Smart Nanocarriers as an Emerging Platform for Cancer Therapy: A Review
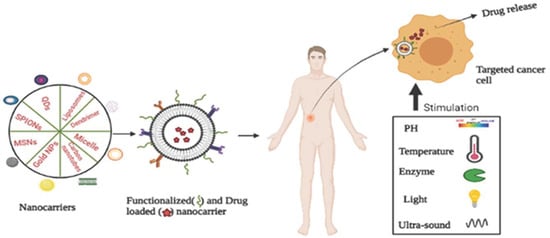
Abstract
:1. Introduction
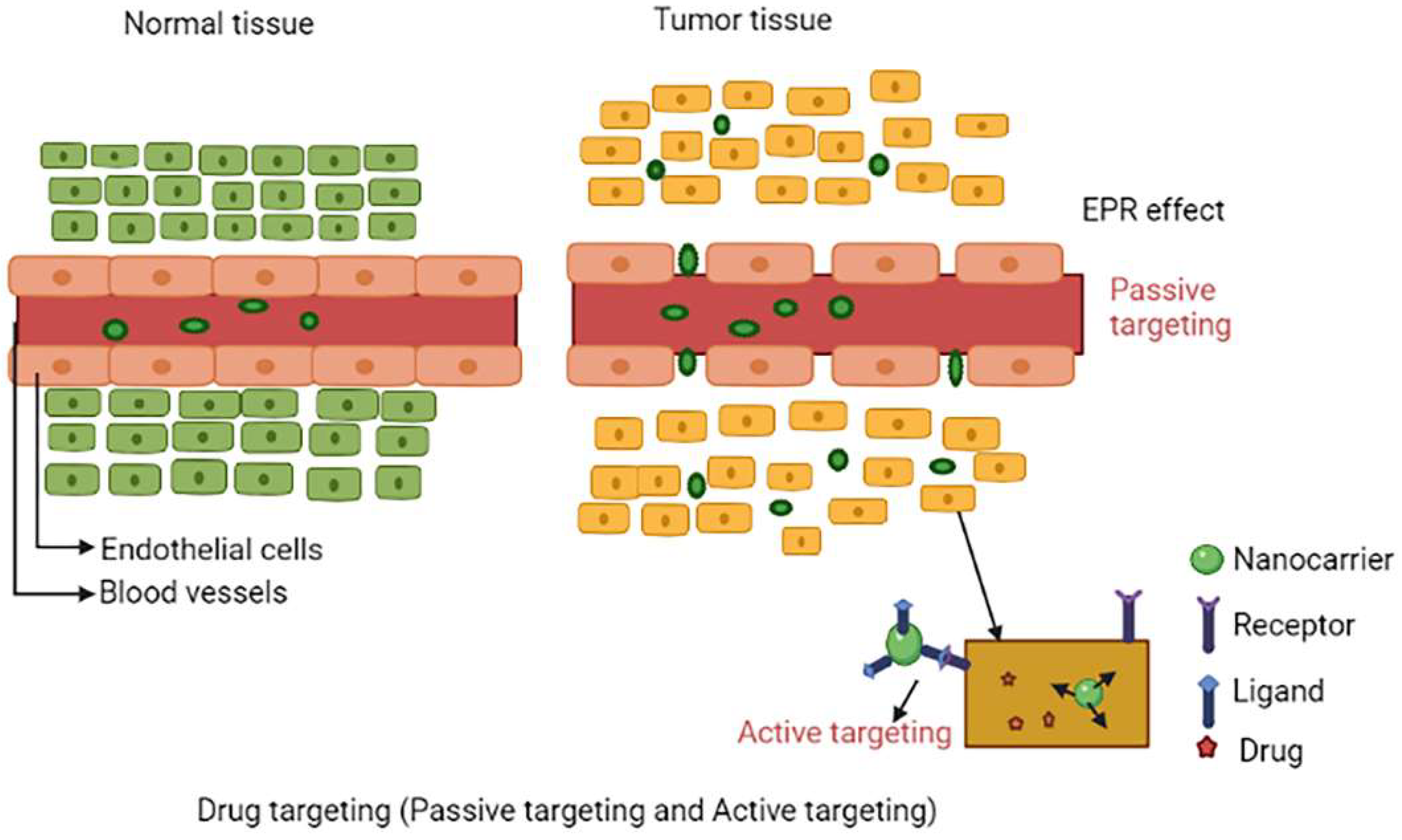
2. Drug Targeting
2.1. Passive Targeting
2.2. Active Targeting
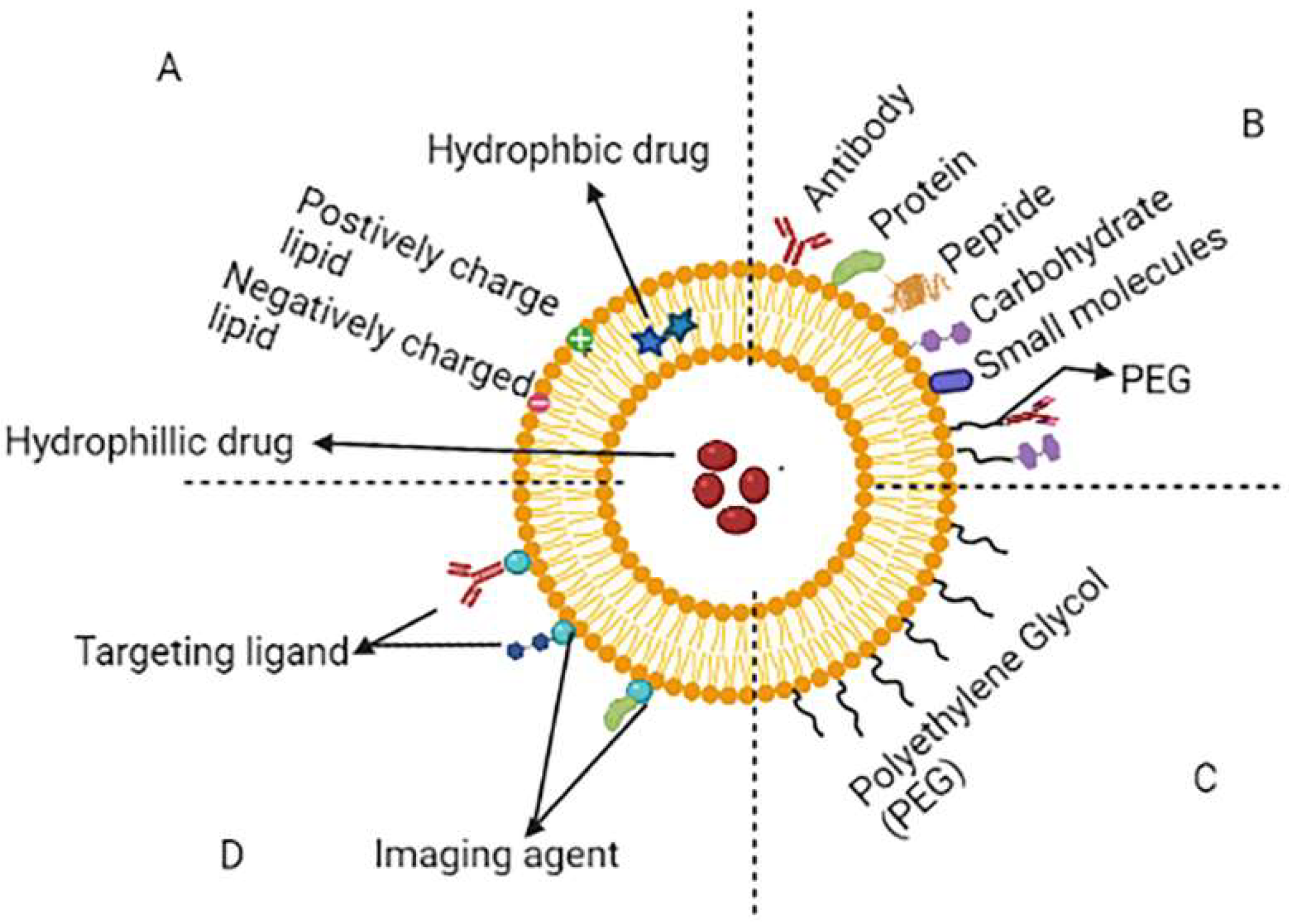
3. Nanocarriers Used in Cancer Therapy
3.1. Liposomes
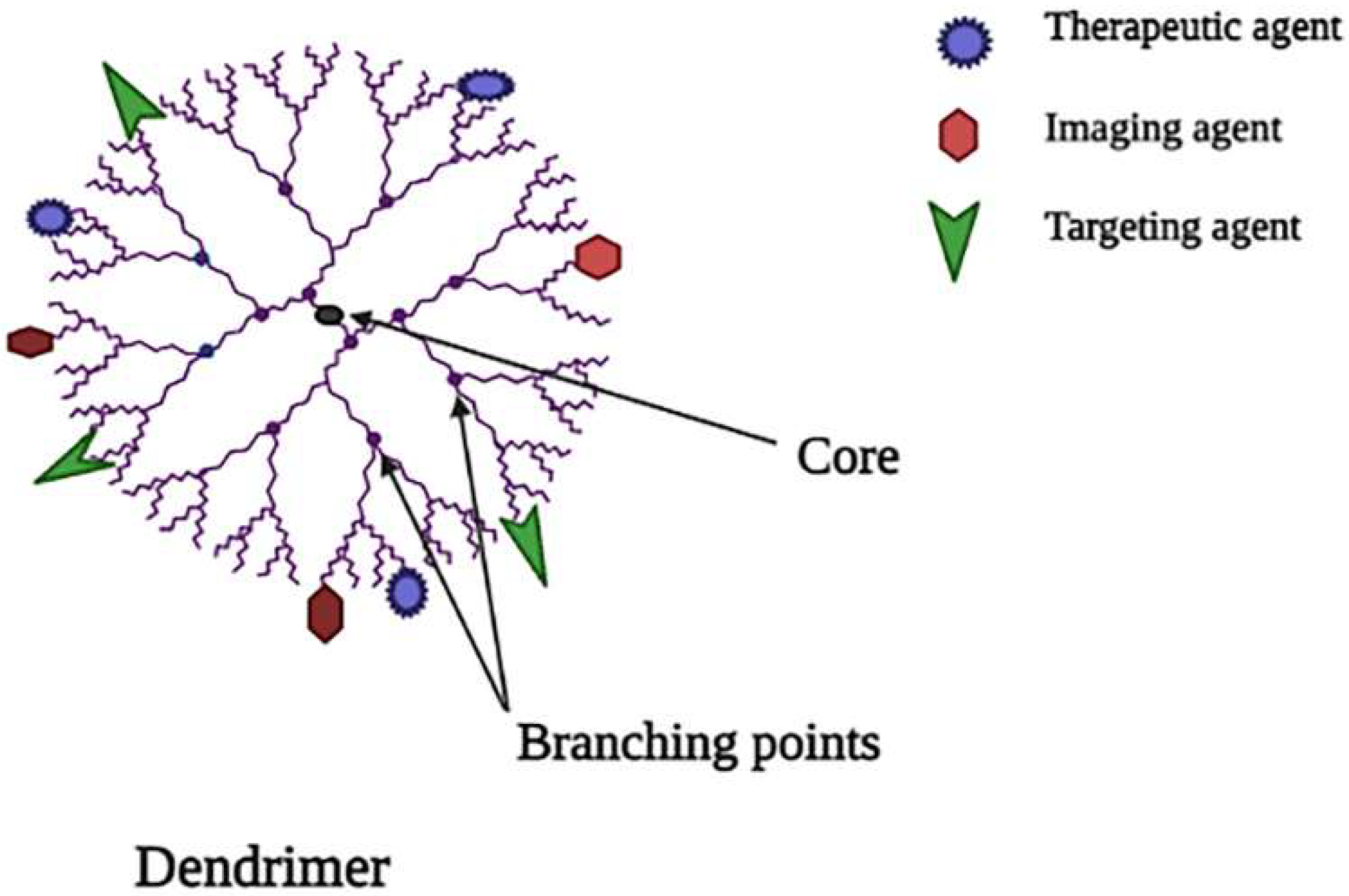
3.2. Dendrimers
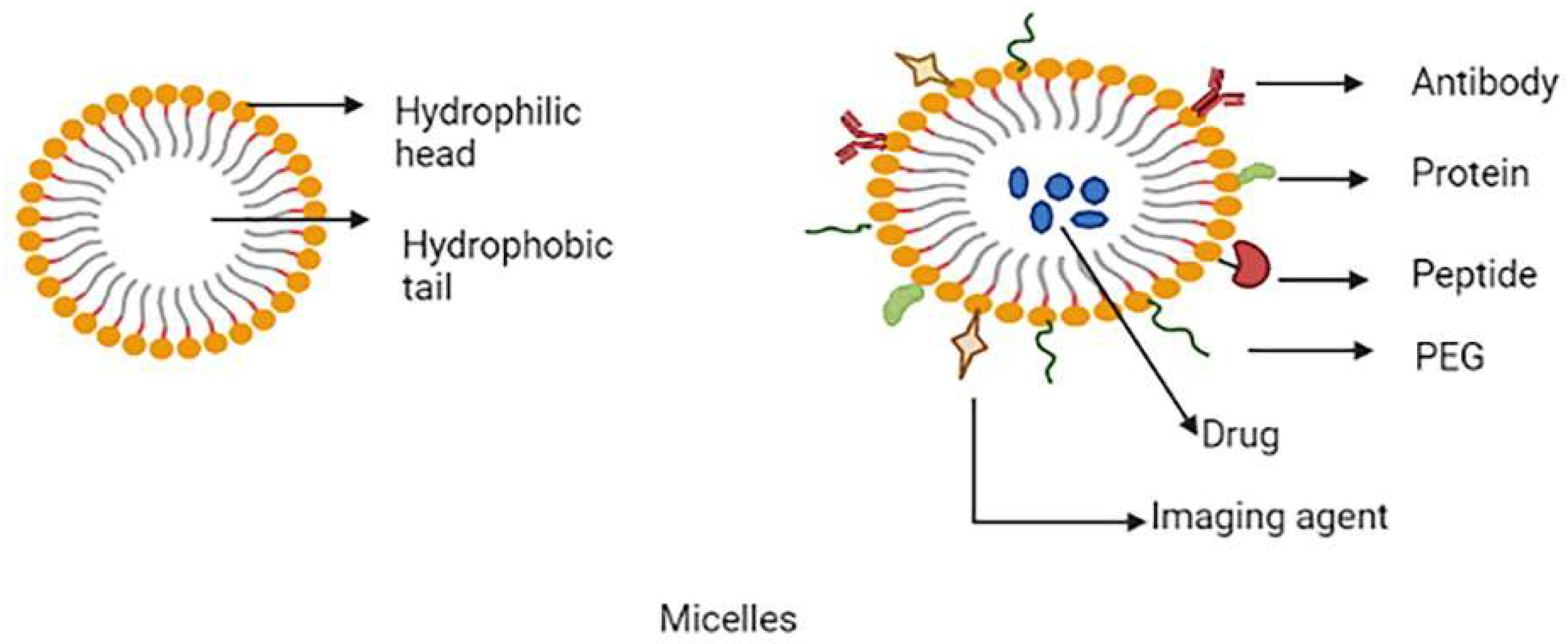
3.3. Micelles
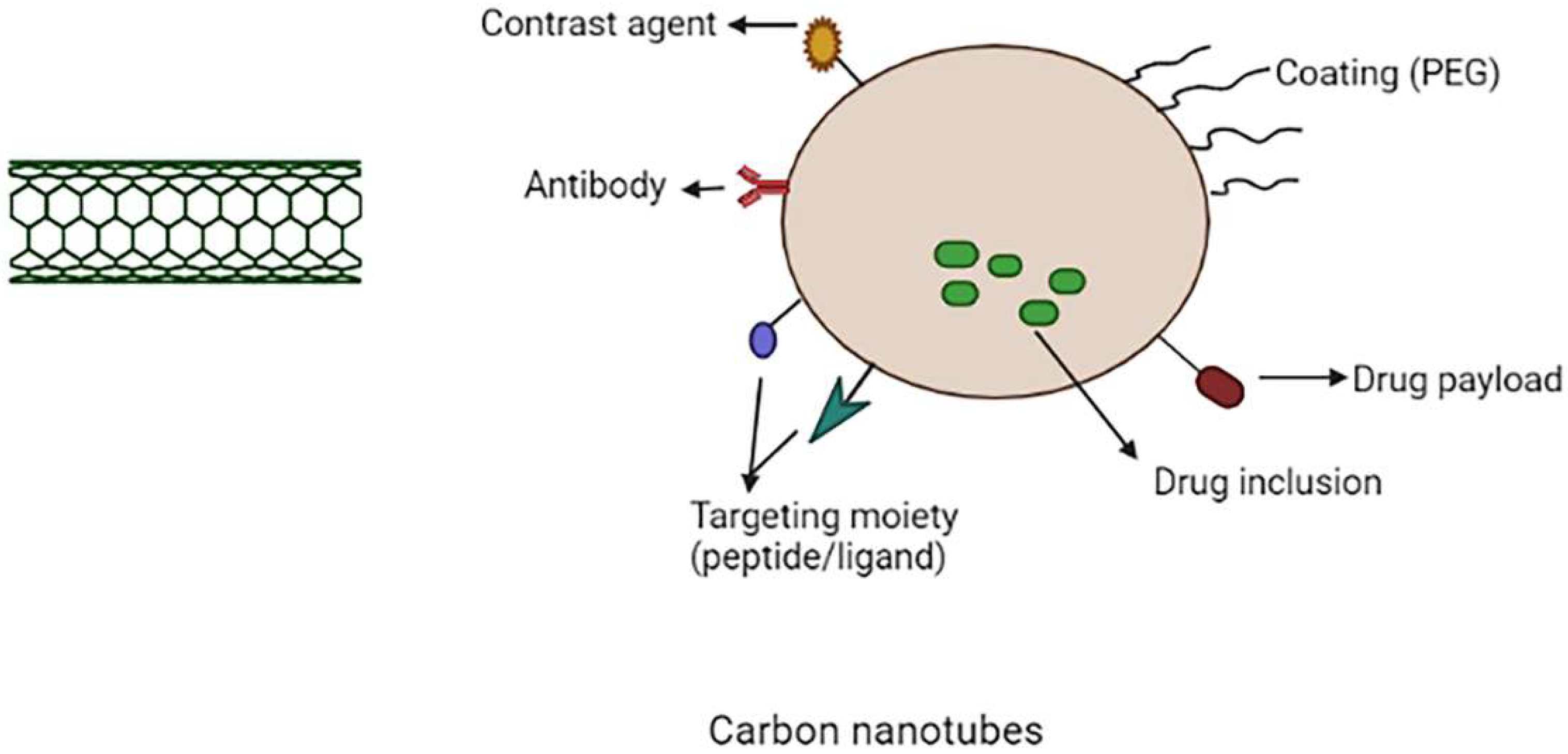
3.4. Carbon Nanotubes (CNTs)
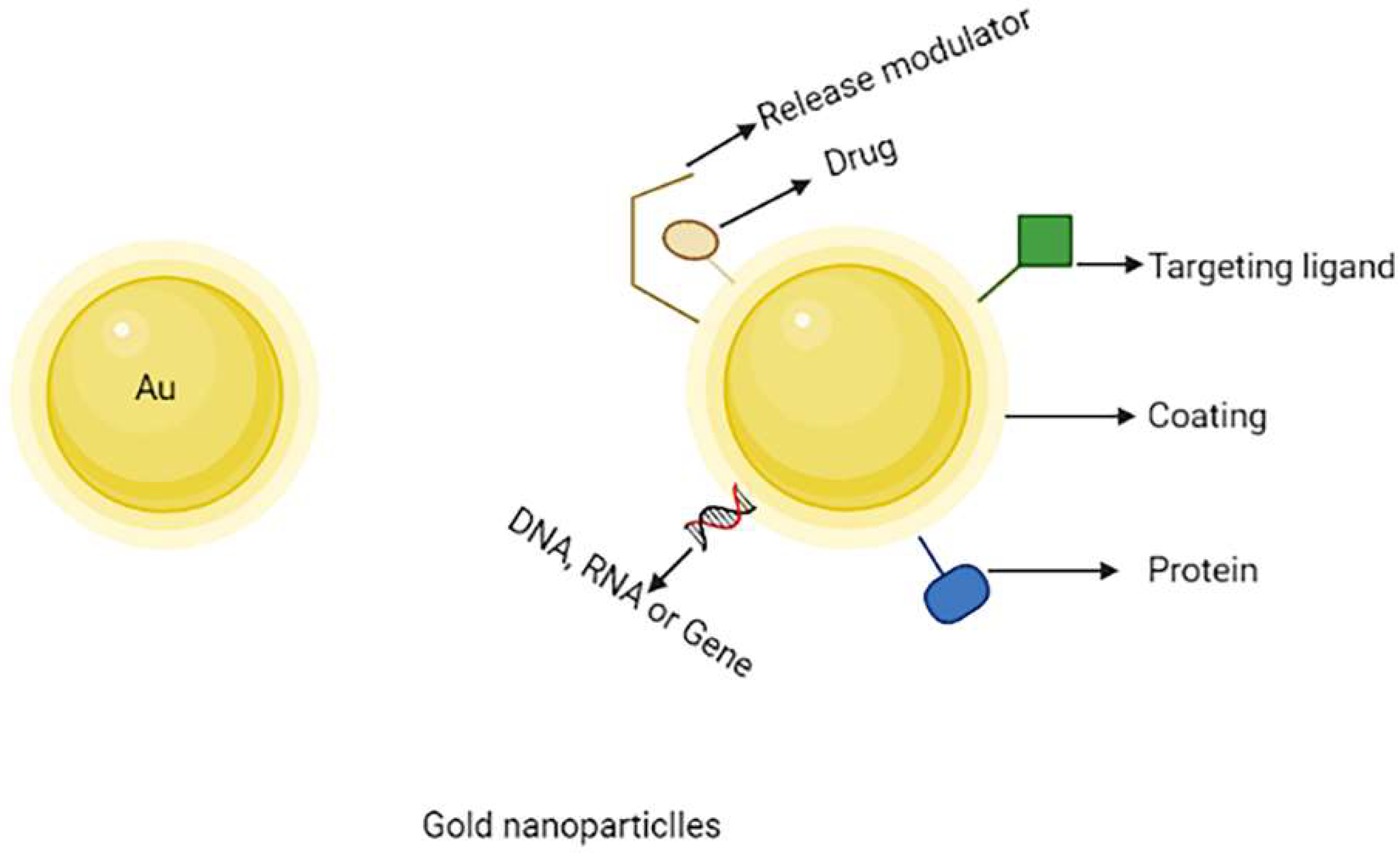
3.5. Gold Nanoparticles (AuNPs)
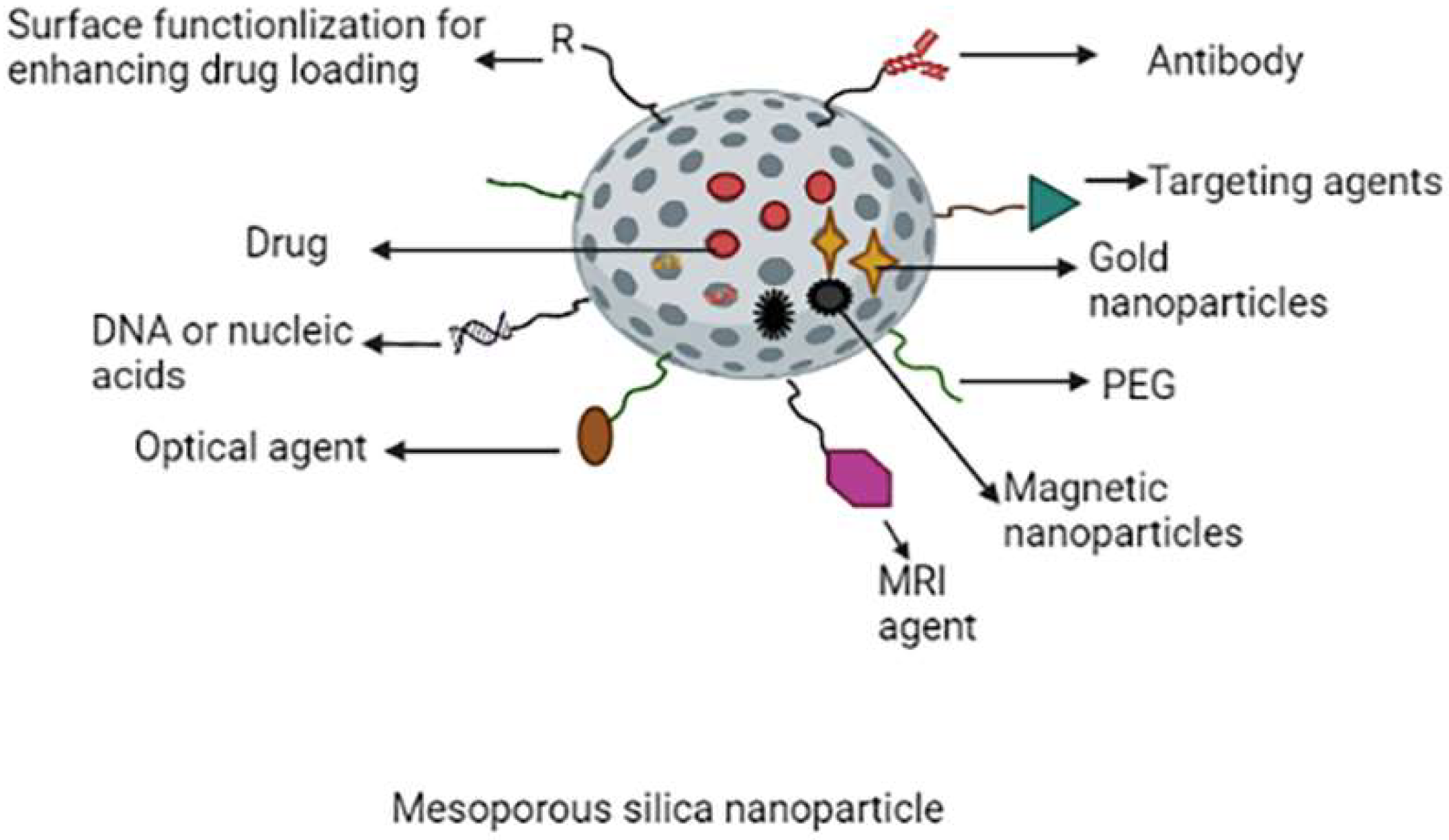
3.6. Mesoporous Silica Nanoparticles (MSNs)
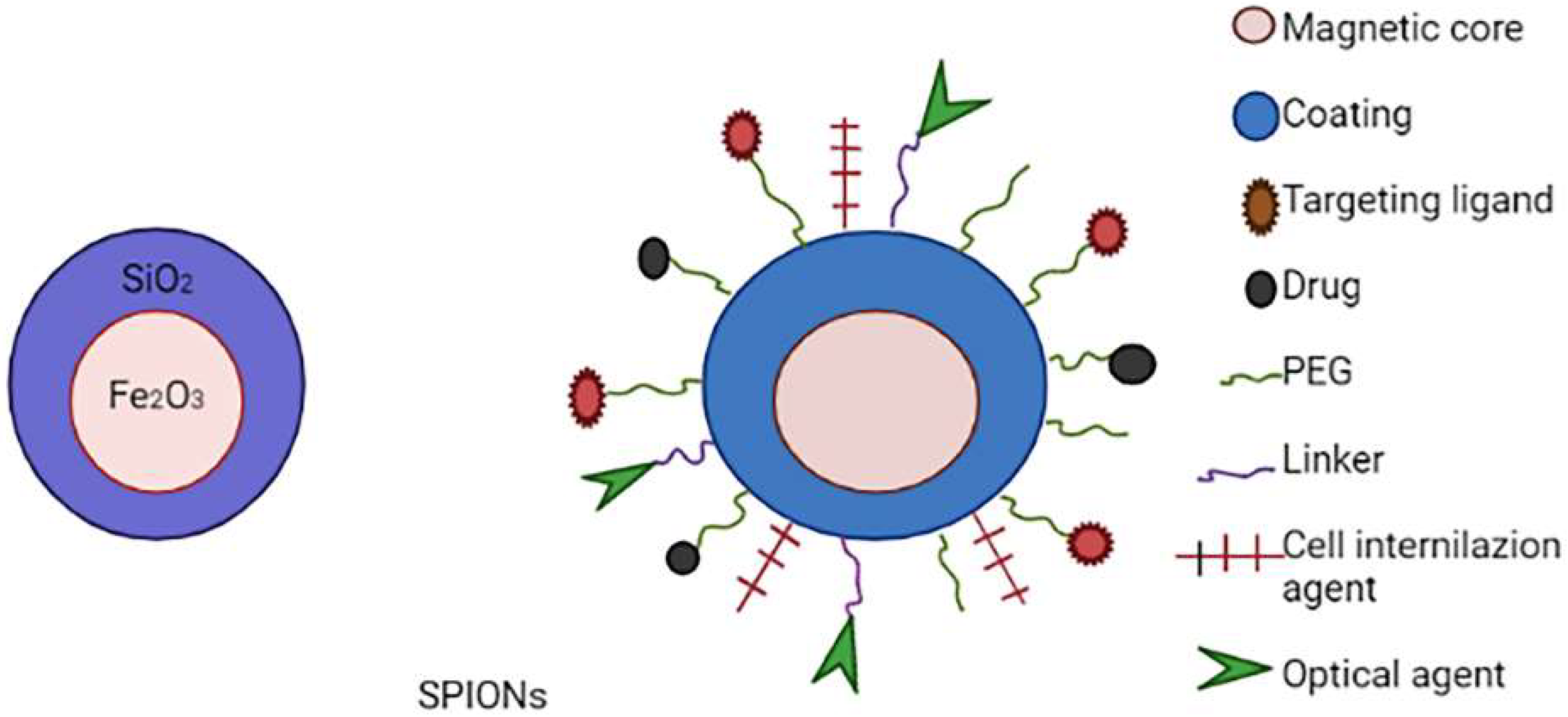
3.7. Superparamagnetic Iron Oxide Nanoparticlesd (SPIONs)
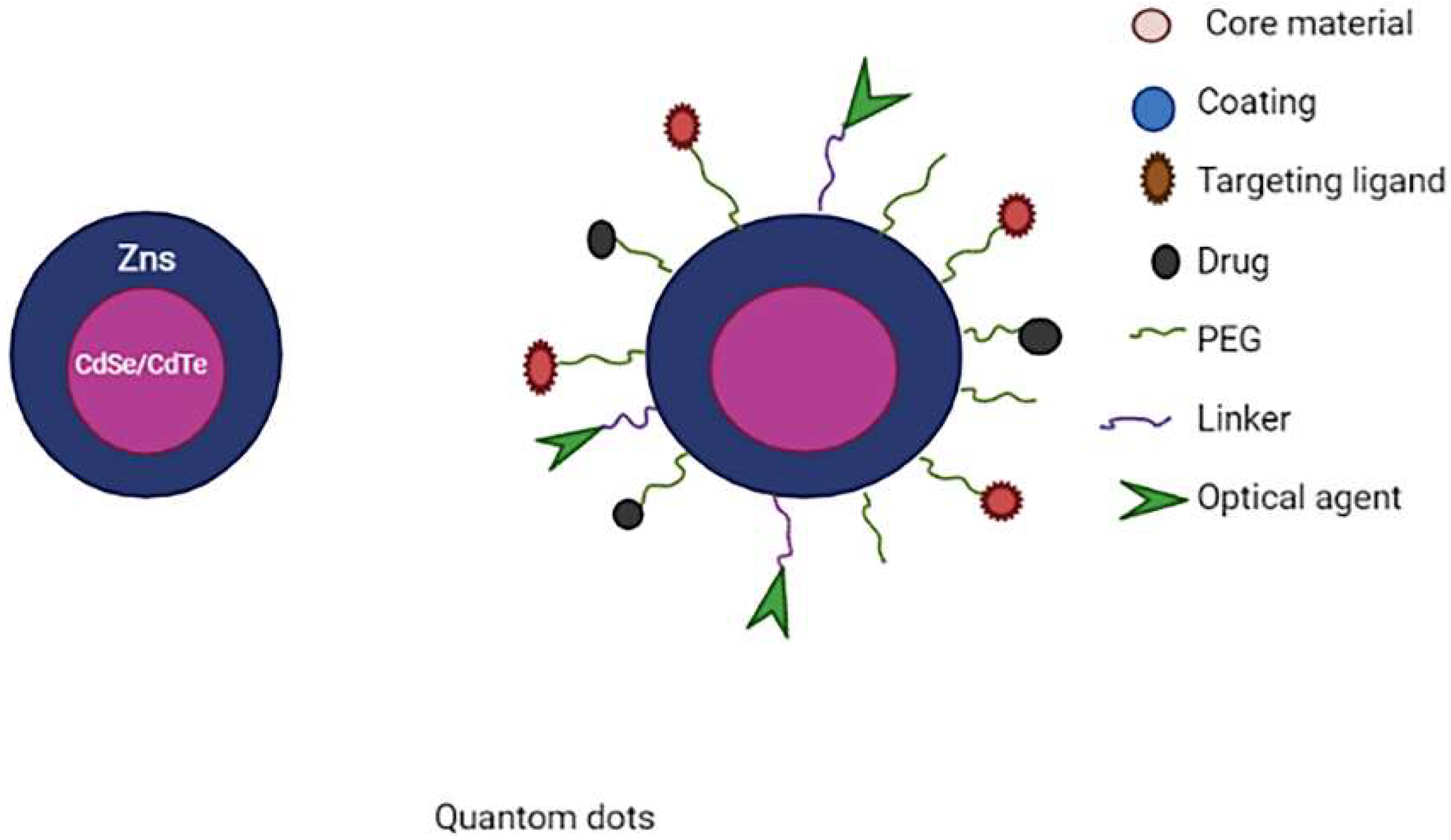
3.8. Quantum Dots (QDs)
4. Types of Targeting Moieties
4.1. Aptamer-Based Targeting
4.2. Small Molecule-Based Targeting
4.3. Peptide Based Targeting
4.4. Antibody-Based Targeting
5. Stimulus for Drug Release
5.1. Endogenous Stimulus
5.1.1. pH-Responsive Stimulus DDS
5.1.2. Redox-Sensitive Stimulus DDS
5.1.3. Enzyme Responsive Stimulus DDS
5.2. Exogenous Stimulus
5.2.1. Temperature Responsive Stimulus DDS
5.2.2. Light-Responsive Delivery Systems
5.2.3. Magnetic Field Responsive DDS
5.2.4. Ultra-Sound Responsive DDS
6. Nanomedicines: Development, Cost-Effectiveness and Commercialization
7. Future Perspectives in Cancer Treatment
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Pérez-Herrero, E.; Fernández-Medarde, A. Advanced targeted therapies in cancer: Drug nanocarriers, the future of chemotherapy. Eur. J. Pharm. Biopharm. 2015, 93, 52–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huda, S.; Alam, M.A.; Sharma, P.K. Smart nanocarriers-based drug delivery for cancer therapy: An innovative and developing strategy. J. Drug Deliv. Sci. Technol. 2020, 60, 102018. [Google Scholar] [CrossRef]
- Hossen, S.; Hossain, M.K.; Basher, M.K.; Mia, M.N.H.; Rahman, M.T.; Uddin, M.J. Smart nanocarrier-based drug delivery systems for cancer therapy and toxicity studies: A review. J. Adv. Res. 2019, 15, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sohrabi Kashani, A.; Packirisamy, M. Cancer-Nano-Interaction: From Cellular Uptake to Mechanobiological Responses. Int. J. Mol. Sci. 2021, 22, 9587. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.; Li, J.; Zhao, Q.; Pan, T.; Zhong, H.; Wang, W. Advanced and innovative nano-systems for anticancer targeted drug delivery. Pharmaceutics 2021, 13, 1151. [Google Scholar] [CrossRef]
- Bae, Y.H.; Park, K. Targeted drug delivery to tumors: Myths, reality and possibility. J. Control. Release 2011, 153, 198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, B.O.; Tai, H.C.; Xue, W.; Lee, L.J.; Lee, R.J. Receptor-targeted nanocarriers for therapeutic delivery to cancer. Mol. Membr. Biol. 2010, 27, 286–298. [Google Scholar] [CrossRef] [Green Version]
- Kumari, P.; Ghosh, B.; Biswas, S. Nanocarriers for cancer-targeted drug delivery. J. Drug Target. 2016, 24, 179–191. [Google Scholar] [CrossRef]
- Nakamura, Y.; Mochida, A.; Choyke, P.L.; Kobayashi, H. Nanodrug delivery: Is the enhanced permeability and retention effect sufficient for curing cancer? Bioconjug. Chem. 2016, 27, 2225–2238. [Google Scholar] [CrossRef]
- Albanese, A.; Tang, P.S.; Chan, W.C.W. The effect of nanoparticle size, shape and surface chemistry on biological systems. Annu. Rev. Biomed. Eng. 2012, 14, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Attia, M.F.; Anton, N.; Wallyn, J.; Omran, Z.; Vandamme, T.F. An overview of active and passive targeting strategies to improve the nanocarriers efficiency to tumour sites. J. Pharm. Pharmacol. 2019, 71, 1185–1198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gullotti, E.; Yeo, Y. Extracellularly activated nanocarriers: A new paradigm of tumor targeted drug delivery. Mol. Pharm. 2009, 6, 1041–1051. [Google Scholar] [CrossRef] [Green Version]
- Hansen, A.E.; Petersen, A.L.; Henriksen, J.R.; Boerresen, B.; Rasmussen, P.; Elema, D.R.; af Rosenschöld, P.M.; Kristensen, A.T.; Kjær, A.; Andresen, T.L. Positron Emission Tomography Based Elucidation of the Enhanced Permeability and Retention Effect in Dogs with Cancer Using Copper-64 Liposomes. ACS Nano 2015, 9, 6985–6995. [Google Scholar] [CrossRef] [Green Version]
- Blanco, E.; Shen, H.; Ferrari, M. Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nat. Biotechnol. 2015, 33, 941–951. [Google Scholar] [CrossRef] [PubMed]
- Iyer, A.K.; Khaled, G.; Fang, J.; Maeda, H. Exploiting the enhanced permeability and retention effect for tumor targeting. Drug Discov. Today 2006, 11, 812–818. [Google Scholar] [CrossRef]
- Kumar Khanna, V. Targeted delivery of nanomedicines. ISRN Pharmacol. 2012, 2012, 571394. [Google Scholar] [CrossRef] [Green Version]
- Park, J.W.; Hong, K.; Kirpotin, D.B.; Colbern, G.; Shalaby, R.; Baselga, J.; Shao, Y.; Nielsen, U.B.; Marks, J.D.; Moore, D. Anti-HER2 immunoliposomes: Enhanced efficacy attributable to targeted delivery. Clin. Cancer Res. 2002, 8, 1172–1181. [Google Scholar]
- Cai, H.; Dai, X.; Wang, X.; Tan, P.; Gu, L.; Luo, Q.; Zheng, X.; Li, Z.; Zhu, H.; Zhang, H. A nanostrategy for efficient imaging-guided antitumor therapy through a stimuli-responsive branched polymeric prodrug. Adv. Sci. 2020, 7, 1903243. [Google Scholar] [CrossRef]
- Xu, K.; Wang, M.; Tang, W.; Ding, Y.; Hu, A. Flash nanoprecipitation with Gd(III)-based metallosurfactants to fabricate polylactic acid nanoparticles as highly efficient contrast agents for magnetic resonance imaging. Chem. Asian J. 2020, 15, 2475–2479. [Google Scholar] [CrossRef]
- Jain, A.; Kumari, R.; Tiwari, A.; Verma, A.; Tripathi, A.; Shrivastava, A.; Jain, S.K. Nanocarrier based advances in drug delivery to tumor: An overview. Curr. Drug Targets 2018, 19, 1498–1518. [Google Scholar] [CrossRef]
- Mu, L.-M.; Ju, R.-J.; Liu, R.; Bu, Y.-Z.; Zhang, J.-Y.; Li, X.-Q.; Zeng, F.; Lu, W.-L. Dual-functional drug liposomes in treatment of resistant cancers. Adv. Drug Deliv. Rev. 2017, 115, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Hurkat, P.; Jain, S.K. Development of liposomes using formulation by design: Basics to recent advances. Chem. Phys. Lipids 2019, 224, 104764. [Google Scholar] [CrossRef] [PubMed]
- Alwattar, J.K.; Mneimneh, A.T.; Abla, K.K.; Mehanna, M.M.; Allam, A.N. Smart stimuli-responsive liposomal nanohybrid systems: A critical review of theranostic behavior in cancer. Pharmaceutics 2021, 13, 355. [Google Scholar] [CrossRef]
- Li, M.; Du, C.; Guo, N.; Teng, Y.; Meng, X.; Sun, H.; Li, S.; Yu, P.; Galons, H. Composition design and medical application of liposomes. Eur. J. Med. Chem. 2019, 164, 640–653. [Google Scholar] [CrossRef] [PubMed]
- Paolino, D.; Cosco, D.; Gaspari, M.; Celano, M.; Wolfram, J.; Voce, P.; Puxeddu, E.; Filetti, S.; Celia, C.; Ferrari, M. Targeting the thyroid gland with thyroid-stimulating hormone (TSH)-nanoliposomes. Biomaterials 2014, 35, 7101–7109. [Google Scholar] [CrossRef] [Green Version]
- Brown, B.S.; Patanam, T.; Mobli, K.; Celia, C.; Zage, P.E.; Bean, A.J.; Tasciotti, E. Etoposide-loaded immunoliposomes as active targeting agents for GD2-positive malignancies. Cancer Biol. Ther. 2014, 15, 851–861. [Google Scholar] [CrossRef] [Green Version]
- De Pauw, B.E. Fungal infections: Diagnostic problems and choice of therapy. Leuk. Suppl. 2012, 1, S22–S23. [Google Scholar] [CrossRef]
- Jain, A.; Jain, S.K. Stimuli-responsive smart liposomes in cancer targeting. Curr. Drug Targets 2018, 19, 259–270. [Google Scholar] [CrossRef]
- Jain, A.; Tiwari, A.; Verma, A.; Jain, S.K. Ultrasound-based triggered drug delivery to tumors. Drug Deliv. Transl. Res. 2018, 8, 150–164. [Google Scholar] [CrossRef]
- Moosavian, S.A.; Sahebkar, A. Aptamer-functionalized liposomes for targeted cancer therapy. Cancer Lett. 2019, 448, 144–154. [Google Scholar] [CrossRef] [PubMed]
- Di Francesco, M.; Celia, C.; Primavera, R.; D’Avanzo, N.; Locatelli, M.; Fresta, M.; Cilurzo, F.; Ventura, C.A.; Paolino, D.; Di Marzio, L. Physicochemical characterization of pH-responsive and fusogenic self-assembled non-phospholipid vesicles for a potential multiple targeting therapy. Int. J. Pharm. 2017, 528, 18–32. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.; Im, H.-J. Theranostics based on liposome: Looking back and forward. Nucl. Med. Mol. Imaging 2019, 53, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Pasut, G.; Paolino, D.; Celia, C.; Mero, A.; Joseph, A.S.; Wolfram, J.; Cosco, D.; Schiavon, O.; Shen, H.; Fresta, M. Polyethylene glycol (PEG)-dendron phospholipids as innovative constructs for the preparation of super stealth liposomes for anticancer therapy. J. Control. Release 2015, 199, 106–113. [Google Scholar] [CrossRef]
- Tu, A.B.; Lewis, J.S. Biomaterial-based immunotherapeutic strategies for rheumatoid arthritis. Drug Deliv. Transl. Res. 2021, 11, 2371–2393. [Google Scholar] [CrossRef] [PubMed]
- Paliwal, S.R.; Paliwal, R.; Vyas, S.P. A review of mechanistic insight and application of pH-sensitive liposomes in drug delivery. Drug Deliv. 2015, 22, 231–242. [Google Scholar] [CrossRef] [PubMed]
- Riaz, M.K.; Riaz, M.A.; Zhang, X.; Lin, C.; Wong, K.H.; Chen, X.; Zhang, G.; Lu, A.; Yang, Z. Surface functionalization and targeting strategies of liposomes in solid tumor therapy: A review. Int. J. Mol. Sci. 2018, 19, 195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paliwal, S.R.; Paliwal, R.; Agrawal, G.P.; Vyas, S.P. Hyaluronic acid modified pH-sensitive liposomes for targeted intracellular delivery of doxorubicin. J. Liposome Res. 2016, 26, 276–287. [Google Scholar] [CrossRef]
- Crain, M.L. Daunorubicin & Cytarabine liposome (vyxeosTM). Oncol. Times 2018, 40, 30. [Google Scholar]
- Fan, Y.; Zhang, Q. Development of liposomal formulations: From concept to clinical investigations. Asian J. Pharm. Sci. 2013, 8, 81–87. [Google Scholar] [CrossRef] [Green Version]
- Kopeckova, K.; Eckschlager, T.; Sirc, J.; Hobzova, R.; Plch, J.; Hrabeta, J.; Michalek, J. Nanodrugs used in cancer therapy. Biomed. Pap. Med. 2019, 163, 122–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghaffari, M.; Dehghan, G.; Abedi-Gaballu, F.; Kashanian, S.; Baradaran, B.; Ezzati Nazhad Dolatabadi, J.; Losic, D. Surface functionalized dendrimers as controlled-release delivery nanosystems for tumor targeting. Eur. J. Pharm. Sci. 2018, 122, 311–330. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Z.; Cooper, S.L. Recent advances in antimicrobial dendrimers. Adv. Mater. 2000, 12, 843–846. [Google Scholar] [CrossRef]
- Sheikh, A.; Kesharwani, P. An insight into aptamer engineered dendrimer for cancer therapy. Eur. Polym. J. 2021, 159, 110746. [Google Scholar] [CrossRef]
- Moradi, M.; Abdolhosseini, M.; Zarrabi, A. A review on application of Nano-structures and Nano-objects with high potential for managing different aspects of bone malignancies. Nano-Struct. Nano-Objects 2019, 19, 100348. [Google Scholar] [CrossRef]
- Wolinsky, J.B.; Grinstaff, M.W. Therapeutic and diagnostic applications of dendrimers for cancer treatment. Adv. Drug Deliv. Rev. 2008, 60, 1037–1055. [Google Scholar] [CrossRef] [PubMed]
- Khemtong, C.; Kessinger, C.W.; Gao, J. Polymeric nanomedicine for cancer MR imaging and drug delivery. Chem. Commun. 2009, 3497–3510. [Google Scholar] [CrossRef]
- Bazak, R.; Houri, M.; El Achy, S.; Kamel, S.; Refaat, T. Cancer active targeting by nanoparticles: A comprehensive review of literature. J. Cancer Res. Clin. Oncol. 2015, 141, 769–784. [Google Scholar] [CrossRef] [Green Version]
- Gupta, U.; Dwivedi, S.K.D.; Bid, H.K.; Konwar, R.; Jain, N.K. Ligand anchored dendrimers based nanoconstructs for effective targeting to cancer cells. Int. J. Pharm. 2010, 393, 186–197. [Google Scholar] [CrossRef]
- Mura, S.; Nicolas, J.; Couvreur, P. Stimuli-responsive nanocarriers for drug delivery. Nat. Mater. 2013, 12, 991–1003. [Google Scholar] [CrossRef]
- Ambekar, R.S.; Choudhary, M.; Kandasubramanian, B. Recent advances in dendrimer-based nanoplatform for cancer treatment: A review. Eur. Polym. J. 2020, 126, 109546. [Google Scholar] [CrossRef]
- Lai, P.-S.; Lou, P.-J.; Peng, C.-L.; Pai, C.-L.; Yen, W.-N.; Huang, M.-Y.; Young, T.-H.; Shieh, M.-J. Doxorubicin delivery by polyamidoamine dendrimer conjugation and photochemical internalization for cancer therapy. J. Control. Release 2007, 122, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Alam, F.; Naim, M.; Aziz, M.; Yadav, N. Unique roles of nanotechnology in medicine and cancer-II. Indian J. Cancer 2015, 52, 1. [Google Scholar] [CrossRef] [PubMed]
- Mu, W.; Chu, Q.; Liu, Y.; Zhang, N. A review on nano-based drug delivery system for cancer chemoimmunotherapy. Nano-Micro Lett. 2020, 12, 1. [Google Scholar] [CrossRef] [PubMed]
- Fan, W.; Zhang, L.; Li, Y.; Wu, H. Recent progress of crosslinking strategies for polymeric micelles with enhanced drug delivery in cancer therapy. Curr. Med. Chem. 2019, 26, 2356–2376. [Google Scholar] [CrossRef] [PubMed]
- Alven, S.; Aderibigbe, B.A. The therapeutic efficacy of dendrimer and micelle formulations for breast cancer treatment. Pharmaceutics 2020, 12, 1212. [Google Scholar] [CrossRef] [PubMed]
- Das, A.; Gupta, N.V.; Gowda, D.V.; Bhosale, R.R. A Review on pH-Sensitive Polymeric Nanoparticles for Cancer Therapy. Int. J. ChemTech Res. 2017, 10, 575–588. [Google Scholar]
- Seo, S.; Lee, S.; Choi, S.; Kim, H. Tumor-Targeting Co-Delivery of Drug and Gene from Temperature-Triggered Micelles. Macromol. Biosci. 2015, 15, 1198–1204. [Google Scholar] [CrossRef]
- Nishiyama, N.; Kataoka, K. Current state, achievements and future prospects of polymeric micelles as nanocarriers for drug and gene delivery. Pharmacol. Ther. 2006, 112, 630–648. [Google Scholar] [CrossRef]
- Wan, X.; Beaudoin, J.J.; Vinod, N.; Min, Y.; Makita, N.; Bludau, H.; Jordan, R.; Wang, A.; Sokolsky, M.; Kabanov, A.V. Co-delivery of paclitaxel and cisplatin in poly (2-oxazoline) polymeric micelles: Implications for drug loading, release, pharmacokinetics and outcome of ovarian and breast cancer treatments. Biomaterials 2019, 192, 1–14. [Google Scholar] [CrossRef]
- Razzaq, S.; Rauf, A.; Raza, A.; Akhtar, S.; Tabish, T.A.; Sandhu, M.A.; Zaman, M.; Ibrahim, I.M.; Shahnaz, G.; Rahdar, A.; et al. A Multifunctional Polymeric Micelle for Targeted Delivery of Paclitaxel by the Inhibition of the P-Glycoprotein Transporters. Nanomaterials 2021, 11, 2858. [Google Scholar] [CrossRef]
- Liao, Z.; Wong, S.W.; Yeo, H.L.; Zhao, Y. Nanocarriers for cancer treatment: Clinical impact and safety. NanoImpact 2020, 20, 100253. [Google Scholar] [CrossRef]
- Ahmed, W.; Elhissi, A.; Dhanak, V.; Subramani, K. Carbon nanotubes: Applications in cancer therapy and drug delivery research. In Emerging Nanotechnologies in Dentistry; Elsevier: Amsterdam, The Netherlands, 2018; pp. 371–389. [Google Scholar]
- Beg, S.; Rizwan, M.; Sheikh, A.M.; Hasnain, M.S.; Anwer, K.; Kohli, K. Advancement in carbon nanotubes: Basics, biomedical applications and toxicity. J. Pharm. Pharmacol. 2011, 63, 141–163. [Google Scholar] [CrossRef] [PubMed]
- Ali-Boucetta, H.; Al-Jamal, K.T.; McCarthy, D.; Prato, M.; Bianco, A.; Kostarelos, K. Multiwalled carbon nanotube–doxorubicin supramolecular complexes for cancer therapeutics. Chem. Commun. 2008, 459–461. [Google Scholar] [CrossRef]
- Arsawang, U.; Saengsawang, O.; Rungrotmongkol, T.; Sornmee, P.; Wittayanarakul, K.; Remsungnen, T.; Hannongbua, S. How do carbon nanotubes serve as carriers for gemcitabine transport in a drug delivery system? J. Mol. Graph. Model. 2011, 29, 591–596. [Google Scholar] [CrossRef]
- Son, K.H.; Hong, J.H.; Lee, J.W. Carbon nanotubes as cancer therapeutic carriers and mediators. Int. J. Nanomed. 2016, 11, 5163. [Google Scholar] [CrossRef] [Green Version]
- Kiran, A.R.; Kumari, G.K.; Krishnamurthy, P.T. Carbon nanotubes in drug delivery: Focus on anticancer therapies. J. Drug Deliv. Sci. Technol. 2020, 59, 101892. [Google Scholar] [CrossRef]
- Dizaji, B.F.; Farboudi, A.; Rahbar, A.; Azarbaijan, M.H.; Asgary, M.R. The role of single-and multi-walled carbon nanotube in breast cancer treatment. Ther. Deliv. 2020, 11, 653. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Hu, J.; Yang, D.; Long, J.; Luo, G.; Jin, C.; Yu, X.; Xu, J.; Wang, C.; Ni, Q. Pilot study of targeting magnetic carbon nanotubes to lymph nodes. Nanomedicine 2009, 4, 317–330. [Google Scholar] [CrossRef]
- Li, Z.; de Barros, A.L.B.; Soares, D.C.F.; Moss, S.N.; Alisaraie, L. Functionalized single-walled carbon nanotubes: Cellular uptake, biodistribution and applications in drug delivery. Int. J. Pharm. 2017, 524, 41–54. [Google Scholar] [CrossRef]
- Lay, C.L.; Liu, J.; Liu, Y. Functionalized carbon nanotubes for anticancer drug delivery. Expert Rev. Med. Devices 2011, 8, 561–566. [Google Scholar] [CrossRef]
- Karimi, M.; Solati, N.; Ghasemi, A.; Estiar, M.A.; Hashemkhani, M.; Kiani, P.; Mohamed, E.; Saeidi, A.; Taheri, M.; Avci, P. Carbon nanotubes part II: A remarkable carrier for drug and gene delivery. Expert Opin. Drug Deliv. 2015, 12, 1089–1105. [Google Scholar] [CrossRef] [PubMed]
- Varkouhi, A.K.; Foillard, S.; Lammers, T.; Schiffelers, R.M.; Doris, E.; Hennink, W.E.; Storm, G. SiRNA delivery with functionalized carbon nanotubes. Int. J. Pharm. 2011, 416, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; Al-Jamal, W.T.; Toma, F.M.; Bianco, A.; Prato, M.; Al-Jamal, K.T.; Kostarelos, K. Design of cationic multiwalled carbon nanotubes as efficient siRNA vectors for lung cancer xenograft eradication. Bioconjug. Chem. 2015, 26, 1370–1379. [Google Scholar] [CrossRef] [PubMed]
- JSSchiffman SR, M. Tumor targeting with antibody-functionalized, radiolabeled carbon nanotubes. J. Nucl. Med. 2007, 48, 11801189. [Google Scholar]
- Augustine, S.; Singh, J.; Srivastava, M.; Sharma, M.; Das, A.; Malhotra, B.D. Recent advances in carbon based nanosystems for cancer theranostics. Biomater. Sci. 2017, 5, 901–952. [Google Scholar] [CrossRef]
- Lim, Z.-Z.J.; Li, J.-E.J.; Ng, C.-T.; Yung, L.-Y.L.; Bay, B.-H. Gold nanoparticles in cancer therapy. Acta Pharmacol. Sin. 2011, 32, 983–990. [Google Scholar] [CrossRef] [Green Version]
- Lewinski, N.; Colvin, V.; Drezek, R. Cytotoxicity of nanoparticles. Small 2008, 4, 26–49. [Google Scholar] [CrossRef]
- Li, W.; Cao, Z.; Liu, R.; Liu, L.; Li, H.; Li, X.; Chen, Y.; Lu, C.; Liu, Y. AuNPs as an important inorganic nanoparticle applied in drug carrier systems. Artif. Cells Nanomed. Biotechnol. 2019, 47, 4222–4233. [Google Scholar] [CrossRef] [Green Version]
- Wang, F.; Li, C.; Cheng, J.; Yuan, Z. Recent advances on inorganic nanoparticle-based cancer therapeutic agents. Int. J. Environ. Res. Public Health 2016, 13, 1182. [Google Scholar] [CrossRef]
- Singh, P.; Pandit, S.; Mokkapati, V.R.S.S.; Garg, A.; Ravikumar, V.; Mijakovic, I. Gold Nanoparticles in Diagnostics and Therapeutics for Human Cancer. Int. J. Mol. Sci. 2018, 19, 1979. [Google Scholar] [CrossRef]
- Ajnai, G.; Chiu, A.; Kan, T.; Cheng, C.C.; Tsai, T.H.; Chang, J. Trends of Gold Nanoparticle-based Drug Delivery System in Cancer Therapy. J. Exp. Clin. Med. 2014, 6, 172–178. [Google Scholar] [CrossRef]
- Kong, F.-Y.; Zhang, J.-W.; Li, R.-F.; Wang, Z.-X.; Wang, W.-J.; Wang, W. Unique roles of gold nanoparticles in drug delivery, targeting and imaging applications. Molecules 2017, 22, 1445. [Google Scholar] [CrossRef] [Green Version]
- Pawar, H.R.; Bhosale, S.S.; Derle, N.D. Use of liposomes in cancer therapy: A review. Int. J. Pharm. Sci. Res. 2012, 3, 3585–3590. [Google Scholar]
- Xin, J.; Wang, S.; Wang, B.; Wang, J.; Wang, J.; Zhang, L.; Xin, B.; Shen, L.; Zhang, Z.; Yao, C. AlPcS(4)-PDT for gastric cancer therapy using gold nanorod, cationic liposome and Pluronic(®) F127 nanomicellar drug carriers. Int. J. Nanomed. 2018, 13, 2017–2036. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barani, M.; Hosseinikhah, S.M.; Rahdar, A.; Farhoudi, L.; Arshad, R.; Cucchiarini, M.; Pandey, S. Nanotechnology in Bladder Cancer: Diagnosis and Treatment. Cancers 2021, 13, 2214. [Google Scholar] [CrossRef]
- Yafout, M.; Ousaid, A.; Khayati, Y.; El Otmani, I.S. Gold nanoparticles as a drug delivery system for standard chemotherapeutics: A new lead for targeted pharmacological cancer treatments. Sci. Afr. 2021, 11, e00685. [Google Scholar] [CrossRef]
- Chen, F.; Hong, H.; Shi, S.; Goel, S.; Valdovinos, H.F.; Hernandez, R.; Theuer, C.P.; Barnhart, T.E.; Cai, W. Engineering of hollow mesoporous silica nanoparticles for remarkably enhanced tumor active targeting efficacy. Sci. Rep. 2014, 4, 5080. [Google Scholar] [CrossRef]
- Barabadi, H.; Vahidi, H.; Mahjoub, M.A.; Kosar, Z.; Kamali, K.D.; Ponmurugan, K.; Hosseini, O.; Rashedi, M.; Saravanan, M. Emerging antineoplastic gold nanomaterials for cervical Cancer therapeutics: A systematic review. J. Clust. Sci. 2019, 31, 1173–1184. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, Q.; Han, N.; Bai, L.; Li, J.; Liu, J.; Che, E.; Hu, L.; Zhang, Q.; Jiang, T. Mesoporous silica nanoparticles in drug delivery and biomedical applications. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 313–327. [Google Scholar] [CrossRef]
- Yang, S.; Chen, D.; Li, N.; Xu, Q.; Li, H.; Gu, F.; Xie, J.; Lu, J. Hollow mesoporous silica nanocarriers with multifunctional capping agents for in vivo cancer imaging and therapy. Small 2016, 12, 360–370. [Google Scholar] [CrossRef]
- Feng, Y.; Panwar, N.; Tng, D.J.H.; Tjin, S.C.; Wang, K.; Yong, K.-T. The application of mesoporous silica nanoparticle family in cancer theranostics. Coord. Chem. Rev. 2016, 319, 86–109. [Google Scholar] [CrossRef]
- Chan, M.-H.; Lin, H.-M. Preparation and identification of multifunctional mesoporous silica nanoparticles for in vitro and in vivo dual-mode imaging, theranostics and targeted tracking. Biomaterials 2015, 46, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Möller, K.; Bein, T. Talented mesoporous silica nanoparticles. Chem. Mater. 2017, 29, 371–388. [Google Scholar] [CrossRef]
- Liu, Q.; Xia, W. Mesoporous silica nanoparticles for cancer therapy. In New Advances on Disease Biomarkers and Molecular Targets in Biomedicine; Springer: Singapore, 2013; pp. 231–242. [Google Scholar]
- Xu, C.; Chen, F.; Valdovinos, H.F.; Jiang, D.; Goel, S.; Yu, B.; Sun, H.; Barnhart, T.E.; Moon, J.J.; Cai, W. Bacteria-like mesoporous silica-coated gold nanorods for positron emission tomography and photoacoustic imaging-guided chemo-photothermal combined therapy. Biomaterials 2018, 165, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Shen, X.; Geng, Y.; Chen, Z.; Li, L.; Li, S.; Yang, H.; Wu, C.; Zeng, H.; Liu, Y. Folate-Functionalized Magnetic-Mesoporous Silica Nanoparticles for Drug/Gene Codelivery to Potentiate the Antitumor Efficacy. ACS Appl. Mater. Interfaces 2016, 8, 13748–13758. [Google Scholar] [CrossRef]
- Yang, H.; Chen, Y.; Chen, Z.; Geng, Y.; Xie, X.; Shen, X.; Li, T.; Li, S.; Wu, C.; Liu, Y. Chemo-photodynamic combined gene therapy and dual-modal cancer imaging achieved by pH-responsive alginate/chitosan multilayer-modified magnetic mesoporous silica nanocomposites. Biomater. Sci. 2017, 5, 1001–1013. [Google Scholar] [CrossRef]
- Yang, H.; Li, Y.; Li, T.; Xu, M.; Chen, Y.; Wu, C.; Dang, X.; Liu, Y. Multifunctional core/shell nanoparticles cross-linked polyetherimide-folic acid as efficient Notch-1 siRNA carrier for targeted killing of breast cancer. Sci. Rep. 2014, 4, 7072. [Google Scholar] [CrossRef] [Green Version]
- Wang, Z.; Chang, Z.; Lu, M.; Shao, D.; Yue, J.; Yang, D.; Zheng, X.; Li, M.; He, K.; Zhang, M.; et al. Shape-controlled magnetic mesoporous silica nanoparticles for magnetically-mediated suicide gene therapy of hepatocellular carcinoma. Biomaterials 2018, 154, 147–157. [Google Scholar] [CrossRef]
- Li, X.; Chen, Y.; Wang, M.; Ma, Y.; Xia, W.; Gu, H. A mesoporous silica nanoparticle–PEI–fusogenic peptide system for siRNA delivery in cancer therapy. Biomaterials 2013, 34, 1391–1401. [Google Scholar] [CrossRef]
- Chen, L.; She, X.; Wang, T.; Shigdar, S.; Duan, W.; Kong, L. Mesoporous silica nanorods toward efficient loading and intracellular delivery of siRNA. J. Nanopart. Res. 2018, 20, 37. [Google Scholar] [CrossRef]
- Zhao, S.; Xu, M.; Cao, C.; Yu, Q.; Zhou, Y.; Liu, J. A redox-responsive strategy using mesoporous silica nanoparticles for co-delivery of siRNA and doxorubicin. J. Mater. Chem. B 2017, 5, 6908–6919. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Su, H.; Shi, W.; Liu, Y.; Sun, Y.; Ge, D. Functionalized poly (pyrrole-3-carboxylic acid) nanoneedles for dual-imaging guided PDT/PTT combination therapy. Biomaterials 2018, 167, 177–190. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Shi, S.; Goel, S.; Shen, X.; Xie, X.; Chen, Z.; Zhang, H.; Li, S.; Qin, X.; Yang, H. Recent advancements in mesoporous silica nanoparticles towards therapeutic applications for cancer. Acta Biomater. 2019, 89, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.; He, Y.; Bo, R.; Ma, Z.; Wang, Z.; Dong, L.; Lin, T.; Xue, X.; Li, Y. A facile approach to fabricate self-assembled magnetic nanotheranostics for drug delivery and imaging. Nanoscale 2018, 10, 21634–21639. [Google Scholar] [CrossRef] [PubMed]
- Cryer, A.M.; Thorley, A.J. Nanotechnology in the diagnosis and treatment of lung cancer. Pharmacol. Ther. 2019, 198, 189–205. [Google Scholar] [CrossRef] [PubMed]
- Balk, M.; Haus, T.; Band, J.; Unterweger, H.; Schreiber, E.; Friedrich, R.P.; Alexiou, C.; Gostian, A.O. Cellular SPION uptake and toxicity in various head and neck cancer cell lines. Nanomaterials 2021, 11, 726. [Google Scholar] [CrossRef] [PubMed]
- Solar, P.; González, G.; Vilos, C.; Herrera, N.; Juica, N.; Moreno, M.; Simon, F.; Velásquez, L. Multifunctional polymeric nanoparticles doubly loaded with SPION and ceftiofur retain their physical and biological properties. J. Nanobiotechnol. 2015, 13, 14. [Google Scholar] [CrossRef] [Green Version]
- Chomoucka, J.; Drbohlavova, J.; Huska, D.; Adam, V.; Kizek, R.; Hubalek, J. Magnetic nanoparticles and targeted drug delivering. Pharmacol. Res. 2010, 62, 144–149. [Google Scholar] [CrossRef]
- Liang, R.; Wei, M.; Evans, D.G.; Duan, X. Inorganic nanomaterials for bioimaging, targeted drug delivery and therapeutics. Chem. Commun. 2014, 50, 14071–14081. [Google Scholar] [CrossRef]
- Kang, T.; Li, F.; Baik, S.; Shao, W.; Ling, D.; Hyeon, T. Surface design of magnetic nanoparticles for stimuli-responsive cancer imaging and therapy. Biomaterials 2017, 136, 98–114. [Google Scholar] [CrossRef]
- Zou, P.; Yu, Y.; Wang, Y.A.; Zhong, Y.; Welton, A.; Galbán, C.; Wang, S.; Sun, D. Superparamagnetic iron oxide nanotheranostics for targeted cancer cell imaging and pH-dependent intracellular drug release. Mol. Pharm. 2010, 7, 1974–1984. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhi, D.; Zhao, Y.; Cui, S.; Chen, H.; Zhang, S. Conjugates of small targeting molecules to non-viral vectors for the mediation of siRNA. Acta Biomater. 2016, 36, 21–41. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Zhou, Z.; Mao, H.; Yang, L. Magnetic nanoparticles for precision oncology: Theranostic magnetic iron oxide nanoparticles for image-guided and targeted cancer therapy. Nanomedicine 2017, 12, 73–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, Y.; Zhong, Y.; Wang, J.; Su, Y.; Peng, F.; Zhou, Y.; Jiang, X.; He, Y. Aqueous synthesized near-infrared-emitting quantum dots for RGD-based in vivo active tumour targeting. Nanotechnology 2013, 24, 135101. [Google Scholar] [CrossRef]
- Ghasemi, Y.; Peymani, P.; Afifi, S. Quantum dot: Magic nanoparticle for imaging, detection and targeting. Acta Biomed. 2009, 80, 156–165. [Google Scholar]
- Mashinchian, O.; Johari-Ahar, M.; Ghaemi, B.; Rashidi, M.; Barar, J.; Omidi, Y. Impacts of quantum dots in molecular detection and bioimaging of cancer. BioImpacts 2014, 4, 149. [Google Scholar] [CrossRef] [Green Version]
- Liu, L.; Yong, K.-T.; Roy, I.; Law, W.-C.; Ye, L.; Liu, J.; Liu, J.; Kumar, R.; Zhang, X.; Prasad, P.N. Bioconjugated pluronic triblock-copolymer micelle-encapsulated quantum dots for targeted imaging of cancer: In vitro and in vivo studies. Theranostics 2012, 2, 705. [Google Scholar] [CrossRef] [Green Version]
- Ulusoy, M.; Jonczyk, R.; Walter, J.-G.; Springer, S.; Lavrentieva, A.; Stahl, F.; Green, M.; Scheper, T. Aqueous synthesis of PEGylated quantum dots with increased colloidal stability and reduced cytotoxicity. Bioconjug. Chem. 2016, 27, 414–426. [Google Scholar] [CrossRef]
- Vibin, M.; Vinayakan, R.; Fernandez, F.B.; John, A.; Abraham, A. A novel fluorescent quantum dot probe for the rapid diagnostic high contrast imaging of tumor in mice. J. Fluoresc. 2017, 27, 669–677. [Google Scholar] [CrossRef]
- Kim, J.; Huy, B.T.; Sakthivel, K.; Choi, H.J.; Joo, W.H.; Shin, S.K.; Lee, M.J.; Lee, Y.-I. Highly fluorescent CdTe quantum dots with reduced cytotoxicity-A Robust biomarker. Sens. Bio-Sens. Res. 2015, 3, 46–52. [Google Scholar] [CrossRef] [Green Version]
- Singh, S.C.; Mishra, S.K.; Srivastava, R.K.; Gopal, R. Optical properties of selenium quantum dots produced with laser irradiation of water suspended Se nanoparticles. J. Phys. Chem. C 2010, 114, 17374–17384. [Google Scholar] [CrossRef]
- Li, K.; Zhao, X.; Wei, G.; Su, Z. Recent advances in the cancer bioimaging with graphene quantum dots. Curr. Med. Chem. 2018, 25, 2876–2893. [Google Scholar] [CrossRef]
- Namdari, P.; Negahdari, B.; Eatemadi, A. Synthesis, properties and biomedical applications of carbon-based quantum dots: An updated review. Biomed. Pharmacother. 2017, 87, 209–222. [Google Scholar] [CrossRef] [PubMed]
- Iannazzo, D.; Celesti, C.; Espro, C. Recent advances on graphene quantum dots as multifunctional nanoplatforms for cancer treatment. Biotech. J. 2021, 16, 1900422. [Google Scholar] [CrossRef]
- Yao, X.; Tian, Z.; Liu, J.; Zhu, Y.; Hanagata, N. Mesoporous silica nanoparticles capped with graphene quantum dots for potential chemo–photothermal synergistic cancer therapy. Langmuir 2017, 33, 591–599. [Google Scholar] [CrossRef]
- Kulkarni, N.S.; Guererro, Y.; Gupta, N.; Muth, A.; Gupta, V. Exploring potential of quantum dots as dual modality for cancer therapy and diagnosis. J. Drug Deliv. Sci. Technol. 2019, 49, 352–364. [Google Scholar] [CrossRef]
- Kim, M.; Kim, D.-M.; Kim, K.-S.; Jung, W.; Kim, D.-E. Applications of cancer cell-specific aptamers in targeted delivery of anticancer therapeutic agents. Molecules 2018, 23, 830. [Google Scholar] [CrossRef] [Green Version]
- Ma, Y.; Li, W.; Zhou, Z.; Qin, X.; Wang, D.; Gao, Y.; Yu, Z.; Yin, F.; Li, Z. Peptide-Aptamer Coassembly Nanocarrier for Cancer Therapy. Bioconjug. Chem. 2019, 30, 536–540. [Google Scholar] [CrossRef]
- Ravichandran, G.; Rengan, A.K. Aptamer-mediated nanotheranostics for cancer treatment: A review. ACS Appl. Nano Mater. 2020, 3, 9542. [Google Scholar] [CrossRef]
- Mou, Q.; Ma, Y.; Zhu, X.; Yan, D. A small molecule nanodrug consisting of amphiphilic targeting ligand-chemotherapy drug conjugate for targeted cancer therapy. J. Control. Release 2016, 230, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Steichen, S.D.; Caldorera-Moore, M.; Peppas, N.A. A review of current nanoparticle and targeting moieties for the delivery of cancer therapeutics. Eur. J. Pharm. Sci. 2013, 48, 416–427. [Google Scholar] [CrossRef] [Green Version]
- Xin, H.; Jiang, X.; Gu, J.; Sha, X.; Chen, L.; Law, K.; Chen, Y.; Wang, X.; Jiang, Y.; Fang, X. Angiopep-conjugated poly(ethylene glycol)-co-poly(ε-caprolactone) nanoparticles as dual-targeting drug delivery system for brain glioma. Biomaterials 2011, 32, 4293–4305. [Google Scholar] [CrossRef] [PubMed]
- Yousefpour, P.; McDaniel, J.R.; Prasad, V.; Ahn, L.; Li, X.; Subrahmanyan, R.; Weitzhandler, I.; Suter, S.; Chilkoti, A. Genetically Encoding Albumin Binding into Chemotherapeutic-loaded Polypeptide Nanoparticles Enhances Their Antitumor Efficacy. Nano Lett. 2018, 18, 7784–7793. [Google Scholar] [CrossRef] [PubMed]
- Van Cutsem, E.; Köhne, C.-H.; Hitre, E.; Zaluski, J.; Chang Chien, C.-R.; Makhson, A.; D’Haens, G.; Pintér, T.; Lim, R.; Bodoky, G. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N. Engl. J. Med. 2009, 360, 1408–1417. [Google Scholar] [CrossRef] [Green Version]
- Yao, V.J.; D’Angelo, S.; Butler, K.S.; Theron, C.; Smith, T.L.; Marchiò, S.; Gelovani, J.G.; Sidman, R.L.; Dobroff, A.S.; Brinker, C.J. Ligand-targeted theranostic nanomedicines against cancer. J. Control. Release 2016, 240, 267–286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arslan, F.B.; Ozturk Atar, K.; Calis, S. Antibody-mediated drug delivery. Int. J. Pharm. 2021, 596, 120268. [Google Scholar] [CrossRef]
- Liu, M.; Du, H.; Zhang, W.; Zhai, G. Internal stimuli-responsive nanocarriers for drug delivery: Design strategies and applications. Mater. Sci. Eng. C 2017, 71, 1267–1280. [Google Scholar] [CrossRef]
- Vander Heiden, M.G.; Cantley, L.C.; Thompson, C.B. Understanding the Warburg effect: The metabolic requirements of cell proliferation. Science 2009, 324, 1029–1033. [Google Scholar] [CrossRef] [Green Version]
- Karimi, M.; Ghasemi, A.; Zangabad, P.S.; Rahighi, R.; Basri, S.M.M.; Mirshekari, H.; Amiri, M.; Pishabad, Z.S.; Aslani, A.; Bozorgomid, M. Smart micro/nanoparticles in stimulus-responsive drug/gene delivery systems. Chem. Soc. Rev. 2016, 45, 1457–1501. [Google Scholar] [CrossRef] [Green Version]
- Lai, W.-F.; Shum, H.C. A stimuli-responsive nanoparticulate system using poly (ethylenimine)-graft-polysorbate for controlled protein release. Nanoscale 2016, 8, 517–528. [Google Scholar] [CrossRef] [PubMed]
- Pafiti, K.; Cui, Z.; Adlam, D.; Hoyland, J.; Freemont, A.J.; Saunders, B.R. Hydrogel composites containing sacrificial collapsed hollow particles as dual action pH-responsive biomaterials. Biomacromolecules 2016, 17, 2448–2458. [Google Scholar] [CrossRef] [Green Version]
- Jin, Y.; Song, L.; Su, Y.; Zhu, L.; Pang, Y.; Qiu, F.; Tong, G.; Yan, D.; Zhu, B.; Zhu, X. Oxime linkage: A robust tool for the design of pH-sensitive polymeric drug carriers. Biomacromolecules 2011, 12, 3460–3468. [Google Scholar] [CrossRef]
- Du, Y.; Chen, W.; Zheng, M.; Meng, F.; Zhong, Z. pH-sensitive degradable chimaeric polymersomes for the intracellular release of doxorubicin hydrochloride. Biomaterials 2012, 33, 7291–7299. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Huang, Y.; Kumar, A.; Tan, A.; Jin, S.; Mozhi, A.; Liang, X.-J. pH-sensitive nano-systems for drug delivery in cancer therapy. Biotechnol. Adv. 2014, 32, 693–710. [Google Scholar] [CrossRef] [PubMed]
- Du, J.-Z.; Du, X.-J.; Mao, C.-Q.; Wang, J. Tailor-made dual pH-sensitive polymer–doxorubicin nanoparticles for efficient anticancer drug delivery. J. Am. Chem. Soc. 2011, 133, 17560–17563. [Google Scholar] [CrossRef] [PubMed]
- Ren, D.; Kratz, F.; Wang, S. Protein nanocapsules containing doxorubicin as a pH-responsive delivery system. Small 2011, 7, 1051–1060. [Google Scholar] [CrossRef] [Green Version]
- Kanamala, M.; Wilson, W.R.; Yang, M.; Palmer, B.D.; Wu, Z. Mechanisms and biomaterials in pH-responsive tumour targeted drug delivery: A review. Biomaterials 2016, 85, 152–167. [Google Scholar] [CrossRef]
- Lee, J.M.; Park, H.; Oh, K.T.; Lee, E.S. pH-Responsive hyaluronated liposomes for docetaxel delivery. Int. J. Pharm. 2018, 547, 377–384. [Google Scholar] [CrossRef]
- Liu, W.T.; Yang, Y.; Shen, P.H.; Gao, X.J.; He, S.Q.; Liu, H.; Zhu, C.S. Facile and simple preparation of pH-sensitive chitosan-mesoporous silica nanoparticles for future breast cancer treatment. Express Polym. Lett. 2015, 9, 1068–1075. [Google Scholar] [CrossRef]
- Chiang, Y.-T.; Yen, Y.-W.; Lo, C.-L. Reactive oxygen species and glutathione dual redox-responsive micelles for selective cytotoxicity of cancer. Biomaterials 2015, 61, 150–161. [Google Scholar] [CrossRef]
- Belbekhouche, S.; Reinicke, S.; Espeel, P.; Du Prez, F.E.; Eloy, P.; Dupont-Gillain, C.; Jonas, A.M.; Demoustier-Champagne, S.; Glinel, K. Polythiolactone-Based Redox-Responsive Layers for the Reversible Release of Functional Molecules. ACS Appl. Mater. Interfaces 2014, 6, 22457–22466. [Google Scholar] [CrossRef]
- Zhao, N.; Lin, X.; Zhang, Q.; Ji, Z.; Xu, F. Redox-triggered gatekeeper-enveloped starlike hollow silica nanoparticles for intelligent delivery systems. Small 2015, 11, 6467–6479. [Google Scholar] [CrossRef]
- Kang, Y.; Ju, X.; Ding, L.-S.; Zhang, S.; Li, B.-J. Reactive oxygen species and glutathione dual redox-responsive supramolecular assemblies with controllable release capability. ACS Appl. Mater. Interfaces 2017, 9, 4475–4484. [Google Scholar] [CrossRef]
- Qin, B.; Liu, L.; Wu, X.; Liang, F.; Hou, T.; Pan, Y.; Song, S. mPEGylated solanesol micelles as redox-responsive nanocarriers with synergistic anticancer effect. Acta Biomater. 2017, 64, 211–222. [Google Scholar] [CrossRef]
- Chen, L.; Zhou, X.; Nie, W.; Zhang, Q.; Wang, W.; Zhang, Y.; He, C. Multifunctional Redox-Responsive Mesoporous Silica Nanoparticles for Efficient Targeting Drug Delivery and Magnetic Resonance Imaging. ACS Appl. Mater. Interfaces 2016, 8, 33829–33841. [Google Scholar] [CrossRef] [PubMed]
- Zheng, N.; Song, Z.; Liu, Y.; Zhang, R.; Zhang, R.; Yao, C.; Uckun, F.M.; Yin, L.; Cheng, J. Redox-responsive, reversibly-crosslinked thiolated cationic helical polypeptides for efficient siRNA encapsulation and delivery. J. Control. Release 2015, 205, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.-T.; Liu, Z.-K.; Zhu, Q.-L.; Rong, X.-H.; Liang, C.-L.; Wang, J.; Ma, D.; Sun, J.; Wang, G.-H. Redox-responsive nanocarriers for drug and gene co-delivery based on chitosan derivatives modified mesoporous silica nanoparticles. Colloids Surf. B Biointerfaces 2017, 155, 41–50. [Google Scholar] [CrossRef]
- Zhao, Y.; Berger, R.; Landfester, K.; Crespy, D. Double Redox-Responsive Release of Encoded and Encapsulated Molecules from Patchy Nanocapsules. Small 2015, 11, 2995–2999. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Li, X.; Du, X.; Wang, T. Redox-responsive micelles for triggered drug delivery and effective laryngopharyngeal cancer therapy. Int. J. Biol. Macromol. 2018, 112, 65–73. [Google Scholar] [CrossRef]
- Li, X.; Burger, S.; O’Connor, A.J.; Ong, L.; Karas, J.A.; Gras, S.L. An enzyme-responsive controlled release system based on a dual-functional peptide. Chem. Commun. 2016, 52, 5112–5115. [Google Scholar] [CrossRef]
- Zhu, S.; Nih, L.; Carmichael, S.T.; Lu, Y.; Segura, T. Enzyme-Responsive Delivery of Multiple Proteins with Spatiotemporal Control. Adv. Mater. 2015, 27, 3620–3625. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Zheng, B.; Chen, W.; Schalley, C.A. Enzyme-responsive pillar[5]arene-based polymer-substituted amphiphiles: Synthesis, self-assembly in water and application in controlled drug release. Chem. Commun. 2015, 51, 14901–14904. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Zhang, G.; Liu, S. Enzyme-responsive polymeric assemblies, nanoparticles and hydrogels. Chem. Soc. Rev. 2012, 41, 5933–5949. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Pan, D.; Li, J.; Hu, J.; Bains, A.; Guys, N.; Zhu, H.; Li, X.; Luo, K.; Gong, Q. Enzyme-responsive peptide dendrimer-gemcitabine conjugate as a controlled-release drug delivery vehicle with enhanced antitumor efficacy. Acta Biomater. 2017, 55, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Cai, H.; Jiang, L.; Hu, J.; Bains, A.; Hu, J.; Gong, Q.; Luo, K.; Gu, Z. Enzyme-Sensitive and Amphiphilic PEGylated Dendrimer-Paclitaxel Prodrug-Based Nanoparticles for Enhanced Stability and Anticancer Efficacy. ACS Appl. Mater. Interfaces 2017, 9, 6865–6877. [Google Scholar] [CrossRef]
- Li, N.; Li, N.; Yi, Q.; Luo, K.; Guo, C.; Pan, D.; Gu, Z. Amphiphilic peptide dendritic copolymer-doxorubicin nanoscale conjugate self-assembled to enzyme-responsive anti-cancer agent. Biomaterials 2014, 35, 9529–9545. [Google Scholar] [CrossRef]
- Lee, S.; Song, S.J.; Lee, J.; Ha, T.H.; Choi, J.S. Cathepsin B-Responsive Liposomes for Controlled Anticancer Drug Delivery in Hep G2 Cells. Pharmaceutics 2020, 12, 876. [Google Scholar] [CrossRef]
- Chen, K.-J.; Liang, H.-F.; Chen, H.-L.; Wang, Y.; Cheng, P.-Y.; Liu, H.-L.; Xia, Y.; Sung, H.-W. A thermoresponsive bubble-generating liposomal system for triggering localized extracellular drug delivery. ACS Nano 2013, 7, 438–446. [Google Scholar] [CrossRef]
- Shen, B.; Ma, Y.; Yu, S.; Ji, C. Smart multifunctional magnetic nanoparticle-based drug delivery system for cancer thermo-chemotherapy and intracellular imaging. ACS Appl. Mater. Interfaces 2016, 8, 24502–24508. [Google Scholar] [CrossRef]
- Poelma, S.O.; Oh, S.S.; Helmy, S.; Knight, A.S.; Burnett, G.L.; Soh, H.T.; Hawker, C.J.; de Alaniz, J. Controlled drug release to cancer cells from modular one-photon visible light-responsive micellar system. Chem. Commun. 2016, 52, 10525–10528. [Google Scholar] [CrossRef] [PubMed]
- Rwei, A.Y.; Wang, W.; Kohane, D.S. Photoresponsive nanoparticles for drug delivery. Nano Today 2015, 10, 451–467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taurin, S.; Almomen, A.A.; Pollak, T.; Kim, S.J.; Maxwell, J.; Peterson, C.M.; Owen, S.C.; Janát-Amsbury, M.M. Thermosensitive hydrogels a versatile concept adapted to vaginal drug delivery. J. Drug Target. 2018, 26, 533–550. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Fan, H.; Yin, L.; Zhang, J.; Dong, A.; Deng, L.; Tang, H. Thermosensitive hydrogel system assembled by PTX-loaded copolymer nanoparticles for sustained intraperitoneal chemotherapy of peritoneal carcinomatosis. Eur. J. Pharm. Biopharm. 2016, 104, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Allam, A.A.; Potter, S.J.; Bud’ko, S.L.; Shi, D.; Mohamed, D.F.; Habib, F.S.; Pauletti, G.M. Lipid-coated superparamagnetic nanoparticles for thermoresponsive cancer treatment. Int. J. Pharm. 2018, 548, 297–304. [Google Scholar] [CrossRef]
- Geng, Y.; Wang, Z.-F.; Lin, B.-P.; Yang, H. Amphiphilic Diblock Co-polymers Bearing a Cysteine Junction Group: Synthesis, Encapsulation of Inorganic Nanoparticles and Near-Infrared Photoresponsive Properties. Chemistry 2016, 22, 18197–18207. [Google Scholar] [CrossRef]
- Shiao, Y.-S.; Chiu, H.-H.; Wu, P.-H.; Huang, Y.-F. Aptamer-functionalized gold nanoparticles as photoresponsive nanoplatform for co-drug delivery. ACS Appl. Mater. Interfaces 2014, 6, 21832–21841. [Google Scholar] [CrossRef]
- Cai, W.; Gao, H.; Chu, C.; Wang, X.; Wang, J.; Zhang, P.; Lin, G.; Li, W.; Liu, G.; Chen, X. Engineering Phototheranostic Nanoscale Metal-Organic Frameworks for Multimodal Imaging-Guided Cancer Therapy. ACS Appl. Mater. Interfaces 2017, 9, 2040–2051. [Google Scholar] [CrossRef]
- Chung, J.W.; Lee, K.; Neikirk, C.; Nelson, C.M.; Priestley, R.D. Photoresponsive coumarin-stabilized polymeric nanoparticles as a detectable drug carrier. Small 2012, 8, 1693–1700. [Google Scholar] [CrossRef]
- Nahain, A.-A.; Lee, J.-E.; Jeong, J.H.; Park, S.Y. Photoresponsive fluorescent reduced graphene oxide by spiropyran conjugated hyaluronic acid for in vivo imaging and target delivery. Biomacromolecules 2013, 14, 4082–4090. [Google Scholar] [CrossRef]
- Yang, Y.; Velmurugan, B.; Liu, X.; Xing, B. NIR photoresponsive crosslinked upconverting nanocarriers toward selective intracellular drug release. Small 2013, 9, 2937–2944. [Google Scholar] [CrossRef]
- Zhang, A.; Hai, L.; Wang, T.; Cheng, H.; Li, M.; He, X.; Wang, K. NIR-triggered drug delivery system based on phospholipid coated ordered mesoporous carbon for synergistic chemo-photothermal therapy of cancer cells. Chin. Chem. Lett. 2020, 31, 3158–3162. [Google Scholar] [CrossRef]
- Hua, M.-Y.; Liu, H.-L.; Yang, H.-W.; Chen, P.-Y.; Tsai, R.-Y.; Huang, C.-Y.; Tseng, I.-C.; Lyu, L.-A.; Ma, C.-C.; Tang, H.-J.; et al. The effectiveness of a magnetic nanoparticle-based delivery system for BCNU in the treatment of gliomas. Biomaterials 2011, 32, 516–527. [Google Scholar] [CrossRef]
- Plassat, V.; Wilhelm, C.; Marsaud, V.; Ménager, C.; Gazeau, F.; Renoir, J.-M.; Lesieur, S. Anti-Estrogen-Loaded Superparamagnetic Liposomes for Intracellular Magnetic Targeting and Treatment of Breast Cancer Tumors. Adv. Funct. Mater. 2011, 21, 83–92. [Google Scholar] [CrossRef]
- Dalmina, M.; Pittella, F.; Sierra, J.A.; Souza, G.R.R.; Silva, A.H.; Pasa, A.A.; Creczynski-Pasa, T.B. Magnetically responsive hybrid nanoparticles for in vitro siRNA delivery to breast cancer cells. Mater. Sci. Eng. C 2019, 99, 1182–1190. [Google Scholar] [CrossRef] [PubMed]
- Rapoport, N.Y.; Kennedy, A.M.; Shea, J.E.; Scaife, C.L.; Nam, K.-H. Controlled and targeted tumor chemotherapy by ultrasound-activated nanoemulsions/microbubbles. J. Control. Release 2009, 138, 268–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dromi, S.; Frenkel, V.; Luk, A.; Traughber, B.; Angstadt, M.; Bur, M.; Poff, J.; Xie, J.; Libutti, S.K.; Li, K.C.P.; et al. Pulsed-high intensity focused ultrasound and low temperature-sensitive liposomes for enhanced targeted drug delivery and antitumor effect. Clin. Cancer Res. 2007, 13, 2722–2727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schroeder, A.; Kost, J.; Barenholz, Y. Ultrasound, liposomes and drug delivery: Principles for using ultrasound to control the release of drugs from liposomes. Chem. Phys. Lipids 2009, 162, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Geers, B.; Dewitte, H.; De Smedt, S.C.; Lentacker, I. Crucial factors and emerging concepts in ultrasound-triggered drug delivery. J. Control. Release 2012, 164, 248–255. [Google Scholar] [CrossRef] [Green Version]
- Rahdar, A.; Hasanein, P.; Bilal, M.; Beyzaei, H.; Kyzas, G.Z. Quercetin-loaded F127 nanomicelles: Antioxidant activity and protection against renal injury induced by gentamicin in rats. Life Sci. 2021, 276, 119420. [Google Scholar] [CrossRef]
- Rauf, A.; Tabish, T.A.; Ibrahim, I.M.; Rauf ul Hassan, M.; Tahseen, S.; Abdullah Sandhu, M.; Shahnaz, G.; Rahdar, A.; Cucchiarini, M.; Pandey, S. Design of Mannose-Coated Rifampicin nanoparticles modulating the immune response and Rifampicin induced hepatotoxicity with improved oral drug delivery. Arab. J. Chem. 2021, 14, 103321. [Google Scholar] [CrossRef]
- Morigi, V.; Tocchio, A.; Bellavite Pellegrini, C.; Sakamoto, J.H.; Arnone, M.; Tasciotti, E. Nanotechnology in medicine: From inception to market domination. J. Drug Deliv. 2011, 2012, 14. [Google Scholar] [CrossRef] [PubMed]
- Bosetti, R.; Vereeck, L. Future of nanomedicine: Obstacles and remedies. Nanomedicine 2011, 6, 747. [Google Scholar] [CrossRef]
- Osmani, R.A.M.; Hani, U.; Bhosale, R.R.; Kulkarni, P.K.; Shanmuganathan, S. Nanosponge carriers-an archetype swing in cancer therapy: A comprehensive review. Curr. Drug Targets 2017, 18, 108. [Google Scholar] [CrossRef]
- Vuorenkoski, L.; Toiviainen, H.; Hemminki, E. Decision-making in priority setting for medicines: A review of empirical studies. Health Policy 2008, 86, 1. [Google Scholar] [CrossRef] [PubMed]
- Bosetti, R.; Marneffe, W.; Vereeck, L. Assessing the need of quality-adjusted cost-effectiveness studies of nanotechnological cancer therapies. Nanomedicine 2013, 8, 487. [Google Scholar] [CrossRef]
- Bosetti, R. Medical nanotechnology: The obstacles hampering a future dominant market. Chem. Today 2014, 32, 50. [Google Scholar]
- Bosetti, R.; Ferrandina, F.; Marneffe, W.; Scambia, G.; Vereeck, L. Cost-effectiveness of gemcitabine versus PEGylated liposomal doxorubicin for advanced ovarian cancer: Comparing chemotherapy and nanotherapy. Nanomedicine 2014, 9, 2175. [Google Scholar] [CrossRef] [PubMed]
- Osmani, R.A.M.; Bhosale, R.R.; Hani, U.; Vaghela, R.; Kulkarni, P.K. Cyclodextrin based nanosponges: Impending carters in drug delivery and nanotherapeutics. Curr. Drug Ther. 2015, 10, 3. [Google Scholar] [CrossRef]
- Osmani, R.A.M.; Kulkarni, P.K.; Shanmuganathan, S.; Hani, U.; Srivastava, A.; Prerana, M.; Shinde, C.G.; Bhosale, R.R. A 32 full factorial design for development and characterization of a nanosponge-based intravaginal in situ gelling system for vulvovaginal candidiasis. RSC Adv. 2016, 6, 18737. [Google Scholar] [CrossRef]
- Puri, A. Phototriggerable Liposomes: Current Research and Future Perspectives. Pharmaceutics 2014, 6, 1–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sabir, F.; Zeeshan, M.; Laraib, U.; Barani, M.; Rahdar, A.; Cucchiarini, M.; Pandey, S. DNA Based and Stimuli-Responsive Smart Nanocarrier for Diagnosis and Treatment of Cancer: Applications and Challenges. Cancers 2021, 13, 3396. [Google Scholar] [CrossRef] [PubMed]
- Thangam, R.; Patel, K.D.; Kang, H.; Paulmurugan, R. Advances in Engineered Polymer Nanoparticle Tracking Platforms towards Cancer Immunotherapy—Current Status and Future Perspectives. Vaccines 2021, 9, 935. [Google Scholar] [CrossRef] [PubMed]
| Sr. No. | Product Name | Type | Drug | Uses/Treatment | Ref. |
|---|---|---|---|---|---|
| 1 | Vyxeos® | Liposome | Daunorubicin and Cytarabine | Acute myeloid leukaemia | [38] |
| 2 | Doxil® | PEGylated liposome | Doxorubicin | Ovarian and breast cancer | [39] |
| 3 | Lipo-Dox® | PEGylated liposome | Doxorubicin | Multiple myeloma, Ovarian and breast cancer | [40] |
| 4 | Onivyde® | PEGylated liposome | Irinotecan | Metastatic pancreatic cancer | [41] |
| 5 | Marqibo® | Liposome | Vincristine sulfate | Acute lymphoblastic leukemia | [41] |
| S. N. | Formulation | Type | Drug | Uses/Treatment |
|---|---|---|---|---|
| 1 | PAMAM # dendrimer | Dual-drug loaded dendrimer | Cisplatin and small interfering RNA # | Solid tumours |
| 2 | PAMAM-PEG # dendrimer | PEGylated dendrimer | Doxorubicin | Breast, bladder, ovarian, lung and thyroid cancer |
| 3 | Folic acid-PAMAM dendrimer | PPI #-dendrimer | Methotrexate | Epithelial cancer |
| 4 | PAMAM-PEG dendrimer | PEGylated dendrimer | 5-Flouro uracil | Pancreatic cancer |
| Sr. No. | Product Name | Type | Drug | Status | Uses/Treatment |
|---|---|---|---|---|---|
| 1 | NK105 | PEG-PAA # micelle | Paclitaxel | Phase 2 or 3 | Breast cancer, Gastric cancer |
| 2 | NK911 | PEG-PAA micelle | Doxorubicin | Phase 3 | Solid malignancies |
| 3 | NC-6004 | PEG-Polyglutamic acid | Cisplatin | Phase 3 | Pancreatic cancer |
| 4 | Genexol-PM | PEG-PLA # micelle | Paclitaxel | FDA # Approved | Breast cancer, ovarian and lung cancer |
| S. N. | Type | Drug | Functionalization | Cancer Cells |
|---|---|---|---|---|
| 1 | SWCNTs # | Doxorubicin & mitoxantrone | Polyethylene glycol, fluorescein, folic acid | HeLa cells |
| 2 | SWCNTs | 7-Ethyl-10-hydroxycamptothecin (SN38) | Polyethylene glycol, antibody C225, folic acid | Colorectal cancer cells |
| 3 | SWCNTs | Doxorubicin | Folic acid, Chitosan & its derivatives (palmitoyl chitosan & carboxymethyl chitosan) | Human cervical cancer HeLa cells |
| 4 | MWCNTs # | Doxorubicin | Polyethyleneimine, hyaluronic acid, fluorescein isothiocyanate | HeLa cells |
| 5 | MWCNT | Docetaxel, coumarin-6 | d-Alpha-tocopheryl, polyethylene glycol 1000 succinate (TPGS), transferrin | Human lung cancer cells |
| 6 | MWCNTs | Doxorubicin | folic acid, Polyethylene glycol | HeLa cells |
| Types of Nanoparticles | Drug | Outcomes |
|---|---|---|
| Folate-AuNP # | Cyclophosphamide | αHFR-positive # breast cancer cells were more sensitive to cyclophosphamide therapy. |
| MTX-AuNP # | Methotrexate | Compared to free MTX, the MTX-AuNP have depicted higher cytotoxicity and tumour cell accumulation, as well as improved tumour inhibition. |
| VCR-AuNP # | Vincristine (VCR) | Higher cytotoxicity and tumour cell accumulation compared to free VCR. |
| 6MP-AuNP # | 6-mercaptopurine | Compared to 6MP alone, the 6MP-AuNP have greater antiproliferative effect. |
| 5-FU-Glutathione-AuNP # | 5-Flourouracil | Compared to free 5-FU, the 5-FU-Glutathione-AuNP have greater anticancer effect. |
| Types of Nanoparticles | Drugs/Payloads | Applications/Outcomes |
|---|---|---|
| Magnetic MSNs #- Neutrophils carrying | Doxorubicin | Precise diagnosis and high anti-glioma efficacy |
| MSNs- Poly-L-histidine and PEG coated | Sorafenib | Improved cancer therapy by PH trigger drug release |
| MSNs-CuS #- Nanodots coated | Doxorubicin | Imaging and synergetic chemo-photothermal effect |
| MSNs-PEGylated lipid bilayer coating | Axitinib, celastrol | Improved cancer therapy |
| Organo MSNS- Polyethyleneimine coated | Doxorubicin P-gp SiRNA # | Preventing multi drug resistance and promotion of chemotherapy |
| S. N. | Product Name | Formulation | Status | Application |
|---|---|---|---|---|
| 1 | Gastromark® | Aqueous suspension of silicone coated SPIONs | FDA-approved | Magnetic resonance imaging |
| 2 | Feridex® | SPIONs coated with dextran | FDA-approved | Magnetic resonance imaging |
| 3 | Feraheme® | SPIONs coated with polyglucose sorbitol carboxymethylether | FDA-approved | Magnetic resonance imaging |
| 4 | NCT01270139 | Iron bearing nanoparticles | Clinical trial | Hyperthermia |
| 5 | NCT01436123 | Gold nanoparticles with iron oxide-silica shells | Clinical trial | Hyperthermia |
| S. N. | Delivery System | Purpose |
|---|---|---|
| 1 | Zinc oxide QDs | Liver cancer |
| 2 | GQD-mesoporous silica nanoparticle-DOX # | PH dependent release + Photothermal therapy |
| 3 | Silicon dioxide -GQD-DOX # | Cancer theragnostic |
| 4 | Nitrogen functionalized GQD-methotrexate | Breast cancer |
| 5 | GQD-Biotin-Doxorubicin | Targeting overexpressed biotin receptor for cancer therapy |
| 6 | Black phosphorous QDs-PEG # | Combination of PTT # and PDT # |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kenchegowda, M.; Rahamathulla, M.; Hani, U.; Begum, M.Y.; Guruswamy, S.; Osmani, R.A.M.; Gowrav, M.P.; Alshehri, S.; Ghoneim, M.M.; Alshlowi, A.; et al. Smart Nanocarriers as an Emerging Platform for Cancer Therapy: A Review. Molecules 2022, 27, 146. https://doi.org/10.3390/molecules27010146
Kenchegowda M, Rahamathulla M, Hani U, Begum MY, Guruswamy S, Osmani RAM, Gowrav MP, Alshehri S, Ghoneim MM, Alshlowi A, et al. Smart Nanocarriers as an Emerging Platform for Cancer Therapy: A Review. Molecules. 2022; 27(1):146. https://doi.org/10.3390/molecules27010146
Chicago/Turabian StyleKenchegowda, Madhuchandra, Mohamed Rahamathulla, Umme Hani, Mohammed Y. Begum, Sagar Guruswamy, Riyaz Ali M. Osmani, Mysore P. Gowrav, Sultan Alshehri, Mohammed M. Ghoneim, Areej Alshlowi, and et al. 2022. "Smart Nanocarriers as an Emerging Platform for Cancer Therapy: A Review" Molecules 27, no. 1: 146. https://doi.org/10.3390/molecules27010146