VH-4-A Bioactive Peptide from Soybean and Exercise Training Constrict Hypertension in Rats through Activating Cell Survival and AMPKα1, Sirt1, PGC1α, and FoX3α
Abstract
:1. Introduction
2. Results
2.1. Effect of Combination of VH-4 Peptide and Exercise on Heart Weight, Blood Pressure, Ejection Fraction (EF), and Fractional Shortening (FS) of SHR Rats
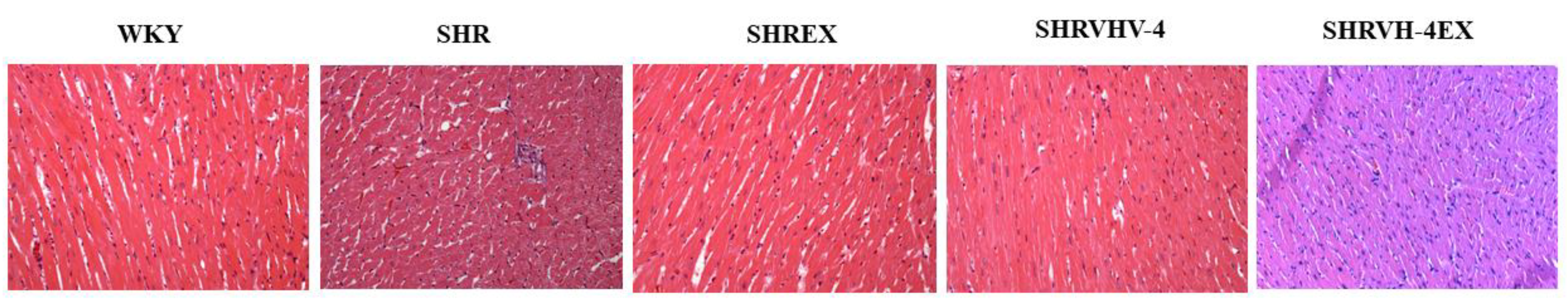
2.2. Effect of VH-4 and Exercise on Histology of Control and Treatment Groups
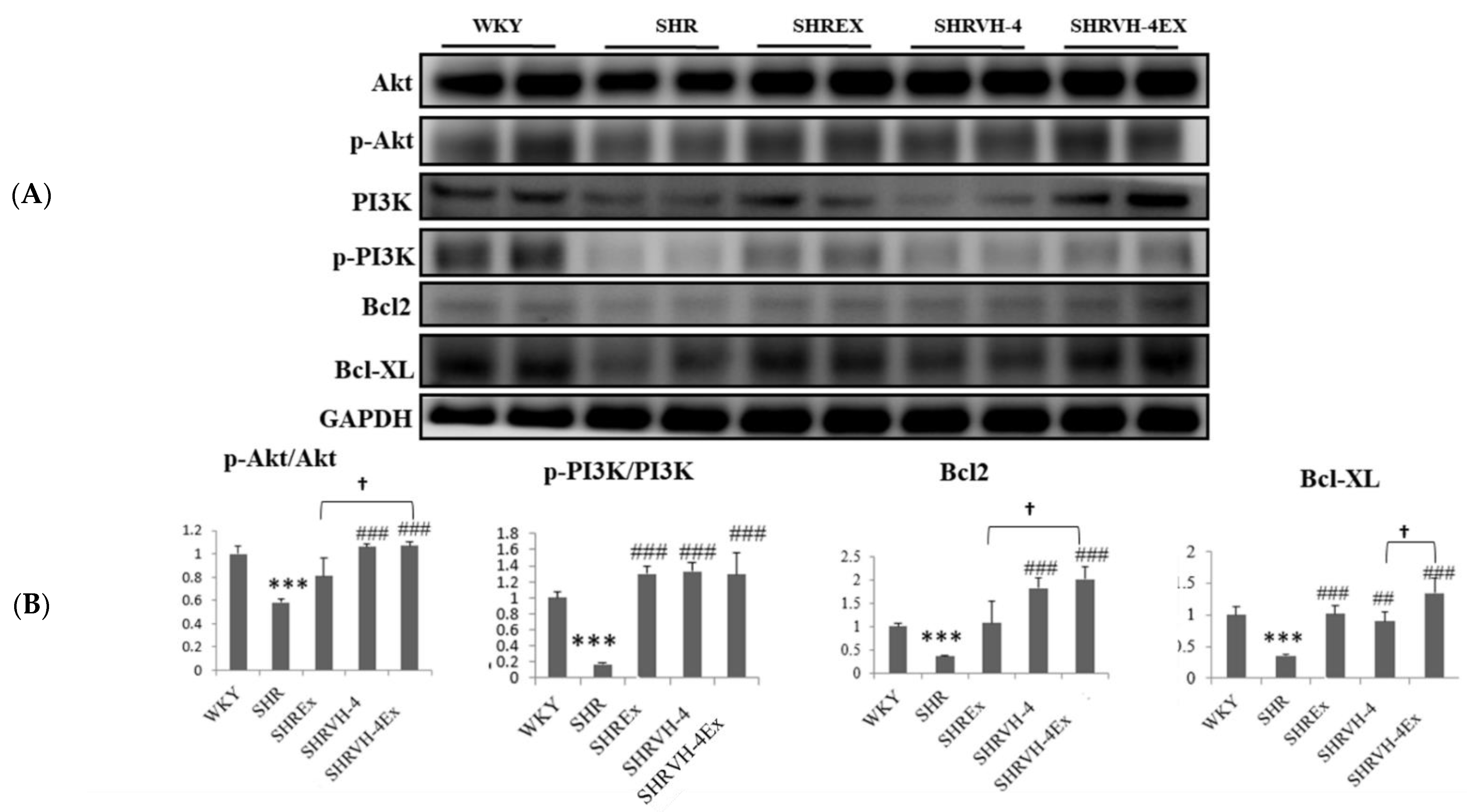
2.3. Effect of VH-4 and Exercise Training on the Cell Survival Pathway and Apoptosis in the Heart Tissue Section of SHR Animals
2.4. Effect of VH-4 and Exercise Training on AMPKα1, Sirt1, PGC1α, and FoX3α Signaling Pathway in SHR Animals
3. Discussion
4. Materials and Methods
4.1. Animal Grouping and Treatment
4.2. Blood Pressure Analysis
4.3. Tissue Staining
4.4. Western Blotting Analysis
4.5. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kearney, P.M.; Whelton, M.; Reynolds, K.; Muntner, P.; Whelton, P.K.; He, J. Global burden of hypertension: Analysis of worldwide data. Lancet 2005, 365, 217–223. [Google Scholar] [CrossRef]
- Gupta, R.; Xavier, D. Hypertension: The most important non communicable disease risk factor in India. Indian Heart J. 2018, 70, 565–572. [Google Scholar] [CrossRef]
- McEniry, M.; Samper-Ternent, R.; Flórez, C.E.; Cano-Gutierrez, C. Early life displacement due to armed conflict and violence, early nutrition, and older adult hypertension, diabetes, and obesity in the middle-income country of Colombia. J. Aging Health 2019, 31, 1479–1502. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.; Aronow, W.; Casey, D.; Collins, K.; Dennison Himmelfarb, C.; DePalma, S.; Gidding, S.; Jamerson, K.; Jones, D. Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, 1269–1324. [Google Scholar] [CrossRef] [PubMed]
- Janzen, N.R.; Whitfield, J.; Hoffman, N.J. Interactive roles for AMPK and glycogen from cellular energy sensing to exercise metabolism. Int. J. Mol. Sci. 2018, 19, 3344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scotto Rosato, A.; Montefusco, S.; Soldati, C.; Di Paola, S.; Capuozzo, A.; Monfregola, J.; Polishchuk, E.; Amabile, A.; Grimm, C.; Lombardo, A. TRPML1 links lysosomal calcium to autophagosome biogenesis through the activation of the CaMKKβ/VPS34 pathway. Nat. Commun. 2019, 10, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoshitomi, H.; Zhou, J.; Nishigaki, T.; Li, W.; Liu, T.; Wu, L.; Gao, M. Morinda citrifolia (Noni) fruit juice promotes vascular endothelium function in hypertension via glucagon-like peptide-1 receptor-CaMKKβ-AMPK-eNOS pathway. Phytother. Res. 2020, 34, 2341–2350. [Google Scholar] [CrossRef]
- Kosuru, R.; Kandula, V.; Rai, U.; Prakash, S.; Xia, Z.; Singh, S. Pterostilbene decreases cardiac oxidative stress and inflammation via activation of AMPK/Nrf2/HO-1 pathway in fructose-fed diabetic rats. Cardiovasc. Drugs Ther. 2018, 32, 147–163. [Google Scholar] [CrossRef]
- Cui, Y.-K.; Hong, Y.-X.; Wu, W.-Y.; Han, W.-M.; Wu, Y.; Wu, C.; Li, G.-R.; Wang, Y. Acacetin ameliorates cardiac hypertrophy by activating Sirt1/AMPK/PGC-1α pathway. Eur. J. Pharmacol. 2022, 920, 174858. [Google Scholar] [CrossRef]
- Cai, G.; Liu, J.; Wang, M.; Su, L.; Cai, M.; Huang, K.; Li, X.; Li, M.; Wang, L.; Huang, X. Mutual promotion of FGF21 and PPARγ attenuates hypoxia-induced pulmonary hypertension. Exp. Biol. Med. 2019, 244, 252–261. [Google Scholar] [CrossRef]
- Vallabha, S.V.; Tiku, P.K. Antihypertensive peptides derived from soy protein by fermentation. Int. J. Pept. Res. Ther. 2014, 20, 161–168. [Google Scholar] [CrossRef]
- Maubois, J.-L.; Lorient, D. Dairy proteins and soy proteins in infant foods nitrogen-to-protein conversion factors. Dairy Sci. Technol. 2016, 96, 15–25. [Google Scholar] [CrossRef] [Green Version]
- George, K.S.; Muñoz, J.; Akhavan, N.S.; Foley, E.M.; Siebert, S.C.; Tenenbaum, G.; Khalil, D.A.; Chai, S.C.; Arjmandi, B.H. Is soy protein effective in reducing cholesterol and improving bone health? Food Funct. 2020, 11, 544–551. [Google Scholar] [CrossRef] [PubMed]
- Birch, C.S.; Bonwick, G.A. Ensuring the future of functional foods. Int. J. Food Sci. Technol. 2019, 54, 1467–1485. [Google Scholar] [CrossRef]
- Wu, J.; Ding, X. Characterization of inhibition and stability of soy-protein-derived angiotensin I-converting enzyme inhibitory peptides. Food Res. Int. 2002, 35, 367–375. [Google Scholar] [CrossRef]
- Sun, X.; Acquah, C.; Aluko, R.E.; Udenigwe, C.C. Considering food matrix and gastrointestinal effects in enhancing bioactive peptide absorption and bioavailability. J. Funct. Foods 2020, 64, 103680. [Google Scholar] [CrossRef]
- Gardner, M.; Illingworth, K.M.; Kelleher, J.; Wood, D. Intestinal absorption of the intact peptide carnosine in man, and comparison with intestinal permeability to lactulose. J. Physiol. 1991, 439, 411–422. [Google Scholar] [CrossRef] [PubMed]
- Lopes, S.; Mesquita-Bastos, J.; Alves, A.J.; Ribeiro, F. Exercise as a tool for hypertension and resistant hypertension management: Current insights. Integr. Blood Press. Control 2018, 11, 65. [Google Scholar] [CrossRef] [Green Version]
- Rêgo, M.L.; Cabral, D.A.; Costa, E.C.; Fontes, E.B. Physical exercise for individuals with hypertension: It is time to emphasize its benefits on the brain and cognition. Clin. Med. Insights: Cardiol. 2019, 13, 1179546819839411. [Google Scholar] [CrossRef] [Green Version]
- Tian, D.; Meng, J. Exercise for prevention and relief of cardiovascular disease: Prognoses, mechanisms, and approaches. Oxidative Med. Cell. Longev. 2019, 2019, 1–11. [Google Scholar] [CrossRef]
- Kim, J.; Park, J.; Lim, K. Nutrition supplements to stimulate lipolysis: A review in relation to endurance exercise capacity. J. Nutr. Sci. Vitaminol. 2016, 62, 141–161. [Google Scholar] [CrossRef] [Green Version]
- Chiang, W.-D.; Shibu, M.A.; Lee, K.-I.; Wu, J.-P.; Tsai, F.-J.; Pan, L.-F.; Huang, C.-Y.; Lin, W.-T. Lipolysis-stimulating peptide-VHVV ameliorates high fat diet induced hepatocyte apoptosis and fibrosis. J. Funct. Foods 2014, 11, 482–492. [Google Scholar] [CrossRef]
- Ju, D.-T.; Kuo, W.-W.; Ho, T.-J.; Chang, R.-L.; Lin, W.-T.; Day, C.H.; Viswanadha, V.V.P.; Liao, P.-H.; Huang, C.-Y. Bioactive peptide VHVV upregulates the long-term memory-related biomarkers in adult spontaneously hypertensive rats. Int. J. Mol. Sci. 2019, 20, 3069. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsai, B.C.-K.; Kuo, W.-W.; Day, C.H.; Hsieh, D.J.-Y.; Kuo, C.-H.; Daddam, J.; Chen, R.-J.; Padma, V.V.; Wang, G.; Huang, C.-Y. The soybean bioactive peptide VHVV alleviates hypertension-induced renal damage in hypertensive rats via the SIRT1-PGC1α/Nrf2 pathway. J. Funct. Foods 2020, 75, 104255. [Google Scholar] [CrossRef]
- Lan, N.S.; Massam, B.D.; Kulkarni, S.S.; Lang, C.C. Pulmonary arterial hypertension: Pathophysiology and treatment. Diseases 2018, 6, 38. [Google Scholar] [CrossRef] [Green Version]
- Schmieder, R.E. End organ damage in hypertension. Dtsch. Ärzteblatt Int. 2010, 107, 866. [Google Scholar] [CrossRef]
- Cleven, L.; Krell-Roesch, J.; Nigg, C.R.; Woll, A. The association between physical activity with incident obesity, coronary heart disease, diabetes and hypertension in adults: A systematic review of longitudinal studies published after 2012. BMC Public Health 2020, 20, 1–15. [Google Scholar] [CrossRef]
- Ingelfinger, J.R. Angiotensin-converting enzyme 2: Implications for blood pressure and kidney disease. Curr. Opin. Nephrol. Hypertens. 2009, 18, 79–84. [Google Scholar] [CrossRef]
- Shu, Z.; Wan, J.; Read, R.J.; Carrell, R.W.; Zhou, A. Angiotensinogen and the modulation of blood pressure. Front. Cardiovasc. Med. 2021, 8, 645123. [Google Scholar] [CrossRef] [PubMed]
- Gangnus, T.; Burckhardt, B.B. Targeted LC-MS/MS platform for the comprehensive determination of peptides in the kallikrein-kinin system. Anal. Bioanal. Chem. 2021, 413, 2971–2984. [Google Scholar] [CrossRef]
- Attique, S.A.; Hassan, M.; Usman, M.; Atif, R.M.; Mahboob, S.; Al-Ghanim, K.A.; Bilal, M.; Nawaz, M.Z. A molecular docking approach to evaluate the pharmacological properties of natural and synthetic treatment candidates for use against hypertension. Int. J. Environ. Res. Public Health 2019, 16, 923. [Google Scholar] [CrossRef] [Green Version]
- Cicero, A.; Gerocarni, B.; Laghi, L.; Borghi, C. Blood pressure lowering effect of lactotripeptides assumed as functional foods: A meta-analysis of current available clinical trials. J. Hum. Hypertens. 2011, 25, 425–436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pan, D.; Guo, H.; Zhao, B.; Cao, J. The molecular mechanisms of interactions between bioactive peptides and angiotensin-converting enzyme. Bioorganic Med. Chem. Lett. 2011, 21, 3898–3904. [Google Scholar] [CrossRef] [PubMed]
- Morales-Camacho, J.I.; Espinosa-Hernández, E.; Rosas-Cárdenas, F.F.; Semería-Maitret, T.; Luna-Suárez, S. Insertions of antihypertensive peptides and their applications in pharmacy and functional foods. Appl. Microbiol. Biotechnol. 2019, 103, 2493–2505. [Google Scholar] [CrossRef]
- Yu, Z.; Wang, L.; Wu, S.; Zhao, W.; Ding, L.; Liu, J. In vivo antihypertensive effect of peptides from egg white and its molecular mechanism with ACE. Int. J. Food Sci. Technol. 2021, 56, 1030–1039. [Google Scholar] [CrossRef]
- Li, T.; Zhang, X.; Ren, Y.; Zeng, Y.; Huang, Q.; Wang, C. Antihypertensive effect of soybean bioactive peptides: A review. Curr. Opin. Pharmacol. 2022, 62, 74–81. [Google Scholar] [CrossRef]
- Wang, Z.; Cui, Y.; Liu, P.; Zhao, Y.; Wang, L.; Liu, Y.; Xie, J. Small peptides isolated from enzymatic hydrolyzate of fermented soybean meal promote endothelium-independent vasorelaxation and ACE inhibition. J. Agric. Food Chem. 2017, 65, 10844–10850. [Google Scholar] [CrossRef]
- Marthandam Asokan, S.; Wang, T.; Su, W.T.; Lin, W.T. Short Tetra-peptide from soy-protein hydrolysate attenuates hyperglycemia associated damages in H9c2 cells and ICR mice. J. Food Biochem. 2018, 42, e12638. [Google Scholar] [CrossRef]
- Lahera, V.; de Las Heras, N.; López-Farré, A.; Manucha, W.; Ferder, L. Role of mitochondrial dysfunction in hypertension and obesity. Curr. Hypertens. Rep. 2017, 19, 1–9. [Google Scholar] [CrossRef]
- Iglewski, M.; Hill, J.A.; Lavandero, S.; Rothermel, B.A. Mitochondrial fission and autophagy in the normal and diseased heart. Curr. Hypertens. Rep. 2010, 12, 418–425. [Google Scholar] [CrossRef]
- Quiles, J.M.; Gustafsson, Å.B. The role of mitochondrial fission in cardiovascular health and disease. Nat. Rev. Cardiol. 2022, 19, 723–736. [Google Scholar] [CrossRef]
- Schreckenberger, Z.J.; Wenceslau, C.F.; Joe, B.; McCarthy, C.G. Mitophagy in hypertension-associated premature vascular aging. Am. J. Hypertens. 2020, 33, 804–812. [Google Scholar] [CrossRef]
- Ko, S.-C.; Kang, M.C.; Kang, N.; Kim, H.-S.; Lee, S.-H.; Ahn, G.; Jung, W.-K.; Jeon, Y.-J. Effect of angiotensin I-converting enzyme (ACE) inhibition and nitric oxide (NO) production of 6, 6′-bieckol, a marine algal polyphenol and its antihypertensive effect in spontaneously hypertensive rats. Process Biochem. 2017, 58, 326–332. [Google Scholar] [CrossRef]
- Chen, C.; Kassan, A.; Castañeda, D.; Gabani, M.; Choi, S.-K.; Kassan, M. Metformin prevents vascular damage in hypertension through the AMPK/ER stress pathway. Hypertens. Res. 2019, 42, 960–969. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Wang, M.; Ma, J.; Pang, X.; Yuan, J.; Pan, Y.; Fu, Y.; Laher, I. MOTS-c and Exercise Restore Cardiac Function by Activating of NRG1-ErbB Signaling in Diabetic Rats. Front. Endocrinol. 2022, 13, 812032. [Google Scholar] [CrossRef] [PubMed]
- Potthoff, M.J.; Inagaki, T.; Satapati, S.; Ding, X.; He, T.; Goetz, R.; Mohammadi, M.; Finck, B.N.; Mangelsdorf, D.J.; Kliewer, S.A. FGF21 induces PGC-1α and regulates carbohydrate and fatty acid metabolism during the adaptive starvation response. Proc. Natl. Acad. Sci. USA 2009, 106, 10853–10858. [Google Scholar] [CrossRef] [Green Version]
- Ho, M.-Y.; Wang, C.-Y. Role of irisin in myocardial infarction, heart failure, and cardiac hypertrophy. Cells 2021, 10, 2103. [Google Scholar] [CrossRef]
- Chao, Y.-M.; Wu, K.L.; Tsai, P.-C.; Tain, Y.-L.; Leu, S.; Lee, W.-C.; Chan, J.Y. Anomalous AMPK-regulated angiotensin AT1R expression and SIRT1-mediated mitochondrial biogenesis at RVLM in hypertension programming of offspring to maternal high fructose exposure. J. Biomed. Sci. 2020, 27, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Boutcher, Y.N.; Boutcher, S.H. Exercise intensity and hypertension: What’s new? J. Hum. Hypertens. 2017, 31, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Parpa, K.M.; Michaelides, M.A.; Brown, B.S. Effect of High Intensity Interval Training on Heart Rate Variability in Individuals with Type 2 Diabetes. J. Exerc. Physiol. Online 2009, 12, 23–29. [Google Scholar]
- Wisløff, U.; Støylen, A.; Loennechen, J.P.; Bruvold, M.; Rognmo, Ø.; Haram, P.M.; Tjønna, A.E.; Helgerud, J.; Slørdahl, S.A.; Lee, S.J. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: A randomized study. Circulation 2007, 115, 3086–3094. [Google Scholar] [CrossRef]
- Marthandam Asokan, S.; Hung, T.-H.; Chiang, W.-D.; Lin, W.-T. Lipolysis-stimulating peptide from soybean protects against high fat diet-induced apoptosis in skeletal muscles. J. Med. Food 2018, 21, 225–232. [Google Scholar] [CrossRef]
- Priya, L.B.; Baskaran, R.; Huang, C.-Y.; Padma, V.V. Neferine ameliorates cardiomyoblast apoptosis induced by doxorubicin: Possible role in modulating NADPH oxidase/ROS-mediated NFκB redox signaling cascade. Sci. Rep. 2017, 7, 1–13. [Google Scholar]


| BP | WKY | SHR | SHREX | SHRVH-4 | SHRVH-4EX |
|---|---|---|---|---|---|
| HR | 328.8 ± 14.70 | 423.0 ± 5.16 # | 357.6 ± 14.69 *** | 380.67 ± 9.79 *** | 358.0 ± 7.55 *** |
| SBP | 147.3 ± 12.09 | 212.0 ± 7.48 # | 187.6 ± 8.50 | 189 ± 7.68 | 192.3 ± 22.50 |
| MBP | 116.6 ± 5.13 | 188.6 ± 9.46 # | 147.0 ± 2.00 * | 158 ± 6.22 * | 149.6 ± 14.43 * |
| DBP | 106.0 ± 5.29 | 175.3 ± 8.95 # | 126.6 ± 2.51 ** | 142 ± 7.99 ** | 116.0 ± 12.52 *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baskaran, R.; Balasubramanian, B.; Ho, J.-H.; Wang, M.-F.; Abomughaid, M.M.; Yang, H.-S.; Lin, W.-T. VH-4-A Bioactive Peptide from Soybean and Exercise Training Constrict Hypertension in Rats through Activating Cell Survival and AMPKα1, Sirt1, PGC1α, and FoX3α. Molecules 2022, 27, 7705. https://doi.org/10.3390/molecules27227705
Baskaran R, Balasubramanian B, Ho J-H, Wang M-F, Abomughaid MM, Yang H-S, Lin W-T. VH-4-A Bioactive Peptide from Soybean and Exercise Training Constrict Hypertension in Rats through Activating Cell Survival and AMPKα1, Sirt1, PGC1α, and FoX3α. Molecules. 2022; 27(22):7705. https://doi.org/10.3390/molecules27227705
Chicago/Turabian StyleBaskaran, Rathinasamy, Balamuralikrishnan Balasubramanian, Jou-Hsuan Ho, Ming-Fu Wang, Mosleh Mohammad Abomughaid, Hong-Siang Yang, and Wan-Teng Lin. 2022. "VH-4-A Bioactive Peptide from Soybean and Exercise Training Constrict Hypertension in Rats through Activating Cell Survival and AMPKα1, Sirt1, PGC1α, and FoX3α" Molecules 27, no. 22: 7705. https://doi.org/10.3390/molecules27227705
APA StyleBaskaran, R., Balasubramanian, B., Ho, J. -H., Wang, M. -F., Abomughaid, M. M., Yang, H. -S., & Lin, W. -T. (2022). VH-4-A Bioactive Peptide from Soybean and Exercise Training Constrict Hypertension in Rats through Activating Cell Survival and AMPKα1, Sirt1, PGC1α, and FoX3α. Molecules, 27(22), 7705. https://doi.org/10.3390/molecules27227705








