Dystrophin Protein Quantification as a Duchenne Muscular Dystrophy Diagnostic Biomarker in Dried Blood Spots Using Multiple Reaction Monitoring Tandem Mass Spectrometry: A Preliminary Study
Abstract
:1. Introduction
2. Results and Discussion
2.1. Signature Peptide Selection and LC–MS/MS Method Development
2.2. Validation of LC–MS/MS Method
2.2.1. Curve Linearity
2.2.2. Specificity and Sensitivity
2.2.3. Inter- and Intraday Validation
2.2.4. Peptide Stability Study
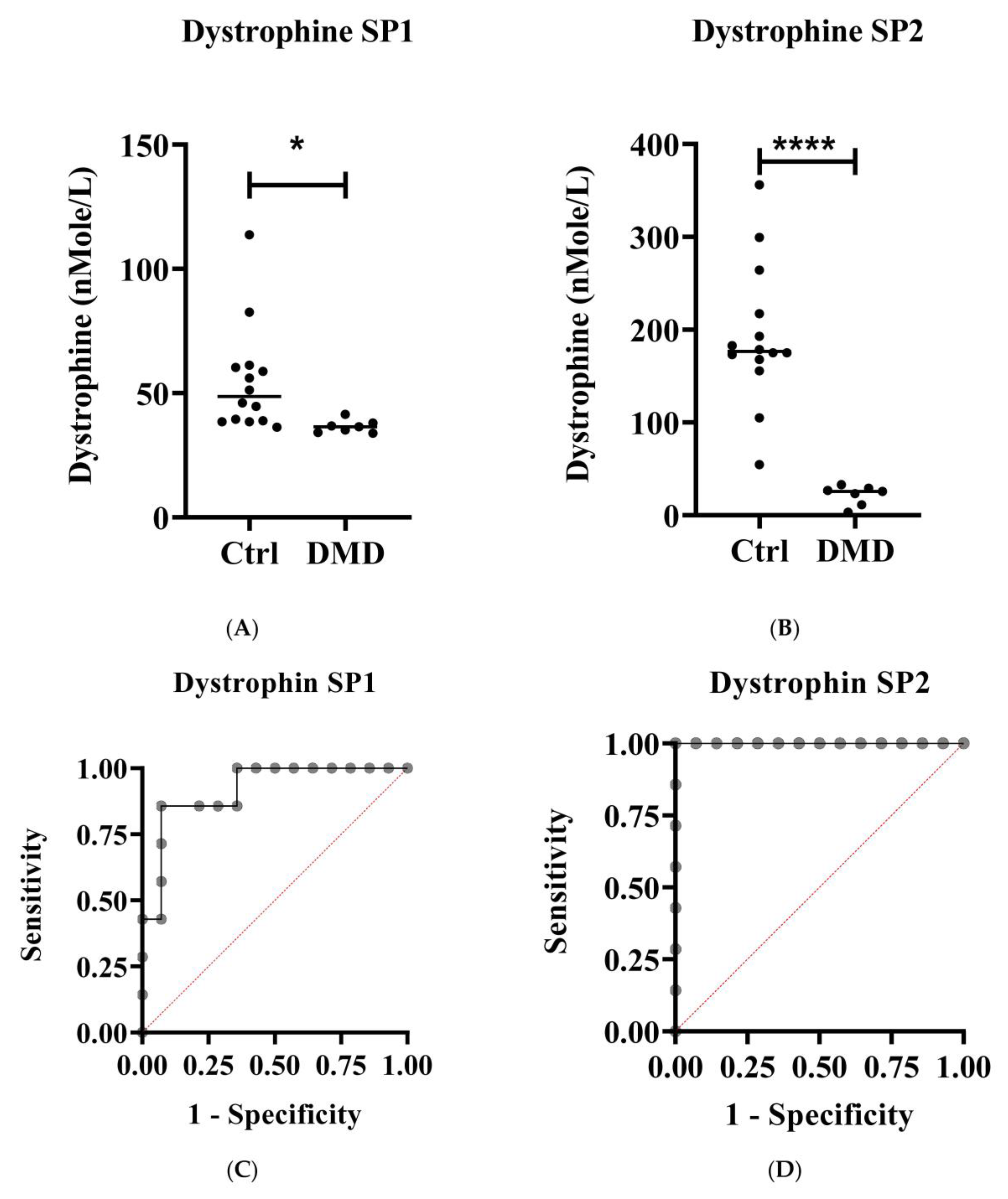
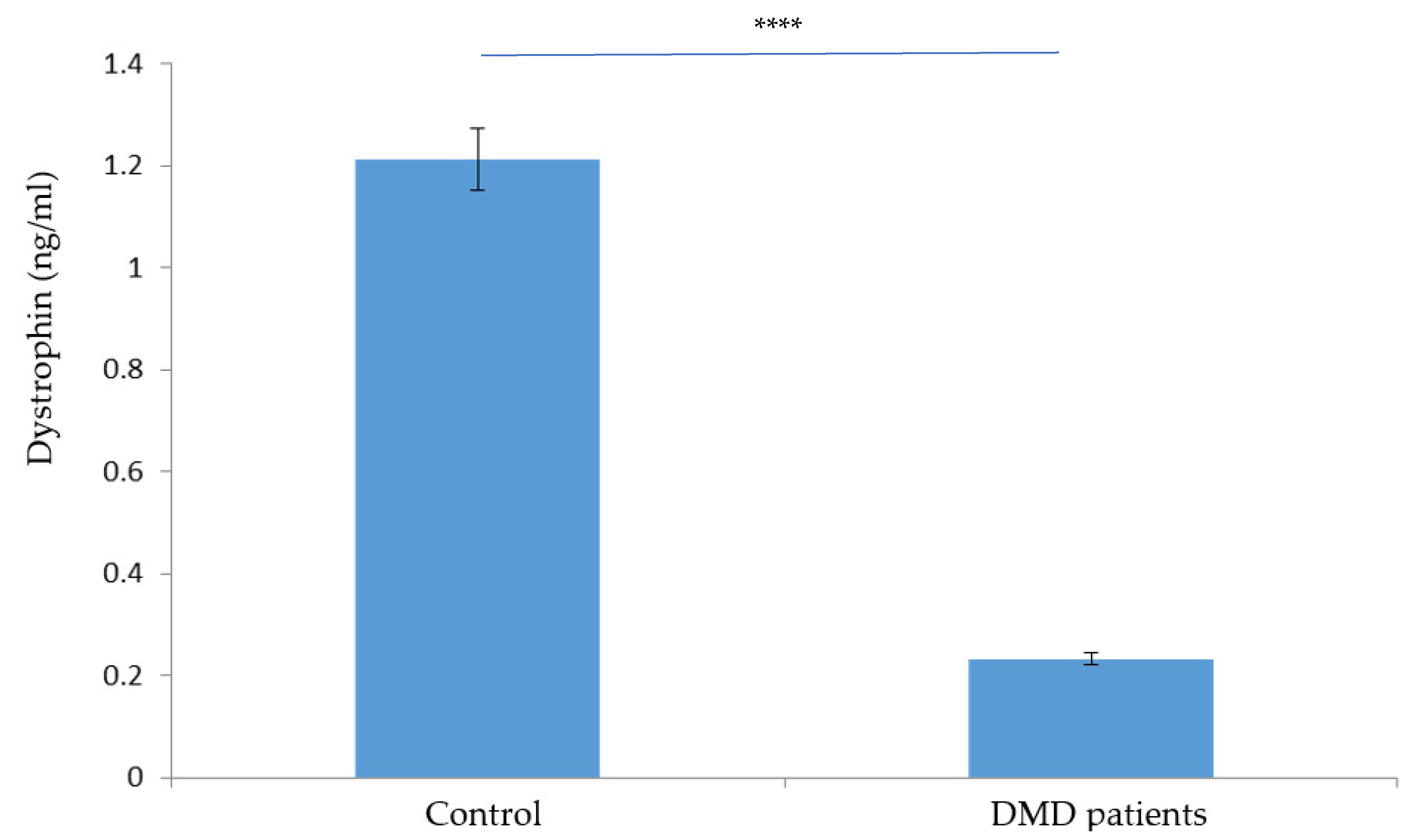
2.3. Dystrophin Protein Absolute Quantification in Clinical Samples
2.3.1. Diagnostic Evaluation
2.3.2. Reference Range Determination
3. Materials and Methods
3.1. Materials Used
3.2. Subjects and Blood Samples
3.3. Signature Peptide Selection
3.4. MRM Transition Development for Analytes
3.4.1. Stock and Working Solution Preparation
3.4.2. LC–MS/MS Analysis
3.5. DBS Sample Preparation
3.5.1. Protein Elution and Trypsin Digestion from DBS
3.5.2. Solid-Phase Extraction
3.6. LC–MS/MS Method Validation
3.6.1. Curve Linearity
3.6.2. Specificity and Sensitivity
3.6.3. Inter- and Intraday Validation
3.6.4. Peptide Stability Study
3.6.5. Carryover
3.7. Quantification of Dystrophin Protein by Sandwich Enzyme-Linked Immunosorbent Assay (ELISA)
3.8. Data and Statistical Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Fröhlich, T.; Kemter, E.; Flenkenthaler, F.; Klymiuk, N.; Otte, K.A.; Blutke, A.; Krause, S.; Walter, M.C.; Wanke, R.; Wolf, E.; et al. Progressive muscle proteome changes in a clinically relevant pig model of Duchenne muscular dystrophy. Sci. Rep. 2016, 6, 33362. [Google Scholar] [CrossRef]
- Mah, J.K.; Korngut, L.; Dykeman, J.; Day, L.; Pringsheim, T.; Jette, N. A systematic review and meta-analysis on the epidemiology of Duchenne and Becker muscular dystrophy. Neuromuscul. Disord. 2014, 24, 482–491. [Google Scholar] [CrossRef]
- Aartsma-Rus, A.; Van Deutekom, J.C.; Fokkema, I.F.; Van Ommen, G.J.B.; Den Dunnen, J.T. Entries in the Leiden Duchenne muscular dystrophy mutation database: An overview of mutation types and paradoxical cases that confirm the reading-frame rule. Muscle Nerve Off. J. Am. Assoc. Electrodiagn. Med. 2006, 34, 135–144. [Google Scholar] [CrossRef]
- Muntoni, F.; Torelli, S.; Ferlini, A. Dystrophin and mutations: One gene, several proteins, multiple phenotypes. Lancet Neurol. 2003, 2, 731–740. [Google Scholar] [CrossRef]
- Van Westering, T.L.; Betts, C.A.; Wood, M.J. Current understanding of molecular pathology and treatment of cardiomyopathy in duchenne muscular dystrophy. Molecules 2015, 20, 8823–8855. [Google Scholar] [CrossRef]
- Verhaart, I.E.C.; Aartsma-Rus, A. Therapeutic developments for Duchenne muscular dystrophy. Nat. Rev. Neurol. 2019, 15, 373–386. [Google Scholar] [CrossRef] [PubMed]
- Duan, D.; Goemans, N.; Takeda, S.i.; Mercuri, E.; Aartsma-Rus, A. Duchenne muscular dystrophy. Nat. Rev. Dis. Primers 2021, 7, 13. [Google Scholar] [CrossRef]
- Guiraud, S.; Aartsma-Rus, A.; Vieira, N.M.; Davies, K.E.; van Ommen, G.-J.B.; Kunkel, L.M. The pathogenesis and therapy of muscular dystrophies. Annu. Rev. Genom. Hum. Genet. 2015, 16, 281–308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bushby, K.; Finkel, R.; Birnkrant, D.J.; Case, L.E.; Clemens, P.R.; Cripe, L.; Kaul, A.; Kinnett, K.; McDonald, C.; Pandya, S. Diagnosis and management of Duchenne muscular dystrophy, part 1: Diagnosis, and pharmacological and psychosocial management. Lancet Neurol. 2010, 9, 77–93. [Google Scholar] [CrossRef]
- Sansović, I.; Barišić, I.; Dumić, K. Improved detection of deletions and duplications in the DMD gene using the multiplex ligation-dependent probe amplification (MLPA) method. Biochem Genet. 2013, 51, 189–201. [Google Scholar] [CrossRef]
- Hegde, M.R.; Chin, E.L.; Mulle, J.G.; Okou, D.T.; Warren, S.T.; Zwick, M.E. Microarray-based mutation detection in the dystrophin gene. Hum. Mutat 2008, 29, 1091–1099. [Google Scholar] [CrossRef] [Green Version]
- Ankala, A.; da Silva, C.; Gualandi, F.; Ferlini, A.; Bean, L.J.; Collins, C.; Tanner, A.K.; Hegde, M.R. A comprehensive genomic approach for neuromuscular diseases gives a high diagnostic yield. Ann. Neurol. 2015, 77, 206–214. [Google Scholar] [CrossRef]
- Okubo, M.; Minami, N.; Goto, K.; Goto, Y.; Noguchi, S.; Mitsuhashi, S.; Nishino, I. Genetic diagnosis of Duchenne/Becker muscular dystrophy using next-generation sequencing: Validation analysis of DMD mutations. J. Hum. Genet. 2016, 61, 483–489. [Google Scholar] [CrossRef]
- Birnkrant, D.J.; Bushby, K.; Bann, C.M.; Apkon, S.D.; Blackwell, A.; Brumbaugh, D.; Case, L.E.; Clemens, P.R.; Hadjiyannakis, S.; Pandya, S.; et al. Diagnosis and management of Duchenne muscular dystrophy, part 1: Diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management. Lancet Neurol. 2018, 17, 251–267. [Google Scholar] [CrossRef] [Green Version]
- Santos, R.; Gonçalves, A.; Oliveira, J.; Vieira, E.; Vieira, J.P.; Evangelista, T.; Moreno, T.; Santos, M.; Fineza, I.; Bronze-da-Rocha, E. New variants, challenges and pitfalls in DMD genotyping: Implications in diagnosis, prognosis and therapy. J. Hum. Genet. 2014, 59, 454–464. [Google Scholar] [CrossRef]
- Anthony, K.; Arechavala-Gomeza, V.; Taylor, L.E.; Vulin, A.; Kaminoh, Y.; Torelli, S.; Feng, L.; Janghra, N.; Bonne, G.; Beuvin, M. Dystrophin quantification: Biological and translational research implications. Neurology 2014, 83, 2062–2069. [Google Scholar] [CrossRef] [Green Version]
- Brown, K.J.; Marathi, R.; Fiorillo, A.A.; Ciccimaro, E.F.; Sharma, S.; Rowlands, D.S.; Rayavarapu, S.; Nagaraju, K.; Hoffman, E.P.; Hathout, Y. Accurate Quantitation of Dystrophin Protein in Human Skeletal Muscle Using Mass Spectrometry. J. Bioanal. Biomed. 2012, S7. [Google Scholar] [CrossRef] [Green Version]
- Carr, S.J.; Zahedi, R.P.; Lochmüller, H.; Roos, A. Mass spectrometry-based protein analysis to unravel the tissue pathophysiology in Duchenne muscular dystrophy. PROTEOMICS–Clin. Appl. 2018, 12, 1700071. [Google Scholar] [CrossRef]
- Szigyarto, C.A.-K.; Spitali, P. Biomarkers of Duchenne muscular dystrophy: Current findings. Degener. Neurol. Neuromuscul. Dis. 2018, 8, 1. [Google Scholar]
- Johansson, C. Exploring Genotype to Phenotype Correlations in Duchenne Muscular Dystrophy. Master’s Thesis, KTH Royal Institute of Technology, Stockholm, Sweden, 2017. [Google Scholar]
- Parad, R.B.; Sheldon, Y.; Bhattacharjee, A. Implementation of Hospital-Based Supplemental Duchenne Muscular Dystrophy Newborn Screening (sDMDNBS): A Pathway to Broadening Adoption. Int. J. Neonatal Screen. 2021, 7, 77. [Google Scholar] [CrossRef]
- Pan, S.; Aebersold, R.; Chen, R.; Rush, J.; Goodlett, D.R.; McIntosh, M.W.; Zhang, J.; Brentnall, T.A. Mass spectrometry based targeted protein quantification: Methods and applications. J. Proteome Res. 2009, 8, 787–797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, E.H.; Combe, P.C.; Schug, K.A. Multiple reaction monitoring for direct quantitation of intact proteins using a triple quadrupole mass spectrometer. J. Am. Soc. Mass Spectrom. 2016, 27, 886–896. [Google Scholar] [CrossRef]
- Kondrat, R.W.; McClusky, G.A.; Cooks, R.G. Multiple reaction monitoring in mass spectrometry/mass spectrometry for direct analysis of complex mixtures. Anal. Chem. 1978, 50, 2017–2021. [Google Scholar] [CrossRef]
- Kuzyk, M.A.; Parker, C.E.; Domanski, D.; Borchers, C.H. Development of MRM-based assays for the absolute quantitation of plasma proteins. In The Low Molecular Weight Proteome; Springer: Berlin/Heidelberg, Germany, 2013; pp. 53–82. [Google Scholar]
- Parker, C.E.; Borchers, C.H. Mass spectrometry based biomarker discovery, verification, and validation--quality assurance and control of protein biomarker assays. Mol. Oncol. 2014, 8, 840–858. [Google Scholar] [CrossRef]
- Picotti, P.; Bodenmiller, B.; Mueller, L.N.; Domon, B.; Aebersold, R. Full dynamic range proteome analysis of S. cerevisiae by targeted proteomics. Cell 2009, 138, 795–806. [Google Scholar] [CrossRef] [Green Version]
- Bauer, K.M.; Turko, I.V.; Phinney, K.W. Quantitative performance of internal standard platforms for absolute protein quantification using MRM-MS. Anal. Chem. 2015, 87, 4429–4435. [Google Scholar]
- Tuli, L.; Ressom, H.W. LC-MS Based Detection of Differential Protein Expression. J. Proteom. Bioinform 2009, 2, 416–438. [Google Scholar] [CrossRef] [Green Version]
- Rahman, A.M.A.; Lopata, A.L.; Randell, E.W.; Helleur, R.J. Absolute quantification method and validation of airborne snow crab allergen tropomyosin using tandem mass spectrometry. Anal. Chim. Acta 2010, 681, 49–55. [Google Scholar] [CrossRef]
- Ozcan, S.; Cooper, J.D.; Lago, S.G.; Kenny, D.; Rustogi, N.; Stocki, P.; Bahn, S. Towards reproducible MRM based biomarker discovery using dried blood spots. Sci. Rep. 2017, 7, 45178. [Google Scholar] [CrossRef] [PubMed]
- Hopfgartner, G.; Lesur, A.; Varesio, E. Analysis of biopharmaceutical proteins in biological matrices by LC-MS/MS II. LC-MS/MS analysis. TrAC Trends Anal. Chem. 2013, 48, 52–61. [Google Scholar] [CrossRef]
- Galal, M.A.; Jabar, M.A.; Zhra, M.; Rahman, A.M.A.; Aljada, A. Absolute quantification of senescence mediators in cells using multiple reaction monitoring liquid chromatography-Tandem mass spectrometry. Anal. Chim. Acta 2021, 1184, 339009. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. Bioanalytical Method Validation Guidance for Industry; US Department of Health and Human Services: Washington, DC, USA, 2018; pp. 1–41.
- ICH Harmonised Tripartite Guideline. Validation of Analytical Procedures: Text and Methodology Q2(R1). In Proceedings of the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use, Geneva, Switzerland, 2–4 March 2005; Volume 11.
- European Medicines Agency (EMEA), I. Topic Q 2 (R1), Validation of Analytical Procedures: Text and Methodology. In International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use; 2006; Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/ich-q-2-r1-validation-analytical-procedures-text-methodology-step-5_en.pdf (accessed on 17 May 2022).
- Solberg, H.E. A guide to IFCC recommendations on reference values. J. Int. Fed. Clin. Chem. 1993, 5, 162–165. [Google Scholar]
- Sasse, E.A. How to define and determine reference intervals in the clinical laboratory; Approved guideline. NCCLS Doc. C28-A2. 2000. Available online: https://docs.ufpr.br/~taconeli/CE06219/Artigo_FR3.pdf (accessed on 17 May 2022).
- Jones, G.; Barker, A. Reference intervals. Clin. Biochem Rev. 2008, 29 (Suppl. S1), S93–S97. [Google Scholar]
- Sumaily, K.M.; Nimer, R.; Alzahrani, M.; Abdel Jabar, M.; Alodib, A.; Sabi, E.M.; Nizami, I.; Abdel Rahman, A.M. CFTR protein quantification as a cystic fibrosis diagnostic biomarker in dried blood spots using multiple reaction monitoring tandem mass spectrometry. J. Pharm. Biomed. Anal. 2022, 216, 114801. [Google Scholar] [CrossRef]
- Al-Qahtani, W.S.; Abduljabbar, M.; AlSuhaibani, E.S.; Abdel Rahman, A.; Aljada, A. Quantification of the lamin A/C transcript variants in cancer cell lines by targeted absolute quantitative proteomics and correlation with mRNA expression. Int. J. Mol. Sci. 2019, 20, 1902. [Google Scholar] [CrossRef] [Green Version]
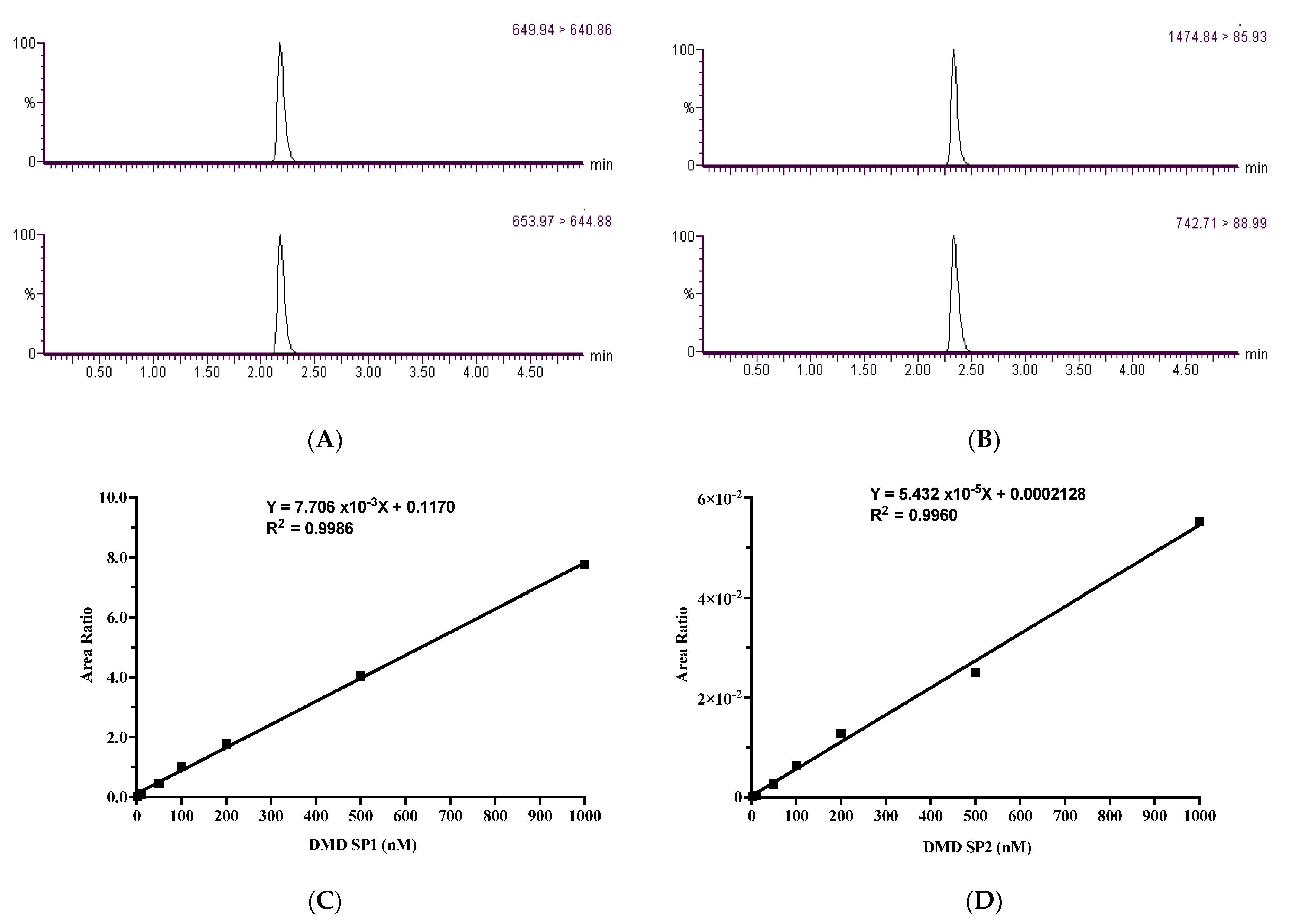
| DMD Signature Peptides | Quantification Property | Peptide Amino Acid Sequence | Molecular Weight (g/mol) | Purity (%) | Precursor Ion (m/z) | Product Ion (m/z) | Cone Voltage (V) | Collision Energy (v) | Retention Time (min) |
|---|---|---|---|---|---|---|---|---|---|
| Dystrophin SP1 | Quant | QVASSTGFCDQR | 1298.2 | 98.05 | 649.94 | 640.86 | 30 | 20 | 2.25 |
| Qual | 182.5 | 30 | 44 | ||||||
| Dystrophin SP1-labelled | Quant | QVASSTGFCDQR (V: d8-Val) | 1306.4 | 99.3 | 653.97 | 644.88 | 28 | 20 | 2.25 |
| Qual | 190.36 | 28 | 40 | ||||||
| Dystrophin SP2 | Quant | LGLLLHDSIQIPR | 1475.0 | 98.15 | 1474.84 | 85.93 | 100 | 80 | 2.42 |
| Qual | 109.95 | 100 | 78 | ||||||
| Dystrophin SP2-labelled | Quant | LGLLLHDSIQIPR (L: d3-Leu) | 1483.5 | 98.99 | 742.71 | 88.99 | 42 | 54 | 2.41 |
| Qual | 109.95 | 42 | 74 |
| Dystrophin Peptide | Linearity (n = 3) | LLOQ (nM) | ||
|---|---|---|---|---|
| Slope | Intercept | R2 | ||
| Dystrophin SP1 | 0.0202 | 0.19353 | 0.9991 | 2.0 |
| Dystrophin SP2 | 4.373 × 10−5 | 0.00083 | 0.9931 | 2.0 |
| QC Concentration (nM) | Summary | Inter-Day Validation (n = 18) | Intra-Day Validation (n = 6) | ||
|---|---|---|---|---|---|
| Dystrophin SP1 | Dystrophin SP2 | Dystrophin SP1 | Dystrophin SP2 | ||
| 25.0 | Mean | 26.41 | 25.78 | 25.86 | 25.49 |
| SD | 3.69 | 5.20 | 4.74 | 3.30 | |
| Accuracy % | 105.62 | 103.11 | 103.43 | 101.95 | |
| Imprecision CV% | 14.42 | 19.60 | 18.33 | 12.93 | |
| 150.0 | Mean | 159.79 | 143.96 | 155.76 | 146.32 |
| SD | 35.41 | 31.86 | 4.68 | 5.87 | |
| Accuracy % | 106.53 | 95.98 | 103.84 | 97.55 | |
| Imprecision CV% | 22.02 | 22.19 | 3.01 | 4.02 | |
| 750.0 | Mean | 833.47 | 751.79 | 732.71 | 753.25 |
| SD | 157.41 | 27.82 | 109.71 | 32.33 | |
| Accuracy % | 111.13 | 100.24 | 97.70 | 100.43 | |
| Imprecision CV% | 18.42 | 3.70 | 14.97 | 4.29 | |
| Dystrophin SP | QC (nM) | Stability (%) | ||||
|---|---|---|---|---|---|---|
| Fresh | RT | 4 °C | Freezer (−20 °C) | |||
| 24 h | 1 Week | 2 Weeks | 1 Month | |||
| Dystrophin SP1 | 25 | 100.00 | 141.2 | 141.2 | 94.7 | 102.9 |
| 150 | 100.00 | 104.9 | 104.9 | 95.6 | 98.8 | |
| 750 | 100.00 | 86.5 | 86.5 | 106.2 | 102.8 | |
| Dystrophin SP2 | 25 | 100.00 | 95.2 | 102.4 | 108.7 | 106.4 |
| 150 | 100.00 | 119.4 | 108.5 | 107.3 | 105.9 | |
| 750 | 100.00 | 102.0 | 96.7 | 98.0 | 103.9 | |
| Statistical Parameters | Dystrophin SP1 | Dystrophin SP2 | ||
|---|---|---|---|---|
| Ctrl | DMD | Ctrl | DMD | |
| Number of values (n) | 17 | 7 | 17 | 7 |
| Minimum (nM) | 36.24 | 2.280 | 37.90 | 2.280 |
| Maximum (nM) | 113.7 | 41.42 | 356.0 | 32.93 |
| Range | 77.46 | 39.14 | 318.1 | 30.65 |
| 95% CI of median | ||||
| Actual confidence level | 95.10% | 97.85% | 95.10% | 97.85% |
| Lower confidence limit | 38.87 | 3.140 | 105.1 | 3.140 |
| Upper confidence limit | 58.79 | 37.94 | 192.9 | 29.14 |
| Mean | 52.77 | 26.49 | 166.3 | 16.18 |
| Std. deviation | 19.76 | 16.31 | 89.69 | 12.50 |
| Std. error of mean | 4.793 | 5.158 | 21.75 | 3.954 |
| Lower 95% CI of mean | 42.60 | 14.82 | 120.2 | 7.234 |
| Upper 95% CI of mean | 62.93 | 38.15 | 212.5 | 25.12 |
| ID # | Gender | Age | DMD Mutation 1 | Muscle Biopsy |
|---|---|---|---|---|
| DMD 1 | M | 12 | exon 10 and 11 deletion c.650−?_1331?del | Yes |
| DMD 2 | F | 10 | c.10141C>T; p.Arg3381 * | No |
| DMD 3 | M | 8 | deletion of exon 49-50 (out of frame) c.7099−?_7309?del | No |
| DMD 4 | M | 10 | duplication of exon 18 to 44 c.650−?_6438+?dup | No |
| DMD 5 | M | 10 | c.2650C>T; p Gln884 * | Yes |
| DMD 6 | M | 5 | exon 48 through 53 c.6913−? _7872? del | Yes |
| DMD 7 | M | 8 | exon extension c.2862G>A; p.Trp954 * | No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nimer, R.M.; Sumaily, K.M.; Almuslat, A.; Abdel Jabar, M.; Sabi, E.M.; Al-Muhaizea, M.A.; Abdel Rahman, A.M. Dystrophin Protein Quantification as a Duchenne Muscular Dystrophy Diagnostic Biomarker in Dried Blood Spots Using Multiple Reaction Monitoring Tandem Mass Spectrometry: A Preliminary Study. Molecules 2022, 27, 3662. https://doi.org/10.3390/molecules27123662
Nimer RM, Sumaily KM, Almuslat A, Abdel Jabar M, Sabi EM, Al-Muhaizea MA, Abdel Rahman AM. Dystrophin Protein Quantification as a Duchenne Muscular Dystrophy Diagnostic Biomarker in Dried Blood Spots Using Multiple Reaction Monitoring Tandem Mass Spectrometry: A Preliminary Study. Molecules. 2022; 27(12):3662. https://doi.org/10.3390/molecules27123662
Chicago/Turabian StyleNimer, Refat M., Khalid M. Sumaily, Arwa Almuslat, Mai Abdel Jabar, Essa M. Sabi, Mohammad A. Al-Muhaizea, and Anas M. Abdel Rahman. 2022. "Dystrophin Protein Quantification as a Duchenne Muscular Dystrophy Diagnostic Biomarker in Dried Blood Spots Using Multiple Reaction Monitoring Tandem Mass Spectrometry: A Preliminary Study" Molecules 27, no. 12: 3662. https://doi.org/10.3390/molecules27123662






