Naphthoquine: A Potent Broad-Spectrum Anti-Coronavirus Drug In Vitro
Abstract
:1. Introduction
2. Results
2.1. NPQ Inhibits HCoV-229E and HCoV-OC43 Replication In Vitro
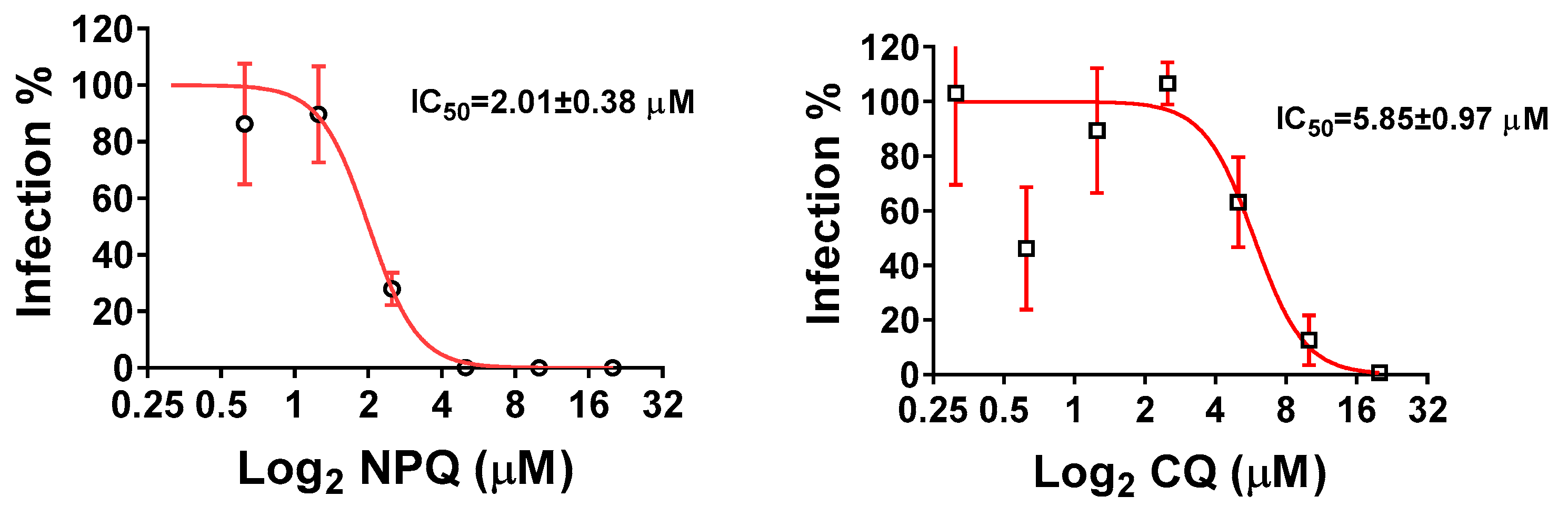
2.2. NPQ Inhibits SARS-CoV-2 Replication In Vitro
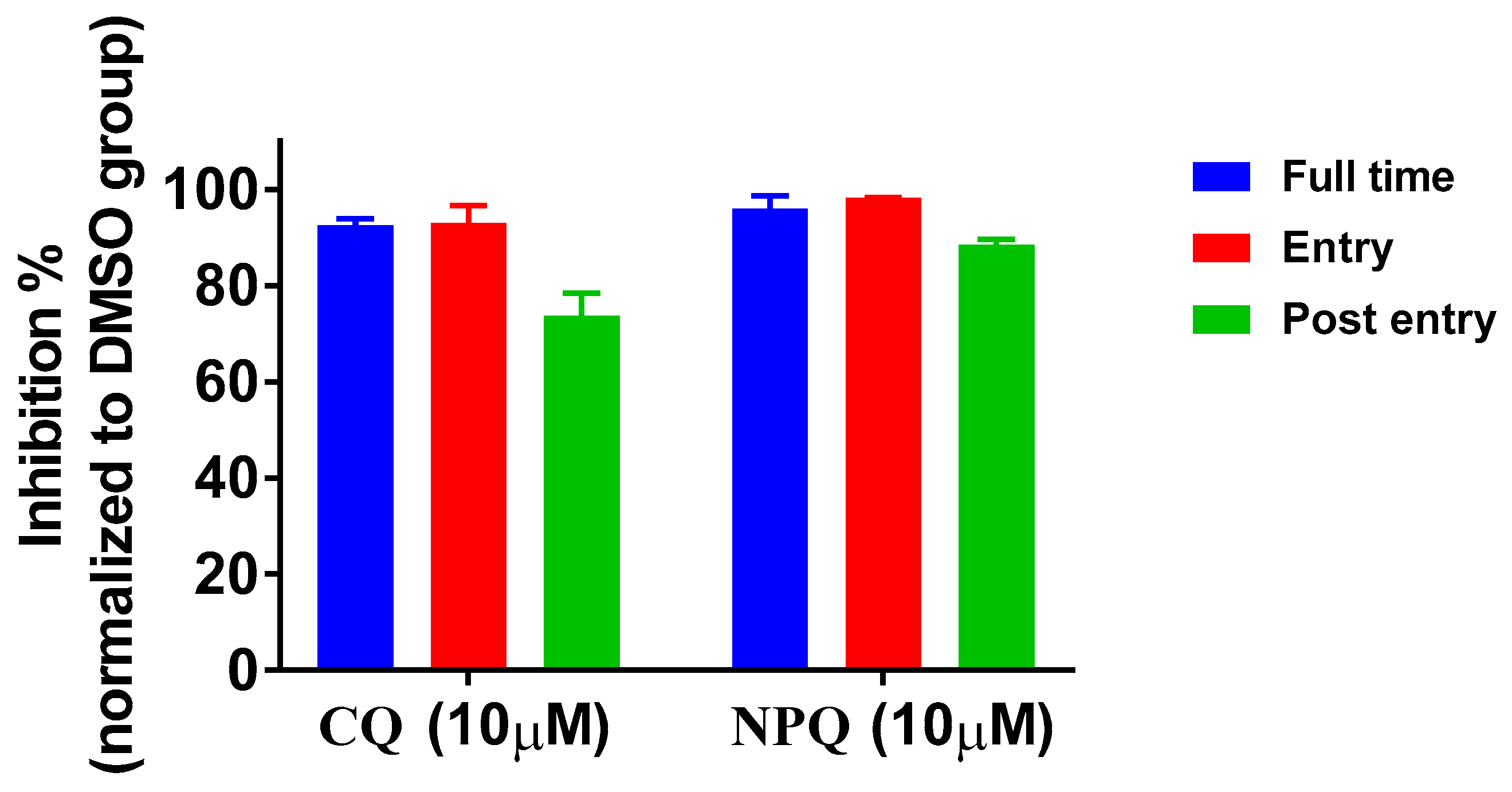
2.3. Time-of-Addition Analysis of NPQ against SARS-CoV-2
3. Discussion
4. Materials and Methods
4.1. Cell Culture
4.2. Reagents
4.3. Viruses
4.4. Cytotoxicity Measurement
4.5. CPE Inhibition Assay in H460 and Huh7 Cells
4.6. Measurement of Viral RNA
4.7. The Anti-SARS-CoV-2 Activity in Vero Cells
4.8. Time-of-Addition Assay
5. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- Cui, J.; Li, F.; Shi, Z.L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 2019, 17, 181–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corman, V.M.; Muth, D.; Niemeyer, D.; Drosten, C. Hosts and sources of endemic human coronaviruses. Adv. Virus Res. 2018, 100, 163–188. [Google Scholar] [PubMed]
- Guarner, J. Three Emerging Coronaviruses in Two Decades. Am. J. Clin. Pathol. 2020, 153, 420–421. [Google Scholar] [CrossRef] [PubMed]
- Pillaiyar, T.; Wendt, L.L.; Manickam, M.; Easwaran, M. The recent outbreaks of human coronaviruses: A medicinal chemistry perspective. Med. Res. Rev. 2021, 41, 72–135. [Google Scholar] [CrossRef] [PubMed]
- The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 2020, 5, 536–544. [CrossRef] [Green Version]
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 23 December 2021).
- Binagwaho, A.; Mathewos, K.; Davis, S. Time for the ethical management of COVID-19 vaccines. Lancet Glob. Health 2021, 9, e1169–e1171. [Google Scholar] [CrossRef]
- Aryeetey, E.; Engebretsen, E.; Gornitzka, A.; Maassen, P.; Stolen, S. A step backwards in the fight against global vaccine inequities. Lancet 2021, 397, 23–24. [Google Scholar] [CrossRef]
- Asundi, A.; O’Leary, C.; Bhadelia, N. Global COVID-19 vaccine inequity: The scope, the impact, and the challenges. Cell Host Microbe 2021, 29, 1036–1039. [Google Scholar] [CrossRef]
- Dolgin, E. The race for antiviral drugs to beat COVID—and the next pandemic. Nature 2021, 592, 340–343. [Google Scholar] [CrossRef]
- Pushpakom, S.; Iorio, F.; Eyers, P.A.; Escott, K.J.; Hopper, S.; Wells, A.; Doig, A.; Guilliams, T.; Latimer, J.; McNamee, C.; et al. Drug repurposing: Progress, challenges and recommendations. Nat. Rev. Drug. Discov. 2019, 18, 41–58. [Google Scholar] [CrossRef]
- Agrawal, P. Advantages and challenges in drug Re-profiling. J. Pharmacovigil. 2015, s2, e002. [Google Scholar] [CrossRef]
- Touret, F.; Gilles, M.; Barral, K.; Nougairède, A.; van Helden, J.; Decroly, E.; de Lamballerie, X.; Coutard, B. In vitro screening of a FDA approved chemical library reveals potential inhibitors of SARS-CoV-2 replication. Sci. Rep. 2020, 10, 13093. [Google Scholar] [CrossRef] [PubMed]
- Yousefifard, M.; Zali, A.; Mohamed Ali, K.; MadaniNeishaboori, A.; Zarghi, A.; Hosseini, M.; Safari, S. Antiviral therapy in management of COVID-19: A systematic review on current evidence. Arch. Acad. Emerg. Med. 2020, 8, e45. [Google Scholar] [PubMed]
- Liu, J.; Cao, R.; Xu, M.; Wang, X.; Zhang, H.; Hu, H.; Li, Y.; Hu, Z.; Zhong, W.; Wang, M. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. 2020, 6, 16. [Google Scholar] [CrossRef] [Green Version]
- Devaux, C.A.; Rolain, J.M.; Colson, P.; Raoult, D. New insights on the antiviral effects of chloroquine against coronavirus: What to expect for COVID-19? Int. J. Antimicrob. Agents 2020, 55, 105938. [Google Scholar] [CrossRef]
- Shionoya, K.; Yamasaki, M.; Iwanami, S.; Ito, Y.; Fukushi, S.; Ohashi, H.; Saso, W.; Tanaka, T.; Aoki, S.; Kuramochi, K.; et al. Mefloquine, a Potent Anti-severe Acute Respiratory Syndrome-Related Coronavirus 2 (SARS-CoV-2) Drug as an Entry Inhibitor in vitro. Front. Microbiol. 2021, 12, 651403. [Google Scholar] [CrossRef]
- Cortegiani, A.; Ippolito, M.; Ingoglia, G.; Iozzo, P.; Giarratano, A.; Einav, S. Update I. A systematic review on the efficacy and safety of chloroquine/hydroxychloroquine for COVID-19. J. Crit. Care 2020, 59, 176–190. [Google Scholar] [CrossRef]
- Doyno, C.; Sobieraj, D.M.; Baker, W.L. Toxicity of chloroquine and hydroxychloroquine following therapeutic use or overdose. Clin. Toxicol. 2021, 59, 12–23. [Google Scholar] [CrossRef]
- Geleris, J.; Sun, Y.; Platt, J.; Zucker, J.; Baldwin, M.; Hripcsak, G.; Labella, A.; Manson, D.K.; Kubin, C.; Barr, R.G.; et al. Observational Study of Hydroxychloroquine in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2020, 382, 2411–2418. [Google Scholar] [CrossRef]
- Tang, W.; Cao, Z.; Han, M.; Wang, Z.; Chen, J.; Sun, W.; Wu, Y.; Xiao, W.; Liu, S.; Chen, E.; et al. Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: Open label, randomised controlled trial. BMJ 2020, 369, m1849. [Google Scholar] [CrossRef]
- Funnell, S.; Dowling, W.E.; Muñoz-Fontela, C.; Gsell, P.S.; Ingber, D.E.; Hamilton, G.A.; Delang, L.; Rocha-Pereira, J.; Kaptein, S.; Dallmeier, K.H.; et al. Emerging preclinical evidence does not support broad use of hydroxychloroquine in COVID-19 patients. Nat. Commun. 2020, 11, 4253. [Google Scholar] [CrossRef]
- Moore, B.R.; Laman, M.; Salman, S.; Batty, K.T.; Page-Sharp, M.; Hombhanje, F.; Manning, L.; Davis, T.M. Naphthoquine: An Emerging Candidate for Artemisinin Combination Therapy. Drugs 2016, 76, 789–804. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Wang, J.; Liu, H.; Zhao, Y.; Lakshmi, S.; Li, X.; Nie, R.; Li, C.; Wang, H.; Cao, Y.; et al. Efficacy and Safety of a Naphthoquine-Azithromycin Coformulation for Malaria Prophylaxis in Southeast Asia: A Phase 3, Double-blind, Randomized, Placebo-controlled Trial. Clin. Infect. Dis. 2021, 73, e2470–e2476. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Cao, R.; Zhang, L.; Yang, X.; Liu, J.; Xu, M.; Shi, Z.; Hu, Z.; Zhong, W.; Xiao, G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020, 30, 269–271. [Google Scholar] [CrossRef]
- Gendrot, M.; Andreani, J.; Boxberger, M.; Jardot, P.; Fonta, I.; Le Bideau, M.; Duflot, I.; Mosnier, J.; Rolland, C.; Bogreau, H.; et al. Antimalarial drugs inhibit the replication of SARS-CoV-2: An in vitro evaluation. Travel Med. Infect. Dis. 2020, 37, 101873. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a ClinicallyProven Protease Inhibitor. Cell 2020, 181, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Wei, X.L.; Su, R.B.; Wang, J.Y.; Shi, Y.L. Effect of complex naphthoquine on DNA content and pH value of the lysosome in Plasmodium berghei. Bull. Acad. Mil. Med. Sci. 2002, 26, 191. [Google Scholar]
- Wong, R.P.; Lautu, D.; Tavul, L.; Hackett, S.L.; Siba, P.; Karunajeewa, H.A.; Ilett, K.F.; Mueller, I.; Davis, T.M. In vitro sensitivity of Plasmodium falciparum to conventional and novel antimalarial drugs in Papua New Guinea. Trop. Med. Int. Health 2010, 15, 342–349. [Google Scholar] [CrossRef]
- Vincent, M.J.; Bergeron, E.; Benjannet, S.; Erickson, B.R.; Rollin, P.; Ksiazek, T.G.; Seidah, N.G.; Nichol, S.T. Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol. J. 2005, 2, 69. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.Y.; Zuo, B.; Xu, Z.H.; Sun, G.Z.; Zhang, M.; Wang, C.E.; Liu, C.; Lv, F.S.; Sun, Z.W.; Hong, S.F. Long-term toxicity of co-naphthoquine in beagle dogs. Bull. Acad. Mil. Med. Sci. 2003, 27, 196–198. [Google Scholar]
- Batty, K.T.; Salman, S.; Moore, B.R.; Benjamin, J.; Lee, S.T.; Page-Sharp, M.; Pitus, N.; Ilett, K.F.; Mueller, I.; Hombhanje, F.W.; et al. Artemisinin-naphthoquine combination therapy for uncomplicated pediatric malaria: A pharmacokinetic study. Antimicrob. Agents Chemother. 2012, 56, 2472–2484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J.; Luo, P.; Shi, K.; Lin, Y.; Wang, J. Observation on malaria prophylaxis using naphthoquine phosphate. Chin. J. Parasitol. Parasit. Dis. 1998, 16, 236. [Google Scholar]
- Yang, H.; Li, X.; Yang, P.; Li, C.; Wu, C.; Zhang, Z.; Gao, B. Preventive effect on naphthoquine against vivax malaria and drug resistant falciparum malaria in Yunnan, China. Chin. J. Parasit. Dis. Control 2003, 16, 137–139. [Google Scholar]



| Compounds | CC50 (µM) | IC50 (µM) | SI |
|---|---|---|---|
| NPQ | 11.50 ± 6.19 | 2.05 ± 1.44 | 5.61 |
| CQ | 71.76 ± 35.59 | 8.74 ± 7.27 | 8.21 |
| RBV | 409.48 ± 0 | 15.43 ± 5.57 | 26.54 |
| Compounds | CC50 (µM) | IC50 (µM) | SI |
|---|---|---|---|
| NPQ | >82.52 | 5.83 ± 0.74 | >14.15 |
| CQ | >96.92 | 3.16 ± 0.60 | >30.67 |
| RBV | 317.80 ± 0 | 20.72 ± 7.86 | 15.34 |
| Compounds | CC50 (µM) 1 | IC50 (µM) | SI |
|---|---|---|---|
| NPQ | 13.50 ± 0.20 | 2.01 ± 0.38 | 6.72 |
| CQ | 76.58 ± 0.02 | 5.85 ± 0.97 | 13.09 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, Y.; Deng, Y.; Wang, H.; Bei, Z.; Gu, H.; Zhao, H.; Wang, H.; Zhang, D.; Xu, L.; Wang, B.; et al. Naphthoquine: A Potent Broad-Spectrum Anti-Coronavirus Drug In Vitro. Molecules 2022, 27, 712. https://doi.org/10.3390/molecules27030712
Song Y, Deng Y, Wang H, Bei Z, Gu H, Zhao H, Wang H, Zhang D, Xu L, Wang B, et al. Naphthoquine: A Potent Broad-Spectrum Anti-Coronavirus Drug In Vitro. Molecules. 2022; 27(3):712. https://doi.org/10.3390/molecules27030712
Chicago/Turabian StyleSong, Yabin, Yongqiang Deng, Huiqiang Wang, Zhuchun Bei, Hongjing Gu, Hui Zhao, Hong Wang, Dongna Zhang, Likun Xu, Baogang Wang, and et al. 2022. "Naphthoquine: A Potent Broad-Spectrum Anti-Coronavirus Drug In Vitro" Molecules 27, no. 3: 712. https://doi.org/10.3390/molecules27030712
APA StyleSong, Y., Deng, Y., Wang, H., Bei, Z., Gu, H., Zhao, H., Wang, H., Zhang, D., Xu, L., Wang, B., Li, Y., & Wang, H. (2022). Naphthoquine: A Potent Broad-Spectrum Anti-Coronavirus Drug In Vitro. Molecules, 27(3), 712. https://doi.org/10.3390/molecules27030712






