Rapid Detection of Recurrent Non-Muscle Invasive Bladder Cancer in Urine Using ATR-FTIR Technology
Abstract
1. Introduction
2. Results
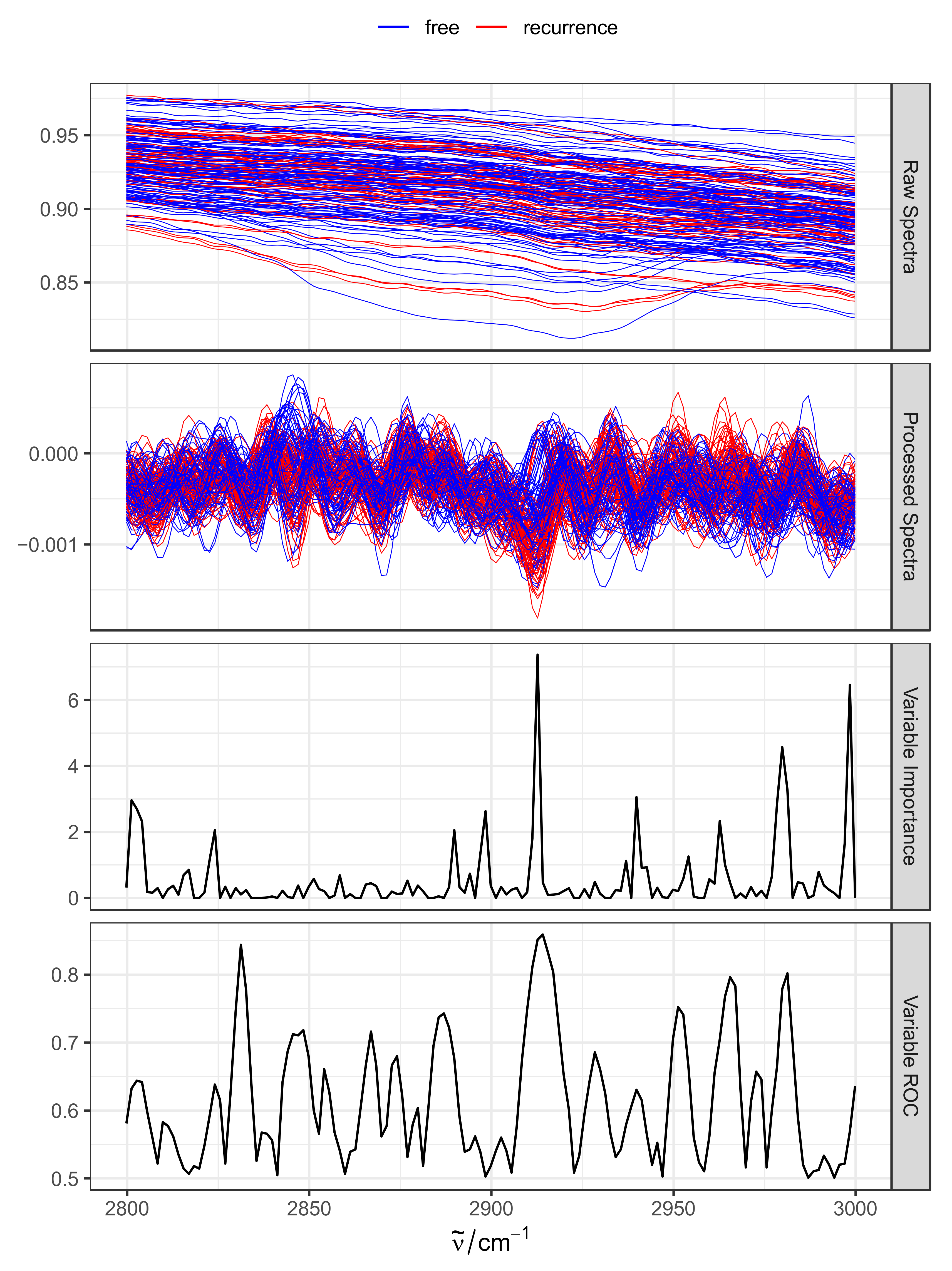
2.1. Overview FTIR Spectra Dataset
2.2. Assessment of Technical Variability and Batch Effects
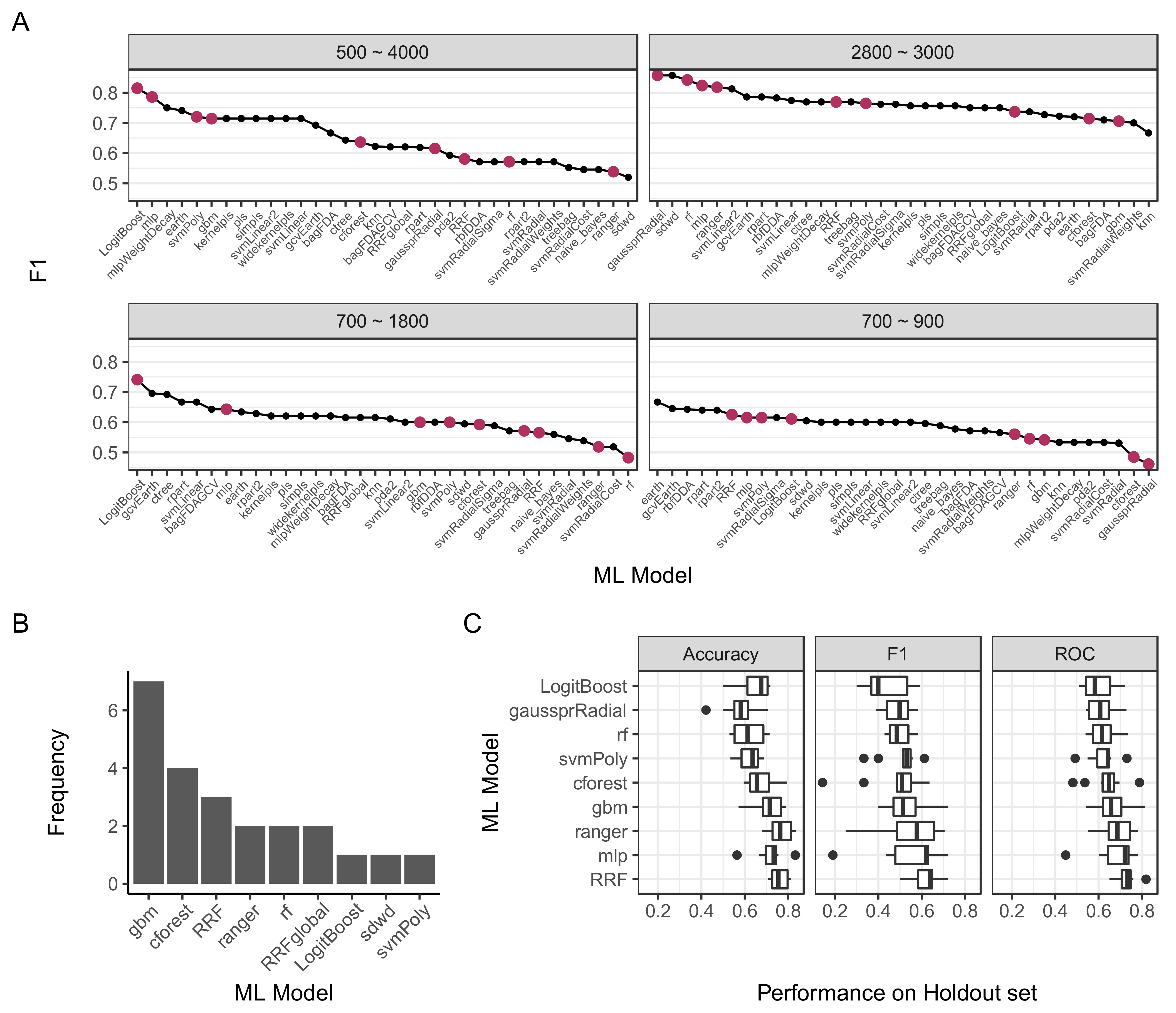
2.3. Preprocessing Parameters and Model Selection
2.4. Model Validation and Tuning
2.5. Extraction of Feature Importance
3. Discussion
4. Materials and Methods
4.1. Patients and Samples Collection
4.2. ATR-FTIR Measurement
4.3. Spectral Data Pre-Processing
4.4. Machine Learning
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- David, D.J. The application of atomic absorption to chemical analysis. A review. Analyst 1960, 85, 779–791. [Google Scholar] [CrossRef]
- Cassell, A.; Yunusa, B.; Jalloh, M.; Mbodji, M.M.; Diallo, A.; Ndoye, M.; Diallo, Y.; Labou, I.; Niang, L.; Gueye, S.M. Non-muscle invasive bladder cancer: A review of the current trend in Africa. World J. Oncol. 2019, 10, 123–131. [Google Scholar] [CrossRef]
- Oosterlinck, W.; Lobel, B.; Jakse, G.; Malmström, P.-U.; Stöckle, M.; Sternberg, C.; EAU Working Group on Oncological Urology. Guidelines on bladder cancer. Eur. Urol. 2002, 41, 105–112. [Google Scholar] [CrossRef]
- Babjuk, M.; Böhle, A.; Burger, M.; Capoun, O.; Cohen, D.; Compérat, E.M.; Hernández, V.; Kaasinen, E.; Palou, J.; Rouprêt, M.; et al. EAU Guidelines on Non-Muscle-invasive Urothelial Carcinoma of the Bladder: Update 2016. Eur. Urol. 2017, 71, 447–461. [Google Scholar] [CrossRef]
- Almallah, Y.; Rennie, C.; Stone, J.; Lancashire, M. Urinary tract infection and patient satisfaction after flexible cystoscopy and urodynamic evaluation. Urology 2000, 56, 37–39. [Google Scholar] [CrossRef]
- Van Der Aa, M.N.; Steyerberg, E.W.; Sen, E.F.; Zwarthoff, E.C.; Kirkels, W.J.; Van Der Kwast, T.H.; Essink-Bot, M.L. Patients’ perceived burden of cystoscopic and urinary surveillance of bladder cancer: A randomized comparison. BJU Int. 2008, 101, 1106–1110. [Google Scholar] [CrossRef]
- Lotan, Y.; Roehrborn, C.G. Cost-effectiveness of a modified care protocol substituting bladder tumor markers for cystoscopy for the followup of patients with transitional cell carcinoma of the bladder: A decision analytical approach. J. Urol. 2002, 167, 75–79. [Google Scholar] [CrossRef]
- Locatelli, F.; Canaud, B.; Eckardt, K.-U.; Stenvinkel, P.; Wanner, C.; Zoccali, C. The importance of diabetic nephropathy in current nephrological practice. Nephrol. Dial. Transplant. 2003, 18, 1716–1725. [Google Scholar] [CrossRef]
- Sun, W.; Li, F.; Wu, S.; Wang, X.; Zheng, D.; Wang, J.; Gao, Y. Human urine proteome analysis by three separation approaches. Proteomics 2005, 5, 4994–5001. [Google Scholar] [CrossRef]
- Shao, C.; Li, M.; Li, X.; Wei, L.; Zhu, L.; Yang, F.; Jia, L.; Mu, Y.; Wang, J.; Guo, Z. A tool for biomarker discovery in the urinary proteome: A manually curated human and animal urine protein biomarker database. Mol. Cell. Proteom. 2011, 10, 1–8. [Google Scholar] [CrossRef]
- Shaw, R.A.; Low-Ying, S.; Man, A.; Liu, K.-Z.; Mansfield, C.; Rileg, C.B.; Vijarnsorn, M. Infrared spectroscopy of biofluids in clinical chemistry and medical diagnostics. In Biomedical Vibrational Spectroscopy; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2008; pp. 79–103. [Google Scholar]
- Sala, A.; Anderson, D.J.; Brennan, P.M.; Butler, H.J.; Cameron, J.M.; Jenkinson, M.D.; Rinaldi, C.; Theakstone, A.G.; Baker, M.J. Biofluid diagnostics by FTIR spectroscopy: A platform technology for cancer detection. Cancer Lett. 2020, 477, 122–130. [Google Scholar] [CrossRef]
- Wijesinghe, H.G.; Hare, D.J.; Mohamed, A.; Shah, A.K.; Harris, P.N.; Hill, M.M. Detecting antimicrobial resistance in Escherichia coli using benchtop attenuated total reflectance-Fourier transform infrared spectroscopy and machine learning. Analyst 2021, 146, 6211–6219. [Google Scholar] [CrossRef]
- Korb, E.; Bağcıoğlu, M.; Garner-Spitzer, E.; Wiedermann, U.; Ehling-Schulz, M.; Schabussova, I. Machine learning-empowered FTIR spectroscopy serum analysis stratifies healthy, allergic, and SIT-treated mice and humans. Biomolecules 2020, 10, 1058. [Google Scholar] [CrossRef]
- Sitnikova, V.E.; Kotkova, M.A.; Nosenko, T.N.; Kotkova, T.N.; Martynova, D.M.; Uspenskaya, M.V. Breast cancer detection by ATR-FTIR spectroscopy of blood serum and multivariate data-analysis. Talanta 2020, 214, 120857. [Google Scholar] [CrossRef]
- Yang, X.; Ou, Q.; Yang, W.; Shi, Y.; Liu, G. Diagnosis of liver cancer by FTIR spectra of serum. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2021, 263, 120181. [Google Scholar] [CrossRef]
- Gray, E.; Cameron, J.M.; Butler, H.J.; Jenkinson, M.D.; Hegarty, M.G.; Palmer, D.S.; Brennan, P.M.; Baker, M.J. Early economic evaluation to guide the development of a spectroscopic liquid biopsy for the detection of brain cancer. Int. J. Technol. Assess. Health Care 2021, 37, 1–6. [Google Scholar] [CrossRef]
- Theakstone, A.G.; Brennan, P.M.; Jenkinson, M.D.; Mills, S.J.; Syed, K.; Rinaldi, C.; Xu, Y.; Goodacre, R.; Butler, H.J.; Palmer, D.S. Rapid spectroscopic liquid biopsy for the universal detection of brain tumours. Cancers 2021, 13, 3851. [Google Scholar] [CrossRef]
- Mordechai, S.; Shufan, E.; Katz, B.P.; Salman, A. Early diagnosis of Alzheimer’s disease using infrared spectroscopy of isolated blood samples followed by multivariate analyses. Analyst 2017, 142, 1276–1284. [Google Scholar] [CrossRef]
- Yap, X.-L.; Wood, B.; Ong, T.-A.; Lim, J.; Goh, B.-H.; Lee, W.-L. Detection of prostate cancer via IR spectroscopic analysis of urinary extracellular vesicles: A pilot study. Membranes 2021, 11, 591. [Google Scholar] [CrossRef]
- Gok, S.; Aydin, O.Z.; Sural, Y.S.; Zorlu, F.; Bayol, U.; Severcan, F. Bladder cancer diagnosis from bladder wash by Fourier transform infrared spectroscopy as a novel test for tumor recurrence. J. Biophotonics 2016, 9, 967–975. [Google Scholar] [CrossRef]
- Barauna, V.G.; Singh, M.N.; Barbosa, L.L.; Marcarini, W.D.; Vassallo, P.F.; Mill, J.G.; Ribeiro-Rodrigues, R.; Campos, L.C.; Warnke, P.H.; Martin, F.L. Ultrarapid on-site detection of SARS-CoV-2 infection using simple ATR-FTIR spectroscopy and an analysis algorithm: High sensitivity and specificity. Anal. Chem. 2021, 93, 2950–2958. [Google Scholar] [CrossRef]
- Paraskevaidi, M.; Martin-Hirsch, P.L.; Martin, F.L. ATR-FTIR spectroscopy tools for medical diagnosis and disease investigation. In Nanotechnology Characterization Tools for Biosensing and Medical Diagnosis; Springer: Berlin/Heidelberg, Germany, 2018; pp. 163–211. [Google Scholar]
- Finlayson, D.; Rinaldi, C.; Baker, M.J. Is infrared spectroscopy ready for the clinic? Anal. Chem. 2019, 91, 12117–12128. [Google Scholar] [CrossRef]
- Grant-Peters, M.; Rich-Griffin, C.; Grant-Peters, J.E.; Cinque, G.; Dendrou, C.A. Photizo: An open-source library for cross-sample analysis of FTIR spectroscopy data. Bioinformatics 2022, 38, 3490–3492. [Google Scholar] [CrossRef]
- Savitzky, A.; Golay, M.J. Smoothing and differentiation of data by simplified least squares procedures. Anal. Chem. 1964, 36, 1627–1639. [Google Scholar] [CrossRef]
- Chawla, N.V.; Bowyer, K.W.; Hall, L.O.; Kegelmeyer, W.P. SMOTE: Synthetic minority over-sampling technique. J. Artif. Intell. Res. 2002, 16, 321–357. [Google Scholar] [CrossRef]
- Liaw, A.; Wiener, M. Classification and regression by randomForest. R News 2002, 2, 18–22. [Google Scholar]
- Archer, K.J.; Kimes, R.V. Empirical characterization of random forest variable importance measures. Comput. Stat. Data Anal. 2008, 52, 2249–2260. [Google Scholar] [CrossRef]
- Soria, F.; Krabbe, L.M.; Todenhöfer, T.; Dobruch, J.; Mitra, A.P.; Inman, B.A.; Gust, K.M.; Lotan, Y.; Shariat, S.F. Molecular markers in bladder cancer. World J. Urol. 2019, 37, 31–40. [Google Scholar] [CrossRef]
- Yossepowitch, O.; Herr, H.W.; Donat, S.M. Use of urinary biomarkers for bladder cancer surveillance: Patient perspectives. J. Urol. 2007, 177, 1277–1282. [Google Scholar] [CrossRef]
- Kavalieris, L.; O’Sullivan, P.; Frampton, C.; Guilford, P.; Darling, D.; Jacobson, E.; Suttie, J.; Raman, J.D.; Shariat, S.F.; Lotan, Y. Performance Characteristics of a Multigene Urine Biomarker Test for Monitoring for Recurrent Urothelial Carcinoma in a Multicenter Study. J. Urol. 2017, 197, 1419–1426. [Google Scholar] [CrossRef]
- Pan, C.C. The value of molecular markers in classification and prediction of progression in non-muscle-invasive bladder cancer. Transl. Androl. Urol. 2018, 7, 736–739. [Google Scholar] [CrossRef]
- Dyrskjøt, L.; Zieger, K.; Kruhøffer, M.; Thykjaer, T.; Jensen, J.L.; Primdahl, H.; Aziz, N.; Marcussen, N.; Møller, K.; Orntoft, T.F. A molecular signature in superficial bladder carcinoma predicts clinical outcome. Clin. Cancer Res. 2005, 11, 4029–4036. [Google Scholar] [CrossRef]
- Menendez, J.A.; Lupu, R. Fatty acid synthase and the lipogenic phenotype in cancer pathogenesis. Nat. Rev. Cancer 2007, 7, 763–777. [Google Scholar] [CrossRef]
- Molendijk, J.; Robinson, H.; Djuric, Z.; Hill, M.M. Lipid mechanisms in hallmarks of cancer. Mol. Omics 2020, 16, 6–18. [Google Scholar] [CrossRef]
- Sahu, D.; Lotan, Y.; Wittmann, B.; Neri, B.; Hansel, D.E. Metabolomics analysis reveals distinct profiles of nonmuscle-invasive and muscle-invasive bladder cancer. Cancer Med. 2017, 6, 2106–2120. [Google Scholar] [CrossRef]
- Chen, S.; Zhu, S.; Cui, X.; Xu, W.; Kong, C.; Zhang, Z.; Qian, W. Identifying non-muscle-invasive and muscle-invasive bladder cancer based on blood serum surface-enhanced Raman spectroscopy. Biomed. Opt. Express 2019, 10, 3533–3544. [Google Scholar] [CrossRef]
- Beleites, C. Package ‘hyperSpec version 0.100.0.’; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Ligges, U.; Short, T.; Kienzle, P.; Schnackenberg, S.; Billinghurst, D.; Borchers, H.-W.; Carezia, A.; Dupuis, P.; Eaton, J.W.; Farhi, E. Package ‘signal version 0.7-7.’; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Kuhn, M. Building predictive models in R using the caret package. J. Stat. Softw. 2008, 28, 1–26. [Google Scholar] [CrossRef]



| Cystoscopy Result | Number of Patients |
|---|---|
| Free | 31 |
| Hyperplasia | 1 |
| Inflammation | 9 |
| Recurrence | 21 |
| Preprocessing Parameter | Variants |
|---|---|
| Spectrum Range | 500~4000 cm−1 |
| 700~900 cm−1 | |
| 700~1800 cm−1 | |
| 2800~3000 cm−1 | |
| Savitzky-Golay Derivative | 0, 1, 2 |
| Normalization | No normalization |
| Amide 1500~1700 cm−1 | |
| Urea 1400~1500 cm−1 | |
| Savitzky-Golay Window Size | 5, 7, 9, 13 |
| Bin size | 1, 2, 3, 5, 10 |
| Model | CV ROC | Test Accuracy | F1 Score | Spectrumrange | SG Derivative | SG Window | Bin Size | Normalization Peak |
|---|---|---|---|---|---|---|---|---|
| cforest | 0.83 | 0.74 | 0.62 | 2800~3000 | 1 | 13 | 1 | urea |
| gbm | 0.81 | 0.79 | 0.67 | 2800~3000 | 1 | 7 | 1 | none |
| ranger | 0.82 | 0.77 | 0.64 | 2800~3000 | 1 | 13 | 1 | urea |
| RRF | 0.82 | 0.81 | 0.71 | 2800~3000 | 1 | 13 | 1 | urea |
| gaussprRadial | 0.46 | 0.92 | 0.86 | 2800~3000 | 0 | 9 | 1 | none |
| LogitBoost | 0.53 | 0.88 | 0.81 | 500~4000 | 1 | 9 | 3 | amide |
| mlp | 0.67 | 0.85 | 0.82 | 2800~3000 | 0 | 7 | 2 | amide |
| rf | 0.42 | 0.92 | 0.84 | 2800~3000 | 0 | 5 | 2 | none |
| svmPoly | 0.7 | 0.85 | 0.76 | 2800~3000 | 2 | 7 | 10 | amide |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Falouji, A.I.; Sabri, D.M.; Lotfi, N.M.; Medany, D.M.; Mohamed, S.A.; Alaa-eldin, M.; Selim, A.M.; El Leithy, A.A.; Kalil, H.; El-Tobgy, A.; et al. Rapid Detection of Recurrent Non-Muscle Invasive Bladder Cancer in Urine Using ATR-FTIR Technology. Molecules 2022, 27, 8890. https://doi.org/10.3390/molecules27248890
El-Falouji AI, Sabri DM, Lotfi NM, Medany DM, Mohamed SA, Alaa-eldin M, Selim AM, El Leithy AA, Kalil H, El-Tobgy A, et al. Rapid Detection of Recurrent Non-Muscle Invasive Bladder Cancer in Urine Using ATR-FTIR Technology. Molecules. 2022; 27(24):8890. https://doi.org/10.3390/molecules27248890
Chicago/Turabian StyleEl-Falouji, Abdullah I., Dalia M. Sabri, Naira M. Lotfi, Doaa M. Medany, Samar A. Mohamed, Mai Alaa-eldin, Amr Mounir Selim, Asmaa A. El Leithy, Haitham Kalil, Ahmed El-Tobgy, and et al. 2022. "Rapid Detection of Recurrent Non-Muscle Invasive Bladder Cancer in Urine Using ATR-FTIR Technology" Molecules 27, no. 24: 8890. https://doi.org/10.3390/molecules27248890
APA StyleEl-Falouji, A. I., Sabri, D. M., Lotfi, N. M., Medany, D. M., Mohamed, S. A., Alaa-eldin, M., Selim, A. M., El Leithy, A. A., Kalil, H., El-Tobgy, A., & Mohamed, A. (2022). Rapid Detection of Recurrent Non-Muscle Invasive Bladder Cancer in Urine Using ATR-FTIR Technology. Molecules, 27(24), 8890. https://doi.org/10.3390/molecules27248890






