rep. 2018, 8, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Sim, B.-Y.; Choi, H.-J.; Kim, M.-G.; Jeong, D.-G.; Lee, D.-G.; Yoon, J.-M.; Kang, D.-J.; Park, S.; Ji, J.-G.; Joo, I.-H.; et al. Effects of ID-CBT5101 in Preventing and Alleviating Osteoarthritis Symptoms in a Monosodium Iodoacetate-Induced Rat Model. J. Microbiol. Biotechnol. 2018, 28, 1199–1208. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.J.; Kim, M.J.; Qiu, J.; Zhang, T.; Wu, X.; Jang, D.-J.; Park, S. Rice Porridge Containing Welsh Onion Root Water Extract Alleviates Osteoarthritis-Related Pain Behaviors, Glucose Levels, and Bone Metabolism in Osteoarthritis-Induced Ovariectomized Rats. Nutrients 2019, 11, 1503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cho, S.H. Effect of Green Lipped Mussel Extract Oil Complex (Gwanjeolpalpal) on Monosodium Iodoacetate-Induced Osteoarthritis in Animal Model. J. Korean Soc. Food Sci. Nutr. 2019, 48, 206–214. [Google Scholar] [CrossRef]
- Kapoor, M.; Martel-Pelletier, J.; Lajeunesse, D.; Pelletier, J.-P.; Fahmi, H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat. Rev. Rheumatol. 2011, 7, 33–42. [Google Scholar] [CrossRef]
- Burrage, P.S.; Mix, K.S.; Brinckerhoff, C.E. Matrix metalloproteinases: Role in arthritis. Front. Biosci. 2006, 11, 529–843. [Google Scholar] [CrossRef] [Green Version]
- Karlapudi, V.; Mungara, A.V.V.P.; Sengupta, K.; Davis, B.A.; Raychaudhuri, S.P. A Placebo-Controlled Double-Blind Study Demonstrates the Clinical Efficacy of a Novel Herbal Formulation for Relieving Joint Discomfort in Human Subjects with Osteoarthritis of Knee. J. Med. Food 2018, 21, 511–520. [Google Scholar] [CrossRef]
- Casale, T.B.; Abbas, M.K.; Carolan, E.J. Degree of Neutrophil Chemotaxis Is Dependent upon the Chemoattractant and Barrier. Am. J. Respir. Cell Mol. Biol. 1992, 7, 112–117. [Google Scholar] [CrossRef]
- Gök, Ş.; Ülker, S.; Hüseyinov, A.; Hatip, F.B.; Çınar, M.G.; Evinç, A. Role of Leukotrienes on Coronary Vasoconstriction in Isolated Hearts of Arthritic Rats: Effect of in vivo Treatment with CI-986, a Dual Inhibitor of Cyclooxygenase and Lipoxygenase. Pharmacology 2000, 60, 41–46. [Google Scholar] [CrossRef]
- Haroyan, A.; Mukuchyan, V.; Mkrtchyan, N.; Minasyan, N.; Gasparyan, S.; Sargsyan, A.; Narimanyan, M.; Hovhannisyan, A. Efficacy and safety of curcumin and its combination with boswellic acid in osteoarthritis: A comparative, randomized, double-blind, placebo-controlled study. BMC Complement. Altern. Med. 2018, 18, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertocchi, M.; Isani, G.; Medici, F.; Andreani, G.; Tubon, I.; Roncada, P.; Forni, M.; Bernardini, C. Anti-Inflammatory Activity of Boswellia serrata Extracts: An In Vitro Study on Porcine Aortic Endothelial Cells. Oxidative Med. Cell. Longev. 2018, 2018, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soleimani, V.; Sahebkar, A.; Hosseinazadeh, H. Tumeric (Curcuma longa) and its major constituent (Curcumin) as nontoxic and safe substances: Review. Phytother. Res. 2018, 32, 985–995. [Google Scholar] [CrossRef] [PubMed]
- Daily, J.W.; Yang, M.; Park, S. Efficacy of Turmeric Extracts and Curcumin for Alleviating the Symptoms of Joint Arthritis: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. J. Med. Food 2016, 19, 717–729. [Google Scholar] [CrossRef] [Green Version]
- Kuptniratsaikul, V.; Dajpratham, P.; Taechaarpornkul, W.; Buntragulpoontawee, M.; Lukkanapichonchut, P.; Chootip, C.; Saengsuwan, J.; Tantayakom, K.; Laongpech, S. Efficacy and safety of Curcuma domestica extracts compared with ibuprofen in patients with knee osteoarthritis: A multicenter study. Clin. Interv. Aging 2014, 9, 451–458. [Google Scholar] [CrossRef] [Green Version]
- Afshari, A.R.; Sadeghina, H.R.; Mollazadeh, H. A Review on Potential Mechanisms of Terminallia chebula in Alzheimer’s Disease. Adv. Pharmacol. Pharm. Sci. 2016, 2016, 8964849. [Google Scholar]
- Kim, H.L.; Lee, H.J.; Lee, D.-R.; Choi, B.-K.; Yang, S.H. Anti-osteoarthritic effects of an herbal composition LI73014F2 on primary human articular chondrocytes. Molecules 2020, 25, 2033. [Google Scholar] [CrossRef]
- Pitcher, T.; Sousa-Valente, J.; Malcangio, M. The Monoiodoacetate Model of Osteoarthritis Pain in the Mouse. J. Vis. Exp. 2016, 111, e53746. [Google Scholar] [CrossRef] [Green Version]
- Park, S.; Lee, L.R.; Seo, J.H.; Kang, S. Curcumin and tetrahydrocurcumin both prevent osteoarthritis symptoms and decrease the expressions of pro-inflammatory cytokines in estrogen-deficient rats. Genes Nutr. 2016, 11, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Sabri, M.I.; Ochs, S. Inhibition of glyceraldehyde-3-phosphate dehydrogenase in mammalian nerve by iodoacetic acid. J. Neurochem. 1971, 18, 1509–1514. [Google Scholar] [CrossRef]
- Van Der Kraan, P.M.; Vitters, E.L.; Van De Putte, L.B.; Berg, W.B.V.D. Development of osteoarthritic lesions in mice by “metabolic” and “mechanical” alterations in the knee joints. Am. J. Pathol. 1989, 135, 1001–1014. [Google Scholar] [PubMed]
- Jeong, J.-W.; Lee, H.H.; Kim, J.; Choi, E.-O.; Hwang-Bo, H.; Kim, H.J.; Kim, M.Y.; Ahn, K.I.; Kim, G.-Y.; Lee, K.W.; et al. Mori Folium water extract alleviates articular cartilage damages and inflammatory responses in monosodium iodoacetate-induced osteoarthritis rats. Mol. Med. Rep. 2017, 16, 3841–3848. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.S.; Ellman, M.B.; Yan, D.; Kroin, J.S.; Cole, B.J.; Van Wijnen, A.J.; Im, H.-J. A current review of molecular mechanisms regarding osteoarthritis and pain. Gene 2013, 527, 440–447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bove, S.; Calcaterra, S.; Brooker, R.; Huber, C.; Guzman, R.; Juneau, P.; Schrier, D.; Kilgore, K. Weight bearing as a measure of disease progression and efficacy of anti-inflammatory compounds in a model of monosodium iodoacetate-induced osteoarthritis. Osteoarthr. Cartil. 2003, 11, 821–830. [Google Scholar] [CrossRef] [Green Version]
- Woo, Y.J.; Bin Joo, Y.; Jung, Y.O.; Ju, J.H.; La Cho, M.; Oh, H.J.; Jhun, J.Y.; Park, M.K.; Park, J.S.; Kang, C.M.; et al. Grape seed proanthocyanidin extract ameliorates monosodium iodoacetate-induced osteoarthritis. Exp. Mol. Med. 2011, 43, 561–570. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.M.; Son, E.; Kim, S.-H.; Kim, O.S.; Kim, D.-S. Anti-inflammatory and anti-osteoarthritis effect of Mollugo pentaphylla extract. Pharm. Biol. 2019, 57, 73–80. [Google Scholar] [CrossRef] [Green Version]
- Chun, J.M.; Lee, A.Y.; Kim, J.S.; Choi, G.; Kim, S.-H. Protective Effects of Peucedanum japonicum Extract against Osteoarthritis in an Animal Model Using a Combined Systems Approach for Compound-Target Prediction. Nutrients 2018, 10, 754. [Google Scholar] [CrossRef] [Green Version]
- Vincent, T.L. IL-1 in osteoarthritis: Time for a critical review of the literature. F1000Research 2019, 8, 934. [Google Scholar] [CrossRef]
- Miller, R.E.; Miller, R.J.; Malfait, A.-M. Osteoarthritis joint pain: The cytokine connection. Cytokine 2014, 70, 185–193. [Google Scholar] [CrossRef] [Green Version]
- Orita, S.; Ishikawa, T.; Miyagi, M.; Ochiai, N.; Inoue, G.; Eguchi, Y.; Kamoda, H.; Arai, G.; Toyone, T.; Aoki, Y.; et al. Pain-related sensory innervation in monoiodoacetate-induced osteoarthritis in rat knees that gradually develops neuronal injury in addition to inflammatory pain. BMC Musculoskelet. Disord. 2011, 12, 134. [Google Scholar] [CrossRef] [Green Version]
- Kellesarian, S.V.; Al-Kheraif, A.A.; Vohra, F.; Ghanem, A.; Malmstrom, H.; Romanos, G.E.; Javed, F. Cytokine profile in the synovial fluid of patients with temporomandibular joint disorders: A systematic review. Cytokine 2016, 77, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-H.; Woo, C.-H. Effects of Curcumae Longae Rhizoma Pharmacopuncture on Monosodium Iodoacetate-induced Osteoarthritis Rats. J. Korean Med. Rehabil. 2019, 29, 115–133. [Google Scholar] [CrossRef]
- Troeberg, L.; Nagase, H. Proteases involved in cartilage matrix degradation in osteoarthritis. Biochim. Biophys. Acta (BBA) Proteins Proteom. 2012, 1824, 133–145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, Y.J.; Cho, Y.-R.; Oh, J.S.; Ahn, E.-K. Effects of Tribulus terrestris on monosodium iodoacetate-induced osteoarthritis pain in rats. Mol. Med. Rep. 2017, 16, 5303–5311. [Google Scholar] [CrossRef] [Green Version]
- Choi, D.J.; Choi, S.-I.; Choi, B.-R.; Lee, Y.-S.; Lee, D.Y.; Kim, G.-S. Cartilage protective and anti-analgesic effects of ALM16 on monosodium iodoacetate induced osteoarthritis in rats. BMC Complement. Altern. Med. 2019, 19, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Gho, W.G.; Choi, Y.; Park, K.-H.; Huh, J.-K. Expression of collagenases (matrix metalloproteinase-1, 8, 13) and tissue inhibitor of metalloproteinase-1 of retrodiscal tissue in temporomandibular joint disorder patients. J. Korean Assoc. Oral Maxillofac. Surg. 2018, 44, 120–127. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Yun, S.-B.; Shin, S.H.; Jeong, J.M. Effect of Mulberry Extract Complex on Degenerative Arthritis in Vivo Models. J. Korean Soc. Food Sci. Nutr. 2016, 45, 634–641. [Google Scholar] [CrossRef]
- Kim, S.-H.; Choi, H.-J.; Yang, W.-K.; Lee, J.-E.; Cho, J.-H.; Park, I.-J.; Park, S.; Park, B.-K.; Jin, M. Suppressive Effect of the n-Hexane Extract of Litsea japonica Fruit Flesh on Monosodium-Iodoacetate-Induced Osteoarthritis in Rats. Evid. Based Complement. Altern. Med. 2017, 2017, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Mankin, H.J.; Lippiello, L. Biochemical and Metabolic Abnormalities in Articular Cartilage from Osteo-Arthritic Human Hips. J. Bone Jt. Surg. Am. Vol. 1970, 52, 424–434. [Google Scholar] [CrossRef]



| Treatment | Weight Bearing Distribution (%) | |||
|---|---|---|---|---|
| Day 0 | Day 7 | Day 14 | Day 21 | |
| Normal Control | 50.91 ± 0.95 | 49.62 ± 0.60 | 50.58 ± 0.82 | 48.56 ± 0.49 |
| MIA Control | 31.32 ± 2.84 ## | 29.19 ± 3.52 ## | 34.53 ± 1.51 ## | 39.39 ± 1.23 ## |
| LI73014F2 25 mg/kg | 31.13 ± 2.87 | 37.40 ± 2.43 | 38.39 ± 1.29 | 42.67 ± 1.02 * |
| LI73014F2 50 mg/kg | 32.21 ± 3.27 | 38.90 ± 2.97 * | 40.10 ± 1.90 * | 43.19 ± 0.96 * |
| LI73014F2 100 mg/kg | 32.04 ± 2.78 | 38.20 ± 1.85 * | 40.06 ± 1.78 * | 44.95 ± 0.89 ** |
| Ibuprofen 20 mg/kg | 31.32 ± 3.08 | 36.39 ± 2.95 | 41.68 ± 1.08 ** | 45.35 ± 0.66 ** |
| Treatment | Arthritis Index (AI) | |||
|---|---|---|---|---|
| Day 0 | Day 7 | Day 14 | Day 21 | |
| Normal Control | 0.00 | 0.00 | 0.00 | 0.00 |
| MIA Control | 2.00 ± 0.31 ## | 2.06 ± 0.27 ## | 1.54 ± 0.05 ## | 1.50 ± 0.11 ## |
| LI73014F2 25 mg/kg | 1.95 ± 0.20 | 1.70 ± 0.18 | 1.00 ± 0.07 ** | 0.74 ± 0.10 ** |
| LI73014F2 50 mg/kg | 2.00 ± 0.21 | 1.51 ± 0.24 | 1.04 ± 0.10 ** | 0.74 ± 0.10 ** |
| LI73014F2 100 mg/kg | 2.05 ± 0.17 | 1.48 ± 0.15 | 0.99 ± 0.11 ** | 0.71 ± 0.10 ** |
| Ibuprofen 20 mg/kg | 1.95 ± 0.19 | 1.60 ± 0.28 | 1.04 ± 0.07 ** | 0.71 ± 0.11 ** |
Sample Availability: Samples of the compounds are not available from the authors. | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.L.; Lee, H.J.; Lee, D.-R.; Choi, B.-K.; Yang, S.H. Herbal Composition LI73014F2 Alleviates Articular Cartilage Damage and Inflammatory Response in Monosodium Iodoacetate-Induced Osteoarthritis in Rats. Molecules 2020, 25, 5467. https://doi.org/10.3390/molecules25225467
Kim HL, Lee HJ, Lee D-R, Choi B-K, Yang SH. Herbal Composition LI73014F2 Alleviates Articular Cartilage Damage and Inflammatory Response in Monosodium Iodoacetate-Induced Osteoarthritis in Rats. Molecules. 2020; 25(22):5467. https://doi.org/10.3390/molecules25225467
Chicago/Turabian StyleKim, Hae Lim, Hae Jin Lee, Dong-Ryung Lee, Bong-Keun Choi, and Seung Hwan Yang. 2020. "Herbal Composition LI73014F2 Alleviates Articular Cartilage Damage and Inflammatory Response in Monosodium Iodoacetate-Induced Osteoarthritis in Rats" Molecules 25, no. 22: 5467. https://doi.org/10.3390/molecules25225467
APA StyleKim, H. L., Lee, H. J., Lee, D.-R., Choi, B.-K., & Yang, S. H. (2020). Herbal Composition LI73014F2 Alleviates Articular Cartilage Damage and Inflammatory Response in Monosodium Iodoacetate-Induced Osteoarthritis in Rats. Molecules, 25(22), 5467. https://doi.org/10.3390/molecules25225467








