Film-Forming Spray of Water-Soluble Chitosan Containing Liposome-Coated Human Epidermal Growth Factor for Wound Healing
Abstract
1. Introduction
2. Result
2.1. Excipient Optimization and the Preparation of Film-Forming Solutions
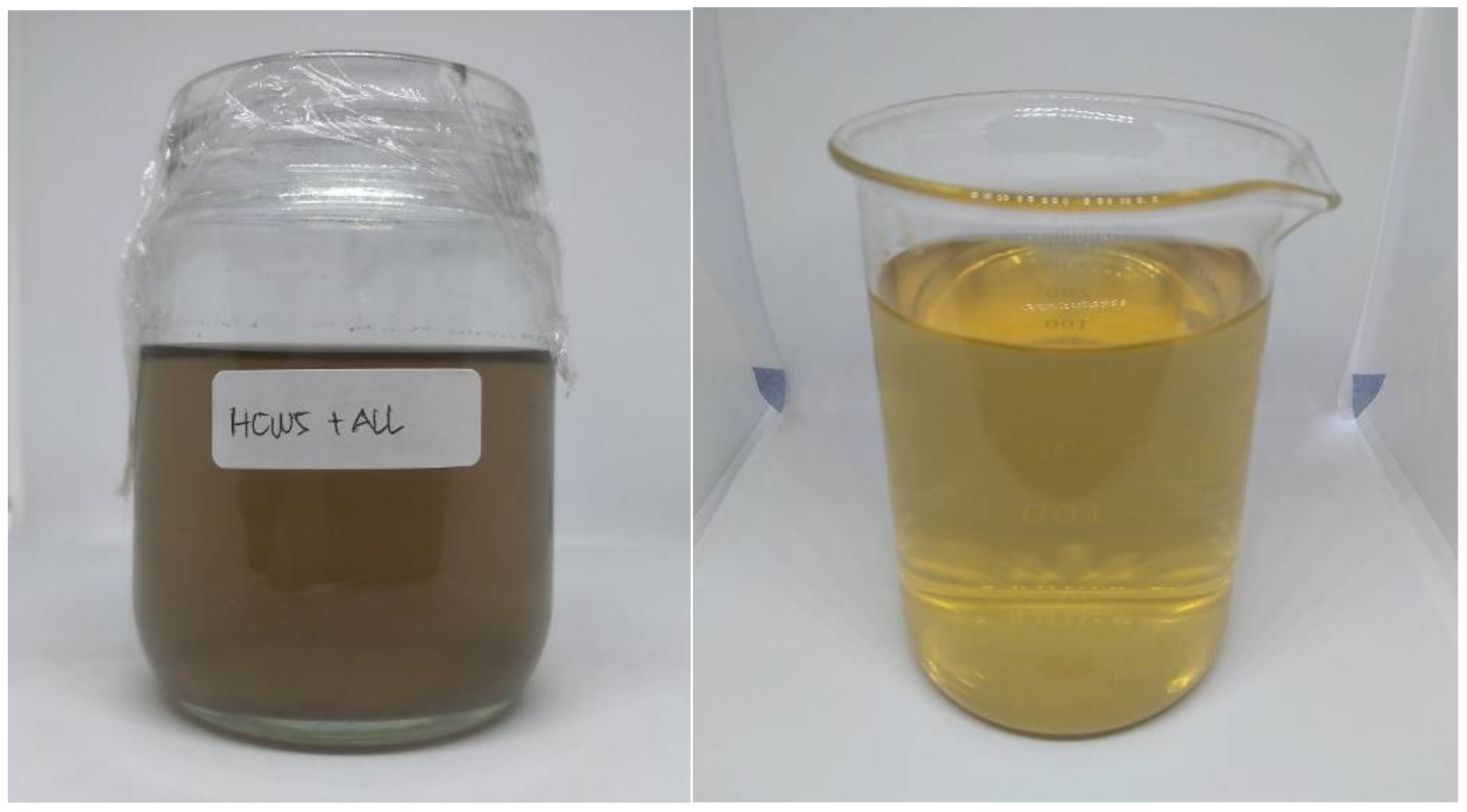
2.2. Preparation of hEGF-Liposomes
2.3. Entrapment Efficiency
2.4. Measurement of Viscosity and pH
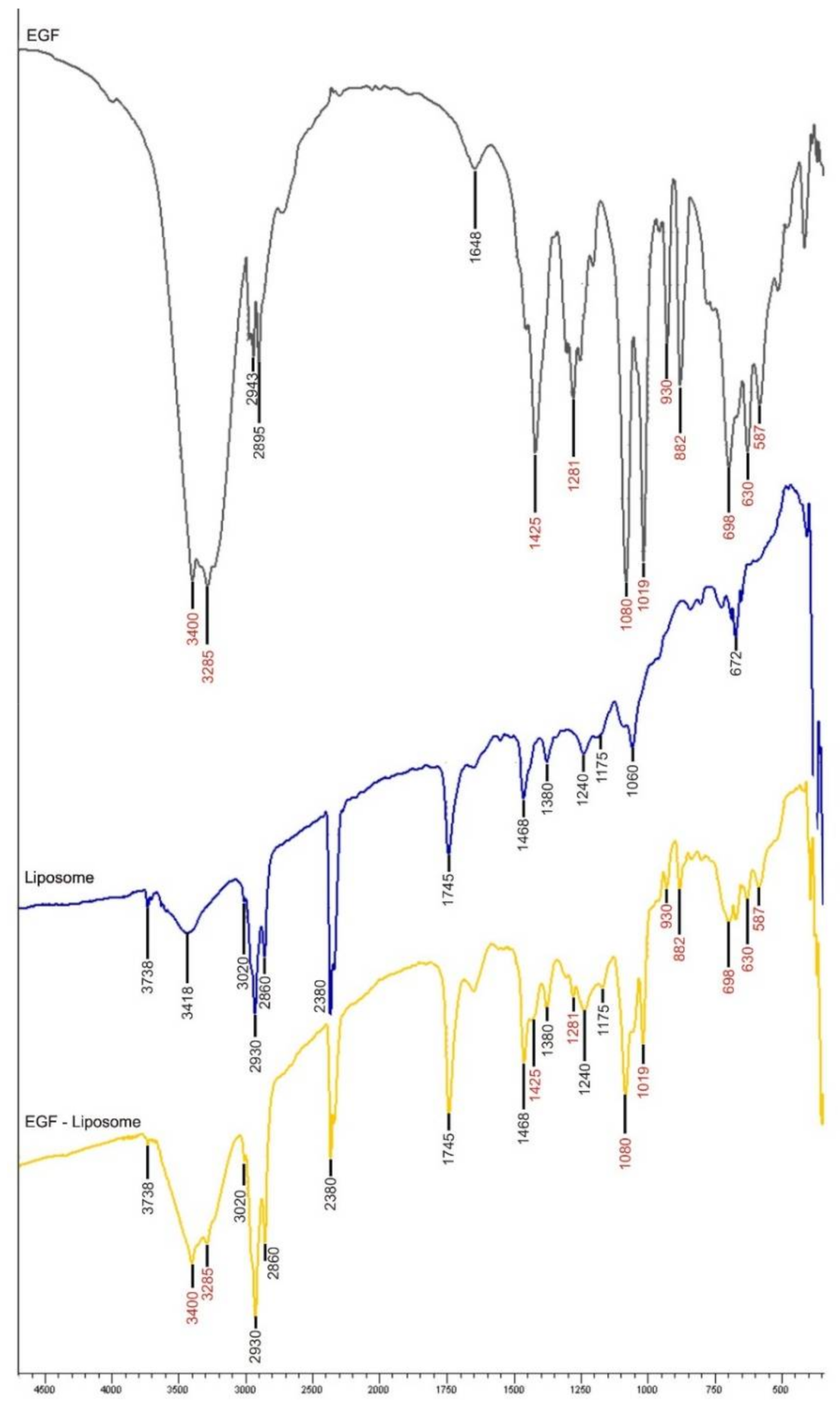
2.5. Observation of hEGF-Liposome FTIR Spectrum
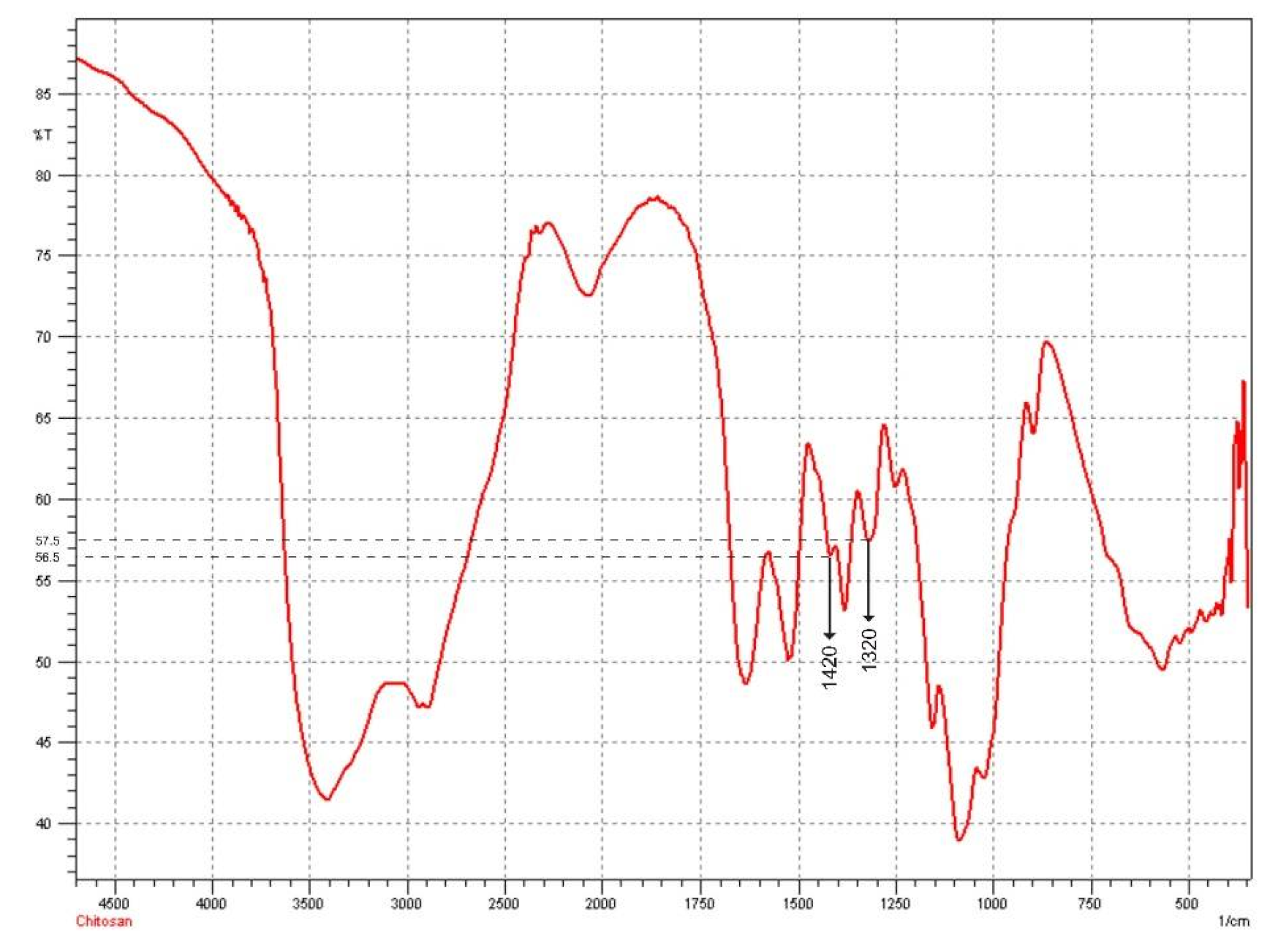
2.6. Determination of the Deacetylation Degree of Chitosan
2.7. Determination of Particle Size, Polydispersity Index, and Zeta Potential
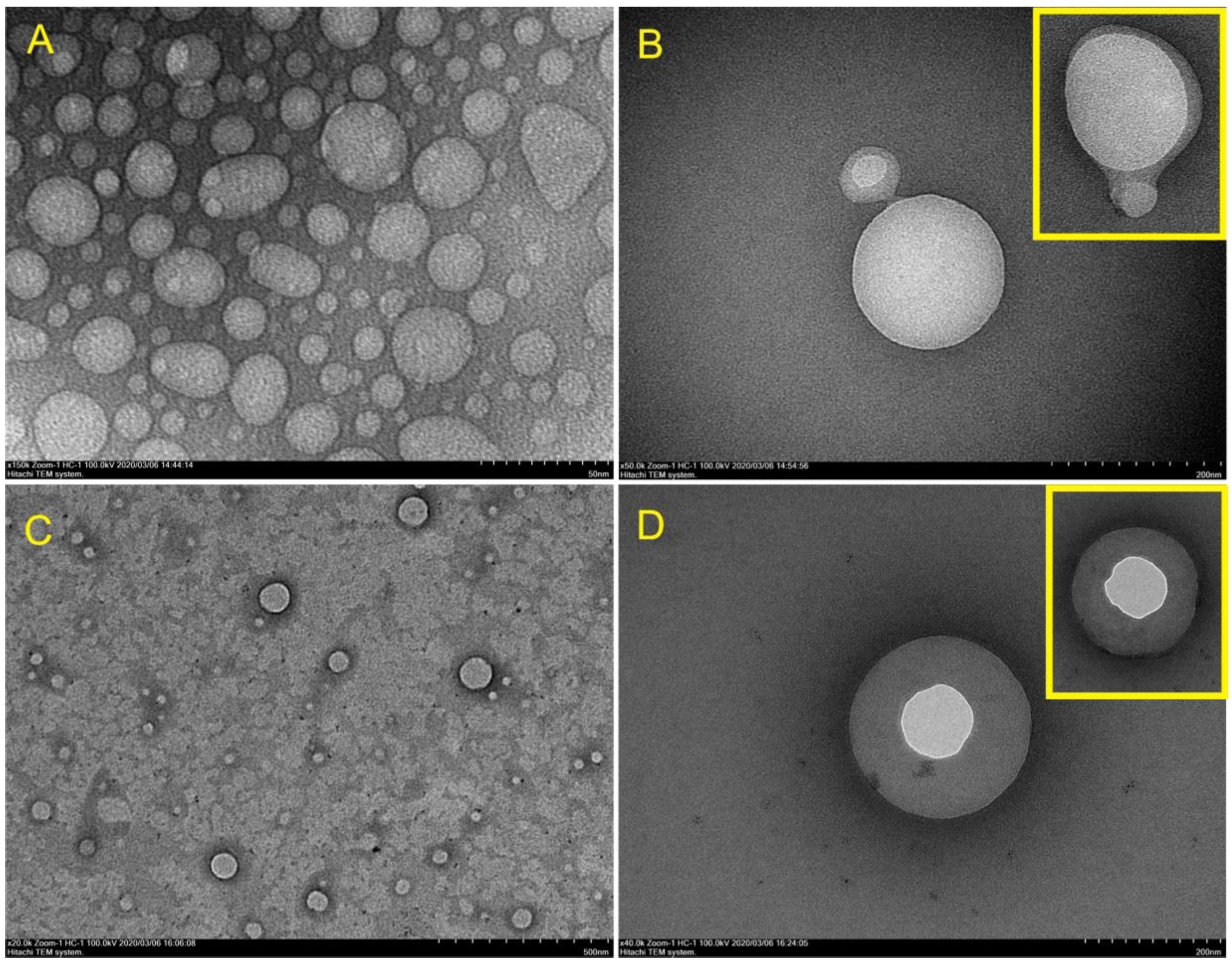
2.8. Observation of hEGF–Liposome Surface Morphology and TEM Analysis
2.9. Occlusion Potential of Film
2.10. Spray Angle, Pattern, and Droplet Size Distribution
2.11. Uniformity of Weight per Spray
2.12. Drying Shrinkage of the Film-Forming Solution
2.13. Theoritical Film Thickness
2.14. Stability Test
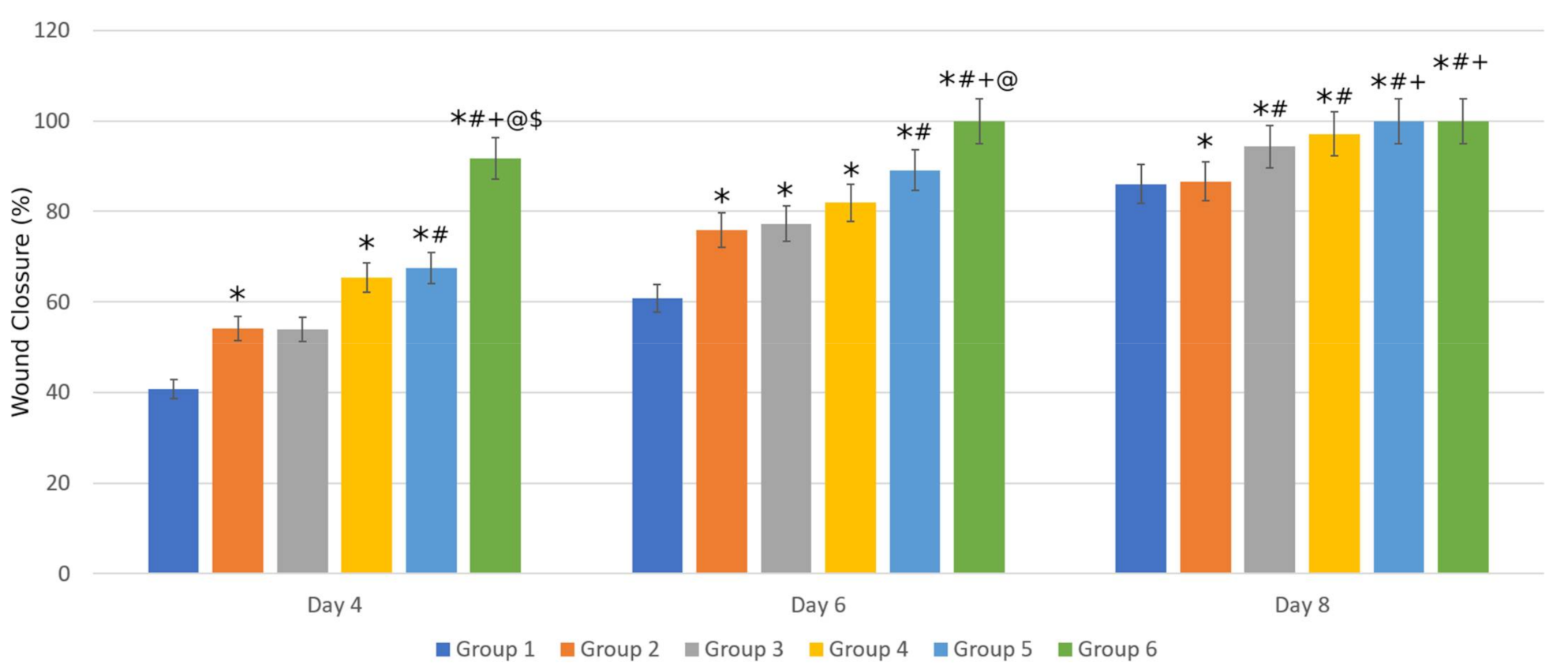
2.15. In Vivo Study
3. Discussion
4. Material and Methods
4.1. Materials
4.2. Excipient Optimization and Preparation of Film-Forming Solution (Base Solution)
4.3. Preparation of hEGF-Liposomes
4.4. Entrapment Efficiency
4.5. Preparation of Film-Forming Spray
4.6. Measurement of Viscosity and pH
4.7. Observation of the hEGF–Liposome FTIR Spectrum
4.8. Determination of the Deacetylation Degree of Chitosan
4.9. Determination of Particle Size, Polydispersity Index, and Zeta Potential
4.10. Observation of hEGF–Liposome Surface Morphology and TEM Analysis
4.11. Occlusion Potential of Film
4.12. Spray Angle, Pattern, and Droplet Size Distribution
4.13. Uniformity of Weight per Spray
4.14. Drying Shrinkage of the Film
4.15. Theoritical Film Thickness
4.16. Stability Test
4.17. In Vivo Study
4.17.1. Animal Preparation
4.17.2. Animal Grouping and Wound Making
4.18. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
Abbreviations
| CAS | Acid-soluble chitosan |
| CWS | Water-soluble chitosan |
| DD | Deacetylation degree |
| DFU | Diabetic foot ulcer |
| GFs | Growth factors |
| hEGF | Human epidermal growth factor |
| PDI | Polydispersity index |
| PG | Propylene glycol |
| WVP | Water vapor permeability |
| FFS | Film-forming spray |
| FFSWSC | Film-forming spray of water-soluble chitosan |
References
- Martí-Carvajal, A.J.; Gluud, C.; Nicola, S.; Simancas-Racines, D.; Reveiz, L.; Oliva, P.; Cedeño-Taborda, J. Growth factors for treating diabetic foot ulcers. Cochrane Database Syst. Rev. 2015, 28. [Google Scholar] [CrossRef]
- Sridharan, K.; Sivaramakrishnan, G. Growth factors for diabetic foot ulcers: Mixed treatment comparison analysis of randomized clinical trials. Br. J. Clin. Pharmacol. 2018, 84, 434–444. [Google Scholar] [CrossRef]
- Park, J.W.; Hwang, S.R.; Yoon, I.-S. Advanced Growth Factor Delivery Systems in Wound Management and Skin Regeneration. Molecules 2017, 22, 1259. [Google Scholar] [CrossRef]
- Gainza, G.; Pastor, M.; Aguirre, J.J.; Villullas, S.; Pedraz, J.L.; Hernandez, R.M.; Igartua, M. A novel strategy for the treatment of chronic wounds based on the topical administration of rhEGF-loaded lipid nanoparticles: In vitro bioactivity and in vivo effectiveness in healing-impaired db/db mice. J. Control. Release 2014, 185, 51–61. [Google Scholar] [CrossRef]
- Griol-Charhbili, V.; Fassot, C.; Messaoudi, S.; Perret, C.; Agrapart, V.; Jaisser, F. Epidermal Growth Factor Receptor Mediates the Vascular Dysfunction But Not the Remodeling Induced by Aldosterone/Salt. Hypertension 2011, 57, 238–244. [Google Scholar] [CrossRef]
- Singla, S.; Singla, S.; Kumar, A.; Singla, M. Role of Epidermal Growth Factor in Healing of Diabetic Foot Ulcers. Indian J. Surg. 2012, 74, 451–455. [Google Scholar] [CrossRef] [PubMed]
- Tsang, M.W.; Wong, W.K.R.; Hung, C.S.; Lai, K.-M.; Tang, W.; Cheung, E.Y.; Kam, G.; Leung, L.; Chan, C.W.; Chu, C.M.; et al. Human Epidermal Growth Factor Enhances Healing of Diabetic Foot Ulcers. Diabetes Care 2003, 26, 1856–1861. [Google Scholar] [CrossRef] [PubMed]
- Berlanga-Acosta, J.; Fernández-Montequín, J.; Valdés-Pérez, C.; Savigne-Gutiérrez, W.; Mendoza-Marí, Y.; García-Ojalvo, A.; Falcón-Cama, V.; Del Barco-Herrera, D.G.; Fernández-Mayola, M.; Pérez-Saad, H.; et al. Diabetic Foot Ulcers and Epidermal Growth Factor: Revisiting the Local Delivery Route for a Successful Outcome. BioMed Res. Int. 2017, 2017, 1–10. [Google Scholar] [CrossRef]
- Bozzuto, G.; Molinari, A. Liposomes as nanomedical devices. Int. J. Nanomed. 2015, 10, 975–999. [Google Scholar] [CrossRef] [PubMed]
- Mahmoudi, R.; Ardakani, M.T.; Verdom, B.H.; Bagheri, A.; Mohammad-Beigi, H.; Aliakbari, F.; Salehpour, Z.; Alipour, M.; Afrouz, S.; Bardania, H. Chitosan nanoparticles containing Physalis alkekengi-L extract: Preparation, optimization and their antioxidant activity. Bull. Mater. Sci. 2019, 42, 131. [Google Scholar] [CrossRef]
- Bardania, H.; Shojaosadati, S.A.; Kobarfard, F.; Morshedi, D.; Aliakbari, F.; Tahoori, M.T.; Roshani, E. RGD-Modified Nano-Liposomes Encapsulated Eptifibatide with Proper Hemocompatibility and Cytotoxicity Effect. Iran. J. Biotechnol. 2019, 17, 8–13. [Google Scholar] [CrossRef]
- Mahmoudi, R.; Mirahmadi-Babaheidri, S.A.; Delaviz, H.; Fouani, M.H.; Alipour, M.; Barmak, M.J.; Christiansen, G.; Bardania, H. RGD peptide-mediated liposomal curcumin targeted delivery to breast cancer cells. J. Biomater. Appl. 2020, 35, 743–753. [Google Scholar] [CrossRef] [PubMed]
- Mahmoudi, R.; Hassandokht, F.; Ardakani, M.T.; Karimi, B.; Roustazadeh, A.; Tarvirdipour, S.; Barmak, M.J.; Nikseresht, M.; Baneshi, M.; Mousavizadeh, A.; et al. Intercalation of curcumin into liposomal chemotherapeutic agent augments apoptosis in breast cancer cells. J. Biomater. Appl. 2020, 35, 1005–1018. [Google Scholar] [CrossRef] [PubMed]
- Alemdaroǧlu, C.; Deǧim, Z.; Çelebi, N.; Zor, F.; Öztürk, S.; Erdoǧan, D. An investigation on burn wound healing in rats with chitosan gel formulation containing epidermal growth factor. Burns 2006, 32, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Parchen, G.P.; Jacumazo, J.; Koop, H.S.; Biscaia, S.M.P.; Trindade, E.S.; Silveira, J.L.M.; de Freitas, R.A. Modulation of Epidermal Growth Factor Release by Biopolymer-Coated Liposomes. J. Pharm. Sci. 2020, 109, 2294–2301. [Google Scholar] [CrossRef]
- Prats, P.; Duconge, J.; Valenzuela, C.; Berlanga, J.; Edrosa, C.; Fernández-Sánchez, E. Disposition and receptor-site binding of125I-EGF after topical administration to skin wounds. Biopharm. Drug Dispos. 2002, 23, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Mandal, U.K.; Chatterjee, B.; Pauzi, F.H.B. A Review on Transdermal Spray: Formulation Aspect. Mathews J. Pharm. Sci. 2016, 2, 006. [Google Scholar]
- Ibrahim, S.A. Spray-on transdermal drug delivery systems. Expert Opin. Drug Deliv. 2014, 12, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Kahya, N. Water Soluble Chitosan Derivatives and their Biological Activities: A Review. Polym. Sci. 2019, 5, 1–16. [Google Scholar] [CrossRef]
- Değim, Z.; Çelebi, N.; Alemdaroğlu, C.; Deveci, M.; Öztürk, S.; Özoğul, C. Evaluation of chitosan gel containing liposome-loaded epidermal growth factor on burn wound healing. Int. Wound J. 2011, 8, 343–354. [Google Scholar] [CrossRef]
- Rachtanapun, P.; Jakkaew, M.; Suriyatem, R. Characterization of Chitosan and Carboxymethyl Chitosan Films from Various Sources and Molecular Sizes. Adv. Mater. Res. 2012, 506, 417–420. [Google Scholar] [CrossRef]
- Umar, A.K.; Butarbutar, M.E.T.; Sriwidodo, S.; Wathoni, N. Film-Forming Sprays for Topical Drug Delivery. Drug Des. Dev. Ther. 2020, 14, 2909–2925. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.C.; Coelho, M.G.; Pires, R.F.; Franco, M.R. Solubility of Benzoic Acid in Mixed Solvents. J. Chem. Eng. Data 2007, 52, 298–300. [Google Scholar] [CrossRef]
- Blaug, S.M.; Ahsan, S.S. Interaction of Parabens with Nonionic Macromolecules. J. Pharm. Sci. 1961, 50, 441–443. [Google Scholar] [CrossRef]
- Blanchard, J. Effect of Polyols on Interaction of Paraben Preservatives with Polysorbate 80. J. Pharm. Sci. 1980, 69, 169–173. [Google Scholar] [CrossRef]
- Patel, N.K.; Kostenbauder, H.B. Interaction of Preservatives with Macromolecules I. J. Pharm. Sci. 1958, 47, 289–293. [Google Scholar] [CrossRef]
- Yati, K.; Srifiana, Y.; Putra, F. Effect of optimization of Tween 80 and propylene glycol as a surfactant and cosurfactant on the physical properties of aspirin microemulsion. Int. J. Appl. Pharm. 2017, 30, 127. [Google Scholar] [CrossRef]
- Shashidhar, G.M.; Manohar, B. Nanocharacterization of liposomes for the encapsulation of water soluble compounds from Cordyceps sinensis CS1197 by a supercritical gas anti-solvent technique. RSC Adv. 2018, 8, 34634–34649. [Google Scholar] [CrossRef]
- Ranade, S.; Bajaj, A.; Londhe, V.; Babul, N.; Kao, D. Fabrication of topical metered dose film forming sprays for pain management. Eur. J. Pharm. Sci. 2017, 100, 132–141. [Google Scholar] [CrossRef]
- Lombardo, D.; Calandra, P.; Barreca, D.; Magazù, S.; Kiselev, M.A. Soft Interaction in Liposome Nanocarriers for Therapeutic Drug Delivery. Nanomaterials 2016, 6, 125. [Google Scholar] [CrossRef]
- Yokota, D.; Moraes, M.; Pinho, S. Characterization of lyophilized liposomes produced with non-purified soy lecithin: A case study of casein hydrolysate microencapsulation. Braz. J. Chem. Eng. 2012, 29, 325–335. [Google Scholar] [CrossRef]
- Nunthanid, J.; Puttipipatkhachorn, S.; Yamamoto, K.; Peck, G.E. Physical Properties and Molecular Behavior of Chitosan Films. Drug Dev. Ind. Pharm. 2001, 27, 143–157. [Google Scholar] [CrossRef]
- Danaei, M.; Dehghankhold, M.; Ataei, S.; Davarani, F.H.; Javanmard, R.; Dokhani, A.; Khorasani, S.; Mozafari, M.R. Impact of Particle Size and Polydispersity Index on the Clinical Applications of Lipidic Nanocarrier Systems. Pharmaceutics 2018, 10, 57. [Google Scholar] [CrossRef]
- Caputo, F.; Clogston, J.; Calzolai, L.; Rösslein, M.; Prina-Mello, A. Measuring particle size distribution of nanoparticle enabled medicinal products, the joint view of EUNCL and NCI-NCL. A step by step approach combining orthogonal measurements with increasing complexity. J. Control. Release 2019, 299, 31–43. [Google Scholar] [CrossRef]
- Kumar, A.; Dixit, C.K. Methods for characterization of nanoparticles. In Advances in Nanomedicine for the Delivery of Therapeutic Nucleic Acids; Elsevier: Leiden, The Netherlands, 2017; pp. 43–58. [Google Scholar]
- Yadav, D.; Sandeep, K.; Pandey, D.; Dutta, R.K. Liposomes for Drug Delivery. J. Biotechnol. Biomater. 2017, 7, 4. [Google Scholar] [CrossRef]
- Zhuang, C.; Zhong, Y.; Zhao, Y. Effect of deacetylation degree on properties of Chitosan films using electrostatic spraying technique. Food Control. 2018, 97, 25–31. [Google Scholar] [CrossRef]
- Gohel, M.C.; Nagori, S.A. Fabrication of Modified Transport Fluconazole Transdermal Spray Containing Ethyl Cellulose and Eudragit® RS100 as Film Formers. AAPS PharmSciTech 2009, 10, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Paradkar, M.; Thakkar, V.; Soni, T.; Gandhi, T.; Gohel, M. Formulation and evaluation of clotrimazole transdermal spray. Drug Dev. Ind Pharm. 2015, 41, 1718–1725. [Google Scholar] [CrossRef]
- Maksum, I.P.; Rostinawati, T.; Subroto, T. Extracellular secretion recombinant of human epidermal growth factor (hEGF) using pectate lyase B (PelB) signal peptide in escherichia coli BL21(DE3). Int. J. Res. Pharm. Sci. 2017, 8, 33–40. [Google Scholar]
- Torres, M.A. Viscous and Viscoelastic Properties of Chitosan Solutions and Gels. Response 2006, 9, 101–108. [Google Scholar]
- Cho, J.; Heuzey, M.-C.; Bégin, A.; Carreau, P.J. Viscoelastic properties of chitosan solutions: Effect of concentration and ionic strength. J. Food Eng. 2006, 74, 500–515. [Google Scholar] [CrossRef]
- Budai, L.; Szabadi, E.; Hajdú, M.; Budai, M.; Klebovich, I.; Antal, I. The influence of selected excipients on the rheological behaviour of chitosan based ocular pharmaceutical systems. J. Phys. Conf. Ser. 2015, 602, 012041. [Google Scholar] [CrossRef]
- Suyatama, N.E.; Tighzert, L.; Copinet, A. Effects of Hydrophilic Plasticizers on Mechanical, Thermal, and Surface Properties of Chitosan Films. J. Agric. Food Chem. 2005, 53, 3950–3957. [Google Scholar] [CrossRef]
- Yeh, M.-K.; Chang, W.-K.; Tai, Y.-J.; Chiang, C.-H.; Hu, C.-S.; Hong, P.-D. The comparison of protein-entrapped liposomes and lipoparticles: Preparation, characterization, and efficacy of cellular uptake. Int. J. Nanomed. 2011, 6, 2403–2417. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Carugo, D.; Bottaro, E.; Owen, J.; Stride, E.; Nastruzzi, C. Liposome production by microfluidics: Potential and limiting factors. Sci. Rep. 2016, 6, 25876. [Google Scholar] [CrossRef]
- Foteini, P.; Pippa, N.; Naziris, N.; Demetzos, C. Physicochemical study of the protein–liposome interactions: Influence of liposome composition and concentration on protein binding. J. Liposome Res. 2019, 29, 313–321. [Google Scholar] [CrossRef]
- Sabın, J.; Prieto, G.; Ruso, J.M.; Hidalgo-Alvarez, R.; Sarmiento, F.; Sabin, J. Size and stability of liposomes: A possible role of hydration and osmotic forces. Eur. Phys. J. E 2006, 20, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Wolfram, J.; Suri, K.; Yang, Y.; Shen, J.; Celia, C.; Fresta, M.; Zhao, Y.; Shen, H.; Ferrari, M. Shrinkage of pegylated and non-pegylated liposomes in serum. Colloids Surf. B Biointerfaces 2014, 114, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Carnwath, R.; Graham, E.; Reynolds, K.; Pollock, P. The antimicrobial activity of honey against common equine wound bacterial isolates. Veter J. 2014, 199, 110–114. [Google Scholar] [CrossRef]
- Al-Niaimi, F.; Chiang, N.Y.Z. Topical Vitamin C and the Skin: Mechanisms of Action and Clinical Applications. J. Clin. Aesthetic Dermatol. 2017, 10, 14–17. [Google Scholar]
- Vollmer, D.L.; West, V.A.; Lephart, E.D. Enhancing Skin Health: By Oral Administration of Natural Compounds and Minerals with Implications to the Dermal Microbiome. Int. J. Mol. Sci. 2018, 19, 3059. [Google Scholar] [CrossRef] [PubMed]
- Geh, K.; Stelzl, A.; Gröne, A.; Wagner, L.; Förster, B.; Winter, G. Development of a sprayable hydrogel formulation for the skin application of therapeutic antibodies. Eur. J. Pharm. Biopharm. 2019, 142, 123–132. [Google Scholar] [CrossRef]
- Brugnerotto, J.; Lizardi, J.; Goycoolea, F.M.; Argüelles-Monal, W.; Desbrières, J.; Rinaudo, M. An infrared investigation in relation with chitin and chitosan characterization. Polymer 2001, 42, 3569–3580. [Google Scholar] [CrossRef]
- Rachmawati, A.L.; Surini, S. Formulasi dan Karakterisasi Nanopartikel Sambungsilang Gom Xantan dan Gom Akasia Untuk Penghantaran Insulin Oral. Pharm. Sci. Res. 2018, 5, 159–168. [Google Scholar]
- Gohli, T.; Shah, P. Formulation and Development of Transdermal Spray of Ibandronate Sodium. Int. J. Pharm. Pharm. Res. 2019, 16, 46–58. [Google Scholar]
- Lu, W.; Luo, H.; Wu, Y.; Zhu, Z.; Wang, H. Preparation and characterization of a metered dose transdermal spray for testosterone. Acta Pharm. Sin. B 2013, 3, 392–399. [Google Scholar] [CrossRef]
- Hidayat, F.K.; Elfiah, U.; Sofiana, K.D. Perbandingan Jumlah Makrofag pada Luka Insisi Full Thickness antara Pemberian Ekstrak Umbi Bidara Upas dengan NaCl pada Tikus Wistar Jantan (Comparison of The Number of Macrophage in Full Thickness Wound Incision between Merremia mammosa Extract Treatment and NaCl in Male Wistar Rats). J. AMS 2015, 1, 9–13. [Google Scholar]
- Federer, W.T. Randomization and Sample Size in Experimentation. Food Drug Adm. Stat. Semin. 1966, 1–14. [Google Scholar]
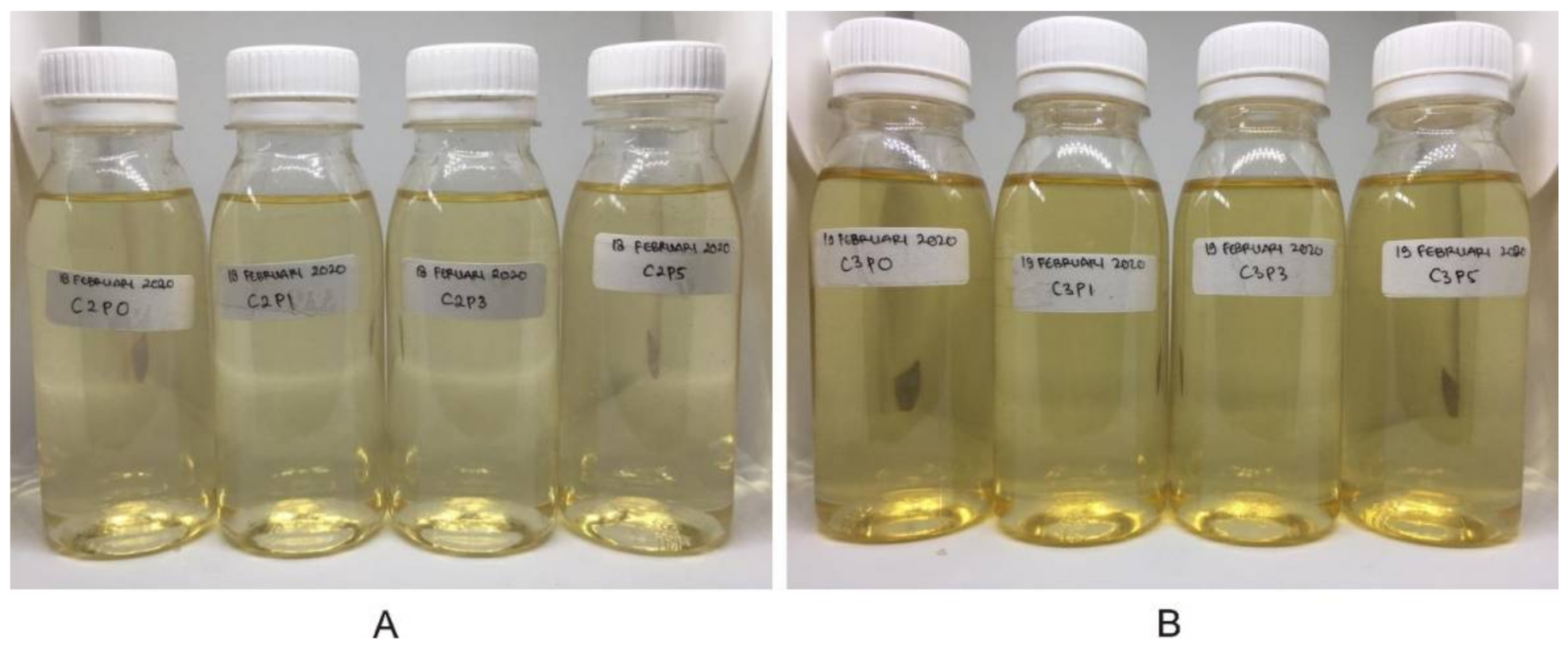



| Formula | Excipient (%) | |||
|---|---|---|---|---|
| Chitosan | Propylene Glycol | Tween 80 | Sodium Benzoate | |
| C2P0 | 2 | 0 | 2 | 0.1 |
| C2P1 | 2 | 1 | 2 | 0.1 |
| C2P3 | 2 | 3 | 2 | 0.1 |
| C2P5 | 2 | 5 | 2 | 0.1 |
| C3P0 | 3 | 0 | 2 | 0.1 |
| C3P1 | 3 | 1 | 2 | 0.1 |
| C3P3 | 3 | 3 | 2 | 0.1 |
| C3P5 | 3 | 5 | 2 | 0.1 |
| Figure | Z-Average (nm) | Polydispersity Index | Zeta Potential (mV) |
|---|---|---|---|
| Empty liposome * | 64 | 0.34 | - |
| Empty liposome | 338.9 | 0.41 | −57.3 |
| hEGF–liposome | 219.3 | 0.22 | −39.7 |
| Empty liposome KIT | 341.0 | 0.50 | 12.8 |
| hEGF–liposome KIT | 853.8 | 0.66 | 25.8 |
| Formula | Viscosity (mPa.s) | pH | Spray Angle (θ) | Droplet Size (µm) | Spray Weight (g) | Occlusion Factor (%) * |
|---|---|---|---|---|---|---|
| C2P0 | 20.90 ± 0.06 | 4.3 ± 0.1 | 74.67 ± 1.96 | 92.90 ± 14.10 | 0.14 ± 0.00 | 12.44 ± 2.97 |
| C2P1 | 21.00 ± 0.00 | 4.4 ± 0.1 | 77.05 ± 0.85 | 88.90 ± 46.04 | 0.15 ± 0.00 | 14.44 ± 5.26 |
| C2P3 | 21.94 ± 0.05 | 4.2 ± 0.1 | 73.03 ± 1.28 | 54.25 ± 13.34 | 0.14 ± 0.00 | 14.57 ± 3.41 |
| C2P5 | 23.46 ± 0.23 | 4.2 ± 0.1 | 75.51 ± 1.94 | 69.07 ± 12.05 | 0.14 ± 0.00 | 19.69 ± 3.79 |
| C3P0 | 52.00 ± 0.00 | 3.9 ± 0.1 | 76.90 ± 0.84 | 82.55 ± 22.44 | 0.14 ± 0.00 | 25.26 ± 4.11 |
| C3P1 | 53.18 ± 0.26 | 4.0 ± 0.1 | 77.87 ± 0.71 | 112.82 ± 44.70 | 0.13 ± 0.00 | 22.93 ± 4.42 |
| C3P3 | 55.12 ± 0.24 | 4.0 ± 0.1 | 77.74 ± 0.83 | 117.15 ± 14.60 | 0.14 ± 0.00 | 22.28 ± 3.03 |
| C3P5 | 56.20 ± 0.24 | 3.9 ± 0.1 | 79.17 ± 0.48 | 84.29 ± 37.44 | 0.14 ± 0.00 | 20.47 ± 1.46 |
| Day | pH | Viscosity (mPa.s) | Particle Size (nm) | PDI |
|---|---|---|---|---|
| 0 | 4.24 ± 0.05 | 21.94 ± 0.05 | 219.3 | 0.219 |
| 1 | 4.24 ± 0.05 | 21.74 ± 0.05 | - | - |
| 7 | 4.26 ± 0.05 | 21.62 ± 0.16 | - | - |
| 14 | 4.22 ± 0.05 | 21.60 ± 0.14 | - | - |
| 28 | 4.24 ± 0.05 | 21.58 ± 0.13 | 207.9 | 0.260 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Umar, A.K.; Sriwidodo, S.; Maksum, I.P.; Wathoni, N. Film-Forming Spray of Water-Soluble Chitosan Containing Liposome-Coated Human Epidermal Growth Factor for Wound Healing. Molecules 2021, 26, 5326. https://doi.org/10.3390/molecules26175326
Umar AK, Sriwidodo S, Maksum IP, Wathoni N. Film-Forming Spray of Water-Soluble Chitosan Containing Liposome-Coated Human Epidermal Growth Factor for Wound Healing. Molecules. 2021; 26(17):5326. https://doi.org/10.3390/molecules26175326
Chicago/Turabian StyleUmar, Abd. Kakhar, Sriwidodo Sriwidodo, Iman Permana Maksum, and Nasrul Wathoni. 2021. "Film-Forming Spray of Water-Soluble Chitosan Containing Liposome-Coated Human Epidermal Growth Factor for Wound Healing" Molecules 26, no. 17: 5326. https://doi.org/10.3390/molecules26175326
APA StyleUmar, A. K., Sriwidodo, S., Maksum, I. P., & Wathoni, N. (2021). Film-Forming Spray of Water-Soluble Chitosan Containing Liposome-Coated Human Epidermal Growth Factor for Wound Healing. Molecules, 26(17), 5326. https://doi.org/10.3390/molecules26175326









