The Therapeutic Potential of Psilocybin
Abstract
1. Introduction
| Diseased State/Condition | Reference | |
|---|---|---|
| 1. | Alcohol dependence | [23,24,25] |
| 2. | Stimulant dependence | [25] |
| 3. | Cocaine addiction | [26,27] |
| 4. | Tobacco addiction | [25,28,29,30] |
| 5. | Nicotine addiction | [26,29] |
| 6. | Opioid addiction | [25] |
| 7. | Cannabis dependence | [25] |
| 8. | Anxiety disorders such as:
| |
| [26] | ||
| [26] | ||
| [31,32] | ||
| [33,34,35,36,37] | ||
| [26] | ||
| [26,38] | ||
| 9. | Cancer-related depression | [33,34,35,36,37,39] |
| 10. | Treatment-resistant depression | [40,41,42,43,44] |
| 11. | Major Depressive Disorder | [45] |
| 12. | Severe existential depression | [26,33,36] |
| 13. | Suicidality (ideation and actual attempts) | [13,46] |
| 14. | Cluster (“suicide”) headaches | [6,47] |
| 15. | Chronic pain | [48,49,50] |
| 16. | Intractable phantom pain | [51] |
| 17. | Demoralization | [52] |
| 18. | Demoralization in older, long-term AIDS survivor men (OLTAS) | [53] |
| 19. | Dysfunctional social cognition | [54] |
| 20. | Maladaptive narcissism | [55] |
| 21. | Borderline Personality Disorder (BPD) | [56,57] |
| 22. | Narcissistic Personality Disorder (NPD) | [58,59,60] |
| 23. | Epilepsy | [61] |
| 24. | Psychopathy | [54] |
| 25. | Emotional dysregulation and violence against one’s partner | [62,63,64] |
| 26. | Inflammation | [49] |
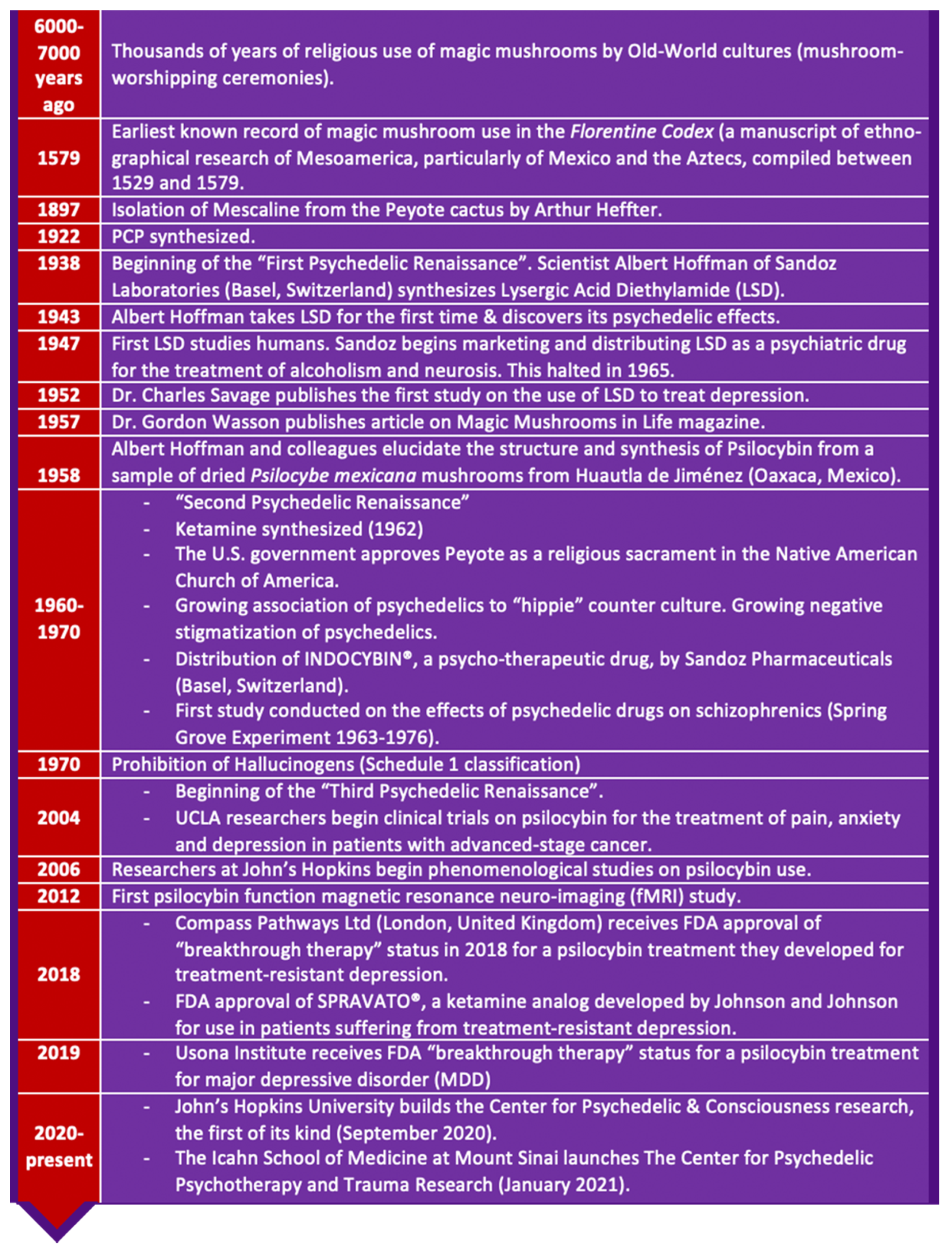
1.1. History
1.2. Transition to Modern-Day Clinical Studies
2. Examples of Psilocybin Producing Mushrooms

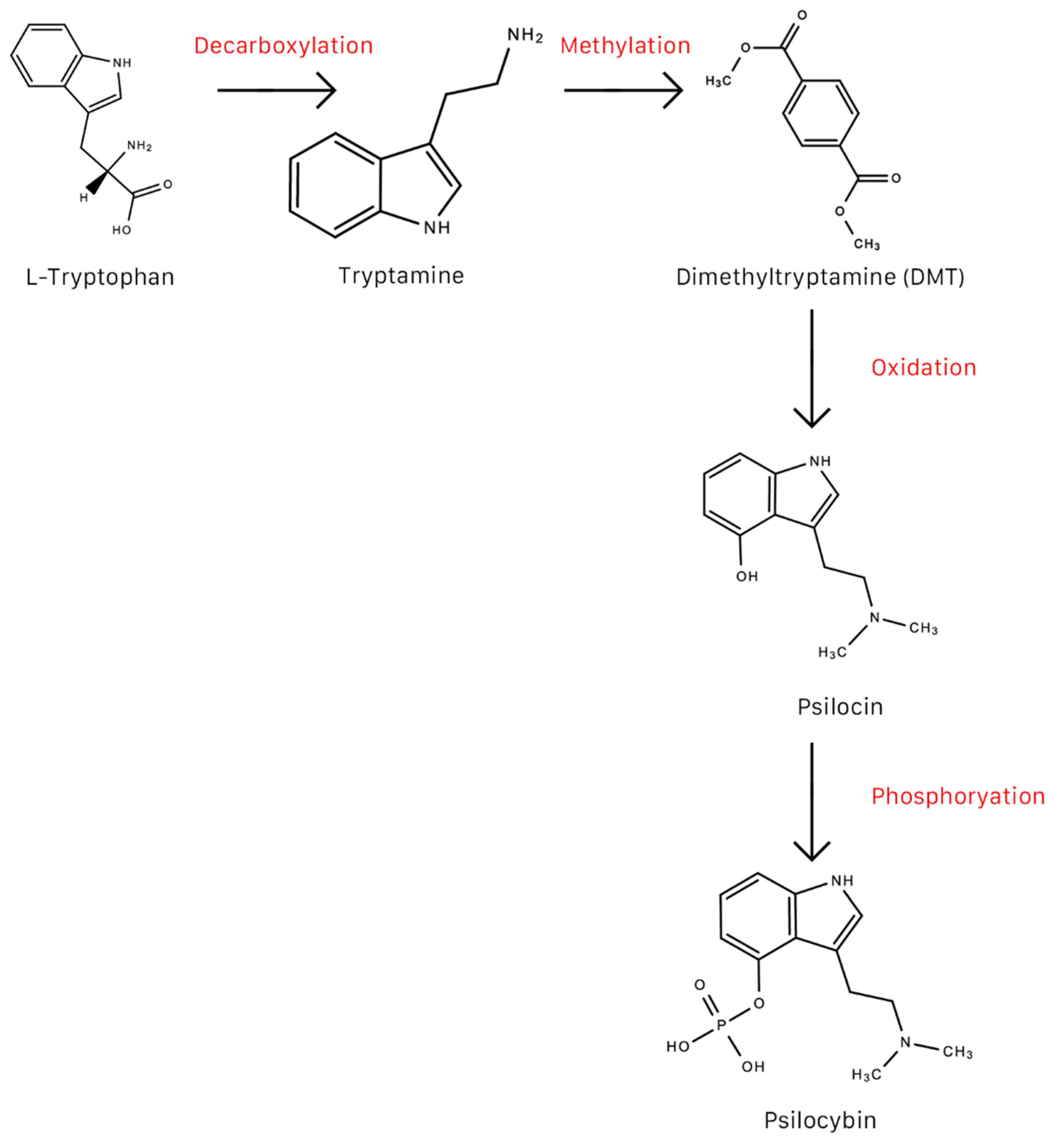
3. Psilocybin Synthesis
3.1. Production of Synthetic Psilocybin
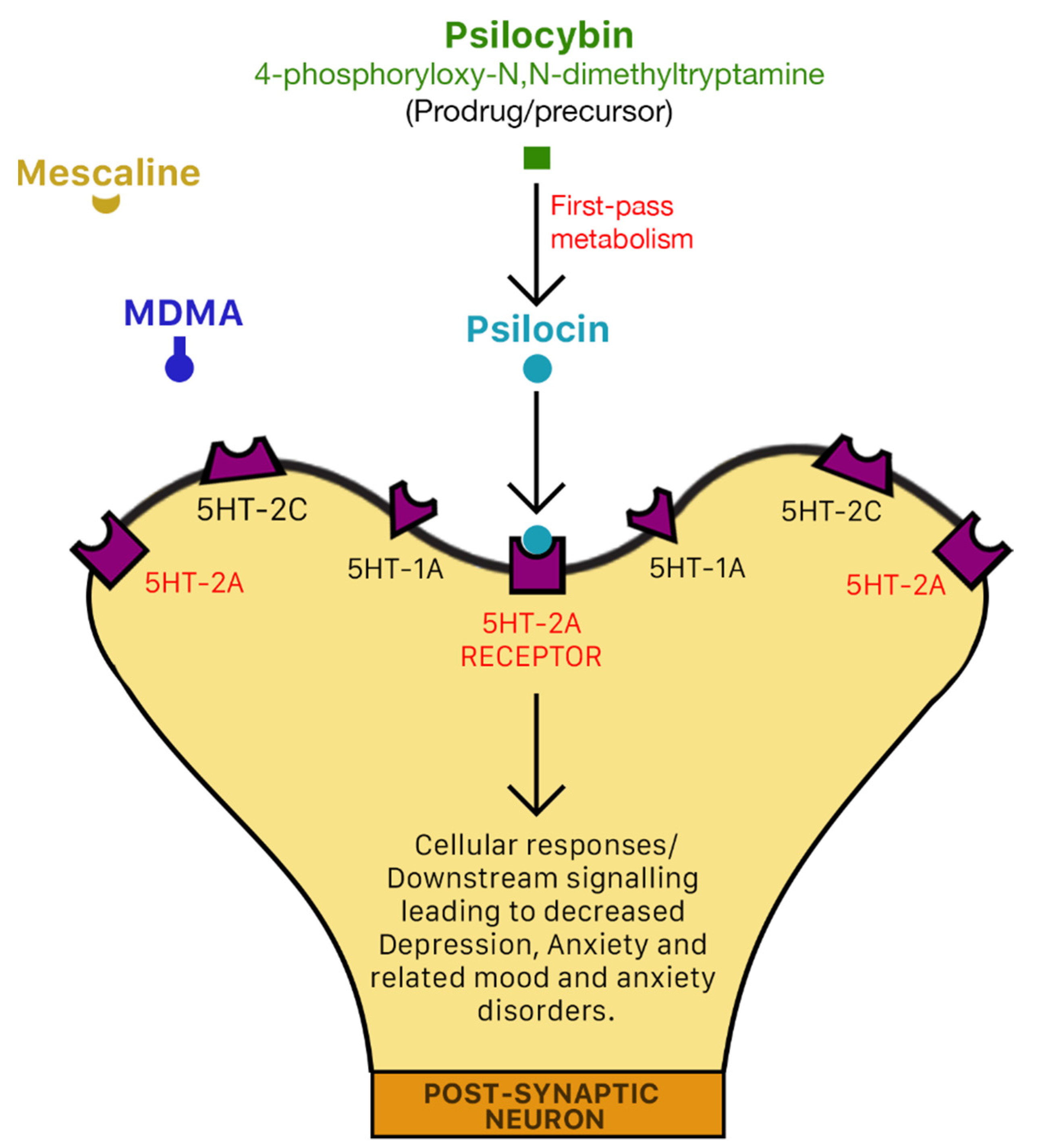
3.2. Mechanism of Action of Psilocybin
3.3. Effects of Magic Mushrooms
3.4. The Possible Entourage Effect Phenomena in Magic Mushrooms
3.5. Adverse Effects, Risks and Contraindications
3.6. Pharmacokinetics of Psilocin
4. Economic Analysis of Neuropharmaceuticals Market
5. Conclusions and Future Direction
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- Dyck, E. Flashback: Psychiatric Experimentation with LSD in Historical Perspective. Can. J. Psychiatry 2005, 50, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.W.; Griffiths, R.R. Potential Therapeutic Effects of Psilocybin. Neurotherapeutics 2017, 14, 734–740. [Google Scholar] [CrossRef] [PubMed]
- Buddy, T. The Types of Dissociative Drugs. 2020. Available online: https://www.verywellmind.com/what-are-dissociative-drugs-63387 (accessed on 23 March 2021).
- NIDA. What Are the Effects of Common Dissociative Drugs on the Brain and Body? 2020. Available online: https://www.drugabuse.gov/publications/research-reports/hallucinogens-dissociative-drugs/what-are-effects-common-dissociative-drugs-brain-body (accessed on 23 March 2021).
- Passie, T.; Seifert, J.; Schneider, U.; Emrich, H.M. The pharmacology of psilocybin. Addict. Biol. 2002, 7, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Schindler, E.A.D.; Gottschalk, C.H.; Weil, M.J.; Shapiro, R.E.; Wright, D.A.; Sewell, R.A. Indoleamine Hallucinogens in Cluster Headache: Results of the Clusterbusters Medication Use Survey. J. Psychoact. Drugs 2015, 47, 372–381. [Google Scholar] [CrossRef] [PubMed]
- Halberstadt, A.L.; Geyer, M.A. Multiple receptors contribute to the behavioral effects of indoleamine hallucinogens. Neuropharmacology 2011, 61, 364–381. [Google Scholar] [CrossRef]
- Beliveau, V.; Ganz, M.; Feng, L.; Ozenne, B.; Højgaard, L.; Fisher, P.M.; Svarer, C.; Greve, D.N.; Knudsen, G.M. A high-resolution in vivo atlas of the human brain’s serotonin system. J. Neurosci. 2017, 37, 120–128. [Google Scholar] [CrossRef]
- Canal, C.E. Serotonergic Psychedelics: Experimental Approaches for Assessing Mechanisms of Action; New Psychoactive Substances; Springer Science and Business Media LLC: Berlin/Heidelberg, Germany, 2018; Volume 252, pp. 227–260. [Google Scholar]
- Nichols, D.E.; Nichols, C.D. Serotonin Receptors. Chem. Rev. 2008, 108, 1614–1641. [Google Scholar] [CrossRef]
- Hoyer, D.; Clarke, D.E.; Fozard, J.R.; Hartig, P.R.; Martin, G.R.; Mylecharane, E.J.; Saxena, P.R.; Humphrey, P.P. International Union of Pharmacology classification of receptors for 5-hydroxytryptamine (Serotonin). Pharmacol. Rev. 1994, 46, 157–203. [Google Scholar]
- Frazer, A.; Hensler, J.G. Serotonin. Basic Neurochem. 1999, 6, 335–346. [Google Scholar]
- Hendricks, P.S.; Johnson, M.W.; Griffiths, R.R. Psilocybin, psychological distress, and suicidality. J. Psychopharmacol. 2015, 29, 1041–1043. [Google Scholar] [CrossRef]
- Elflein, J. Psychedelic therapy—Statistics & Facts. 2018. Available online: https://www.statista.com/topics/4277/psychedelic-therapy/ (accessed on 23 March 2021).
- Zamaria, J.A. A Phenomenological Examination of Psilocybin and its Positive and Persisting Aftereffects. NeuroQuantology 2016, 14. [Google Scholar] [CrossRef]
- Stafford, P. Psychedelics Encyclopedia, Third ed.; Ronin Publishing: Berkeley, CA, USA, 2013. [Google Scholar]
- WHO. Mental Disorders. 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed on 24 March 2021).
- Rehm, J.; Shield, K.D. Global Burden of Disease and the Impact of Mental and Addictive Disorders. Curr. Psychiatry Rep. 2019, 21. [Google Scholar] [CrossRef] [PubMed]
- WHO. World Mental Health Day: An Opportunity to Kick-Start a Massive scale-Up in Investment in Mental Health. 2020. Available online: https://www.who.int/news/item/27-08-2020-world-mental-health-day-an-opportunity-to-kick-start-a-massive-scale-up-in-investment-in-mental-health (accessed on 24 March 2021).
- Ritchie, H.; Roser, M. 2018. Mental Health. Available online: https://ourworldindata.org/mental-health (accessed on 24 March 2021).
- WHO. Suicide. 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/suicide (accessed on 24 March 2021).
- PAHO. COVID-19 Pandemic Exacerbates Suicide Risk Factors. 2020. Available online: https://www.paho.org/en/news/10-9-2020-covid-19-pandemic-exacerbates-suicide-risk-factors (accessed on 24 March 2021).
- Bogenschutz, M.P.; Forcehimes, A.A.; Pommy, J.A.; Wilcox, C.E.; Barbosa, P.C.R.; Strassman, R.J. Psilocybin-assisted treatment for alcohol dependence: A proof-of-concept study. J. Psychopharmacol. 2015, 29, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.; McAndrew, A.; Stevens, T.; Nutt, D.; Lawn, W. Tripping up addiction: The use of psychedelic drugs in the treatment of problematic drug and alcohol use. Curr. Opin. Behav. Sci. 2017, 13, 71–76. [Google Scholar] [CrossRef]
- Garcia-Romeu, A.; Griffiths, R.; Johnson, W.M. Psilocybin-occasioned mystical experiences in the treatment of tobacco addiction. Curr. Drug Abuse Rev. 2014, 7, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Daniel, J.; Haberman, M. Clinical potential of psilocybin as a treatment for mental health conditions. Ment. Health Clin. 2017, 7, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Lawrence, A.J. Drugs currently in Phase II clinical trials for cocaine addiction. Expert Opin. Investig. Drugs 2014, 23, 1105–1122. [Google Scholar] [CrossRef]
- Johnson, M.W.; Garcia-Romeu, A.; Cosimano, M.P.; Griffiths, R.R. Pilot study of the 5-HT2AR agonist psilocybin in the treatment of tobacco addiction. J. Psychopharmacol. 2014, 28, 983–992. [Google Scholar] [CrossRef]
- Johnson, M.W.; Garcia-Romeu, A.; Johnson, P.S.; Griffiths, R.R. An online survey of tobacco smoking cessation associated with naturalistic psychedelic use. J. Psychopharmacol. 2017, 31, 841–850. [Google Scholar] [CrossRef]
- Johnson, M.W.; Garcia-Romeu, A.; Griffiths, R.R. Long-term follow-up of psilocybin-facilitated smoking cessation. Am. J. Drug Alcohol Abus. 2017, 43, 55–60. [Google Scholar] [CrossRef]
- Wilcox, J.A. Psilocybin and Obsessive Compulsive Disorder. J. Psychoact. Drugs 2014, 46, 393–395. [Google Scholar] [CrossRef] [PubMed]
- Moreno, F.A.; Wiegand, C.B.; Taitano, E.K.; Delgado, P.L. Safety, tolerability, and efficacy of psilocybin in 9 patients with obsessive-compulsive disorder. J. Clin. Psychiatry 2006, 67, 1735–1740. [Google Scholar] [CrossRef] [PubMed]
- Grob, C.S.; Danforth, A.L.; Chopra, G.S.; Hagerty, M.; McKay, C.R.; Halberstadt, A.L.; Greer, G.R. Pilot Study of Psilocybin Treatment for Anxiety in Patients with Advanced-Stage Cancer. Arch. Gen. Psychiatry 2011, 68, 71–78. [Google Scholar] [CrossRef]
- Griffiths, R.R.; Johnson, M.W.; A Carducci, M.; Umbricht, A.; A Richards, W.; Richards, B.D.; Cosimano, M.P.; A Klinedinst, M. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: A randomized double-blind trial. J. Psychopharmacol. 2016, 30, 1181–1197. [Google Scholar] [CrossRef] [PubMed]
- Ross, S.; Bossis, A.; Guss, J.; Agin-Liebes, G.; Malone, T.; Cohen, B.; Mennenga, S.E.; Belser, A.; Kalliontzi, K.; Babb, J.; et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: A randomized controlled trial. J. Psychopharmacol. 2016, 30, 1165–1180. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, D. Psilocybin-assisted psychotherapy for dying cancer patients—aiding the final trip. J. Psychopharmacol. 2016, 30, 1215–1217. [Google Scholar] [CrossRef]
- Swift, T.C.; Belser, A.B.; Agin-Liebes, G.; Devenot, N.; Terrana, S.; Friedman, H.L.; Guss, J.; Bossis, A.P.; Ross, S. Cancer at the Dinner Table: Experiences of Psilocybin-Assisted Psychotherapy for the Treatment of Cancer-Related Distress. J. Humanist. Psychol. 2017, 57, 488–519. [Google Scholar] [CrossRef]
- Shelton, R.C.; Hendricks, P.S. Psilocybin and palliative end-of-life care. J. Psychopharmacol. 2016, 30, 1207–1208. [Google Scholar] [CrossRef]
- Malone, T.C.; Mennenga, S.E.; Guss, J.; Podrebarac, S.K.; Owens, L.T.; Bossis, A.P.; Belser, A.B.; Agin-Liebes, G.; Bogenschutz, M.P.; Ross, S. Individual Experiences in Four Cancer Patients Following Psilocybin-Assisted Psychotherapy. Front. Pharmacol. 2018, 9. [Google Scholar] [CrossRef]
- Lyons, T.; Carhart-Harris, R.L. Increased nature relatedness and decreased authoritarian political views after psilocybin for treatment-resistant depression. J. Psychopharmacol. 2018, 32, 811–819. [Google Scholar] [CrossRef]
- Carhart-Harris, R.L.; Bolstridge, M.; Rucker, J.; Day, C.M.J.; Erritzoe, D.; Kaelen, M.; Bloomfield, M.; A Rickard, J.; Forbes, B.; Feilding, A.; et al. Psilocybin with psychological support for treatment-resistant depression: An open-label feasibility study. Lancet Psychiatry 2016, 3, 619–627. [Google Scholar] [CrossRef]
- Beck, S. Psilocybin-Assisted Psychotherapy: Treating Depression and Anxiety with Mushrooms. Physician Assist. Stud. Stud. Artic. 2020, 7. [Google Scholar] [CrossRef]
- Reynolds, C.F., III. Psilocybin-Assisted Supportive Psychotherapy in the Treatment of Major Depression—Quo Vadis? JAMA Psychiatry 2020. [Google Scholar] [CrossRef] [PubMed]
- Roseman, L.; Nutt, D.J.; Carhart-Harris, R.L. Quality of Acute Psychedelic Experience Predicts Therapeutic Efficacy of Psilocybin for Treatment-Resistant Depression. Front. Pharmacol. 2018, 8. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.K.; Barrett, F.S.; May, D.G.; Cosimano, M.P.; Sepeda, N.D.; Johnson, M.W.; Finan, P.H.; Griffiths, R.R. Effects of Psilocybin-Assisted Therapy on Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry 2020. [Google Scholar] [CrossRef] [PubMed]
- Zeifman, R.J.; Wagner, A.C.; Watts, R.; Kettner, H.; Mertens, L.J.; Carhart-Harris, R.L. Post-Psychedelic Reductions in Experiential Avoidance Are Associated with Decreases in Depression Severity and Suicidal Ideation. Front. Psychiatry 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- Sewell, R.A.; Halpern, J.H.; Pope, H.G. Response of cluster headache to psilocybin and LSD. Neurology 2006, 66, 1920–1922. [Google Scholar] [CrossRef]
- Whelan, A.; Johnson, M.I. Lysergic acid diethylamide and psilocybin for the management of patients with persistent pain: A potential role? Pain Manag. 2018, 8, 217–229. [Google Scholar] [CrossRef]
- Nkadimeng, S.M.; Nabatanzi, A.; Steinmann, C.M.L.; Eloff, J.N. Phytochemical, Cytotoxicity, Antioxidant and Anti-Inflammatory Effects of Psilocybe Natalensis Magic Mushroom. Plants 2020, 9, 1127. [Google Scholar] [CrossRef]
- Castellanos, J.P.; Woolley, C.; Bruno, K.A.; Zeidan, F.; Halberstadt, A.; Furnish, T. Chronic pain and psychedelics: A review and proposed mechanism of action. Reg. Anesth. Pain Med. 2020, 45, 486–494. [Google Scholar] [CrossRef]
- Ramachandran, V.; Chunharas, C.; Marcus, Z.; Furnish, T.; Lin, A. Relief from intractable phantom pain by combining psilocybin and mirror visual-feedback (MVF). Neurocase 2018, 24, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Hendricks, P.S. Psilocybin-assisted group therapy: A new hope for demoralization. EClinicalMedicine 2020, 27. [Google Scholar] [CrossRef] [PubMed]
- Anderson, B.T.; Danforth, A.; Daroff, R.; Stauffer, C.; Ekman, E.; Agin-Liebes, G.; Trope, A.; Boden, M.T.; Dilley, J.; Mitchell, J.; et al. Psilocybin-assisted group therapy for demoralized older long-term AIDS survivor men: An open-label safety and feasibility pilot study. EClinicalMedicine 2020, 27. [Google Scholar] [CrossRef]
- Pokorny, T.; Preller, K.H.; Kometer, M.; Dziobek, I.; Vollenweider, F.X. Effect of Psilocybin on Empathy and Moral Decision-Making. Int. J. Neuropsychopharmacol. 2017, 20, 747–757. [Google Scholar] [CrossRef]
- Van Mulukom, V.; Patterson, R.E.; van Elk, M. Broadening Your Mind to Include Others: The relationship between serotonergic psychedelic experiences and maladaptive narcissism. Psychopharmacology 2020, 237, 1–13. [Google Scholar] [CrossRef]
- Zeifman, R.J.; Wagner, A.C. Exploring the case for research on incorporating psychedelics within interventions for borderline personality disorder. J. Context. Behav. Sci. 2020, 15, 1–11. [Google Scholar] [CrossRef]
- Healy, M. Feeling rejected? Mushrooms could help. Available online: https://www.latimes.com/science/sciencenow/la-sci-social-rejection-psilocybin-mushrooms-20160418-story.html (accessed on 26 April 2021).
- Dolan, E.W. Awe-inspiring psychedelic trips reduce narcissism by boosting connectedness and empathy, study suggests. Available online: https://www.psypost.org/2020/10/awe-inspiring-psychedelic-trips-reduce-narcissism-by-boosting-connectedness-and-empathy-study-suggests-58277 (accessed on 26 April 2021).
- Lennon, A. Psychedelic Experiences Reduce Narcissistic Personality Traits. 2020. Available online: https://www.labroots.com/trending/neuroscience/18989/psychedelic-experiences-reduce-narcissistic-personality-traits (accessed on 24 March 2021).
- Combstrong, A. Has Science Found a Cure for Narcissism? 2020. Available online: https://medium.com/happy-brain-club/finally-a-cure-for-narcissism-b8d36d51a518 (accessed on 24 March 2021).
- Meldrum, B.; Naquet, R. Effects of psilocybin, dimethyltryptamine, mescaline and various lysergic acid derivatives on the EEG and on photically induced epilepsy in the baboon (Papio papio). Electroencephalogr. Clin. Neurophysiol. 1971, 31, 563–572. [Google Scholar] [CrossRef]
- Thiessen, M.S.; Walsh, Z.; Bird, B.M.; Lafrance, A. Psychedelic use and intimate partner violence: The role of emotion regulation. J. Psychopharmacol. 2018, 32, 749–755. [Google Scholar] [CrossRef] [PubMed]
- Inaba, D.; Cohen, W.E. Uppers, Downers, All Arounders: Physical and Mental Effects of Psychoactive Drugs, 7th ed.; CNS Productions: Medford, OR, USA, 2014. [Google Scholar]
- Krediet, E.; Bostoen, T.; Breeksema, J.; van Schagen, A.; Passie, T.; Vermetten, E. Reviewing the Potential of Psychedelics for the Treatment of PTSD. Int. J. Neuropsychopharmacol. 2020, 23, 385–400. [Google Scholar] [CrossRef] [PubMed]
- Nichols, D.E. Psilocybin: From ancient magic to modern medicine. J. Antibiot. 2020, 73, 679–686. [Google Scholar] [CrossRef]
- Heffter, A. Ueber Pellote. Arch. Exp. Pathol. Pharmakol. 1898, 40, 385–429. [Google Scholar] [CrossRef]
- Schultes, R.E. Hallucinogens of Plant Origin. Science 1969, 163, 245–254. [Google Scholar] [CrossRef]
- Mithoefer, M.C.; Grob, C.S.; Brewerton, T.D. Novel psychopharmacological therapies for psychiatric disorders: Psilocybin and MDMA. Lancet Psychiatry 2016, 3, 481–488. [Google Scholar] [CrossRef]
- Brenan, J.P.M.; Schultes, R.E.; Hofmann, A. Plants of the Gods: Origins of Hallucinogenic Use. Kew Bull. 1980, 35, 708. [Google Scholar] [CrossRef][Green Version]
- Carod-Artal, F.J. Hallucinogenic drugs in pre-Columbian Mesoamerican cultures. Neurologia (Barcelona, Spain) 2015, 30, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, A. LSD, My Problem Child: Reflections on Sacred Drugs, Mysticism, and Science, 4th ed.; Multidisciplinary Association for Psychedelic Studies (MAPS): Santa Cruz, CA, USA, 2009. [Google Scholar]
- Thomas, K.; Malcolm, B.; Lastra, D. Psilocybin-Assisted Therapy: A Review of a Novel Treatment for Psychiatric Disorders. J. Psychoact. Drugs 2017, 49, 446–455. [Google Scholar] [CrossRef] [PubMed]
- Davies, B. Lysergic acid (LSD 25) and ritalin in the treatment of neurosis. J. Psychosom. Res. 1964, 8, 164–165. [Google Scholar] [CrossRef]
- Johnson, F.G. LSD in the Treatment of Alcoholism. Am. J. Psychiatry 1969, 126, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, A.; Levine, J.; Stark, L.; Lazar, R. A Clinical Study of LSD Treatment in Alcoholism. Am. J. Psychiatry 1969, 126, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Smart, R.G.; Storm, T. The efficacy of LSD in the treatment of alcoholism. Q. J. Stud. Alcohol 1964, 25, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Visotsky, H.M. LSD and alcoholism: A clinical study of treatment efficacy. J. Chronic Dis. 1971, 24, 597. [Google Scholar] [CrossRef]
- Jordy, S.S. Book Reviews—LSD and alcoholism; a clinical study of treatment efficacy. Q. J. Stud. Alcohol 1971, 32, 589–592. [Google Scholar] [CrossRef]
- Dahlberg, C.C. Lysergic Acid Diethylamide (LSD) in the Treatment of Alcoholism. Arch. Gen. Psychiatry 1968, 19, 508–510. [Google Scholar] [CrossRef]
- Abuzzahab, F.S.; Anderson, B.J. A review of LSD treatment in alcoholism. Int. Pharm. 1971, 6, 223–235. [Google Scholar] [CrossRef]
- Dyck, E. LSD: A new treatment emerging from the past. CMAJ Can. Med Assoc. J. J. l’Association Med Can. 2015, 187, 1079–1080, Advance online publication. [Google Scholar] [CrossRef]
- Rice, M.E.; Harris, G.T.; Cormier, C.A. An evaluation of a maximum security therapeutic community for psychopaths and other mentally disordered offenders. Law Hum. Behav. 1992, 16, 399–412. [Google Scholar] [CrossRef]
- Harris, G.T.; Rice, M.; Cormier, C.A. Psychopaths: Is a therapeutic community therapeutic? Int. J. Ther. Supportive Organ. 1994, 15, 283–300. [Google Scholar]
- Reidy, D.E.; Kearns, M.C.; Degue, S. Reducing psychopathic violence: A review of the treatment literature. Aggress. Violent Behav. 2013, 18, 527–538. [Google Scholar] [CrossRef] [PubMed]
- Bender, L.; Goldschmidt, L.; Sankar, D. Treatment of autistic schizophrenic children with LSD-25 and UML-491. Recent Adv. Biol. Psychiatry 1961, 4, 170–179. [Google Scholar] [PubMed]
- Bender, L. D-lysergic acid in the treatment of the biological features of childhood schizophrenia. Dis. Nerv. Syst. 1966, 7 (Suppl. 7), 43–46. [Google Scholar]
- Freedman, A.; Ebin, E.V.; Wilson, E.A. Autistic schizophrenic children. An experiment in the use of d-lysergic acid diethylamide (LSD-25). Arch. Gen. Psychiatry 1962, 6, 203–213. [Google Scholar] [CrossRef]
- Simmons, J.Q.; Benor, D.; Daniel, D. The variable effects of LSD-25 on the behavior of a heterogeneous group of childhood schizophrenics. Behav. Neuropsychiatry 1972, 4, 10–24. [Google Scholar]
- Moller, H. The treatment of childhood schizophrenia in a public school system. Psychol. Sch. 1964, 1, 297–304. [Google Scholar] [CrossRef]
- Ball, J.R.; Armstrong, J.J. The Use of L.S.D. 25 (D-Lysergic Acid Diethylamide) in the Treatment of the Sexual Perversions. Can. Psychiatr. Assoc. J. 1961, 6, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Simmons, J.Q.; Leiken, S.J.; Lovaas, O.I.; Schaeffer, B.; Perloff, B. Modification of autistic behavior with LSD-25. Am. J. Psychiatry 1966, 122, 1201–1211. [Google Scholar] [CrossRef]
- Sigafoos, J.; Green, V.A.; Edrisinha, C.; Lancioni, G.E. Flashback to the 1960s: LSD in the treatment of autism. Dev. Neurorehabilit. 2007, 10, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Honigfeld, G. Temporal effects of LSD-25 and epinephrine on verbal behavior. PsycEXTRA Dataset 1964, 70, 303–306. [Google Scholar] [CrossRef]
- Hofmann, A.; Heim, R.; Brack, A.; Kobel, H. Psilocybin, ein psychotroper Wirkstoff aus dem mexikanischen RauschpilzPsilocybe mexicana Heim. Experientia 1958, 14, 107–109. [Google Scholar] [CrossRef] [PubMed]
- Timothy, L.; Ralph, M.; Madison, P.; Gunther, W.; Ralph, S.; Sara, K. A new behavior change program using psilocybin. Psychotherapy 1965, 2, 61–72. [Google Scholar] [CrossRef]
- Keusch, S.; Turk, A.; Saxer, S.; Ehlken, N.; Grunig, E.; Ulrich, S. Rehabilitation in patients with pulmonary arterial hypertension. Swiss Med. Week. 2017, 147, w14462. [Google Scholar]
- Leary, T. The effects of consciousness-expanding drugs on prisoner rehabilitation. Psychedelic Rev. 1969, 10, 29–45. [Google Scholar]
- Doblin, R. Pahnke’s "Good Friday experiment": A long-term follow-up and methodological critique. J. Transpers. Psychol. 1991, 23, 1–28. [Google Scholar]
- Kargbo, R.B. Psilocybin Therapeutic Research: The Present and Future Paradigm. ACS Med. Chem. Lett. 2020, 11, 399–402. [Google Scholar] [CrossRef] [PubMed]
- Hoch, P.H.; Cattell, J.P.; Pennes, H.H. Effects of mescaline and lysergic acid (d-LSD-25). Am. J. Psychiatry 1952, 108, 579–584. [Google Scholar] [CrossRef] [PubMed]
- Wong, S. Mind menders: How psychedelic drugs rebuild broken brains. 2017. Available online: https://www.newscientist.com/article/mg23631530-300-mind-menders-how-psychedelic-drugs-rebuild-broken-brains/ (accessed on 25 March 2021).
- Griffiths, R.R.; Richards, W.A.; McCann, U.; Jesse, R. Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology 2006, 187, 268–283. [Google Scholar] [CrossRef] [PubMed]
- Johns Hopkins Center for Psychedelic & Consciousness Research: Publications. Available online: https://hopkinspsychedelic.org/publications (accessed on 27 April 2021).
- Compass Pathways. Treatment Resistant Depression & Clinical Trials: COMPASS. 2021. Available online: https://compasspathways.com/our-research/psilocybin-therapy/clinical-trials/treatment-resistant-depression/ (accessed on 25 March 2021).
- Bahr, R.; Lopez, A.; A Rey, J. Intranasal Esketamine (SpravatoTM) for Use in Treatment-Resistant Depression In Conjunction With an Oral Antidepressant. P T Peer-Rev. J. Formul. Manag. 2019, 44, 340–375. [Google Scholar]
- Business Wire. FDA Grants Breakthrough Therapy Designation to Usona Institute’s psilocybin program for major depressive disorder. 2019. Available online: https://www.businesswire.com/news/home/20191122005452/en/FDA-grants-Breakthrough-Therapy-Designation-to-Usona-Institutes-psilocybin-program-for-major-depressive-disorder (accessed on 25 March 2021).
- Stamets, P.; Weil, A. Psilocybin Mushrooms of the World: An Identification Guide, 1st ed.; Ten Speed Press: Berkeley, CA, USA, 1996. [Google Scholar]
- Johns Hopkins University. 2021. Available online: https://hopkinspsychedelic.org/ (accessed on 25 March 2021).
- Newswire, P. Global Psychedelic Therapeutics Market, 2020-2030. 2020. Available online: https://www.prnewswire.com/news-releases/global-psychedelic-therapeutics-market-2020-2030-301148314.html (accessed on 25 March 2021).
- Griffiths, R.R.; Hurwitz, E.S.; Davis, A.K.; Johnson, M.W.; Jesse, R. Survey of subjective “God encounter experiences”: Comparisons among naturally occurring experiences and those occasioned by the classic psychedelics psilocybin, LSD, ayahuasca, or DMT. PLoS ONE 2019, 14, e0214377. [Google Scholar] [CrossRef]
- Barrett, F.S.; Doss, M.K.; Sepeda, N.D.; Pekar, J.J.; Griffiths, R.R. Emotions and brain function are altered up to one month after a single high dose of psilocybin. Sci. Rep. 2020, 10, 2214. [Google Scholar] [CrossRef]
- Barrett, F.S.; Krimmel, S.R.; Griffiths, R.R.; Seminowicz, D.A.; Mathur, B.N. Psilocybin acutely alters the functional connectivity of the claustrum with brain networks that support perception, memory, and attention. NeuroImage 2020, 218. [Google Scholar] [CrossRef]
- Carbonaro, T.M.; Johnson, M.W.; Griffiths, R.R. Subjective features of the psilocybin experience that may account for its self-administration by humans: A double-blind comparison of psilocybin and dextromethorphan. Psychopharmacology 2020, 237, 2293–2304. [Google Scholar] [CrossRef]
- Network Newswire. Multi-Billion-Dollar Market Forecast in Psychedelic Therapeutics. 2020. Available online: https://www.networknewswire.com/multi-billion-dollar-market-forecast-in-psychedelic-therapeutics/ (accessed on 25 March 2021).
- Garcia-Romeu, A.; Barrett, F.S.; Carbonaro, T.M.; Johnson, M.W.; Griffiths, R.R. Optimal dosing for psilocybin pharmacotherapy: Considering weight-adjusted and fixed dosing approaches. J. Psychopharmacol. 2021, 35, 353–361. [Google Scholar] [CrossRef]
- Usona Institute. A Study of Psilocybin for Major Depressive Disorder (MDD); ClinicalTrials.gov Identifier: NCT03866174. 2021. Available online: https://clinicaltrials.gov/ct2/show/NCT03866174 (accessed on 25 March 2021).
- Vollenweider, F.X.; Leenders, K.L.; Scharfetter, C.; Maguire, P.; Stadelmann, O.; Angst, J. Positron Emission Tomography and Fluorodeoxyglucose Studies of Metabolic Hyperfrontality and Psychopathology in the Psilocybin Model of Psychosis. Neuropsychopharmacology 1997, 16, 357–372. [Google Scholar] [CrossRef]
- Gouzoulis-Mayfrank, E.; Schreckenberger, M.; Sabri, O.; Arning, C.; Thelen, B.; Spitzer, M.; Kovar, K.-A.; Hermle, L.; Büll, U.; Sass, H. Neurometabolic Effects of Psilocybin, 3,4-Methylenedioxyethylamphetamine (MDE) and d-Methamphetamine in Healthy Volunteers A Double-Blind, Placebo-Controlled PET Study with [18F]FDG. Neuropsychopharmacology 1999, 20, 565–581. [Google Scholar] [CrossRef]
- Hasler, F.; Grimberg, U.; Benz, M.A.; Huber, T.; Vollenweider, F.X. Acute psychological and physiological effects of psilocybin in healthy humans: A double-blind, placebo-controlled dose?effect study. Psychopharmacology 2004, 172, 145–156. [Google Scholar] [CrossRef]
- Carter, O.L.; Hasler, F.; Pettigrew, J.D.; Wallis, G.M.; Liu, G.B.; Vollenweider, F.X. Psilocybin links binocular rivalry switch rate to attention and subjective arousal levels in humans. Psychopharmacology 2007, 195, 415–424. [Google Scholar] [CrossRef]
- Griffiths, R.R.; Richards, W.A.; Johnson, M.W.; McCann, U.D.; Jesse, R. Mystical-type experiences occasioned by psilocybin mediate the attribution of personal meaning and spiritual significance 14 months later. J. Psychopharmacol. 2008, 22, 621–632. [Google Scholar] [CrossRef]
- Doblin, R. Dr. Leary’s Concord Prison Experiment: A 34-Year Follow-up Study. J. Psychoact. Drugs 1998, 30, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Leary, T.; Litwin, G.H.; Metzner, R. Reactions to psilocybjn administered in a supportive environment. J. Nerv. Ment. Dis. 1963, 137, 561–573. [Google Scholar] [CrossRef] [PubMed]
- Kelmendi, B.; Corlett, P.; Ranganathan, M.; D’Souza, C.; Krystal, J.H. The role of psychedelics in palliative care reconsidered: A case for psilocybin. J. Psychopharmacol. 2016, 30, 1212–1214. [Google Scholar] [CrossRef] [PubMed]
- Guss, J.; Krause, R.; Sloshower, J. The Yale Manual for Psilocybin-Assisted Therapy of Depression (using Acceptance and Commitment Therapy as a Therapeutic Frame). PsyArXiv 2020. [Google Scholar] [CrossRef]
- Yale University. Psilocybin for the Treatment of Cluster Headache. 2021. Available online: https://clinicaltrials.gov/ct2/show/NCT02981173 (accessed on 25 March 2021).
- Yale University. Psilocybin—Induced Neuroplasticity in the Treatment of Major Depressive Disorder. 2021. Available online: https://clinicaltrials.gov/ct2/show/NCT03554174 (accessed on 25 March 2021).
- Petranker, R.; Kim, J.; Anderson, T. Microdosing as a response to the meaning crisis. PsyArXiv 2020. [Google Scholar] [CrossRef]
- Petranker, R.; Anderson, T.; Maier, L.J.; Barratt, M.J.; A Ferris, J.; Winstock, A.R. Microdosing psychedelics: Subjective benefits and challenges, substance testing behavior, and the relevance of intention. J. Psychopharmacol. 2020. [Google Scholar] [CrossRef]
- Psyence. 2021. Available online: https://www.psyence.com/ (accessed on 25 March 2021).
- Rockefeller, A. Psilocybe cubensis (Earle) Singer (345579). 2013. Available online: https://mushroomobserver.org/image/show_image/345579?obs=138685 (accessed on 26 March 2021).
- Alfonso, W. Psilocybe caerulescens Murrill. 2020. Available online: https://mushroomobserver.org/417062?q=1aXNX (accessed on 26 March 2021).
- Rockefeller, A. Psilocybe mexicana R. Heim. 2014. Available online: https://mushroomobserver.org/168203?q=1aXOX (accessed on 26 March 2021).
- Stewart, T. Psilocybe caerulipes (Peck) Sacc. 2019. Available online: https://mushroomobserver.org/380223?q=1aTcf (accessed on 26 March 2021).
- Rockefeller, A. Psilocybe stuntzii Guzmán & J. Ott. 2014. Available online: https://mushroomobserver.org/image/show_image/465307?obs=181566&q=1aXRI (accessed on 26 March 2021).
- Psilocybe cyanescens Wakef. 2020. Available online: https://mushroomobserver.org/440264?q=1aJM3 (accessed on 26 March 2021).
- Brown, C. Psilocybe azurescens Stamets & Gartz. 2019. Available online: https://mushroomobserver.org/394045?q=1aM7H (accessed on 26 March 2021).
- Psilocybe pelliculosa (A.H. Sm.) Singer & A.H. 2020. Available online: https://mushroomobserver.org/439276?q=1aXUf (accessed on 26 March 2021).
- Psilocybe tampanensis Guzmán & Pollock. 2013. Available online: https://mushroomobserver.org/140217?q=1aXVZ (accessed on 26 March 2021).
- Brown, C. Psilocybe baeocystis Singer & A.H. Sm. 2013. Available online: https://mushroomobserver.org/149218?q=1aXWC (accessed on 26 March 2021).
- Rockefeller, A. Psilocybe hoogshagenii R. Heim 2017. Available online: https://mushroomobserver.org/284430?q=1aXXY (accessed on 26 March 2021).
- Hasler, F.; Bourquin, D.; Brenneisen, R.; Bär, T.; Vollenweider, F.X. Determination of psilocin and 4-hydroxyindole-3-acetic acid in plasma by HPLC-ECD and pharmacokinetic profiles of oral and intravenous psilocybin in man. Pharm. Acta Helv. 1997, 72, 175–184. [Google Scholar] [CrossRef]
- Tylš, F.; Pálenîcek, T.; Horácek, J. Psilocybin Summary of knowledge and new perspectives. Eur. Neuropsychopharmacol. 2014, 24, 342–356. [Google Scholar] [CrossRef] [PubMed]
- Nichols, D.E. Psychedelics. Pharmacol. Rev. 2016, 68, 264–355. [Google Scholar] [CrossRef] [PubMed]
- Horita, A. Some biochemical studies on psilocybin and psilogin. J. Neuropsychiatr. 1963, 4, 270–273. [Google Scholar] [PubMed]
- Fricke, J.; Kargbo, R.; Regestein, L.; Lenz, C.; Peschel, G.; Rosenbaum, M.A.; Sherwood, A.; Hoffmeister, D. Scalable Hybrid Synthetic/Biocatalytic Route to Psilocybin. Chem. A Eur. J. 2020, 26, 8281–8285. [Google Scholar] [CrossRef]
- Nichols, D.E. Improvements to the Synthesis of Psilocybin and a Facile Method for Preparing the O-Acetyl Prodrug of Psilocin. Synthesis 1999, 1999, 935–938. [Google Scholar] [CrossRef]
- Ullrich, R.; Hofrichter, M. Enzymatic hydroxylation of aromatic compounds. Cell. Mol. Life Sci. 2007, 64, 271–293. [Google Scholar] [CrossRef]
- Londesbrough, D.J.; Brown, C.; Northen, J.S.; Moore, G.; Patil, H.; Nichols, D. Preparation of Psilocybin, Different Polymorphic Forms, Intermediates, Formulations and Their. Use. Patent Number WO2019073379A1, 18 April 2019. [Google Scholar]
- Sliwoski, V. This Psilocybin Patent could be a Really Big Deal. 2020. Available online: https://harrisbricken.com/cannalawblog/this-psilocybin-patent-could-be-a-really-big-deal/ (accessed on 27 March 2021).
- Fricke, J.; Blei, F.; Hoffmeister, D. Enzymatic Synthesis of Psilocybin. Angew. Chem. Int. Ed. 2017, 56, 12352–12355. [Google Scholar] [CrossRef]
- Hoefgen, S.; Lin, J.; Fricke, J.; Stroe, M.C.; Mattern, D.J.; Kufs, J.E.; Hortschansky, P.; Brakhage, A.A.; Hoffmeister, D.; Valiante, V. Facile assembly and fluorescence-based screening method for heterologous expression of biosynthetic pathways in fungi. Metab. Eng. 2018, 48, 44–51. [Google Scholar] [CrossRef]
- Adams, A.M.; Kaplan, N.A.; Wei, Z.; Brinton, J.D.; Monnier, C.S.; Enacopol, A.L.; Ramelot, T.A.; Jones, J.A. In vivo production of psilocybin in E. coli. Metab. Eng. 2019, 56, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Milne, N.; Thomsen, P.; Mølgaard Knudsen, N.; Rubaszka, P.; Kristensen, M.; Borodina, I. Metabolic engineering of Saccharomyces cerevisiae for the de novo production of psilocybin and related tryptamine derivatives. Metab. Eng. 2020, 60, 25–36. [Google Scholar] [CrossRef]
- Borodina, I.; Nielsen, J. Advances in metabolic engineering of yeast Saccharomyces cerevisiae for production of chemicals. Biotechnol. J. 2014, 9, 609–620. [Google Scholar] [CrossRef]
- Hassan, Z.; Bosch, O.G.; Singh, D.; Narayanan, S.; Kasinather, B.V.; Seifritz, E.; Kornhuber, J.; Quednow, B.B.; Müller, C.P. Novel Psychoactive Substances—Recent Progress on Neuropharmacological Mechanisms of Action for Selected Drugs. Front. Psychiatry 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Chávez-Castillo, M.; Núñez, V.; Nava, M.; Ortega, Á.; Rojas, M.; Bermúdez, V.; Rojas-Quintero, J. Depression as a Neuroendocrine Disorder: Emerging Neuropsychopharmacological Approaches beyond Monoamines. Adv. Pharmacol. Sci. 2019, 2019, 1–20. [Google Scholar] [CrossRef]
- Mahapatra, A.; Gupta, R. Role of psilocybin in the treatment of depression. Ther. Adv. Psychopharmacol. 2017, 7, 54–56. [Google Scholar] [CrossRef] [PubMed]
- Holtzheimer, P.E.; Mayberg, H.S. Stuck in a rut: Rethinking depression and its treatment. Trends Neurosci. 2011, 34, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Grimm, O.; Kraehenmann, R.; Preller, K.; Seifritz, E.; Vollenweider, F. Psilocybin modulates functional connectivity of the amygdala during emotional face discrimination. Eur. Neuropsychopharmacol. 2018, 28, 691–700. [Google Scholar] [CrossRef] [PubMed]
- Tagliazucchi, E.; Carhart-Harris, R.; Leech, R.; Nutt, D.; Chialvo, D.R. Enhanced repertoire of brain dynamical states during the psychedelic experience. Hum. Brain Mapp. 2014, 35, 5442–5456. [Google Scholar] [CrossRef] [PubMed]
- Lord, L.-D.; Expert, P.; Atasoy, S.; Roseman, L.; Rapuano, K.; Lambiotte, R.; Nutt, D.J.; Deco, G.; Carhart-Harris, R.L.; Kringelbach, M.L.; et al. Dynamical exploration of the repertoire of brain networks at rest is modulated by psilocybin. NeuroImage 2019, 199, 127–142. [Google Scholar] [CrossRef] [PubMed]
- Müller, F.; Liechti, M.E.; Lang, U.E.; Borgwardt, S. Advances and challenges in neuroimaging studies on the effects of serotonergic hallucinogens: Contributions of the resting brain. Prog. Brain Res. 2018, 242, 159–177. [Google Scholar] [PubMed]
- Bortolozzi, A.; Masana, M.; Díaz-Mataix, L.; Cortés, R.; Scorza, M.C.; Gingrich, J.A.; Toth, M.; Artigas, F. Dopamine release induced by atypical antipsychotics in prefrontal cortex requires 5-HT1A receptors but not 5-HT2A receptors. Int. J. Neuropsychopharmacol. 2010, 13, 1299–1314. [Google Scholar] [CrossRef] [PubMed]
- De Veen, B.T.; Schellekens, A.F.; Verheij, M.M.; Homberg, J.R. Psilocybin for treating substance use disorders? Expert Rev. Neurother. 2016, 17, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Nagaeva, E.; Zubarev, I.; Gonzales, C.B.; Forss, M.; Nikouei, K.; De Miguel, E.; Elsilä, L.; Linden, A.-M.; Hjerling-Leffler, J.; Augustine, G.J.; et al. Heterogeneous somatostatin-expressing neuron population in mouse ventral tegmental area. eLife 2020, 9. [Google Scholar] [CrossRef] [PubMed]
- Dailly, E.; Chenu, F.; Renard, C.E.; Bourin, M. Dopamine, depression and antidepressants. Fundam. Clin. Pharmacol. 2004, 18, 601–607. [Google Scholar] [CrossRef]
- Vollenweider, F.X.; Vontobel, P.; Hell, D.; Leenders, K.L. 5-HT Modulation of Dopamine Release in Basal Ganglia in Psilocybin-Induced Psychosis in Man—A PET Study with [11C]raclopride. Neuropsychopharmacology 1999, 20, 424–433. [Google Scholar] [CrossRef]
- Maust, D.T.; Bonar, E.E.; Ilgen, M.A.; Blow, F.C.; Kales, H.C. Agitation in Alzheimer Disease as a Qualifying Condition for Medical Marijuana in the United States. Am. J. Geriatr. Psychiatry 2016, 24, 1000–1003. [Google Scholar] [CrossRef]
- Grandjean, J.; Buehlmann, D.; Buerge, M.; Sigrist, H.; Seifritz, E.; Vollenweider, F.X.; Pryce, C.R.; Rudin, M. Psilocybin exerts distinct effects on resting state networks associated with serotonin and dopamine in mice. NeuroImage 2021, 225. [Google Scholar] [CrossRef]
- Carhart-Harris, R.L.; Erritzoe, D.; Williams, T.; Stone, J.M.; Reed, L.J.; Colasanti, A.; Tyacke, R.J.; Leech, R.; Malizia, A.L.; Murphy, K.; et al. Neural correlates of the psychedelic state as determined by fMRI studies with psilocybin. Proc. Natl. Acad. Sci. USA 2012, 109, 2138–2143. [Google Scholar] [CrossRef]
- Sakashita, Y.; Abe, K.; Katagiri, N.; Kambe, T.; Saitoh, T.; Utsunomiya, I.; Horiguchi, Y.; Taguchi, K. Effect of Psilocin on Extracellular Dopamine and Serotonin Levels in the Mesoaccumbens and Mesocortical Pathway in Awake Rats. Biol. Pharm. Bull. 2015, 38, 134–138. [Google Scholar] [CrossRef]
- Coull, J.T.; Cheng, R.-K.; Meck, W.H. Neuroanatomical and Neurochemical Substrates of Timing. Neuropsychopharmacology 2010, 36, 3–25. [Google Scholar] [CrossRef] [PubMed]
- Hindley, G.; Beck, K.; Borgan, F.; Ginestet, C.E.; McCutcheon, R.; Kleinloog, D.; Ganesh, S.; Radhakrishnan, R.; D’Souza, D.C.; Howes, O.D. Psychiatric symptoms abused by cannabis constituents: A systematic review and meta-analysis. Lancet Psychiatry 2020, 7, 344–353. [Google Scholar] [CrossRef]
- Carhart-Harris, R.L.; Roseman, L.; Bolstridge, M.; Demetriou, L.; Pannekoek, J.N.; Wall, M.B.; Tanner, M.; Kaelen, M.; McGonigle, J.; Murphy, K. Psilocybin for treatment-resistant depression: fMRI-measured brain mechanisms. Sci. Rep. 2017, 7. [Google Scholar] [CrossRef]
- Geyer, M.A. Lysergic Acid Diethylamide and Psilocybin Revisited. Biol. Psychiatry 2015, 78, 516–518. [Google Scholar] [CrossRef] [PubMed]
- Kraehenmann, R.; Preller, K.H.; Scheidegger, M.; Pokorny, T.; Bosch, O.G.; Seifritz, E.; Vollenweider, F.X. Psilocybin-Induced Decrease in Amygdala Reactivity Correlates with Enhanced Positive Mood in Healthy Volunteers. Biol. Psychiatry 2015, 78, 572–581. [Google Scholar] [CrossRef] [PubMed]
- Kraehenmann, R.; Schmidt, A.; Friston, K.; Preller, K.H.; Seifritz, E.; Vollenweider, F.X. The mixed serotonin receptor agonist psilocybin reduces threat-induced modulation of amygdala connectivity. Neuroimage Clin. 2016, 11, 53–60. [Google Scholar] [CrossRef]
- DeRubeis, R.J.; Siegle, G.J.; Hollon, S.D. Cognitive therapy versus medication for depression: Treatment outcomes and neural mechanisms. Nat. Rev. Neurosci. 2008, 9, 788–796. [Google Scholar] [CrossRef]
- Magic Mushrooms and the Amygdala. 2014. Available online: https://www.neuroscientificallychallenged.com/blog/2014/5/12/magic-mushrooms-and-the-amygdala (accessed on 30 March 2021).
- Mertens, L.J.; Wall, M.B.; Roseman, L.; Demetriou, L.; Nutt, D.J.; Carhart-Harris, R.L. Therapeutic mechanisms of psilocybin: Changes in amygdala and prefrontal functional connectivity during emotional processing after psilocybin for treatment-resistant depression. J. Psychopharmacol. 2020, 34, 167–180. [Google Scholar] [CrossRef]
- Stroud, J.B.; Freeman, T.P.; Leech, R.; Hindocha, C.; Lawn, W.; Nutt, D.; Curran, H.; Carhart-Harris, R.L. Psilocybin with psychological support improves emotional face recognition in treatment-resistant depression. Psychopharmacol. 2018, 235, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Creese, I.; Burt, D.R.; Synder, S.H.; Snyder, S.H. The dopamine receptor: Differential binding of d-LSD and related agents to agonist and antagonist states. Life Sci. 1975, 17, 1715–1719. [Google Scholar] [CrossRef]
- Roseman, L.; Leech, R.; Feilding, A.; Nutt, D.J.; Carhart-Harris, R.L. The effects of psilocybin and MDMA on between-network resting state functional connectivity in healthy volunteers. Front. Hum. Neurosci. 2014, 8. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, J.F.; Fernandesl, S.V.; Soares, J.M.; Maia, L.; Gonçalves Ó, F.; Sampaio, A. Default mode network dissociation in depressive and anxiety states. Brain Imaging Behav. 2016, 10, 147–157. [Google Scholar] [CrossRef]
- Carhart-Harris, R.L.; Leech, R.; Hellyer, P.J.; Shanahan, M.; Feilding, A.; Tagliazucchi, E.; Chialvo, D.R.; Nutt, D. The entropic brain: A theory of conscious states informed by neuroimaging research with psychedelic drugs. Front. Hum. Neurosci. 2014, 8. [Google Scholar] [CrossRef]
- Kong, L.; Chen, K.; Tang, Y.; Wu, F.; Driesen, N.; Womer, F.; Fan, G.; Ren, L.; Jiang, W.; Cao, Y.; et al. Functional connectivity between the amygdala and prefrontal cortex in medication-naive individuals with major depressive disorder. J. Psychiatry Neurosci. 2013, 38, 417–422. [Google Scholar] [CrossRef]
- Puig, M.V.; Gulledge, A.T. Serotonin and Prefrontal Cortex Function: Neurons, Networks, and Circuits. Mol. Neurobiol. 2011, 44, 449–464. [Google Scholar] [CrossRef]
- Quetin, A. Psilocybin in clinical and experimental psychiatry. Impr. Modern. 1960. [Google Scholar] [CrossRef]
- IIsbell, H. Comparison of the reactions induced by psilocybin and LSD-25 in man. Psychopharmacol. 1959, 1, 29–38. [Google Scholar] [CrossRef]
- Hollister, L.E. Clinical, biochemical and psychologic effects of psilocybin. Arch. Int. Pharmacodyn. Ther. 1961, 130, 42–52. [Google Scholar] [PubMed]
- James, E.; Robertshaw, T.L.; Hoskins, M.; Sessa, B. Psilocybin occasioned mystical-type experiences. Hum. Psychopharmacol. Clin. Exp. 2020, 35. [Google Scholar] [CrossRef]
- Elsey, J.W. Psychedelic drug use in healthy individuals: A review of benefits, costs, and implications for drug policy. Drug Sci. Policy Law 2017, 3. [Google Scholar] [CrossRef]
- Madsen, M.K.; Fisher, P.M.; Stenbæk, D.S.; Kristiansen, S.; Burmester, D.; Lehel, S.; Páleníček, T.; Kuchař, M.; Svarer, C.; Ozenne, B.; et al. A single psilocybin dose is associated with long-term increased mindfulness, preceded by a proportional change in neocortical 5-HT2A receptor binding. Eur. Neuropsychopharmacol. 2020, 33, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Erritzoe, D.; Roseman, L.; Nour, M.M.; MacLean, K.; Kaelen, M.; Nutt, D.J.; Carhart-Harris, R.L. Effects of psilocybin therapy on personality structure. Acta Psychiatr. Scand. 2018, 138, 368–378. [Google Scholar] [CrossRef] [PubMed]
- Watts, R.; Day, C.; Krzanowski, J.; Nutt, D.; Carhart-Harris, R. Patients’ Accounts of Increased “Connectedness” and “Acceptance” After Psilocybin for Treatment-Resistant Depression. J. Hum. Psychol. 2017, 57, 520–564. [Google Scholar] [CrossRef]
- Forstmann, M.; Sagioglou, C. Lifetime experience with (classic) psychedelics predicts pro-environmental behavior through an increase in nature relatedness. J. Psychopharmacol. 2017, 31, 975–988. [Google Scholar] [CrossRef] [PubMed]
- Hendricks, P.S.; Crawford, M.S.; Cropsey, K.L.; Copes, H.; Sweat, N.W.; Walsh, Z.; Pavela, G. The relationships of classic psychedelic use with criminal behavior in the United States adult population. J. Psychopharmacol. 2018, 32, 37–48. [Google Scholar] [CrossRef]
- Walsh, Z.; Hendricks, P.S.; Smith, S.; Kosson, D.S.; Thiessen, M.S.; Lucas, P.; Swogger, M.T. Hallucinogen use and intimate partner violence: Prospective evidence consistent with protective effects among men with histories of problematic substance use. J. Psychopharmacol. 2016, 30, 601–607. [Google Scholar] [CrossRef]
- Hendricks, P.S.; Thorne, C.B.; Clark, C.B.; Coombs, D.W.; Johnson, M.W. Classic psychedelic use is associated with reduced psychological distress and suicidality in the United States adult population. J. Psychopharmacol. 2015, 29, 280–288. [Google Scholar] [CrossRef]
- MacLean, K.A.; Johnson, M.W.; Griffiths, R.R. Mystical experiences occasioned by the hallucinogen psilocybin lead to increases in the personality domain of openness. J. Psychopharmacol. 2011, 25, 1453–1461. [Google Scholar] [CrossRef]
- Nour, M.M.; Evans, L.; Carhart-Harris, R.L. Psychedelics, Personality and Political Perspectives. J. Psychoact. Drugs 2017, 49, 182–191. [Google Scholar] [CrossRef]
- Miller, W.R. The phenomenon of quantum change. J. Clin. Psychol. 2004, 60, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, R.R.; Johnson, M.W.; Richards, W.A.; Richards, B.D.; McCann, U.; Jesse, R. Psilocybin occasioned mystical-type experiences: Immediate and persisting dose-related effects. Psychopharmacology 2011, 218, 649–665. [Google Scholar] [CrossRef] [PubMed]
- Smigielski, L.; Kometer, M.; Scheidegger, M.; Krähenmann, R.; Huber, T.; Vollenweider, F.X. Characterization and prediction of acute and sustained response to psychedelic psilocybin in a mindfulness group retreat. Sci. Rep. 2019, 9, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Gotvaldová, K.; Hájková, K.; Borovička, J.; Jurok, R.; Cihlářová, P.; Kuchař, M. Stability of psilocybin and its four analogs in the biomass of the psychotropic mushroom Psilocybe cubensis. Drug Test. Anal. 2021, 13, 439–446. [Google Scholar] [CrossRef]
- Sherwood, A.M.; Halberstadt, A.L.; Klein, A.K.; McCorvy, J.D.; Kaylo, K.W.; Kargbo, R.B.; Meisenheimer, P. Synthesis and Biological Evaluation of Tryptamines Found in Hallucinogenic Mushrooms: Norbaeocystin, Baeocystin, Norpsilocin, and Aeruginascin. J. Nat. Prod. 2020, 83, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Blei, F.; Dörner, S.; Fricke, J.; Baldeweg, F.; Trottmann, F.; Komor, A.; Meyer, F.; Hertweck, C.; Hoffmeister, D. Simultaneous Production of Psilocybin and a Cocktail of β-Carboline Monoamine Oxidase Inhibitors in “Magic” Mushrooms. Chemistry 2020, 26, 729–734. [Google Scholar] [CrossRef]
- Smith, W.R.; Sisti, D. Ethics and ego dissolution: The case of psilocybin. J. Med. Ethic 2020. [Google Scholar] [CrossRef]
- Gartz, J. Biotransformation of tryptamine derivatives in mycelial cultures ofPsilocybe. J. Basic Microbiol. 1989, 29, 347–352. [Google Scholar] [CrossRef]
- Bauer, B. Psilocybin Receives FDA Breakthrough Treatment Designation. 2019. Available online: https://psychedelicreview.com/psilocybin-receives-fda-breakthrough-treatment-designation/ (accessed on 31 March 2021).
- Bauer, B. The Top 10 Psilocybin Research Papers of 2020. 2020. Available online: https://psychedelicreview.com/the-top-10-psilocybin-research-papers-of-2020/ (accessed on 31 March 2021).
- Matsushima, Y.; Shirota, O.; Kikura-Hanajiri, R.; Goda, Y.; Eguchi, F. Effects of Psilocybe argentipes on marble-burying behavior in mice. Biosci. Biotechnol. Biochem. 2009, 73, 1866–1868. [Google Scholar] [CrossRef]
- Gartz, J. Variation of the amount of Alkaloids in Fruit Bodies of Inocybe aeruginascens. Planta Med. 1987, 53, 539–541. [Google Scholar] [CrossRef]
- Jensen, N.; Gartz, J.; Laatsch, H. Aeruginascin, a Trimethylammonium Analogue of Psilocybin from the Hallucinogenic Mushroom Inocybe aeruginascens. Planta Med. 2006, 72, 665–666. [Google Scholar] [CrossRef] [PubMed]
- Chadeayne, A.R.; Pham, D.; Reid, B.G.; Golen, J.A.; Manke, D.R. Active Metabolite of Aeruginascin (4-Hydroxy-N,N,N-trimethyltryptamine): Synthesis, Structure, and Serotonergic Binding Affinity. ACS Omega 2020, 5, 16940–16943. [Google Scholar] [CrossRef]
- Gartz, J. Analysis of Aeruginascin in Fruit Bodies of the Mushroom Inocybe aeruginascens. Int. J. Crude Drug Res. 1989, 27, 141–144. [Google Scholar] [CrossRef]
- Fricke, J.; Lenz, C.; Wick, J.; Blei, F.; Hoffmeister, D. Production Options for Psilocybin: Making of the Magic. Chem. A Eur. J. 2019, 25, 897–903. [Google Scholar] [CrossRef]
- Lew-Sang, E. Factors affecting drug action. Aust. Nurses J. 1975, 4, 21–22. [Google Scholar]
- Ona, G. Inside bad trips: Exploring extra-pharmacological factors. J. Psychedelic Stud. 2018, 2, 53–60. [Google Scholar] [CrossRef]
- Hartogsohn, I. Set and setting, psychedelics and the placebo response: An extra-pharmacological perspective on psychopharmacology. J. Psychopharmacol. 2016, 30, 1259–1267. [Google Scholar] [CrossRef]
- Bègue, L.; Subra, B.; Arvers, P.; Muller, D.; Bricout, V.; Zorman, M. A message in a bottle: Extrapharmacological effects of alcohol on aggression. J. Exp. Soc. Psychol. 2009, 45, 137–142. [Google Scholar] [CrossRef]
- Ahmed, S.H.; Badiani, A.; Miczek, K.A.; Müller, C.P. Non-pharmacological factors that determine drug use and addiction. Neurosci. Biobehav. Rev. 2020, 110, 3–27. [Google Scholar] [CrossRef] [PubMed]
- Haijen, E.C.H.M.; Kaelen, M.; Roseman, L.; Timmermann, C.; Kettner, H.; Russ, S.; Nutt, D.; Daws, R.E.; Hampshire, A.D.G.; Lorenz, R.; et al. Predicting Responses to Psychedelics: A Prospective Study. Front. Pharmacol. 2018, 9. [Google Scholar] [CrossRef]
- Olson, J.A.; Suissa-Rocheleau, L.; Lifshitz, M.; Raz, A.; Veissière, S.P.L. Tripping on nothing: Placebo psychedelics and contextual factors. Psychopharmacology 2020, 237, 1371–1382. [Google Scholar] [CrossRef]
- Studerus, E.; Kometer, M.; Hasler, F.; Vollenweider, F.X. Acute, subacute and long-term subjective effects of psilocybin in healthy humans: A pooled analysis of experimental studies. J. Psychopharmacol. 2010, 25, 1434–1452. [Google Scholar] [CrossRef]
- Johnson, M.W.; Richards, W.A.; Griffiths, R.R. Human hallucinogen research: Guidelines for safety. J. Psychopharmacol. 2008, 22, 603–620. [Google Scholar] [CrossRef]
- Davis, K. Psilocybin and Magic Mushrooms. Available online: https://www.medicalnewstoday.com/articles/308850#effects (accessed on 31 March 2021).
- Hartney, E. Magic mushrooms: Everything You’ve been Afraid to Ask. Available online: https://www.verywellmind.com/what-are-magic-mushrooms-22085 (accessed on 10 April 2020).
- Peden, N.R.; Pringle, S.D.; Crooks, J. The Problem of Psilocybin Mushroom Abuse. Hum. Toxicol. 1982, 1, 417–424. [Google Scholar] [CrossRef]
- Hyde, C.; Glancy, G.; Omerod, P.; Hall, D.; Taylor, G.S. Abuse of Indigenous Psilocybin Mushrooms: A New Fashion and Some Psychiatric Complications. Br. J. Psychiatry 1978, 132, 602–604. [Google Scholar] [CrossRef]
- Vollenweider, F.X.; Vollenweider-Scherpenhuyzen, M.F.I.; Bäbler, A.; Vogel, H.; Hell, D. Psilocybin induces schizophrenia-like psychosis in humans via a serotonin-2 agonist action. NeuroReport 1998, 9, 3897–3902. [Google Scholar] [CrossRef]
- Van Amsterdam, J.; Opperhuizen, A.; Brink, W.V.D. Harm potential of magic mushroom use: A review. Regul. Toxicol. Pharmacol. 2011, 59, 423–429. [Google Scholar] [CrossRef]
- Mitrokostas, S. 10 potential risks of taking ‘MAGIC’ MUSHROOMS. Available online: https://www.insider.com/are-magic-mushrooms-dangerous-2019-1 (accessed on 10 April 2020).
- Jo, W.-S.; Hossain, A.; Park, S.-C. Toxicological Profiles of Poisonous, Edible, and Medicinal Mushrooms. Mycobiology 2014, 42, 215–220. [Google Scholar] [CrossRef]
- Dos Santos, R.G.; Bouso, J.C.; Alcázar-Córcoles, M.Á.; Hallak, J.E.C. Efficacy, tolerability, and safety of serotonergic psychedelics for the management of mood, anxiety, and substance-use disorders: A systematic review of systematic reviews. Expert Rev. Clin. Pharmacol. 2018, 11, 889–902. [Google Scholar] [CrossRef]
- Gable, R.S. Toward a Comparative Overview of Dependence Potential and Acute Toxicity of Psychoactive Substances Used Nonmedically. Am. J. Drug Alcohol Abus. 1993, 19, 263–281. [Google Scholar] [CrossRef]
- Gable, R.S. Comparison of acute lethal toxicity of commonly abused psychoactive substances. Addiction 2004, 99, 686–696. [Google Scholar] [CrossRef]
- Yirka, B. Phase 1 clinical trials for Psilocybin show no adverse effects. Available online: https://medicalxpress.com/news/2019-12-phase-clinical-trials-psilocybin-adverse.html (accessed on 27 April 2021).
- Fantegrossi, W.E.; Woods, J.H.; Winger, G. Transient reinforcing effects of phenylisopropylamine and indolealkylamine hallucinogens in rhesus monkeys. Behav. Pharmacol. 2004, 15, 149–157. [Google Scholar] [CrossRef]
- How risky are Psilocybin Mushrooms Compared to other Drugs? Available online: https://drugpolicy.org/drug-facts/how-risky-are-psilocybin-mushrooms (accessed on 17 April 2021).
- Johnson, M.W.; Griffiths, R.R.; Hendricks, P.S.; Henningfield, J.E. The abuse potential of medical psilocybin according to the 8 factors of the Controlled Substances Act. Neuropharmacology 2018, 142, 143–166. [Google Scholar] [CrossRef]
- Lim, T.H.; Wasywich, C.A.; Ruygrok, P.N. A fatal case of ‘magic mushroom’ ingestion in a heart transplant recipient. Intern. Med. J. 2012, 42, 1268–1269. [Google Scholar] [CrossRef]
- Müller, K.; Püschel, K.; Iwersen-Bergmann, S. Suizid unter Psilocin-Einfluss [Suicide under the influence of “magic mushrooms”]. Arch. Kriminol. 2013, 231, 193–198. [Google Scholar]
- Byock, I. Taking Psychedelics Seriously. J. Palliat. Med. 2018, 21, 417–421. [Google Scholar] [CrossRef]
- Appel, J.B.; Freedman, D.X. Tolerance and cross-tolerance among psychotomimetic drugs. Psychopharmacol. 1968, 13, 267–274. [Google Scholar] [CrossRef]
- Passie, T.; Halpern, J.H.; Stichtenoth, D.O.; Emrich, H.M.; Hintzen, A. The Pharmacology of Lysergic Acid Diethylamide: A Review. CNS Neurosci. Ther. 2008, 14, 295–314. [Google Scholar] [CrossRef]
- Strassman, R. Inner Paths to Outer Space: Journeys to Alien Worlds through Psychedelics and Other Spiritual Technologies; Paperback Edition; Park Street Press: Rochester, VT, USA, 2008. [Google Scholar]
- Freye, E. The Mushroom Psilocybin with Psychedelic Properties. In Pharmacology and Abuse of Cocaine, Amphetamines, Ecstasy and Related Designer Drugs; Springer Science and Business Media LLC: Berlin/Heidelberg, Germany, 2009; pp. 221–223. [Google Scholar]
- Gable, R.S. The Toxicity of Recreational Drugs. Am. Sci. 2006, 94, 207. [Google Scholar] [CrossRef]
- Hasler, F.; Bourquin, D.; Brenneisen, R.; Vollenweider, F.X. Renal excretion profiles of psilocin following oral administration of psilocybin: A controlled study in man. J. Pharm. Biomed. Anal. 2002, 30, 331–339. [Google Scholar] [CrossRef]
- Brown, R.T.; Nicholas, C.R.; Cozzi, N.V.; Gassman, M.C.; Cooper, K.M.; Muller, D.; Thomas, C.D.; Hetzel, S.J.; Henriquez, K.M.; Ribaudo, A.S.; et al. Pharmacokinetics of Escalating Doses of Oral Psilocybin in Healthy Adults. Clin. Pharmacokinet. 2017, 56, 1543–1554. [Google Scholar] [CrossRef]
- Kamata, T.; Nishikawa, M.; Katagi, M.; Tsuchihashi, H. Direct detection of serum psilocin glucuronide by LC/MS and LC/MS/MS: Time-courses of total and free (unconjugated) psilocin concentrations in serum specimens of a “magic mushroom” user. Forensic Toxicol. 2006, 24, 36–40. [Google Scholar] [CrossRef]
- Shoda, T.; Fukuhara, K.; Goda, Y.; Okuda, H. Enzyme-assisted synthesis of the glucuronide conjugate of psilocin, an hallucinogenic component of magic mushrooms. Drug Test. Anal. 2011, 3, 594–596. [Google Scholar] [CrossRef]
- Alexandrov, N. 2020 Psychedelics Industry Insights Report. 2020. Available online: https://stockhouse.com/news/newswire/2020/01/17/2020-psychedelics-industry-insights-report (accessed on 10 April 2020).
- Numinus Completes First Extraction of its Psilocybe Mushrooms. 2020. Available online: https://psilocybinalpha.com/news/numinus-completes-first-extraction-of-its-psilocybe-mushrooms (accessed on 10 April 2020).
- Carhart-Harris, R.L.; Goodwin, G.M. The Therapeutic Potential of Psychedelic Drugs: Past, Present, and Future. Neuropsychopharmacology 2017, 42, 2105–2113. [Google Scholar] [CrossRef]
- Hirschfeld, A. Why Magic Mushrooms are the Next Big Booming (and Legal!) Drug Market. 2020. Available online: https://observer.com/2020/10/why-magic-mushrooms-are-the-next-big-booming-and-legal-drug-market/ (accessed on 10 April 2020).
- Segreaves, M.; Smith, C. Effort to Decriminalize Psychedelic Mushrooms Moves Closer to Place on November Ballot. 2020. Available online: https://www.nbcwashington.com/news/local/effort-to-decriminalize-psychedelic-mushrooms-moves-closer-to-place-on-november-ballot/2210420/ (accessed on 15 April 2020).
- Moyer, J.D.C. Voters Approve Ballot Question to Decriminalize Psychedelic Mushrooms. 2020. Available online: https://www.washingtonpost.com/local/dc-politics/dc-magic-mushrooms-result/2020/11/03/bb929e86-1abc-11eb-bb35-2dcfdab0a345_story.html (accessed on 15 April 2020).
- News, K. Oregon becomes first state to legalize ‘magic’ mushrooms. 2020. Available online: https://www.valleycentral.com/news/national-news/oregon-becomes-first-state-to-legalize-magic-mushrooms/ (accessed on 15 April 2020).
- Acker, L. Oregon becomes First State to Legalize Psychedelic Mushrooms. 2020. Available online: https://www.oregonlive.com/politics/2020/11/oregon-becomes-first-state-to-legalize-psychedelic-mushrooms.html (accessed on 15 April 2020).
- Leonhardt, M. Here’s How much ‘Magic Mushroom Retreats’ Like Goop Lab’s Actually Cost. 2020. Available online: https://www.cnbc.com/2020/01/24/heres-how-much-magic-mushroom-retreats-like-goop-labs-actually-cost.html (accessed on 15 April 2020).
- Berger, M. Cybin Corp’s Clinical Trials in Jamaica Are Setting The Company Up For A Quicker Route To Market Than Their Peers. 2020. Available online: https://mushroomstocks.com/cannabis-article/cybin-corps-clinical-trials-in-jamaica-are-setting-the-company-up-for-a-quicker-route-to-market-than-their-peers/ (accessed on 15 April 2020).
- Küçüksen, M.; Küçüksen, A.N. Psilocybin and/or psilocin in combination with cannabinoids and/or terpenes. U.S. Patent No. US10729706B2, 4 August 2020. [Google Scholar]
- Bauer, B. The Miller School of Medicine is Studying CBD + Psilocybin for Treating Traumatic Brain Injury and PTSD. 2020. Available online: https://psychedelicreview.com/the-miller-school-of-medicine-is-studying-cbd-psilocybin-for-treating-traumatic-brain-injury-and-ptsd/ (accessed on 15 April 2020).


| Institute or Organization | Some Publications/Areas of Study/Clinical Trials | References to Psilocybin Studies. | |
|---|---|---|---|
| 1. | Center for Psychedelic and Consciousness Research (John Hopkins University, USA) Founded in 2019. |
| [45,103,108,110,111,112,113,114,115] |
| 2. | Department of Psychiatry (Harbor-UCLA Medical Center, USA). | Pilot Study of Psilocybin Treatment for Anxiety in Patients with Advanced-Stage Cancer | [33] |
| 3. | Usona Institute (Wisconsin, USA). | 2018—U.S. Food and Drug Administration (USFDA) approval for a psilocybin treatment for major depressive disorder (MDD) | [116] |
| 4. | Compass Pathways Ltd. (London, UK). | 2018—U.S. Food and Drug Administration (USFDA) approval of “breakthrough therapy” status in 2018 for a psilocybin treatment they developed for treatment-resistant depression | [104] |
| 5. | Cybin, Corp. (Toronto, ON, Canada)Founded in 2019. |
| [117,118,119] |
| 6. | Multidisciplinary Association for Psychedelic Studies (MAPS). Founded in 1986. |
| [5,47,68,108,117,118,119,120,121,122] |
| 7. | Harvard Psilocybin Project (Department of Psychology at Harvard University, USA). |
| [97,98,123] |
| 8. | Heffter Research Institute (founded and Incorporated in New Mexico, USA 1993). |
| [23,28,32,35,53] |
| 9. | University of New Mexico Health Sciences Center (USA) in association with the Heffter Research Institute and University of New Mexico. | A Double-Blind Trial of Psilocybin-Assisted Treatment of Alcohol Dependence | [23] |
| 10. | Department of Psychiatry (Yale University, USA). |
| [124,125,126,127] |
| 11. | Canadian Centre for Psychedelic Science. |
| [128,129] |
| 12. | The Psyence Group (Toronto, ON, Canada).Founded in 1994. | Granted one of the first federally (Lesotho, Africa) licensed producers of medicinal-grade mushrooms for treatment of psychological trauma and its mental health consequences. | [130] |
| Psychic Effects in Humans and Animals (in Medium Dose (12–20 mg p.o.) | Somatic Effects in Humans (Barely Noticeable/Secondary Pharmacological Effects) [5] |
|---|---|
At 8–12 mg p.o., i.m.;
|
| Effect | Reference | |
|---|---|---|
| 1. | Positive changes in personality and increased altruism. This may, in turn, have wider benefits to society and the global environment. | [192,193,194,195,196] |
| 2. | Enhanced feelings of connectedness | [192] |
| 3. | Enhanced-nature relatedness | [40,192] |
| 4. | Pro-environmental behaviour | [192,197] |
| 5. | Decreased violent and criminal behaviour | [198,199,200] |
| 6. | Reduced suicidal ideation | [13,192,200] |
| 7. | Protection against suicidality and psychological distress (lifetime psilocybin-use) | [13] |
| 8. | Tempered politically authoritarian views | [40,192] |
| 9. | Increase in personality domain of openness | [192,201,202] |
| 10. | Ego dissolution. Reduction of egotistical attitudes, narcissism and induces greater prosocial behaviour. | [65,192,203] |
| 11. | Sustained/persisting improvement in attitudes and behaviour.One study reports substantial decreases in depressive and anxious symptoms persisting up to 6 months after a single active treatment. In another study, participants report positive persisting effects in areas of mood, behaviour, and attitudes after up to 14 months after psilocybin therapy. | [2,15,204] |
| 12. | Improved psychological flexibility and feelings of personal meaningfulness, and subsequent improved psychological outlook. Ability to reframe how a patient views their medical conditions, themselves, their lives and relationships with others. | [192] |
| 13. | Increase in one’s subjective sense of wellbeing. | [121,158] |
| 14. | Quantum change (meaningful personal transformations) | [192,203] |
| 15. | Enhancement of “meaning responses” | [192] |
| 16. | Increased meditation depth | [205] |
| 17. | Increased incidence of positive self-dissolution | [205] |
| Subjective, First-Hand Accounts of Experience with Psilocybin Treatment | Reference | |
|---|---|---|
| 1. |
| [15] |
| 2. | Changes in outlook
| [15] |
| 3. |
| [15,196] |
| 4. | Peace and Happiness
| [15] |
| 5. |
| [15] |
| 6. | Physical/Mental
| [15] |
| Factor | Reference | |
|---|---|---|
| 1. | Extra-pharmacological elements (as with any drug). These include age factors, body weight, body size, muscle mass, genetics, drug tolerance, drug interactions, drug purity, dosage, gender, recreational consumption and inexperience with recreational drug use, past experiences with drug use, mindset, setting (context in which drug is used), experimental setting, social interaction, cultural influences, medical history, placebo design and response to placebo, and drug instrumentalization (instruments used to administer drugs). | [192,205,219,220,221,222,223,224,225] |
| 2. | Mindset
| [2,192,221] |
| 3. | Setting
| [192] |
| 4. | Psychological support
| [15,192] |
| 5. | Specific types of psychological experiences | [2] |
| 6. | Treatment type
| |
| 7. | Type of mood or anxiety disorder | |
| 8. | Degree of suicidality (ideation and actual attempts) in a patient. It is recommended that such patients who will be less likely to benefit from such treatment should be excluded from psychedelic therapy. | [15,192] |
| 9. | Patients with a family history of psychotic disorders. It is recommended that such patients who will be less likely to benefit from such treatment should be excluded from psychedelic therapy. Psychedelics may augment/compound symptoms of psychoses. | [192] |
| 10. | Patients who score high on neuroticism, a Big Five higher-order personality trait. It is recommended that such patients who will be less likely to benefit from such treatment should be excluded from psychedelic therapy. | [192,226] |
| 11. | Patients with history or current diagnosis of bipolar disorder and schizophrenia. It is recommended that such patients who will be less likely to benefit from such treatment should be excluded from psychedelic therapy. | [15,192] |
| 12. | Patients at high risk for developing psychosis, even though psilocybin does not cause lasting anxiety, depression or psychosis. It is recommended that such patients who will be less likely to benefit from such treatment should be excluded from psychedelic therapy. | [192] |
| 13. | Patients on other psychedelic/anti-psychotic/anti-depressant medications such as selective serotonin re-uptake inhibitors (SSRIs), haloperidol, tricyclic anti-depressants, lithium, and monoamine oxidase inhibitors. | [192,227] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lowe, H.; Toyang, N.; Steele, B.; Valentine, H.; Grant, J.; Ali, A.; Ngwa, W.; Gordon, L. The Therapeutic Potential of Psilocybin. Molecules 2021, 26, 2948. https://doi.org/10.3390/molecules26102948
Lowe H, Toyang N, Steele B, Valentine H, Grant J, Ali A, Ngwa W, Gordon L. The Therapeutic Potential of Psilocybin. Molecules. 2021; 26(10):2948. https://doi.org/10.3390/molecules26102948
Chicago/Turabian StyleLowe, Henry, Ngeh Toyang, Blair Steele, Henkel Valentine, Justin Grant, Amza Ali, Wilfred Ngwa, and Lorenzo Gordon. 2021. "The Therapeutic Potential of Psilocybin" Molecules 26, no. 10: 2948. https://doi.org/10.3390/molecules26102948
APA StyleLowe, H., Toyang, N., Steele, B., Valentine, H., Grant, J., Ali, A., Ngwa, W., & Gordon, L. (2021). The Therapeutic Potential of Psilocybin. Molecules, 26(10), 2948. https://doi.org/10.3390/molecules26102948







