Green Tea Catechin Association with Ultraviolet Radiation-Induced Erythema: A Systematic Review and Meta-Analysis
Abstract
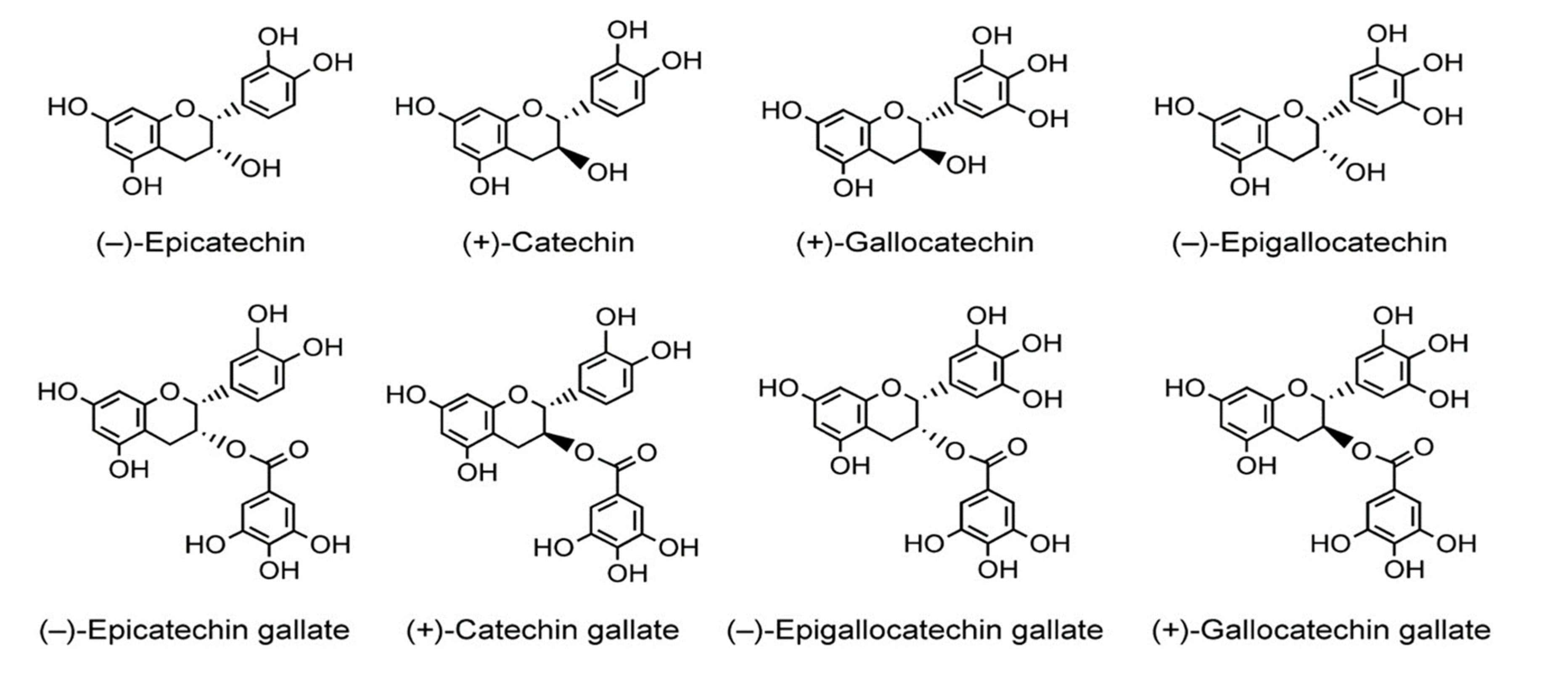
:1. Introduction
2. Results
2.1. Literature Search Results
2.2. Description of Retrieved Studies
2.3. Meta-Analysis Results
2.3.1. Erythema Index (Pre-/Post-Interventions)
2.3.2. Erythema Index (Green Tea Catechins vs. Placebo)
2.3.3. Pro-Inflammatory Mediators (Pre-/Post-Oral Green Tea Catechin Interventions)
3. Materials and Methods
3.1. Literature Search Strategy
3.2. Study Selection Criteria, Data Extraction and Assessment of the Risk of Bias and Outcome
3.3. Data Management and Statistical Procedures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Mahmoud, B.H.; Hexsel, C.L.; Hamzavi, I.H.; Lim, H.W. Effects of visible light on the skin. Photochem. Photobiol. 2008, 84, 450–462. [Google Scholar] [CrossRef]
- Miller, S.A.; Coelho, S.G.; Zmudzka, B.Z.; Bushar, H.F.; Yamaguchi, Y.; Hearing, V.J.; Beer, J.Z. Dynamics of pigmentation induction by repeated ultraviolet exposures: Dose, dose interval, and ultraviolet spectrum dependence. Br. J. Dermatol. 2008, 159, 921–930. [Google Scholar] [CrossRef] [Green Version]
- Healy, Z.R.; Dinkova-Kostova, A.T.; Wehage, S.L.; Thompson, R.E.; Fahey, J.W.; Talalay, P. Precise determination of the erythema response of human skin to ultraviolet radiation and quantification of effects of protectors. Photodermatol. Photoimmunol. Photomed. 2009, 25, 45–50. [Google Scholar] [CrossRef] [Green Version]
- Nicolaou, A.; Masoodi, M.; Gledhill, K.; Haylett, A.K.; Thody, A.J.; Tobin, D.J.; Rhodes, L.E. The eicosanoid response to high dose UVR exposure of individuals prone and resistant to sunburn. Photochem. Photobiol. Sci. 2012, 11, 371–380. [Google Scholar] [CrossRef] [Green Version]
- Huang, M.T.; Ghai, G.; Ho, C.T. Inflammatory process and molecular targets for antiinflammatory nutraceuticals. Compr. Rev. Food Sci. Food Saf. 2004, 3, 127–139. [Google Scholar] [CrossRef]
- Swindells, K.; Rhodes, L.E. Influence of oral antioxidants on ultraviolet radiation-induced skin damage in humans. Photodermatol. Photoimmunol. Photomed. 2004, 20, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, L.E.; Gledhill, K.; Masoodi, M.; Haylett, A.K.; Brownrigg, M.; Thody, A.J.; Nicolaou, A. The sunburn response in human skin is characterized by sequential eicosanoid profiles that may mediate its early and late phases. FASEB J. 2009, 23, 3947–3956. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nicolaou, A.; Pilkington, S.M.; Rhodes, L.E. Ultraviolet-radiation induced skin inflammation: Dissecting the role of bioactive lipids. Chem. Phys. Lipids 2011, 164, 535–543. [Google Scholar] [CrossRef] [PubMed]
- Pilkington, S.M.; Murphy, S.A.; Kudva, S.; Nicolaou, A.; Rhodes, L.E. COX inhibition reduces vasodilator PGE2 but is shown to increase levels of chemoattractant 12-HETE in vivo in human sunburn. Exp. Dermatol. 2015, 24, 790–791. [Google Scholar] [CrossRef] [Green Version]
- Rhodes, L.E.; Belgi, G.; Parslew, R.; McLoughlin, L.; Clough, G.F.; Friedmann, P.S. Ultraviolet-B-induced erythema is mediated by nitric oxide and prostaglandin E2 in combination. J. Investig. Dermatol. 2001, 117, 880–885. [Google Scholar] [CrossRef] [Green Version]
- Rundhaug, J.E.; Fischer, S.M. Cyclo-oxygenase-2 plays a critical role in UV-induced skin carcinogenesis. Photochem. Photobiol. 2008, 84, 322–329. [Google Scholar] [CrossRef]
- Liu, D.; Fernandez, B.O.; Hamilton, A.; Lang, N.N.; Gallagher, J.M.; Newby, D.E.; Weller, R.B. UVA irradiation of human skin vasodilates arterial vasculature and lowers blood pressure independently of nitric oxide synthase. J. Investig. Dermatol. 2014, 134, 1839–1846. [Google Scholar] [CrossRef] [Green Version]
- Feelisch, M.; Kolb-Bachofen, V.; Liu, D.; Lundberg, J.O.; Revelo, L.P.; Suschek, C.V.; Weller, R.B. Is sunlight good for our heart? Eur. Heart J. 2010, 31, 1041–1045. [Google Scholar] [CrossRef] [Green Version]
- Fechtner, S.; Singh, A.; Chourasia, M.; Ahmed, S. Molecular insights into the differences in anti-inflammatory activities of green tea catechins on IL-1β signaling in rheumatoid arthritis synovial fibroblasts. Toxicol. Appl. Pharmacol. 2017, 329, 112–120. [Google Scholar] [CrossRef]
- Bangha, E.; Elsner, P.; Kistler, G.S. Suppression of UV-induced erythema by topical treatment with melatonin (N-acetyl-5-methoxytryptamine). A dose response study. Arch. Dermatol. Res. 1996, 288, 522–526. [Google Scholar] [CrossRef] [PubMed]
- Damian, D.L.; Patterson, C.R.; Stapelberg, M.; Park, J.; Barnetson, R.S.; Halliday, G.M. UV radiation-induced immunosuppression is greater in men and prevented by topical nicotinamide. J. Investig. Dermatol. 2008, 128, 447–454. [Google Scholar] [CrossRef] [Green Version]
- Yiasemides, E.; Sivapirabu, G.; Halliday, G.M.; Park, J.; Damian, D.L. Oral nicotinamide protects against ultraviolet radiation-induced immunosuppression in humans. Carcinogenesis 2009, 30, 101–105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parrado, C.; Philips, N.; Gilaberte, Y.; Juarranz, A.; González, S. Oral photoprotection: Effective agents and potential candidates. Front. Med. 2018, 5, 188. [Google Scholar] [CrossRef] [Green Version]
- Kapoor, M.P.; Okubo, T.; Rao, T.P.; Juneja, L.R. Green Tea Polyphenols in Food and Nonfood Applications. In Green Tea Polyphenols: Nutraceuticals of Modern Life; CRC Press: Boca Raton, FL, USA, 2013; pp. 315–335. [Google Scholar]
- Farrar, M.D.; Nicolaou, A.; Clarke, K.A.; Mason, S.; Massey, K.A.; Dew, T.P.; Rhodes, L.E. A randomized controlled trial of green tea catechins in protection against ultraviolet radiation-induced cutaneous inflammation. Am. J. Clin. Nutr. 2015, 102, 608–615. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rhodes, L.E.; Darby, G.; Massey, K.A.; Clarke, K.A.; Dew, T.P.; Farrar, M.D.; Nicolaou, A. Oral gen tea catechin metabolites are incorporated into human skin and protect against UV radiation-induced cutaneous inflammation in association with reduced production of pro-inflammatory eicosanoid 12-hydroxyeicosatetraenoic acid. Br. J. Nutr. 2013, 110, 891–900. [Google Scholar] [CrossRef] [Green Version]
- Heinrich, U.; Moore, C.E.; De Spirt, S.; Tronnier, H.; Stahl, W. Green tea polyphenols provide photoprotection, increase microcirculation, and modulate skin properties of women. J. Nutr. 2011, 141, 1202–1208. [Google Scholar] [CrossRef] [Green Version]
- Farrar, M.D.; Huq, R.; Mason, S.; Nicolaou, A.; Clarke, K.A.; Dew, T.P.; Rhodes, L.E. Oral green tea catechins do not provide photoprotection from direct DNA damage induced by higher dose solar simulated radiation: A randomized controlled trial. J. Am. Acad. Dermatol. 2018, 78, 414–416. [Google Scholar] [CrossRef] [Green Version]
- Katiyar, S.K.; Matsui, M.S.; Elmets, C.A.; Mukhtar, H. Polyphenolic Antioxidant (−)-Epigallocatechin-3-Gallate from Green Tea Reduces UVB-induced Inflammatory Responses and Infiltration of Leukocytes in Human Skin. Photochem. Photobiol. 1999, 69, 148–153. [Google Scholar] [CrossRef]
- Katiyar, S.K.; Perez, A.; Mukhtar, H. Green tea polyphenol treatment to human skin prevents formation of ultraviolet light B-induced pyrimidine dimers in DNA. Clin. Cancer Res. 2000, 6, 3864–3869. [Google Scholar]
- Hong, Y.H.; Jung, E.Y.; Shin, K.S.; Kim, T.Y.; Yu, K.W.; Chang, U.J.; Suh, H.J. Photoprotective effects of a formulation containing tannase-converted green tea extract against UVB-induced oxidative stress in hairless mice. Appl. Biochem. Biotechnol. 2012, 166, 165–175. [Google Scholar] [CrossRef]
- Santo Domingo, D.; Camouse, M.M.; Hsia, A.H.; Matsui, M.; Maes, D.; Ward, N.L.; Baron, E.D. Anti-angiogenic effects of epigallocatechin-3-gallate in human skin. Int. J. Clin. Exp. Pathol. 2010, 3, 705–709. [Google Scholar]
- Rajbhar, K.; Dawda, H.; Mukundan, U. Tea Polyphenols for Skin Care. Res. J. Top. Cosmet. Sci. 2015, 6, 1–6. [Google Scholar] [CrossRef]
- OyetakinWhite, P.; Tribout, H.; Baron, E. Protective mechanisms of green tea polyphenols in skin. Oxidative Med. Cell. Longev. 2012, 2012, 560682. [Google Scholar] [CrossRef] [Green Version]
- Silverberg, J.I.; Jagdeo, J.; Patel, M.; Siegel, D.; Brody, N. Green tea extract protects human skin fibroblasts from reactive oxygen species induced necrosis. J. Drugs Dermatol. 2011, 10, 1096–1101. [Google Scholar]
- Liu, J.D.; Chen, S.H.; Lin, C.L.; Tsai, S.H.; Liang, Y.C. Inhibition of melanoma growth and metastasis by combination with (−)-epigallocatechin-3-gallate and dacarbazine in mice. J. Cell. Biochem. 2001, 83, 631–642. [Google Scholar] [CrossRef]
- Tzellos, T.G.; Sardeli, C.; Lallas, A.; Papazisis, G.; Chourdakis, M.; Kouvelas, D. Efficacy, safety and tolerability of green tea catechins in the treatment of external anogenital warts: A systematic review and meta-analysis. J. Eur. Acad. Dermatol. Venereol. 2011, 25, 345–353. [Google Scholar] [CrossRef]
- Scheinfeld, N. Sinecatechins. Treatment of genital warts. Drugs Future 2008, 33, 27–30. [Google Scholar] [CrossRef]
- Puviani, M.; Galluzzo, M.; Talamonti, M.; Mazzilli, S.; Campione, E.; Bianchi, L.; Milani, M.; Luppino, I.; Micali, G. Efficacy of sinecatechins 10% as proactive sequential therapy of external genital warts after laser CO2 ablative therapy: The PACT study (post-ablation immunomodulator treatment of condylomata with sinecatechins): A randomized, masked outcome assessment, multicenter trial. Int. J. STD AIDS 2019, 30, 131–136. [Google Scholar]
- Elmets, C.A.; Singh, D.; Tubesing, K.; Matsui, M.; Katiyar, S.; Mukhtar, H. Cutaneous photoprotection from ultraviolet injury by green tea polyphenols. J. Am. Acad. Dermatol. 2001, 44, 425–432. [Google Scholar] [CrossRef]
- Chiu, A.E.; Chan, J.L.; Kern, D.G.; Kohler, S.; Rehmus, W.E.; Kimball, A.B. Double-blinded, placebo-controlled trial of green tea extracts in the clinical and histologic appearance of photoaging skin. Dermatol. Surg. 2005, 31, 855–860. [Google Scholar] [CrossRef]
- Hsu, S. Green tea and the skin. J. Am. Acad. Dermatol. 2005, 52, 1049–1059. [Google Scholar] [CrossRef]
- Türkoğlu, M.; Uğurlu, T.; Gedik, G.; Yılmaz, A.M.; Yalçin, A.S. In vivo evaluation of black and green tea dermal products against UV radiation. Drug Discov. Ther. 2010, 4, 362–367. [Google Scholar]
- Heinrich, U.; Tronnier, H.; De Spirt, S.; Stahl, W. Green tea polyphenols provide photoprotection and improve physiological parameters of human skin. Agro Food Ind. Hi-Tech 2011, 22, 38–39. [Google Scholar]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Viechtbauer, W. Hypothesis tests for population heterogeneity in meta-analysis. Br. J. Math. Stat. Psychol. 2007, 60, 29–60. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Oxman, A.D.; Vist, G.E.; Higgins, J.P.T.; Deeks, J.J.; Glasziou, P.; Guyatt, G.H. Interpreting results and drawing conclusions. In Cochrane Handbook for Systematic Reviews of Interventions; Higgins, J., Green, S., Eds.; Cohrane: London, UK, 2008; Chapter 12. [Google Scholar]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. Br. Med. J. 2015, 349, g7647. [Google Scholar] [CrossRef] [Green Version]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.M.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control. Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- DerSimonian, R.; Kacker, R. Random-effects model for meta-analysis of clinical trials: An update. Contemp. Clin. Trials 2007, 28, 105–114. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.A.D.; Altman, D.G. PRISMA 2009 flow diagram. The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [Green Version]
- Follmann, D.; Elliott, P.; Suh, I.L.; Cutler, J. Variance imputation for overviews of clinical trials with continuous response. J. Clin. Epidemiol. 1992, 45, 769–773. [Google Scholar] [CrossRef]
- Viechtbauer, W. Bias and efficiency of meta-analytic variance estimators in the random-effects model. J. Educ. Behav. Stat. 2005, 30, 261–293. [Google Scholar] [CrossRef]
- Veroniki, A.A.; Jackson, D.; Viechtbauer, W.; Bender, R.; Bowden, J.; Knapp, G.; Salanti, G. Methods to estimate the between-study variance and its uncertainty in meta-analysis. Res. Synth. Methods 2016, 7, 55–79. [Google Scholar] [CrossRef] [Green Version]
- Snyder, D.S. Effect of topical indomethacin on UVR-induced redness and prostaglandin E levels in sunburned guinea pig skin. Prostaglandins 1976, 11, 631–643. [Google Scholar] [CrossRef]
- Nakagawa, T.; Yokozawa, T. Direct scavenging of nitric oxide and superoxide by green tea. Food Chem. Toxicol. 2002, 40, 1745–1750. [Google Scholar] [CrossRef]
- Mukhtar, H.; Ahmad, N. Tea polyphenols: Prevention of cancer and optimizing health. Am. J. Clin. Nutr. 2000, 71, 1698S–1702S. [Google Scholar] [CrossRef] [Green Version]
- De Mejia, E.G.; Ramirez-Mares, M.V.; Puangpraphant, S. Bioactive components of tea: Cancer, inflammation, and behavior. Brain Behav. Immun. 2009, 23, 721–731. [Google Scholar] [CrossRef]
- Horiko, T.; Kushimoto, H.; Akimoto, T.; Fujita, M.; Aoki, T.; Kozuka, T.; Ikenaga, M. Minimum Erythema Dose of Group-A Xeroderma Pigmentation Patients and Their Protection from Sun Light. Skin Res. 1983, 25, 222–229. [Google Scholar]
- Katiyar, S.K.; Afaq, F.; Azizuddin, K.; Mukhtar, H. Inhibition of UVB-induced oxidative stress-mediated phosphorylation of mitogen-activated protein kinase signaling pathways in cultured human epidermal keratinocytes by green tea polyphenol (−)-epigallocatechin-3-gallate. Toxicol. Appl. Pharmacol. 2001, 176, 110–117. [Google Scholar] [CrossRef]
- Afaq, F.; Adhami, V.M.; Ahmad, N.; Mukhtar, H. Inhibition of ultraviolet B-mediated activation of nuclear factor κ B in normal human epidermal keratinocytes by green tea Constituent (−)-epigallocatechin-3-gallate. Oncogene 2003, 22, 1035–1044. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clarke, K.A.; Dew, T.P.; Watson, R.E.; Farrar, M.D.; Osman, J.E.; Nicolaou, A.; Williamson, G. Green tea catechins and their metabolites in human skin before and after exposure to ultraviolet radiation. J. Nutr. Biochem. 2016, 27, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.Y.; Zhu, Q.Y.; Wong, Y.F.; Zhang, Z.; Chung, H.Y. Stabilizing effect of ascorbic acid on green tea catechins. J. Agric. Food Chem. 1998, 46, 2512–2516. [Google Scholar] [CrossRef]
- McArdle, F.; Rhodes, L.E.; Parslew, R.; Jack, C.I.A.; Friedmann, P.S.; Jackson, M.J. UVR-induced oxidative stress in human skin in vivo: Effects of oral vitamin C supplementation. Free Radic. Biol. Med. 2002, 33, 1355–1362. [Google Scholar] [CrossRef]
- Peters, C.M.; Green, R.J.; Janle, E.M.; Ferruzzi, M.G. Formulation with ascorbic acid and sucrose modulates catechin bioavailability from green tea. Food Res. Int. 2010, 43, 95–102. [Google Scholar] [CrossRef] [Green Version]
- Fitzpatrick, T.B. The validity and practicality of sun-reactive skin types I through VI. Arch. Dermatol. 1988, 124, 869–871. [Google Scholar] [CrossRef]





| Study [Reference] | Study Design | Study Population | Dosage/ Day | Study Duration | Study Descriptions # | x. MED | Meta-Analysis Parameters | Study Details/ Remarks |
|---|---|---|---|---|---|---|---|---|
| Farrar et al., 2015 [20] | Randomized Double-blind Placebo controlled (RCT) | Healthy adults (male and female) GTC 25; Placebo 25 Age 18–65 years | Capsules GTC, 1080 mg | 12 weeks | Farrar 2015-a Farrar 2015-b Farrar 2015-c | 1.25–1.30 1.70–1.75 2.0–2.3 | Ultraviolet Radiation-induced Erythema index △E-value PGE2 12-HETE | Studied 10 dosages of simulated Ultraviolet radiation (7–80 mJ/cm2); irradiated sites were examined after 24 h; skin biopsy, analysis of skin blister fluid, urinary analysis of GTC metabolites; Cutaneous production of eicosanoids, Ultraviolet radiation-induced erythema response (threshold value) |
| Rhodes et al., 2013 [21] | Open Oral Intervention Pre- and post- intervention | Healthy adults (male and female) GTC 16 Age 29–59 years | Capsules GTC, 540 mg | 12 weeks | Rhodes 2013-a Rhodes 2013-b Rhodes 2013-c Rhodes 2013-d | 1.0–1.1 1.25–1.30 1.60–1.65 2.0–2.1 | Ultraviolet Radiation -induced Erythema index △E-value PGE2 12-HETE | Studied 10 dosages of simulated Ultraviolet radiation (6.67–68 mJ/cm2); irradiated sites were examined visually after 24 h; Skin tissues and blister fluid sampling; evaluated cutaneous eicosanoid levels; Urinary metabolites; Ultraviolet radiation-induced erythema Index (threshold value) |
| Heinrich et al., 2011 [22] | Randomized Double-blind Placebo controlled (RCT) | Healthy adults (female) GTC 30; Placebo 30 Age 40–65 years | Capsules GTC, 1402 mg | 6 weeks, and 12 weeks | Heinrich 2011-a Heinrich 2011-b | 1.25 1.25 | Ultraviolet Radiation -induced Erythema index △a-value | MED estimation; Irradiation with 1.25 MED at wk 0, wk 6, and wk 12 (time points); Erythema measured before and 24 h after exposure; measurement of reddening (a-value); skin elasticity, structure and texture, and hydration and transepidermal water loss. |
| Farrar et al., 2018 [23] | Randomized Double-blind Placebo controlled (RCT) | Healthy adults (male and female) GTC 20; Placebo 24 Age 18–65 years | Capsules GTC, 1080 mg | 12 weeks | Farrar 2018-a Farrar 2018-b Farrar 2018-c Farrar 2018-d | 3.0 2.0 2.0 2.0 | CPD | Ultraviolet radiation-induced epidermis compared post-supplementation for Immunohistochemically staining with CPDs; Placebo vs. GTC; up to 3xMED erythema dose; studied photoprotection of skin from direct DNA damage. |
| Katiyar et al. 1999 [24] | In-vivo Topical application | Healthy adults (male and female) n = 4 Age 18–65 years | GTC (EGCG) 3 mg/2.5 cm2 skin area | Single-dose | Katiyar 1999 | 4.0 | Ultraviolet Radiation -induced Erythema index △E-value PGE2 | Topical application of GTC (EGCG, 3 mg/2.5 cm2 skin area); Ultraviolet radiation-induced erythema response; Exposures at 4.0 MED; studied MPO and leukocyte inhibition; Cyclooxygenase activity (prostaglandin metabolites) |
| Katiyar et al. 2000 [25] | In-vivo Topical application | Healthy adults (male and female) n = 6 Age 18–65 years | GTC (EGCG) 3 mg/2.5 cm2 skin area | Single-dose | Katiyar 2000-a Katiyar 2000-b Katiyar 2000-c Katiyar 2000-d | 0.50 1.0 2.0 4.0 | Ultraviolet Radiation -induced Erythema index △E-value CPD | Topical application of GTC (3 mg/2.5 cm2 skin area); Ultraviolet radiation-induced erythema response; Exposures at 0.5–4.0 MED; Skin punch biopsies; Immunostaining of CPDs (Ultraviolet radiation dose-dependent at epidermis level) |
| Author and Year | Farrar et al., 2015 | Rhodes et al., 2013 | Heinrich et al., 2011 | Farrar et al., 2018 | Katiyar et al., 1999 | Katiyar et al., 2000 |
|---|---|---|---|---|---|---|
| Reference No. | [20] | [21] | [22] | [23] | [24] | [25] |
| Study type | Oral | Oral | Oral | Oral | Topical | Topical |
| Allocation Concealment | Adequate | Adequate | Adequate | Adequate | Adequate | Adequate |
| Sequence Generation | Yes | Yes | Yes | Yes | No | No |
| Randomization | Yes | Yes | Yes | Yes | No | No |
| Blinding | Yes | Yes | Yes | Yes | No | No |
| Incomplete Outcome | No | No | No | No | No | No |
| Withdrawal/Other reporting | Yes | Yes | Yes | Yes | Yes | Yes |
| Jadad Score | 5 | 4 | 5 | 5 | 2 | 2 |
| Study Characteristics | Outcomes Measured | Study/ Subjects | Meta-Analysis (Estimation) | Test of Heterogeneity | Pooled p-Value | ||
|---|---|---|---|---|---|---|---|
| Inverse Variance, Net Change (95% CI) | Chi-Square Test | p | I2 (%) | ||||
| Oral Intake | |||||||
| Pre-test/ GTC-test (Controlled test) | (i) GTC effect on Erythema Index at varied MED (Between 1.0–2.5) | 9/175 | a SMD: −0.35 [−0.57, −0.13] | 8.36 | 0.40 | 4 | 0.002 |
| b SMD: −0.35 [−0.56, −0.14] | 8.36 | 0.40 | 4 | 0.001 | |||
| a MD: −1.01 [−1.56, −0.47] | 7.60 | 0.47 | 0 | 0.003 | |||
| b MD: −1.01 [−1.56, −0.47] | 7.60 | 0.47 | 0 | 0.003 | |||
| (ii) GTC effect on Erythema Index at identical MED (1.25 ≤ 1.30) | 4/95 | a SMD: −0.49 [−0.78, −0.20] | 2.36 | 0.50 | 0 | 0.0009 | |
| b SMD: −0.49 [−0.78, −0.20] | 2.36 | 0.50 | 0 | 0.0009 | |||
| a MD: −0.99 [−1.54, −0.45] | 1.93 | 0.59 | 0 | 0.0004 | |||
| (iii) Dose–response of GTC on Erythema Index at higher MED | 4/70 | a SMD: −0.19 [−0.58, −0.20] | 3.85 | 0.28 | 22 | 0.34 | |
| b SMD: −0.16 [−0.49, 0.18] | 3.85 | 0.28 | 22 | 0.36 | |||
| a MD: −5.24 [−15.16, 4.68] | 4.49 | 0.21 | 33 | 0.3 | |||
| b MD: −4.02 [−11.74, 3.71] | 4.49 | 0.21 | 33 | 0.31 | |||
| (≥1.50) | |||||||
| RCT studies (Placebo-Controlled) | (i) GTC effect on Erythema Index compared to Placebo at varied MED (Between 1.0–2.5) | 5/P132 5/GTC 135 | a SMD: −0.29 [−0.53, −0.05] | 3.30 | 0.51 | 0 | 0.02 |
| b SMD: −0.29 [−0.53, −0.05] | 3.30 | 0.51 | 0 | 0.02 | |||
| a MD: −1.38 [−2.28, −0.47] | 0.57 | 0.97 | 0 | 0.003 | |||
| b MD: −1.38 [−2.28, −0.47] | 0.57 | 0.97 | 0 | 0.003 | |||
| Topical Application | |||||||
| Pre-test/ GTC-test (Controlled test) | GTC effect on Erythema Index at varied MED (Between 0.5–4.0) | 5/28 | a SMD: −4.52 [−7.72, −1.31] | 29.68 | <0.00001 | 87 | 0.006 |
| b SMD: −1.98 [−2.89, −1.07] | 29.70 | <0.00001 | 87 | <0.0001 | |||
| a MD: -6.68 [−11.37, −1.99] | 372.5 | <0.00001 | 99 | 0.005 | |||
| b MD: −4.38 [−4.84, −3.91] | 0.57 | <0.00001 | 99 | <0.00001 | |||
| GTC effect on Erythema Index at MED ≤ 2.0 | 3/18 | a SMD: −3.02 [−6.40, 0.37] | 16.70 | 0.0002 | 88 | 0.08 | |
| b SMD: −1.48 [−2.44, −10.52] | 16.70 | 0.0002 | 88 | 0.002 | |||
| a MD: −3.44 [−7.01, 0.13] | 83.60 | <0.00001 | 98 | 0.06 | |||
| b MD: −2.27 [−2.79, −1.75] | 83.60 | <0.00001 | 98 | <0.00001 | |||
| Study Characteristics | Outcomes Measured | Study/Subjects | Meta-Analysis (Estimation) | Test of Heterogeneity | Pooled p-Value | ||
|---|---|---|---|---|---|---|---|
| Inverse Variance, Net Change (95% CI) | Chi-Square Test | p | I2 (%) | ||||
| Pre-test/ GTC-test (Controlled test) | (i) GTC effect on PGE2 | 2/30 | a MD: −2.93 [−35.61, 28.75] | 0.01 | 0.9 | 0 | 0.86 |
| b MD: −2.93 [−35.61, 28.75] | 0.01 | 0.9 | 0 | 0.86 | |||
| (ii) GTC effect on 12-HETE | 2/34 | a MD: −7.49 [−33.04, 18.05] | 2.75 | 0.1 | 64 | 0.57 | |
| b MD: −2.05 [−14.24, 10.14] | 2.75 | 0.1 | 64 | 0.74 | |||
| (iii) GTC effect on CPD | 4/35 | a MD: −0.03 [−0.30, 0.23] | 0.16 | 0.98 | 0 | 0.79 | |
| b MD: −0.03 [−0.30, 0.23] | 0.16 | 0.98 | 0 | 0.79 | |||
| RCT studies (Placebo-Controlled) | (i) GTC effect on PGE2 compared to Placebo | 1/P21 1/GTC 20 | a MD: −12.80 [−37.08, 11.48] | na | na | na | 0.3 |
| b MD: −12.80 [−37.08, 11.48] | na | na | na | 0.3 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kapoor, M.P.; Sugita, M.; Fukuzawa, Y.; Timm, D.; Ozeki, M.; Okubo, T. Green Tea Catechin Association with Ultraviolet Radiation-Induced Erythema: A Systematic Review and Meta-Analysis. Molecules 2021, 26, 3702. https://doi.org/10.3390/molecules26123702
Kapoor MP, Sugita M, Fukuzawa Y, Timm D, Ozeki M, Okubo T. Green Tea Catechin Association with Ultraviolet Radiation-Induced Erythema: A Systematic Review and Meta-Analysis. Molecules. 2021; 26(12):3702. https://doi.org/10.3390/molecules26123702
Chicago/Turabian StyleKapoor, Mahendra P., Masaaki Sugita, Yoshitaka Fukuzawa, Derek Timm, Makoto Ozeki, and Tsutomu Okubo. 2021. "Green Tea Catechin Association with Ultraviolet Radiation-Induced Erythema: A Systematic Review and Meta-Analysis" Molecules 26, no. 12: 3702. https://doi.org/10.3390/molecules26123702
APA StyleKapoor, M. P., Sugita, M., Fukuzawa, Y., Timm, D., Ozeki, M., & Okubo, T. (2021). Green Tea Catechin Association with Ultraviolet Radiation-Induced Erythema: A Systematic Review and Meta-Analysis. Molecules, 26(12), 3702. https://doi.org/10.3390/molecules26123702





