Discovery of Selective SIRT2 Inhibitors as Therapeutic Agents in B-Cell Lymphoma and Other Malignancies
Abstract
:1. Introduction
2. Results
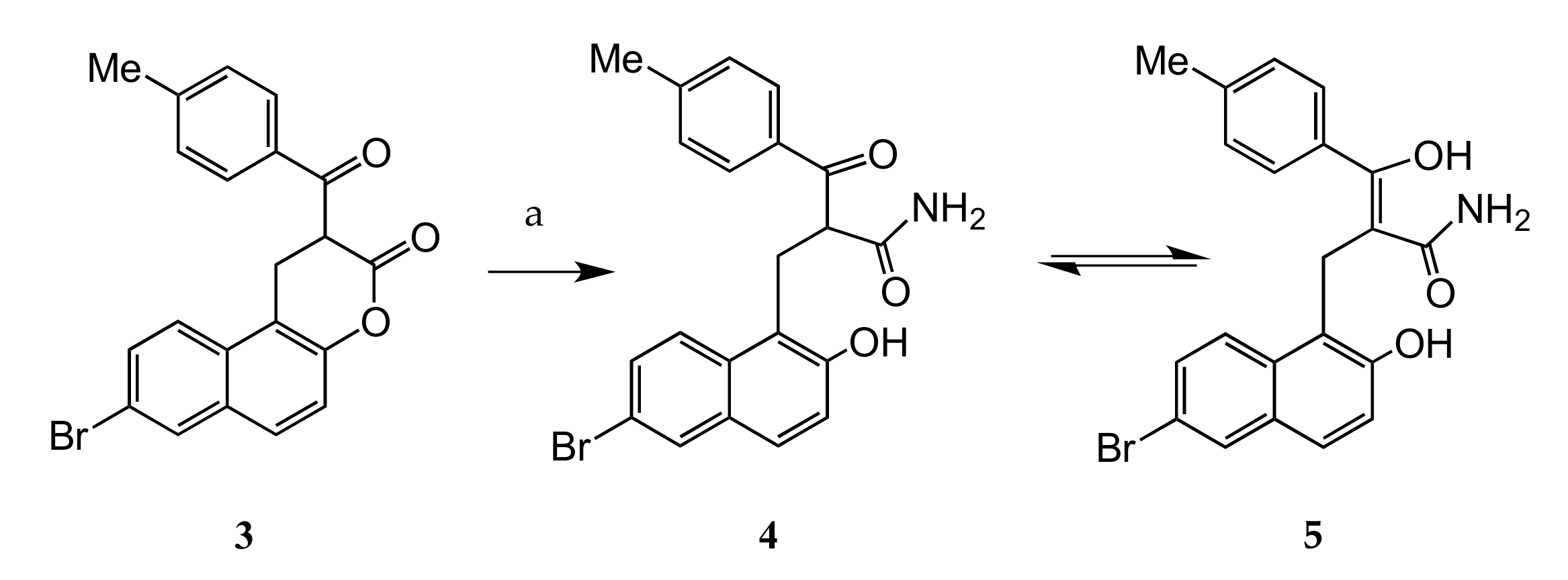
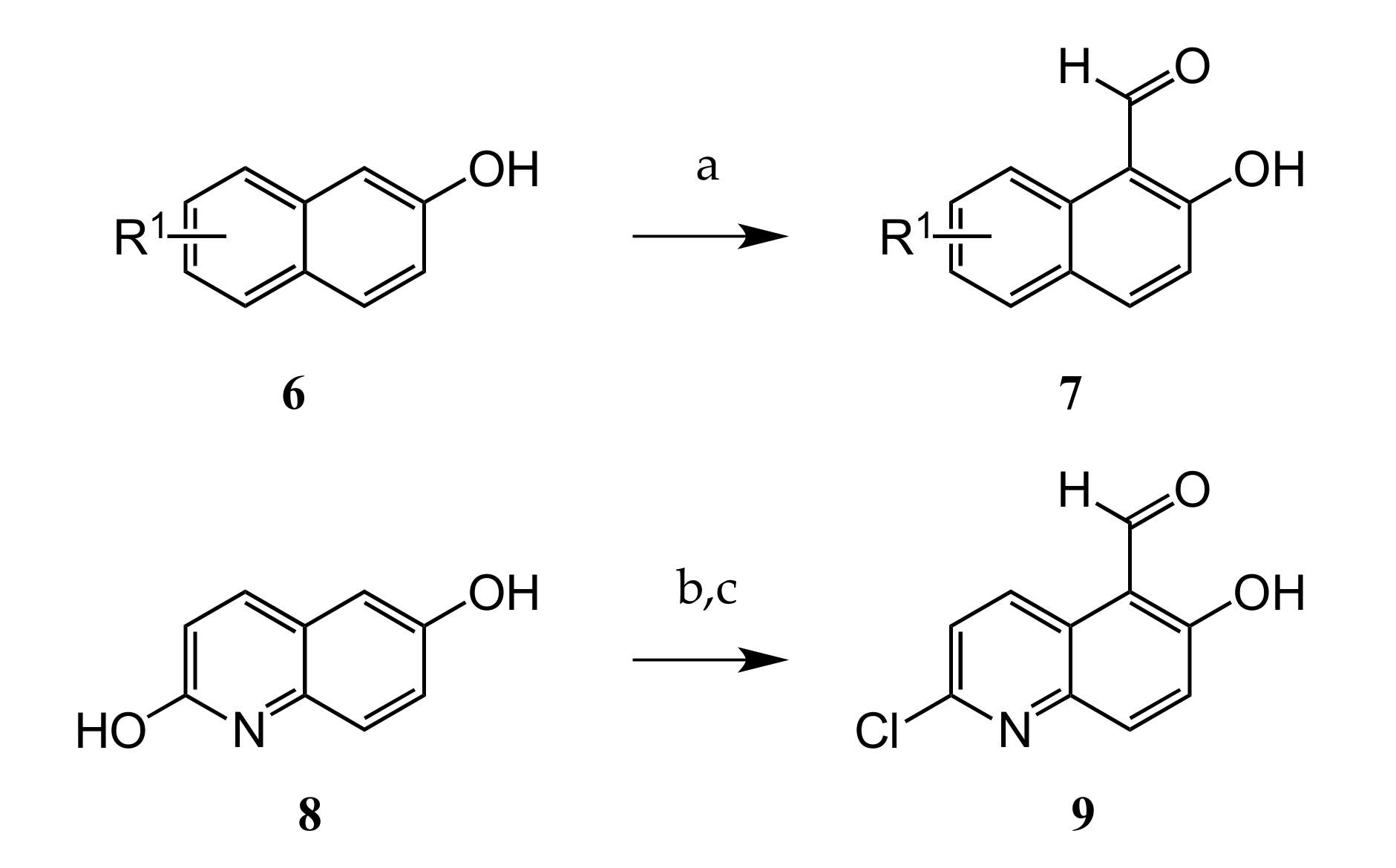
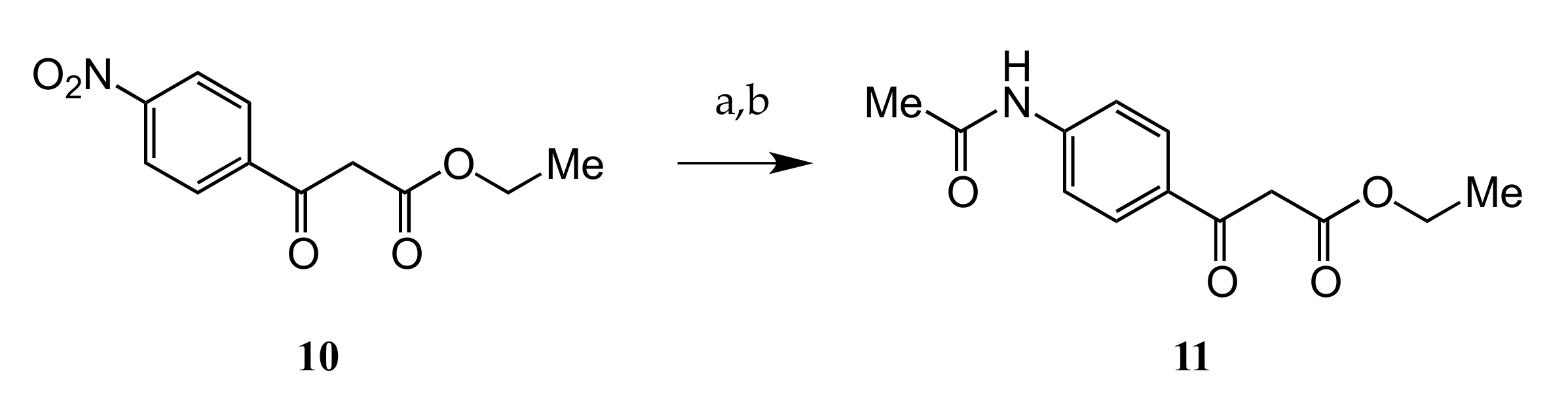
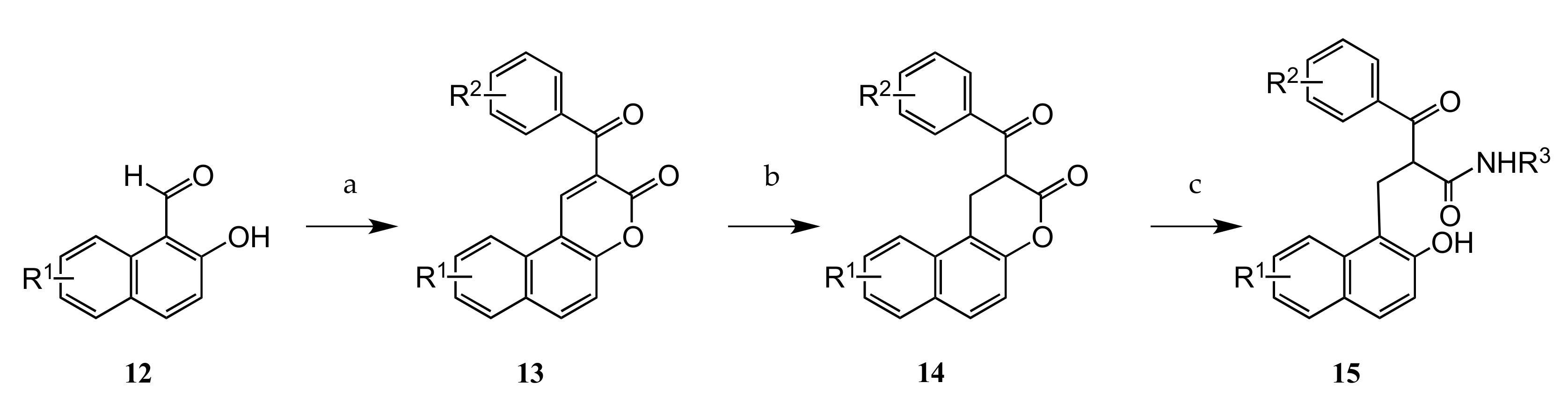
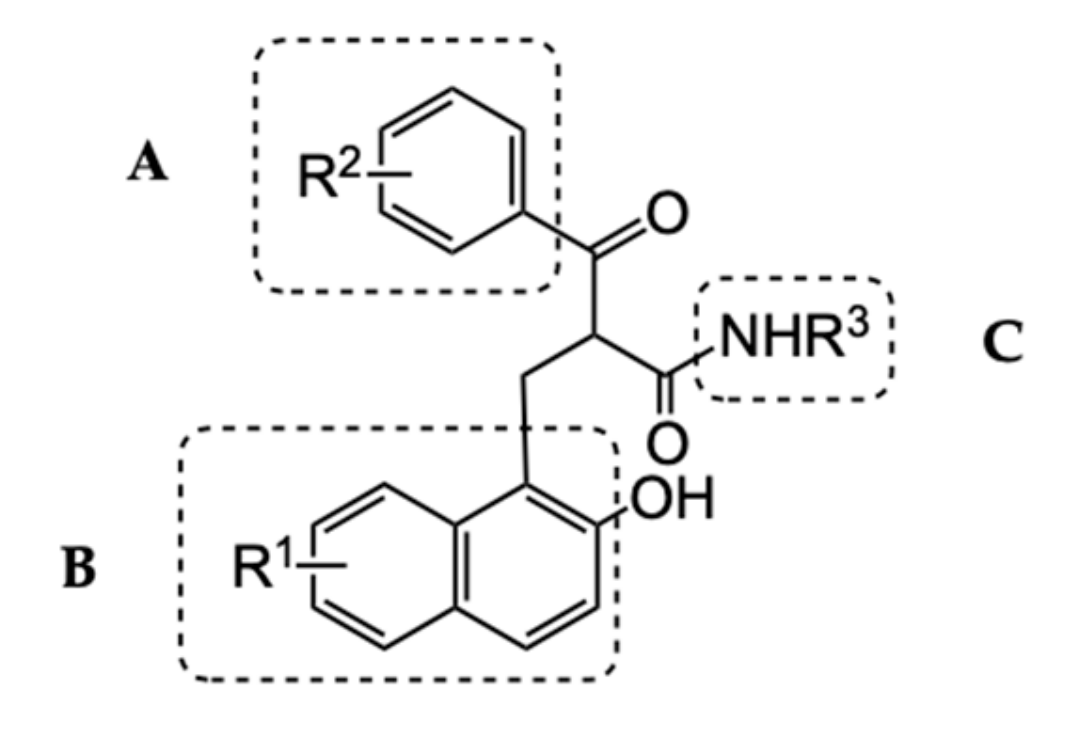
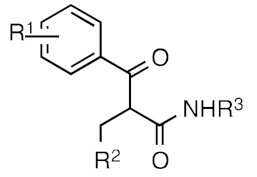
2.1. Chemistry
2.2. Structure Activity Relationship Study (SAR)
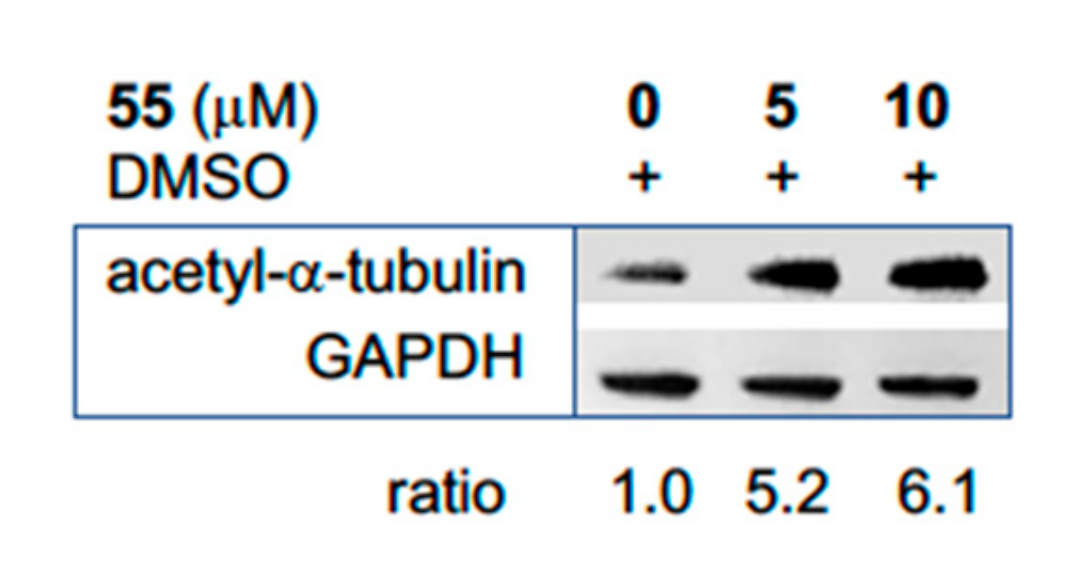
2.3. Biological Evaluation of Sirtuin 2 Inhibitors
2.4. SIRT 2 Inhibitor as Anti-Proliferation and Apoptosis Inducing Agent in OCI-Ly8-LAM53 (OCI) Cells
3. Discussion
4. Materials and Methods
4.1. Enzyme Inhibition Assays
4.2. Cell Viability Assays
4.3. General Chemistry Information
4.4. Representative Procedure (I) for Preparation of Substituted 2-Hydroxy-1-Naphthalene Carbaldehydes (7)
4.5. Representative Procedure (II) for Preparation of Substituted 2-Benzoyl-3H-benzo-[f]chromen-3-ones (13)
4.6. Representative Procedure (III) for Preparation of Substituted 2-(Benzoyl)-1H,2H-naphtho [2,1-b]pyran-3-ones (14)
4.7. Representative Procedure (IV) for Preparation of Substituted 2-[(2-Hydroxynaphthalen-1-yl)methyl]-3-oxo-3-phenylpropanamides
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chalkiadaki, A.; Guarente, L. The multifaceted functions of sirtuins in cancer. Nat. Rev. Cancer 2015, 15, 608–624. [Google Scholar] [CrossRef] [PubMed]
- Imai, S.; Guarente, L. NAD+ and sirtuins in aging and disease. Trends. Cell Biol. 2014, 24, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Dryden, S.C.; Nahhas, F.A.; Nowak, J.E.; Goustin, A.S.; Tainsky, M.A. Role for human SIRT2 NAD-dependent deacetylase activity in control of mitotic exit in the cell cycle. Mol. Cell Biol. 2003, 23, 3173–3185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Oliveira, R.M.; Sarkander, J.; Kazantsev, A.G.; Outeiro, T.F. SIRT2 as a Therapeutic Target for Age-Related Disorders. Front. Pharm. 2012, 3, 82. [Google Scholar] [CrossRef] [Green Version]
- Luthi-Carter, R.; Taylor, D.M.; Pallos, J.; Lambert, E.; Amore, A.; Parker, A.; Moffitt, H.; Smith, D.L.; Runne, H.; Gokce, O.; et al. SIRT2 inhibition achieves neuroprotection by decreasing sterol biosynthesis. Proc. Natl. Acad. Sci. USA 2010, 107, 7927–7932. [Google Scholar] [CrossRef] [Green Version]
- Outeiro, T.F.; Kontopoulos, E.; Altmann, S.M.; Kufareva, I.; Strathearn, K.E.; Amore, A.M.; Volk, C.B.; Maxwell, M.M.; Rochet, J.C.; McLean, P.J.; et al. Sirtuin 2 inhibitors rescue alpha-synuclein-mediated toxicity in models of Parkinson’s disease. Science 2007, 317, 516–519. [Google Scholar] [CrossRef]
- Yang, M.H.; Laurent, G.; Bause, A.S.; Spang, R.; German, N.; Haigis, M.C.; Haigis, K.M. HDAC6 and SIRT2 Regulate the Acetylation State and Oncogenic Activity of Mutant K-RAS. Mol. Cancer Res. 2013, 11, 1072–1077. [Google Scholar] [CrossRef] [Green Version]
- Liu, P.Y.; Xu, N.; Malyukova, A.; Scarlett, C.J.; Sun, Y.T.; Zhang, X.D.; Ling, D.; Su, S.P.; Nelson, C.; Chang, D.K.; et al. The histone deacetylase SIRT2 stabilizes Myc oncoproteins. Cell Death Differ. 2013, 20, 503–514. [Google Scholar] [CrossRef] [Green Version]
- He, X.; Nie, H.; Hong, Y.; Sheng, C.; Xia, W.; Ying, W. SIRT2 activity is required for the survival of C6 glioma cells. Biochem. Biophys. Res. Commun. 2012, 417, 468–472. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Chan, A.W.; To, K.F.; Chen, W.; Zhang, Z.; Ren, J.; Song, C.; Cheung, Y.S.; Lai, P.B.; Cheng, S.H.; et al. SIRT2 overexpression in hepatocellular carcinoma mediates epithelial to mesenchymal transition by protein kinase B/glycogen synthase kinase-3beta/beta-catenin signaling. Hepatology 2013, 57, 2287–2298. [Google Scholar] [CrossRef]
- Vaquero, A.; Scher, M.B.; Lee, D.H.; Sutton, A.; Cheng, H.L.; Alt, F.W.; Serrano, L.; Sternglanz, R.; Reinberg, D. SirT2 is a histone deacetylase with preference for histone H4 Lys 16 during mitosis. Genes Dev. 2006, 20, 1256–1261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- North, B.J.; Marshall, B.L.; Borra, M.T.; Denu, J.M.; Verdin, E. The human Sir2 ortholog, SIRT2, is an NAD+-dependent tubulin deacetylase. Mol. Cell 2003, 11, 437–444. [Google Scholar] [CrossRef]
- Li, Y.Z.; Matsumori, H.; Nakayama, Y.; Osaki, M.; Kojima, H.; Kurimasa, A.; Ito, H.; Mori, S.; Katoh, M.; Oshimura, M.; et al. SIRT2 down-regulation in HeLa can induce p53 accumulation via p38 MAPK activation-dependent p300 decrease, eventually leading to apoptosis. Genes Cells 2011, 16, 34–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Black, J.C.; Mosley, A.; Kitada, T.; Washburn, M.; Carey, M. The SIRT2 deacetylase regulates autoacetylation of p300. Mol. Cell 2008, 32, 449–455. [Google Scholar] [CrossRef] [Green Version]
- Jing, E.; Gesta, S.; Kahn, C.R. SIRT2 regulates adipocyte differentiation through FoxO1 acetylation/deacetylation. Cell Metab. 2007, 6, 105–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, S.N.; Wang, T.S.; Li, X.; Wang, Y.P. SIRT2 activates G6PD to enhance NADPH production and promote leukaemia cell proliferation. Sci. Rep.UK 2016, 6. [Google Scholar] [CrossRef] [Green Version]
- Serrano, L.; Martinez-Redondo, P.; Marazuela-Duque, A.; Vazquez, B.N.; Dooley, S.J.; Voigt, P.; Beck, D.B.; Kane-Goldsmith, N.; Tong, Q.; Rabanal, R.M.; et al. The tumor suppressor SirT2 regulates cell cycle progression and genome stability by modulating the mitotic deposition of H4K20 methylation. Genes Dev. 2013, 27, 639–653. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.S.; Vassilopoulos, A.; Wang, R.H.; Lahusen, T.; Xiao, Z.; Xu, X.L.; Li, C.L.; Veenstra, T.D.; Li, B.; Yu, H.T.; et al. SIRT2 Maintains Genome Integrity and Suppresses Tumorigenesis through Regulating APC/C Activity. Cancer Cell 2011, 20, 487–499. [Google Scholar] [CrossRef] [Green Version]
- Bosch-Presegue, L.; Vaquero, A. The dual role of sirtuins in cancer. Genes Cancer 2011, 2, 648–662. [Google Scholar] [CrossRef]
- Park, S.H.; Zhu, Y.M.; Ozden, O.; Kim, H.S.; Jiang, H.Y.; Deng, C.X.; Gius, D.; Vassilopoulos, A. SIRT2 is a tumor suppressor that connects aging, acetylome, cell cycle signaling, and carcinogenesis. Transl. Cancer Res. 2012, 1, 15–21. [Google Scholar] [CrossRef]
- Byles, V.; Zhu, L.; Lovaas, J.D.; Chmilewski, L.K.; Wang, J.; Faller, D.V.; Dai, Y. SIRT1 induces EMT by cooperating with EMT transcription factors and enhances prostate cancer cell migration and metastasis. Oncogene 2012, 31, 4619–4629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brooks, C.L.; Gu, W. How does SIRT1 affect metabolism, senescence and cancer? Nat. Rev. Cancer 2009, 9, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Alhazzazi, T.Y.; Kamarajan, P.; Verdin, E.; Kapila, Y.L. Sirtuin-3 (SIRT3) and the Hallmarks of Cancer. Genes Cancer 2013, 4, 164–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donmez, G.; Outeiro, T.F. SIRT1 and SIRT2: Emerging targets in neurodegeneration. EMBO Mol. Med. 2013, 5, 344–352. [Google Scholar] [CrossRef]
- Chen, J.; Zhou, Y.; Mueller-Steiner, S.; Chen, L.F.; Kwon, H.; Yi, S.; Mucke, L.; Gan, L. SIRT1 protects against microglia-dependent amyloid-beta toxicity through inhibiting NF-kappaB signaling. J. Biol. Chem. 2005, 280, 40364–40374. [Google Scholar] [CrossRef] [Green Version]
- Li, X. SIRT1 and energy metabolism. Acta Biochim. Biophys Sin. 2013, 45, 51–60. [Google Scholar] [CrossRef] [Green Version]
- Nogueiras, R.; Habegger, K.M.; Chaudhary, N.; Finan, B.; Banks, A.S.; Dietrich, M.O.; Horvath, T.L.; Sinclair, D.A.; Pfluger, P.T.; Tschop, M.H. Sirtuin 1 and sirtuin 3: Physiological modulators of metabolism. Physiol. Rev. 2012, 92, 1479–1514. [Google Scholar] [CrossRef] [Green Version]
- Bedalov, A.; Chowdhury, S.; Simon, J.A. Biology, Chemistry, and Pharmacology of Sirtuins. Methods Enzym. 2016, 574, 183–211. [Google Scholar] [CrossRef]
- Frye, R.A. Phylogenetic classification of prokaryotic and eukaryotic Sir2-like proteins. Biochem. Biophys Res. Commun. 2000, 273, 793–798. [Google Scholar] [CrossRef]
- North, B.J.; Verdin, E. Sirtuins: Sir2-related NAD-dependent protein deacetylases. Genome Biol. 2004, 5, 224. [Google Scholar] [CrossRef] [Green Version]
- Zhao, X.; Allison, D.; Condon, B.; Zhang, F.; Gheyi, T.; Zhang, A.; Ashok, S.; Russell, M.; MacEwan, I.; Qian, Y.; et al. The 2.5 A crystal structure of the SIRT1 catalytic domain bound to nicotinamide adenine dinucleotide (NAD+) and an indole (EX527 analogue) reveals a novel mechanism of histone deacetylase inhibition. J. Med. Chem. 2013, 56, 963–969. [Google Scholar] [CrossRef] [PubMed]
- Peck, B.; Chen, C.Y.; Ho, K.K.; Di Fruscia, P.; Myatt, S.S.; Coombes, R.C.; Fuchter, M.J.; Hsiao, C.D.; Lam, E.W. SIRT inhibitors induce cell death and p53 acetylation through targeting both SIRT1 and SIRT2. Mol. Cancer 2010, 9, 844–855. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirao, M.; Posakony, J.; Nelson, M.; Hruby, H.; Jung, M.; Simon, J.A.; Bedalov, A. Identification of selective inhibitors of NAD+-dependent deacetylases using phenotypic screens in yeast. J. Biol. Chem. 2003, 278, 52773–52782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neugebauer, R.C.; Uchiechowska, U.; Meier, R.; Hruby, H.; Valkov, V.; Verdin, E.; Sippl, W.; Jung, M. Structure-activity studies on splitomicin derivatives as sirtuin inhibitors and computational prediction of binding mode. J. Med. Chem. 2008, 51, 1203–1213. [Google Scholar] [CrossRef]
- Jing, H.; Hu, J.; He, B.; Abril, Y.L.N.; Stupinski, J.; Weiser, K.; Carbonaro, M.; Chiang, Y.L.; Southard, T.; Giannakakou, P.; et al. A SIRT2-Selective Inhibitor Promotes c-Myc Oncoprotein Degradation and Exhibits Broad Anticancer Activity. Cancer Cell 2016, 29, 297–310. [Google Scholar] [CrossRef] [Green Version]
- Cui, H.; Kamal, Z.; Ai, T.; Xu, Y.; More, S.S.; Wilson, D.J.; Chen, L. Discovery of potent and selective sirtuin 2 (SIRT2) inhibitors using a fragment-based approach. J. Med. Chem. 2014, 57, 8340–8357. [Google Scholar] [CrossRef]
- Rumpf, T.; Schiedel, M.; Karaman, B.; Roessler, C.; North, B.J.; Lehotzky, A.; Olah, J.; Ladwein, K.I.; Schmidtkunz, K.; Gajer, M.; et al. Selective Sirt2 inhibition by ligand-induced rearrangement of the active site. Nat. Commun. 2015, 6, 6263. [Google Scholar] [CrossRef]
- Sundriyal, S.; Moniot, S.; Mahmud, Z.; Yao, S.; Di Fruscia, P.; Reynolds, C.R.; Dexter, D.T.; Sternberg, M.J.; Lam, E.W.; Steegborn, C.; et al. Thienopyrimidinone Based Sirtuin-2 (SIRT2)-Selective Inhibitors Bind in the Ligand Induced Selectivity Pocket. J. Med. Chem. 2017, 60, 1928–1945. [Google Scholar] [CrossRef]
- Heltweg, B.; Gatbonton, T.; Schuler, A.D.; Posakony, J.; Li, H.; Goehle, S.; Kollipara, R.; Depinho, R.A.; Gu, Y.; Simon, J.A.; et al. Antitumor activity of a small-molecule inhibitor of human silent information regulator 2 enzymes. Cancer Res. 2006, 66, 4368–4377. [Google Scholar] [CrossRef] [Green Version]
- Mahajan, S.S.; Scian, M.; Sripathy, S.; Posakony, J.; Lao, U.; Loe, T.K.; Leko, V.; Thalhofer, A.; Schuler, A.D.; Bedalov, A.; et al. Development of pyrazolone and isoxazol-5-one cambinol analogues as sirtuin inhibitors. J. Med. Chem. 2014, 57, 3283–3294. [Google Scholar] [CrossRef]
- Vassilopoulos, A.; Fritz, K.S.; Petersen, D.R.; Gius, D. The human sirtuin family: Evolutionary divergences and functions. Hum. Genom. 2011, 5, 485–496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, S.W.; Wang, H.; Poitras, M.F.; Coombs, C.; Bowers, W.J.; Federoff, H.J.; Poirier, G.G.; Dawson, T.M.; Dawson, V.L. Mediation of poly(ADP-ribose) polymerase-1-dependent cell death by apoptosis-inducing factor. Science 2002, 297, 259–263. [Google Scholar] [CrossRef] [PubMed]
- Medda, F.; Joseph, T.L.; Pirrie, L.; Higgins, M.; Slawin, A.M.Z.; Lain, S.; Verma, C.; Westwood, N.J. N1-Benzyl substituted cambinol analogues as isozyme selective inhibitors of the sirtuin family of protein deacetylases. Medchemcomm 2011, 2, 611–615. [Google Scholar] [CrossRef]
- Zhou, W.; Ni, T.K.; Wronski, A.; Glass, B.; Skibinski, A.; Beck, A.; Kuperwasser, C. The SIRT2 Deacetylase Stabilizes Slug to Control Malignancy of Basal-like Breast Cancer. Cell Rep. 2016, 17, 1302–1317. [Google Scholar] [CrossRef] [Green Version]
- Hoffmann, G.; Breitenbucher, F.; Schuler, M.; Ehrenhofer-Murray, A.E. A novel sirtuin 2 (SIRT2) inhibitor with p53-dependent pro-apoptotic activity in non-small cell lung cancer. J. Biol. Chem. 2014, 289, 5208–5216. [Google Scholar] [CrossRef] [Green Version]
- Imaoka, N.; Hiratsuka, M.; Osaki, M.; Kamitani, H.; Kambe, A.; Fukuoka, J.; Kurimoto, M.; Nagai, S.; Okada, F.; Watanabe, T.; et al. Prognostic significance of sirtuin 2 protein nuclear localization in glioma: An immunohistochemical study. Oncol. Rep. 2012, 28, 923–930. [Google Scholar] [CrossRef] [Green Version]
- Amengual, J.E.; Clark-Garvey, S.; Kalac, M.; Scotto, L.; Marchi, E.; Neylon, E.; Johannet, P.; Wei, Y.; Zain, J.; O’Connor, O.A. Sirtuin and pan-class I/II deacetylase (DAC) inhibition is synergistic in preclinical models and clinical studies of lymphoma. Blood 2013, 122, 2104–2113. [Google Scholar] [CrossRef] [Green Version]
- Sayd, S.; Junier, M.P.; Chneiweiss, H. [SIRT2, a multi-talented deacetylase]. Med. Sci. 2014, 30, 532–536. [Google Scholar] [CrossRef] [Green Version]
Sample Availability


 | R1 | R2 | SIRT1 * | SIRT2 * | SIRT3 * | SIRT2 ** |
|---|---|---|---|---|---|---|
| 1 | Cambinol | 54 | 46 | 16 | 59.0 | |
| 4 | 4-Me-phenyl | H | 9.0 | 89 | n.d. | 13.0 |
| 16 | 3-Me-phenyl | H | 38 | 70 | n.d. | n.d. |
| 17 | 2-Me-phenyl | H | 0.0 | 3.0 | n.d. | n.d. |
| 18 | Phenyl | H | 0.0 | 57 | n.d. | n.d. |
| 19 | 4-Chlorophenyl | H | 0.0 | 95 | 30 | 2.79 |
| 20 | 4-Trifluoromethylphenyl | H | 0.0 | 100 | 5.0 | 1.90 |
| 21 | 3-Trifluoromethylphenyl | H | 0.0 | 89 | 15 | 12.6 |
| 22 | 4-Bromophenyl | H | 7.0 | 93 | 42 | 2.50 |
| 23 | 3-Bromophenyl | H | 53 | 91 | n.d. | 8.95 |
| 24 | 4-Methoxyphenyl | H | 34 | 72 | n.d. | n.d. |
| 25 | 4-Fluorophenyl | H | 35 | 96 | 39 | 12.4 |
| 26 | 4-Pyridyl | Me | 13 | 40 | n.d. | n.d. |
| 27 | 3-Pyridyl | Me | 30 | 52 | n.d. | n.d. |
| 28 | 4 Acetamidophenyl | Me | 0.0 | 58 | n.d. | n.d. |
 | R1 | R2 | R3 | SIRT1 * | SIRT2 * | SIRT3 * | SIRT2 ** |
|---|---|---|---|---|---|---|---|
| 23 | 3-Br | 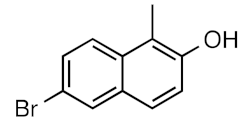 | H | 53 | 91 | n.d. | 8.95 |
| 29 | 3-Br |  | H | 12 | 14 | n.d. | n.d. |
| 30 | 3-Br | 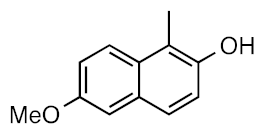 | H | 0.0 | 32 | n.d. | n.d |
| 31 | 3-Br | 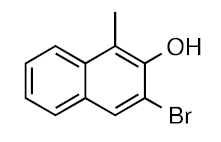 | H | 0.0 | 37 | n.d. | n.d. |
| 32 | 3-Br |  | H | 0.0 | 16 | n.d. | n.d. |
| 33 | 4-CF3 |  | Me | 12 | 97 | 6.0 | 0.59 |
| 34 | 4-CF3 | 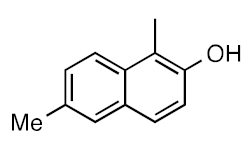 | Me | 0.0 | 97 | >200 | 0.77 |
| 35 | 4-CF3 | 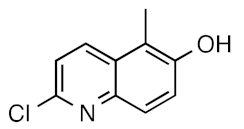 | Me | 0.0 | 84 | >200 | 12.1 |
 | R1 | R2 | SIRT1 * | SIRT2 * | SIRT3 * | SIRT2 ** |
|---|---|---|---|---|---|---|
| 23 | 3-Br | NH2 | 53 | 91 | 41 | 8.95 |
| 36 | 3-Br |  | 0.0 | 94 | 43 | 4.75 |
| 37 | 3-Br | 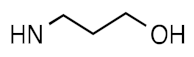 | 28 | 86 | 46 | 7.62 |
| 38 | 3-Br | 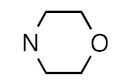 | 1.0 | 22 | n.d. | n.d. |
| 39 | 4-Br | 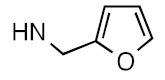 | 13 | 30 | n.d. | n.d. |
| 40 | 4-Br | 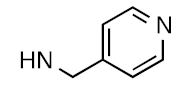 | 23 | 40 | n.d. | n.d. |
| 41 | 3-Br | 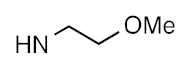 | 0.0 | 53 | n.d. | n.d. |
| 42 | 3-Br | 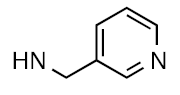 | 3.0 | 6.0 | n.d. | n.d. |
| 43 | 3-Br | 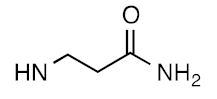 | 0.0 | 89 | 20 | 0.96 |
| 44 | 3-Br |  | 0.0 | 98 | n.d. | 6.50 |
| 20 | 4-CF3 | NH2 | 0.0 | 100 | 5.0 | 1.90 |
| 45 | 4-CF3 |  | 10 | 88 | n.d. | n.d. |
| 46 | 4-CF3 | 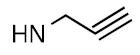 | 28 | 88 | n.d. | n.d. |
| 33 | 4-CF3 | NHMe | 35 | 98 | n.d. | 0.49 |
 | R1 | R2 | SIRT1 * | SIRT2 * | SIRT3 * | SIRT2 ** |
|---|---|---|---|---|---|---|
| 47 | 4-Cl |  | 0.0 | 98 | 5 | 0.96 |
| 48 | 4-Br | 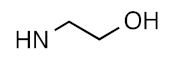 | 18 | 96 | 29 | 0.52 |
| 49 | 4-CF3 | 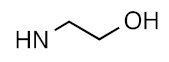 | 15 | 99 | 27 | 0.27 |
| 50 | 4-Cl | 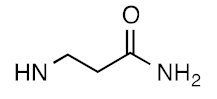 | 4.0 | 99 | 17 | 0.65 |
| 51 | 4-Br | 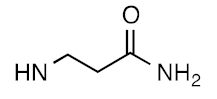 | 20 | 98 | 14 | 0.58 |
| 52 | 4-CF3 | 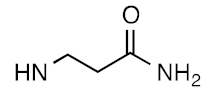 | 0.0 | 93 | 21 | 0.65 |
| 53 | 3-CF3 | 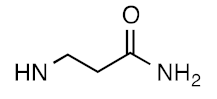 | 8.0 | 91 | 16 | 1.57 |
| 54 | 4-Cl | 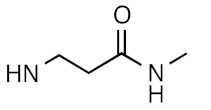 | 12 | 99 | 6 | 0.59 |
| 55 | 4-CF3 |  | 0.0 | 100 | 20 | 0.25 |
| 56 | 4-Br | NHMe | 12 | 95 | 22 | 0.78 |
| Compound | SIRT2 IC50 | Daudi LC50 | Raji | OCI | MCF7 | MDA-MB231 | PC3 | U251 |
|---|---|---|---|---|---|---|---|---|
| 19 | 2.8 | 5.0 | 7.3 | 8.2 | n.d. | n.d. | n.d. | n.d. |
| 22 | 2.5 | 7.0 | 7.8 | 1.6 | n.d. | n.d. | n.d. | n.d. |
| 33 | 0.49 | 14.5 | 18.5 | 16.4 | n.d. | n.d. | n.d. | n.d. |
| 43 | 0.96 | 15.8 | 19.4 | n.d. | n.d. | n.d. | n.d. | n.d. |
| 47 | 0.96 | n.d. | 20.2 | 9.7 | n.d. | n.d. | n.d. | n.d. |
| 48 | 0.52 | 10.5 | 10.0 | 5.0 | 11.8 | 14.7 | 11.8 | 15.8 |
| 49 | 0.27 | 12.0 | 16.5 | 13.1 | 20.2 | 23.5 | 18.4 | 15.7 |
| 50 | 0.65 | n.d. | 19.9 | 11.7 | n.d. | n.d. | n.d. | n.d. |
| 51 | 0.58 | 19.2 | 16.7 | 10.2 | n.d. | n.d. | n.d. | 25.9 |
| 52 | 0.65 | 28.2 | 19.4 | 25.5 | n.d. | n.d. | n.d. | n.d. |
| 54 | 0.59 | 15.8 | 18.5 | 11.2 | 18.0 | 23.8 | 16.5 | 17.3 |
| 55 | 0.25 | 11.9 | 11.9 | 24.9 | 21.6 | 22.8 | 17.2 | 21.1 |
| 56 | 0.78 | 7.1 | 9.1 | 5.7 | n.d. | n.d. | n.d. | n.d. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chowdhury, S.; Sripathy, S.; Webster, A.A.; Park, A.; Lao, U.; Hsu, J.H.; Loe, T.; Bedalov, A.; Simon, J.A. Discovery of Selective SIRT2 Inhibitors as Therapeutic Agents in B-Cell Lymphoma and Other Malignancies. Molecules 2020, 25, 455. https://doi.org/10.3390/molecules25030455
Chowdhury S, Sripathy S, Webster AA, Park A, Lao U, Hsu JH, Loe T, Bedalov A, Simon JA. Discovery of Selective SIRT2 Inhibitors as Therapeutic Agents in B-Cell Lymphoma and Other Malignancies. Molecules. 2020; 25(3):455. https://doi.org/10.3390/molecules25030455
Chicago/Turabian StyleChowdhury, Sarwat, Smitha Sripathy, Alyssa A. Webster, Angela Park, Uyen Lao, Joanne H. Hsu, Taylor Loe, Antonio Bedalov, and Julian A. Simon. 2020. "Discovery of Selective SIRT2 Inhibitors as Therapeutic Agents in B-Cell Lymphoma and Other Malignancies" Molecules 25, no. 3: 455. https://doi.org/10.3390/molecules25030455






