Comparison of LC-MS3 and LC-MRM Methods for Quantifying Amantadine and Its Application in Therapeutic Amantadine Monitoring in Human Plasma
Abstract
:1. Introduction
2. Results and Discussion
2.1. Optimization of MS Conditions for Amantadine and Amantadine-d15
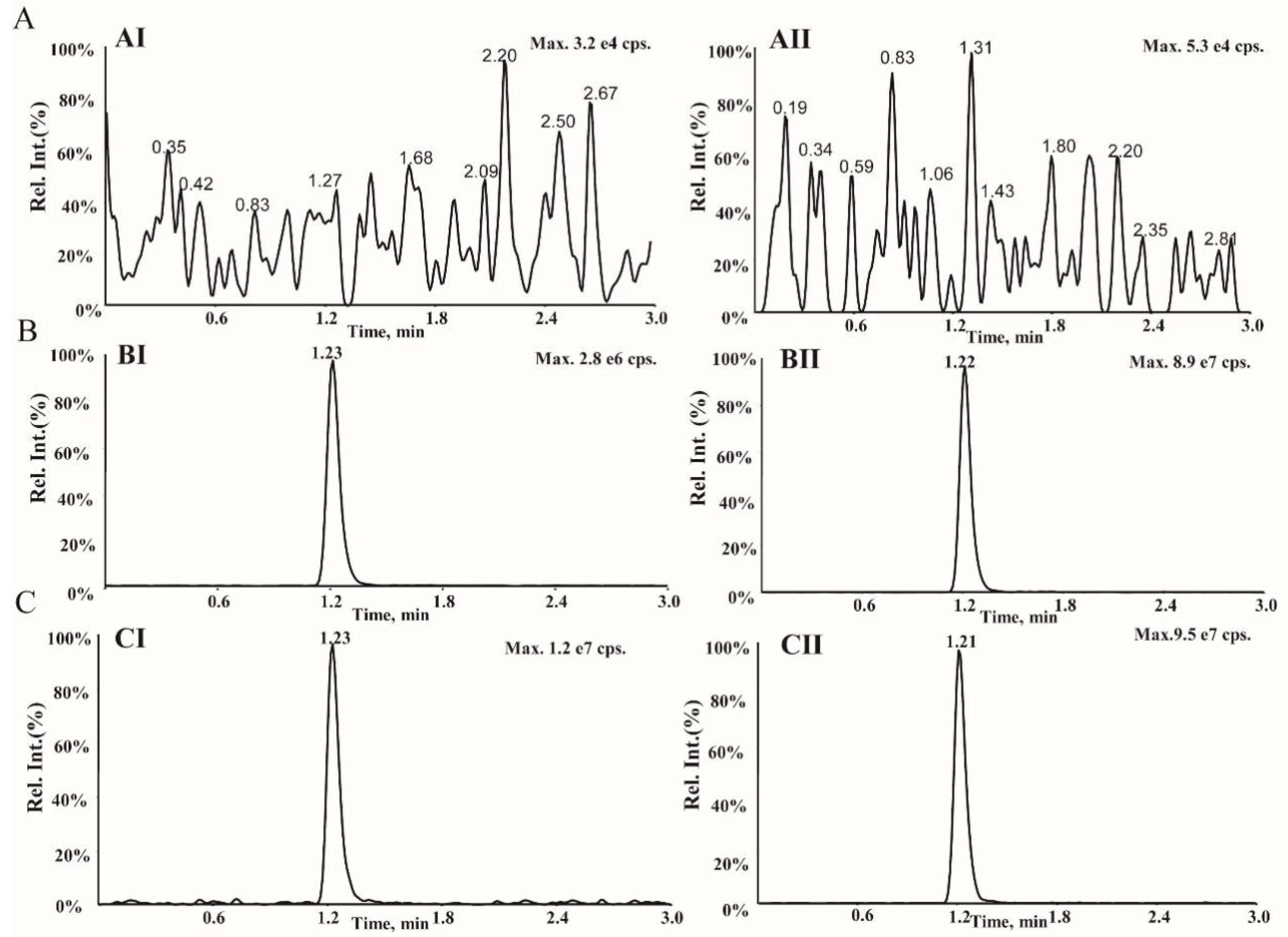
2.2. Optimization of LC Conditions
2.3. Optimization of Sample Processing
2.4. Assay Validation
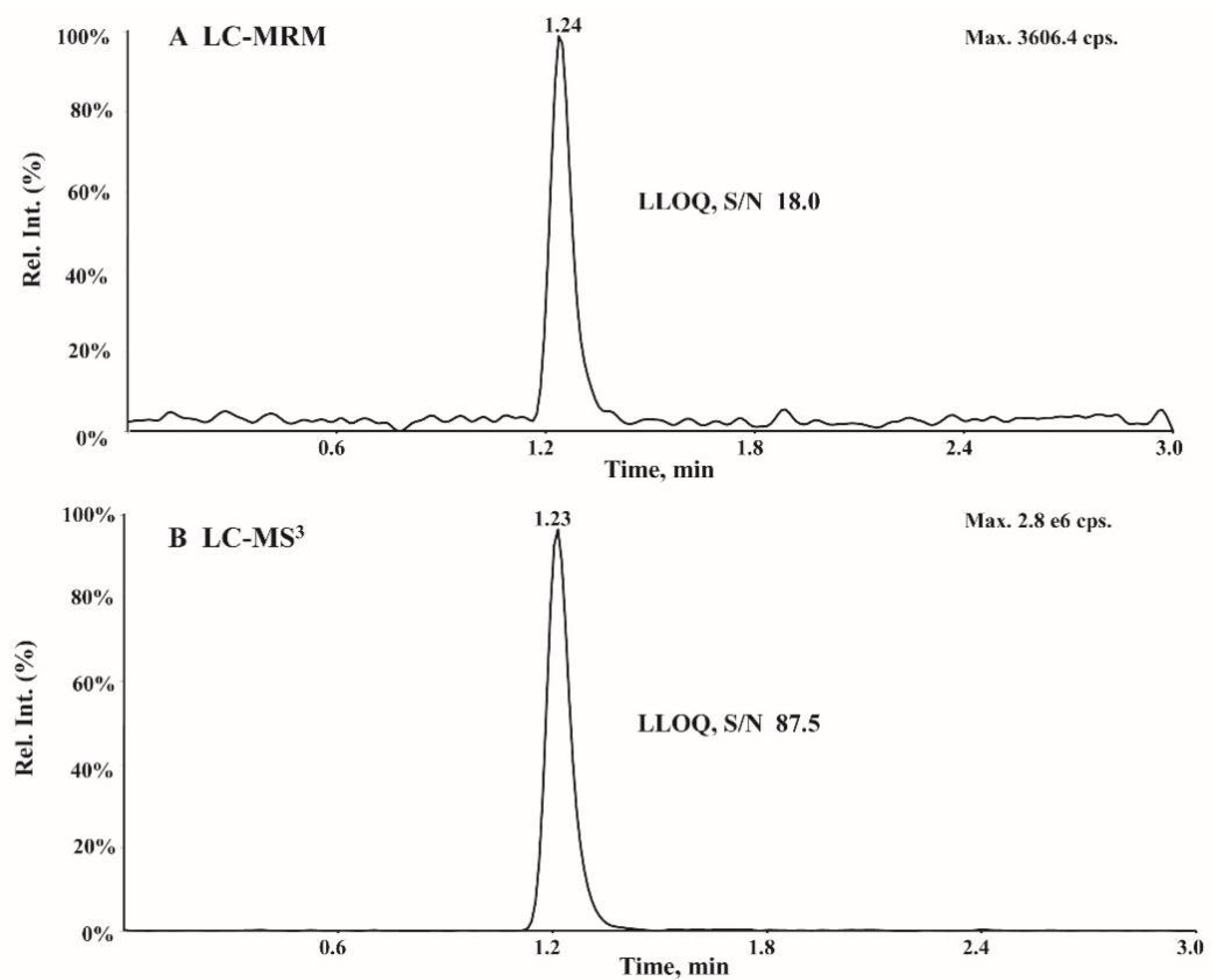
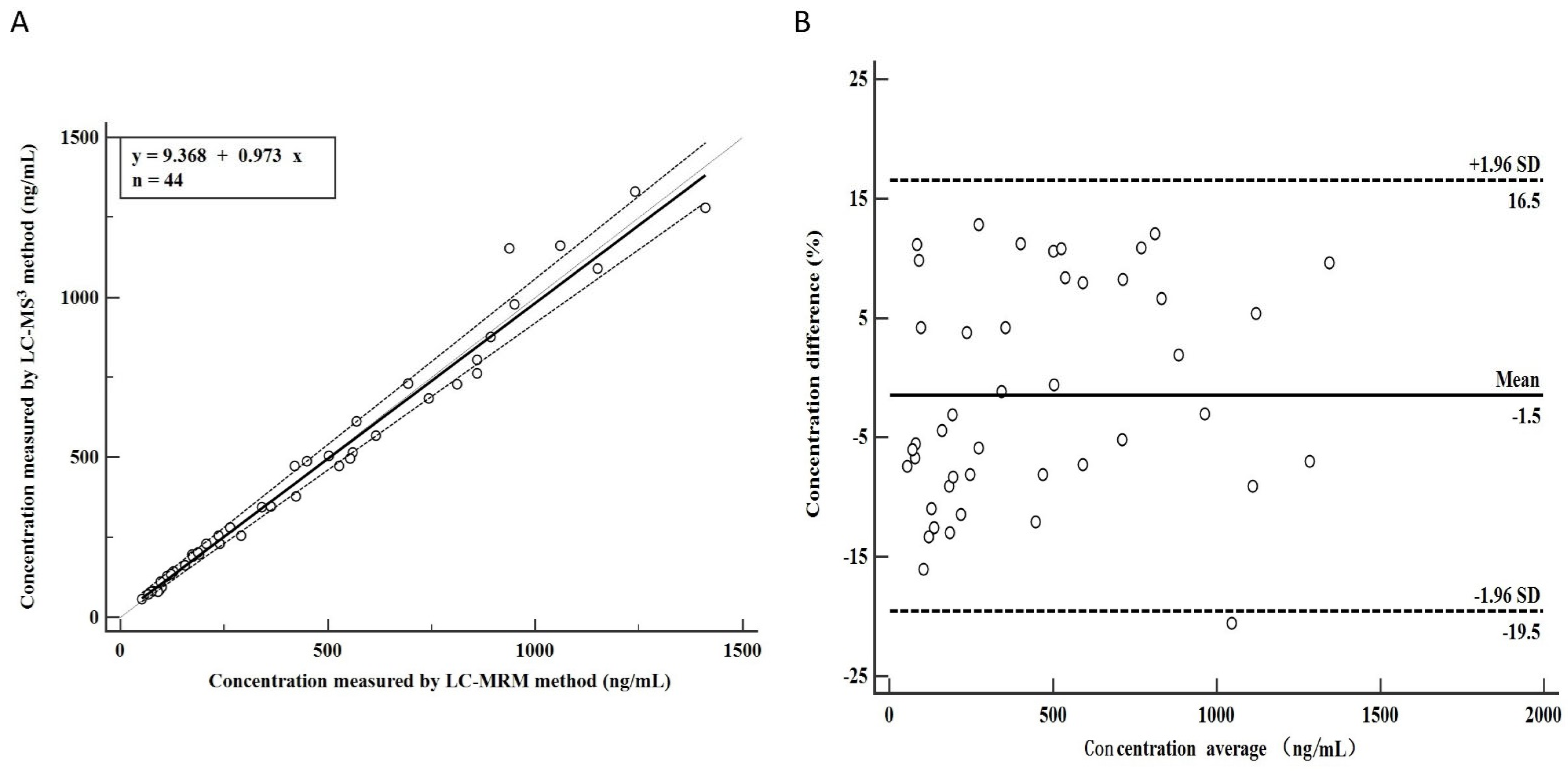
2.5. Comparison between LC-MS3 and LC-MRM
2.6. The Novelty and Significance of the LC-MS3 Method
2.7. Method Application
3. Materials and Methods
3.1. Chemical Reagents
3.2. Chromatographic and Mass Spectrometric Conditions
3.3. Preparation of Calibration Standards and Quality Control Samples
3.4. Plasma Sample Preparation
3.5. Method Validation
3.6. Clinical Application
3.7. Statistical Analysis
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- Stiver, G. The treatment of influenza with antiviral drugs. CMAJ 2003, 168, 49–56. [Google Scholar] [PubMed]
- Leonov, H.; Astrahan, P.; Krugliak, M.; Arkin, I.T. How do aminoadamantanes block the influenza M2 channel, and how does resistance develop? J. Am. Chem. Soc. 2011, 133, 9903–9911. [Google Scholar] [CrossRef] [PubMed]
- Brigham, E.F.; Johnston, T.H.; Brown, C.; Holt, J.D.S.; Fox, S.H.; Hill, M.P.; Howson, P.A.; Brotchie, J.M.; Nguyen, J.T. Pharmacokinetic/Pharmacodynamic Correlation Analysis of Amantadine for Levodopa-Induced Dyskinesia. J. Pharmacol. Exp. Ther. 2018, 367, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.C.; Wu, T.L.; Lin, F.J.; Tai, C.H.; Lin, C.H.; Wu, R.M. Amantadine treatment and delayed onset of levodopa-induced dyski-nesia in patients with early Parkinson’s disease. Eur. J. Neurol. 2022, 29, 1044–1055. [Google Scholar] [CrossRef] [PubMed]
- Romrell, J.; Fernandez, H.H.; Okun, M.S. Rationale for current therapies in Parkinson’s disease. Expert. Opin. Pharmacother. 2003, 4, 1747–1761. [Google Scholar] [CrossRef]
- Deep, P.; Dagher, A.; Sadikot, A.; Gjedde, A.; Cumming, P. Stimulation of dopa decarboxylase activity in striatum of healthy human brain secondary to NMDA receptor antagonism with a low dose of amantadine. Synapse 1999, 34, 313–318. [Google Scholar] [CrossRef]
- Bleidner, W.E.; Harmon, J.B.; Hewes, W.E.; Lynes, T.E.; Hermann, E.C. Absorption, distribution and excretion of amantadine hydrochloride. J. Pharmacol. Exp. Ther. 1965, 150, 484–490. [Google Scholar]
- Aoki, F.Y.; Sitar, D.S. Clinical pharmacokinetics of amantadine hydrochloride. Clin. Pharmacokinet. 1988, 14, 35–51. [Google Scholar] [CrossRef]
- Horadam, V.W.; Sharp, J.G.; Smilack, J.D.; McAnalley, B.H.; Garriott, J.C.; Stephens, M.K.; Prati, R.C.; Brater, D.C. Pharmacokinetics of amantadine hydrochloride in subjects with normal and impaired renal function. Ann. Intern. Med. 1981, 94, 454–458. [Google Scholar] [CrossRef]
- deVries, T.; Dentiste, A.; Di Lea, C.; Pichette, V.; Jacobs, D. Effects of Renal Impairment on the Pharmacokinetics of Once-Daily Amantadine Extended-Release Tablets. CNS Drugs 2019, 33, 783–789. [Google Scholar] [CrossRef] [Green Version]
- Yu, W.; Zhang, T.; Ma, M.; Chen, C.; Liang, X.; Wen, K.; Wang, Z.; Shen, J. Highly sensitive visual detection of amantadine residues in poultry at the ppb level: A colorimetric immunoassay based on a Fenton reaction and gold nanoparticles aggregation. Anal. Chim. Acta. 2018, 1027, 130–136. [Google Scholar] [CrossRef]
- Xie, S.; Wen, K.; Wang, S.; Wang, J.; Peng, T.; Mari, G.M.; Li, J.; Wang, Z.; Yu, X.; Jiang, H. Quantitative and rapid detection of amantadine and chloramphenicol based on various quantum dots with the same excitations. Anal. Bioanal. Chem. 2019, 411, 2131–2140. [Google Scholar] [CrossRef]
- Puente, B.; Hernandez, E.; Perez, S.; Pablo, L.; Prieto, E.; Garcia, M.A.; Bregante, M.A. Determination of memantine in plasma and vitreous humour by HPLC with precolumn derivatization and fluorescence detection. J. Chromatogr. Sci. 2011, 49, 745–752. [Google Scholar] [CrossRef] [Green Version]
- Higashi, Y.; Uemori, I.; Fujii, Y. Simultaneous determination of amantadine and rimantadine by HPLC in rat plasma with pre-column derivatization and fluorescence detection for pharmacokinetic studies. Biomed. Chromatogr. 2005, 19, 655–662. [Google Scholar] [CrossRef]
- Michail, K.; Daabees, H.; Beltagy, Y.; Elkhalek, M.A.; Khamis, M. High-performance liquid chromatographic determination of memantine in human urine following solid-phase extraction and precolumn derivatization. J. AOAC Int. 2013, 96, 1302–1307. [Google Scholar] [CrossRef]
- Bhadoriya, A.; Rathnam, S.; Dasandi, B.; Parmar, D.; Sanyal, M.; Shrivastav, P.S. Sensitive and rapid determination of amantadine without derivatization in human plasma by LC-MS/MS for a bioequivalence study. J. Pharm. Anal. 2018, 8, 202–207. [Google Scholar] [CrossRef]
- Maksymiuk, A.W.; Tappia, P.S.; Bux, R.A.; Moyer, D.; Huang, G.; Joubert, P.; Miller, D.W.; Ramjiawan, B.; Sitar, D.S. Use of amantadine in the evaluation of response to chemotherapy in lung cancer: A pilot study. Future. Sci. OA 2021, 7, FSO679. [Google Scholar] [CrossRef]
- Jiang, J.G.; Zhang, X.R.; Zhang, Y.H.; Song, G.S. Rapid identification 15 effective components of anti common cold medicine with MRM by LC-MS/MS. Acta Pharm. Sin. 2013, 48, 94–97. [Google Scholar]
- Liu, Z.; Yang, F.; Yu, K.; Lin, Y.; Liu, S.; Zhang, Q.; Su, Z. Multi-residue determination of five antiviral drugs in chicken tissues by liquid chromatography-electrospray ionization tandem mass spectrometry. Chin. J. Chromatogr. 2012, 30, 1253–1259. [Google Scholar] [CrossRef]
- Yun, H.; Cui, F.; Yan, H.; Liu, X.; He, Y.; Zhang, Z. Determination of ribavirin and amantadine in chicken by ultra performance liquid chromatography-tandem mass spectrometry. Chin. J. Chromatogr. 2013, 31, 724–728. [Google Scholar] [CrossRef]
- Dziadosz, M.; Klintschar, M.; Teske, J. Imatinib quantification in human serum with LC-MS3 as an effective way of protein kinase inhibitor analysis in biological matrices. Drug Metab. Pers. Ther. 2017, 32, 147–150. [Google Scholar] [CrossRef] [PubMed]
- Sanda, M.; Pompach, P.; Benicky, J.; Goldman, R. LC-MS3 quantification of O-glycopeptides in human serum. Electrophoresis 2013, 34, 2342–2349. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, H.; Imai, K. Recent Progress in FD-LC-MS/MS Proteomics Method. Front. Chem. 2021, 9, 640336. [Google Scholar] [CrossRef] [PubMed]
- Seger, C.; Salzmann, L. After another decade: LC-MS/MS became routine in clinical diagnostics. Clin. Biochem. 2020, 82, 2–11. [Google Scholar] [CrossRef]
- Okhina, A.A.; Rogachev, A.D.; Yarovaya, O.I.; Khvostov, M.V.; Tolstikova, T.G.; Pokrovsky, A.G.; Khazanov, V.A.; Salakhutdinov, N.F. Development and validation of an LC-MS/MS method for the quantitative analysis of the anti-influenza agent camphecene in rat plasma and its application to study the blood-to-plasma distribution of the agent. J. Pharm. Biomed. Anal. 2020, 180, 113039. [Google Scholar] [CrossRef]
- Arndt, T.; Guessregen, B.; Hohl, A.; Reis, J. Determination of serum amantadine by liquid chromatography-tandem mass spectrometry. Clin. Chim. Acta. 2005, 359, 125–131. [Google Scholar] [CrossRef]
- van Nuland, M.; Rosing, H.; Schellens, J.H.M.; Beijnen, J.H. Bioanalytical LC-MS/MS validation of therapeutic drug monitoring assays in oncology. Biomed. Chromatogr. 2020, 34, e4623. [Google Scholar] [CrossRef]
- Van Eeckhaut, A.; Lanckmans, K.; Sarre, S.; Smolders, I.; Michotte, Y. Validation of bioanalytical LC-MS/MS assays: Evaluation of matrix effects. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2009, 877, 2198–2207. [Google Scholar] [CrossRef]

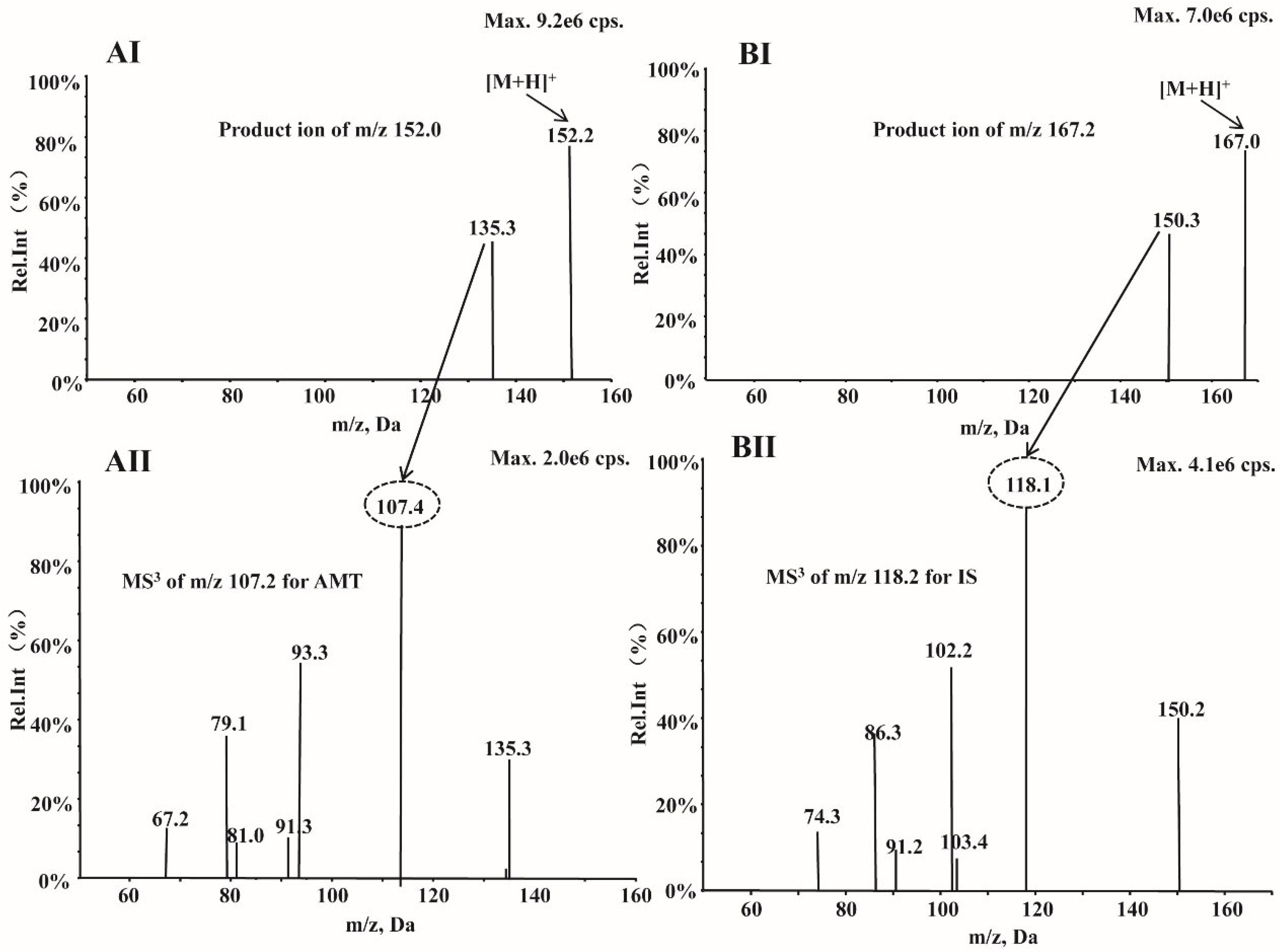
| Parameters | MS3 | |
|---|---|---|
| Amantadine | Amantadine-d15(IS) | |
| MS3 transitions | 152.2→135.3→107.4 | 167.0→150.3→118.1 |
| Declustering potential (V) | 43 | 43 |
| Entrance potential (V) | 10 | 10 |
| Collision energy (eV) | 25 | 25 |
| Excitation energy (AF2) (V) | 0.1 | 0.1 |
| Scan rate (Da/s) | 10,000 | 10,000 |
| LIT fill time (ms) | 80 | 80 |
| Excitation time (ms) | 25 | 25 |
| Turboheater temperature (°C) | 450 | 450 |
| Ionspray voltage (V) | 5500 | 5500 |
| Curtain gas (N2,psi) | 15 | 15 |
| Nebulizer gas (N2,psi) | 50 | 50 |
| Heater gas (N2,psi) | 50 | 50 |
| Compound | Spiked Concentration (ng/mL) | Intra-Day (n = 6) | Inter-Day (n = 18) | ||
|---|---|---|---|---|---|
| Accuracy (%) | Precision (CV, %) | Accuracy (%) | Precision (CV, %) | ||
| AMT | 50 | 90.4 ± 9.5 | 10.6 | 94.5 ± 10.1 | 10.7 |
| 150 | 93.9 ± 5.0 | 5.3 | 94.0 ± 7.8 | 8.3 | |
| 600 | 99.6 ± 4.0 | 4.1 | 102.4 ± 2.8 | 2.7 | |
| 1200 | 97.1 ± 4.2 | 4.3 | 98.5 ± 4.5 | 4.5 | |
| Compound | Spiked Concentration (ng/mL) | Recovery (%) | Matrix Effect (%) | ||
|---|---|---|---|---|---|
| Average | CV | Average | CV | ||
| AMT | 150 | 97.5 ± 10.5 | 10.7 | 100.8 ± 6.6 | 6.5 |
| 600 | 98.2 ± 7.6 | 7.7 | 99.0 ± 8.8 | 8.9 | |
| 1200 | 97.2 ± 3.6 | 3.7 | 102.9 ± 4.9 | 4.0 | |
| Compound | Spiked Concentration (ng/mL) | Bench-Top (3 h, RT) | Processed Auto-Sampler (24 h, RT) | Freeze-Thaw (−20 °C) | Long-Term (4 W, −80 °C) |
|---|---|---|---|---|---|
| AMT | 150 | 90.7 ± 6.7 | 104.3 ± 3.5 | 104.3 ± 5.8 | 106.1 ± 3.8 |
| 1200 | 93.6 ± 7.9 | 91.7 ± 4.3 | 97.5 ± 1.7 | 99.5 ± 4.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, Q.; Cao, H.; Liu, Y.; Li, Y.; Huang, J. Comparison of LC-MS3 and LC-MRM Methods for Quantifying Amantadine and Its Application in Therapeutic Amantadine Monitoring in Human Plasma. Molecules 2022, 27, 7619. https://doi.org/10.3390/molecules27217619
Sun Q, Cao H, Liu Y, Li Y, Huang J. Comparison of LC-MS3 and LC-MRM Methods for Quantifying Amantadine and Its Application in Therapeutic Amantadine Monitoring in Human Plasma. Molecules. 2022; 27(21):7619. https://doi.org/10.3390/molecules27217619
Chicago/Turabian StyleSun, Qiang, Haiwei Cao, Yong Liu, Yanyan Li, and Jing Huang. 2022. "Comparison of LC-MS3 and LC-MRM Methods for Quantifying Amantadine and Its Application in Therapeutic Amantadine Monitoring in Human Plasma" Molecules 27, no. 21: 7619. https://doi.org/10.3390/molecules27217619




